Factors Associated with College Students’ Human Papillomavirus (HPV) Vaccination and Preferred Strategies for Catch-Up Vaccine Promotion: A Mixed-Methods Study
Abstract
1. Introduction
1.1. HPV Vaccination among College Students
1.2. Barriers to HPV Vaccination among College Students
1.3. Facilitators to HPV Vaccination among College Students
1.4. Research Gaps
1.5. Study Aim
2. Materials and Methods
2.1. Study Design and Setting
2.2. Survey
2.2.1. Sampling and Data Collection
2.2.2. Measures
2.2.3. Data Analysis
2.3. Dyadic Interview
2.3.1. Sampling and Data Collection
2.3.2. Data Analysis
2.4. Data Synthesis
3. Results
3.1. Survey
3.1.1. Sociodemographic Characteristics and Sex Differences of the Sample
3.1.2. Bivariate Analyses of Variables of Interest for Female and Male Students
3.1.3. Distributions of HPV Vaccination Status and Influences on HPV Vaccination for Female and Male Students
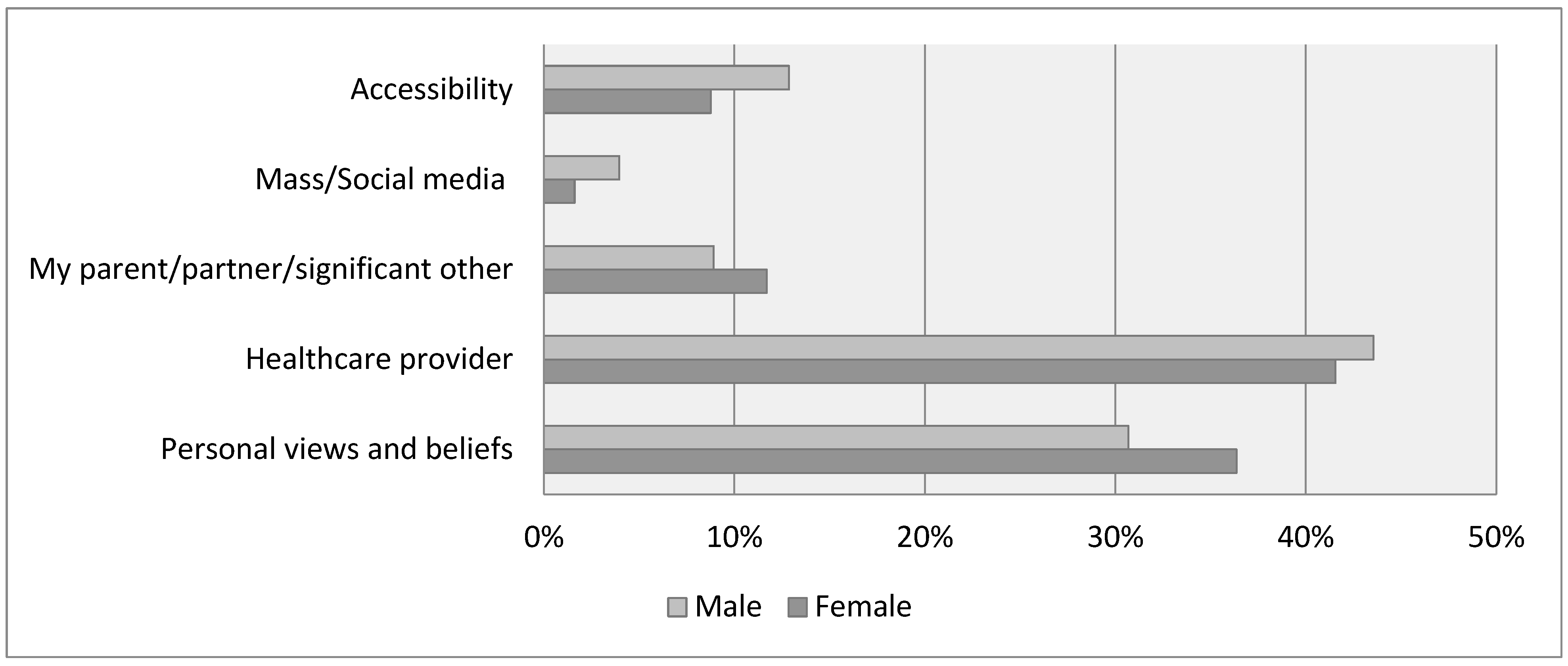
3.1.4. Distributions of Cancer-Related Information Sources for Female and Male Students
3.1.5. Binary Logistic Regression for Female and Male Students
3.2. Dyadic Interview
3.2.1. College Students’ Perceived Barriers to HPV Vaccination
3.2.2. College Students’ Preferred Strategies for Promoting Catch-Up HPV Vaccination
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- STD Facts—Human Papillomavirus (HPV). Available online: https://www.cdc.gov/std/hpv/stdfact-hpv.htm (accessed on 27 August 2022).
- CDC. HPV Vaccination and Cancer Prevention. Available online: https://www.cdc.gov/vaccines/vpd/hpv/index.html (accessed on 14 March 2022).
- Goldfarb, J.A.; Comber, J.D. Human papillomavirus (HPV) infection and vaccination: A cross-sectional study of college students’ knowledge, awareness, and attitudes in Villanova, PA. Vaccine X 2022, 10, 100141. [Google Scholar] [CrossRef]
- McLendon, L.; Puckett, J.; Green, C.; James, J.; Head, K.J.; Lee, H.Y.; Pierce, J.Y.; Beasley, M.; Daniel, C.L. Factors associated with HPV vaccination initiation among United States college students. Hum. Vaccines Immunother. 2021, 17, 1033–1043. [Google Scholar] [CrossRef]
- Kellogg, C.; Shu, J.; Arroyo, A.; Dinh, N.T.; Wade, N.; Sanchez, E.; Equils, O. A significant portion of college students are not aware of HPV disease and HPV vaccine recommendations. Hum. Vaccines Immunother. 2019, 15, 1760–1766. [Google Scholar] [CrossRef]
- Radzki, D.; Kusiak, A.; Ordyniec-Kwaśnica, I.; Bondarczuk, A. Human papillomavirus and leukoplakia of the oral cavity: A systematic review. Adv. Dermatol. Allergol. 2021, 39, 594–600. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. CDC Six Reasons to Get Vaccinated against HPV. 2020. Available online: https://www.cdc.gov/hpv/parents/vaccine/six-reasons.html (accessed on 12 June 2021).
- HPV and HPV Testing. Available online: https://www.cancer.org/healthy/cancer-causes/infectious-agents/hpv/hpv-and-hpv-testing.html (accessed on 31 December 2022).
- Kasymova, S.; Harrison, S.E.; Pascal, C. Knowledge and Awareness of Human Papillomavirus Among College Students in South Carolina. Infect. Dis. 2019, 12, 1178633718825077. [Google Scholar] [CrossRef]
- Santacroce, L.; Di Cosola, M.; Bottalico, L.; Topi, S.; Charitos, I.A.; Ballini, A.; Inchingolo, F.; Cazzolla, A.P.; Dipalma, G. Focus on HPV Infection and the Molecular Mechanisms of Oral Carcinogenesis. Viruses 2021, 13, 559. [Google Scholar] [CrossRef]
- Dufour, L.; Carrouel, F.; Dussart, C. Human Papillomaviruses in Adolescents: Knowledge, Attitudes, and Practices of Pharmacists Regarding Virus and Vaccination in France. Viruses 2023, 15, 778. [Google Scholar] [CrossRef]
- Koskan, A.; Cantley, A.; Li, R.; Silvestro, K.; Helitzer, D. College Students’ Digital Media Preferences for future HPV Vaccine Campaigns. J. Cancer Educ. 2021, 37, 1743–1751. [Google Scholar] [CrossRef]
- CDC. HPV-Associated Cancer Statistics. Available online: https://www.cdc.gov/cancer/hpv/statistics/index.htm (accessed on 18 January 2022).
- HPV and Cancer—National Cancer Institute. Available online: https://www.cancer.gov/about-cancer/causes-prevention/risk/infectious-agents/hpv-and-cancer (accessed on 23 October 2020).
- Ou, L.; Youngstedt, S.D. The Role of Vaccination Interventions to Promote HPV Vaccine Uptake Rates in a College-Aged Population: A Systematic Review. J. Cancer Educ. 2022, 37, 244–250. [Google Scholar] [CrossRef] [PubMed]
- Yusupov, A.; Popovsky, D.; Mahmood, L.; Kim, A.S.; Akman, A.E.; Yuan, H. The nonavalent vaccine: A review of high-risk HPVs and a plea to the CDC. Am. J. Stem Cells 2019, 8, 52–64. [Google Scholar] [PubMed]
- Kessler, R.; Auwaerter, P. Strategies to improve human papillomavirus (HPV) vaccination rates among college students. J. Am. Coll. Health 2021, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Meites, E. Human Papillomavirus Vaccination for Adults: Updated Recommendations of the Advisory Committee on Immunization Practices. Morb. Mortal. Wkly. Rep. 2019, 68, 698–702. Available online: https://www.cdc.gov/mmwr/volumes/68/wr/mm6832a3.htm (accessed on 16 October 2020). [CrossRef] [PubMed]
- CDC. HPV Vaccine Safety and Effectiveness. Available online: https://www.cdc.gov/vaccines/vpd/hpv/hcp/safety-effectiveness.html (accessed on 30 March 2022).
- Giuliano, A.R.; Palefsky, J.M.; Goldstone, S.; Moreira, E.D.; Penny, M.E.; Aranda, C.; Vardas, E.; Moi, H.; Jessen, H.; Hillman, R.; et al. Efficacy of Quadrivalent HPV Vaccine against HPV Infection and Disease in Males. N. Engl. J. Med. 2011, 364, 401–411. [Google Scholar] [CrossRef] [PubMed]
- Slade, B.A.; Leidel, L.; Vellozzi, C.; Woo, E.J.; Hua, W.; Sutherland, A.; Izurieta, H.S.; Ball, R.; Miller, N.; Braun, M.M.; et al. Postlicensure Safety Surveillance for Quadrivalent Human Papillomavirus Recombinant Vaccine. JAMA 2009, 302, 750–757. [Google Scholar] [CrossRef]
- Arana, J.E.; Harrington, T.; Cano, M.; Lewis, P.; Mba-Jonas, A.; Rongxia, L.; Stewart, B.; Markowitz, L.E.; Shimabukuro, T.T. Post-licensure safety monitoring of quadrivalent human papillomavirus vaccine in the Vaccine Adverse Event Reporting System (VAERS), 2009–2015. Vaccine 2018, 36, 1781–1788. [Google Scholar] [CrossRef]
- Block, S.L.; Brown, D.R.; Chatterjee, A.; Gold, M.A.; Sings, H.L.; Meibohm, A.; Dana, A.; Haupt, R.M.; Barr, E.; Tamms, G.M.; et al. Clinical trial and post-licensure safety profile of a prophylactic human papillomavirus (types 6, 11, 16, and 18) l1 virus-like particle vaccine. Pediatr. Infect. Dis. J. 2010, 29, 95–101. [Google Scholar] [CrossRef]
- Chen, M.M.; Mott, N.; Clark, S.J.; Harper, D.M.; Shuman, A.G.; Prince, M.E.P.; Dossett, L.A. HPV Vaccination Among Young Adults in the US. JAMA 2021, 325, 1673–1674. [Google Scholar] [CrossRef]
- Lu, P.-J. Surveillance of Vaccination Coverage among Adult Populations—United States, 2018. MMWR Surveill. Summ. 2021, 70, 1–26. Available online: https://www.cdc.gov/mmwr/volumes/70/ss/ss7003a1.htm (accessed on 19 January 2022). [CrossRef]
- National Vaccine Advisory Committee. Overcoming Barriers to Low HPV Vaccine Uptake in the United States: Recommendations from the National Vaccine Advisory Committee: Approved by the National Vaccine Advisory Committee on June 9, 2015. Public Health Rep. 2016, 131, 17–25. [Google Scholar] [CrossRef]
- Survey Data. Available online: https://www.acha.org/ACHA/Resources/Survey_Data/ACHA/Resources/Survey_Data.aspx (accessed on 2 January 2023).
- Pingali, C. National Vaccination Coverage Among Adolescents Aged 13–17 Years—National Immunization Survey-Teen, United States, 2021. Morb. Mortal. Wkly. Rep. 2022, 71, 1101–1108. Available online: https://www.cdc.gov/mmwr/volumes/71/wr/mm7135a1.htm (accessed on 4 September 2022). [CrossRef]
- Increase the Proportion of Adolescents Who Get Recommended Doses of the HPV Vaccine—IID-08—Healthy People 2030. Available online: https://health.gov/healthypeople/objectives-and-data/browse-objectives/vaccination/increase-proportion-adolescents-who-get-recommended-doses-hpv-vaccine-iid-08 (accessed on 4 September 2022).
- Klasko-Foster, L.B.; Przybyla, S.; Orom, H.; Gage-Bouchard, E.; Kiviniemi, M.T. The influence of affect on HPV vaccine decision making in an HPV vaccine naïve college student population. Prev. Med. Rep. 2020, 20, 101195. [Google Scholar] [CrossRef] [PubMed]
- Barnard, M.; Cole, A.C.; Ward, L.; Gravlee, E.; Cole, M.L.; Compretta, C. Interventions to increase uptake of the human papillomavirus vaccine in unvaccinated college students: A systematic literature review. Prev. Med. Rep. 2019, 14, 100884. [Google Scholar] [CrossRef] [PubMed]
- Natipagon-Shah, B.; Lee, E.; Lee, S.-Y. Knowledge, Beliefs, and Practices among U. S. College Students Concerning Papillomavirus Vaccination. J. Community Health 2021, 46, 380–388. [Google Scholar] [CrossRef] [PubMed]
- Kitur, H.; Horowitz, A.M.; Beck, K.; Wang, M.Q. HPV Knowledge, Vaccine Status, and Health Literacy among University Students. J. Cancer Educ. 2022, 37, 1606–1613. [Google Scholar] [CrossRef] [PubMed]
- D’Errico, M.P.; Tung, W.-C.; Lu, M.; D’Errico, R. Barriers and Recommendations Associated with Human Papillomavirus Vaccination among College Students. J. Nurse Pract. 2020, 16, 533–537. [Google Scholar] [CrossRef]
- Barnard, M.; George, P.; Perryman, M.L.; Wolff, L.A. Human papillomavirus (HPV) vaccine knowledge, attitudes, and uptake in college students: Implications from the Precaution Adoption Process Model. PLoS ONE 2017, 12, e0182266. [Google Scholar] [CrossRef]
- Marshall, S.; Fleming, A.; Moore, A.C.; Sahm, L.J. Views of parents regarding human papillomavirus vaccination: A systematic review and meta-ethnographic synthesis of qualitative literature. Res. Soc. Adm. Pharm. 2019, 15, 331–337. [Google Scholar] [CrossRef]
- Dellino, M.; Cascardi, E.; Tomasone, V.; Zaccaro, R.; Maggipinto, K.; Giacomino, M.E.; De Nicolò, M.; De Summa, S.; Cazzato, G.; Scacco, S.; et al. Communications Is Time for Care: An Italian Monocentric Survey on Human Papillomavirus (HPV) Risk Information as Part of Cervical Cancer Screening. J. Pers. Med. 2022, 12, 1387. [Google Scholar] [CrossRef]
- Dyne, E.A.V. Trends in Human Papillomavirus–Associated Cancers—United States, 1999–2015. Morb. Mortal. Wkly. Rep. 2018, 67, 918. Available online: https://www.cdc.gov/mmwr/volumes/67/wr/mm6733a2.htm (accessed on 23 October 2020). [CrossRef]
- Interactive Reports. Available online: https://www.memphis.edu/oir/data/index.php (accessed on 17 January 2023).
- CDC. ACIP HPV Vaccine Recommendations. Available online: https://www.cdc.gov/vaccines/hcp/acip-recs/vacc-specific/hpv.html (accessed on 2 December 2022).
- Qualtrics XM: The Leading Experience Management Software. Available online: https://www.qualtrics.com/?utm_source=google&utm_medium=ppc&utm_campaign=US-Brand-Qualtrics-Brand&utm_keyword=qualtrics&MatchType=e&adid=522505679922&utm_content=522505679922&adgroupid=41339289338&campaignid=755409789&Target=&targetid=kwd-8232955280&Device=c&devicemodel=&loc_phsyical_ms=9013543&network=g&adposition=&gclid=Cj0KCQiA4aacBhCUARIsAI55maGCqGhim4Xhai5GQP7-hDI7BFCYn4M9CDlsldJqVzrsrTPP5jq_h6saAv3CEALw_wcB (accessed on 2 December 2022).
- Karki, I.; Dobbs, P.D.; Larson, D.; Maness, S.B. Human papillomavirus (HPV) knowledge, beliefs, and vaccine uptake among United States and international college students. J. Am. Coll. Health 2021, 70, 2483–2490. [Google Scholar] [CrossRef]
- Szilagyi, P.G.; Albertin, C.S.; Gurfinkel, D.; Saville, A.W.; Vangala, S.; Rice, J.D.; Helmkamp, L.; Zimet, G.D.; Valderrama, R.; Breck, A.; et al. Prevalence and characteristics of HPV vaccine hesitancy among parents of adolescents across the US. Vaccine 2020, 38, 6027–6037. [Google Scholar] [CrossRef] [PubMed]
- Morgan, D.L.; Ataie, J.; Carder, P.; Hoffman, K. Introducing Dyadic Interviews as a Method for Collecting Qualitative Data. Qual. Health Res. 2013, 23, 1276–1284. [Google Scholar] [CrossRef]
- Peterson, C.E.; Silva, A.; Holt, H.K.; Balanean, A.; Goben, A.H.; Dykens, J.A. Barriers and facilitators to HPV vaccine uptake among US rural populations: A scoping review. Cancer Causes Control 2020, 31, 801–814. [Google Scholar] [CrossRef]
- Downs, L.S.; Scarinci, I.; Einstein, M.H.; Collins, Y.; Flowers, L. Overcoming the barriers to HPV vaccination in high-risk populations in the US. Gynecol. Oncol. 2010, 117, 486–490. [Google Scholar] [CrossRef]
- Golden, S.D.; Earp, J.A.L. Social Ecological Approaches to Individuals and Their Contexts: Twenty Years of Health Education & Behavior Health Promotion Interventions. Health Educ. Behav. 2012, 39, 364–372. [Google Scholar] [CrossRef]
- Elliott, L.; Yang, K. Vaccine Acceptance and Hesitancy among College Students in Nevada: A State-Wide Cross-Sectional Study. Vaccines 2022, 10, 105. [Google Scholar] [CrossRef]
- Larson, H.J.; Gakidou, E.; Murray, C.J.L. The Vaccine-Hesitant Moment. N. Engl. J. Med. 2022, 387, 58–65. [Google Scholar] [CrossRef]
- Paskett, E.; Thompson, B.; Ammerman, A.S.; Ortega, A.N.; Marsteller, J.; Richardson, D. Multilevel Interventions To Address Health Disparities Show Promise In Improving Population Health. Health Aff. 2016, 35, 1429–1434. [Google Scholar] [CrossRef]
- Reports_ACHA-NCHAIII. Available online: https://www.acha.org/NCHA/ACHA-NCHA_Data/Publications_and_Reports/NCHA/Data/Reports_ACHA-NCHAIII.aspx (accessed on 10 April 2023).
- Choi, J.; Tamí-Maury, I.; Cuccaro, P.; Kim, S.; Markham, C. Digital Health Interventions to Improve Adolescent HPV Vaccination: A Systematic Review. Vaccines 2023, 11, 249. [Google Scholar] [CrossRef] [PubMed]
- Brandt, H.M.; Sundstrom, B.; Monroe, C.M.; Turner-McGrievy, G.; Larsen, C.; Stansbury, M.; Magradey, K.; Gibson, A.; West, D.S. Evaluating a Technology-Mediated HPV Vaccination Awareness Intervention: A Controlled, Quasi-Experimental, Mixed Methods Study. Vaccines 2020, 8, 749. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.J.; Cho, J. Promoting HPV Vaccination Online: Message Design and Media Choice. Health Promot. Pract. 2017, 18, 645–653. [Google Scholar] [CrossRef]
- Argyris, Y.A.; Nelson, V.R.; Wiseley, K.; Shen, R.; Roscizewski, A. Do social media campaigns foster vaccination adherence? A systematic review of prior intervention-based campaigns on social media. Telemat. Inform. 2023, 76, 101918. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.K.; Su, L.Y.-F. When a Personal HPV Story on a Blog Influences Perceived Social Norms: The Roles of Personal Experience, Framing, Perceived Similarity, and Social Media Metrics. Health Commun. 2020, 35, 438–446. [Google Scholar] [CrossRef]
- Ma, Z. The use of immersive stories to influence college students’ attitudes and intentions related to drinking and driving. J. Am. Coll. Health 2022, 70, 2042–2049. [Google Scholar] [CrossRef]
- Ryan, J.J.; Kreiner, D.S.; Chapman, M.D.; Stark-Wroblewski, K. Virtual reality cues for binge drinking in college students. Cyberpsychol. Behav. Soc. Netw. 2010, 13, 159–162. [Google Scholar] [CrossRef]
- Lu, A.S.; Pelarski, V.; Alon, D.; Baran, A.; McGarrity, E.; Swaminathan, N.; Sousa, C.V. The effect of narrative element incorporation on physical activity and game experience in active and sedentary virtual reality games. Virtual Real 2023, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Han, J.; Liu, G.; Zheng, Q. Prior knowledge as a moderator between signaling and learning performance in immersive virtual reality laboratories. Front. Psychol. 2023, 14, 1118174. [Google Scholar] [CrossRef]
- Zeng, N.; Pope, Z.; Gao, Z. Acute Effect of Virtual Reality Exercise Bike Games on College Students’ Physiological and Psychological Outcomes. Cyberpsychol. Behav. Soc. Netw. 2017, 20, 453–457. [Google Scholar] [CrossRef]
- Johnston, J.D.; Massey, A.P.; Marker-Hoffman, R.L. Using an alternate reality game to increase physical activity and decrease obesity risk of college students. J. Diabetes Sci. Technol. 2012, 6, 828–838. [Google Scholar] [CrossRef] [PubMed]
- Porras Garcia, B.; Ferrer Garcia, M.; Olszewska, A.; Yilmaz, L.; González Ibañez, C.; Gracia Blanes, M.; Gültekin, G.; Serrano Troncoso, E.; Gutiérrez Maldonado, J. Is This My Own Body? Changing the Perceptual and Affective Body Image Experience among College Students Using a New Virtual Reality Embodiment-Based Technique. J. Clin. Med. 2019, 8, 925. [Google Scholar] [CrossRef]
- Xu, W.; Liang, H.-N.; Baghaei, N.; Ma, X.; Yu, K.; Meng, X.; Wen, S. Effects of an Immersive Virtual Reality Exergame on University Students’ Anxiety, Depression, and Perceived Stress: Pilot Feasibility and Usability Study. JMIR Serious Games 2021, 9, e29330. [Google Scholar] [CrossRef]
- Yang, S.; Lin, L.; Zhang, X. Adjustment Method of College Students’ Mental Health Based on Data Analysis Under the Background of Positive Psychology. Front. Psychol. 2022, 13, 921621. [Google Scholar] [CrossRef] [PubMed]
- Browning, M.H.E.M.; Shin, S.; Drong, G.; McAnirlin, O.; Gagnon, R.J.; Ranganathan, S.; Sindelar, K.; Hoptman, D.; Bratman, G.N.; Yuan, S.; et al. Daily exposure to virtual nature reduces symptoms of anxiety in college students. Sci. Rep. 2023, 13, 1239. [Google Scholar] [CrossRef]
- Real, F.J.; Ollberding, N.J.; Meisman, A.R.; DeBlasio, D.J.; Pero, M.B.; Davis, D.; Cruse, B.; Klein, M.D.; Kahn, J.A.; Rosen, B.L. Impact of a Virtual Reality Curriculum on Human Papillomavirus Vaccination: A Pilot Trial. Am. J. Prev. Med. 2022, 63, 865–873. [Google Scholar] [CrossRef] [PubMed]
- Plechatá, A.; Vandeweerdt, C.; Atchapero, M.; Luong, T.; Holz, C.; Betsch, C.; Dietermann, B.; Schultka, Y.; Böhm, R.; Makransky, G. Experiencing herd immunity in virtual reality increases COVID-19 vaccination intention: Evidence from a large-scale field intervention study. Comput. Human Behav. 2023, 139, 107533. [Google Scholar] [CrossRef] [PubMed]
- Darville-Sanders, G.; Anderson-Lewis, C.; Stellefson, M.; Lee, Y.H.; MacInnes, J.; Pigg, R.M.; Mercado, R.; Gaddis, C. mHealth video gaming for human papillomavirus vaccination among college men-qualitative inquiry for development. Mhealth 2022, 8, 22. [Google Scholar] [CrossRef]
- Real, F.J.; Zackoff, M.W.; Rosen, B.L. Using Technology to Overcome Vaccine Hesitancy. Pediatr. Clin. N. Am. 2023, 70, 297–308. [Google Scholar] [CrossRef] [PubMed]
- Vandeweerdt, C.; Luong, T.; Atchapero, M.; Mottelson, A.; Holz, C.; Makransky, G.; Böhm, R. Virtual reality reduces COVID-19 vaccine hesitancy in the wild: A randomized trial. Sci. Rep. 2022, 12, 4593. [Google Scholar] [CrossRef]
| Variables | Total (N = 417) | Female (n = 312) | Male (n = 101) | (p-Value) | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Vaccinated | |||||||
| Yes | 201 | 48.67 | 163 | 52.92 | 36 | 35.64 | 9.09 (0.003) |
| No | 212 | 51.33 | 145 | 47.08 | 65 | 64.36 | |
| Age | |||||||
| 20 or below | 145 | 34.77 | 107 | 34.29 | 35 | 34.65 | 2.01 (0.570) |
| 21–22 | 178 | 42.69 | 131 | 41.99 | 46 | 45.54 | |
| 23–24 | 65 | 15.59 | 49 | 15.71 | 16 | 15.84 | |
| 25 or above | 29 | 6.95 | 25 | 8.01 | 4 | 3.96 | |
| Race | |||||||
| Black | 152 | 37.44 | 121 | 39.93 | 29 | 29.29 | 7.98 (0.018) |
| White | 190 | 46.80 | 142 | 46.86 | 46 | 46.46 | |
| Others | 64 | 15.76 | 40 | 13.20 | 24 | 24.24 | |
| School year | |||||||
| 1st year | 32 | 7.90 | 21 | 6.93 | 10 | 10.20 | 4.45 (0.349) |
| 2nd year | 80 | 19.75 | 54 | 17.82 | 24 | 24.49 | |
| 3rd year | 124 | 30.62 | 93 | 30.69 | 30 | 30.61 | |
| 4th year | 121 | 29.88 | 97 | 32.01 | 24 | 24.49 | |
| 5th year | 48 | 11.85 | 38 | 12.54 | 10 | 10.20 | |
| Annual income | |||||||
| Less than USD 20,000 | 175 | 43.53 | 135 | 45.00 | 39 | 39.80 | 3.60 (0.609) |
| USD 20,001 to USD 40,000 | 92 | 22.89 | 70 | 23.33 | 22 | 22.45 | |
| USD 40,001 to USD 60,000 | 44 | 10.95 | 33 | 11.00 | 11 | 11.22 | |
| USD 60,001 to USD 80,000 | 29 | 7.21 | 19 | 6.33 | 9 | 9.18 | |
| USD 80,001 to USD 100,000 | 26 | 6.47 | 15 | 5.00 | 9 | 9.18 | |
| Over USD 100,000 | 36 | 8.96 | 28 | 9.33 | 8 | 8.16 | |
| Religious importance | |||||||
| Important | 302 | 74.94 | 239 | 79.40 | 60 | 61.22 | 13.01 (0.000) |
| Not important | 101 | 25.06 | 62 | 20.60 | 38 | 38.78 | |
| Having medical health insurance | |||||||
| Yes | 435 | 85.19 | 260 | 86.09 | 82 | 82.83 | 0.64 (0.426) |
| No | 60 | 14.81 | 42 | 13.91 | 17 | 17.17 | |
| Having a primary health care provider | |||||||
| Yes | 295 | 72.84 | 225 | 74.50 | 68 | 68.69 | 1.28 (0.258) |
| No | 110 | 27.16 | 77 | 25.50 | 31 | 31.31 | |
| Health condition | |||||||
| Very poor/poor/fair | 109 | 27.25 | 79 | 26.25 | 30 | 30.30 | 1.95 (0.378) |
| Good | 194 | 48.50 | 152 | 50.50 | 42 | 42.42 | |
| Excellent | 97 | 24.25 | 70 | 23.26 | 27 | 27.27 | |
| Variables | Total (N = 417) | Female (n = 312) | Male (n = 101) | |t-Value| (p-Value) | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| HPV knowledge | 3.88 | 2.41 | 4.05 | 2.39 | 3.35 | 2.40 | 2.44 (0.015) |
| HPV vaccine knowledge | 4.82 | 1.72 | 4.97 | 1.63 | 4.28 | 1.89 | 3.32 (0.001) |
| HPV belief model | |||||||
| Benefit | 9.28 | 1.54 | 9.22 | 1.51 | 9.48 | 1.62 | 1.44 (0.150) |
| Severity | 9.15 | 1.78 | 8.95 | 1.70 | 9.76 | 1.90 | 4.06 (0.000) |
| Barrier | 7.39 | 2.40 | 7.10 | 2.18 | 8.32 | 2.80 | 4.54 (0.000) |
| Susceptibility | 4.11 | 1.64 | 3.97 | 1.57 | 4.52 | 1.78 | 2.98 (0.003) |
| Perceived risk of HPV | 9.40 | 2.96 | 9.59 | 2.96 | 8.82 | 3.10 | 2.23 (0.026) |
| HPV vaccine hesitancy | 14.85 | 4.41 | 14.73 | 4.54 | 15.24 | 3.97 | 1.01 (0.314) |
| Variables | Female | Male | ||||
|---|---|---|---|---|---|---|
| OR | [95% CI] | p | OR | [95% CI] | p | |
| HPV knowledge | 1.07 | [0.92, 1.25] | 0.382 | 1.07 | [0.79, 1.45] | 0.678 |
| HPV vaccine knowledge | 1.79 | [1.38, 2.32] | 0.000 | 1.57 | [1.04, 2.39] | 0.033 |
| Health belief model | ||||||
| Benefit | 0.98 | [0.74, 1.30] | 0.877 | 0.70 | [0.39, 1.26] | 0.234 |
| Severity | 1.00 | [0.81, 1.22] | 0.970 | 0.93 | [0.61, 1.44] | 0.756 |
| Barrier | 0.62 | [0.49, 0.78] | 0.000 | 0.58 | [0.38, 0.87] | 0.008 |
| Susceptibility | 0.93 | [0.72, 1.19] | 0.558 | 0.76 | [0.47, 1.22] | 0.259 |
| Perceived risk of HPV | 1.18 | [1.04, 1.34] | 0.010 | 1.04 | [0.82, 1.33] | 0.726 |
| HPV vaccine hesitancy | 0.86 | [0.77, 0.97] | 0.014 | 0.86 | [0.67, 1.11] | 0.254 |
| Age | 1.36 | [1.03, 1.81] | 0.031 | 0.70 | [0.37, 1.33] | 0.278 |
| Race (ref. = Black) | ||||||
| White | 0.70 | [0.33, 1.50] | 0.363 | 0.39 | [0.07, 2.03] | 0.260 |
| Others | 0.61 | [0.20, 1.84] | 0.381 | 0.43 | [0.06, 2.93] | 0.389 |
| School year | 0.67 | [0.43, 1.05] | 0.079 | 1.57 | [0.63, 3.93] | 0.333 |
| Income | 0.95 | [0.78, 1.16] | 0.606 | 0.80 | [0.54, 1.19] | 0.265 |
| Religious importance (ref. = Not important) | ||||||
| Important | 3.55 | [1.53, 8.21] | 0.003 | 0.78 | [0.17, 3.48] | 0.742 |
| Insurance (ref. = No) | ||||||
| Yes | 1.14 | [0.39, 3.36] | 0.813 | 1.44 | [0.20, 10.44] | 0.721 |
| Primary healthcare provider (ref. = No) | ||||||
| Yes | 1.33 | [0.61, 2.90] | 0.475 | 3.67 | [0.69, 19.47] | 0.126 |
| Health status | 0.95 | [0.63, 1.43] | 0.807 | 1.25 | [0.43, 3.62] | 0.677 |
| Number of observations | 281 | 80 | ||||
| (p) | 149.89 (0.000) | 39.89 (0.001) | ||||
| McFadden’s | 0.389 | 0.366 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jin, S.W.; Lee, Y.; Lee, S.; Jin, H.; Brandt, H.M. Factors Associated with College Students’ Human Papillomavirus (HPV) Vaccination and Preferred Strategies for Catch-Up Vaccine Promotion: A Mixed-Methods Study. Vaccines 2023, 11, 1124. https://doi.org/10.3390/vaccines11061124
Jin SW, Lee Y, Lee S, Jin H, Brandt HM. Factors Associated with College Students’ Human Papillomavirus (HPV) Vaccination and Preferred Strategies for Catch-Up Vaccine Promotion: A Mixed-Methods Study. Vaccines. 2023; 11(6):1124. https://doi.org/10.3390/vaccines11061124
Chicago/Turabian StyleJin, Seok Won, Yeonggeul Lee, Sohye Lee, Haeun Jin, and Heather M. Brandt. 2023. "Factors Associated with College Students’ Human Papillomavirus (HPV) Vaccination and Preferred Strategies for Catch-Up Vaccine Promotion: A Mixed-Methods Study" Vaccines 11, no. 6: 1124. https://doi.org/10.3390/vaccines11061124
APA StyleJin, S. W., Lee, Y., Lee, S., Jin, H., & Brandt, H. M. (2023). Factors Associated with College Students’ Human Papillomavirus (HPV) Vaccination and Preferred Strategies for Catch-Up Vaccine Promotion: A Mixed-Methods Study. Vaccines, 11(6), 1124. https://doi.org/10.3390/vaccines11061124







