High Levels of Anti-SARS-CoV-2 Receptor-Binding Domain (RBD) Antibodies One Year Post Booster Vaccinations among Hospital Workers in Indonesia: Was the Second Booster Needed?
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethics Approval
2.2. Study Design
2.3. Inclusion Criteria
2.4. Operational Definition
2.5. Antibody Level Examination
2.6. Data Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Novel Coronavirus (COVID-19) Situation. 25 February 2022. Available online: https://covid19.who.int/ (accessed on 25 February 2022).
- Sadarangani, M.; Marchant, A.; Kollmann, T.R. Immunological mechanisms of vaccine-induced protection against COVID-19 in humans. Nat. Rev. Immunol. 2021, 21, 475–484. [Google Scholar] [CrossRef] [PubMed]
- Shrotri, M.; Navaratnam, A.M.D.; Nguyen, V.; Byrne, T.; Geismar, C.; Fragaszy; Beale, S.; Fong, W.L.E.; Patel, P.; Kovar, J.; et al. Spike-antibody waning after second dose of BNT162b2 or ChAdOx1. Lancet 2021, 398, 385–387. [Google Scholar] [CrossRef] [PubMed]
- Zeng, G.; Wu, Q.; Pan, H.; Li, M.; Yang, J.; Wang, L.; Wu, Z.; Jiang, D.; Deng, X.; Chu, K.; et al. Immunogenicity and safety of a third dose of CoronaVac, and immune persistence of a two-dose schedule, in healthy adults: Interim results from two single-centre, double-blind, randomised, placebo-controlled phase 2 clinical trials. Lancet Infect. Dis. 2021, 22, 483–495. [Google Scholar] [CrossRef] [PubMed]
- Minister of Health. Decree of the Minister of Health of the Republic of Indonesia. Technical Instructions for the Implementation of Vaccination in the Context of Combating the 2019 Corona Virus Disease (COVID-19) Pandemic; 2022. Database: Management of Public Information on the Supreme Audit Board. Available online: https://peraturan.bpk.go.id/Home/Details/169665/permenkes-no-10-tahun-2021 (accessed on 20 February 2022).
- Ministry of Health of the Republic of Indonesia. Circular Letter Number Hk.02.02/C/3615/2022 Concerning the 2nd Booster Dose of COVID-19 Vaccination for Health Human Resources. Ministry of Health of the Republic of Indonesia. 28 July 2022. Available online: https://www.kemkes.go.id/downloads/resources/download/lain/Surat-Edaran-Vaksinasi-COVID_19-Dosis-Booster-2.pdf (accessed on 30 July 2022).
- Lo Sasso, B.; Giglio, R.V.; Vidali, M.; Scazzone, C.; Bivona, G.; Gambino, C.M.; Ciaccio, A.M.; Agnello, L.; Ciaccio, M. Evaluation of Anti-SARS-CoV-2 S-RBD IgG Antibodies after COVID-19 mRNA BNT162b2 Vaccine. Diagnostics 2021, 11, 1135. [Google Scholar] [CrossRef] [PubMed]
- Burhan, E.; Agus, D.; Nasution, S.; Eka, G.; Ceva, W.; Adityo, S.; Firdaus, I.; Santoso, A.; Juzar, D.A.; Arif, S.K.; et al. (Eds.) Guidelines for Managing COVID-19, 4th ed.; Organizations 5 Associations: Jakarta, Indonesia, 2022; p. 6. [Google Scholar]
- Infantino, M.; Pieri, M.; Nuccetelli, M.; Grossi, V.; Lari, B.; Tomassetti, F.; Calugi, G.; Pancani, S.; Benucci, M.; Casprini, P.; et al. The WHO International Standard for COVID-19 serological tests: Towards harmonization of anti-spike assays. Int. Immunopharmacol. 2021, 100, 108095. [Google Scholar] [CrossRef] [PubMed]
- Guangzhou Wondfo Biotech Co. (China, Guangzhou). Result Report on Finecare 2019-nCoV RBD Antibody Test; Guangzhou Wondfo Biotech Co.: Guangzhou, China, 2019. [Google Scholar]
- Shurrab, F.M.; Younes, N.; Al-Sadeq, D.W.; Liu, N.; Qotba, H.; Laith, J.; Abu-Raddad, L.J.; Nasrallah, G.K. Performance evaluation of novel fluorescent-based lateral flow immunoassay (LFIA) for rapid detection and quantification of total anti-SARS-CoV-2 S-RBD binding antibodies in infected individu. Int. J. Infect. Dis. 2022, 118, 132–137. [Google Scholar] [CrossRef] [PubMed]
- GenScript. cPass SARS-CoV-2 Neutralization Antibody Detection Kit Instruction for Use; Nanjing GenScript Diagnostics Technology Co., Ltd.: Nanjing, China, 2022. [Google Scholar]
- Dinc, H.O.; Saltoglu, N.; Can, G.; Balkan, I.I.; Budak, B.; Ozbey, D.; Caglar, B.; Karaali, R.; Mete, B.; Tuyji Tok, Y.; et al. Inactive SARS-CoV-2 vaccine generates high antibody responses in healthcare workers with and without prior infection. Vaccine 2022, 40, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Fonseca, M.H.G.; de Souza, T.F.G.; de Carvalho Araújo, F.M.; de Andrade, L.O.M. Dynamics of antibody response to CoronaVac vaccine. J. Med. Virol. 2022, 94, 2139–2148. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, P.; Curtis, N. Factors That Influence the Immune Response to Vaccination. Cli. Microbiol. Rev. 2019, 32, e00084-18. [Google Scholar] [CrossRef] [PubMed]
- Vargas, L.; Valdivieso, N.; Tempio, F.; Simon, V.; Sauma, D.; Valenzuela, L.; Beltrán, C.; Castillo-Delgado, L.; Contreras-Benavides, X.; Acevedo, M.L.; et al. Serological study of CoronaVac vaccine and booster doses in Chile: Immunogenicity and persistence of anti-SARS-CoV-2 spike antibodies. BMC Med. 2022, 20, 216. [Google Scholar] [CrossRef] [PubMed]
- Steensels, D.; Pierlet, N.; Penders, J.; Mesotten, D.; Heylen, L. Comparison of SARS-CoV-2 antibody response following vaccination with BNT162b2 and mRNA-1273. JAMA 2021, 326, 1533–1535. [Google Scholar] [CrossRef] [PubMed]
- Collier, A.Y.; Yu, J.; McMahan, K.; Liu, J.; Chandrashekar, A.; Maron, J.S.; Atyeo, C.; Martinez, D.R.; Ansel, J.L.; Aguayo, R.; et al. Differential kinetics of immune responses elicited by COVID-19 vaccines. N. Engl. J. Med. 2021, 385, 2010–2012. [Google Scholar] [CrossRef] [PubMed]
- Indonesian Health Ministry. National Survey Serology Results. 18 March 2022. Available online: https://covid19.go.id/artikel/2022/03/18/hasil-survei-serologi-COVID-19-di-indonesia-november-desember-2021 (accessed on 24 January 2023).
- Indonesian Health Ministry. Third National Serology Survey. September 2022. Available online: https://www.youtube.com/watch?v=cgESZbe9rC0 (accessed on 24 January 2023).
- Lo Sasso, B.; Agnello, L.; Giglio, R.V.; Gambino, C.M.; Ciaccio, A.M.; Vidali, M.; Ciaccio, M. Longitudinal analysis of anti-SARS-CoV-2 S-RBD IgG antibodies before and after the third dose of the BNT162b2 vaccine. Sci. Rep. 2022, 12, 8679. [Google Scholar] [CrossRef] [PubMed]
- Chakraborty, C.; Sharma, A.R.; Bhattacharya, M.; Lee, S.S. A Detailed Overview of Immune Escape, Antibody Escape, Partial Vaccine Escape of SARS-CoV-2 and Their Emerging Variants with Escape Mutations. Front. Immunol. 2022, 9, 801522. [Google Scholar] [CrossRef] [PubMed]
- Cromer, D.; Steain, M.; Reynaldi, A.; Schlub, T.E.; Wheatley, A.K.; Juno, J.A.; Kent, S.J.; Triccas, J.A.; Khoury, D.S.; Davenport, M.P. Neutralizing antibody titers as predictors of protection against SARS-CoV-2 variants and the impact of boosting: A meta-analysis. Lancet Microbe. 2022, 3, e52–e61. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.J.; Hu, Y.F.; Liu, X.X.; Yao, X.Q.; Wang, Q.F.; Liu, L.P.; Yang, D.; Li, D.J.; Wang, P.G.; He, Q.Q. Household infection: The predominant risk factor for close contacts of patients with COVID-19. Travel Med. Infect. Dis. 2020, 36, 101809. [Google Scholar] [CrossRef] [PubMed]
- Feng, S.; Phillips, D.J.; White, T.; Sayal, H.; Aley, P.K.; Bibi, S.; Dold, C.; Fuskova, M.; Gilbert, S.C.; Hirsch, I.; et al. Correlates of protection against symptomatic and asymptomatic SARS-CoV-2 infection. Nat. Med. 2021, 27, 2032–2040. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Weekly Epidemiological Report. 2 June 2023. Available online: https://www.who.int/publications/i/item/who-wer9822-239-256 (accessed on 5 July 2023).
| Variables | First Survey (n = 570) | Second Survey (n = 355) | Third Survey (n = 330) |
|---|---|---|---|
| Sex | |||
| Male, n (%) | 215 (37.8) | 120 (33.9) | 112 (34.0) |
| Female, n (%) | 355 (62.2) | 235 (66.1) | 218 (66.0) |
| Age category, median (IQR) | |||
| 18–30 years, n (%) | 88 (15.5) | 55 (15.5) | 39 (12) |
| 31–40 years, n (%) | 223 (39.1) | 130(36.7) | 122 (36.9) |
| 41–50 years, n (%) | 118 (20.7) | 72 (20.3) | 70 (21.2) |
| 51–60 years, n (%) | 108 (18.9) | 69 (19.4) | 79 (23.9) |
| >60 years, n (%) | 33 (5.8) | 29 (8.1) ** | 20 (6.0) + |
| Occupation | |||
| Physician, n (%) | 283 (49.6) * | 208 (58.5) ** | 155 (46.9) ^ |
| Nonphysician, n (%) | 287 (50.4) | 147 (41.5) | 175 (53.1) |
| Work zone, n (%) | |||
| In COVID-19 ward | 147 (25.8) * | 119 (33.5) | 102 (30.9) |
| Not in COVID-19 ward | 254 (44.5) | 155 (43.7) ** | 134 (40.6) + |
| Administrative work | 169 (29.7) * | 81 (22.8) | 94 (28.5) |
| History of close contact with confirmed case, n (%) | 210 (36.8) * | 15 (4.2) ** | 68 (20) + |
| Last COVID-19 infection (having previous COVID-19 infection in between surveys), n (%) | 127 (22.2) * | 34 (9.5) ** | 124 (37.5) + |
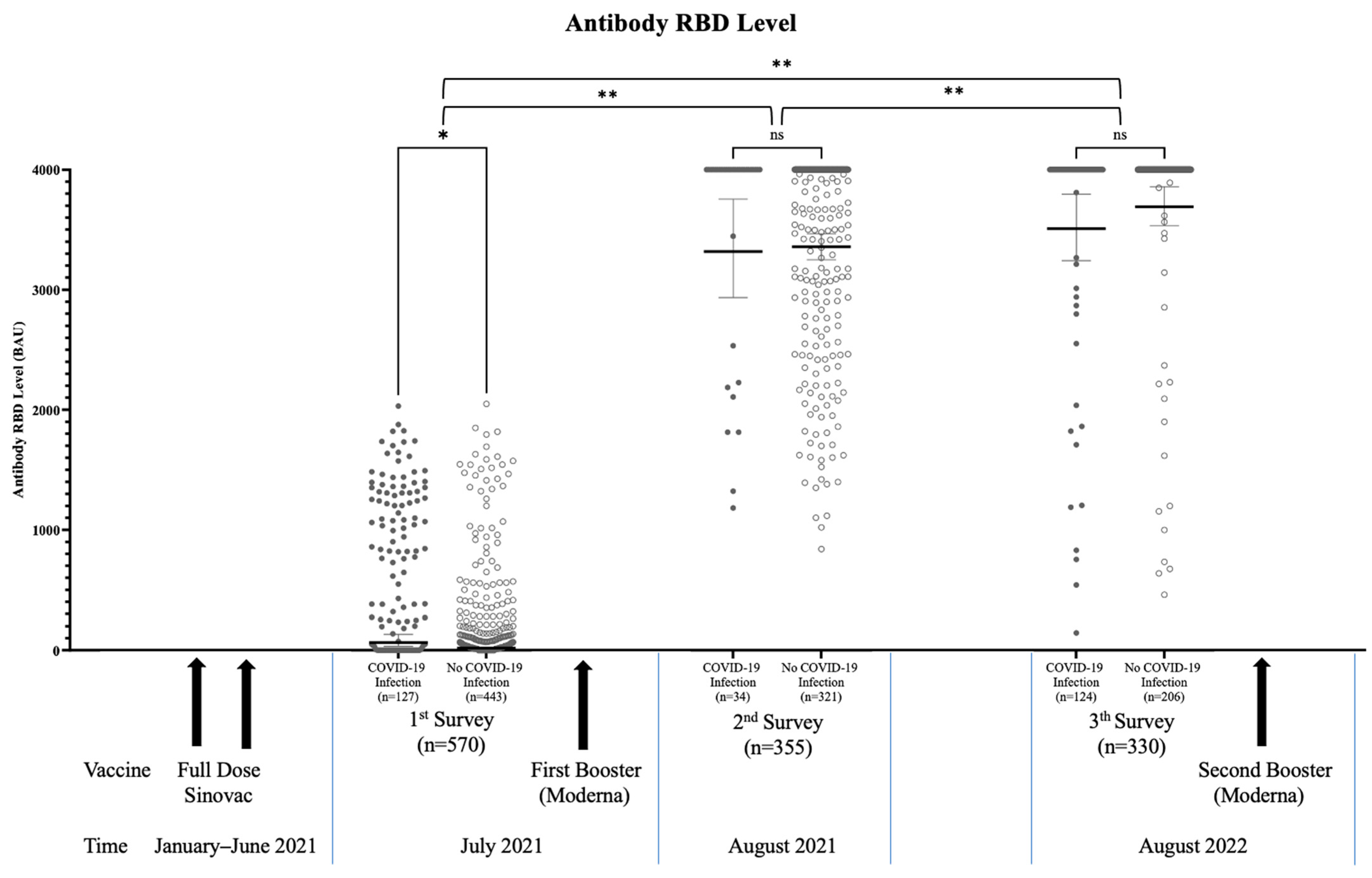
| Antibody level (median, IQR) BAU/mL | 41.4 * (10–629.4) | 4000 (3081–4000) | 4000 (4000–4000) |
| Antibody level classification | |||
| ≥4000 BAU/mL | 0 (0) | 205 (57.7) ** | 291 (88.1) |
| <4000 BAU/mL | 570 (100) | 150 (42.3) | 39 (11.9) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Muslimah, A.H.; Tiara, M.R.; Djauhari, H.; Dewantara, M.H.; Susandi, E.; Indrati, A.R.; Alisjahbana, B.; Soeroto, A.Y.; Wisaksana, R. High Levels of Anti-SARS-CoV-2 Receptor-Binding Domain (RBD) Antibodies One Year Post Booster Vaccinations among Hospital Workers in Indonesia: Was the Second Booster Needed? Vaccines 2023, 11, 1300. https://doi.org/10.3390/vaccines11081300
Muslimah AH, Tiara MR, Djauhari H, Dewantara MH, Susandi E, Indrati AR, Alisjahbana B, Soeroto AY, Wisaksana R. High Levels of Anti-SARS-CoV-2 Receptor-Binding Domain (RBD) Antibodies One Year Post Booster Vaccinations among Hospital Workers in Indonesia: Was the Second Booster Needed? Vaccines. 2023; 11(8):1300. https://doi.org/10.3390/vaccines11081300
Chicago/Turabian StyleMuslimah, Amila Hanifan, Marita Restie Tiara, Hofiya Djauhari, Muhammad Hafizh Dewantara, Evan Susandi, Agnes Rengga Indrati, Bachti Alisjahbana, Arto Yuwono Soeroto, and Rudi Wisaksana. 2023. "High Levels of Anti-SARS-CoV-2 Receptor-Binding Domain (RBD) Antibodies One Year Post Booster Vaccinations among Hospital Workers in Indonesia: Was the Second Booster Needed?" Vaccines 11, no. 8: 1300. https://doi.org/10.3390/vaccines11081300
APA StyleMuslimah, A. H., Tiara, M. R., Djauhari, H., Dewantara, M. H., Susandi, E., Indrati, A. R., Alisjahbana, B., Soeroto, A. Y., & Wisaksana, R. (2023). High Levels of Anti-SARS-CoV-2 Receptor-Binding Domain (RBD) Antibodies One Year Post Booster Vaccinations among Hospital Workers in Indonesia: Was the Second Booster Needed? Vaccines, 11(8), 1300. https://doi.org/10.3390/vaccines11081300






