Parental Justifications for Not Vaccinating Children or Adolescents against Human Papillomavirus (HPV)
Abstract
1. Introduction
2. Materials and Methods
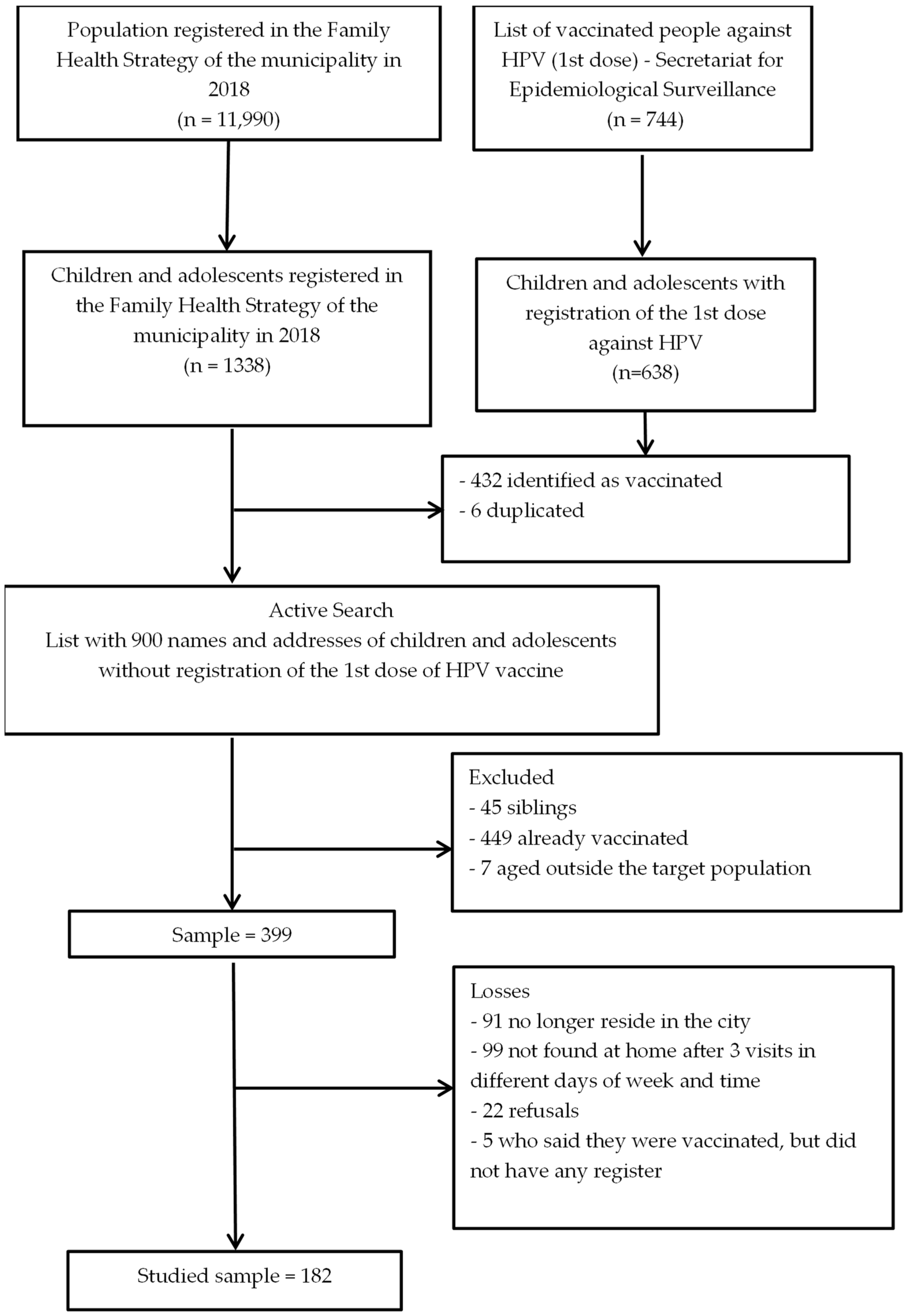
2.1. Study Design and Sample
2.2. Measures
2.3. Analysis
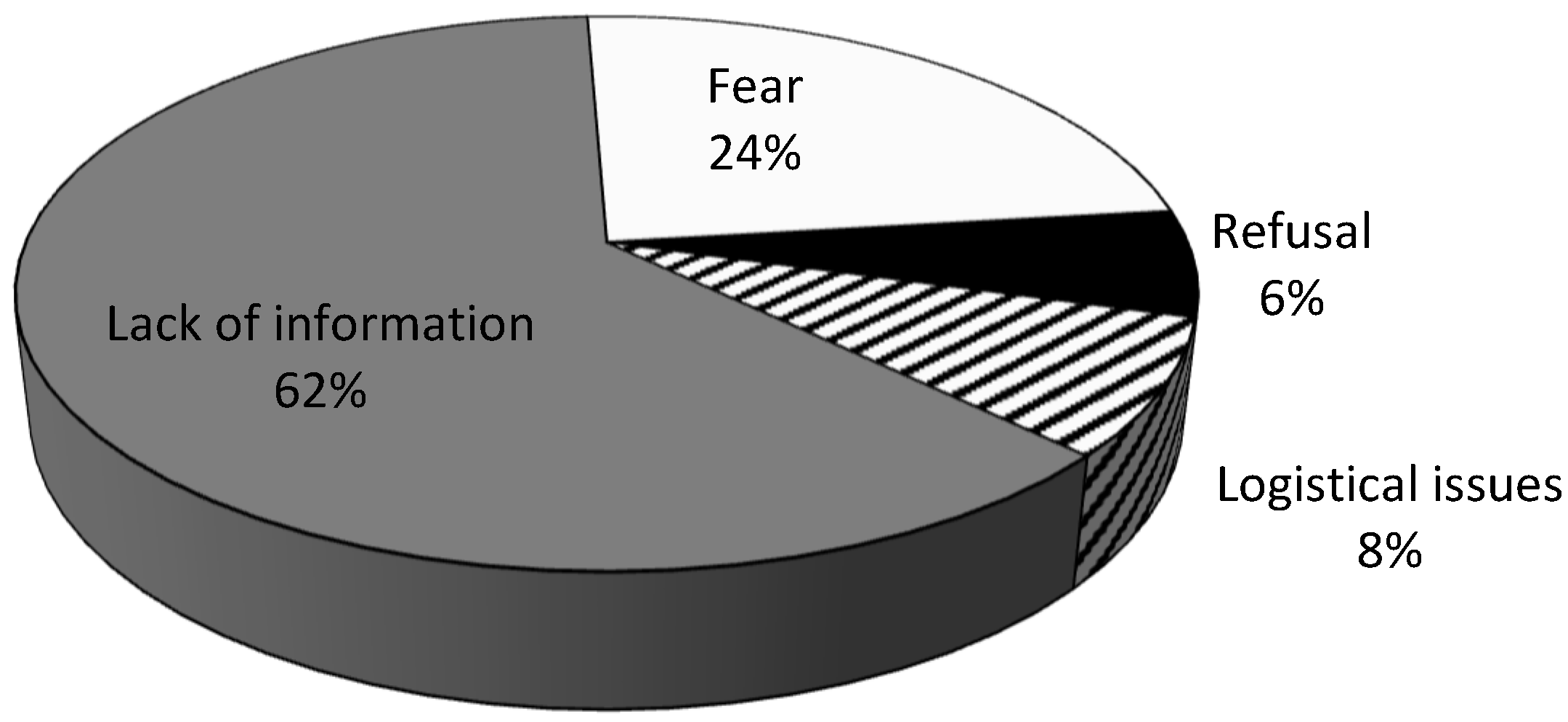
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization Human Papillomavirus (HPV) and Cervical Cancer. Available online: https://www.who.int/news-room/fact-sheets/detail/human-papillomavirus-(hpv)-and-cervical-cancer (accessed on 12 January 2021).
- Malagón, T.; Laurie, C.; Franco, E.L. Human Papillomavirus Vaccination and the Role of Herd Effects in Future Cancer Control Planning: A Review. Expert Rev. Vaccines 2018, 17, 395–409. [Google Scholar] [CrossRef]
- Drolet, M.; Bénard, É.; Pérez, N.; Brisson, M.; Ali, H.; Boily, M.-C.; Baldo, V.; Brassard, P.; Brotherton, J.M.L.; Callander, D.; et al. Population-Level Impact and Herd Effects Following the Introduction of Human Papillomavirus Vaccination Programmes: Updated Systematic Review and Meta-Analysis. Lancet 2019, 394, 497–509. [Google Scholar] [CrossRef]
- Bruni, L.; Diaz, M.; Barrionuevo-Rosas, L.; Herrero, R.; Bray, F.; Bosch, F.X.; de Sanjosé, S.; Castellsagué, X. Global Estimates of Human Papillomavirus Vaccination Coverage by Region and Income Level: A Pooled Analysis. Lancet Glob. Health 2016, 4, e453–e463. [Google Scholar] [CrossRef]
- Global Strategy to Accelerate the Elimination of Cervical Cancer as a Public Health Problem; Licence: CC BY-NC-SA 3.0 IGO; World Health Organization: Geneva, Switzerland, 2020.
- Brisson, M.; Kim, J.J.; Canfell, K.; Drolet, M.; Gingras, G.; Burger, E.A.; Martin, D.; Simms, K.T.; Bénard, É.; Boily, M.C.; et al. Impact of HPV Vaccination and Cervical Screening on Cervical Cancer Elimination: A Comparative Modelling Analysis in 78 Low-Income and Lower-Middle-Income Countries. Lancet 2020, 395, 575–590. [Google Scholar] [CrossRef]
- Pan American Health Organization Vaccine Coverage. Available online: http://ais.paho.org/imm/IM_JRF_COVERAGE.asp (accessed on 9 January 2023).
- Nogueira-Rodrigues, A.; Bukowski, A.; Paulino, E.; St. Louis, J.; Barrichello, A.; Sternberg, C.; Gifoni, M.A.C.; Luciani, S.; Goss, P.E. An Alert to Latin America: Current Human Papillomavirus Vaccination Trends Highlight Key Barriers to Successful Implementation. Cancer 2017, 123, 2193–2199. [Google Scholar] [CrossRef]
- Nogueira-Rodrigues, A.; Flores, M.G.; Macedo Neto, A.O.; Braga, L.A.C.; Vieira, C.M.; de Sousa-Lima, R.M.; de Andrade, D.A.P.; Machado, K.K.; Guimarães, A.P.G. HPV Vaccination in Latin America: Coverage Status, Implementation Challenges and Strategies to Overcome It. Front. Oncol. 2022, 12, 984449. [Google Scholar] [CrossRef]
- Faisal-Cury, A.; Levy, R.B.; Tourinho, M.F.; Grangeiro, A.; Eluf-Neto, J. Vaccination Coverage Rates and Predictors of HPV Vaccination among Eligible and Non-Eligible Female Adolescents at the Brazilian HPV Vaccination Public Program. BMC Public Health 2020, 20, 458. [Google Scholar] [CrossRef]
- Wong, A.; Kraschnewski, J.L.; Spanos, K.E.; Fogel, B.; Calo, W.A. Parental Motivations for Seeking Second Medical Opinions for Their Child’s HPV Vaccine. Prev. Med. Rep. 2021, 24, 101550. [Google Scholar] [CrossRef]
- Kruse, M.H.; Bednarczyk, R.A.; Evans, D.P. A Human Rights Approach to Understanding Provider Knowledge and Attitudes toward the Human Papillomavirus Vaccine in São Paulo, Brazil. Papillomavirus Res. 2020, 9, 100197. [Google Scholar] [CrossRef]
- Mendes Lobão, W.; Duarte, F.G.; Burns, J.D.; de Souza Teles Santos, C.A.; Chagas de Almeida, M.C.; Reingold, A.; Duarte Moreira, E. Low Coverage of HPV Vaccination in the National Immunization Programme in Brazil: Parental Vaccine Refusal or Barriers in Health-Service Based Vaccine Delivery? PLoS ONE 2018, 13, e0206726. [Google Scholar] [CrossRef]
- Patty, N.J.S.; van Dijk, H.M.; Wallenburg, I.; Bal, R.; Helmerhorst, T.J.M.; van Exel, J.; Cramm, J.M. To Vaccinate or Not to Vaccinate? Perspectives on HPV Vaccination among Girls, Boys, and Parents in the Netherlands: A Q-Methodological Study. BMC Public Health 2017, 17, 872. [Google Scholar] [CrossRef] [PubMed]
- de Moura, L.; Codeço, C.T.; Luz, P.M. Human Papillomavirus (HPV) Vaccination Coverage in Brazil: Spatial and Age Cohort Heterogeneity. Rev. Bras. Epidemiol. 2021, 24, e210001. [Google Scholar] [CrossRef]
- Instituto Brasileiro de Geografia e Estatística Indicadores Sociais Municipais: Uma Análise Dos Resultados Do Universo Do Censo Demográfico. Available online: https://cidades.ibge.gov.br/brasil/mg/alterosa/panorama (accessed on 13 April 2022).
- Giovanella, L.; Bousquat, A.; Schenkman, S.; de Almeida, P.F.; Sardinha, L.M.V.; Vieira, M.L.F.P. The Family Health Strategy Coverage in Brazil: What Reveal the 2013 and 2019 National Health Surveys. Cien. Saude Colet. 2021, 26, 2543–2556. [Google Scholar] [CrossRef] [PubMed]
- Rosenstock, I.M. The Health Belief Model and Preventive Health Behavior. Health Educ. Monogr. 1974, 2, 354–386. [Google Scholar] [CrossRef]
- Saulle, R.; Miccoli, S.; Unim, B.; Semyonov, L.; Giraldi, G.; de Vito, E.; Ficarra, M.G.; Firenze, A.; Gregorio, P.; Boccia, A.; et al. Validation of a Questionnaire for Young Women to Assess Knowledge, Attitudes and Behaviors towards Cervical Screening and Vaccination against HPV: Survey among an Italian Sample. Epidemiol. Biostat. Public Health 2013, 11, e8913-1-12. [Google Scholar]
- Restivo, V.; Costantino, C.; Fazio, T.; Casuccio, N.; D’Angelo, C.; Vitale, F.; Casuccio, A. Factors Associated with HPV Vaccine Refusal among Young Adult Women after Ten Years of Vaccine Implementation. Int. J. Environ. Res. Public Health 2018, 15, 770. [Google Scholar] [CrossRef]
- Grandahl, M.; Chun Paek, S.; Grisurapong, S.; Sherer, P.; Tydén, T.; Lundberg, P. Parents’ Knowledge, Beliefs, and Acceptance of the HPV Vaccination in Relation to Their Socio-Demographics and Religious Beliefs: A Cross-Sectional Study in Thailand. PLoS ONE 2018, 13, e0193054. [Google Scholar] [CrossRef]
- Marlow, L.A.V.; Waller, J.; Evans, R.E.C.; Wardle, J. Predictors of Interest in HPV Vaccination: A Study of British Adolescents. Vaccine 2009, 27, 2483–2488. [Google Scholar] [CrossRef]
- Donadiki, E.M.; Jiménez-García, R.; Hernández-Barrera, V.; Sourtzi, P.; Carrasco-Garrido, P.; López de Andrés, A.; Jimenez-Trujillo, I.; Velonakis, E.G. Health Belief Model Applied to Non-Compliance with HPV Vaccine among Female University Students. Public Health 2014, 128, 268–273. [Google Scholar] [CrossRef]
- Loke, A.Y.; Kwan, M.L.; Wong, Y.-T.; Wong, A.K.Y. The Uptake of Human Papillomavirus Vaccination and Its Associated Factors Among Adolescents: A Systematic Review. J. Prim. Care Community Health 2017, 8, 349–362. [Google Scholar] [CrossRef]
- Grandahl, M.; Oscarsson, M.; Stenhammar, C.; Nevéus, T.; Westerling, R.; Tydén, T. Not the Right Time: Why Parents Refuse to Let Their Daughters Have the Human Papillomavirus Vaccination. Acta Paediatr. Int. J. Paediatr. 2014, 103, 436–441. [Google Scholar] [CrossRef] [PubMed]
- Krawczyk, A.; Knäuper, B.; Gilca, V.; Dubé, E.; Perez, S.; Joyal-Desmarais, K.; Rosberger, Z. Parents’ Decision-Making about the Human Papillomavirus Vaccine for Their Daughters: I. Quantitative Results. Hum. Vaccines Immunother. 2015, 11, 322–329. [Google Scholar] [CrossRef] [PubMed]
- Olagoke, A.; Caskey, R.; Floyd, B.; Hebert-Beirne, J.; Boyd, A.; Molina, Y. The Interdependent Roles of the Psychosocial Predictors of Human Papillomavirus Vaccination among Christian Parents of Unvaccinated Adolescents. Hum. Vaccin. Immunother. 2021, 17, 5433–5438. [Google Scholar] [CrossRef]
- Frio, G.S.; França, M.T.A. Human Papillomavirus Vaccine and Risky Sexual Behavior: Regression Discontinuity Design Evidence from Brazil. Econ. Hum. Biol. 2021, 40, 100946. [Google Scholar] [CrossRef]
- Cunningham-Erves, J.; Hull, P.C.; Wilkins, C.H.; Edwards, K.M.; Davis, M.; Jones, J.; Graham, J.; Adekunle, A.; Dempsey, A.F. Healthcare Providers’ Practice Protocols, Strategies, and Needed Tools to Address Parental HPV Vaccine Hesitancy: An Exploratory Study. Hum. Vaccin. Immunother. 2022, 18, 2136862. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.; Mullen, J.; Smith, D.; Kotarba, M.; Kaplan, S.J.; Tu, P. Healthcare Providers’ Vaccine Perceptions, Hesitancy, and Recommendation to Patients: A Systematic Review. Vaccines 2021, 9, 713. [Google Scholar] [CrossRef]
- Manoel, A.L.; Rodrigues, A.B.; Piva, E.Z.; Warpechowski, T.P.; Schuelter-Trevisol, F. Evaluation of Knowledge about the Human Papilloma Virus (HPV) and Its Vaccination among Community Health Agents in the Municipality of Tubarão, Santa Catarina, Brazil, in 2014. Epidemiol. E Serv. Saude Rev. Do Sist. Unico Saude Do Bras. 2017, 26, 399–404. [Google Scholar] [CrossRef]
- Hohenberger, G.F.; Kops, N.L.; Bessel, M.; Horvath, J.D.; Wendland, E.M. Perception of Primary Health Care Professionals as Participants in a National Survey about HPV in Brazil: An Experience Report. Epidemiol. E Serviços Saúde 2019, 28, e2018234. [Google Scholar] [CrossRef]
- Sato, A.P.S. What Is the Importance of Vaccine Hesitancy in the Drop of Vaccination Coverage in Brazil? Rev. Saude Publica 2018, 52, 96. [Google Scholar] [CrossRef]
- Instituto de Estudos Para Políticas de Saúde; Nunes, L. [Vaccination Coverage in Brazil]. Available online: https://ieps.org.br/wp-content/uploads/2021/05/Panorama_IEPS_01.pdf (accessed on 6 February 2023).
- Horvath, J.D.C.; Kops, N.L.; Caierão, J.; Bessel, M.; Hohenberger, G.; Wendland, E.M. Human Papillomavirus Knowledge, Beliefs, and Behaviors: A Questionnaire Adaptation. Eur. J. Obstet. Gynecol. Reprod. Biol. 2018, 230, 103–108. [Google Scholar] [CrossRef]
- Ebert, J.F.; Huibers, L.; Christensen, B.; Christensen, M.B. Paper- or Web-Based Questionnaire Invitations as a Method for Data Collection: Cross-Sectional Comparative Study of Differences in Response Rate, Completeness of Data, and Financial Cost. J. Med. Internet Res. 2018, 20, e24. [Google Scholar] [CrossRef] [PubMed]
- Wei, Z.; Liu, Y.; Zhang, L.; Sun, X.; Jiang, Q.; Li, Z.; Wu, Y.; Fu, C. Stages of HPV Vaccine Hesitancy Among Guardians of Female Secondary School Students in China. J. Adolesc. Health 2022, 72, 73–79. [Google Scholar] [CrossRef]
- Rujumba, J.; Akugizibwe, M.; Basta, N.E.; Banura, C. Why Don’t Adolescent Girls in a Rural Uganda District Initiate or Complete Routine 2-Dose HPV Vaccine Series: Perspectives of Adolescent Girls, Their Caregivers, Healthcare Workers, Community Health Workers and Teachers. PLoS ONE 2021, 16, e0253735. [Google Scholar] [CrossRef]
- Sallam, M.; Al-Mahzoum, K.; Eid, H.; Assaf, A.M.; Abdaljaleel, M.; Al-Abbadi, M.; Mahafzah, A. Attitude towards Hpv Vaccination and the Intention to Get Vaccinated among Female University Students in Health Schools in Jordan. Vaccines 2021, 9, 1432. [Google Scholar] [CrossRef]
- Sidiropoulou, M.; Gerogianni, G.; Kourti, F.E.; Pappa, D.; Zartaloudi, A.; Koutelekos, I.; Dousis, E.; Margari, N.; Mangoulia, P.; Ferentinou, E.; et al. Perceptions, Knowledge and Attitudes among Young Adults about Prevention of HPV Infection and Immunization. Healthcare 2022, 10, 1721. [Google Scholar] [CrossRef]
| Category | Questions |
|---|---|
| Perceived benefits of vaccines | I have no confidence in vaccines |
| Vaccines are not effective in preventing diseases | |
| It is not necessary to take all vaccines | |
| It is preferable to contract the disease to obtain natural protection | |
| Perceived benefits of the HPV vaccine | I do not consider the HPV vaccine safe |
| I believe that if I receive the HPV vaccine, I will not be protected against cervical cancer | |
| I believe that if I receive the HPV vaccine, I will not be protected against HPV | |
| The HPV vaccine prevents the appearance of genital warts (condyloma) | |
| The HPV vaccine prevents cervical cancer | |
| Perceived barriers to vaccination | I don’t have enough information about vaccine-preventable infections |
| I don’t have enough information about vaccines | |
| The vaccination unit is difficult to access | |
| Perceived barriers to HPV vaccination | The pediatrician/general practitioner discouraged me from taking <the teenager> to get the HPV vaccine |
| Social media / internet discouraged me from getting the HPV vaccine | |
| The HPV vaccine has severe side effects | |
| It is difficult to find the vaccine at the clinic | |
| Perceived vulnerability | I think the <adolescent> is too young to think about sexually transmitted diseases |
| Women can be infected with HPV | |
| Men can be infected with HPV | |
| Perceived severity | HPV can cause a serious illness |
| Cervical cancer can be dangerous and lead to death | |
| HPV can cause other types of cancer |
| Categories | Reasons for Non-Vaccination | n | % |
|---|---|---|---|
| Lack of information | Not receiving guidance from a health professional | 94 | 51.7 |
| Did not know about the vaccine | 39 | 21.4 | |
| Child/adolescent is very young | 3 | 1.7 | |
| Child/adolescent is not sexually active | 3 | 1.7 | |
| Fear or refusal | Fear of injection | 29 | 15.9 |
| Fear of side effects | 15 | 8.2 | |
| Mentioned news or social network coverage | 10 | 5.5 | |
| Child/adolescent refused | 8 | 4.4 | |
| I don’t believe in this vaccine | 6 | 3.3 | |
| Religion prohibited vaccination | 2 | 1.1 | |
| Logistic issues | Forgetfulness | 12 | 6.6 |
| Lack of time | 8 | 4.4 | |
| Tried, but vaccination unit was closed | 7 | 3.9 | |
| Shortage of vaccine | 3 | 1.7 | |
| Restricted vaccination hours | 1 | 0.6 | |
| Other reasons | 8 | 4.4 |
| Total Sample | Lack of Information (n = 110) | Fear or Refusal (n = 53) | Logistical Issues (n = 14) | ||
|---|---|---|---|---|---|
| Characteristics | n (%) * | n (%) ** | n (%) ** | n (%) ** | p-Value |
| Age (in years) | |||||
| ≤40 | 66 (37.3) | 35 (53.0) | 24 (36.4) | 7 (10.6) | 0.293 a |
| 41 to 49 | 69 (39.0) | 44 (63.8) | 20 (29.0) | 5 (7.3) | |
| ≥50 | 42 (23.7) | 31 (73.8) | 9 (21.4) | 2 (7.8) | |
| Sex | |||||
| Male | 13 (7.3) | 8 (61.5) | 4 (30.8) | 1 (7.7) | 1.000 b |
| Female | 164 (92.7) | 102 (62.2) | 49 (29.9) | 13 (7.9) | |
| Relationship with the child/adolescent | |||||
| Father/mother | 158 (89.3) | 98 (62.0) | 46 (29.1) | 14 (8.9) | 0.363 a |
| Other | 19 (10.7) | 12 (63.2) | 7 (36.8) | 0 (0.0) | |
| Religion (n = 175) | |||||
| Catholic | 123 (70.3) | 77 (62.6) | 37 (30.1) | 9 (7.3) | 0.630 b |
| Christian | 42 (24.0) | 25 (59.5) | 14 (33.3) | 3 (7.1) | |
| Other | 10 (5.7) | 6 (60.0) | 2 (20.0) | 2 (20.0) | |
| Social status (n = 172) | |||||
| A–B | 46 (26.7) | 32 (69.6) | 12 (26.1) | 2 (4.4) | 0.608 b |
| C | 82 (47.7) | 50 (61.0) | 24 (29.3) | 8 (9.8) | |
| D–E | 44 (25.6) | 24 (54.6) | 16 (36.4) | 4 (9.1) | |
| Children/adolescent | |||||
| age (in years) | |||||
| ≤15 | 71 (40.1) | 39 (54.9) | 24 (33.8) | 8 (11.3) | 0.424 a |
| 16–17 | 70 (39.5) | 47 (67.1) | 20 (28.6) | 3 (4.3) | |
| ≥18 | 36 (20.3) | 24 (66.7) | 9 (25.0) | 3 (8.3) | |
| Sex | |||||
| Male | 93 (52.5) | 64 (68.8) | 20 (21.5) | 9 (9.7) | 0.033 a |
| Female | 84 (47.5) | 46 (54.8) | 33 (39.3) | 5 (6.0) |
| Domains | Lack of Information | Fear or Refusal | Logistical Issues | p-Value |
|---|---|---|---|---|
| Mean (95%CI) | Mean (95%CI) | Mean (95%CI) | ||
| Knowledge about HPV | 3.33 (3.17–3.49) | 3.25 (3.00–3.50) | 3.05 (2.35–3.74) | 0.503 |
| Knowledge about prevention | 4.18 (4.04–4.31) | 4.19 (3.97–4.41) | 3.79 (2.94–4.63) | 0.221 |
| Perceived benefits of vaccines | 4.06 (3.92–4.20) | 3.97 (3.68–4.25) | 4.14 (3.36–4.92) | 0.746 |
| Perceived benefits of HPV vaccine | 3.62 (3.43–3.81) | 3.58 (3.32–3.85) | 3.82 (3.21–4.42) | 0.752 |
| Perceived barriers of vaccines | 2.98 (2.83–3.12) | 3.06 (2.81–3.31) | 2.92 (2.38–3.46) | 0.771 |
| Perceived barriers of HPV vaccines | 3.44 (3.29–3.59) | 3.36 (3.10–3.62) | 3.21 (2.48–3.95) | 0.635 |
| Perceived vulnerability | 3.81 (3.67–3.95) | 3.84 (3.60–4.07) | 4.31 (3.94–4.68) | 0.094 |
| Perceived gravity | 3.72 (3.56–3.89) | 3.77 (3.53–4.01) | 4.05 (3.63–4.48) | 0.422 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodrigues, E.S.; Mendes, E.D.T.; Nucci, L.B. Parental Justifications for Not Vaccinating Children or Adolescents against Human Papillomavirus (HPV). Vaccines 2023, 11, 506. https://doi.org/10.3390/vaccines11030506
Rodrigues ES, Mendes EDT, Nucci LB. Parental Justifications for Not Vaccinating Children or Adolescents against Human Papillomavirus (HPV). Vaccines. 2023; 11(3):506. https://doi.org/10.3390/vaccines11030506
Chicago/Turabian StyleRodrigues, Eliza S., Elisa D. T. Mendes, and Luciana B. Nucci. 2023. "Parental Justifications for Not Vaccinating Children or Adolescents against Human Papillomavirus (HPV)" Vaccines 11, no. 3: 506. https://doi.org/10.3390/vaccines11030506
APA StyleRodrigues, E. S., Mendes, E. D. T., & Nucci, L. B. (2023). Parental Justifications for Not Vaccinating Children or Adolescents against Human Papillomavirus (HPV). Vaccines, 11(3), 506. https://doi.org/10.3390/vaccines11030506






