Association between Religious Beliefs and HPV Vaccination Attitudes among College Students
Abstract
:1. Introduction
2. Materials and Methods
2.1. Survey Population and Recruitment
2.2. Survey Description
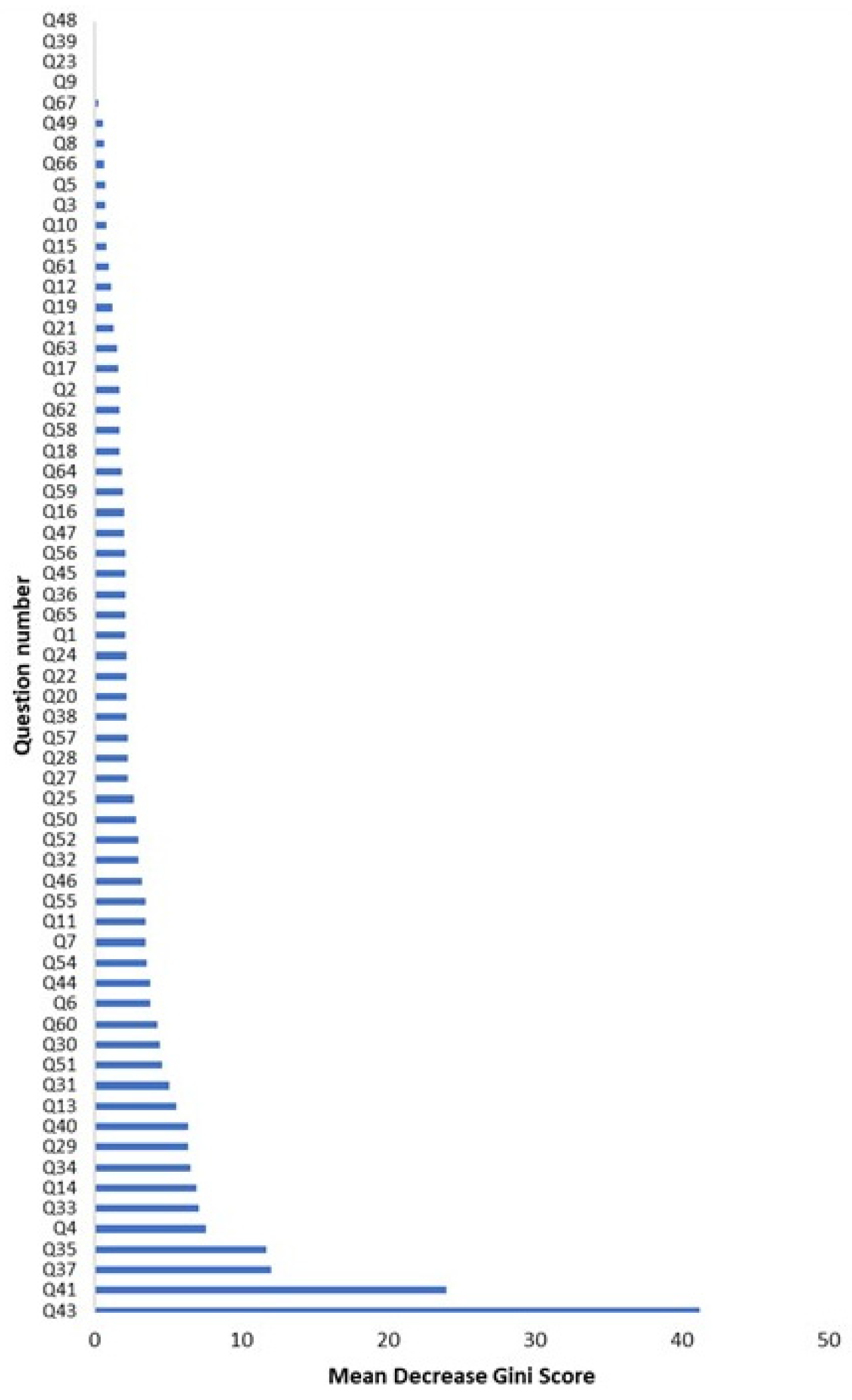
2.3. Statistical Analysis
3. Results
3.1. Descriptive Analysis of Study Population
3.2. Analysis of Indicators of HPV Catch-Up Vaccination Attitudes
3.3. Analysis of Indicators of Hesitancy toward Vaccinating Future Children against HPV
3.4. Bivariate Analysis of Religious Participation and Stance toward Vaccinating Future Children against HPV
3.5. Beliefs Concerning Sexual Activity and Administration of the HPV Vaccine to a Future Child
3.6. Analysis of Other Concerns and Stance toward Vaccinating Future Children against HPV
4. Discussion
5. Conclusions
Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- HPV Fact Sheet. Centers for Disease Control and Prevention. 2022. Available online: https://www.cdc.gov/std/hpv/stdfact-hpv.htm (accessed on 10 January 2023).
- Chesson, H.W.; Dunne, E.F.; Hariri, S.; Markowitz, L.E. The Estimated Lifetime Probability of Acquiring Human Papillomavirus in the United States. Sex. Transm. Dis. 2014, 41, 660–664. [Google Scholar] [CrossRef]
- Hirth, J. Disparities in HPV vaccination rates and HPV prevalence in the United States: A review of the literature. Hum. Vaccines Immunother. 2018, 15, 146–155. [Google Scholar] [CrossRef]
- Koutsky, P.L. Epidemiology of Genital Human Papillomavirus Infection. Am. J. Med. 1997, 102 (Suppl. S1), 3–8. [Google Scholar] [CrossRef]
- Alrajjal, A.; Pansare, V.; Choudhury, M.S.R.; Khan, M.Y.A.; Shidham, V.B. Squamous intraepithelial lesions (SIL: LSIL, HSIL, ASCUS, ASC-H, LSIL-H) of Uterine Cervix and Bethesda System. Cytojournal 2021, 18, 16. [Google Scholar] [CrossRef]
- HPV Vaccination: Understanding HPV Coverage | CDC. 2021. Available online: https://www.cdc.gov/hpv/partners/outreach-hcp/hpv-coverage.html (accessed on 27 October 2021).
- Saraiya, M.; Unger, E.R.; Thompson, T.D.; Lynch, C.F.; Hernandez, B.Y.; Lyu, C.W.; Steinau, M.; Watson, M.; Wilkinson, E.J.; Hopenhayn, C.; et al. US Assessment of HPV Types in Cancers: Implications for Current and 9-Valent HPV Vaccines. JNCI J. Natl. Cancer Inst. 2015, 107, djv086. [Google Scholar] [CrossRef]
- EtR for HPV Vaccination of Adults 27–45 Years Old | CDC. 2019. Available online: https://www.cdc.gov/vaccines/acip/recs/grade/HPV-adults-etr.html (accessed on 6 October 2022).
- Oh, K.M.; Alqahtani, N.; Chang, S.; Cox, C. Knowledge, beliefs, and practice regarding human papillomavirus (HPV) vaccination among American college students: Application of the health belief model. J. Am. Coll. Health J. ACH 2021, 29, 1–10. [Google Scholar] [CrossRef]
- Natipagon-Shah, B.; Lee, E.; Lee, S.Y. Knowledge, Beliefs, and Practices Among U. S. College Students Concerning Papillomavirus Vaccination. J. Community Health 2021, 46, 380–388. [Google Scholar] [CrossRef]
- Shah, S.F.A.; Ginossar, T.; Bentley, J.M.; Zimet, G.; McGrail, J.P. Using the Theory of Planned behavior to identify correlates of HPV vaccination uptake among college students attending a rural university in Alabama. Vaccine 2021, 39, 7421–7428. [Google Scholar] [CrossRef]
- Chatterjee, A. The next generation of HPV vaccines: Nonavalent vaccine V503 on the horizon. Expert. Rev. Vaccines 2014, 13, 1279–1290. [Google Scholar] [CrossRef]
- Giuliano, A.R.; Palefsky, J.M.; Goldstone, S.; Moreira, E.D.; Penny, M.E.; Aranda, C.; Vardas, E.; Moi, H.; Jessen, H.; Hillman, R.; et al. Efficacy of quadrivalent HPV vaccine against HPV Infection and disease in males. N. Engl. J. Med. 2011, 364, 401–411. [Google Scholar] [CrossRef]
- CDC. Immunization Schedules for 18 & Younger. Centers for Disease Control and Prevention. 2022. Available online: https://www.cdc.gov/vaccines/schedules/hcp/imz/child-adolescent.html (accessed on 11 April 2022).
- Pingali, C.; Yankey, D.; Elam-Evans, L. National Vaccination Coverage Among Adolescents Aged 13–17 Years—National Immunization Survey-Teen, United States, 2021. MMWR Morb Mortal Wkly Rep. 2021, 71, 1101–1108. [Google Scholar] [CrossRef] [PubMed]
- Preston, S.M.; Darrow, W.W. Are Men Being Left Behind (Or Catching Up)? Differences in HPV Awareness, Knowledge, and Attitudes Between Diverse College Men and Women. Am. J. Mens. Health 2019, 13, 1557988319883776. [Google Scholar] [CrossRef]
- Rohde, R.L.; Adjei Boakye, E.; Christopher, K.M.; Geneus, C.J.; Walker, R.J.; Varvares, M.A.; Osazuwa-Peters, N. Assessing university students’ sexual risk behaviors as predictors of human papillomavirus (HPV) vaccine uptake behavior. Vaccine 2018, 36, 3629–3634. [Google Scholar] [CrossRef] [PubMed]
- McLendon, L.; Puckett, J.; Green, C.; James, J.; Head, K.J.; Lee, H.Y.; Pierce, J.Y.; Beasley, M.; Daniel, C.L. Factors associated with HPV vaccination initiation among United States college students. Hum. Vaccines Immunother. 2021, 17, 1033–1043. [Google Scholar] [CrossRef] [PubMed]
- Suk, R.; Montealegre, J.R.; Nemutlu, G.S.; Nyitray, A.G.; Schmeler, K.M.; Sonawane, K.; Deshmukh, A.A. Public Knowledge of Human Papillomavirus and Receipt of Vaccination Recommendations. JAMA Pediatr. 2019, 173, 1099–1102. [Google Scholar] [CrossRef] [PubMed]
- Staras, S.A.S.; Vadaparampil, S.T.; Patel, R.P.; Shenkman, E.A. Parent Perceptions Important for HPV Vaccine Initiation among Low Income Adolescent Girls. Vaccine 2014, 32, 6163–6169. [Google Scholar] [CrossRef]
- Gilkey, M.B.; Parks, M.J.; Margolis, M.A.; McRee, A.L.; Terk, J.V. Implementing Evidence-Based Strategies to Improve HPV Vaccine Delivery. Pediatrics 2019, 144, e20182500. [Google Scholar] [CrossRef]
- Dorell, C.; Yankey, D.; Kennedy, A.; Stokley, S. Factors that influence parental vaccination decisions for adolescents, 13 to 17 years old: National Immunization Survey-Teen, 2010. Clin. Pediatr. 2013, 52, 162–170. [Google Scholar] [CrossRef]
- Nguyen, K.H.; Santibanez, T.A.; Stokley, S.; Lindley, M.C.; Fisher, A.; Kim, D.; Greby, S.; Srivastav, A.; Singleton, J. Parental vaccine hesitancy and its association with adolescent HPV vaccination. Vaccine 2021, 39, 2416–2423. [Google Scholar] [CrossRef]
- Bernat, D.H.; Gerend, M.A.; Chevallier, K.; Zimmerman, M.A.; Bauermeister, J.A. Characteristics Associated With Initiation of the HPV Vaccine Among a National Sample of Male and Female Young Adults. J. Adolesc. Health Off. Publ. Soc. Adolesc. Med. 2013, 53, 630–636. [Google Scholar] [CrossRef]
- Best, A.L.; Thompson, E.L.; Adamu, A.M.; Logan, R.; Delva, J.; Thomas, M.; Cunningham, E.; Vamos, C.; Daley, E. Examining the Influence of Religious and Spiritual Beliefs on HPV Vaccine Uptake Among College Women. J. Relig. Health 2019, 58, 2196–2207. [Google Scholar] [CrossRef] [PubMed]
- Bodson, J.; Wilson, A.; Warner, E.L.; Kepka, D. Religion and HPV vaccine-related awareness, knowledge, and receipt among insured women aged 18-26 in Utah. PLoS ONE 2017, 12, e0183725. [Google Scholar] [CrossRef]
- Thomas, T.; Blumling, A.; Delaney, A. The Influence of Religiosity and Spirituality on Rural Parents’ Health Decision Making and Human Papillomavirus Vaccine Choices. ANS Adv. Nurs. Sci. 2015, 38, E1–E12. [Google Scholar] [CrossRef] [PubMed]
- Constantine, N.A.; Jerman, P. Acceptance of human papillomavirus vaccination among Californian parents of daughters: A representative statewide analysis. J. Adolesc. Health Off. Publ. Soc. Adolesc. Med. 2007, 40, 108–115. [Google Scholar] [CrossRef]
- Redd, D.S.; Jensen, J.L.; Bodily, R.J.; Lee, A.A.; Skyles, T.J.; Poole, B.D. Cautious Sexual Attitudes Diminish Intent to Vaccinate Children against HPV in Utah. Vaccines 2022, 10, 1382. [Google Scholar] [CrossRef] [PubMed]
- Shelton, R.C.; Snavely, A.C.; De Jesus, M.; Othus, M.D.; Allen, J.D. HPV Vaccine Decision-Making and Acceptance: Does Religion Play a Role? J. Relig. Health 2013, 52, 1120–1130. [Google Scholar] [CrossRef]
- Koskan, A.; Stecher, C.; Helitzer, D. College males’ behaviors, intentions, and influencing factors related to vaccinating against HPV. Hum Vaccines Immunother. 2020, 17, 1044–1051. [Google Scholar] [CrossRef]
- Krawczyk, A.L.; Perez, S.; Lau, E.; Holcroft, C.A.; Amsel, R.; Knäuper, B.; Rosberger, Z. Human papillomavirus vaccination intentions and uptake in college women. Health Psychol. Off. J. Div. Health Psychol. Am. Psychol. Assoc. 2012, 31, 685–693. [Google Scholar] [CrossRef]
- Chen, M.M.; Mott, N.; Clark, S.J.; Harper, D.M.; Shuman, A.G.; Prince, M.E.P.; Dossett, L.A. HPV Vaccination Among Young Adults in the US. JAMA 2021, 325, 1673–1674. [Google Scholar] [CrossRef]
- Moore, G.R.; Crosby, R.A.; Young, A.; Charnigo, R. Low rates of free human papillomavirus vaccine uptake among young women. Sex Health 2010, 7, 287–290. [Google Scholar] [CrossRef]
- Patel, D.A.; Zochowski, M.; Peterman, S.; Dempsey, A.F.; Ernst, S.; Dalton, V.K. Human Papillomavirus Vaccine Intent and Uptake among Female College Students. J. Am. Coll. Health J. ACH 2012, 60, 151–161. [Google Scholar] [CrossRef] [PubMed]
- Foster, S.; Carvallo, M.; Song, H.; Lee, J.; Lee, J. When culture and health collide: Feminine honor endorsement and attitudes toward catch-up HPV vaccinations in college women. J. Am. Coll. Health J. ACH 2021, 71, 1454–1462. [Google Scholar] [CrossRef] [PubMed]
- Glenn, B.A.; Nonzee, N.J.; Tieu, L.; Pedone, B.; Cowgill, B.O.; Bastani, R. Human papillomavirus (HPV) vaccination in the transition between adolescence and adulthood. Vaccine 2021, 39, 3435–3444. [Google Scholar] [CrossRef] [PubMed]
- Koskan, A.M.; Stecher, C.; Helitzer, D.L. Influences on male college students’ patient-provider communications and uptake behaviors related to the human papillomavirus vaccine. J. Am. Coll. Health J ACH 2022, 1–7. [Google Scholar] [CrossRef]
- Ragan, K.R.; Bednarczyk, R.A.; Butler, S.M.; Omer, S.B. Missed opportunities for catch-up human papillomavirus vaccination among university undergraduates: Identifying health decision-making behaviors and uptake barriers. Vaccine 2018, 36, 331–341. [Google Scholar] [CrossRef]
- Katz, M.L.; Krieger, J.L.; Roberto, A. Human papillomavirus (HPV): College male’s knowledge, perceived risk, sources of information, vaccine barriers and communication. J. Mens. Health Gend. 2011, 8, 175–184. [Google Scholar] [CrossRef]
- Goldfarb, J.A.; Comber, J.D. Human papillomavirus (HPV) infection and vaccination: A cross-sectional study of college students’ knowledge, awareness, and attitudes in Villanova, PA. Vaccine X 2022, 10, 100141. [Google Scholar] [CrossRef]
- Stout, M.E.; Christy, S.M.; Winger, J.G.; Vadaparampil, S.T.; Mosher, C.E. Self-efficacy and HPV Vaccine Attitudes Mediate the Relationship Between Social Norms and Intentions to Receive the HPV Vaccine Among College Students. J. Community Health 2020, 45, 1187–1195. [Google Scholar] [CrossRef]
| Characteristic | ||
|---|---|---|
| n | % | |
| Age (years) | ||
| Mean Age + SD | 19.2 + 1.3 | - |
| Age Range | 18–30 | - |
| Gender | ||
| Female | 1052 | 67.7 |
| Male | 497 | 32.0 |
| Preferred not to answer | 6 | 0.4 |
| Race/Ethnicity | ||
| White | 948 | 60.9 |
| Asian | 285 | 18.3 |
| Hispanic/Latino | 192 | 12.3 |
| Black or African American | 79 | 5.0 |
| Other/Unknown | 34 | 2.2 |
| American Indian or Alaskan Native | 8 | 0.5 |
| Native Hawaiian or Pacific Islander | 4 | 0.3 |
| USA Region of Origin | ||
| Southwest—AZ, NM, OK, TX | 800 | 51.4 |
| West—AK, CA, CO, HI, ID, MT, NV, OR, UT, WA, WY | 291 | 18.7 |
| Midwest—IA, IL, IN, KS, MI, MIN, MO, ND, NE, OH, SD, WI | 158 | 10.2 |
| Southeast—AL, AR, FL, GA, KY, LA, MS, NC, SC, TN, VA, WV | 124 | 8.0 |
| Northeast—CT, DC, DE, MA, MD, ME, NH, NJ, NY, PA, RI, VT | 79 | 5.1 |
| Other | 105 | 6.7 |
| Academic Area of Study | ||
| Non-STEM | 417 | 26.8 |
| STEM | 1140 | 73.2 |
| Average Family Income | ||
| <10,000 USD | 31 | 2.0 |
| 10,000–39,999 USD | 72 | 4.7 |
| 40,000–69,999 USD | 171 | 11.1 |
| 70,000–99,999 USD | 231 | 15.0 |
| >100,000 USD | 1035 | 67.2 |
| Religion | ||
| Christian | 1236 | 79.6 |
| Other World Religions | 172 | 11.1 |
| Atheist/Agnostic | 144 | 9.3 |
| Christian Denomination Affiliation | ||
| Mainline Protestant | 177 | 14.4 |
| Evangelical Protestant | 37 | 3.0 |
| Baptist | 314 | 25.5 |
| Catholic | 262 | 21.2 |
| Non-denominational | 404 | 32.8 |
| Other | 39 | 3.2 |
| Relationship Status | ||
| In a relationship with another individual | 466 | 29.9 |
| Married | 10 | 0.6 |
| Single | 1081 | 69.4 |
| HPV Vaccination Status | ||
| Vaccinated | 828 | 53.2 |
| Not Vaccinated | 328 | 21.1 |
| Unknown | 400 | 25.7 |
| Church Attendance/Religious Activity Participation (times per month) | ||
| 0 | 348 | 24.8 |
| <1 | 124 | 8.8 |
| 2–4 | 462 | 32.9 |
| 5–8 | 306 | 21.8 |
| >8 | 163 | 11.6 |
| Religion or religiously related values |
| I strictly adhere to my religion’s teachings concerning sexual behavior Premarital sex is unacceptable |
| Views regarding HPV administration and indications |
| If an individual abstains from sexual activity prior to marriage, they do not need to receive the HPV vaccine |
| The HPV vaccine is not necessary if an individual has only one sexual partner in life |
| Vaccinating 11–15-year-old children against HPV is unnecessary because children are not likely to be sexually active |
| Views regarding the efficacy or safety of the HPV vaccine |
| The HPV vaccine is not required for enrollment in all public middle schools, so it must not be beneficial or needed The HPV vaccine is relatively new and has not been highly tested; therefore, it cannot be trusted |
| Other social, ethical, or cultural factors |
| If getting the HPV vaccine would protect my significant other from HPV and HPV-related cancers, I would consider receiving the vaccine |
| Which category best describes your parents’ (or guardian’s) yearly household income before taxes I am likely to vaccinate my children against HPV I have initiated or completed the HPV vaccine series |
| Characteristic | Catch-Up Vaccination Hesitant | Catch-Up Vaccination Accepting | Total N | p Value | |||
|---|---|---|---|---|---|---|---|
| n = 189 | n = 529 | n = 718 | |||||
| n | % | n | % | n | % | X2 | |
| Students’ openness to considering catch-up vaccination | 189 | 26.3 | 529 | 73.7 | 718 | 100 | - |
| Which category best describes your parents’ (or guardians’) yearly household income before taxes? | |||||||
| <100,000 USD | 80 | 29.4 | 192 | 70.6 | 272 | 38.3 | 0.09 |
| ≥100,000 USD | 104 | 23.7 | 335 | 76.3 | 439 | 61.7 | |
| Religion | <0.0001 | ||||||
| Christian | 170 | 29.5 | 406 | 70.5 | 576 | 80.6 | |
| Other World Religion, Agnostic/Atheist | 18 | 13.0 | 121 | 87.1 | 112 | 19.4 | |
| Christian Denomination Affiliation | <0.0001 | ||||||
| Mainline Protestant | 10 | 50.0 | 10 | 50.0 | 20 | 3.5 | |
| Evangelical Protestant | 15 | 21.7 | 54 | 78.0 | 69 | 12.0 | |
| Baptist | 62 | 38.3 | 100 | 61.7 | 162 | 28.1 | |
| Catholic | 21 | 18.8 | 91 | 81.2 | 112 | 19.4 | |
| Non-denominational | 56 | 29.2 | 136 | 70.8 | 192 | 33.3 | |
| Other | 6 | 28.6 | 15 | 71.4 | 21 | 3.7 | |
| Among religious students: The HPV vaccine contains ingredients that conflict with my religious beliefs. | |||||||
| Strongly/Somewhat Agree | 43 | 65.1 | 23 | 34.9 | 66 | 10.1 | <0.0001 |
| Neither Agree nor Strongly/Somewhat Disagree | 137 | 23.3 | 451 | 76.7 | 588 | 89.9 | |
| Premarital sex is unacceptable. | |||||||
| Strongly/Somewhat Agree | 143 | 41.8 | 199 | 58.2 | 342 | 47.7 | <0.0001 |
| Neither Agree nor Strongly/Somewhat Disagree | 46 | 12.3 | 329 | 87.7 | 375 | 52.3 | |
| Among students whose religion has teachings regarding sexual behavior: I strictly adhere to my religion’s teachings concerning sexual behavior. | |||||||
| Strongly/Somewhat Agree | 160 | 34.6 | 303 | 65.4 | 463 | 74.4 | <0.0001 |
| Neither Agree nor Strongly/Somewhat Disagree | 13 | 8.2 | 146 | 91.8 | 159 | 25.6 | |
| People with diseases caused by HPV are responsible for their own suffering because the virus is only transmitted through promiscuous sexual practices. | |||||||
| Strongly/Somewhat Agree | 49 | 47.1 | 55 | 52.9 | 104 | 14.5 | <0.0001 |
| Neither Agree nor Strongly/Somewhat Disagree | 140 | 22.8 | 473 | 77.2 | 613 | 85.5 | |
| The HPV vaccine is not necessary if an individual has only one sexual partner in their lifetime. | |||||||
| Strongly/Somewhat Agree | 83 | 62.9 | 49 | 37.1 | 132 | 18.4 | <0.0001 |
| Neither Agree nor Strongly/Somewhat Disagree | 106 | 18.1 | 479 | 81.9 | 585 | 81.6 | |
| If an individual abstains from sexual activity before marriage, they do not need to receive the HPV vaccine. | |||||||
| Strongly/Somewhat Agree | 85 | 62.0 | 52 | 38.0 | 137 | 19.1 | <0.0001 |
| Neither Agree nor Strongly/Somewhat Disagree | 104 | 18.0 | 475 | 82.0 | 579 | 80.9 | |
| HPV vaccine has serious side effects. | |||||||
| Strongly/Somewhat Agree | 61 | 47.7 | 67 | 52.3 | 128 | 17.9 | <0.0001 |
| Neither Agree nor Strongly/Somewhat Disagree | 127 | 21.6 | 462 | 78.4 | 589 | 82.2 | |
| The HPV vaccine is relatively new and not highly tested, therefore it cannot be trusted. | |||||||
| Strongly/Somewhat Agree | 48 | 64.9 | 26 | 35.1 | 74 | 10.3 | <0.0001 |
| Neither Agree nor Strongly/Somewhat Disagree | 140 | 21.8 | 503 | 78.2 | 643 | 89.7 | |
| Vaccines often have serious side effects. | |||||||
| Strongly/Somewhat Agree | 70 | 37.2 | 118 | 62.8 | 188 | 26.2 | <0.0001 |
| Neither Agree nor Strongly/Somewhat Disagree | 119 | 22.5 | 411 | 77.6 | 530 | 73.8 | |
| Vaccines are effective at preventing disease. | |||||||
| Strongly/Somewhat Agree | 155 | 23.3 | 511 | 76.7 | 666 | 92.8 | <0.0001 |
| Neither Agree nor Strongly/Somewhat Disagree | 34 | 64.4 | 18 | 34.6 | 52 | 7.2 | |
| Vaccines contain dangerous toxins. | |||||||
| Strongly/Somewhat Agree | 43 | 55.8 | 34 | 44.2 | 77 | 10.7 | <0.0001 |
| Neither Agree nor Strongly/Somewhat Disagree | 146 | 22.8 | 495 | 77.2 | 641 | 89.3 | |
| Vaccines are more helpful than harmful. | |||||||
| Strongly/Somewhat Agree | 134 | 21.4 | 493 | 78.6 | 627 | 86.8 | <0.0001 |
| Neither Agree nor Strongly/Somewhat Disagree | 59 | 62.1 | 36 | 37.9 | 95 | 13.2 | |
| The HPV vaccine is not required for enrollment in all public middle schools, so it must not be beneficial or needed. | 22 | 66.7 | 11 | 33.3 | 33 | 4.6 | <0.0001 |
| Strongly/Somewhat Agree | |||||||
| Neither Agree nor Strongly/Somewhat Disagree | 167 | 24.5 | 516 | 75.6 | 683 | 95.4 | |
| If getting the HPV vaccine would protect my significant other from HPV and HPV-related cancers, I would consider receiving the vaccine. | |||||||
| Strongly/Somewhat Agree | 111 | 20.7 | 425 | 79.3 | 536 | 74.7 | <0.0001 |
| Neither Agree nor Strongly/Somewhat Disagree | 78 | 42.9 | 104 | 57.1 | 182 | 25.4 | |
| Method of Transmission | Indicated Awareness | No Indicated Awareness | ||
|---|---|---|---|---|
| n = 1559 | ||||
| n | % | n | % | |
| Vaginal–penile sex | 1498 | 96.1 | 61 | 3.9 |
| Penile–anal sex | 1357 | 87.0 | 202 | 13.0 |
| Penile–oral sex | 1295 | 83.1 | 264 | 16.9 |
| Vaginal–oral sex | 1294 | 83.0 | 265 | 17.0 |
| Sex even when condoms and/or dental dams are used | 836 | 53.6 | 723 | 46.4 |
| Sharing of hairbrushes | 92 | 5.9 | 1467 | 94.1 |
| Characteristic | Vaccination Hesitant | Vaccination Accepting | Total N | p Value | |||
|---|---|---|---|---|---|---|---|
| n = 330 | n = 1073 | n = 1403 | |||||
| n | % | n | % | n | % | X2 | |
| Religious Preference | |||||||
| Christian | 305 | 24.8 | 927 | 75.2 | 1232 | 87.8 | <0.0001 |
| Other World Religions | 25 | 14.7 | 146 | 85.3 | 171 | 12.1 | |
| Christian Denomination Affiliation | |||||||
| Mainline Protestant | 29 | 16.4 | 148 | 83.6 | 176 | 14.4 | <0.0001 |
| Evangelical Protestant | 12 | 32.4 | 25 | 67.6 | 37 | 3.0 | |
| Baptist | 101 | 32.3 | 212 | 67.7 | 313 | 25.5 | |
| Catholic | 50 | 19.2 | 211 | 80.8 | 261 | 21.2 | |
| Non-denominational | 100 | 24.8 | 303 | 75.2 | 403 | 32.8 | |
| Other | 13 | 34.2 | 25 | 65.8 | 38 | 3.1 | |
| Church Attendance/Religious Activity Participation (times per month) | |||||||
| 0 | 55 | 15.8 | 293 | 84.2 | 348 | 24.8 | <0.0001 |
| <1 | 23 | 18.6 | 101 | 81.5 | 124 | 8.8 | |
| 2–4 | 95 | 20.6 | 367 | 79.4 | 462 | 32.9 | |
| 5–8 | 96 | 31.4 | 210 | 68.6 | 306 | 21.8 | |
| >8 | 61 | 37.4 | 102 | 62.6 | 163 | 11.6 | |
| The HPV vaccine contains ingredients that conflict with my religious beliefs. | |||||||
| Strongly/Somewhat Agree | 56 | 68.3 | 36 | 31.7 | 92 | 5.9 | <0.0001 |
| Strongly/Somewhat Disagree | 270 | 20.6 | 1043 | 79.4 | 1313 | 94.1 | |
| Premarital sex is unacceptable. | |||||||
| Strongly/Somewhat Agree | 220 | 34.9 | 410 | 65.1 | 630 | 45.1 | <0.0001 |
| Neither Agree nor Strongly/Somewhat Disagree | 110 | 14.3 | 658 | 85.7 | 768 | 54.9 | |
| People with diseases caused by HPV are responsible for their own suffering because the virus is only transmitted through promiscuous sexual practices. | |||||||
| Strongly/Somewhat Agree | 59 | 30.9 | 123 | 69.1 | 191 | 13.6 | 0.013 |
| Neither Agree nor Strongly/Somewhat Disagree | 271 | 22.4 | 938 | 77.6 | 1209 | 86.4 | |
| Among students whose religion has teachings regarding sexual behavior: I strictly adhere to my religion’s teachings concerning sexual behavior. | |||||||
| Strongly/Somewhat Agree | 262 | 28.6 | 653 | 71.4 | 915 | 71.2 | <0.0001 |
| Neither Agree nor Strongly/Somewhat Disagree | 48 | 12.9 | 323 | 87.1 | 371 | 28.9 | |
| Characteristic | Vaccination Hesitant | Vaccination Accepting | Total N | p Value | |||
|---|---|---|---|---|---|---|---|
| n = 346 | n = 1207 | n = 1553 | |||||
| n | % | n | % | n | % | X2 | |
| Vaccinating children against HPV sends them mixed messages about the acceptability of sexual activity. | |||||||
| Strongly/Somewhat Agree | 111 | 60.3 | 73 | 39.4 | 184 | 11.9 | <0.0001 |
| Neither Agree nor Strongly/Somewhat Disagree | 234 | 17.1 | 1132 | 82.9 | 1366 | 88.1 | |
| Vaccinating children against HPV will make them more likely to have premarital sex. | |||||||
| Strongly/Somewhat Agree | 73 | 57 | 55 | 43 | 128 | 8.3 | <0.0001 |
| Neither Agree nor Strongly/Somewhat Disagree | 273 | 19.2 | 1150 | 80.8 | 1423 | 91.8 | |
| If an individual abstains from sexual activity prior to marriage, they do not need to receive the HPV vaccine. | |||||||
| Strongly/Somewhat Agree | 106 | 60.2 | 70 | 39.8 | 167 | 10.9 | <0.0001 |
| Neither Agree nor Strongly/Somewhat Disagree | 239 | 17.4 | 1132 | 82.6 | 1371 | 89.1 | |
| The HPV vaccine is not necessary if an individual has only one sexual partner in life. | |||||||
| Strongly/Somewhat Agree | 104 | 59.4 | 71 | 40.6 | 175 | 11.3 | <0.0001 |
| Neither Agree nor Strongly/Somewhat Disagree | 242 | 17.6 | 1131 | 82.4 | 1373 | 88.7 | |
| The possibility of contracting HPV helps prevent premarital sex. | |||||||
| Strongly/Somewhat Agree | 124 | 27 | 340 | 73 | 466 | 30.1 | 0.0034 |
| Neither Agree nor Strongly/Somewhat Disagree | 219 | 20.2 | 865 | 79.8 | 1084 | 69.9 | |
| Among students whose religion has teachings on sexual behavior: Because HPV is sexually transmitted, my family’s values will protect my children from contracting HPV. | |||||||
| Strongly/Somewhat Agree | 201 | 26.1 | 568 | 73.8 | 769 | 60.6 | 0.0295 |
| Neither Agree nor Strongly/Somewhat Disagree | 106 | 20.8 | 403 | 79.1 | 509 | 39.4 | |
| Vaccinating 11–15-year-old children against HPV is unnecessary because children are not likely to be sexually active. | |||||||
| Strongly/Somewhat Agree | 88 | 64.2 | 49 | 35.8 | 137 | 8.8 | 0.0014 |
| Neither Agree nor Strongly/Somewhat Disagree | 258 | 18.3 | 1155 | 81.7 | 1413 | 91.2 | |
| Because only females are at risk of developing cancer following HPV infection, males do not need to consider being vaccinated against HPV. | |||||||
| Strongly/Somewhat Agree | 6 | 42.9 | 8 | 57.1 | 14 | 0.9 | 0.0861 |
| Neither Agree nor Strongly/Somewhat Disagree | 340 | 22.1 | 1196 | 77.9 | 1536 | 99.1 | |
| Women, but not men, can experience health problems after HPV infection. | |||||||
| Strongly/Somewhat Agree | 88 | 22.3 | 307 | 77.7 | 395 | 25.5 | 0.9973 |
| Neither Agree nor Strongly/Somewhat Disagree | 257 | 22.3 | 897 | 77.7 | 1154 | 74.5 | |
| Characteristic | Vaccination Hesitant | Vaccination Accepting | Total N | p Value | |||
|---|---|---|---|---|---|---|---|
| n = 346 | n = 1207 | n = 1553 | |||||
| n | % | n | % | n | % | X2 | |
| Vaccines are effective at preventing disease. | |||||||
| Strongly/Somewhat Agree | 294 | 19.9 | 1186 | 80.1 | 1480 | 95.3 | <0.0001 |
| Neither Agree nor Strongly/Somewhat Disagree | 52 | 71.2 | 21 | 28.8 | 73 | 4.7 | |
| Vaccines are more helpful than harmful. | |||||||
| Strongly/Somewhat Agree | 259 | 18.5 | 1143 | 81.5 | 1402 | 90.3 | <0.0001 |
| Neither Agree nor Strongly/Somewhat Disagree | 87 | 58 | 63 | 42 | 150 | 9.7 | |
| The HPV vaccine is relatively new and has not been highly tested; therefore, it cannot be trusted. | |||||||
| Strongly/Somewhat Agree | 60 | 71.4 | 24 | 28.6 | 84 | 5.4 | <0.0001 |
| Neither Agree nor Strongly/Somewhat Disagree | 285 | 19.5 | 1179 | 80.5 | 1464 | 94.6 | |
| HPV vaccine has serious side effects. | |||||||
| Strongly/Somewhat Agree | 92 | 49.5 | 94 | 50.5 | 186 | 12.0 | <0.0001 |
| Neither Agree nor Strongly/Somewhat Disagree | 253 | 18.5 | 1112 | 81.5 | 1365 | 88.0 | |
| Vaccines often have serious side effects. | |||||||
| Strongly/Somewhat Agree | 115 | 42.4 | 156 | 57.6 | 271 | 17.5 | <0.0001 |
| Neither Agree nor Strongly/Somewhat Disagree | 231 | 18.0 | 1050 | 82.0 | 1281 | 82.5 | |
| Vaccines contain dangerous toxins. | |||||||
| Strongly/Somewhat Agree | 59 | 58.4 | 42 | 41.6 | 101 | 6.5 | <0.0001 |
| Neither Agree nor Strongly/Somewhat Disagree | 287 | 19.8 | 1162 | 80.2 | 1449 | 93.5 | |
| I am likely to fully vaccinate my children with the basic recommended childhood vaccines (do not consider HPV vaccine in your response). | |||||||
| Strongly/Somewhat Agree | 307 | 20.4 | 1296 | 79.6 | 1503 | 96.8 | <0.0001 |
| Neither Agree nor Strongly/Somewhat Disagree | 39 | 79.6 | 10 | 20.4 | 49 | 3.2 | |
| Characteristic | Vaccination Hesitant | Vaccination Accepting | Total N | p Value | |||
|---|---|---|---|---|---|---|---|
| n = 346 | n = 1207 | n = 1553 | |||||
| n | % | n | % | n | % | X2 | |
| In what region of the United States did you spend most of your childhood? | |||||||
| Southwest—AZ, NM, OK, TX | 170 | 21.3 | 628 | 78.7 | 798 | 51.4 | <0.0001 |
| West—AK, CA, CO, HI, ID, MT, NV, OR, UT, WA, WY | 67 | 23.1 | 223 | 76.9 | 290 | 18.7 | |
| Midwest—IA, IL, IN, KS, MI, MIN, MO, ND, NE, OH, SD, WI | 35 | 22.3 | 122 | 77.7 | 157 | 10.1 | |
| Southeast—AL, AR, FL, GA, KY, LA, MS, NC, SC, TN, VA, WV | 21 | 16.9 | 103 | 83.1 | 124 | 8.0 | |
| Northeast—CT, DC, DE, MA, MD, ME, NH, NJ, NY, PA, RI, VT | 22 | 27.9 | 57 | 72.2 | 79 | 5.1 | |
| Other | 31 | 29.5 | 74 | 70.5 | 105 | 6.8 | |
| Academic Area of Study | |||||||
| Non-STEM | 82 | 28.2 | 209 | 71.8 | 291 | 18.7 | 0.0086 |
| STEM | 264 | 20.9 | 998 | 79.1 | 1262 | 81.3 | |
| Which category best describes your parents’ (or guardians’) yearly household income before taxes? | |||||||
| <100,000 USD | 134 | 26.6 | 369 | 73.4 | 503 | 32.7 | 0.0037 |
| ≥100,000 USD | 207 | 20.0 | 827 | 80.0 | 1034 | 67.3 | |
| I have initiated or completed the HPV vaccine series. | |||||||
| Yes, Previously Vaccinated | 31 | 3.7 | 797 | 96.3 | 828 | 53.3 | <0.0001 |
| No, Not Vaccinated/Unaware of Vaccination Status | 315 | 43.5 | 410 | 56.6 | 725 | 46.7 | |
| Among students who are unvaccinated or unaware of their vaccination status: Would you agree to consider receiving the HPV vaccine? | |||||||
| Strongly/Somewhat Agree | 133 | 25.1 | 396 | 74.9 | 529 | 73.7 | <0.0001 |
| Neither Agree nor Strongly/Somewhat Disagree | 180 | 96.2 | 9 | 4.8 | 189 | 26.3 | |
| Receiving the HPV vaccine will affect how people in my social circle will view me. | |||||||
| Strongly/Somewhat Agree | 37 | 52.9 | 33 | 47.2 | 70 | 4.5 | <0.0001 |
| Neither Agree nor Strongly/Somewhat Disagree | 309 | 20.9 | 1173 | 79.2 | 1482 | 95.5 | |
| The HPV vaccine is not required for enrollment in all public middle schools, so it must not be beneficial or needed. | |||||||
| Strongly/Somewhat Agree | 26 | 54.2 | 22 | 45.8 | 48 | 3.1 | <0.0001 |
| Neither Agree nor Strongly/Somewhat Disagree | 320 | 21.3 | 1180 | 78.7 | 1500 | 96.9 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hittson, H.; McAleer, L.; Saucedo, L.; Mahler, L.; Andino, G.; Zorba, A.; Walden, S.; Pickett, B.E.; Poole, B.D.; Abel, E.L. Association between Religious Beliefs and HPV Vaccination Attitudes among College Students. Vaccines 2023, 11, 1623. https://doi.org/10.3390/vaccines11101623
Hittson H, McAleer L, Saucedo L, Mahler L, Andino G, Zorba A, Walden S, Pickett BE, Poole BD, Abel EL. Association between Religious Beliefs and HPV Vaccination Attitudes among College Students. Vaccines. 2023; 11(10):1623. https://doi.org/10.3390/vaccines11101623
Chicago/Turabian StyleHittson, Hannah, Leah McAleer, Lydia Saucedo, Lindsay Mahler, Gabriel Andino, Andie Zorba, Sarah Walden, Brett E. Pickett, Brian D. Poole, and Erika L. Abel. 2023. "Association between Religious Beliefs and HPV Vaccination Attitudes among College Students" Vaccines 11, no. 10: 1623. https://doi.org/10.3390/vaccines11101623
APA StyleHittson, H., McAleer, L., Saucedo, L., Mahler, L., Andino, G., Zorba, A., Walden, S., Pickett, B. E., Poole, B. D., & Abel, E. L. (2023). Association between Religious Beliefs and HPV Vaccination Attitudes among College Students. Vaccines, 11(10), 1623. https://doi.org/10.3390/vaccines11101623








