Incremental Net Benefit and Incremental Cost-Effectiveness Ratio of COVID-19 Vaccination Campaigns: Systematic Review of Cost-Effectiveness Evidence
Abstract
:1. Introduction
2. Materials and Methods
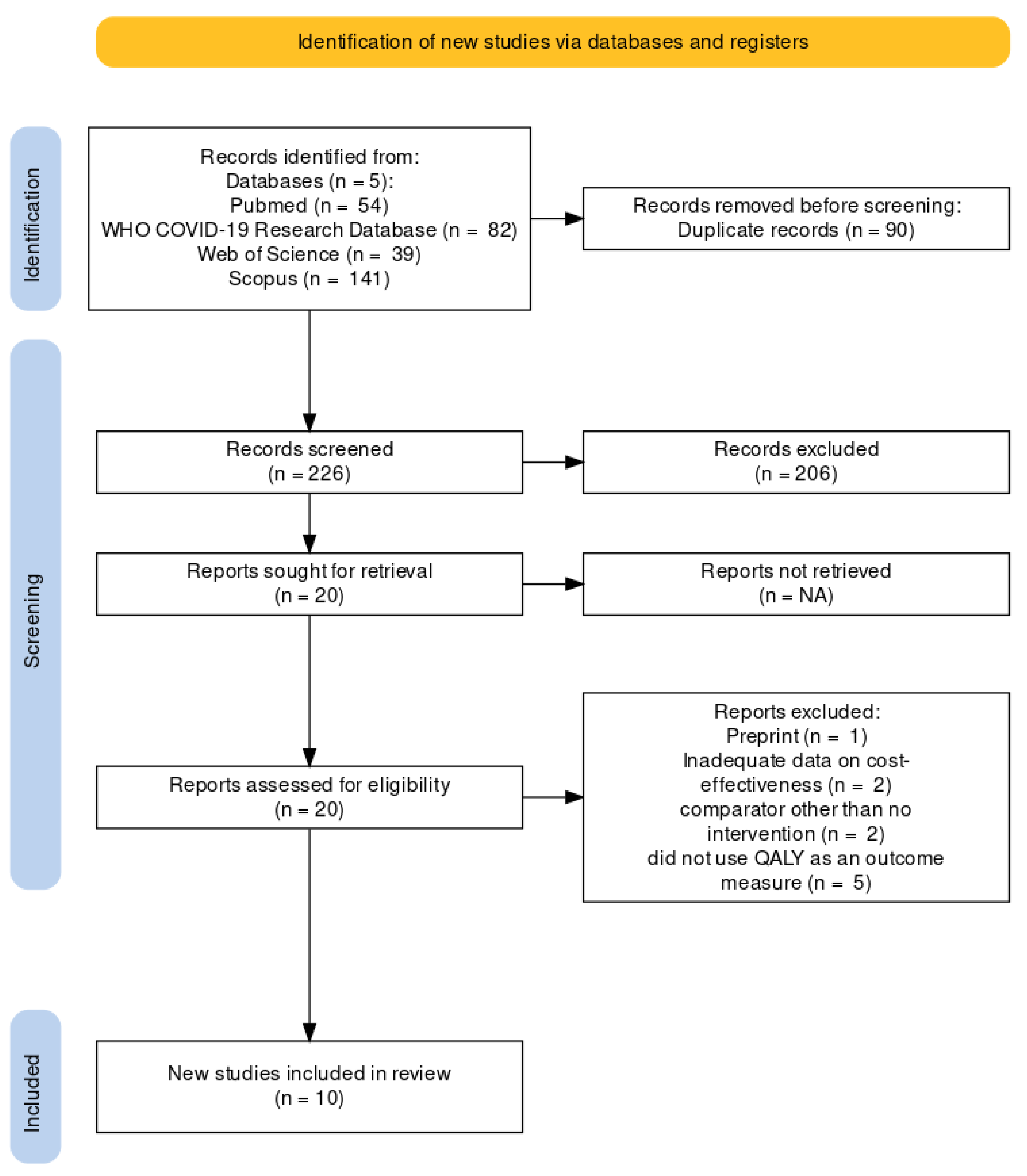
2.1. Study Design and Search Strategy
2.2. Study Selection
2.3. Quality Assessment
2.4. Data Extraction
2.5. Data Synthesis
3. Results
3.1. Study Selection
3.2. Study Characteristics
3.3. Quality Assessment
| Author, Year | Country | WHO Region | GDP Per Capita | Type of Vaccine | Perspective | Outcome Measure | Currency | Intervention Costs (I$) | Comparator Costs (I$) | Intervention Effects (QALYs) | Comparator Effects (QALYs) | ICER (I$/QALY) | NMB (I$) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wang et al., 2021 [23] | Israel | EUR | 39,481 | mRNA (Comirnaty) | Health system Societal | ICER | USD | 1,577,960 | 4,278,161 | 1,798,286 | 1,790,002 | −326 | Not reported |
| ibidem | mRNA (Moderna) | 1,338,638 | 4,278,161 | 1,798,120 | 1,790,002 | −362 | |||||||
| ibidem | Viral vector (Vaxzevria) | 1,694,309 | 4,278,161 | 1,797,458 | 1,790,002 | −347 | |||||||
| Debrabant et al., 2021 [24] | Denmark | EUR | 61,063 | mRNA | Health system | ICER | DKK | 45,281,649.8 | 88,429,852.1 | −714 | −5410 | 8193.7–18,242.5 | Not reported |
| Jiang et al., 2022 [25] | Hong Kong | WPR | 46,324 | inactivated | Societal | ICER/INB | USD | 76,643,624 | 96,007,188 | −181 | −218 | Cost-saving | 45,379,143 |
| ibidem | Indonesia | SEAR | 3870 | 44,388,774 | 48,144,281 | −544 | −570 | 5,662,212 | |||||
| ibidem | PRC | WPR | 10,435 | 20,625,625 | 23,056,317 | −189 | −205 | 8,645,824 | |||||
| ibidem | Philippines | WPR | 3299 | 17,608,767 | 17,850,779 | −925 | −972 | 1,019,699 | |||||
| ibidem | Singapore | WPR | 59,798 | 52,772,707 | 101,156,430 | −202 | −231 | 28,632,981 | |||||
| ibidem | Thailand | SEAR | 7187 | 79,995,715 | 94,299,089 | −3391 | −3989 | 7,984,741 | |||||
| Sandmann et al., 2021 [26] | United Kingdom | EUR | 41,059 | Not stated | Health system | INB | GBP | 215 × 109 | 130 × 109 | −78,900,000 | −93,100,000 | Not reported | 737.1 × 109 |
| Marco-Franco et al., 2021 [27] | Spain | EUR | 30,116 | Not stated | Health system | ICER | EUR | Not stated | Not stated | Not stated | Not stated | 8565 | Not reported |
| Hagens et al., 2021 [31] | Turkey | EUR | 8536 | Not stated | Health system Societal | ICER | USD | 1,339,290,179 | 407,011,036 | Not stated | Not stated | 1250 | Not reported |
| Kohli et al., 2021 [28] | United States | AMR | 63,593 | Not stated | Health system | ICER | USD | 29.4 × 106 | 21.3 × 106 | not stated | not stated | 8476 | Not reported |
| Kirwin et al., 2021 [32] | Canada | AMR | 67,656 | mRNA | Health system | NMB | CAD | Not stated | Not stated | not stated | not stated | Not reported | 240.9 × 106 |
| Padula et al., 2021 [29] | United States | AMR | 63,593 | Not stated | Health system | ICER | USD | 13.5 × 109 | 34.9 × 109 | −0.879 | −0.899 | Cost-saving | Not reported |
| Fernandes et al., 2022 [30] | Brazil | AMR | 7519 | Inactivated (CoronaVac) | Health system | ICER | USD | 121 per patient | 88.55 per patient | 0.87 | 0.869 | 17,758 | Not reported |
| ibidem | Viral vector (Vaxzevria) | 41.1 per patient | 88.55 per patient | 0.871 | 0.869 | −23,161 | |||||||
| ibidem | Viral vector (Janssen) | 77.8 per patient | 88.55 per patient | 0.87 | 0.869 | −1690.8 |
3.4. Vaccination Cost-Effectiveness
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 29 December 2022).
- World Bank. Global Economic Prospects, June 2020; World Bank: Washington, DC, USA, 2020. [Google Scholar] [CrossRef]
- Coronavirus Disease (COVID-19): Vaccines. Available online: https://www.who.int/news-room/questions-and-answers/item/coronavirus-disease-(covid-19)-vaccines?gclid=CjwKCAiAz--OBhBIEiwAG1rIOgyiVjv0V25YyulXzGkzeHf0jwEHjPOvq5bBTiuv9M0g6o2GBLzxzxoCZB8QAvD_BwEtopicsurvey=v8kj13 (accessed on 30 December 2022).
- The Different Types of COVID-19 Vaccines. Available online: https://www.who.int/news-room/feature-stories/detail/the-race-for-a-covid-19-vaccine-explained (accessed on 27 December 2022).
- Acosta-Coley, I.; Cervantes-Ceballos, L.; Tejeda-Benítez, L.; Sierra-Márquez, L.; Cabarcas-Montalvo, M.; García-Espiñeira, M.; Coronell-Rodríguez, W.; Arroyo-Salgado, B. Vaccines Platforms and COVID-19: What You Need to Know. Trop. Dis. Travel Med. Vaccines 2022, 8, 20. [Google Scholar] [CrossRef]
- Sridhar, S.; Brokstad, K.; Cox, R. Influenza Vaccination Strategies: Comparing Inactivated and Live Attenuated Influenza Vaccines. Vaccines 2015, 3, 373–389. [Google Scholar] [CrossRef]
- Wang, N.; Shang, J.; Jiang, S.; Du, L. Subunit Vaccines Against Emerging Pathogenic Human Coronaviruses. Front. Microbiol. 2020, 11, 298. [Google Scholar] [CrossRef]
- van Riel, D.; de Wit, E. Next-Generation Vaccine Platforms for COVID-19. Nat. Mater. 2020, 19, 810–812. [Google Scholar] [CrossRef]
- University of Oxford. Coronavirus (COVID-19) Vaccinations. Our World in Data. Available online: https://ourworldindata.org/covid-vaccinations. (accessed on 29 December 2022).
- Africa Clocks Fastest Surge in COVID-19 Cases This Year, but Deaths Remain Low. WHO Africa. Available online: https://www.afro.who.int/news/africa-clocks-fastest-surge-covid-19-cases-year-deaths-remain-low (accessed on 30 December 2022).
- Drummond, M. Methods for the Economic Evaluation of Health Care Programmes; Oxford medical publications; Fourth edition.; Oxford University Press: Oxford, UK; New York, NY, USA, 2015; ISBN 978-0-19-966588-4. [Google Scholar]
- World Health Organization. WHO Guide for Standardization of Economic Evaluations of Immunization Programmes, 2nd ed.; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- Hoch, J.S.; Dewa, C.S. A Clinician’s Guide to Correct Cost-Effectiveness Analysis: Think Incremental Not Average. Can. J. Psychiatry 2008, 53, 267–274. [Google Scholar] [CrossRef] [PubMed]
- Ramsey, S.; Willke, R.; Briggs, A.; Brown, R.; Buxton, M.; Chawla, A.; Cook, J.; Glick, H.; Liljas, B.; Petitti, D.; et al. Good Research Practices for Cost-Effectiveness Analysis Alongside Clinical Trials: The ISPOR RCT-CEA Task Force Report. Value Health 2005, 8, 521–533. [Google Scholar] [CrossRef] [PubMed]
- Elliott, R.; Payne, K. Essentials of Economic Evaluation in Healthcare, 1st ed.; Pharmaceutical Press: London, UK, 2005. [Google Scholar]
- Willan, A.R. Incremental Net Benefit in the Analysis of Economic Data from Clinical Trials, with Application to the CADET-Hp Trial. Eur. J. Gastroenterol. Hepatol. 2004, 16, 543–549. [Google Scholar] [CrossRef] [PubMed]
- Stinnett, A.A.; Mullahy, J. Net Health Benefits: A New Framework for the Analysis of Uncertainty in Cost-Effectiveness Analysis. Med. Decis. Making 1998, 18 (Suppl. 2), S68–S80. [Google Scholar] [CrossRef]
- Doran, C.M. Economic Evaluation of Interventions to Treat Opiate Dependence: A Review of the Evidence. PharmacoEconomics 2008, 26, 371–393. [Google Scholar] [CrossRef]
- International Monetary Fund. Consumer Price Index (CPI). Available online: https://data.imf.org/?sk=4FFB52B2-3653-409A-B471-D47B46D904B5&sId=1485878855236 (accessed on 7 August 2022).
- OECD. Purchasing Power Parities (PPP). 2022. Available online: https://data.oecd.org/conversion/purchasing-power-parities-ppp.htm (accessed on 7 August 2022).
- The Joanna Briggs Institute. The Joanna Briggs Institute Joanna Briggs Institute Reviewers’ Manual. Available online: https://nursing.lsuhsc.edu/JBI/docs/ReviewersManuals/Economic.pdf (accessed on 11 September 2022).
- Iino, H.; Hashiguchi, M.; Hori, S. Estimating the Range of Incremental Cost-Effectiveness Thresholds for Healthcare Based on Willingness to Pay and GDP per Capita: A Systematic Review. PLoS ONE 2022, 17, e0266934. [Google Scholar] [CrossRef]
- Wang, W.-C.; Fann, J.C.-Y.; Chang, R.-E.; Jeng, Y.-C.; Hsu, C.-Y.; Chen, H.-H.; Liu, J.-T.; Yen, A.M.-F. Economic Evaluation for Mass Vaccination against COVID-19. J. Formos. Med. Assoc. 2021, 120, S95–S105. [Google Scholar] [CrossRef] [PubMed]
- Debrabant, K.; Grønbæk, L.; Kronborg, C. The Cost-Effectiveness of a COVID-19 Vaccine in a Danish Context. Clin. Drug Investig. 2021, 41, 975–988. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.; Cai, D.; Shi, S. Economic Evaluations of Inactivated COVID-19 Vaccines in Six Western Pacific and South East Asian Countries and Regions: A Modeling Study. Infect. Dis. Model. 2022, 7, 109–121. [Google Scholar] [CrossRef]
- Sandmann, F.G.; Davies, N.G.; Vassall, A.; Edmunds, W.J.; Jit, M.; Sun, F.Y.; Villabona-Arenas, C.J.; Nightingale, E.S.; Showering, A.; Knight, G.M.; et al. The Potential Health and Economic Value of SARS-CoV-2 Vaccination alongside Physical Distancing in the UK: A Transmission Model-Based Future Scenario Analysis and Economic Evaluation. Lancet Infect. Dis. 2021, 21, 962–974. [Google Scholar] [CrossRef]
- Marco-Franco, J.E.; Pita-Barros, P.; González-de-Julián, S.; Sabat, I.; Vivas-Consuelo, D. Simplified Mathematical Modelling of Uncertainty: Cost-Effectiveness of COVID-19 Vaccines in Spain. Mathematics 2021, 9, 566. [Google Scholar] [CrossRef]
- Kohli, M.; Maschio, M.; Becker, D.; Weinstein, M.C. The Potential Public Health and Economic Value of a Hypothetical COVID-19 Vaccine in the United States: Use of Cost-Effectiveness Modeling to Inform Vaccination Prioritization. Vaccine 2021, 39, 1157–1164. [Google Scholar] [CrossRef]
- Padula, W.V.; Malaviya, S.; Reid, N.M.; Cohen, B.G.; Chingcuanco, F.; Ballreich, J.; Tierce, J.; Alexander, G.C. Economic Value of Vaccines to Address the COVID-19 Pandemic: A U.S. Cost-Effectiveness and Budget Impact Analysis. J. Med. Econ. 2021, 24, 1060–1069. [Google Scholar] [CrossRef]
- Fernandes, R.R.A.; da Silva Santos, M.; da Silva Magliano, C.A.; Tura, B.R.; Macedo, L.S.D.N.; Padila, M.P.; França, A.C.W.; Braga, A.A. Cost Utility of Vaccination Against COVID-19 in Brazil. Value Health Reg. Issues 2022, 31, 18–24. [Google Scholar] [CrossRef]
- Hagens, A.; İnkaya, A.Ç.; Yildirak, K.; Sancar, M.; van der Schans, J.; Acar Sancar, A.; Ünal, S.; Postma, M.; Yeğenoğlu, S. COVID-19 Vaccination Scenarios: A Cost-Effectiveness Analysis for Turkey. Vaccines 2021, 9, 399. [Google Scholar] [CrossRef]
- Kirwin, E.; Rafferty, E.; Harback, K.; Round, J.; McCabe, C. A Net Benefit Approach for the Optimal Allocation of a COVID-19 Vaccine. PharmacoEconomics 2021, 39, 1059–1073. [Google Scholar] [CrossRef]
- WHO Regional Offices. World Health Organizaton. Available online: https://www.who.int/about/who-we-are/regional-offices (accessed on 20 November 2022).
- Pugh, S.J.; Fletcher, M.A.; Charos, A.; Imekraz, L.; Wasserman, M.; Farkouh, R. Cost-Effectiveness of the Pneumococcal Conjugate Vaccine (10- or 13-Valent) Versus No Vaccination for a National Immunization Program in Tunisia or Algeria. Infect. Dis. Ther. 2019, 8, 63–74. [Google Scholar] [CrossRef] [PubMed]
- Rafferty, E.R.S.; McDonald, W.; Osgood, N.D.; Doroshenko, A.; Farag, M. What We Know Now: An Economic Evaluation of Chickenpox Vaccination and Dose Timing Using an Agent-Based Model. Value Health 2021, 24, 50–60. [Google Scholar] [CrossRef] [PubMed]
- Scholz, S.M.; Weidemann, F.; Damm, O.; Ultsch, B.; Greiner, W.; Wichmann, O. Cost-Effectiveness of Routine Childhood Vaccination Against Seasonal Influenza in Germany. Value Health 2021, 24, 32–40. [Google Scholar] [CrossRef] [PubMed]
- Syeed, M.S.; Ghule, P.; Le, L.M.; Veettil, S.K.; Horn, E.K.; Perdrizet, J.; Wasserman, M.; Thakkinstian, A.; Chaiyakunapruk, N. Pneumococcal Vaccination in Children: A Systematic Review and Meta-Analysis of Cost-Effectiveness Studies. Value Health 2022, S1098301522046927. [Google Scholar] [CrossRef]
- Yue, M.; Dickens, B.L.; Yoong, J.S.; I-Cheng Chen, M.; Teerawattananon, Y.; Cook, A.R. Cost-Effectiveness Analysis for Influenza Vaccination Coverage and Timing in Tropical and Subtropical Climate Settings: A Modeling Study. Value Health 2019, 22, 1345–1354. [Google Scholar] [CrossRef] [PubMed]
- Bartsch, S.M.; Wedlock, P.T.; O’Shea, K.J.; Cox, S.N.; Strych, U.; Nuzzo, J.B.; Ferguson, M.C.; Bottazzi, M.E.; Siegmund, S.S.; Hotez, P.J.; et al. Lives and Costs Saved by Expanding and Expediting Coronavirus Disease 2019 Vaccination. J. Infect. Dis. 2021, 224, 938–948. [Google Scholar] [CrossRef]
- Calabro’, G.E.; Carini, E.; Tognetto, A.; Giacchetta, I.; Bonanno, E.; Mariani, M.; Ricciardi, W.; de Waure, C. The Value(s) of Vaccination: Building the Scientific Evidence According to a Value-Based Healthcare Approach. Front. Public Health 2022, 10, 786662. [Google Scholar] [CrossRef]
- de Waure, C.; Calabrò, G.E.; Ricciardi, W. Recommendations to Drive a Value-Based Decision-Making on Vaccination. Expert Rev. Vaccines 2022, 21, 289–296. [Google Scholar] [CrossRef]
- World Health Organization. Regional Office for Europe, European Observatory on Health Systems and Policies & McDaid, D. In Using Economic Evidence to Help Make the Case for Investing in Health Promotion and Disease Prevention; World Health Organization. Regional Office for Europe, European Observatory on Health Systems and Policies: Geneva, Switzerland.
- Smith, P.C.; Sagan, A.; Siciliani, L.; Panteli, D.; McKee, M.; Soucat, A.; Figueras, J. Building on Value-Based Health Care: Towards a Health System Perspective; European Observatory Policy Briefs; European Observatory on Health Systems and Policies: Copenhagen, Denmark, 2020. [Google Scholar]
- European Commission. Directorate General for Health and Food Safety. Defining Value in ‘Value-Based Healthcare’: Report of the Expert Panel on Effective Ways of Investing in Health (EXPH); Publications Office: Luxembourg, 2019.
- Gross, D.P.; Sampat, B.N. The Economics of Crisis Innovation Policy: A Historical Perspective. AEA Pap. Proc. 2021, 111, 346–350. [Google Scholar] [CrossRef]
- Hodes, S.; Majeed, A. Building a Sustainable Infrastructure for Covid-19 Vaccinations Long Term. BMJ 2021, 373, n1578. [Google Scholar] [CrossRef]
- Majeed, A.; Pollock, K.; Hodes, S.; Papaluca, M. Implementation of Covid-19 Vaccination in the United Kingdom. BMJ 2022, 378, e070344. [Google Scholar] [CrossRef] [PubMed]
- Deb, P.; Furceri, D.; Jimenez, D.; Kothari, S.; Ostry, J.D.; Tawk, N. The Effects of COVID-19 Vaccines on Economic Activity. Swiss J. Econ. Stat. 2022, 158, 3. [Google Scholar] [CrossRef] [PubMed]
- Working for Global Equitable Access to COVID-19 Vaccines. COVAX. Available online: https://www.who.int/initiatives/act-accelerator/covax (accessed on 22 November 2022).
- Goldberg, Y.; Mandel, M.; Bar-On, Y.M.; Bodenheimer, O.; Freedman, L.S.; Ash, N.; Alroy-Preis, S.; Huppert, A.; Milo, R. Protection and Waning of Natural and Hybrid Immunity to SARS-CoV-2. N. Engl. J. Med. 2022, 386, 2201–2212. [Google Scholar] [CrossRef]
- Menni, C.; May, A.; Polidori, L.; Louca, P.; Wolf, J.; Capdevila, J.; Hu, C.; Ourselin, S.; Steves, C.J.; Valdes, A.M.; et al. COVID-19 Vaccine Waning and Effectiveness and Side-Effects of Boosters: A Prospective Community Study from the ZOE COVID Study. Lancet Infect. Dis. 2022, 22, 1002–1010. [Google Scholar] [CrossRef] [PubMed]
- Franco-Paredes, C. Transmissibility of SARS-CoV-2 among Fully Vaccinated Individuals. Lancet Infect. Dis. 2022, 22, 16. [Google Scholar] [CrossRef] [PubMed]
- Revealing the Hidden Value of Vaccines. Available online: https://www.nature.com/articles/d42473-021-00520-w (accessed on 10 October 2022).
- Gianino, M.M.; Nurchis, M.C.; Politano, G.; Rousset, S.; Damiani, G. Evaluation of the Strategies to Control COVID-19 Pandemic in Four European Countries. Front. Public Health 2021, 9, 700811. [Google Scholar] [CrossRef]
- Mohammed, I.; Nauman, A.; Paul, P.; Ganesan, S.; Chen, K.-H.; Jalil, S.M.S.; Jaouni, S.H.; Kawas, H.; Khan, W.A.; Vattoth, A.L.; et al. The Efficacy and Effectiveness of the COVID-19 Vaccines in Reducing Infection, Severity, Hospitalization, and Mortality: A Systematic Review. Hum. Vaccines Immunother. 2022, 18, 2027160. [Google Scholar] [CrossRef]
- Thompson, J.; Wattam, S. Estimating the Impact of Interventions against COVID-19: From Lockdown to Vaccination. PLoS ONE 2021, 16, e0261330. [Google Scholar] [CrossRef]
| Items | Wang et al. [23] | Debrabant et al. [24] | Jiang et al. [25] | Marco-Franco et al. [27] | Padula et al. [29] | Sandmann et al. [26] | Hagens et al. [31] | Kohli et al. [28] | Kirwin et al. [32] | Fernandes et al. [30] |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Was a well-defined question posed in an answerable form? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 2. Was a comprehensive description of the competing alternatives given (i.e., can you tell who did what to whom, where, and how often)? | No | No | No | No | No | Yes | No | No | Yes | No |
| 3. Was the effectiveness of the program or services established? | Yes | Yes | Yes | Yes | No | No | Yes | No | No | Yes |
| 4. Were all the important and relevant costs and consequences for each alternative identified? | No | No | No | No | Yes | Yes | Yes | No | Yes | Yes |
| 5. Were costs and consequences measured accurately in appropriate physical units? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 6. Were costs and consequences valued credibly? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 7. Were costs and consequences adjusted for differential timing? | Unclear | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes |
| 8. Was an incremental analysis of costs and consequences of alternatives performed? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 9. Was allowance made for uncertainty in the estimates of costs and consequences? | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes |
| 10. Did the presentation and discussion of study results include all issues of concern to users? | Yes | Unclear | Unclear | No | Yes | Yes | Unclear | No | No | Yes |
| Total score | 7 | 7 | 7 | 6 | 7 | 9 | 8 | 6 | 8 | 9 |
| First Author, Year, Country [Ref] | Costs * | Health Outcomes ** | Judgement |
|---|---|---|---|
| Wang et al., 2021, Israel [23] | − | + | Favored |
| Debrabant et al., 2021, Denmark [24] | − | + | Favored |
| Jiang et al., 2022, Hong Kong, Indonesia, mainland China, Philippines, Singapore, and Thailand [25] | − | + | Favored |
| Sandmann et al., 2021, United Kingdom [26] | + | + | Unclear |
| Marco-Franco et al., 2021, Spain [27] | N/A | N/A | N/a |
| Hagens et al., 2021, Turkey [26] | + | + | Unclear |
| Kohli et al., 2021, United States [28] | + | + | Unclear |
| Kirwin et al., 2021, Canada [32] | N/A | N/A | N/a |
| Padula et al., 2021, United States [29] | − | + | Favored |
| Fernandes et al., 2022 † Brazil [30] | + | + | Unclear |
| Fernandes et al., 2022 ‡, Brazil [30] | − | + | Favored |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Santoli, G.; Nurchis, M.C.; Calabrò, G.E.; Damiani, G. Incremental Net Benefit and Incremental Cost-Effectiveness Ratio of COVID-19 Vaccination Campaigns: Systematic Review of Cost-Effectiveness Evidence. Vaccines 2023, 11, 347. https://doi.org/10.3390/vaccines11020347
Santoli G, Nurchis MC, Calabrò GE, Damiani G. Incremental Net Benefit and Incremental Cost-Effectiveness Ratio of COVID-19 Vaccination Campaigns: Systematic Review of Cost-Effectiveness Evidence. Vaccines. 2023; 11(2):347. https://doi.org/10.3390/vaccines11020347
Chicago/Turabian StyleSantoli, Giuseppe, Mario Cesare Nurchis, Giovanna Elisa Calabrò, and Gianfranco Damiani. 2023. "Incremental Net Benefit and Incremental Cost-Effectiveness Ratio of COVID-19 Vaccination Campaigns: Systematic Review of Cost-Effectiveness Evidence" Vaccines 11, no. 2: 347. https://doi.org/10.3390/vaccines11020347
APA StyleSantoli, G., Nurchis, M. C., Calabrò, G. E., & Damiani, G. (2023). Incremental Net Benefit and Incremental Cost-Effectiveness Ratio of COVID-19 Vaccination Campaigns: Systematic Review of Cost-Effectiveness Evidence. Vaccines, 11(2), 347. https://doi.org/10.3390/vaccines11020347






