The Challenges of Vaccine Trial Participation among Underserved and Hard-to-Reach Communities: An Internal Expert Consultation of the VACCELERATE Consortium
Abstract
:1. Introduction
2. Materials and Methods
2.1. Identification of Underserved/HTR Groups in Terms of Vaccine Trial Participation and Prioritization for Education on Vaccine Trials
2.2. Barriers of Underserved/HTR Groups to Participating in Vaccine Clinical Trials
2.3. Reasons Why Stakeholders Have Difficulties in Recruiting Underserved/HTR Groups in Vaccine Clinical Trials
2.4. Data Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Park, J.J.H.; Mogg, R.; Smith, G.E.; Nakimuli-Mpungu, E.; Jehan, F.; Rayner, C.R.; Condo, J.; Decloedt, E.H.; Nachega, J.B.; Reis, G.; et al. How COVID-19 has fundamentally changed clinical research in global health. Lancet Glob. Health 2021, 9, e711–e720. [Google Scholar] [CrossRef] [PubMed]
- Xiao, H.; Vaidya, R.; Liu, F.; Chang, X.; Xia, X.; Unger, J.M. Sex, Racial, and Ethnic Representation in COVID-19 Clinical Trials: A Systematic Review and Meta-analysis. JAMA Intern. Med. 2023, 183, 50–60. [Google Scholar] [CrossRef]
- Flanagan, S.M.; Hancock, B. ‘Reaching the hard to reach’—Lessons learned from the VCS (voluntary and community Sector). A qualitative study. BMC Health Serv. Res. 2010, 10, 92. [Google Scholar] [CrossRef] [PubMed]
- Avnir, Y.; Watson, C.T.; Glanville, J.; Peterson, E.C.; Tallarico, A.S.; Bennett, A.S.; Qin, K.; Fu, Y.; Huang, C.-Y.; Beigel, J.H.; et al. IGHV1-69 polymorphism modulates anti-influenza antibody repertoires, correlates with IGHV utilization shifts and varies by ethnicity. Sci. Rep. 2016, 6, 20842. [Google Scholar] [CrossRef]
- Wang, L.-Y.; Hu, C.-T.; Ho, T.-Y.; Lin, H.H. Geographic and ethnic variations of long-term efficacy and immunogenicity of hepatitis B vaccination in Hualien, a HBV hyperendemic area. Vaccine 2006, 24, 4427–4432. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.; Carter, B.; Gifford, D.K. Predicted Cellular Immunity Population Coverage Gaps for SARS-CoV-2 Subunit Vaccines and Their Augmentation by Compact Peptide Sets. Cell Syst. 2021, 12, 102–107.e104. [Google Scholar] [CrossRef]
- Gray, D.M., II; Nolan, T.S.; Gregory, J.; Joseph, J.J. Diversity in clinical trials: An opportunity and imperative for community engagement. Lancet Gastroenterol. Hepatol. 2021, 6, 605–607. [Google Scholar] [CrossRef]
- VACCELERATE-European Corona Vaccine Trial Accelerator Platform. Available online: https://vaccelerate.eu/ (accessed on 12 April 2023).
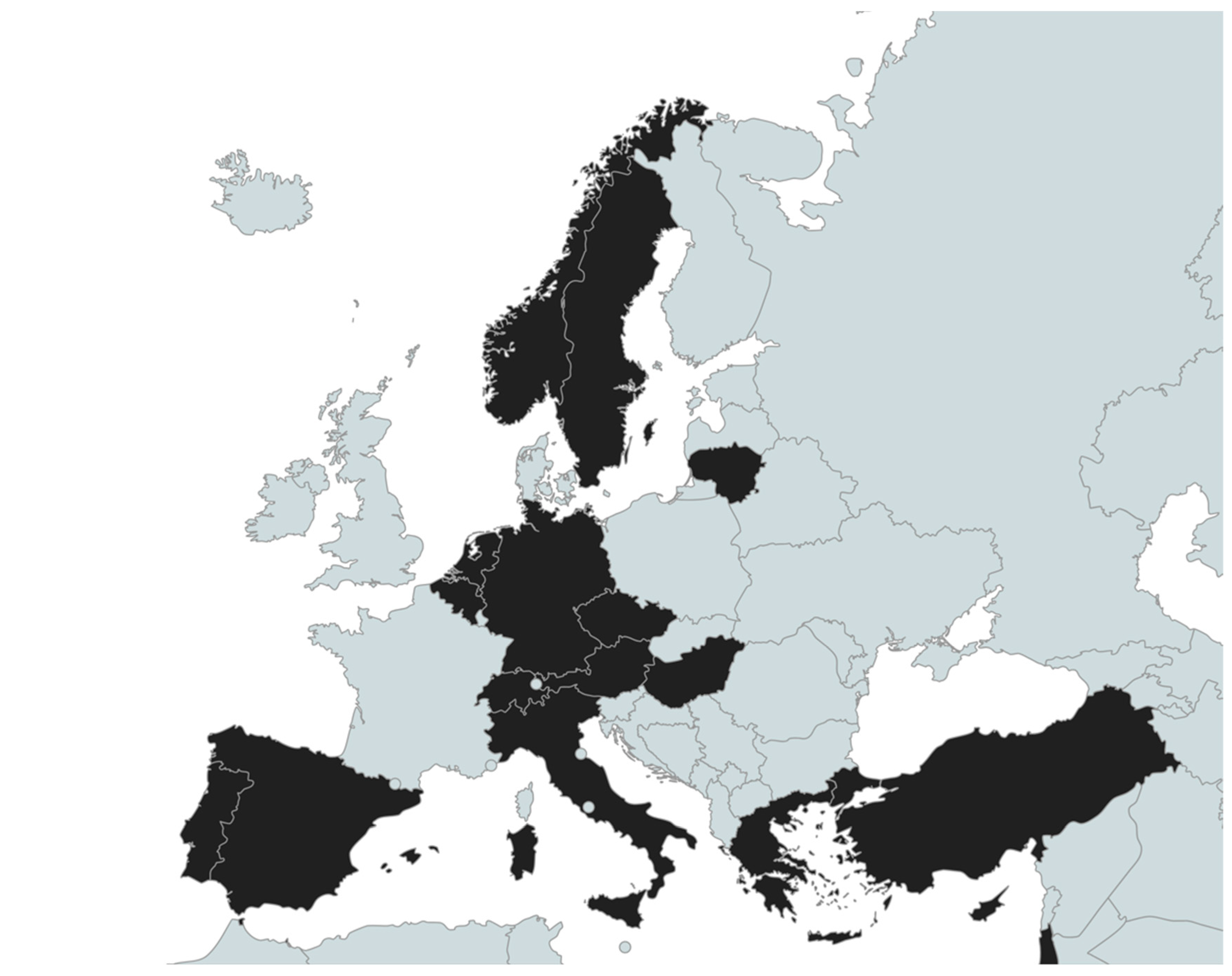
- Salmanton-García, J.; Stewart, F.A.; Heringer, S.; Koniordou, M.; Álvarez-Barco, E.; Argyropoulos, C.D.; Themistocleous, S.C.; Valle-Simón, P.; Spivak, O.; Součková, L.; et al. VACCELERATE Volunteer Registry: A European study participant database to facilitate clinical trial enrolment. Vaccine 2022, 40, 4090–4097. [Google Scholar] [CrossRef]
- Salmanton-García, J.; Wipfler, P.; Valle-Simón, P.; Merakou, C.; Kopsidas, I.; Bethe, U.; Steinbach, A.; Spivak, O.; Součková, L.; Mendonça, M.A.; et al. VACCELERATE Site Network: Real-time definition of clinical study capacity in Europe. Vaccine 2023, 41, 3915–3922. [Google Scholar] [CrossRef]
- Ekezie, W.; Awwad, S.; Krauchenberg, A.; Karara, N.; Dembiński, Ł.; Grossman, Z.; Del Torso, S.; Dornbusch, H.J.; Neves, A.; Copley, S.; et al. Access to Vaccination among Disadvantaged, Isolated and Difficult-to-Reach Communities in the WHO European Region: A Systematic Review. Vaccines 2022, 10, 1038. [Google Scholar] [CrossRef]
- Robinson, R.; Nguyen, E.; Wright, M.; Holmes, J.; Oliphant, C.; Cleveland, K.; Nies, M.A. Factors contributing to vaccine hesitancy and reduced vaccine confidence in rural underserved populations. Humanit. Soc. Sci. Commun. 2022, 9, 416. [Google Scholar] [CrossRef]
- Argyropoulos, C.D.; Leckler, J.; Salmanton-García, J.; Constantinou, M.; Alexandrou, A.; Themistocleous, S.; Noula, E.; Shiamakkides, G.; Nearchou, A.; Stewart, F.A.; et al. Enhancing Public Health Communication Regarding Vaccine Trials: Design and Development of the Pan-European VACCELERATE Toolkit. JMIR Public Health Surveill. 2023, 9, e44491. [Google Scholar] [CrossRef] [PubMed]
- Shaghaghi, A.; Bhopal, R.S.; Sheikh, A. Approaches to Recruiting ‘Hard-To-Reach’ Populations into Re-search: A Review of the Literature. Health Promot. Perspect. 2011, 1, 86–94. [Google Scholar] [CrossRef] [PubMed]
- Ojha, R.P.; Jackson, B.E.; Lu, Y.; Burton, M.; Blair, S.E.; MacDonald, B.R.; Chu, T.C.; Teigen, K.J.; Acosta, M. Participation and retention can be high in randomized controlled trials targeting underserved populations: A systematic review and meta-analysis. J. Clin. Epidemiol. 2018, 98, 154–157. [Google Scholar] [CrossRef] [PubMed]
- Treweek, S.; Banister, K.; Bower, P.; Cotton, S.; Devane, D.; Gardner, H.R.; Isaacs, T.; Nestor, G.; Oshisanya, A.; Parker, A.; et al. Developing the INCLUDE Ethnicity Framework—A tool to help trialists design trials that better reflect the communities they serve. Trials 2021, 22, 337. [Google Scholar] [CrossRef] [PubMed]
- Witham, M.D.; Anderson, E.; Carroll, C.; Dark, P.M.; Down, K.; Hall, A.S.; Knee, J.; Maier, R.H.; Mountain, G.A.; Nestor, G.; et al. Developing a roadmap to improve trial delivery for under-served groups: Results from a UK multi-stakeholder process. Trials 2020, 21, 694. [Google Scholar] [CrossRef] [PubMed]
- Kelsey, M.D.; Patrick-Lake, B.; Abdulai, R.; Broedl, U.C.; Brown, A.; Cohn, E.; Curtis, L.H.; Komelasky, C.; Mbagwu, M.; Mensah, G.A.; et al. Inclusion and diversity in clinical trials: Actionable steps to drive lasting change. Contemp. Clin. Trials 2022, 116, 106740. [Google Scholar] [CrossRef] [PubMed]
- Etti, M.; Fofie, H.; Razai, M.; Crawshaw, A.F.; Hargreaves, S.; Goldsmith, L.P. Ethnic minority and migrant underrepresentation in COVID-19 research: Causes and solutions. eClinicalMedicine 2021, 36, 100903. [Google Scholar] [CrossRef] [PubMed]
- Amorrortu, R.P.; Arevalo, M.; Vernon, S.W.; Mainous, A.G.; Diaz, V.; McKee, M.D.; Ford, M.E.; Tilley, B.C. Recruitment of racial and ethnic minorities to clinical trials conducted within specialty clinics: An intervention mapping approach. Trials 2018, 19, 115. [Google Scholar] [CrossRef]
- Taylor, O.; Loubiere, S.; Tinland, A.; Vargas-Moniz, M.; Spinnewijn, F.; Manning, R.; Gaboardi, M.; Wolf, J.R.L.M.; Bokszczanin, A.; Bernad, R.; et al. Lifetime, 5-year and past-year prevalence of homelessness in Europe: A cross-national survey in eight European nations. BMJ Open 2019, 9, e033237. [Google Scholar] [CrossRef]
- Ojo-Fati, O.; Joseph, A.M.; Ig-Izevbekhai, J.; Thomas, J.L.; Everson-Rose, S.A.; Pratt, R.; Raymond, N.; Cooney, N.L.; Luo, X.; Okuyemi, K.S. Practical issues regarding implementing a randomized clinical trial in a homeless population: Strategies and lessons learned. Trials 2017, 18, 305. [Google Scholar] [CrossRef]
- Young, M.-E.D.T.; Madrigal, D.S. Documenting legal status: A systematic review of measurement of undocumented status in health research. Public Health Rev. 2017, 38, 26. [Google Scholar] [CrossRef] [PubMed]
- Magee, L.; Knights, F.; McKechnie, D.G.J.; Al-bedaery, R.; Razai, M.S. Facilitators and barriers to COVID-19 vaccination uptake among ethnic minorities: A qualitative study in primary care. PLoS ONE 2022, 17, e0270504. [Google Scholar] [CrossRef] [PubMed]
- Luís, C.; Di Marzo, V.R.; Kaur, M.; Argyropoulos, C.D.; Devane, D.; Stewart, F.A.; Antoniou, G.; Hendrickx, G.; Askling, H.H.; Hellemans, M. Vaccination rates in Europe are not associated with online media intensity. J. Sci. Commun. 2022, 21. [Google Scholar] [CrossRef]
- Daniels, D.; Imdad, A.; Buscemi-Kimmins, T.; Vitale, D.; Rani, U.; Darabaner, E.; Shaw, A.; Shaw, J. Vaccine hesitancy in the refugee, immigrant, and migrant population in the United States: A systematic review and meta-analysis. Hum. Vaccines Immunother. 2022, 18, 2131168. [Google Scholar] [CrossRef] [PubMed]
- Hildreth, J.E.K.; Alcendor, D.J. Targeting COVID-19 Vaccine Hesitancy in Minority Populations in the US: Implications for Herd Immunity. Vaccines 2021, 9, 489. [Google Scholar] [CrossRef] [PubMed]
- Heller, C.; Balls-Berry, J.E.; Nery, J.D.; Erwin, P.J.; Littleton, D.; Kim, M.; Kuo, W.P. Strategies addressing barriers to clinical trial enrollment of underrepresented populations: A systematic review. Contemp. Clin. Trials 2014, 39, 169–182. [Google Scholar] [CrossRef] [PubMed]
- Yasmin, F.; Najeeb, H.; Moeed, A.; Naeem, U.; Asghar, M.S.; Chughtai, N.U.; Yousaf, Z.; Seboka, B.T.; Ullah, I.; Lin, C.Y.; et al. COVID-19 Vaccine Hesitancy in the United States: A Systematic Review. Front. Public Health 2021, 9, 770985. [Google Scholar] [CrossRef]
- Tankwanchi, A.S.; Bowman, B.; Garrison, M.; Larson, H.; Wiysonge, C.S. Vaccine hesitancy in migrant communities: A rapid review of latest evidence. Curr. Opin. Immunol. 2021, 71, 62–68. [Google Scholar] [CrossRef]
- Gupta, P.S.; Mohareb, A.M.; Valdes, C.; Price, C.; Jollife, M.; Regis, C.; Munshi, N.; Taborda, E.; Lautenschlager, M.; Fox, A.; et al. Expanding COVID-19 vaccine access to underserved populations through implementation of mobile vaccination units. Prev. Med. 2022, 163, 107226. [Google Scholar] [CrossRef]
- Allison, K.; Patel, D.; Kaur, R. Assessing Multiple Factors Affecting Minority Participation in Clinical Trials: Development of the Clinical Trials Participation Barriers Survey. Cureus 2022, 14, e24424. [Google Scholar] [CrossRef] [PubMed]
- Staples, J.N.; Lester, J.; Li, A.; Walsh, C.; Cass, I.; Karlan, B.Y.; Bresee, C.; Rimel, B.J. Language as a barrier to cancer clinical trial accrual: Assessing consenting team knowledge and practices for cancer clinical trial consent among low English fluency patients. Appl. Cancer Res. 2018, 38, 14. [Google Scholar] [CrossRef]
- Woll, A.; Quick, K.K.; Mazzei, C.; Selameab, T.; Miller, J.L. Working with Interpreters as a Team in Health Care (with Care) Curriculum Tool Kit for Oral Health Professions. MedEdPORTAL 2020, 16, 10894. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Health and Human Services; Food and Drug Administration; Center for Drug Evaluation and Research (CDER); Center for Biologics Evaluation and Research (CBER). Enhancing the Diversity of Clinical Trial Populations—Eligibility Criteria, Enrollment Practices, and Trial Designs Guidance for Industry; Food and Drug Administration: Silver Spring, MD, USA, 2020.
| Ethnic Minorities | PEH | Illegal Workers | Refugees | Sex Workers | Migrants | Immigrants | Religious Groups | Chronic Drug Users | PLW | GIP | Children | LGBT+ | Emigrants | Older Adults | Total (out of 15) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Austria | • | • | • | 3 | ||||||||||||
| Belgium | • | • | • | • | • | • | • | • | • | • | 10 | |||||
| Cyprus | • | • | • | • | • | • | • | • | • | 9 | ||||||
| Czech Republic | • | • | • | • | 4 | |||||||||||
| Germany | • | • | • | • | • | • | • | • | • | 9 | ||||||
| Greece | • | • | • | • | • | • | 6 | |||||||||
| Hungary | • | • | 2 | |||||||||||||
| Israel | • | • | • | • | • | • | • | • | 8 | |||||||
| Italy | • | • | • | • | • | • | • | 7 | ||||||||
| Lithuania | • | • | • | • | • | • | 6 | |||||||||
| The Netherlands | • | • | • | • | • | 5 | ||||||||||
| Norway | • | • | • | • | • | • | • | • | 8 | |||||||
| Portugal | • | • | • | • | 4 | |||||||||||
| Spain | • | • | 2 | |||||||||||||
| Sweden | • | • | • | • | • | • | • | • | • | 9 | ||||||
| Switzerland | • | • | • | • | 4 | |||||||||||
| Turkey | • | • | • | • | • | • | • | 7 | ||||||||
| Total (out of 17) | 13 | 12 | 11 | 11 | 9 | 8 | 8 | 6 | 6 | 4 | 5 | 3 | 4 | 2 | 1 |
| Ethnic Minorities | PEH | Illegal Workers | Refugees | Sex Workers | Migrants | Immigrants | Religious Groups | Chronic Drug Users | PLW | GIP | Children | LGBT+ | Emigrants | Older Adults | Total (out of 15) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Austria | • | • | • | 3 | ||||||||||||
| Belgium | • | • | • | • | • | 5 | ||||||||||
| Cyprus | • | • | • | 3 | ||||||||||||
| Czech Republic | • | • | • | 3 | ||||||||||||
| Germany | • | 1 | ||||||||||||||
| Greece | • | • | • | 3 | ||||||||||||
| Hungary | • | 1 | ||||||||||||||
| Israel | 0 | |||||||||||||||
| Italy | • | • | • | 3 | ||||||||||||
| Lithuania | • | 1 | ||||||||||||||
| The Netherlands | • | • | • | 3 | ||||||||||||
| Norway | • | • | • | 3 | ||||||||||||
| Portugal | 0 | |||||||||||||||
| Spain | 0 | |||||||||||||||
| Sweden | • | 1 | ||||||||||||||
| Switzerland | • | 1 | ||||||||||||||
| Turkey | • | • | • | 3 | ||||||||||||
| Total (out of 17) | 5 | 2 | 1 | 4 | 3 | 5 | 5 | 2 | 0 | 2 | 1 | 2 | 1 | 1 | 0 |
| Refugees | Illegal Workers | Ethnic Minorities | Immigrants | Migrants | Emigrants | PEH | Religious Groups | Chronic Drug Users | GIP | Sex Workers | PLW | LGBT+ | Children | Older Adults | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Language barrier | 11 | 7 | 9 | 11 | 10 | 8 | 2 | 2 | 0 | 0 | 1 | 0 | 1 | 0 | 0 |
| Low levels of health literacy | 6 | 4 | 9 | 5 | 6 | 6 | 5 | 4 | 3 | 2 | 2 | 3 | 1 | 1 | 1 |
| Reluctance to participate in trials due to engagement level | 7 | 6 | 7 | 5 | 6 | 4 | 4 | 1 | 2 | 2 | 3 | 2 | 1 | 1 | 1 |
| Low levels of trust in healthcare | 5 | 7 | 6 | 7 | 6 | 4 | 4 | 6 | 2 | 1 | 0 | 0 | 2 | 0 | 0 |
| Low levels of trust in vaccines/vaccinations | 5 | 4 | 6 | 5 | 5 | 3 | 3 | 6 | 2 | 1 | 1 | 5 | 1 | 2 | 2 |
| Access to health provider: other reasons (social or legal) | 9 | 9 | 4 | 7 | 5 | 3 | 5 | 1 | 3 | 1 | 1 | 0 | 0 | 0 | 1 |
| Access to health provider: distance/time for traveling | 3 | 5 | 5 | 4 | 5 | 3 | 1 | 0 | 2 | 6 | 0 | 2 | 0 | 1 | 2 |
| Uncertainty regarding the impact on their health condition | 5 | 2 | 6 | 4 | 3 | 3 | 1 | 4 | 2 | 2 | 0 | 2 | 0 | 2 | 0 |
| Religious belief restrictions | 5 | 3 | 7 | 5 | 4 | 2 | 1 | 6 | 0 | 0 | 0 | 0 | 0 | 1 | 0 |
| Access to health provider: geographic barriers, transportation | 3 | 4 | 2 | 2 | 3 | 2 | 4 | 0 | 3 | 6 | 0 | 0 | 0 | 0 | 2 |
| Lack of healthcare provider recommendations | 4 | 2 | 2 | 5 | 4 | 2 | 2 | 2 | 1 | 2 | 1 | 2 | 1 | 1 | 0 |
| Transient or nomadic movement | 5 | 3 | 2 | 2 | 2 | 3 | 7 | 0 | 1 | 1 | 2 | 0 | 0 | 0 | 0 |
| Anonymity/Privacy issues | 4 | 4 | 1 | 1 | 1 | 1 | 3 | 1 | 3 | 0 | 4 | 0 | 3 | 1 | 0 |
| Healthcare provider discrimination | 4 | 2 | 2 | 2 | 1 | 2 | 2 | 0 | 2 | 1 | 2 | 0 | 2 | 0 | 0 |
| Legal restrictions | 1 | 5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 |
| War and/or local conflicts | 4 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Compulsory vaccination schedule not provided for free | 1 | 2 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Refugees | Immigrants | PEH | Illegal Workers | Migrants | Ethnic Minorities | Emigrants | LGBT+ | Chronic Drug Users | PLW | Sex Workers | GIP | Religious Groups | Children | Older Adults | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Lack of information adapted to the specific target group | 12 | 10 | 9 | 7 | 11 | 9 | 8 | 7 | 5 | 6 | 7 | 6 | 7 | 3 | 2 |
| Lack of communication channels | 10 | 9 | 9 | 7 | 8 | 8 | 6 | 7 | 7 | 6 | 7 | 5 | 6 | 2 | 2 |
| Limited funds to actively recruit | 8 | 8 | 6 | 7 | 7 | 5 | 7 | 6 | 6 | 5 | 5 | 5 | 4 | 3 | 3 |
| Lack of national infrastructure | 6 | 7 | 6 | 4 | 6 | 4 | 5 | 3 | 2 | 4 | 3 | 3 | 2 | 2 | 2 |
| Not a priority in national research and development agenda | 2 | 2 | 2 | 3 | 2 | 1 | 2 | 2 | 2 | 1 | 2 | 2 | 3 | 0 | 0 |
| Lack of public health system access | 3 | 2 | 3 | 5 | 1 | 3 | 1 | 0 | 1 | 1 | 0 | 2 | 0 | 1 | 1 |
| Legal status | 5 | 2 | 2 | 3 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Poulimeneas, D.; Koniordou, M.; Kousi, D.; Merakou, C.; Kopsidas, I.; Tsopela, G.C.; Argyropoulos, C.D.; Themistocleous, S.C.; Shiamakkides, G.; Constantinou, M.; et al. The Challenges of Vaccine Trial Participation among Underserved and Hard-to-Reach Communities: An Internal Expert Consultation of the VACCELERATE Consortium. Vaccines 2023, 11, 1784. https://doi.org/10.3390/vaccines11121784
Poulimeneas D, Koniordou M, Kousi D, Merakou C, Kopsidas I, Tsopela GC, Argyropoulos CD, Themistocleous SC, Shiamakkides G, Constantinou M, et al. The Challenges of Vaccine Trial Participation among Underserved and Hard-to-Reach Communities: An Internal Expert Consultation of the VACCELERATE Consortium. Vaccines. 2023; 11(12):1784. https://doi.org/10.3390/vaccines11121784
Chicago/Turabian StylePoulimeneas, Dimitrios, Markela Koniordou, Dimitra Kousi, Christina Merakou, Ioannis Kopsidas, Grammatiki Christina Tsopela, Christos D. Argyropoulos, Sophia C. Themistocleous, George Shiamakkides, Marinos Constantinou, and et al. 2023. "The Challenges of Vaccine Trial Participation among Underserved and Hard-to-Reach Communities: An Internal Expert Consultation of the VACCELERATE Consortium" Vaccines 11, no. 12: 1784. https://doi.org/10.3390/vaccines11121784
APA StylePoulimeneas, D., Koniordou, M., Kousi, D., Merakou, C., Kopsidas, I., Tsopela, G. C., Argyropoulos, C. D., Themistocleous, S. C., Shiamakkides, G., Constantinou, M., Alexandrou, A., Noula, E., Nearchou, A., Salmanton-García, J., Stewart, F. A., Heringer, S., Albus, K., Álvarez-Barco, E., Macken, A., ... Zaoutis, T. E., on behalf of the VACCELERATE Consortium. (2023). The Challenges of Vaccine Trial Participation among Underserved and Hard-to-Reach Communities: An Internal Expert Consultation of the VACCELERATE Consortium. Vaccines, 11(12), 1784. https://doi.org/10.3390/vaccines11121784










