Knowledge, Attitudes, and Willingness of Healthcare Workers in Iraq’s Kurdistan Region to Vaccinate against Human Monkeypox: A Nationwide Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Sample Size and Participants
2.3. Study Tools
2.4. Study Variables
2.5. Ethical Consideration
2.6. Data Analysis
3. Results
3.1. Baseline Characteristics and Demographic Data
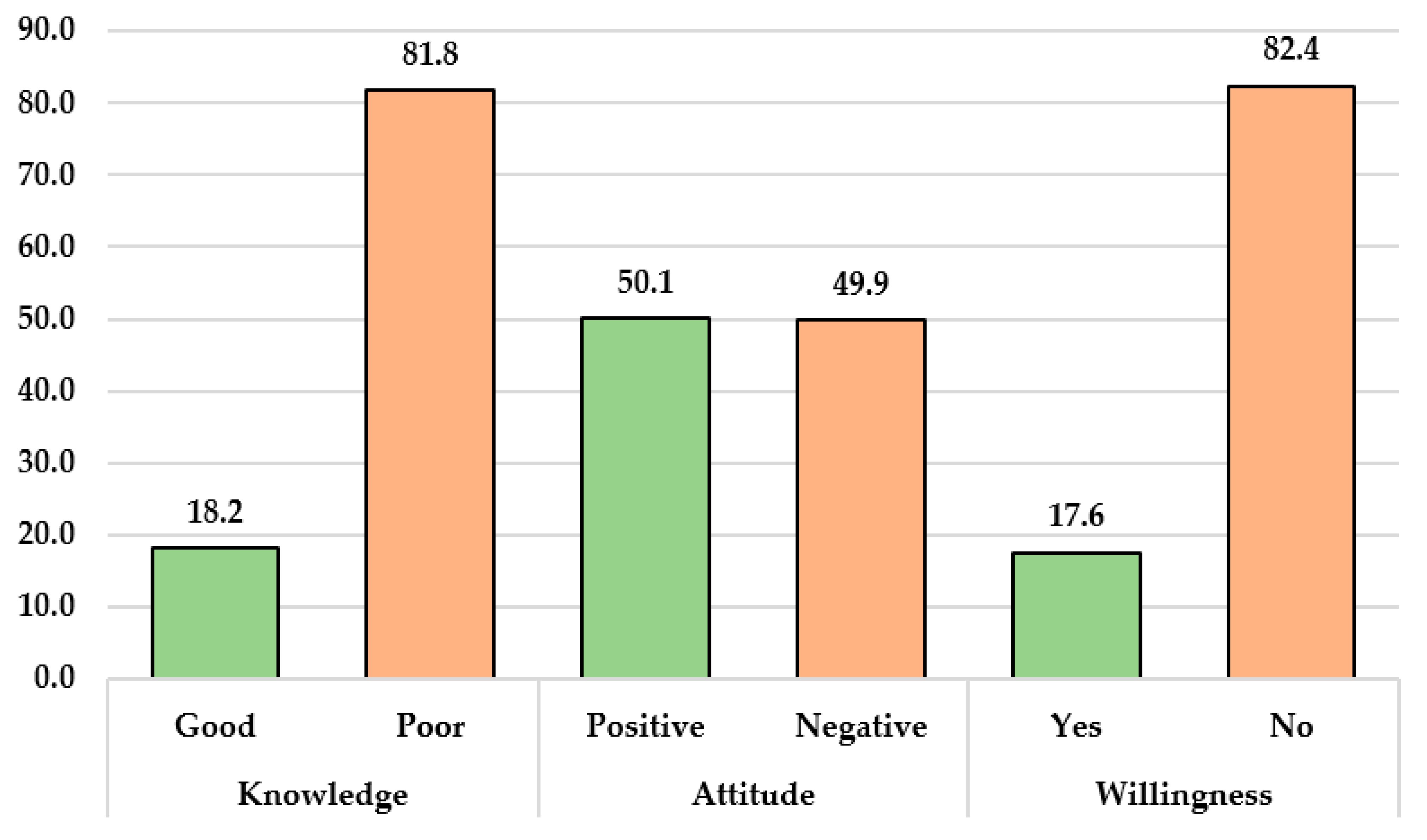
3.2. Knowledge, Attitude, and Willingness to Vaccinate against Monkeypox among HCWs
3.3. Relationships between Baseline Sociodemographic Characteristics and Knowledge, Attitude, and Willingness Scores regarding Monkeypox
3.4. Univariate Binary Logistic Regression Analysis of Knowledge, Attitude, and Willingness toward Monkeypox Vaccination
3.5. Multivariate Binary Logistic Regression Analysis of Knowledge, Attitude, and Willingness toward Monkeypox Vaccination
4. Discussion
5. Strengths and Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Parker, S.; Buller, R.M. A Review of Experimental and Natural Infections of Animals with Monkeypox Virus between 1958 and 2012. Future Virol. 2013, 8, 129–157. [Google Scholar] [CrossRef]
- Thornhill, J.P.; Barkati, S.; Walmsley, S.; Rockstroh, J.; Antinori, A.; Harrison, L.B.; Palich, R.; Nori, A.; Reeves, I.; Habibi, M.S. Monkeypox Virus Infection in Humans across 16 Countries—April–June 2022. N. Engl. J. Med. 2022, 387, 679–691. [Google Scholar] [CrossRef]
- Parker, S.; Nuara, A.; Buller, R.M.L.; Schultz, D.A. Human Monkeypox: An Emerging Zoonotic Disease. Future Microbiol. 2007, 2, 17–34. [Google Scholar] [CrossRef] [PubMed]
- Yinka-Ogunleye, A.; Aruna, O.; Dalhat, M.; Ogoina, D.; McCollum, A.; Disu, Y.; Mamadu, I.; Akinpelu, A.; Ahmad, A.; Burga, J. Outbreak of Human Monkeypox in Nigeria in 2017–18: A Clinical and Epidemiological Report. Lancet Infect. Dis. 2019, 19, 872–879. [Google Scholar] [CrossRef] [PubMed]
- Damon, I.K.; Roth, C.E.; Chowdhary, V. Discovery of Monkeypox in Sudan. N. Engl. J. Med. 2006, 355, 962–963. [Google Scholar] [CrossRef] [PubMed]
- Centres for Disease Control and Prevention (CDC). Monkeypox-Past U.S. Cases and Outbreaks. Available online: https://www.cdc.gov/poxvirus/monkeypox/outbreak/us-outbreaks.html (accessed on 20 January 2023).
- Damon, I.K. Status of Human Monkeypox: Clinical Disease, Epidemiology and Research. Vaccine 2011, 29, D54–D59. [Google Scholar] [CrossRef] [PubMed]
- Vaughan, A.; Aarons, E.; Astbury, J.; Balasegaram, S.; Beadsworth, M.; Beck, C.R.; Chand, M.; O’connor, C.; Dunning, J.; Ghebrehewet, S. Two Cases of Monkeypox Imported to the United Kingdom, September 2018. Eurosurveillance 2018, 23, 1800509. [Google Scholar] [CrossRef]
- Erez, N.; Achdout, H.; Milrot, E.; Schwartz, Y.; Wiener-Well, Y.; Paran, N.; Politi, B.; Tamir, H.; Israely, T.; Weiss, S. Diagnosis of Imported Monkeypox, Israel, 2018. Emerg. Infect. Dis. 2019, 25, 980. [Google Scholar] [CrossRef]
- Yong, S.E.F.; Ng, O.T.; Ho, Z.J.M.; Mak, T.M.; Marimuthu, K.; Vasoo, S.; Yeo, T.W.; Ng, Y.K.; Cui, L.; Ferdous, Z. Imported Monkeypox, Singapore. Emerg. Infect. Dis. 2020, 26, 1826. [Google Scholar] [CrossRef]
- Bunge, E.M.; Hoet, B.; Chen, L.; Lienert, F.; Weidenthaler, H.; Baer, L.R.; Steffen, R. The Changing Epidemiology of Human Monkeypox—A Potential Threat? A Systematic Review. PLoS Negl. Trop. Dis. 2022, 16, e0010141. [Google Scholar] [CrossRef]
- Nuzzo, J.B.; Borio, L.L.; Gostin, L.O. The WHO Declaration of Monkeypox as a Global Public Health Emergency. JAMA 2022, 328, 615–617. [Google Scholar] [CrossRef] [PubMed]
- Centres for Disease Control and Prevention (CDC). 2022 Mpox Outbreak Global Map. Available online: https://www.cdc.gov/poxvirus/monkeypox/response/2022/world-map.html (accessed on 20 January 2023).
- Patel, A.; Bilinska, J.; Tam, J.C.H.; Fontoura, D.D.S.; Mason, C.Y.; Daunt, A.; Snell, L.B.; Murphy, J.; Potter, J.; Tuudah, C. Clinical Features and Novel Presentations of Human Monkeypox in a Central London Centre during the 2022 Outbreak: Descriptive Case Series. BMJ 2022, 378, e072410. [Google Scholar] [CrossRef]
- Mileto, D.; Riva, A.; Cutrera, M.; Moschese, D.; Mancon, A.; Meroni, L.; Giacomelli, A.; Bestetti, G.; Rizzardini, G.; Gismondo, M.R. New Challenges in Human Monkeypox Outside Africa: A Review and Case Report from Italy. Travel. Med. Infect. Dis. 2022, 49, 102386. [Google Scholar] [CrossRef] [PubMed]
- Miura, F.; van Ewijk, C.E.; Backer, J.A.; Xiridou, M.; Franz, E.; de Coul, E.O.; Brandwagt, D.; van Cleef, B.; van Rijckevorsel, G.; Swaan, C. Estimated Incubation Period for Monkeypox Cases Confirmed in The Netherlands, May 2022. Eurosurveillance 2022, 27, 2200448. [Google Scholar] [CrossRef]
- Adler, H.; Gould, S.; Hine, P.; Snell, L.B.; Wong, W.; Houlihan, C.F.; Osborne, J.C.; Rampling, T.; Beadsworth, M.B.J.; Duncan, C.J.A. Clinical Features and Management of Human Monkeypox: A Retrospective Observational Study in the UK. Lancet Infect. Dis. 2022, 22, P1153–P1162. [Google Scholar] [CrossRef]
- Tarín-Vicente, E.J.; Alemany, A.; Agud-Dios, M.; Ubals, M.; Suñer, C.; Antón, A.; Arando, M.; Arroyo-Andrés, J.; Calderón-Lozano, L.; Casañ, C. Clinical Presentation and Virological Assessment of Confirmed Human Monkeypox Virus Cases in Spain: A Prospective Observational Cohort Study. Lancet 2022, 400, 661–669. [Google Scholar] [CrossRef] [PubMed]
- Girometti, N.; Byrne, R.; Bracchi, M.; Heskin, J.; McOwan, A.; Tittle, V.; Gedela, K.; Scott, C.; Patel, S.; Gohil, J. Demographic and Clinical Characteristics of Confirmed Human Monkeypox Virus Cases in Individuals Attending a Sexual Health Centre in London, UK: An Observational Analysis. Lancet Infect. Dis. 2022, 22, 1321–1328. [Google Scholar] [CrossRef]
- Thornhill, J.P.; Palich, R.; Ghosn, J.; Walmsley, S.; Moschese, D.; Cortes, C.P.; Galliez, R.M.; Garlin, A.B.; Nozza, S.; Mitja, O. Human Monkeypox Virus Infection in Women and Non-Binary Individuals during the 2022 Outbreaks: A Global Case Series. Lancet 2022, 400, 1953–1965. [Google Scholar] [CrossRef]
- Heskin, J.; Belfield, A.; Milne, C.; Brown, N.; Walters, Y.; Scott, C.; Bracchi, M.; Moore, L.S.; Mughal, N.; Rampling, T. Transmission of Monkeypox Virus through Sexual Contact-A Novel Route of Infection. J. Infect. 2022, 83, 334–363. [Google Scholar] [CrossRef]
- Parvin, R.; Ali, A. Monkeypox Virus: A Comprehensive Review of Taxonomy, Evolution, Epidemiology, Diagnosis, Prevention, and Control Regiments so Far. Ger. J. Microbiol. 2022, 2, 1–15. [Google Scholar] [CrossRef]
- Reynolds, M.G.; Damon, I.K. Outbreaks of Human Monkeypox after Cessation of Smallpox Vaccination. Trends Microbiol. 2012, 20, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Le Pluart, D.; Ruyer-Thompson, M.; Ferré, V.M.; Mailhe, M.; Descamps, D.; Bouscarat, F.; Lescure, F.-X.; Lucet, J.-C.; Yazdanpanah, Y.; Ghosn, J. A Healthcare-Associated Infection with Monkeypox Virus of a Healthcare Worker during the 2022 Outbreak. Open Forum Infect. Dis. 2022, 9, ofac520. [Google Scholar] [CrossRef]
- Tiecco, G.; Degli Antoni, M.; Storti, S.; Tomasoni, L.R.; Castelli, F.; Quiros-Roldan, E. Monkeypox, a Literature Review: What Is New and Where Does This Concerning Virus Come From? Viruses 2022, 14, 1894. [Google Scholar] [CrossRef] [PubMed]
- Sah, R.; Hada, V.; Mohanty, A.; Alshahrani, N.Z.N.; Chakraborty, S.; Bhattacharya, M.; Chakraborty, C.; Dhama, K. Recent First Report of Human-to-Dog Transmission of Monkeypox Virus Emphasizes an Urgent Need of Enhancing Surveillance and Strengthen Further Explorative Research to Reveal Its Real Magnitude of Reverse Zoonosis from Other Animals Including Pets as Like. Int. J. Surg. 2022, 106, 106949. [Google Scholar] [CrossRef]
- Seang, S.; Burrel, S.; Todesco, E.; Leducq, V.; Monsel, G.; Le Pluart, D.; Cordevant, C.; Pourcher, V.; Palich, R. Evidence of Human-to-Dog Transmission of Monkeypox Virus. Lancet 2022, 400, 658–659. [Google Scholar] [CrossRef] [PubMed]
- Martínez, J.I.; Montalbán, E.G.; Bueno, S.J.; Martínez, F.M.; Juliá, A.N.; Díaz, J.S.; Marín, N.G.; Deorador, E.C.; Forte, A.N.; García, M.A. Monkeypox Outbreak Predominantly Affecting Men Who Have Sex with Men, Madrid, Spain, 26 April to 16 June 2022. Eurosurveillance 2022, 27, 2200471. [Google Scholar] [CrossRef]
- Bragazzi, N.L.; Woldegerima, W.A.; Iyaniwura, S.A.; Han, Q.; Wang, X.; Shausan, A.; Badu, K.; Okwen, P.; Prescod, C.; Westin, M.; et al. Knowing the Unknown: The Underestimation of Monkeypox Cases. Insights and Implications from an Integrative Review of the Literature. Front. Microbiol. 2022, 13, 1011049. [Google Scholar] [CrossRef]
- Vivancos, R.; Anderson, C.; Blomquist, P.; Balasegaram, S.; Bell, A.; Bishop, L.; Brown, C.S.; Chow, Y.; Edeghere, O.; Florence, I. Community Transmission of Monkeypox in the United Kingdom, April to May 2022. Eurosurveillance 2022, 27, 2200422. [Google Scholar] [CrossRef]
- Vusirikala, A.; Charles, H.; Balasegaram, S.; Macdonald, N.; Kumar, D.; Barker-Burnside, C.; Cumiskey, K.; Dickinson, M.; Watson, M.; Olufon, O. Epidemiology of Early Monkeypox Virus Transmission in Sexual Networks of Gay and Bisexual Men, England, 2022. Emerg. Infect. Dis. 2022, 28, 2082–2086. [Google Scholar] [CrossRef]
- Van Furth, A.M.T.; van der Kuip, M.; van Els, A.L.; Fievez, L.C.R.; van Rijckevorsel, G.G.C.; van den Ouden, A.; Jonges, M.; Welkers, M.R.A. Paediatric Monkeypox Patient with Unknown Source of Infection, the Netherlands, June 2022. Eurosurveillance 2022, 27, 2200552. [Google Scholar] [CrossRef]
- Ahmed, S.K.; Abdulqadir, S.O.; Hussein, S.H.; Omar, R.M.; Ahmed, N.A.; Essa, R.A.; Dhama, K.; Lorenzo, J.M.; Abdulla, A.Q. The Impact of Monkeypox Outbreak on Mental Health and Counteracting Strategies: A Call to Action. Int. J. Surg. 2022, 106, 106943. [Google Scholar] [CrossRef]
- Bragazzi, N.L.; Khamisy-Farah, R.; Tsigalou, C.; Mahroum, N.; Converti, M. Attaching a Stigma to the LGBTQI+ Community Should Be Avoided during the Monkeypox Epidemic. J. Med. Virol. 2023, 95, e27913. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.K.; Omar, R.M.; Hussein, S.H.; Ahmed, N.A.; Abdulqadir, S.O.; Essa, R.A.; Dhama, K.; Abdulla, A.Q. Middle East Countries Preparedness for Monkeypox Outbreak: A Call to Action. Int. J. Surg. 2022, 106, 106948. [Google Scholar] [CrossRef] [PubMed]
- Peterson, B.W.; Damon, I.K. Orthopoxviruses: Vaccinia (Smallpox Vaccine), Variola (Smallpox), Monkeypox, and Cowpox. In Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases, 8th ed.; Elsevier: Philadelphia, PA, USA, 2019. [Google Scholar]
- Brown, K.; Leggat, P.A. Human Monkeypox: Current State of Knowledge and Implications for the Future. Trop. Med. Infect. Dis. 2016, 1, 8. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.K.; Rashad, E.A.A.; Mohamed, M.G.; Ravi, R.K.; Essa, R.A.; Abdulqadir, S.O.; Khdir, A.A. The Global Human Monkeypox Outbreak in 2022: An Overview. Int. J. Surg. 2022, 104, 106794. [Google Scholar] [CrossRef]
- Nath, S.D.; Majumder, K.; Rimti, F.H.; Das, J.; Tabassum, M.N.; Oishee, A.N.; Mahmood, T.; Paul, M.; Akhter, M.; Bhadra, A.B. Assessment of Knowledge on Human Monkeypox Virus among General Population in Bangladesh: A Nationwide Cross-Sectional Study. medRxiv 2022. [Google Scholar] [CrossRef]
- Vaughan, A.; Aarons, E.; Astbury, J.; Brooks, T.; Chand, M.; Flegg, P.; Hardman, A.; Harper, N.; Jarvis, R.; Mawdsley, S. Human-to-Human Transmission of Monkeypox Virus, United Kingdom, October 2018. Emerg. Infect. Dis. 2020, 26, 782. [Google Scholar] [CrossRef]
- Gong, Q.; Wang, C.; Chuai, X.; Chiu, S. Monkeypox Virus: A Re-Emergent Threat to Humans. Virol. Sin. 2022, 37, 477–482. [Google Scholar] [CrossRef]
- Philpott, D. Epidemiologic and Clinical Characteristics of Monkeypox Cases—United States, May 17–July 22, 2022. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 1018–1022. [Google Scholar] [CrossRef]
- Ly-Yang, F.; Miranda-Sánchez, A.; Burgos-Blasco, B.; Fernández-Vigo, J.I.; Gegúndez-Fernández, J.A.; Díaz-Valle, D. Conjunctivitis in an Individual with Monkeypox. JAMA Ophthalmol. 2022, 140, 1022–1024. [Google Scholar] [CrossRef]
- Tan, D.H.S.; Jaeranny, S.; Li, M.; Sukhdeo, S.S.; Monge, J.C.; Callejas, M.F.; Hasso, M.; Fattouh, R.; Lalonde, S.D.; Lam, J. Atypical Clinical Presentation of Monkeypox Complicated by Myopericarditis. Proc. Open Forum Infect. Dis. 2022, 9, ofac394. [Google Scholar] [CrossRef]
- Kaler, J.; Hussain, A.; Flores, G.; Kheiri, S.; Desrosiers, D. Monkeypox: A Comprehensive Review of Transmission, Pathogenesis, and Manifestation. Cureus 2022, 14, e26531. [Google Scholar] [CrossRef] [PubMed]
- De Sousa, D.; Frade, J.; Patrocínio, J.; Borges-Costa, J.; Filipe, P. Monkeypox Infection and Bacterial Cellulitis: A Complication to Look For. Int. J. Infect. Dis. 2022, 123, 180–182. [Google Scholar] [CrossRef] [PubMed]
- Milano, E.; Belati, A.; De Santis, L.; Tanese, F.; Vavallo, A.; Dachille, G.; Loconsole, D.; Bavaro, D.F.; Di Gennaro, F.; Chironna, M. First Case of Paraphimosis as a Severe Complication of Monkeypox. Vaccines 2023, 11, 63. [Google Scholar] [CrossRef]
- Billioux, B.J.; Mbaya, O.T.; Sejvar, J.; Nath, A. Potential Complications of Monkeypox. Lancet Neurol. 2022, 21, 872. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.K.; Dabou, E.A.; Abdelsamad, S.; Mohamed, M.G.; Chandran, D.; Chakraborty, S.; Emran, T.B.; Dhama, K. Monkeypox Virus Infection and Myocarditis: A Review of Current Evidence and Possible Pathogenesis. Narra J. 2023, 3, e104. [Google Scholar] [CrossRef]
- Fahrni, M.L.; Choudhary, O.P. Possibility of vertical transmission of the human monkeypox virus. Int. J. Surg. 2022, 105, 106832. [Google Scholar] [CrossRef]
- Boesecke, C.; Monin, M.B.; van Bremen, K.; Schlabe, S.; Hoffmann, C. Severe Monkeypox-Virus Infection in Undiagnosed Advanced HIV Infection. Infection 2022, 50, 1633–1634. [Google Scholar] [CrossRef] [PubMed]
- Menezes, Y.R.; de Miranda, A.B. Severe Disseminated Clinical Presentation of Monkeypox Virus Infection in an Immunosuppressed Patient: First Death Report in Brazil. Rev. Soc. Bras. Med. Trop. 2022, 55, e0392. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.K.; Mohamed, M.G.; Dabou, E.A.A.R.; Abuijlan, I.; Chandran, D.; Nahed, A.; Chopra, H.; Dhama, K. Monkeypox (Mpox) in Immunosuppressed Patients. F1000Research 2023, 12, 127. [Google Scholar] [CrossRef]
- Ogoina, D.; Iroezindu, M.; James, H.I.; Oladokun, R.; Yinka-Ogunleye, A.; Wakama, P.; Otike-Odibi, B.; Usman, L.M.; Obazee, E.; Aruna, O. Clinical Course and Outcome of Human Monkeypox in Nigeria. Clin. Infect. Dis. 2020, 71, e210–e214. [Google Scholar] [CrossRef]
- Chakraborty, S.; Chandran, D.; Mohapatra, R.K.; Alagawany, M.; El-Shall, N.A.; Sharma, A.K.; Chakraborty, C.; Dhama, K. Clinical Management, Antiviral Drugs and Immunotherapeutics for Treating Monkeypox. An Update on Current Knowledge and Futuristic Prospects. Int. J. Surg. 2022, 105, 106847. [Google Scholar] [CrossRef]
- De Clercq, E.; Jiang, Y.; Li, G. Therapeutic Strategies for Human Poxvirus Infections: Monkeypox (Mpox), Smallpox, Molluscipox, and Orf. Travel. Med. Infect. Dis. 2022, 52, 102528. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.K.; El-Kader, R.G.A.; Abdulqadir, S.O.; Abdullah, A.J.; Nahed, A.; Chandran, D.; Dey, A.; Emran, T.B.; Dhama, K. Monkeypox Clinical Symptoms, Pathology, and Advances in Management and Treatment Options: An Update. Int. J. Surg. 2023, 109, 2837–2840. [Google Scholar] [CrossRef] [PubMed]
- Walsh, S.R.; Dolin, R. Vaccinia Viruses: Vaccines against Smallpox and Vectors against Infectious Diseases and Tumors. Expert. Rev. Vaccines 2011, 10, 1221–1240. [Google Scholar] [CrossRef] [PubMed]
- Harapan, H.; Setiawan, A.M.; Yufika, A.; Anwar, S.; Wahyuni, S.; Asrizal, F.W.; Sufri, M.R.; Putra, R.P.; Wijayanti, N.P.; Salwiyadi, S. Knowledge of Human Monkeypox Viral Infection among General Practitioners: A Cross-Sectional Study in Indonesia. Pathog. Glob. Health 2020, 114, 68–75. [Google Scholar] [CrossRef]
- Meo, S.A.; Al-Khlaiwi, T.; Aljofan, Z.F.; Alanazi, A.I.; Meo, A.S. Public Perceptions of the Emerging Human Monkeypox Disease and Vaccination in Riyadh, Saudi Arabia: A Cross-Sectional Study. Vaccines 2022, 10, 1534. [Google Scholar] [CrossRef] [PubMed]
- Ilchmann, H.; Samy, N.; Reichhardt, D.; Schmidt, D.; Powell, J.D.; Meyer, T.P.H.; Silbernagl, G.; Nichols, R.; Weidenthaler, H.; De Moerlooze, L. Single and 2-Dose Vaccinations with Modified Vaccinia Ankara-Bavarian Nordic® Induce Durable B Cell Memory Responses Comparable to Replicating Smallpox Vaccines. J. Infect. Dis. 2023, 227, 1203–1213. [Google Scholar] [CrossRef]
- Islam, M.R.; Hossain, M.J.; Roy, A.; Hasan, A.H.M.N.; Rahman, M.A.; Shahriar, M.; Bhuiyan, M.A. Repositioning Potentials of Smallpox Vaccines and Antiviral Agents in Monkeypox Outbreak: A Rapid Review on Comparative Benefits and Risks. Health Sci. Reports 2022, 5, e798. [Google Scholar] [CrossRef]
- Russo, A.T.; Berhanu, A.; Bigger, C.B.; Prigge, J.; Silvera, P.M.; Grosenbach, D.W.; Hruby, D. Co-Administration of Tecovirimat and ACAM2000TM in Non-Human Primates: Effect of Tecovirimat Treatment on ACAM2000 Immunogenicity and Efficacy versus Lethal Monkeypox Virus Challenge. Vaccine 2020, 38, 644–654. [Google Scholar] [CrossRef]
- Harapan, H.; Wagner, A.L.; Yufika, A.; Setiawan, A.M.; Anwar, S.; Wahyuni, S.; Asrizal, F.W.; Sufri, M.R.; Putra, R.P.; Wijayanti, N.P. Acceptance and Willingness to Pay for a Hypothetical Vaccine against Monkeypox Viral Infection among Frontline Physicians: A Cross-Sectional Study in Indonesia. Vaccine 2020, 38, 6800–6806. [Google Scholar] [CrossRef]
- Aljamaan, F.; Alenezi, S.; Alhasan, K.; Saddik, B.; Alhaboob, A.; Altawil, E.S.; Alshahrani, F.; Alrabiaah, A.; Alaraj, A.; Alkriadees, K. Healthcare Workers’ Worries and Monkeypox Vaccine Advocacy during the First Month of the WHO Monkeypox Alert: Cross-Sectional Survey in Saudi Arabia. Vaccines 2022, 10, 1408. [Google Scholar] [CrossRef]
- Alshahrani, N.Z.; Alzahrani, F.; Alarifi, A.M.; Algethami, M.R.; Alhumam, M.N.; Ayied, H.A.M.; Awan, A.Z.; Almutairi, A.F.; Bamakhrama, S.A.; Almushari, B.S. Assessment of Knowledge of Monkeypox Viral Infection among the General Population in Saudi Arabia. Pathogens 2022, 11, 904. [Google Scholar] [CrossRef]
- Riad, A.; Drobov, A.; Rozmarinová, J.; Drapáčová, P.; Klugarová, J.; Dušek, L.; Pokorná, A.; Klugar, M. Monkeypox Knowledge and Vaccine Hesitancy of Czech Healthcare Workers: A Health Belief Model (HBM)-Based Study. Vaccines 2022, 10, 2022. [Google Scholar] [CrossRef]
- Zucman, D.; Fourn, E.; Touche, P.; Majerholc, C.; Vallée, A. Monkeypox Vaccine Hesitancy in French Men Having Sex with Men with PrEP or Living with HIV in France. Vaccines 2022, 10, 1629. [Google Scholar] [CrossRef]
- Gagneux-Brunon, A.; Dauby, N.; Launay, O.; Botelho-Nevers, E. Attitudes towards Monkeypox Vaccination among Healthcare Workers in France and Belgium: An Element of Complacency? J. Hosp. Infect. 2022, 130, 144–145. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Peng, X.; Li, Y.; Fu, L.; Tian, T.; Liang, B.; Sun, Y.; Chen, Y.; Wu, X.; Liu, Q. Perceptions, Precautions, and Vaccine Acceptance Related to Monkeypox in the Public in China: A Cross-Sectional Survey. J. Infect. Public Health 2022, 16, 163–170. [Google Scholar] [CrossRef] [PubMed]
- Hamdan, N.E.; Fahrni, M.L.; Lazzarino, A.I. COVID-19 Vaccination Prioritization Strategies in Malaysia: A Retrospective Analysis of Early Evidence. Vaccines 2023, 11, 48. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.K.; Abdulqadir, S.O.; Omar, R.M.; Abdullah, A.J.; Rahman, H.A.; Hussein, S.H.; Mohammed Amin, H.I.; Chandran, D.; Sharma, A.K.; Dhama, K. Knowledge, Attitude and Worry in the Kurdistan Region of Iraq during the Mpox (Monkeypox) Outbreak in 2022: An Online Cross-Sectional Study. Vaccines 2023, 11, 610. [Google Scholar] [CrossRef] [PubMed]
- Bendezu-Quispe, G.; Benites-Meza, J.K.; Urrunaga-Pastor, D.; Herrera-Añazco, P.; Uyen-Cateriano, A.; Rodriguez-Morales, A.J.; Toro-Huamanchumo, C.J.; Hernandez, A.V.; Benites-Zapata, V.A. Mass Media Use to Learn About COVID-19 and the Non-Intention to Be Vaccinated Against COVID-19 in Latin America and Caribbean Countries. Front. Med. 2022, 9, 877764. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Morales, A.J.; Franco, O.H. Public Trust, Misinformation and COVID-19 Vaccination Willingness in Latin America and the Caribbean: Today’s Key Challenges. Lancet Reg. Health 2021, 3, 100073. [Google Scholar] [CrossRef] [PubMed]
- Omrani, A.S.; Shalhoub, S. Middle East Respiratory Syndrome Coronavirus (MERS-CoV): What Lessons Can We Learn? J. Hosp. Infect. 2015, 91, 188–196. [Google Scholar] [CrossRef] [PubMed]
- McEachan, R.; Taylor, N.; Harrison, R.; Lawton, R.; Gardner, P.; Conner, M. Meta-Analysis of the Reasoned Action Approach (RAA) to Understanding Health Behaviors. Ann. Behav. Med. 2016, 50, 592–612. [Google Scholar] [CrossRef] [PubMed]
- Rasizadeh, R.; Shamekh, A.; Shiri Aghbash, P.; Bannazadeh Baghi, H. Comparison of Human Monkeypox, Chickenpox and Smallpox: A Comprehensive Review of Pathology and Dermatological Manifestations. Curr. Med. Res. Opin. 2023, 39, 751–760. [Google Scholar] [CrossRef]
- Sallam, M.; Dababseh, D.; Yaseen, A.; Al-Haidar, A.; Ababneh, N.A.; Bakri, F.G.; Mahafzah, A. Conspiracy Beliefs Are Associated with Lower Knowledge and Higher Anxiety Levels Regarding COVID-19 among Students at the University of Jordan. Int. J. Environ. Res. Public Health 2020, 17, 4915. [Google Scholar] [CrossRef]
- Ahmed, S.K.; M-Amin, H.I.; Abdulqadir, S.O.; Hussein, S.H.; Ahmed, Z.K.; Essa, R.A.; Khdir, A.A.; Abdulla, A.Q.; Omar, R.M. Timely Mental Health Care for the 2022 Novel Monkeypox Outbreak Is Urgently Needed. Ann. Med. Surg. 2022, 82, 104579. [Google Scholar] [CrossRef] [PubMed]
- Kluge, H.; Ammon, A. Monkeypox in Europe and beyond–Tackling a Neglected Disease Together. Eurosurveillance 2022, 27, 2200482. [Google Scholar] [CrossRef]
- Dong, C.; Yu, Z.; Zhao, Y.; Ma, X. Knowledge and Vaccination Intention of Monkeypox in China’s General Population: A Cross-Sectional Online Survey. Travel. Med. Infect. Dis. 2022, 52, 102533. [Google Scholar] [CrossRef]
- Gonzales-Zamora, J.; Soriano-Moreno, D.R.; Soriano-Moreno, A.N.; Ponce-Rosas, L.; Sangster-Carrasco, L.; De-Los-Rios-Pinto, A.; Benito-Vargas, R.M.; Murrieta-Ruiz, V.; Morocho-Alburqueque, N.; Caira-Chuquineyra, B. Level of Knowledge Regarding Monkeypox among Peruvian Physicians during the 2022 Outbreak: A Cross-Sectional Study. Res. Sq. 2022. [Google Scholar] [CrossRef]
- Salim, N.A.; Septadina, I.S.; Permata, M. Knowledge, Attitude, and Perception of Anticipating 2022 Global Human Monkeypox Infection among Internal Medicine Residents at Palembang Indonesia: An Online Survey. J. Kedokt Dan Kesehat Publ. Ilm. Fak. Kedokt. Univ. Sriwij 2022, 9, 253–262. [Google Scholar] [CrossRef]
- Al-Mustapha, A.I.; Sikiru, N.A.; Kolawole, B.; Oyewo, M.; Ahmed, H.; Odukoya, A.; Ogundijo, O.A.; Asiegbu, E.C.; Nanven, M.B.; Lawal-Atolagbe, T. A Cross-Sectional Survey of Public Knowledge of the Monkeypox Disease in Nigeria. BMC Public Health 2023, 23, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Ghazy, R.M.; Okeh, D.U.; Sallam, M.; Hussein, M.; Ismail, H.M.; Yazbek, S.; Mahboob, A.; Abd ElHafeez, S. Psychological Antecedents of Healthcare Workers towards Monkeypox Vaccination in Nigeria. Vaccines 2022, 10, 2151. [Google Scholar] [CrossRef] [PubMed]
- Sallam, M.; Al-Mahzoum, K.; Al-Tammemi, A.B.; Alkurtas, M.; Mirzaei, F.; Kareem, N.; Al-Naimat, H.; Jardaneh, L.; Al-Majali, L.; AlHadidi, A. Assessing Healthcare Workers’ Knowledge and Their Confidence in the Diagnosis and Management of Human Monkeypox: A Cross-Sectional Study in a Middle Eastern Country. Healthcare 2022, 10, 1722. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.; Abdulqadir, S.O.; Omar, R.M.; Hussein, S.; Qurbani, K.; Mohamed, M.G.; Blbas, H.T.A.; Fahrni, M.L. Knowledge, Attitudes, and Willingness to Vaccinate for Mpox among Healthcare Workers in Kurdistan Region of Iraq: A Nationwide Cross-Sectional Study. Preprints 2023, 2023081737. [Google Scholar] [CrossRef]
- Alsanafi, M.; Al-Mahzoum, K.; Sallam, M. Monkeypox Knowledge and Confidence in Diagnosis and Management with Evaluation of Emerging Virus Infection Conspiracies among Health Professionals in Kuwait. Pathogens 2022, 11, 994. [Google Scholar] [CrossRef]
- Harapan, H.; Setiawan, A.M.; Yufika, A.; Anwar, S.; Wahyuni, S.; Asrizal, F.W.; Sufri, M.R.; Putra, R.P.; Wijayanti, N.P.; Salwiyadi, S. Physicians’ Willingness to Be Vaccinated with a Smallpox Vaccine to Prevent Monkeypox Viral Infection: A Cross-Sectional Study in Indonesia. Clin. Epidemiol. Glob. Health 2020, 8, 1259–1263. [Google Scholar] [CrossRef]
- Harapan, H.; Setiawan, A.M.; Yufika, A.; Anwar, S.; Wahyuni, S.; Asrizal, F.W.; Sufri, M.R.; Putra, R.P.; Wijayanti, N.P.; Salwiyadi, S. Confidence in Managing Human Monkeypox Cases in Asia: A Cross-Sectional Survey among General Practitioners in Indonesia. Acta Trop. 2020, 206, 105450. [Google Scholar] [CrossRef]
- Alshahrani, N.Z.; Algethami, M.R.; Alarifi, A.M.; Alzahrani, F.; Sheerah, H.A.; Abdelaal, A.; Sah, R.; Rodriguez-Morales, A.J. Knowledge and Attitude Regarding Monkeypox Virus among Physicians in Saudi Arabia, a Cross-Sectional Study. Vaccines 2022, 10, 2099. [Google Scholar] [CrossRef]
- Alshahrani, N.Z.; Mitra, S.; Alkuwaiti, A.A.; Alhumam, M.N.; Altmimi, S.M.B.; Alamri, M.H.M.; Albalawi, Z.A.S.; Almorgi, M.W.; Alharbi, H.K.D.; Alshahrani, S.M. Medical Students’ Perception Regarding the Re-Emerging Monkeypox Virus: An Institution-Based Cross-Sectional Study From Saudi Arabia. Cureus 2022, 14, e28060. [Google Scholar] [CrossRef]
- Bates, B.R.; Grijalva, M.J. Knowledge, Attitudes, and Practices towards Monkeypox during the 2022 Outbreak: An Online Cross-Sectional Survey among Clinicians in Ohio, USA. J. Infect Public Health 2022, 15, 1459–1465. [Google Scholar] [CrossRef]
- Jairoun, A.A.; Al-Hemyari, S.S.; Abdulla, N.M.; El-Dahiyat, F.; Shahwan, M.; Hassan, N.; Alyousef, N.G.; Sharif, S.; Jaber, A.A.S. Awareness and Preparedness of Human Monkeypox Outbreak among University Student: Time to Worry or One to Ignore? J. Infect. Public Health 2022, 15, 1065–1071. [Google Scholar] [CrossRef] [PubMed]
- Lin, G.S.S.; Tan, W.W.; Chan, D.Z.K.; Ooi, K.S.; Hashim, H. Monkeypox Awareness, Knowledge, and Attitude among Undergraduate Preclinical and Clinical Students at a Malaysian Dental School: An Emerging Outbreak during the COVID-19 Era. Asian Pac. J. Trop. Med. 2022, 15, 461. [Google Scholar] [CrossRef]
- Sallam, M.; Eid, H.; Awamleh, N.; Al-Tammemi, A.B.; Barakat, M.; Athamneh, R.Y.; Hallit, S.; Harapan, H.; Mahafzah, A. Conspiratorial Attitude of the General Public in Jordan towards Emerging Virus Infections: A Cross-Sectional Study Amid the 2022 Monkeypox Outbreak. Trop. Med. Infect. Dis. 2022, 7, 411. [Google Scholar] [CrossRef]
- Temsah, M.-H.; Aljamaan, F.; Alenezi, S.; Alhasan, K.; Saddik, B.; Al-Barag, A.; Alhaboob, A.; Bahabri, N.; Alshahrani, F.; Alrabiaah, A. Monkeypox Caused Less Worry than COVID-19 among the General Population during the First Month of the WHO Monkeypox Alert: Experience from Saudi Arabia. Travel. Med. Infect. Dis. 2022, 49, 102426. [Google Scholar] [CrossRef] [PubMed]
- Ogoina, D.; Izibewule, J.H.; Ogunleye, A.; Ederiane, E.; Anebonam, U.; Neni, A.; Oyeyemi, A.; Etebu, E.N.; Ihekweazu, C. The 2017 Human Monkeypox Outbreak in Nigeria—Report of Outbreak Experience and Response in the Niger Delta University Teaching Hospital, Bayelsa State, Nigeria. PLoS ONE 2019, 14, e0214229. [Google Scholar] [CrossRef]
- Ibrahim, P.K.; Abdulrahman, D.S.; Ali, H.M.; Haji, R.M.; Ahmed, S.K.; Ahmed, N.A.; Abdulqadir, S.O.; Kareem, S.A.; Kamali, A.S.M.A. The 2022 Monkeypox Outbreak—Special Attention to Nurses’ Protection Should Be a Top Priority. Ann. Med. Surg. 2022, 82, 104615. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.K. Prevention, Vaccination, Management and Infection Control of Monkeypox Outbreak: An Update Global Recommendation for the Next Year 2023. J. Pure Appl. Microbiol. 2022, 16, 3189–3191. [Google Scholar] [CrossRef]
- Al-Mandhari, A.; Kodama, C.; Abubakar, A.; Hajjeh, R.; Brennan, R. Monkeypox Outbreak and Response Efforts in the Eastern Mediterranean Region. East. Mediterr. Health J. 2022, 28, 465–468. [Google Scholar] [CrossRef] [PubMed]
- Shariq, A.; Rasheed, Z.; Al Abdulmonem, W. Human Monkeypox: An Update on Knowledge and Future Implications. Int. J. Health Sci. 2022, 16, 1–2. [Google Scholar]
- Koenig, K.L.; Beÿ, C.K.; Marty, A.M. Monkeypox 2022: A Primer and Identify-Isolate-Inform (3I) Tool for Emergency Medical Services Professionals. Prehosp. Disaster. Med. 2022, 37, 687–692. [Google Scholar] [CrossRef]
- Ministry of Health. Indicators in the Kurdistan Region. Available online: https://gov.krd/moh-en/publications/ (accessed on 20 January 2023).
- Riccò, M.; Ferraro, P.; Camisa, V.; Satta, E.; Zaniboni, A.; Ranzieri, S.; Baldassarre, A.; Zaffina, S.; Marchesi, F. When a Neglected Tropical Disease Goes Global: Knowledge, Attitudes and Practices of Italian Physicians towards Monkeypox, Preliminary Results. Trop. Med. Infect. Dis. 2022, 7, 135. [Google Scholar] [CrossRef] [PubMed]
- Taber, K.S. The Use of Cronbach’s Alpha When Developing and Reporting Research Instruments in Science Education. Res. Sci. Educ. 2018, 48, 1273–1296. [Google Scholar] [CrossRef]
- Malaeb, D.; Sallam, M.; Salim, N.A.; Dabbous, M.; Younes, S.; Nasrallah, Y.; Iskandar, K.; Matta, M.; Obeid, S.; Hallit, S. Knowledge, Attitude and Conspiracy Beliefs of Healthcare Workers in Lebanon towards Monkeypox. Trop. Med. Infect. Dis. 2023, 8, 81. [Google Scholar] [CrossRef] [PubMed]
- Haldane, V.; De Foo, C.; Abdalla, S.M.; Jung, A.-S.; Tan, M.; Wu, S.; Chua, A.; Verma, M.; Shrestha, P.; Singh, S. Health Systems Resilience in Managing the COVID-19 Pandemic: Lessons from 28 Countries. Nat. Med. 2021, 27, 964–980. [Google Scholar] [CrossRef]
- Lai, C.-C.; Hsu, C.-K.; Yen, M.-Y.; Lee, P.-I.; Ko, W.-C.; Hsueh, P.-R. Monkeypox: An Emerging Global Threat during the COVID-19 Pandemic. J. Microbiol. Immunol. Infect. 2022, 55, 787–794. [Google Scholar] [CrossRef]
- Miraglia del Giudice, G.; Della Polla, G.; Folcarelli, L.; Napoli, A.; Angelillo, I.F.; Longanella, W.; Mensorio, M.M.; Cantore, F.; Group, C.W. Knowledge and Attitudes of Health Care Workers about Monkeypox Virus Infection in Southern Italy. Front. Public Health 2023, 11, 1091267. [Google Scholar] [CrossRef]
- Temsah, M.-H.; Aljamaan, F.; Alenezi, S.; Abouammoh, N.; Alhasan, K.; Dasuqi, S.A.; Alhaboob, A.; Hamad, M.A.; Halwani, R.; Alrabiaah, A. Monkeypox Disease (MPOX) Perceptions among Healthcare Workers versus General Population during the First Month of the WHO Alert: Cross-Sectional Survey in Saudi Arabia. Vaccines 2022, 10, 2071. [Google Scholar] [CrossRef]
- Hasan, M.; Hossain, M.A.; Chowdhury, S.; Das, P.; Jahan, I.; Rahman, M.F.; Haque, M.M.A.; Rashid, M.U.; Khan, M.A.S.; Hossian, M. Human Monkeypox and Preparedness of Bangladesh: A Knowledge and Attitude Assessment Study among Medical Doctors. J. Infect. Public Health 2023, 16, 90–95. [Google Scholar] [CrossRef]
- Sallam, M.; Al-Mahzoum, K.; Dardas, L.A.; Al-Tammemi, A.B.; Al-Majali, L.; Al-Naimat, H.; Jardaneh, L.; AlHadidi, F.; Al-Salahat, K.; Al-Ajlouni, E. Knowledge of Human Monkeypox and Its Relation to Conspiracy Beliefs among Students in Jordanian Health Schools: Filling the Knowledge Gap on Emerging Zoonotic Viruses. Medicina 2022, 58, 924. [Google Scholar] [CrossRef]
- Abd ElHafeez, S.; Gebreal, A.; Khalil, M.A.; Youssef, N.; Sallam, M.; Elshabrawy, A.; Abdel-Rahman, S.; Mahboob, A.S.; Yazbek, S.; Elbanna, E.H.; et al. Assessing Disparities in Medical Students’ Knowledge and Attitude about Monkeypox: A Cross-Sectional Study of 27 Countries across Three Continents. Front. Public Health 2023, 11, 1192542. [Google Scholar] [CrossRef]
- Sobaikhi, N.H.; Alshahrani, N.Z.; Hazazi, R.S.; Al-Musawa, H.I.; Jarram, R.E.; Alabah, A.E.; Haqawi, N.F.; Munhish, F.A.; Shajeri, M.A.; Matari, M.H.; et al. Health Workers’ Knowledge and Attitude towards Monkeypox in Southwestern Saudi Arabia: A Cross-Sectional Study. Diseases 2023, 11, 83. [Google Scholar]
- Masoud, D.; Pierz, A.; Rauh, L.; Cruz, A.K.; Palmedo, C.; Ratzan, S. Vaccine Trust Gauge: Mixed Methods Research to Measure and Understand Vaccine Trust. Vaccine 2023, 41, 4616–4624. [Google Scholar] [CrossRef]
- Ulloque-Badaracco, J.R.; Alarcón-Braga, E.A.; Hernandez-Bustamante, E.A.; Al-kassab-Córdova, A.; Benites-Zapata, V.A.; Bonilla-Aldana, D.K.; Rodriguez-Morales, A.J. Acceptance towards Monkeypox Vaccination: A Systematic Review and Meta-Analysis. Pathogens 2022, 11, 1248. [Google Scholar] [CrossRef] [PubMed]
- Lounis, M.; Riad, A. Monkeypox (MPOX)-Related Knowledge and Vaccination Hesitancy in Non-Endemic Countries: Concise Literature Review. Vaccines 2023, 11, 229. [Google Scholar] [CrossRef] [PubMed]
- Mahameed, H.; Al-Mahzoum, K.; AlRaie, L.A.; Aburumman, R.; Al-Naimat, H.; Alhiary, S.; Barakat, M.; Al-Tammemi, A.B.; Salim, N.A.; Sallam, M. Previous Vaccination History and Psychological Factors as Significant Predictors of Willingness to Receive Mpox Vaccination and a Favorable Attitude towards Compulsory Vaccination. Vaccines 2023, 11, 897. [Google Scholar] [CrossRef]
- Winters, M.; Malik, A.A.; Omer, S.B. Attitudes towards Monkeypox Vaccination and Predictors of Vaccination Intentions among the US General Public. PLoS ONE 2022, 17, e0278622. [Google Scholar] [CrossRef]
- Kumar, N.; Ahmed, F.; Raza, M.S.; Rajpoot, P.L.; Rehman, W.; Khatri, S.A.; Mohammed, M.; Muhammad, S.; Ahmad, R. Monkeypox Cross-Sectional Survey of Knowledge, Attitudes, Practices, and Willingness to Vaccinate among University Students in Pakistan. Vaccines 2022, 11, 97. [Google Scholar] [CrossRef]
- Sahin, T.K.; Erul, E.; Aksun, M.S.; Sonmezer, M.C.; Unal, S.; Akova, M. Knowledge and Attitudes of Turkish Physicians towards Human Monkeypox Disease and Related Vaccination: A Cross-Sectional Study. Vaccines 2022, 11, 19. [Google Scholar] [CrossRef]
- Neufeind, J.; Schmid-Küpke, N.; Rehfuess, E.; Betsch, C.; Wichmann, O. How a Generally Well-Accepted Measles Vaccine Mandate May Lead to Inequities and Decreased Vaccine Uptake: A Preregistered Survey Study in Germany. BMC Public Health 2022, 22, 1846. [Google Scholar] [CrossRef]
- Bardosh, K.; De Figueiredo, A.; Gur-Arie, R.; Jamrozik, E.; Doidge, J.; Lemmens, T.; Keshavjee, S.; Graham, J.E.; Baral, S. The Unintended Consequences of COVID-19 Vaccine Policy: Why Mandates, Passports and Restrictions May Cause More Harm than Good. BMJ Glob. Health 2022, 7, e008684. [Google Scholar] [CrossRef]
| Variables | Items | Frequency | Percentage |
|---|---|---|---|
| Age | 21–30 | 401 | 63.0 |
| 31–40 | 173 | 27.2 | |
| 41+ | 63 | 9.8 | |
| Gender | Male | 318 | 49.9 |
| Female | 319 | 50.1 | |
| Marital status | Single | 314 | 49.3 |
| Married | 304 | 47.7 | |
| Widow/er | 19 | 3 | |
| Level of education | Undergraduate (diploma or BSc degree) | 616 | 96.7 |
| Postgraduate (MSc, PhD, or its equivalent) | 21 | 3.3 | |
| Work experience | Less than 1 year | 168 | 26.4 |
| 1–5 years | 271 | 42.5 | |
| More than 5 years | 198 | 31.1 | |
| Occupational category | Medical technicians | 130 | 20.4 |
| Nurse | 227 | 35.6 | |
| Pharmacist | 121 | 19.0 | |
| Dentist | 65 | 10.2 | |
| Physician | 94 | 14.8 | |
| Residence area | The capital (Erbil) | 166 | 26.1 |
| Outside the capital | 471 | 73.9 | |
| Heard about the human monkeypox before 2022? | Yes | No | |
| 382 (60%) | 255 (40%) | ||
| Knowledge Items | Correct Answers n (%) | Incorrect Answers n (%) |
|---|---|---|
| Q1. Monkeypox is a new infection that appeared this year, 2022. | 324 (50.9) | 313 (49.1) |
| Q2. Monkeypox is a viral disease infection. | 476 (74.7) | 161 (25.3) |
| Q3. Monkeypox is a bacterial infection. | 443 (69.5) | 193 (30.3) |
| Q4. Monkeypox is prevalent in Middle Eastern countries. | 283 (44.4) | 354 (55.6) |
| Q5. Monkeypox is prevalent in Western and Central Africa. | 334 (52.4) | 303 (47.6) |
| Q6. There are many human monkeypox cases in Iraq. | 328 (51.5) | 309 (48.5) |
| Q7. Monkeypox is transmitted from one person to another. | 435 (68.3) | 202 (31.7) |
| Q8. Monkeypox is transmitted to humans through direct contact from infected animals. | 442 (69.4) | 195 (30.6) |
| Q9. Monkeypox is spread by droplets (coughing and sneezing). | 320 (50.2) | 317 (49.8) |
| Q10. Monkeypox and smallpox have similar signs and symptoms. | 176 (27.6) | 461 (72.4) |
| Q11. Monkeypox infection is associated with typical skin lesions. | 377 (59.2) | 260 (40.8) |
| Q12. Lymphadenopathy (swollen lymph nodes) is one clinical sign or symptom that could be used to differentiate between monkeypox and smallpox cases. | 275 (43.2) | 362 (56.8) |
| Q13. There is a specific vaccine for monkeypox. | 195 (30.6) | 442 (69.4) |
| Q14. There is a smallpox vaccine that can be used for monkeypox. | 197 (30.9) | 440 (69.1) |
| Q15. There is a specific treatment for monkeypox. | 224 (35.2) | 413 (64.8) |
| Q16. Antivirals are required in the management of human monkeypox patients. | 385 (60.4) | 252 (39.6) |
| Question No. | Questions | Agree No. (%) | Disagree or Undecided No. (%) | |
|---|---|---|---|---|
| Attitude toward monkeypox | ||||
| A1 | I am confident that the spread of monkeypox infection can be controlled worldwide. | 404 (63.4) | 233 (36.6) | |
| A2 | I am interested in learning more about monkeypox. | 484 (76) | 153 (24.0) | |
| A3 | I think that monkeypox can add a burden on healthcare systems of affected countries. | 422 (66.2) | 215 (33.8) | |
| A4 | I think that mass media coverage of monkeypox influenced prevention worldwide. | 400 (62.8) | 237 (37.2) | |
| A5 | I think that it is dangerous to travel to the countries where monkeypox cases were detected. | 460 (72.2) | 177 (27.8) | |
| Willingness of HCWs to be vaccinated against monkeypox | ||||
| W1 | I am considering getting the smallpox vaccine to prevent against contracting monkeypox infection. | 395 (62) | 242 (38.0) | |
| W2 | The monkeypox infection has been alleviated, and there is no need to be vaccinated against the monkeypox virus. | 177 (27.8) | 460 (72.2) | |
| W3 | I am worried about the possible side effects of the monkeypox vaccine. | 307 (48.2) | 330 (58.1) | |
| W4 | The recommendation for the vaccination by doctors, community pharmacists, and other healthcare professionals has had a great influence on me. | 333 (52.3) | 188 (29.5) | |
| W5 | If the country provides a vaccination against monkeypox infection for free, I am willing to be vaccinated. | 327 (51.3) | 304 (47.7) |
| Variables | Knowledge | Attitude | Willingness | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Good | Poor | X2 | p-Value | Positive | Negative | X2 | p-Value | Yes | No | X2 | p-Value | ||
| Age (years) | 21–30 | 73 (18.2) | 328 (81.8) | 0.03 | 0.98 | 183 (45.6) | 218 (54.4) | 9.17 | 0.01 | 63 (15.7) | 338 (84.3) | 2.61 | 0.27 |
| 31–40 | 32 (18.5) | 141 (81.5) | 97 (56.1) | 76 (43.9) | 36 (20.8) | 137 (79.2) | |||||||
| 41+ | 11 (17.5) | 52 (82.5) | 39 (61.9) | 24 (38.1) | 13 (20.6) | 50 (79.4) | |||||||
| Gender | Male | 54 (16.9) | 265 (83.1) | 0.70 | 0.40 | 162 (74.0) | 157 (26.0) | 0.12 | 0.72 | 50 (15.7) | 269 (84.3) | 1.60 | 0.20 |
| Female | 62 (19.5) | 256 (80.5) | 157 (49.4) | 161 (50.6) | 62 (19.5) | 256 (80.5) | |||||||
| Marital status | Single | 55 (17.5) | 259 (82.5) | 2.71 | 0.25 | 128 (40.8) | 186 (59.2) | 21.6 | <0.01 | 57 (18.2) | 257 (81.8) | 0.16 | 0.92 |
| Married | 60 (19.7) | 244 (80.3) | 179 (58.9) | 125 (41.1) | 52 (17.1) | 252 (82.9) | |||||||
| Widow/er | 1 (5.3) | 18 (94.7) | 12 (63.2) | 7 (36.8) | 3 (15.8) | 16 (84.2) | |||||||
| Level of education | Undergraduate | 115 (18.7) | 501 (81.3) | 2.63 | 0.10 | 308 (50.0) | 308 (50.0) | 0.04 | 0.83 | 109 (17.7) | 507 (82.3) | 0.16 | 0.68 |
| Graduate | 1 (4.8) | 20 (95.2) | 11 (52.4) | 10 (47.6) | 3 (14.3) | 18 (85.7) | |||||||
| Duration of practice | Less than 1 year | 31 (18.5) | 137 (81.5) | 1.54 | 0.46 | 52 (31.0) | 116 (69.0) | 37.0 | <0.01 | 31 (18.5) | 137 (81.5) | 0.31 | 0.85 |
| 1–5 years | 44 (16.2) | 227 (83.8) | 144 (53.1) | 127 (46.9) | 45 (16.6) | 226 (83.4) | |||||||
| More than 5 years | 41 (20.7) | 157 (79.3) | 123 (62.1) | 75 (37.9) | 36 (18.2) | 162 (81.8) | |||||||
| Occupation | Medical technician | 18 (13.8) | 112 (86.2) | 5.77 | 0.21 | 57 (43.8) | 73 (56.2) | 3.48 | 0.48 | 14 (10.8) | 116 (89.2) | 7.63 | 0.10 |
| Nurse | 44 (19.4) | 183 (80.6) | 120 (52.9) | 107 (47.1) | 42 (18.5) | 185 (81.5) | |||||||
| Pharmacist | 29 (24.0) | 92 (76.0) | 59 (48.8) | 62 (51.2) | 22 (18.2) | 99 (81.8) | |||||||
| Dentist | 12 (18.5) | 53 (81.5) | 32 (49.2) | 33 (50.8) | 17 (26.2) | 48 (73.8) | |||||||
| Physician | 13 (13.8) | 81 (86.2) | 51 (54.3) | 43 (45.7) | 17 (18.1) | 77 (81.9) | |||||||
| Place of residence | Outside the capital | 91 (19.3) | 380 (80.7) | 1.49 | 0.21 | 224 (47.6) | 247 (52.4) | 4.59 | 0.03 | 86 (18.3) | 385 (81.7) | 0.57 | 0.45 |
| Inside the capital (Erbil) | 25 (15.1) | 141 (84.9) | 95 (57.2) | 71 (42.8) | 26 (15.7) | 140 (84.3) | |||||||
| Heard about human monkeypox before 2022 | Yes | 98 (25.7) | 284 (74.3) | 35.5 | <0.01 | 196 (51.3) | 186 (48.7) | 0.57 | 0.44 | 65 (17.0) | 317 (83.0) | 0.21 | 0.64 |
| No | 18 (7.1) | 237 (92.9) | 123 (48.2) | 132 (51.8) | 47 (18.4) | 208 (81.6) | |||||||
| Items | Knowledge | Attitude | Willingness | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | ||||
| Age (41+ as ref.) | ||||||||||||
| 21–30 years | 1.05 | 0.52 | 2.11 | 0.887 | 0.51 | 0.29 | 0.89 | 0.018 | 0.71 | 0.36 | 1.39 | 0.328 |
| 31–40 years | 1.07 | 0.50 | 2.28 | 0.855 | 0.78 | 0.43 | 1.41 | 0.423 | 1.01 | 0.49 | 2.06 | 0.977 |
| Gender (female as ref.) | ||||||||||||
| Male | 0.84 | 0.56 | 1.25 | 0.401 | 1.05 | 0.77 | 1.44 | 0.721 | 0.76 | 0.50 | 1.15 | 0.206 |
| Marital status (widow/er as ref.) | ||||||||||||
| Single | 3.82 | 0.50 | 29.23 | 0.196 | 0.40 | 0.15 | 1.04 | 0.062 | 1.18 | 0.33 | 4.19 | 0.795 |
| Married | 4.42 | 0.57 | 33.81 | 0.152 | 0.83 | 0.32 | 2.18 | 0.713 | 1.10 | 0.30 | 3.91 | 0.882 |
| Educational level (postgraduate as ref.) | ||||||||||||
| Undergraduate | 0.21 | 0.02 | 1.64 | 0.139 | 0.90 | 0.38 | 2.17 | 0.830 | 1.29 | 0.37 | 4.45 | 0.687 |
| Duration of practice (more than 5 years as ref.) | ||||||||||||
| Less than 1 year | 0.86 | 0.51 | 1.45 | 0.589 | 0.27 | 0.17 | 0.42 | < 0.01 | 1.01 | 0.59 | 1.73 | 0.947 |
| Between 1 and 5 years | 0.74 | 0.46 | 1.18 | 0.215 | 0.69 | 0.47 | 1.00 | 0.053 | 0.89 | 0.55 | 1.45 | 0.656 |
| Occupation (physician as ref.) | ||||||||||||
| Medical technician | 1.00 | 0.46 | 2.16 | 0.997 | 0.65 | 0.38 | 1.12 | 0.125 | 0.54 | 0.25 | 1.17 | 0.121 |
| Nurse | 1.49 | 0.76 | 2.93 | 0.238 | 0.94 | 0.58 | 1.53 | 0.820 | 1.02 | 0.55 | 1.91 | 0.930 |
| Pharmacist | 1.96 | 0.95 | 4.03 | 0.066 | 0.80 | 0.46 | 1.37 | 0.424 | 1.00 | 0.50 | 2.02 | 0.985 |
| Dentist | 1.41 | 0.59 | 3.32 | 0.432 | 0.81 | 0.43 | 1.54 | 0.533 | 1.60 | 0.74 | 3.44 | 0.225 |
| Residence (inside the capital of “Erbil” as ref.) | ||||||||||||
| Outside the capital | 1.35 | 0.83 | 2.18 | 0.223 | 0.67 | 0.47 | 0.96 | 0.033 | 1.20 | 0.74 | 1.94 | 0.450 |
| Heard about monkeypox before 2022 (no as ref.) | ||||||||||||
| Yes | 4.54 | 2.67 | 7.73 | < 0.01 | 1.13 | 0.82 | 1.55 | 0.447 | 0.90 | 0.60 | 1.37 | 0.64 |
| Items | Knowledge | Attitude | Willingness | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AOR | 95% CI | P | AOR | 95% CI | P | AOR | 95% CI | P | ||||
| Age (41+ as ref.) | ||||||||||||
| 21–30 years | - | - | - | - | 0.95 | 0.51 | 1.77 | 0.887 | - | - | - | - |
| 31–40 years | - | - | - | - | 0.91 | 0.49 | 1.68 | 0.778 | - | - | - | - |
| Gender (female as ref.) | ||||||||||||
| Male | - | - | - | - | - | - | - | - | 0.78 | 0.51 | 1.20 | 0.268 |
| Marital status (widow/er as ref.) | ||||||||||||
| Single | 2.99 | 0.37 | 23.90 | 0.302 | 0.48 | 0.17 | 1.32 | 0.158 | - | - | - | - |
| Married | 3.42 | 0.42 | 27.37 | 0.246 | 0.70 | 0.26 | 1.88 | 0.481 | - | - | - | - |
| Educational level (postgraduate as ref.) | ||||||||||||
| Undergraduate | 4.45 | 0.56 | 35.15 | 0.156 | - | - | - | - | - | - | - | - |
| Duration of practice (more than 5 years as ref.) | ||||||||||||
| Less than 1 year | 0.95 | 0.50 | 1.79 | 0.875 | 0.35 | 0.20 | 0.59 | < 0.01 | - | - | - | - |
| Between 1 and 5 years | 0.75 | 0.44 | 1.28 | 0.299 | 0.79 | 0.51 | 1.22 | 0.294 | - | - | - | - |
| Occupation (physician as ref.) | ||||||||||||
| Medical technician | 1.19 | 0.53 | 2.68 | 0.664 | 0.74 | 0.42 | 1.31 | 0.314 | 0.56 | 0.26 | 1.20 | 0.139 |
| Nurse | 1.82 | 0.89 | 3.72 | 0.099 | 1.07 | 0.64 | 1.79 | 0.787 | 1.03 | 0.55 | 1.93 | 0.916 |
| Pharmacist | 1.81 | 0.85 | 3.86 | 0.122 | 0.83 | 0.47 | 1.46 | 0.529 | 0.96 | 0.47 | 1.94 | 0.918 |
| Dentist | 1.51 | 0.62 | 3.70 | 0.360 | 0.83 | 0.42 | 1.61 | 0.586 | 1.62 | 0.75 | 3.47 | 0.215 |
| Residence (inside the capital of “Erbil” as ref.) | ||||||||||||
| Outside the capital | 1.38 | 0.82 | 2.31 | 0.215 | 0.81 | 0.55 | 1.19 | 0.294 | - | - | - | - |
| Heard about monkeypox before 2022 (no as ref.) | ||||||||||||
| Yes | 4.85 | 2.81 | 8.36 | <0.001 | - | - | - | - | - | - | - | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahmed, S.K.; Abdulqadir, S.O.; Omar, R.M.; Hussein, S.; Qurbani, K.; Mohamed, M.G.; Abubaker Blbas, H.T.; Fahrni, M.L.; Lazzarino, A.I. Knowledge, Attitudes, and Willingness of Healthcare Workers in Iraq’s Kurdistan Region to Vaccinate against Human Monkeypox: A Nationwide Cross-Sectional Study. Vaccines 2023, 11, 1734. https://doi.org/10.3390/vaccines11121734
Ahmed SK, Abdulqadir SO, Omar RM, Hussein S, Qurbani K, Mohamed MG, Abubaker Blbas HT, Fahrni ML, Lazzarino AI. Knowledge, Attitudes, and Willingness of Healthcare Workers in Iraq’s Kurdistan Region to Vaccinate against Human Monkeypox: A Nationwide Cross-Sectional Study. Vaccines. 2023; 11(12):1734. https://doi.org/10.3390/vaccines11121734
Chicago/Turabian StyleAhmed, Sirwan Khalid, Salar Omer Abdulqadir, Rukhsar Muhammad Omar, Safin Hussein, Karzan Qurbani, Mona Gamal Mohamed, Hazhar Talaat Abubaker Blbas, Mathumalar Loganathan Fahrni, and Antonio Ivan Lazzarino. 2023. "Knowledge, Attitudes, and Willingness of Healthcare Workers in Iraq’s Kurdistan Region to Vaccinate against Human Monkeypox: A Nationwide Cross-Sectional Study" Vaccines 11, no. 12: 1734. https://doi.org/10.3390/vaccines11121734
APA StyleAhmed, S. K., Abdulqadir, S. O., Omar, R. M., Hussein, S., Qurbani, K., Mohamed, M. G., Abubaker Blbas, H. T., Fahrni, M. L., & Lazzarino, A. I. (2023). Knowledge, Attitudes, and Willingness of Healthcare Workers in Iraq’s Kurdistan Region to Vaccinate against Human Monkeypox: A Nationwide Cross-Sectional Study. Vaccines, 11(12), 1734. https://doi.org/10.3390/vaccines11121734








