Does Vaccine Confidence Mediate the Relationship between Vaccine Literacy and Influenza Vaccination? Exploring Determinants of Vaccination among Staff Members of Nursing Homes in Tuscany, Italy, during the COVID-19 Pandemic
Abstract
:1. Introduction
2. Materials and Methods
2.1. Questionnaire
2.2. HLVa-IT
2.3. Vaccine Confidence Index
- Influenza is a serious illness (A1)
- The influenza vaccine is effective (A2)
- Healthcare workers must get vaccinated (A3)
- By getting vaccinated, I protect people close to me from influenza (A4)
- It is better to contract influenza than to get the vaccination (B1)
- Influenza vaccines have serious side effects (B2)
- Vaccines can cause influenza (B3)
- Opposed to vaccination (B4)
2.4. Statistical Analysis
3. Results
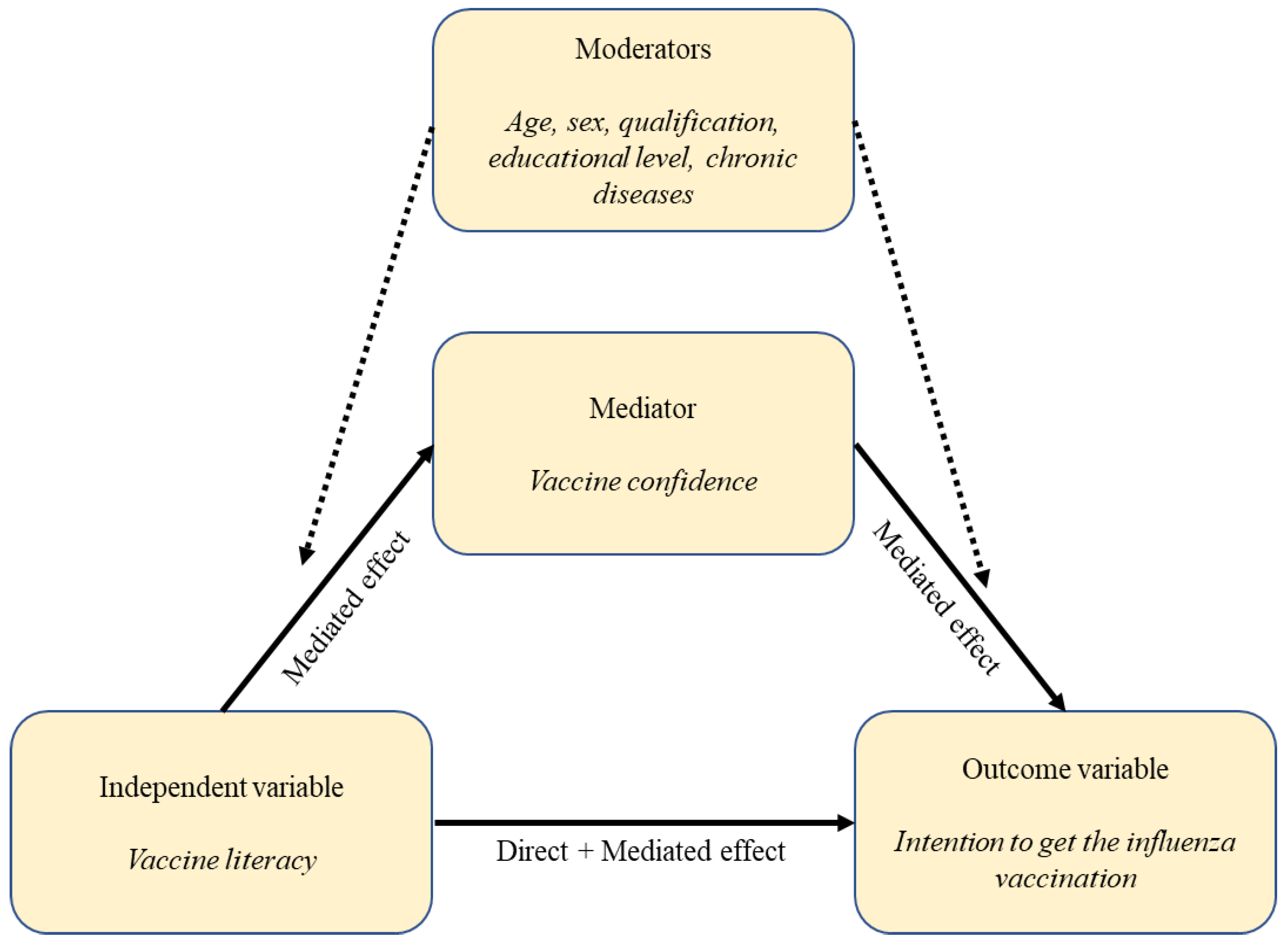
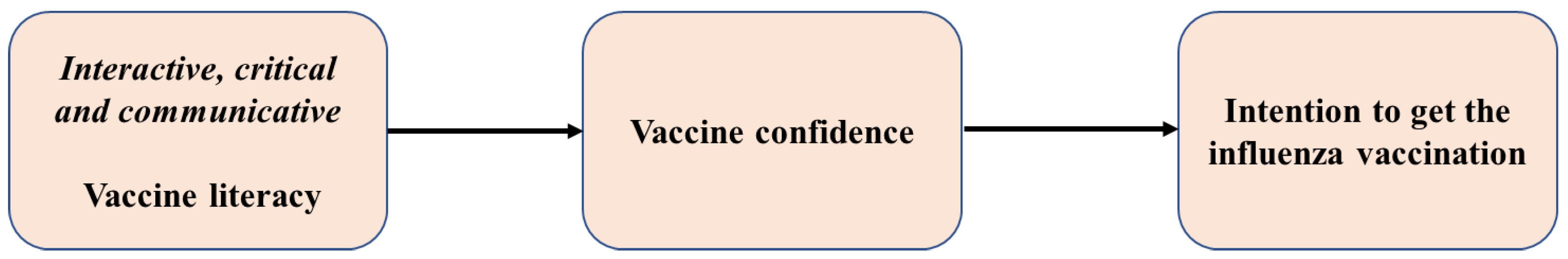
3.1. The Mediator Model
3.1.1. Association between Vaccine Literacy and Vaccine Confidence (Mediator Model)
3.1.2. Association between Intention to Get Vaccinated, Vaccine Literacy, and Vaccine Confidence (Outcome Models and Mediation Analysis)
- For staff members with at least one risk condition, the total and mediated effects were significant only when considering high or medium HLVa-IT-ICC subscale scores compared to low scores;
- For staff members without risk conditions, the total and mediated effects were significant only when comparing high subscale scores to medium or low scores.
| Moderated Mediation Analysis * | Risk Conditions (N = 530) | No Risk Conditions (N = 493) | ||||||
|---|---|---|---|---|---|---|---|---|
| High or Medium vs. Low HLVa-IT-ICC | OR | 95% CI | p | OR | 95% CI | p | ||
| Total Effect | 1.79 | 1.18 | 2.71 | 0.006 | 1.48 | 0.98 | 2.25 | 0.064 |
| Mediated effect | 1.94 | 1.50 | 2.52 | <0.001 | 1.82 | 1.37 | 2.41 | <0.001 |
| Direct effect | 0.92 | 0.68 | 1.24 | 0.583 | 0.82 | 0.66 | 1.01 | 0.058 |
| Moderated mediation analysis * | Risk conditions (N = 530) | No Risk conditions (N = 493) | ||||||
| High vs. Median or Low HLVa-IT-ICC | OR | 95% CI | p | OR | 95% CI | p | ||
| Total Effect | 1.33 | 0.98 | 1.80 | 0.072 | 2.19 | 1.51 | 3.17 | <0.001 |
| Mediated effect | 1.53 | 1.24 | 1.89 | <0.001 | 1.94 | 1.52 | 2.48 | <0.001 |
| Direct effect | 0.87 | 0.69 | 1.08 | 0.209 | 1.12 | 0.86 | 1.47 | 0.394 |
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Influenza Seasonal. Available online: https://www.who.int/health-topics/influenza-seasonal#tab=tab_1 (accessed on 30 June 2023).
- Lansbury, L.E.; Brown, C.S.; Nguyen-Van-Tam, J.S. Influenza in Long-Term Care Facilities. Influenza Other Respir. Viruses 2017, 11, 356–366. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Q&A: Influenza in the Context of COVID-19. Available online: https://www.who.int/europe/news-room/questions-and-answers/item/q-a--influenza-in-the-context-of-covid-19 (accessed on 30 June 2020).
- Khorramdelazad, H.; Kazemi, M.H.; Najafi, A.; Keykhaee, M.; Zolfaghari Emameh, R.; Falak, R. Immunopathological Similarities between COVID-19 and Influenza: Investigating the Consequences of Co-Infection. Microb. Pathog. 2021, 152, 104554. [Google Scholar] [CrossRef] [PubMed]
- Gostin, L.O.; Salmon, D.A. The Dual Epidemics of COVID-19 and Influenza: Vaccine Acceptance, Coverage, and Mandates. JAMA 2020, 324, 335. [Google Scholar] [CrossRef] [PubMed]
- Frentzel, E.; Jump, R.L.P.; Archbald-Pannone, L.; Nace, D.A.; Schweon, S.J.; Gaur, S.; Naqvi, F.; Pandya, N.; Mercer, W. Recommendations for Mandatory Influenza Vaccinations for Health Care Personnel From AMDA’s Infection Advisory Subcommittee. J. Am. Med. Dir. Assoc. 2020, 21, 25–28.e2. [Google Scholar] [CrossRef]
- Monto, A.S.; Rotthoff, J.; Teich, E.; Herlocher, M.L.; Truscon, R.; Yen, H.-L.; Elias, S.; Ohmit, S.E. Detection and Control of Influenza Outbreaks in Well-Vaccinated Nursing Home Populations. Clin. Infect. Dis. 2004, 39, 459–464. [Google Scholar] [CrossRef]
- Smetana, J.; Chlibek, R.; Shaw, J.; Splino, M.; Prymula, R. Influenza Vaccination in the Elderly. Hum. Vaccines Immunother. 2018, 14, 540–549. [Google Scholar] [CrossRef]
- Dolan, G.P.; Harris, R.C.; Clarkson, M.; Sokal, R.; Morgan, G.; Mukaigawara, M.; Horiuchi, H.; Hale, R.; Stormont, L.; Béchard-Evans, L.; et al. Vaccination of Healthcare Workers to Protect Patients at Increased Risk of Acute Respiratory Disease: Summary of a Systematic Review. Influenza Resp. Viruses 2013, 7, 93–96. [Google Scholar] [CrossRef]
- Vaux, S.; Fonteneau, L.; Venier, A.-G.; Gautier, A.; Soing Altrach, S.; Parneix, P.; Lévy-Bruhl, D. Influenza Vaccination Coverage of Professionals Working in Nursing Homes in France and Related Determinants, 2018–2019 Season: A Cross-Sectional Survey. BMC Public Health 2022, 22, 1049. [Google Scholar] [CrossRef]
- Borgey, F.; Henry, L.; Lebeltel, J.; Lescure, P.; Le Coutour, X.; Vabret, A.; Verdon, R.; Thibon, P. Effectiveness of an Intervention Campaign on Influenza Vaccination of Professionals in Nursing Homes: A Cluster-Randomized Controlled Trial. Vaccine 2019, 37, 1260–1265. [Google Scholar] [CrossRef]
- Lorini, C.; Collini, F.; Gasparini, F.; Paolini, D.; Grazzini, M.; Ierardi, F.; Galletti, G.; Zanobini, P.; Gemmi, F.; Bonaccorsi, G. Health Literacy, Vaccine Confidence and Influenza Vaccination Uptake among Nursing Home Staff: A Cross-Sectional Study Conducted in Tuscany. Vaccines 2020, 8, 154. [Google Scholar] [CrossRef]
- Lorini, C.; Ierardi, F.; Gatteschi, C.; Galletti, G.; Collini, F.; Peracca, L.; Zanobini, P.; Gemmi, F.; Bonaccorsi, G. Promoting Influenza Vaccination among Staff of Nursing Homes According to Behavioral Insights: Analyzing the Choice Architecture during a Nudge-Based Intervention. Vaccines 2020, 8, 600. [Google Scholar] [CrossRef]
- World Health Organization. Report of the SAGE Working Group on Vaccine Hesitancy. Available online: https://www.who.int/immunization/sage/meetings/2014/october/1_Report_WORKING_GROUP_vaccine_hesitancy_final.pdf (accessed on 30 June 2023).
- Moretti, F.; Visentin, D.; Bovolenta, E.; Rimondini, M.; Majori, S.; Mazzi, M.; Poli, A.; Tardivo, S.; Torri, E. Attitudes of Nursing Home Staff towards Influenza Vaccination: Opinions and Factors Influencing Hesitancy. IJERPH 2020, 17, 1851. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, N.E. Vaccine Hesitancy: Definition, Scope and Determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef] [PubMed]
- Berkman, N.D.; Sheridan, S.L.; Donahue, K.E.; Halpern, D.J.; Crotty, K. Low health literacy and health outcomes: An updated systematic review. Ann. Intern. Med. 2011, 155, 97–107. [Google Scholar] [CrossRef] [PubMed]
- Siena, L.M.; Isonne, C.; Sciurti, A.; De Blasiis, M.R.; Migliara, G.; Marzuillo, C.; De Vito, C.; Villari, P.; Baccolini, V. The Association of Health Literacy with Intention to Vaccinate and Vaccination Status: A Systematic Review. Vaccines 2022, 10, 1832. [Google Scholar] [CrossRef]
- Cadeddu, C.; Regazzi, L.; Bonaccorsi, G.; Rosano, A.; Unim, B.; Griebler, R.; Link, T.; De Castro, P.; D’Elia, R.; Mastrilli, V.; et al. The Determinants of Vaccine Literacy in the Italian Population: Results from the Health Literacy Survey 2019. Int. J. Environ. Res. Public Health 2022, 19, 4429. [Google Scholar] [CrossRef] [PubMed]
- Ratzan, S.C. Vaccine Literacy: A New Shot for Advancing Health. J. Health Commun. 2011, 16, 227–229. [Google Scholar] [CrossRef]
- Biasio, L.R. Vaccine Literacy Is Undervalued. Hum. Vaccines Immunother. 2019, 15, 2552–2553. [Google Scholar] [CrossRef]
- Lorini, C.; Del Riccio, M.; Zanobini, P.; Biasio, L.R.; Bonanni, P.; Giorgetti, D.; Ferro Allodola, V.; Guazzini, A.; Maghrebi, O.; Lastrucci, V.; et al. Vaccination as a social practice: Towards a definition of personal, community, population, and organizational vaccine literacy. BMC Public. Health. 2023, 23, 1501. [Google Scholar] [CrossRef]
- Ishikawa, H.; Takeuchi, T.; Yano, E. Measuring Functional, Communicative, and Critical Health Literacy Among Diabetic Patients. Diabetes Care 2008, 31, 874–879. [Google Scholar] [CrossRef]
- Nutbeam, D. Health Literacy as a Public Health Goal: A Challenge for Contemporary Health Education and Communication Strategies into the 21st Century. Health Promot. Int. 2000, 15, 259–267. [Google Scholar] [CrossRef]
- Biasio, L.R.; Giambi, C.; Fadda, G.; Lorini, C.; Bonaccorsi, G.; D’Ancona, F. Validation of an Italian tool to assess vaccine literacy in adulthood vaccination: A pilot study. Ann. Ig. 2020, 32, 205–222. [Google Scholar] [CrossRef] [PubMed]
- Lorini, C.; Collini, F.; Galletti, G.; Ierardi, F.; Forni, S.; Gatteschi, C.; Gemmi, F.; Stacchini, L.; Papini, S.; Velpini, B.; et al. Vaccine Literacy and Source of Information about Vaccination among Staff of Nursing Homes: A Cross-Sectional Survey Conducted in Tuscany (Italy). Vaccines 2022, 10, 682. [Google Scholar] [CrossRef] [PubMed]
- Paoli, S.; Lorini, C.; Puggelli, F.; Sala, A.; Grazzini, M.; Paolini, D.; Bonanni, P.; Bonaccorsi, G. Assessing Vaccine Hesitancy among Healthcare Workers: A Cross-Sectional Study at an Italian Paediatric Hospital and the Development of a Healthcare Worker’s Vaccination Compliance Index. Vaccines 2019, 7, 201. [Google Scholar] [CrossRef] [PubMed]
- Larson, H.J.; de Figueiredo, A.; Karafillakis, E.; Rawal, M. State of Vaccine Confidence in the EU 2018. Available online: https://health.ec.europa.eu/system/files/2018-11/2018_vaccine_confidence_en_0.pdf (accessed on 30 June 2023).
- Larson, H.J.; Schulz, W.S.; Tucker, J.D.; Smith, D.M.D. Measuring Vaccine Confidence: Introducing a Global Vaccine Confidence Index. PLoS Curr. 2015, 7, e033245. [Google Scholar] [CrossRef]
- Karlsson, L.C.; Lewandowsky, S.; Antfolk, J.; Salo, P.; Lindfelt, M.; Oksanen, T.; Kivimäki, M.; Soveri, A. The Association between Vaccination Confidence, Vaccination Behavior, and Willingness to Recommend Vaccines among Finnish Healthcare Workers. PLoS ONE 2019, 14, e0224330. [Google Scholar] [CrossRef]
- Paterson, P.; Meurice, F.; Stanberry, L.R.; Glismann, S.; Rosenthal, S.L.; Larson, H.J. Vaccine Hesitancy and Healthcare Providers. Vaccine 2016, 34, 6700–6706. [Google Scholar] [CrossRef]
- Toh, M.P.; Kannan, P.; Chen, Y.; Chng, F.L.; Tang, W.E. Healthcare workers and H1N1 vaccination: Does having a chronic disease make a difference? Vaccine 2012, 30, 1064–1070. [Google Scholar] [CrossRef]
- Singh, P.; Dhalaria, P.; Kashyap, S.; Soni, G.K.; Nandi, P.; Ghosh, S.; Mohapatra, M.K.; Rastogi, A.; Prakash, D. Strategies to Overcome Vaccine Hesitancy: A Systematic Review. Syst. Rev. 2022, 11, 78. [Google Scholar] [CrossRef]
- Hollmeyer, H.G.; Hayden, F.; Poland, G.; Buchholz, U. Influenza Vaccination of Health Care Workers in Hospitals—A Review of Studies on Attitudes and Predictors. Vaccine 2009, 27, 3935–3944. [Google Scholar] [CrossRef]
- Abramson, Z.H.; Levi, O. Influenza Vaccination among Primary Healthcare Workers. Vaccine 2008, 26, 2482–2489. [Google Scholar] [CrossRef] [PubMed]
- Mehta, M.; Pastor, C.A.; Shah, B. Achieving Optimal Influenza Vaccination Rates: A Survey-Based Study of Healthcare Workers in an Urban Hospital. J. Hosp. Infect. 2008, 70, 76–79. [Google Scholar] [CrossRef] [PubMed]
- Esposito, S.; Tremolati, E.; Bellasio, M.; Chiarelli, G.; Marchisio, P.; Tiso, B.; Mosca, F.; Pardi, G.; Principi, N. Attitudes and Knowledge Regarding Influenza Vaccination among Hospital Health Workers Caring for Women and Children. Vaccine 2007, 25, 5283–5289. [Google Scholar] [CrossRef] [PubMed]
- Dey, P.; Ahuja, A.; Panwar, J.; Choudhary, P.; Rani, S.; Kaur, M.; Sharma, A.; Kaur, J.; Yadav, A.K.; Sood, V.; et al. Immune Control of Avian Influenza Virus Infection and Its Vaccine Development. Vaccines 2023, 11, 593. [Google Scholar] [CrossRef]
- Krammer, F.; Schultz-Cherry, S. We need to keep an eye on avian influenza. Nat. Rev. Immunol. 2023, 23, 267–268. [Google Scholar] [CrossRef]
- Li, C.; Su, Z.; Chen, Z.; Cao, J.; Xu, F. Trust of Healthcare Workers in Vaccines May Enhance the Public’s Willingness to Vaccinate. Hum. Vaccines Immunother. 2022, 18, 2158669. [Google Scholar] [CrossRef] [PubMed]
| Variables | Sample | Vaccination Intention | ||||
|---|---|---|---|---|---|---|
| N | % | N | % of Sample | pc | ||
| Total | 1794 | 100 | 995 | 55.5% | ||
| Sex | Males | 230 | 12.8% | 138 | 60.0% | 0.163 |
| Females | 1548 | 86.3% | 853 | 55.1% | ||
| NA b | 16 | 0.9% | 4 | 25.0% | ||
| Age (years) | <40 | 551 | 30.7% | 282 | 51.2% | <0.001 |
| 40–49 | 519 | 28.9% | 261 | 50.3% | ||
| 50–59 | 506 | 28.2% | 310 | 61.3% | ||
| 60+ | 218 | 12.2% | 142 | 65.1% | ||
| Living with | Children of younger than 9 years of age | 357 | 19.9% | 200 | 56.0% | 0.525 |
| Elderly people (>65 years) | 358 | 20.0% | 224 | 62.6% | 0.001 | |
| People with chronic diseases | 285 | 15.9% | 196 | 68.8% | <0.001 | |
| At least one of the previously listed conditions | 759 | 42.3% | 452 | 59.6% | 0.003 | |
| Qualification | Clinical staff | 441 | 24.6% | 265 | 60.1% | 0.021 |
| Assistants/aides | 1042 | 58.1% | 551 | 52.9% | ||
| Other non-clinical staff | 285 | 15.9% | 167 | 58.6% | ||
| NA b | 26 | 1.4% | 12 | 46.2% | ||
| Suffering from | Cardiovascular chronic diseases | 35 | 2.0% | 24 | 68.6% | 0.115 |
| Respiratory chronic diseases | 137 | 7.6% | 91 | 66.4% | 0.007 | |
| Renal chronic diseases | 9 | 0.5% | 8 | 88.9% | 0.043 | |
| Diabetes | 31 | 1.7% | 25 | 80.6% | 0.004 | |
| Autoimmune diseases | 108 | 6.0% | 73 | 67.6% | 0.009 | |
| A respiratory infection in the past year | 48 | 2.7% | 36 | 75.0% | 0.006 | |
| At least one of the previously listed diseases | 285 | 15.9% | 189 | 66.3% | <0.001 | |
| Risk condition a | Yes | 890 | 49.6% | 533 | 59.9% | <0.001 |
| No | 818 | 45.6% | 415 | 50.7% | ||
| NA b | 86 | 4.8% | 47 | 54.7% | ||
| Items | N (%) Total: 1794 | ||||
|---|---|---|---|---|---|
| Totally Disagree | Partially Disagree | Partially Agree | Totally Agree | Not Available | |
| Influenza is a risky disease | 82 (4.6) | 179 (10.0) | 1045 (58.2) | 478 (26.6) | 10 (0.6) |
| It is better to get influenza rather than vaccinate myself | 558 (31.1) | 339 (18.9) | 713 (39.7) | 163 (9.1) | 21 (1.2) |
| The influenza vaccine has serious side effects | 554 (30.9) | 412 (23.0) | 686 (38.2) | 121 (6.7) | 21 (1.2) |
| The influenza vaccine can cause influenza disease | 332 (18.5) | 293 (16.3) | 805 (44.9) | 342 (19.1) | 22 (1.2) |
| The influenza vaccine is effective at preventing influenza disease | 73 (4.1) | 150 (8.4) | 889 (49.5) | 670 (3.3) | 12 (0.7) |
| I am against vaccinations | 779 (43.4) | 235 (13.1) | 570 (31.8) | 186 (10.4) | 24 (1.3) |
| Healthcare workers should be vaccinated against influenza | 161 (9.0) | 240 (13.4) | 681 (37.9) | 700 (39.0) | 12 (0.7) |
| By vaccinating myself, I protect the people I come in contact with from influenza | 145 (8.1) | 189 (10.5) | 627 (35) | 819 (45.6) | 14 (0.8) |
| Mediator Model Dependent Variable: Vaccine Confidence * | Total (1023) | Risk Conditions (530) | No Risk Conditions (493) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HLVa-IT-ICC | Coeff. | 95% CI | p | Coeff. | 95% CI | p | Coeff. | 95% CI | p | |||
| Low | 1 | 1 | 1 | |||||||||
| Medium | 0.20 | 0.07 | 0.33 | 0.002 | 0.30 | 0.12 | 0.48 | 0.001 | 0.11 | −0.07 | 0.29 | 0.227 |
| High | 0.54 | 0.42 | 0.67 | <0.001 | 0.59 | 0.41 | 0.78 | <0.001 | 0.50 | 0.32 | 0.68 | <0.001 |
| Outcome model Dependent Variable: Vaccine Intention * | OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | |||
| Vaccine Confidence | 13.32 | 10.12 | 17.53 | <0.001 | 19.85 | 11.67 | 33.77 | <0.001 | 11.40 | 7.11 | 18.27 | <0.001 |
| HLVa-IT-ICC | ||||||||||||
| Low | 1.00 | 1.00 | 1.00 | |||||||||
| Medium | 1.49 | 1.10 | 2.01 | 0.010 | 2.33 | 1.51 | 3.60 | <0.001 | 0.94 | 0.61 | 1.44 | 0.782 |
| High | 1.92 | 1.41 | 2.63 | <0.001 | 2.15 | 1.39 | 3.33 | 0.001 | 1.75 | 1.13 | 2.73 | 0.013 |
| Moderated mediation analysis * | Total (1023) | Risk conditions (530) | No Risk conditions (493) | |||||||||
| Medium vs. Low HLVa-IT-ICC | OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | |||
| Total Effect | 1.49 | 1.13 | 1.96 | 0.005 | 2.16 | 1.45 | 3.21 | <0.001 | 1.00 | 0.67 | 1.47 | 0.982 |
| Mediated effect | 1.37 | 1.14 | 1.65 | 0.001 | 1.62 | 1.23 | 2.13 | 0.001 | 1.15 | 0.94 | 1.42 | 0.167 |
| Direct effect | 1.08 | 0.87 | 1.35 | 0.480 | 1.33 | 0.96 | 1.86 | 0.089 | 0.86 | 0.61 | 1.21 | 0.393 |
| High vs. Low HLVa-IT-ICC | OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | |||
| Total Effect | 1.98 | 1.47 | 2.68 | <0.001 | 2.21 | 1.34 | 3.65 | 0.002 | 1.78 | 1.21 | 2.62 | 0.003 |
| Mediated effect | 2.22 | 1.80 | 2.73 | <0.001 | 2.40 | 1.67 | 3.46 | <0.001 | 2.05 | 1.59 | 2.65 | <0.001 |
| Direct effect | 0.89 | 0.72 | 1.10 | 0.294 | 0.92 | 0.68 | 1.25 | 0.593 | 0.87 | 0.62 | 1.22 | 0.411 |
| High vs. Medium HLVa-IT-ICC | OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | |||
| Total Effect | 1.34 | 0.99 | 1.80 | 0.057 | 1.03 | 0.62 | 1.71 | 0.922 | 1.79 | 1.28 | 2.50 | 0.001 |
| Mediated effect | 1.59 | 1.28 | 1.98 | <0.001 | 1.40 | 0.99 | 1.96 | 0.055 | 1.83 | 1.42 | 2.36 | <0.001 |
| Direct effect | 0.84 | 0.67 | 1.05 | 0.120 | 0.74 | 0.54 | 1.00 | 0.052 | 0.98 | 0.73 | 1.32 | 0.888 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Collini, F.; Bonaccorsi, G.; Del Riccio, M.; Bruschi, M.; Forni, S.; Galletti, G.; Gemmi, F.; Ierardi, F.; Lorini, C. Does Vaccine Confidence Mediate the Relationship between Vaccine Literacy and Influenza Vaccination? Exploring Determinants of Vaccination among Staff Members of Nursing Homes in Tuscany, Italy, during the COVID-19 Pandemic. Vaccines 2023, 11, 1375. https://doi.org/10.3390/vaccines11081375
Collini F, Bonaccorsi G, Del Riccio M, Bruschi M, Forni S, Galletti G, Gemmi F, Ierardi F, Lorini C. Does Vaccine Confidence Mediate the Relationship between Vaccine Literacy and Influenza Vaccination? Exploring Determinants of Vaccination among Staff Members of Nursing Homes in Tuscany, Italy, during the COVID-19 Pandemic. Vaccines. 2023; 11(8):1375. https://doi.org/10.3390/vaccines11081375
Chicago/Turabian StyleCollini, Francesca, Guglielmo Bonaccorsi, Marco Del Riccio, Mario Bruschi, Silvia Forni, Giacomo Galletti, Fabrizio Gemmi, Francesca Ierardi, and Chiara Lorini. 2023. "Does Vaccine Confidence Mediate the Relationship between Vaccine Literacy and Influenza Vaccination? Exploring Determinants of Vaccination among Staff Members of Nursing Homes in Tuscany, Italy, during the COVID-19 Pandemic" Vaccines 11, no. 8: 1375. https://doi.org/10.3390/vaccines11081375
APA StyleCollini, F., Bonaccorsi, G., Del Riccio, M., Bruschi, M., Forni, S., Galletti, G., Gemmi, F., Ierardi, F., & Lorini, C. (2023). Does Vaccine Confidence Mediate the Relationship between Vaccine Literacy and Influenza Vaccination? Exploring Determinants of Vaccination among Staff Members of Nursing Homes in Tuscany, Italy, during the COVID-19 Pandemic. Vaccines, 11(8), 1375. https://doi.org/10.3390/vaccines11081375









