Abstract
Hendra virus disease (HeVD) is an emerging zoonosis in Australia, resulting from the transmission of Hendra virus (HeV) to horses from Pteropus bats. Vaccine uptake for horses is low despite the high case fatality rate of HeVD in both horses and people. We reviewed evidence-based communication interventions to promote and improve HeV vaccine uptake for horses by horse owners and conducted a preliminary evaluation of potential drivers for HeV vaccine uptake using the Behavioural and Social Drivers of Vaccination (BeSD) framework developed by the World Health Organization. Six records were eligible for review following a comprehensive search and review strategy of peer-reviewed literature, but evidence-based communication interventions to promote and improve HeV vaccine uptake for horses were lacking. An evaluation of potential drivers for HeV vaccine uptake using the BeSD framework indicated that horse owners’ perceptions, beliefs, social processes, and practical issues are similar to those experienced by parents making decisions about childhood vaccines, although the overall motivation to vaccinate is lower amongst horse owners. Some aspects of HeV vaccine uptake are not accounted for in the BeSD framework (for example, alternative mitigation strategies such as covered feeding stations or the zoonotic risk of HeV). Overall, problems associated with HeV vaccine uptake appear well-documented. We, therefore, propose to move from a problems-focused to a solutions-focused approach to reduce the risk of HeV for humans and horses. Following our findings, we suggest that the BeSD framework could be modified and used to develop and evaluate communication interventions to promote and improve HeV vaccine uptake by horse owners, which could have a global application to promote vaccine uptake for other zoonotic diseases in animals, such as rabies.
1. Introduction
Hendra virus (HeV; genus Henipavirus, family Paramyxoviridae) is an emerging zoonotic virus that has been detected in Australia’s four mainland species of Pteropus bats [1,2]. Transmission of HeV to horses is considered to be predominantly from P. alecto [2,3], and infected horses are the source of infection for people [1,4]. Since 1994, sixty-six spillover events between bats and horses have been recorded, resulting in 108 horse deaths and seven reported human infections, including four deaths [2,5,6]. There have also been two reported cases of HeV-infected dogs [7].
The geographical range of detected HeV disease (HeVD) in horses has expanded southward since its initial detection in Hendra, Queensland. Cases have recently been reported as far south as Scone [4,6] and West Wallsend, New South Wales, in 2019 and 2021, respectively [8]. The West Wallsend event was caused by a recently identified variant, HeV-g2 [2]. The variant has been detected in P. poliocephalus in South Australia, Victoria, Queensland, and New South Wales, and also in P. alecto in New South Wales [9,10].
Therapeutics for the treatment of HeVD are not available; however, a vaccine for horses and post-exposure prophylaxis for humans have been developed [1,2]. Horses aged ≥ 4 months can be vaccinated [11], with two doses given 3–6 weeks apart and a third dose six months later; then, an annual booster dose thereafter [11]. Despite the availability of the vaccine since 2012, the expanding range of detected HeVD events in horses, and the high case fatality rate of HeVD in both horses and humans, estimated HeV vaccine uptake ranges from 10.1% to 13.0% of the estimated horse population in Queensland and New South Wales annually from 2016 to 2021 [12]. As well as protecting equine welfare, HeV vaccination of horses remains a priority to protect public health [13,14].
The recent development of the Behavioural and Social Drivers of Vaccination (BeSD) framework has demonstrated value in understanding and promoting vaccine uptake by caregivers in the context of vaccine-preventable childhood diseases [15,16]. In this framework, there are four measurable domains of behavioural and social drivers in individuals that are potentially changeable: (1) Thinking and Feeling, relating to cognitive and emotional responses to vaccine-preventable diseases and vaccines, including disease risk perception and vaccine confidence; (2) Social Processes, defined as the social experiences related to vaccines, including gender equity, social norms about vaccination, and receiving health worker recommendations to be vaccinated; (3) Motivation, influenced by the former two domains and including vaccination intention, willingness, and hesitancy; and (4) Practical Issues, which are people’s experiences when trying to get vaccinated, including access barriers such as availability, affordability, ease of access, quality of service, and respect from health workers [16]. The combination of the four domains helps drive or hinder the uptake of recommended vaccines [16]. Research with non-vaccinating parents demonstrates a variety of reasons for childhood vaccine rejection, including low disease risk perception, fears about vaccine safety and efficacy, perceived “vested interests” of vaccine companies driving vaccine schedules, and perceived adverse events following previously administered vaccines [17]. Regardless of why they rejected vaccines, all parents’ decisions were underpinned by a desire to protect their children, and their decisions changed with time and circumstances [18]. Given the potential similarities between parents making vaccination decisions for their children and horse owners deciding on vaccinations for their horses, the BeSD framework may be useful in helping to understand the drivers of HeV vaccination.
The objective of this review was to identify peer-reviewed information about evidence-based communication interventions that have been used to promote HeV vaccine uptake by horse owners. We hypothesised that there are few interventions; therefore, a secondary objective was to appraise information in the reviewed records against the domains of the BeSD framework as a preliminary assessment of the types of information available about factors that drive or hinder HeV vaccine uptake. This review and assessment will inform research and development of a program to promote HeV vaccination.
2. Materials and Methods
2.1. Study Overview
The primary objective of the current study was to determine if there are evidence-based communication interventions to promote HeV vaccine uptake for horses. The secondary objective was to determine if the drivers of HeV vaccine uptake align with the domains of the behavioural and social drivers of vaccine uptake in the BeSD framework as a preliminary step to developing a framework for promoting HeV vaccine uptake.
To achieve the primary objective, we conducted a comprehensive review using methods for critically appraised topics [19,20] to identify descriptions and evaluations of evidence-based communication interventions to increase HeV vaccine uptake for horses by horse owners (see ‘Search strategy and review process’). To achieve the secondary objective, records identified as sufficiently relevant to Objective 1 to warrant full-text screening (Level 2; see ‘Search strategy and review process’) were assessed using the domains of behavioural and social drivers of vaccine uptake in the BeSD framework [15]. Ethical approval was not required for this review.
2.2. Definitions
The population of interest for the uptake of the HeV vaccine was people living in Australia who owned horses that could be at risk of HeVD. The term “communication intervention” was defined as any medium used to deliver information and ideas between parties to aid the discussion of topics of common interest, as well as inform, guide, and motivate a new or existing behaviour [21,22,23]. Communication interventions included face-to-face conversation, telephone conversation, videoconferencing, articles, pamphlets, email, blog posts, social media posts, website pages, smartphone apps, radio, and television [24]. The term ‘evidence-based’ in this context referred to interventions that were developed following research to systematically promote HeV vaccination uptake.
2.3. Search Strategy and Review Process
Searches were conducted in July 2022 using the terms “Hendra*” and “Vaccin*” and “Communicat*” or “Behavio* change” and “Horse owner*” and “Australia*” in BIOSIS Previews Via Web of Science, Scopus, and Medline via Ovid (Supplementary Information, Table S1).
Duplicates were removed, then records were screened for eligibility for Objective 1 (communication interventions to promote HeV vaccine uptake) based on the title and abstract (Level 1), then on the full record (Level 2). Records eligible for data extraction (Level 3) that identified communication interventions to promote HeV vaccine uptake were peer-reviewed and in English. Planned data extraction included the targeted population, type of communication intervention, including the method of dissemination or use, and pre- or post-use evaluation.
If records were not eligible for Level 3 data extraction for the primary objective but contained information about drivers of HeV vaccine uptake (secondary objective), data were extracted from each record and reported in a summary table including the population included in the study with their location and size, equine sectors represented, study design with objectives and factors studied, and main findings in the context of HeV vaccine uptake and the BeSD domains. The main findings were assessed for consistent and divergent (extraneous) themes according to the domains of the behavioural and social drivers of vaccine uptake in the BeSD framework (Thinking and Feeling, Social Processes, Practical Issues, and Motivation) and described below [15]. Extraneous themes included drivers of HeV vaccine uptake that extended beyond the domains of the BeSD framework.
3. Results
Thirty-three records were identified in the database searches, and six duplicate records were removed. Following a review of the title and abstract (Level 1), six records were eligible for review at Level 2. These records contained information from five studies (two records described different aspects of the same study) conducted from 2017 to 2021. The studies included a total of 239 participants (198 horse owners, 16 veterinary staff, and 25 members of the public).
No records described evidence-based communication interventions to promote HeV vaccination uptake for horses (Figure 1: Level 3—data extraction, communications interventions). However, all of the records contained information that was illustrative of at least one of the four domains of the BeSD framework (Figure 1: Level 3—data extraction, vaccine uptake), as well as aspects that extended beyond the BeSD framework due to the One Health nature of HeV and the need to consider ecological drivers of disease spread and spread between populations (horses and people). This information is summarised in Table S2 and Figure 2 and described below.
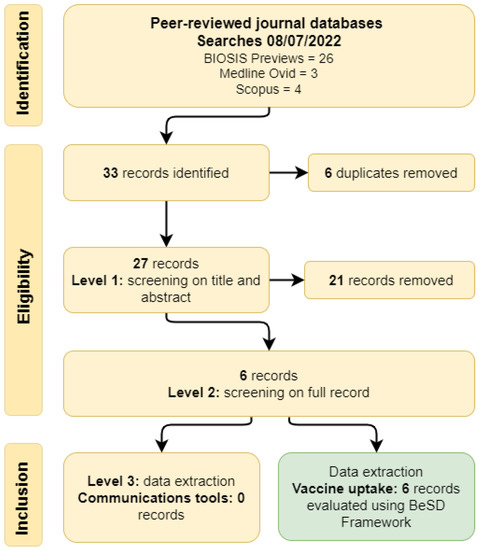
Figure 1.
Review process and records identified in a systematic review to identify evidence-based communication interventions to promote vaccination against Hendra virus in horses and assessment of HeV vaccine uptake using the Behavioural and Social Drivers of Vaccination (BeSD) framework [16].
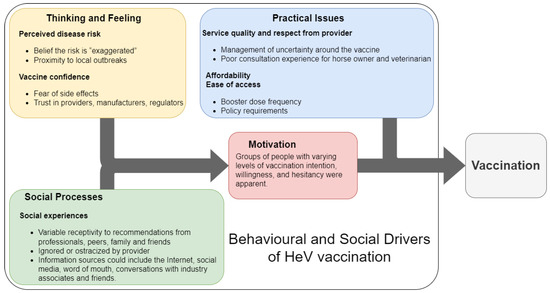
Figure 2.
Diagram of the domains of the Behavioural and Social Drivers of Vaccination framework [16] and information obtained from records identified in a systematic review to identify evidence-based communication interventions to promote vaccination against Hendra virus infection in horses.
3.1. Extracted Data—Drivers of HeV Vaccine Uptake
3.1.1. Thinking and Feeling
Disease risk perception can be low, with some horse owners reporting that HeVD receives excessive attention and that the novelty of HeVD is exaggerated via scaremongering [25]. Risk perception can also change; the temporal and geographic proximity of HeVD outbreaks appears to trigger horse owners to seek information about HeVD and implement both pharmaceutical and property-focused HeVD risk mitigation strategies. Horse owners actively sought more information about HeVD following media reports of local outbreaks. The perceived immediacy of risk promoted HeV vaccine uptake [25,26,27].
Aspects of vaccine confidence, including perceived vaccine benefits and safety and trust in veterinarians and the authorities, were reported. Some owners had low vaccine confidence when they perceived a lack of HeV vaccine safety and efficacy or information transparency and availability [28]. These owners were more likely to discontinue HeV vaccination and believe in conspiracies between vaccine providers, manufacturers, and regulators, with a perception that horse and human welfare were not priorities for these groups [28]. Some owners requested HeV antibody titre testing as an alternative to HeV vaccination due to concern about HeV vaccine reactions and perceived over-vaccination [29]. In contrast, following a deliberative process, community juries who were comprised of the general public (not necessarily horse owners) were confident that vaccination mitigated HeVD risk safely and effectively, with some jurors agreeing that the promotion of HeV vaccination could be implemented immediately and affordably to increase vaccination uptake [14].
3.1.2. Social Processes
Across the records, some social processes were reported as being influential in vaccination decision-making. Wiethoelter, Sawford, Schembri, Taylor, Dhand, Moloney, Wright, Kung, Field, and Toribio [25] reported that many horse owners sought opinions of veterinarians about HeVD and considered their veterinarians to be a valuable and trusted information source relative to governmental or social media sources. However, media reports could also trigger information seeking, and information sources were broad, including the Internet, social media, word of mouth, and conversations with contacts associated with horses and veterinarians. In a survey directed at horse owners who elected not to vaccinate their horses against HeV [26,27], most owners were not influenced by external social processes. Insurance and policy requirements (for example, veterinarians’ refusal to treat unvaccinated horses) and recommendations from veterinarians, medical doctors, industry peers, and friends were all unlikely to promote vaccine uptake. Horse owners could also feel ignored or ostracized following adversarial conversations with veterinarians, further undermining their trust in veterinarians, manufacturers, and regulators [28].
3.1.3. Motivation
There was a range of motivational states described among participants in the included studies. Studies of horse owners who elected not to vaccinate horses demonstrated that there are groups with low motivation to vaccinate despite living in established HeVD risk zones [26,27,28]. These owners preferentially applied non-pharmaceutical and property-based mitigation strategies, such as covering food and water containers [27]. Other studies [25,29] described a range of levels of motivation to vaccinate among horse owners. A community jury study was conducted to assess the acceptability of adding ecological approaches to mitigate HeVD risk [14]. Following deliberation, jurors who reflected the public (and were not primarily horse owners) prioritised current interventions that included vaccination, as well as non-pharmaceutical and property-based mitigation strategies.
3.1.4. Practical Issues
Findings related to the practical issues domain of the BeSD framework included service quality, respect from veterinarians, ease of access to the vaccine, and easily understood information, as well as cost and external requirements.
Service quality and respect were identified as important. For example, poor management of uncertainty around the HeV vaccine during a consultation or perceived ostracism by veterinarians led to a poor experience for both the horse owner and the attending veterinarian [28]. The understandability of the information being given was also found to be an important practical issue. Communication of test results and their meaning also presented challenges. In a study of the communication of HeV antibody titre results, veterinarians acknowledged the difficulty in communicating the results, a titre cut-off value, and the relationship between the titre value and protective immunity [29].
Access and affordability also influenced horse owners’ decisions about vaccine frequency in that the perceived high cost and need for ongoing boosters were barriers to HeV vaccination [26]. Other practical issues influencing the uptake of HeV vaccination were cost, booster dose frequency, policy requirements by veterinarians, and insurance requirements [22,23].
3.1.5. One Health Aspects
Due to the complexity of HeV transmission and prevention, further issues were identified that extended beyond vaccine acceptance to include non-pharmaceutical approaches. These do not align neatly with the current vaccine-focused BeSD framework. This complexity was acknowledged in the community jury study in which participants identified the need for better communication and public education about the behaviours, ecological benefits, and zoonotic risks posed by bats [12]. For example, the proximity of outbreaks that increased disease risk perception and prompted horse owners to seek information was also likely to increase the uptake of property-focused HeVD risk mitigation practices, such as covering horses’ food and water containers, keeping horses off pasture when bats are active, and keeping horses away from fruiting/flowering trees [22].
4. Discussion
The comprehensive review of peer-reviewed literature did not identify any evidence-based communication interventions to promote HeV vaccination by horse owners. However, a subsequent assessment using the BeSD framework enabled the orientation and synthesis of research on horse owner HeV vaccine decision-making, suggesting that the BeSD framework could be adopted and modified to understand and promote HeV vaccination uptake. The BeSD framework was originally developed to characterise the drivers of parental decisions to vaccinate children that are individual, measurable, and potentially changeable with evidence-based interventions [15], and this review demonstrates that there are similarities between the underlying drivers of vaccination decisions among horse owners and parents. Most relate to the BeSD Thinking and Feeling domain in which non-vaccinating parents also perceive low disease risk, are concerned about vaccine side effects, believe that vaccines are unsafe and ineffective, and share a mistrust of health professionals [30,31,32]. Regarding the BeSD Social Processes domain, the social “othering” and dismissal by medical professionals that are experienced by some non-vaccinating parents [33] is comparable with the perceived ostracism from veterinarians reported by HeV vaccine-sceptical horse owners [28]. Within the same domain, healthcare provider recommendations to parents are akin to those from veterinarians to horse owners [17,30,34]. Within the BeSD Practical Issues domain, the cost of vaccination as an influence on horse owner vaccination decisions also influences parents’ vaccination decisions; for example, cost is a known barrier to the Meningococcal B vaccination, which is not included in the National Immunisation Program schedule for all non-Indigenous Australian children [35,36].
The BeSD Motivation domain is a point at which the parents and horse owners might differ. It is not possible to quantify the probability of horse owners’ intention to vaccinate (motivation) in the current review. However, it is clear that there are groups of horse owners with little motivation to vaccinate their horses against HeVD, and overall, motivation appears lower than that of parents for childhood vaccines because there is currently > 95% versus ~12% uptake for childhood vaccines and the HeV vaccine, respectively [33,37]. Generally, horse owners behave similarly to parents in that increased risk perception will result in increased vaccination motivation [17], but the complexity of HeV transmission necessitates that HeVD prevention extends beyond vaccine acceptance to include non-pharmaceutical approaches. The BeSD framework was designed for childhood and COVID vaccination, grounded in the evidence for the drivers of vaccination behaviour. Additional non-pharmaceutical behaviours for HeVD prevention may have different drivers that do not necessarily align well with the current vaccine-focused BeSD framework. This complexity was acknowledged in the community jury study, in which participants identified the need for better communication and public education about the behaviours, ecological benefits, and the zoonotic risk posed by bats [14]. Where the biggest barriers to HeV vaccination lie—whether associated with the domains of ‘Thinking and Feeling’ and ‘Social Processes’ or the domain of ‘Practical Issues’—needs further investigation beyond this preliminary appraisal.
The lack of vaccine uptake for HeV in Australia is paralleled in the United States (US), where there is similarly poor rabies vaccine uptake for horses. Rabies (genus Lyssavirus, family Rhabdoviridae) is caused by a fatal zoonotic neurotropic virus that is transmitted to horses by direct contact (bites) from infected bats, racoons, foxes, and skunks [38]. Similar to HeVD, rabies has a low incidence in horses with severe consequences in both humans and horses [29,39,40]. Thirteen cases of rabid horses and donkeys in the US were reported in 2018 [41]. Like HeV-infected horses, rabid equids can be a source of infection for people [42]. Whilst vaccination of horses against rabies virus infection is not mandatory in the US, the American Association of Equine Practitioners considers the rabies virus vaccine amongst the core vaccines and strongly recommends the annual vaccination of all equids against rabies [43]. In a 2017 study, it was reported that only one in seven horses are vaccinated against rabies in the US, equating to approximately 14% of the 7.25 million owned horses in the US [44,45]. The reasons for the poor uptake of the rabies vaccine by US horse owners and the HeV vaccine by Australian horse owners are similar. Many US owners report not vaccinating their equids (inclusive of domestic horses, miniature horses, ponies, mules, donkeys/burros, and zebra–donkey crosses) against specific diseases (including rabies) due to low exposure risk, effort, and the cost outweighing the benefit [46,47].
Considering the many parallels between non-vaccinating horse owners and non-vaccinating parents and the potential global public health impact, as well as the benefits to horse health and welfare, we are prompted to consider the applicability of communication tools that are available to medical professionals in approaching vaccine discourse with vaccine-hesitant and refusing parents. A clinical communication support intervention for complex communication around childhood vaccination has been developed by the Sharing Knowledge About Immunisation (SKAI) project [48]. The SKAI system has an accessible information website for parents and another for health professionals, including an eLearning module that is designed to adapt the clinical communication skills of health professionals to different immunization consultations [49,50,51]. The interface for parents provides information and resources tailored to address concerns for the level of intention, hesitancy, or refusal present [48,49,51]. The health professional interface similarly provides healthcare workers with tailored information and decision support tools for use before, during, and after immunisation consultations to address concerns and meet communication needs for the level of intention, hesitancy, or refusal present [48]. Research to better understand HeV or rabies vaccination drivers would underpin a modified equine BeSD framework and survey tool and inform the development of an HeV- or rabies-specific SKAI-type system to promote vaccination for these zoonoses in animals [48]. The implementation of such an intervention could then be evaluated using the BeSD tools to allow a comparison of the most effective communication tool to increase HeV vaccine uptake for horses by Australian horse owners.
5. Conclusions
Despite the health impact of Hendra virus disease (HeVD) on horses and people, there are no evidence-based communication interventions to promote Hendra virus (HeV) vaccine uptake for horses in Australia. Using the World Health Organization’s Behavioural and Social Drivers of Vaccination (BeSD) framework for childhood vaccine uptake, we highlighted both similarities and differences in the perceptions, feelings, motivations, social processes, and practical issues that horse owners and parents face in the context of HeV and childhood vaccine decision-making, respectively. This provides some insight into horse owners’ HeVD preventive behaviour and alludes to the circumstances in which they might consider HeV vaccination. This current understanding of the why behind the low uptake of HeVD risk mitigation behaviour by horse owners now needs to be understood in greater detail using mixed social research methods, including other influencing factors, such as the use of alternative mitigation strategies and zoonotic transmission risk, and how these preventive behaviours differ between horse owner types (e.g., recreational versus professional) [15,25,26]. A modified BeSD framework could be developed to produce interventions that reduce HeV vaccine coverage gaps [15], thus reducing the risk of HeVD to horses and, therefore, people. If successful, such modifications to the BeSD framework could have a further application to other zoonoses in One Health contexts, such as vaccination against rabies in endemic regions globally.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/vaccines11050936/s1; Table S1: Search strategy; Table S2: Summaries of the evidence.
Author Contributions
Conceptualization and writing—original draft preparation, J.N.K.-G., V.J.B. and J.M.; investigation, J.N.K.-G.; writing—review and editing, K.E.W., K.R.T., J.M. and V.J.B.; visualization, K.E.W. and V.J.B.; supervision, project administration and funding acquisition, V.J.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research was part funded by the Sydney School of Veterinary Science Research & Enquiry Unit of Study 2022 fund. Wiley is supported by an NHMRC Investigator Grant (Grant number 2008650).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analysed in this study. Data sharing is not applicable to this article.
Acknowledgments
We thank the librarians at the University of Sydney for their assistance with this study. This study was completed in partial fulfilment of the requirements of the Doctor of Veterinary Medicine degree at the University of Sydney (J.N.K.-G.). Thompson is funded by the New South Wales Ministry of Health under the New South Wales Health Prevention Research Support Program.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Middleton, D.; Pallister, J.; Klein, R.; Feng, Y.-R.; Haining, J.; Arkinstall, R.; Frazer, L.; Huang, J.-A.; Edwards, N.; Wareing, M.; et al. Hendra virus vaccine, a one health approach to protecting horse, human, and environmental health. Emerg. Infect. Dis. 2014, 20, 372–379. [Google Scholar] [CrossRef] [PubMed]
- Annand, E.J.; Horsburgh, B.A.; Xu, K.; Reid, P.A.; Poole, B.; de Kantzow, M.C.; Brown, N.; Tweedie, A.; Michie, M.; Grewar, J.D.; et al. Novel Hendra virus variant detected by sentinel surveillance of horses in Australia. Emerg. Infect. Dis. 2022, 28, 693–704. [Google Scholar] [CrossRef] [PubMed]
- Edson, D.; Peel, A.J.; Huth, L.; Mayer, D.G.; Vidgen, M.E.; McMichael, L.; Broos, A.; Melville, D.; Kristoffersen, J.; de Jong, C.; et al. Time of year, age class and body condition predict Hendra virus infection in Australian black flying foxes (Pteropus alecto). Epidemiol. Infect. 2019, 147, e240. [Google Scholar] [CrossRef] [PubMed]
- Yuen, K.Y.; Fraser, N.S.; Henning, J.; Halpin, K.; Gibson, J.S.; Betzien, L.; Stewart, A.J. Hendra virus: Epidemiology dynamics in relation to climate change, diagnostic tests and control measures. One Health 2021, 12, 100207. [Google Scholar] [CrossRef]
- NSW Health. Summary of Human Cases of Hendra Virus Infection. Available online: https://www.health.nsw.gov.au/Infectious/controlguideline/Pages/hendra-case-summary.aspx (accessed on 7 June 2022).
- Business Queensland. Summary of Hendra Virus Incidents in Horses. Available online: https://www.business.qld.gov.au/industries/service-industries-professionals/service-industries/veterinary-surgeons/guidelines-hendra/incident-summary (accessed on 7 June 2022).
- Field, H.E. Hendra virus ecology and transmission. Curr. Opin. Virol. 2016, 16, 120–125. [Google Scholar] [CrossRef]
- Taylor, J.; Thompson, K.; Annand, E.J.; Massey, P.D.; Bennett, J.; Eden, J.-S.; Horsburgh, B.A.; Hodgson, E.; Wood, K.; Kerr, J.; et al. Novel variant Hendra virus genotype 2 infection in a horse in the greater Newcastle region, New South Wales, Australia. One Health 2022, 15, 100423. [Google Scholar] [CrossRef]
- Wang, J.; Anderson, D.E.; Halpin, K.; Hong, X.; Chen, H.; Walker, S.; Valdeter, S.; van der Heide, B.; Neave, M.J.; Bingham, J.; et al. A new Hendra virus genotype found in Australian flying foxes. Virol. J. 2021, 18, 197. [Google Scholar] [CrossRef]
- Peel, A.J.; Yinda, C.K.; Annand, E.J.; Dale, A.S.; Eby, P.; Eden, J.-S.; Jones, D.N.; Kessler, M.K.; Lunn, T.J.; Pearson, T.; et al. Novel Hendra Virus Variant Circulating in Black Flying Foxes and Grey-Headed Flying Foxes, Australia. Emerg. Infect. Dis. 2022, 28, 1043–1047. [Google Scholar] [CrossRef]
- Zoetis Australia Pty Limited. Dosage & Storage. Available online: https://www.zoetis.com.au/all-products/portal-site/equivac-hev.aspx (accessed on 14 August 2022).
- Halpin, K.; Graham, K.; Durr, P.A. Sero-Monitoring of Horses Demonstrates the Equivac® HeV Hendra Virus Vaccine to Be Highly Effective in Inducing Neutralising Antibody Titres. Vaccines 2021, 9, 731. [Google Scholar] [CrossRef]
- Degeling, C.; Kerridge, I. Hendra in the news: Public policy meets public morality in times of zoonotic uncertainty. Soc. Sci. Med. 2013, 82, 156–163. [Google Scholar] [CrossRef]
- Degeling, C.; Gilbert, G.L.; Annand, E.; Taylor, M.; Walsh, M.G.; Ward, M.P.; Wilson, A.; Johnson, J. Managing the risk of Hendra virus spillover in Australia using ecological approaches: A report on three community juries. PLoS ONE 2018, 13, e0209798. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Behavioural and Social Drivers of Vaccination: Tools and Practical Guidance for Achieving High Uptake; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- World Health Organization. Understanding the behavioural and social drivers of vaccine uptake WHO position paper—May 2022. Wkly. Epidemiol. Rec. = Relev. Épidémiologique Hebd. 2022, 20, 209–224. [Google Scholar]
- Helps, C.; Leask, J.; Barclay, L.; Carter, S. Understanding non-vaccinating parents’ views to inform and improve clinical encounters: A qualitative study in an Australian community. BMJ Open 2019, 9, e026299. [Google Scholar] [CrossRef] [PubMed]
- Wiley, K.E.; Leask, J.; Attwell, K.; Helps, C.; Degeling, C.; Ward, P.; Carter, S.M. Parenting and the vaccine refusal process: A new explanation of the relationship between lifestyle and vaccination trajectories. Soc. Sci. Med. 2020, 263, 113259. [Google Scholar] [CrossRef]
- White, S.; Raghavendra, P.; McAllister, S. Letting the CAT out of the bag: Contribution of critically appraised topics to evidence-based practice. Evid. Based Commun. Assess. Interv. 2017, 11, 27–37. [Google Scholar] [CrossRef]
- Brennan, M.L.; Arlt, S.P.; Belshaw, Z.; Buckley, L.; Corah, L.; Doit, H.; Fajt, V.R.; Grindlay, D.J.C.; Moberly, H.K.; Morrow, L.D.; et al. Critically Appraised Topics (CATs) in Veterinary Medicine: Applying Evidence in Clinical Practice. Front. Vet. Sci. 2020, 7, 314. [Google Scholar] [CrossRef]
- Robyn, B.; Charlotte, B. 2—Teaching with technology—Considering your options. In Online Learning and Assessment in Higher Education; Robyn, B., Charlotte, B., Eds.; Elsevier Ltd.: Amsterdam, The Netherlands, 2010; pp. 21–54. [Google Scholar]
- IGI Global. What Is Communication Tool. Available online: https://www.igi-global.com/dictionary/communication-tool/4661 (accessed on 2 May 2022).
- World Organisation for Animal Health. Terrestrial Animal Health Code. In Chapter 3.3. Communication; World Organisation for Animal Health: Paris, France, 2018. [Google Scholar]
- University of Minnesota. 8.4 Different Types of Communication and Channels. In Organizational Behavior; University of Minnesota Libraries: Minneapolis, MN, USA, 2017. [Google Scholar]
- Wiethoelter, A.K.; Sawford, K.; Schembri, N.; Taylor, M.R.; Dhand, N.K.; Moloney, B.; Wright, T.; Kung, N.; Field, H.E.; Toribio, J.-A.L.M.L. “We’ve learned to live with it”—A qualitative study of Australian horse owners’ attitudes, perceptions and practices in response to Hendra virus. Prev. Vet. Med. 2017, 140, 67–77. [Google Scholar] [CrossRef]
- Manyweathers, J.; Field, H.; Longnecker, N.; Agho, K.; Smith, C.; Taylor, M. “Why won’t they just vaccinate?” Horse owner risk perception and uptake of the Hendra virus vaccine. BMC Vet. Res. 2017, 13, 103–112. [Google Scholar] [CrossRef]
- Manyweathers, J.; Field, H.; Jordan, D.; Longnecker, N.; Agho, K.; Smith, C.; Taylor, M. Risk mitigation of emerging zoonoses: Hendra virus and non-vaccinating horse owners. Transbound. Emerg. Dis. 2017, 64, 1898–1911. [Google Scholar] [CrossRef]
- Manyweathers, J.; Taylor, M.; Longnecker, N. Expertise and communicating about infectious disease: A case study of uncertainty and rejection of local knowledge in discourse of experts and decision makers. JCOM J. Sci. Commun. 2020, 19, A01. [Google Scholar] [CrossRef]
- Barrett, R.S.; Wiethoelter, A.; Halpin, K. The Hendra virus vaccine: Perceptions regarding the role of antibody titre testing. Aust. Vet. J. 2021, 99, 412–418. [Google Scholar] [CrossRef] [PubMed]
- Smith, L.E.; Amlôt, R.; Weinman, J.; Yiend, J.; Rubin, G.J. A systematic review of factors affecting vaccine uptake in young children. Vaccine 2017, 35, 6059–6069. [Google Scholar] [CrossRef] [PubMed]
- Chow, M.Y.K.; Danchin, M.; Willaby, H.W.; Pemberton, S.; Leask, J. Parental attitudes, beliefs, behaviours and concerns towards childhood vaccinations in Australia: A national online survey. Aust. Fam. Physician 2017, 46, 145–151. [Google Scholar]
- Brown, K.F.; Kroll, J.S.; Hudson, M.J.; Ramsay, M.; Green, J.; Long, S.J.; Vincent, C.A.; Fraser, G.; Sevdalis, N. Factors underlying parental decisions about combination childhood vaccinations including MMR: A systematic review. Vaccine 2010, 28, 4235–4248. [Google Scholar] [CrossRef]
- Wiley, K.E.; Leask, J.; Attwell, K.; Helps, C.; Barclay, L.; Ward, P.R.; Carter, S.M. Stigmatized for standing up for my child: A qualitative study of non-vaccinating parents in Australia. SSM Popul. Health 2021, 16, 100926. [Google Scholar] [CrossRef] [PubMed]
- Crawford, T.; Leask, J. A discourse analysis of health provider interactions with parents who are reluctant to vaccinate. Patient Educ. Couns. 2022, 105, 1224–1228. [Google Scholar] [CrossRef]
- Wang, B.; Clarke, M.; Afzali, H.H.A.; Marshall, H. Community, parental and adolescent awareness and knowledge of meningococcal disease. Vaccine 2014, 32, 2042–2049. [Google Scholar] [CrossRef]
- Taha, M.-K.; Martinon-Torres, F.; Köllges, R.; Bonanni, P.; Safadi, M.A.P.; Booy, R.; Smith, V.; Garcia, S.; Bekkat-Berkani, R.; Abitbol, V. Equity in vaccination policies to overcome social deprivation as a risk factor for invasive meningococcal disease. Expert Rev. Vaccines 2022, 21, 659–674. [Google Scholar] [CrossRef]
- Taylor, M.; Dhand, N.; Toribio, J.-A.; Wiethoelter, A.; Schembri, N.; Sawford, K.; Kung, N.; Field, H.; Moloney, B.; Wright, T. Longitudinal Cohort Study of Horse Owners. HHALTER: Horse Owners and Hendra Virus: A Longitudinal Study to Evaluate Risk. Final Report; Macquarie University: Sydney, NSW, Australia, 2016. [Google Scholar]
- van der Kolk, J.H.; Veldhuis Kroeze, E.J.B. Infectious Diseases of the Horse: Diagnosis, Pathology, Management and Public Health; Manson Publishing Ltd.: London, UK, 2013. [Google Scholar]
- Young, A. Rabies. Available online: https://ceh.vetmed.ucdavis.edu/health-topics/rabies#:~:text=Rabies%20is%20relatively%20rare%20in,the%20United%20States%20since%201980 (accessed on 21 March 2022).
- Mackenzie, J.S.; Field, H.E. Emerging encephalitogenic viruses: Lyssaviruses and henipaviruses transmitted by frugivorous bats. Arch. Virol. Suppl. 2004, 18, 97–111. [Google Scholar] [CrossRef]
- The Centres for Disease Control and Prevention. Domestic Animals. Available online: https://www.cdc.gov/rabies/location/usa/surveillance/domestic_animals.html (accessed on 21 March 2022).
- Feder, H.M.; Nelson, R.S.; Cartter, M.L.; Sadre, I. Rabies prophylaxis following the feeding of a rabid pony. Clin. Pediatr. 1998, 37, 477–481. [Google Scholar] [CrossRef]
- American Association of Equine Practitioners. Rabies. Available online: https://aaep.org/guidelines/vaccination-guidelines/core-vaccination-guidelines/rabies (accessed on 21 March 2022).
- Zoetis United States. Delivering Complete Core Disease Coverage to Every Horse. Available online: https://www.zoetisus.com/news-and-media/delivering-complete-core-disease-coverage-to-every-horse.aspx (accessed on 23 March 2022).
- Broadway, J. US Horse Population—Statistics. Available online: https://horsecouncil.org/press-releases/us-horse-population-statistics/#:~:text=The%20most%20comprehensive%20number%20comes,7%2C246%2C835%20horses%20in%20the%20US. (accessed on 22 March 2022).
- United States Department of Agriculture Animal and Plant Health Inspection Service Veterinary Services Centers for Epidemiology and Animal Health. Trends in Vaccination Practices on U.S. Equine Operations, 1998–2015. Available online: https://www.aphis.usda.gov/animal_health/nahms/equine/downloads/equine15/Equine15_is_Vaccination.pdf (accessed on 24 March 2022).
- United States Department of Agriculture Animal and Plant Health Inspection Service Veterinary Services Centers for Epidemiology and Animal Health. Vaccination Practices on U.S. Equine Operations. Available online: https://www.aphis.usda.gov/animal_health/nahms/equine/downloads/equine05/Equine05_is_Vaccination_1.pdf (accessed on 24 March 2022).
- Berry, N.J.; Danchin, M.; Trevena, L.; Witteman, H.O.; Kinnersley, P.; Snelling, T.; Robinson, P.; Leask, J. Sharing knowledge about immunisation (SKAI): An exploration of parents’ communication needs to inform development of a clinical communication support intervention. Vaccine 2018, 36, 6480–6490. [Google Scholar] [CrossRef] [PubMed]
- National Centre for Immunisation Research and Surveillance. Sharing Knowledge about Immunisation. Available online: https://talkingaboutimmunisation.org.au/ (accessed on 1 October 2022).
- NPS MedicineWise Learning. Sharing Knowledge about Immunisation. Available online: https://learn.nps.org.au/mod/page/view.php?id=11018#CPD (accessed on 1 October 2022).
- National Centre for Immunisation Research and Surveillance. Sharing Knowledge about Immunisation. Available online: https://ncirs.org.au/our-work/sharing-knowledge-about-immunisation (accessed on 1 October 2022).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).