Attitudes of University Students towards Mandatory COVID-19 Vaccination Policies: A Cross-Sectional Survey in Rome, Italy
Abstract
1. Introduction
2. Materials and Methods
2.1. Setting and Participants
2.2. Questionnaire
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- French, J.; Deshpande, S.; Evans, W. Key Guidelines in Developing a Pre-Emptive COVID-19 Vaccination Uptake Promotion Strategy. Int. J. Environ. Res. Public Health 2020, 17, 5893. [Google Scholar] [CrossRef]
- Schoch-Spana, M.; Brunson, E.K.; Long, R.; Ruth, A.; Ravi, S.J.; Trotochaud, M.; Borio, L.; Brewer, J.; Buccina, J.; Connell, N.; et al. The public’s role in COVID-19 vaccination: Human-centered recommendations to enhance pandemic vaccine awareness, access, and acceptance in the United States. Vaccine 2021, 39, 6004–6012. [Google Scholar] [CrossRef]
- World Health Organization. Report of the Sage Working Group on Vaccine Hesitancy. 2014. Available online: https://www.asset-scienceinsociety.eu/sites/default/files/sage_working_group_revised_report_vaccine_hesitancy.pdf (accessed on 18 November 2022).
- MacDonald, N.E.; Eskola, J.; Liang, X.; Chaudhuri, M.; Dube, E.; Gellin, B.; Goldstein, S.; Larson, H.; Manzo, M.L.; Reingold, A.; et al. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- World Health Organization. Ten Threats to Global Health in 2019. 2019. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 18 November 2022).
- Baccolini, V.; Renzi, E.; Isonne, C.; Migliara, G.; Massimi, A.; De Vito, C.; Marzuillo, C.; Villari, P. COVID-19 vaccine hesitancy among Italian university students: A cross-sectional survey during the first months of the vaccination campaign. Vaccines 2021, 9, 1292. [Google Scholar] [CrossRef] [PubMed]
- Dubé, E.; Gagnon, D.; MacDonald, N.E.; Eskola, J.; Liang, X.; Chaudhuri, M.; Dube, E.; Gellin, B.; Goldstein, S.; Larson, H.; et al. Strategies intended to address vaccine hesitancy: Review of published reviews. Vaccine 2015, 33, 4191–4203. [Google Scholar] [CrossRef]
- Jarrett, C.; Wilson, R.; O’Leary, M.; Eckersberger, E.; Larson, H.J.; Eskola, J.; Liang, X.; Chaudhuri, M.; Dube, E.; Gellin, B.; et al. Strategies for addressing vaccine hesitancy—A systematic review. Vaccine 2015, 33, 4180–4190. [Google Scholar] [CrossRef] [PubMed]
- Vanderslott, S.; Marks, T. Charting mandatory childhood vaccination policies worldwide. Vaccine 2021, 39, 4054–4062. [Google Scholar] [CrossRef] [PubMed]
- Sindoni, A.; Baccolini, V.; Adamo, G.; Massimi, A.; Migliara, G.; De Vito, C.; Marzuillo, C.; Villari, P. Effect of the mandatory vaccination law on measles and rubella incidence and vaccination coverage in Italy (2013–2019). Hum. Vaccines Immunother. 2022, 18, 1950505. [Google Scholar] [CrossRef]
- Squeri, R.; Di Pietro, A.; La Fauci, V.; Genovese, C. Healthcare workers’ vaccination at European and Italian level: A narrative review. Acta Biomed. 2019, 90, 45–53. [Google Scholar] [CrossRef]
- Schumacher, S.; Salmanton-García, J.; Cornely, O.A.; Mellinghoff, S.C. Increasing influenza vaccination coverage in healthcare workers: A review on campaign strategies and their effect. Infection 2021, 49, 387–399. [Google Scholar] [CrossRef]
- Baccolini, V.; Sindoni, A.; Adamo, G.; Rosso, A.; Massimi, A.; Bella, A.; Filia, A.; Magurano, F.; Marzuillo, C.; Villari, P.; et al. Measles among healthcare workers in Italy: Is it time to act? Hum. Vaccines Immunother. 2020, 16, 2618–2627. [Google Scholar] [CrossRef]
- Lytras, T.; Kopsachilis, F.; Mouratidou, E.; Papamichail, D.; Bonovas, S. Interventions to increase seasonal influenza vaccine coverage in healthcare workers: A systematic review and meta-regression analysis. Hum. Vaccines Immunother. 2016, 12, 671–681. [Google Scholar] [CrossRef]
- Pitts, S.I.; Maruthur, N.M.; Millar, K.R.; Perl, T.M.; Segal, J. A systematic review of mandatory influenza vaccination in healthcare personnel. Am. J. Prev. Med. 2014, 47, 330–340. [Google Scholar] [CrossRef] [PubMed]
- Kuznetsova, L.; Cortassa, G.; Trilla, A. Effectiveness of mandatory and incentive-based routine childhood immunization programs in Europe: A systematic review of the literature. Vaccines 2021, 9, 1173. [Google Scholar] [CrossRef] [PubMed]
- Lantos, J.D.; Jackson, M.A.; Opel, D.J.; Marcuse, E.K.; Myers, A.L.; Connelly, B.L. Controversies in Vaccine Mandates. Curr. Probl. Pediatr. Adolesc. Health Care 2010, 40, 38–58. [Google Scholar] [CrossRef]
- Shetty, P. Experts concerned about vaccination backlash. Lancet 2010, 375, 970–971. [Google Scholar] [CrossRef]
- Omer, S.B.; Betsch, C.; Leask, J. Mandate vaccination with care. Nature 2019, 574, 7–10. [Google Scholar] [CrossRef]
- Pitini, E.; Baccolini, V.; Rosso, A.; Massimi, A.; De Vito, C.; Marzuillo, C.; Villari, P. How public health professionals view mandatory vaccination in italy—A cross-sectional survey. Vaccines 2021, 9, 580. [Google Scholar] [CrossRef]
- Karaivanov, A.; Kim, D.; Lu, S.E.; Shigeoka, H. COVID-19 vaccination mandates and vaccine uptake. Nat. Hum. Behav. 2022, 6, 1615–1624. [Google Scholar] [CrossRef]
- Factbox: Countries making COVID-19 vaccines mandatory. Available online: https://www.reuters.com/business/healthcare-pharmaceuticals/countries-making-covid-19-vaccines-mandatory-2021-08-16 (accessed on 18 November 2022).
- Charrier, L.; Garlasco, J.; Thomas, R.; Gardois, P.; Bo, M.; Zotti, C.M. An Overview of Strategies to Improve Vaccination Compliance before and during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 11044. [Google Scholar] [CrossRef] [PubMed]
- Bardosh, K.; De Figueiredo, A.; Gur-Arie, R.; Jamrozik, E.; Doidge, J.; Lemmens, T.; Keshavjee, S.; Graham, J.E.; Baral, S. The unintended consequences of COVID-19 vaccine policy: Why mandates, passports and restrictions may cause more harm than good. BMJ Glob. Health 2022, 7, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Lem, P. Mixed Picture on Mandatory Vaccines. Available online: https://www.researchprofessionalnews.com/rr-news-europe-universities-2021-8-mixed-picture-on-mandatory-vaccines/ (accessed on 16 December 2022).
- Ioannidis, J.P.A. COVID-19 vaccination in children and university students. Eur. J. Clin. Investig. 2021, 51, e13678. [Google Scholar] [CrossRef] [PubMed]
- Burke, C. Should Universities Mandate the COVID-19 Vaccine? J. Physician Assist. Educ. 2021, 32, 189–191. [Google Scholar] [CrossRef]
- Cohen, A.K.; Hoyt, L.T.; Dull, B. A Descriptive Study of COVID-19–Related Experiences and Perspectives of a National Sample of College Students in Spring 2020. J. Adolesc. Health 2020, 67, 369–375. [Google Scholar] [CrossRef]
- Mayan, D.; Nguyen, K.; Keisler, B. National attitudes of medical students towards mandating the COVID-19 vaccine and its association with knowledge of the vaccine. PLoS ONE 2021, 16, e0260898. [Google Scholar] [CrossRef]
- Kakatsaki, I.; Vergadi, E.; Paraskakis, E.; Galanakis, E. Attitudes of junior healthcare professionals towards mandatory vaccination. Vaccine 2022, 40, 2247–2250. [Google Scholar] [CrossRef] [PubMed]
- Baccolini, V.; Siena, L.M.; Renzi, E.; Migliara, G.; Colaprico, C.; Romano, A.; Massimi, A.; Marzuillo, C.; De Vito, C.; Casini, L.; et al. Prevalence of SARS-CoV-2 infection and associated risk factors: A testing program and nested case-control study conducted at Sapienza University of Rome between March and June 2021. Front. Public Health 2022, 10, 1010130. [Google Scholar] [CrossRef]
- Talbot, D.; Massamba, V.K. A descriptive review of variable selection methods in four epidemiologic journals: There is still room for improvement. Eur. J. Epidemiol. 2019, 34, 725–730. [Google Scholar] [CrossRef]
- Vatcheva, K.P.; Lee, M.; McCormick, J.B.; Rahbar, M.H. Multicollinearity in Regression Analyses Conducted in Epidemiologic Studies. Epidemiol. Sunnyvale Calif. 2016, 6, 227. [Google Scholar] [CrossRef]
- Hosmer, D.W.; Lemeshow, S.; Sturdivant, R.X. Assessing the Fit of the Model. In Applied Logistic Regression; Wiley Online Library: Hoboken, NJ, USA, 2013. [Google Scholar]
- Decreto-Legge 26 Novembre 2021, n. 172, Misure Urgenti per il Contenimento Dell’epidemia da COVID-19 e per lo Svolgimento in Sicurezza Delle Attività Economiche e Sociali. Available online: https://www.gazzettaufficiale.it/eli/id/2021/11/26/21G00211/sg (accessed on 19 December 2022).
- Decreto-Legge 1 Aprile 2021, n. 44, Misure Urgenti per il Contenimento Dell’epidemia da COVID-19, in Materia di Vaccinazioni Anti SARS-CoV-2, di Giustizia e di Concorsi Pubblici. Available online: https://www.gazzettaufficiale.it/eli/id/2021/04/01/21G00056/sg (accessed on 19 December 2022).
- Decreto-Legge 7 Gennaio 2022, n. 1, Misure Urgenti per Fronteggiare L’emergenza COVID-19, in Particolare nei Luoghi di Lavoro, Nelle Scuole e Negli Istituti Della Formazione Superiore. Available online: https://www.gazzettaufficiale.it/eli/id/2022/01/07/22G00002/sg (accessed on 19 December 2022).
- Galanakis, E.; D’Ancona, F.; Jansen, A.; Lopalco, P.L. The issue of mandatory vaccination for healthcare workers in Europe. Expert Rev. Vaccines 2014, 13, 277–283. [Google Scholar] [CrossRef]
- Banach, D.B.; Zhang, C.; Factor, S.H.; Calfee, D.P. Support for mandatory health care worker influenza vaccination among allied health professionals, technical staff, and medical students. Am. J. Infect. Control 2013, 41, 354–356. [Google Scholar] [CrossRef]
- Maltezou, H.C.; Pavli, A.; Dedoukou, X.; Georgakopoulou, T.; Raftopoulos, V.; Drositis, I.; Bolikas, E.; Ledda, C.; Adamis, G.; Spyrou, A.; et al. Determinants of intention to get vaccinated against COVID-19 among healthcare personnel in hospitals in Greece. Infect. Dis. Health 2021, 26, 189–197. [Google Scholar] [CrossRef] [PubMed]
- Jain, J.; Saurabh, S.; Kumar, P.; Kumar Verma, M.; Dhanesh Goel, A.; Kumar Gupta, M.; Bhardwaj, P.; Raghav, P.R. COVID-19 vaccine hesitancy among medical students in India. Epidemiol. Infect. 2021, 149, e132. [Google Scholar] [CrossRef] [PubMed]
- Gönüllü, E.; Soysal, A.; Atıcı, S.; Engin, M.; Yeşilbaş, O.; Kasap, T.; Fedakar, A.; Bilgiç, E.; Tavil, E.B.; Tutak, E.; et al. Pediatricians’ COVID-19 experiences and views on the willingness to receive COVID-19 vaccines: A cross-sectional survey in Turkey. Hum. Vaccines Immunother. 2021, 17, 2389–2396. [Google Scholar] [CrossRef]
- Fotiadis, K.; Dadouli, K.; Avakian, I.; Bogogiannidou, Z.; Mouchtouri, V.A.; Gogosis, K.; Speletas, M.; Koureas, M.; Lagoudaki, E.; Kokkini, S.; et al. Factors associated with healthcare workers’ (HCWs) acceptance of COVID-19 vaccinations and indications of a role model towards population vaccinations from a cross-sectional survey in Greece, May 2021. Int. J. Environ. Res. Public Health 2021, 18, 10558. [Google Scholar] [CrossRef] [PubMed]
- Craxì, L.; Casuccio, A.; Amodio, E.; Restivo, V. Who should get COVID-19 vaccine first? A survey to evaluate hospital workers’ opinion. Vaccines 2021, 9, 189. [Google Scholar] [CrossRef]
- Aldosary, A.H.; Alayed, G.H. Willingness to vaccinate against Novel COVID-19 and contributing factors for the acceptance among nurses in Qassim, Saudi Arabia. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 6386–6396. [Google Scholar] [CrossRef]
- Slotte, P.; Karlsson, L.C.; Soveri, A. Attitudes towards mandatory vaccination and sanctions for vaccination refusal. Vaccine 2022, 40, 7378–7388. [Google Scholar] [CrossRef]
- Decreto-Legge 6 Agosto 2021, n. 111, Misure Urgenti per L’esercizio in Sicurezza Delle Attività Scolastiche, Universitarie, Sociali e in Materia di Trasporti. Available online: https://www.gazzettaufficiale.it/eli/id/2021/08/06/21G00125/sg (accessed on 19 December 2022).
- Fine Emergenza Covid-19: Green Pass Base in Università e Afam Fino al 30 Aprile. Available online: https://www.mur.gov.it/it/news/mercoledi-30032022/fine-emergenza-covid-19-green-pass-base-universita-e-afam-fino-al-30-aprile (accessed on 16 December 2022).
- Sprengholz, P.; Korn, L.; Eitze, S.; Felgendreff, L.; Siegers, R.; Goldhahn, L.; De Bock, F.; Huebl, L.; Böhm, R.; Betsch, C. Attitude toward a mandatory COVID-19 vaccination policy and its determinants: Evidence from serial cross-sectional surveys conducted throughout the pandemic in Germany. Vaccine 2022, 40, 7370–7377. [Google Scholar] [CrossRef]
- Sacco, C.; Petrone, D.; Del Manso, M.; Mateo-Urdiales, A.; Fabiani, M.; Bressi, M.; Bella, A.; Pezzotti, P.; Rota, M.C.; Riccardo, F. Risk and protective factors for SARS-CoV-2 reinfections, surveillance data, Italy, August 2021 to March 2022. Euro. Surveill. 2022, 27, 1–7. [Google Scholar] [CrossRef]
- Domnich, A.; Cambiaggi, M.; Vasco, A.; Maraniello, L.; Ansaldi, F.; Baldo, V.; Bonanni, P.; Calabrò, G.E.; Costantino, C.; de Waure, C.; et al. Attitudes and beliefs on influenza vaccination during the covid-19 pandemic: Results from a representative Italian survey. Vaccines 2020, 8, 711. [Google Scholar] [CrossRef]
- Isonne, C.; De Blasiis, M.R.; Turatto, F.; Mazzalai, E.; Marzuillo, C.; De Vito, C.; Villari, P.; Baccolini, V. What Went Wrong with the IMMUNI Contact-Tracing App in Italy? A Cross-Sectional Survey on the Attitudes and Experiences among Healthcare University Students. Life 2022, 12, 871. [Google Scholar] [CrossRef]
- Harris, J.N.; Mauro, C.; Andresen, J.A.; Zimet, G.D.; Rosenthal, S.L. COVID-19 vaccine uptake and attitudes towards mandates in a nationally representative U.S. sample. J. Behav. Med. 2022, 1–15. [Google Scholar] [CrossRef]
- Stojanovic, J.; Boucher, V.G.; Gagne, M.; Gupta, S.; Joyal-Desmarais, K.; Paduano, S.; Aburub, A.S.; Sheinfeld Gorin, S.N.; Kassianos, A.P.; Ribeiro, P.A.B.; et al. Global trends and correlates of covid-19 vaccination hesitancy: Findings from the icare study. Vaccines 2021, 9, 661. [Google Scholar] [CrossRef]
- Vallis, M.; Bacon, S.; Corace, K.; Joyal-Desmarais, K.; Gorin, S.S.; Paduano, S.; Presseau, J.; Rash, J.; Yohannes, A.M.; Lavoie, K. Ending the pandemic: How behavioural science can help optimize global COVID-19 vaccine uptake. Vaccines 2022, 10, 7. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. COVID-19 and Mandatory Vaccination: Ethical Considerations. 2022. Available online: https://www.who.int/publications/i/item/WHO-2019-nCoV-Policy-brief-Mandatory-vaccination-2022.1 (accessed on 16 December 2022).
- Papini, F.; Mazzilli, S.; Paganini, D.; Rago, L.; Arzilli, G.; Pan, A.; Goglio, A.; Tuvo, B.; Privitera, G.; Casini, B. Healthcare Workers Attitudes, Practices and Sources of Information for COVID-19 Vaccination: An Italian National Survey. Int. J. Environ. Res. Public Health 2022, 19, 733. [Google Scholar] [CrossRef] [PubMed]
- Rieger, T.; Schmidt-Petri, C.; Schröder, C. Attitudes Toward Mandatory COVID-19 Vaccination in Germany. Dtsch. Arztebl. Int. 2022, 119, 335–341. [Google Scholar] [CrossRef] [PubMed]
- Siena, L.M.; Isonne, C.; Sciurti, A.; De Blasiis, M.R.; Migliara, G.; Marzuillo, C.; De Vito, C.; Villari, P.; Baccolini, V. The Association of Health Literacy with Intention to Vaccinate and Vaccination Status: A Systematic Review. Vaccines 2022, 10, 1832. [Google Scholar] [CrossRef]
- Tavolacci, M.P.; Dechelotte, P.; Ladner, J. Covid-19 vaccine acceptance, hesitancy, and resistancy among university students in france. Vaccines 2021, 9, 654. [Google Scholar] [CrossRef]
| Total | September– October 2021 | November– December 2021 | January– February 2022 | |
|---|---|---|---|---|
| N = 5287 | N = 1240 | N = 2961 | N = 1086 | |
| Age, years | ||||
| Mean (SD) | 23.9 (4.5) | 24.5 (5.2) | 23.4 (4.0) | 24.6 (4.5) |
| Median (IQR) | 23.1 (21.2–25.2) | 23.2 (21.5–25.8) | 22.7 (21.0–24.6) | 23.8 (21.8–26.1) |
| Gender, N (%) | ||||
| Female | 3580 (67.7) | 823 (66.4) | 2015 (68.1) | 742 (68.3) |
| Male | 1707 (32.3) | 417 (33.6) | 946 (31.9) | 344 (31.7) |
| Nationality, N (%) | ||||
| Italian | 4632 (87.6) | 1036 (83.5) | 2651 (89.5) | 945 (87.0) |
| Non-Italian | 655 (12.4) | 204 (16.5) | 310 (10.5) | 141 (13.0) |
| Area of study, N (%) | ||||
| Healthcare | 1994 (37.7) | 463 (37.3) | 1152 (38.9) | 379 (34.9) |
| Science & Technology | 1628 (30.8) | 315 (25.4) | 960 (32.4) | 353 (32.5) |
| Social Sciences & Humanities | 1665 (31.5) | 462 (37.3) | 849 (28.7) | 354 (32.6) |
| Year of study, N (%) | ||||
| First or second | 3288 (62.2) | 719 (58.0) | 1833 (61.9) | 736 (67.8) |
| Third or above | 1999 (37.8) | 521 (42.0) | 1128 (38.1) | 350 (32.2) |
| Finances, N (%) | ||||
| Many difficulties | 237 (4.5) | 69 (5.6) | 126 (4.3) | 42 (3.9) |
| Some difficulties | 1339 (25.3) | 343 (27.7) | 706 (23.8) | 290 (26.7) |
| Managing well enough | 2753 (52.1) | 615 (49.6) | 1565 (52.9) | 573 (52.8) |
| Managing very well | 958 (18.1) | 213 (17.2) | 564 (19.0) | 181 (16.7) |
| Previous COVID-19 infection, N (%) | ||||
| No infection | 4709 (89.1) | 1113 (89.8) | 2702 (91.3) | 894 (82.3) |
| Asymptomatic or mild symptoms | 501 (9.5) | 112 (9.0) | 227 (7.7) | 162 (14.9) |
| Moderate or severe symptoms | 77 (1.5) | 15 (1.2) | 32 (1.1) | 30 (2.8) |
| Total | September– October 2021 | November– December 2021 | January– February 2022 | |
|---|---|---|---|---|
| N = 5287 | N = 1240 | N = 2961 | N = 1086 | |
| Vaccination status, N (%) | ||||
| Unvaccinated | 103 (1.9) | 54 (4.4) | 43 (1.5) | 6 (0.6) |
| Vaccinated | 5184 (98.1) | 1186 (95.6) | 2918 (98.5) | 1080 (99.4) |
| Reasons for not getting vaccinated (N = 103), N (%) | ||||
| I am suffering from a clinical condition with contraindications to COVID-19 vaccination/waiting for further medical assessment to get vaccinated | 17 (16.5) | 9 (16.7) | 7 (16.3) | 1 (16.7) |
| I’ve already had COVID-19 | 21 (20.4) | 7 (13.0) | 12 (27.9) | 2 (33.3) |
| I’ve booked the vaccination/I am waiting to get vaccinated | 12 (11.7) | 7 (13.0) | 4 (9.3) | 1 (16.7) |
| I don’t consider myself at risk/prefer to obtain natural immunity to COVID-19 | 15 (14.6) | 10 (18.5) | 4 (9.3) | 1 (16.7) |
| I don’t believe in the safety/effectiveness of vaccines against COVID-19 | 33 (32.0) | 21 (38.9) | 12 (27.9) | 0 (0.0) |
| No reason given | 5 (4.9) | 0 (0.0) | 4 (9.3) | 1 (16.7) |
| Vaccine-adverse event (N = 5184), N (%) | ||||
| No adverse event | 1792 (34.6) | 415 (35.0) | 1018 (34.9) | 359 (33.2) |
| Mild adverse event | 2842 (54.8) | 638 (53.8) | 1589 (54.5) | 615 (56.9) |
| Moderate or severe adverse event | 550 (10.6) | 133 (11.2) | 311 (10.7) | 106 (9.8) |
| Perceived COVID-19 severity, mean (SD) | 7.6 (1.9) | 7.6 (2.0) | 7.8 (1.8) | 7.1 (2.0) |
| Concern about the COVID-19 emergency, mean (SD) | 7.5 (2.0) | 7.2 (2.2) | 7.7 (1.9) | 7.3 (2.1) |
| Being afraid of infecting people in the community, mean (SD) | 8.0 (2.3) | 7.8 (2.5) | 8.2 (2.2) | 7.7 (2.4) |
| Being afraid of becoming infected, mean (SD) | 7.4 (2.5) | 7.3 (2.7) | 7.6 (2.5) | 7.2 (2.6) |
| Viewing the vaccine as an effective way to end the pandemic, mean (SD) | 8.8 (2.0) | 8.6 (2.2) | 9.0 (1.8) | 8.6 (2.1) |
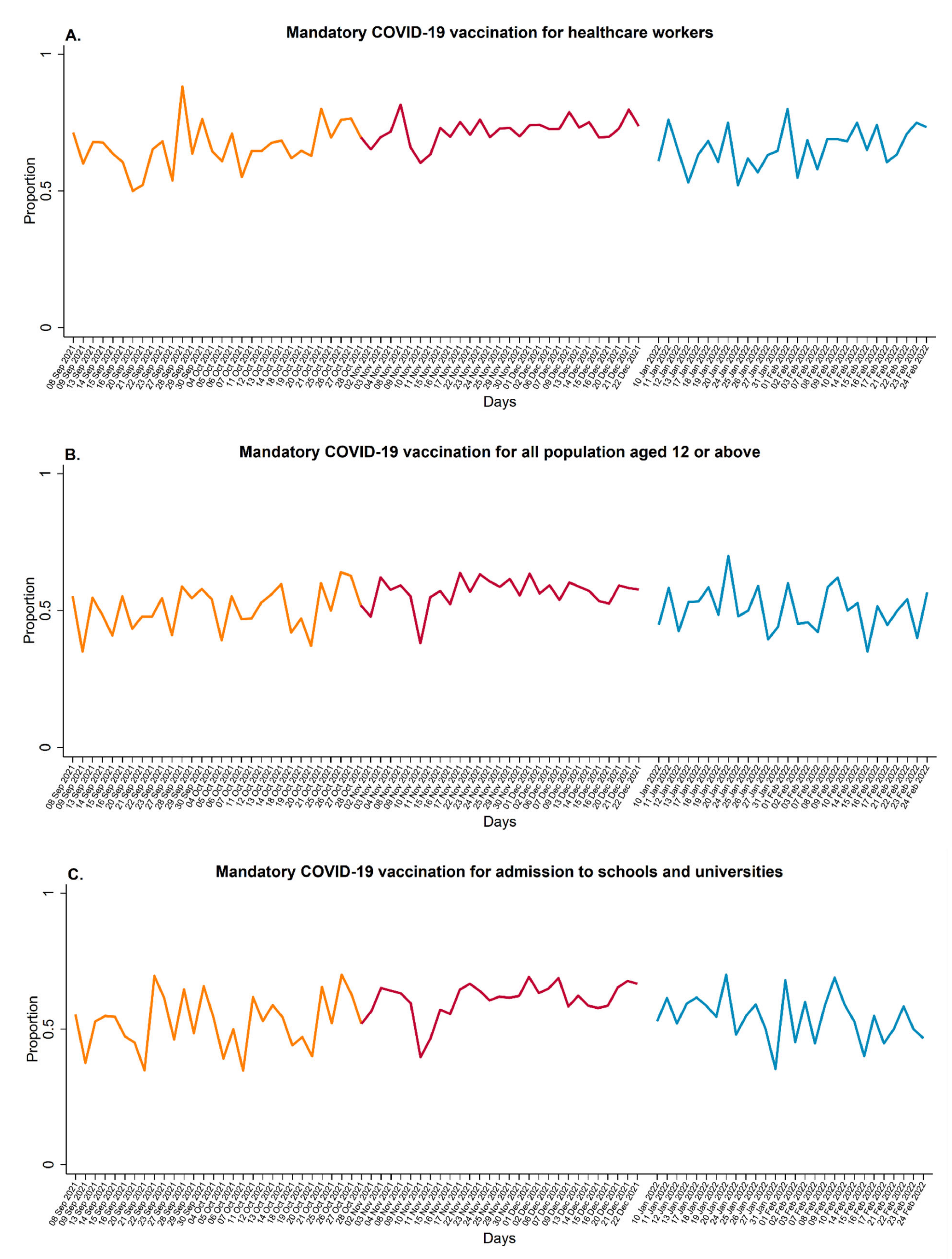
| Attitude towards mandatory COVID-19 vaccination for healthcare workers, N (%) | ||||
| Negative attitude | 1597 (30.2) | 416 (33.5) | 805 (27.2) | 376 (34.6) |
| Positive attitude | 3690 (69.8) | 824 (66.5) | 2156 (72.8) | 710 (65.4) |
| Attitude towards mandatory COVID-19 vaccination for all people aged 12 and above, N (%) | ||||
| Negative attitude | 2398 (45.4) | 602 (48.5) | 1258 (42.5) | 538 (49.5) |
| Positive attitude | 2889 (54.6) | 638 (51.5) | 1703 (57.5) | 548 (50.5) |
| Attitude towards mandatory COVID-19 vaccination for admission to schools and universities, N (%) | ||||
| Negative attitude | 2206 (41.7) | 586 (47.3) | 1125 (38.0) | 495 (45.6) |
| Positive attitude | 3081 (58.3) | 654 (52.7) | 1836 (62.0) | 591 (54.4) |
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| aOR | (95% CI) | p-Value | aOR | (95% CI) | p-Value | aOR | (95% CI) | p-Value | |
| Survey period | |||||||||
| September–October 2021 | Ref. | Ref. | Ref. | ||||||
| November–December 2021 | 1.08 | (0.91–1.28) | 0.371 | 1.09 | (0.94–1.27) | 0.247 | 1.28 | (1.10–1.49) | 0.002 |
| January–February 2022 | 1.01 | (0.82–1.23) | 0.938 | 1.07 | (0.89–1.29) | 0.491 | 1.21 | (1.01–1.46) | 0.045 |
| Vaccination status | |||||||||
| Unvaccinated | Ref. | Ref. | Ref. | ||||||
| Vaccinated | 2.47 | (1.36–4.48) | 0.003 | 1.14 | (0.61–2.10) | 0.684 | 1.81 | (0.96–3.44) | 0.068 |
| Age | 1.00 | (0.98–1.01) | 0.559 | 1.01 | (0.99–1.03) | 0.053 | 1.01 | (0.99–1.03) | 0.055 |
| Gender | |||||||||
| Female | Ref. | Ref. | Ref. | ||||||
| Male | 0.96 | (0.83–1.11) | 0.603 | 1.04 | (0.91–1.19) | 0.585 | 1.06 | (0.93–1.22) | 0.369 |
| Nationality | |||||||||
| Italian | Ref. | Ref. | Ref. | ||||||
| Non-Italian | 0.86 | (0.70–1.06) | 0.168 | 0.93 | (0.76–1.13) | 0.459 | 0.90 | (0.74–1.10) | 0.304 |
| Area of study | |||||||||
| Healthcare | Ref. | Ref. | Ref. | ||||||
| Science & Technology | 0.88 | (0.75–1.05) | 0.157 | 0.86 | (0.74–1.01) | 0.061 | 0.85 | (0.73–0.99) | 0.044 |
| Social Sciences & Humanities | 0.87 | (0.73–1.03) | 0.104 | 0.81 | (0.69–0.94) | 0.006 | 0.80 | (0.69–0.93) | 0.005 |
| Year of study | |||||||||
| First or second | Ref. | Ref. | Ref. | ||||||
| Third or above | 1.00 | (0.86–1.15) | 0.959 | 1.09 | (0.96–1.25) | 0.185 | 1.11 | (0.97–1.27) | 0.138 |
| Finances | |||||||||
| Many or some difficulties | Ref. | Ref. | Ref. | ||||||
| Managing well enough or very well | 1.04 | (0.90–1.20) | 0.609 | 1.04 | (0.91–1.18) | 0.610 | 1.07 | (0.93–1.22) | 0.331 |
| Previous COVID-19 infection | |||||||||
| No infection | Ref. | Ref. | Ref. | ||||||
| Asymptomatic or mild symptoms | 0.86 | (0.69–1.09) | 0.208 | 0.89 | (0.72–1.10) | 0.288 | 0.96 | (0.77–1.19) | 0.720 |
| Moderate or severe symptoms | 0.92 | (0.54–1.59) | 0.776 | 0.87 | (0.52–1.46) | 0.603 | 1.10 | (0.65–1.84) | 0.730 |
| Perceived COVID-19 severity | 1.05 | (1.01–1.10) | 0.027 | 1.05 | (1.01–1.10) | 0.015 | 1.08 | (1.04–1.13) | <0.001 |
| Concern about the COVID-19 emergency | 1.04 | (0.99–1.09) | 0.064 | 1.08 | (1.04–1.13) | <0.001 | 1.09 | (1.04–1.13) | <0.001 |
| Being afraid of becoming infected | 1.01 | (0.98–1.05) | 0.581 | 1.03 | (0.99–1.06) | 0.057 | 1.06 | (1.03–1.10) | <0.001 |
| Being afraid of infecting people in the community | 1.10 | (1.06–1.14) | <0.001 | 1.10 | (1.06–1.14) | <0.001 | 1.08 | (1.04–1.12) | <0.001 |
| Viewing the vaccine as an effective way to end the pandemic | 1.57 | (1.49–1.65) | <0.001 | 1.56 | (1.48–1.64) | <0.001 | 1.49 | (1.42–1.57) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sciurti, A.; Baccolini, V.; Renzi, E.; De Blasiis, M.R.; Siena, L.M.; Isonne, C.; Migliara, G.; Massimi, A.; De Vito, C.; Marzuillo, C.; et al. Attitudes of University Students towards Mandatory COVID-19 Vaccination Policies: A Cross-Sectional Survey in Rome, Italy. Vaccines 2023, 11, 721. https://doi.org/10.3390/vaccines11040721
Sciurti A, Baccolini V, Renzi E, De Blasiis MR, Siena LM, Isonne C, Migliara G, Massimi A, De Vito C, Marzuillo C, et al. Attitudes of University Students towards Mandatory COVID-19 Vaccination Policies: A Cross-Sectional Survey in Rome, Italy. Vaccines. 2023; 11(4):721. https://doi.org/10.3390/vaccines11040721
Chicago/Turabian StyleSciurti, Antonio, Valentina Baccolini, Erika Renzi, Maria Roberta De Blasiis, Leonardo Maria Siena, Claudia Isonne, Giuseppe Migliara, Azzurra Massimi, Corrado De Vito, Carolina Marzuillo, and et al. 2023. "Attitudes of University Students towards Mandatory COVID-19 Vaccination Policies: A Cross-Sectional Survey in Rome, Italy" Vaccines 11, no. 4: 721. https://doi.org/10.3390/vaccines11040721
APA StyleSciurti, A., Baccolini, V., Renzi, E., De Blasiis, M. R., Siena, L. M., Isonne, C., Migliara, G., Massimi, A., De Vito, C., Marzuillo, C., & Villari, P. (2023). Attitudes of University Students towards Mandatory COVID-19 Vaccination Policies: A Cross-Sectional Survey in Rome, Italy. Vaccines, 11(4), 721. https://doi.org/10.3390/vaccines11040721






