Profile and Outcomes of Hospitalized COVID-19 Patients during the Prevalence of the Omicron Variant According to the Brazilian Regions: A Retrospective Cohort Study from 2022
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Setting
2.2. Data Extraction
2.3. Statistical Analysis
3. Results
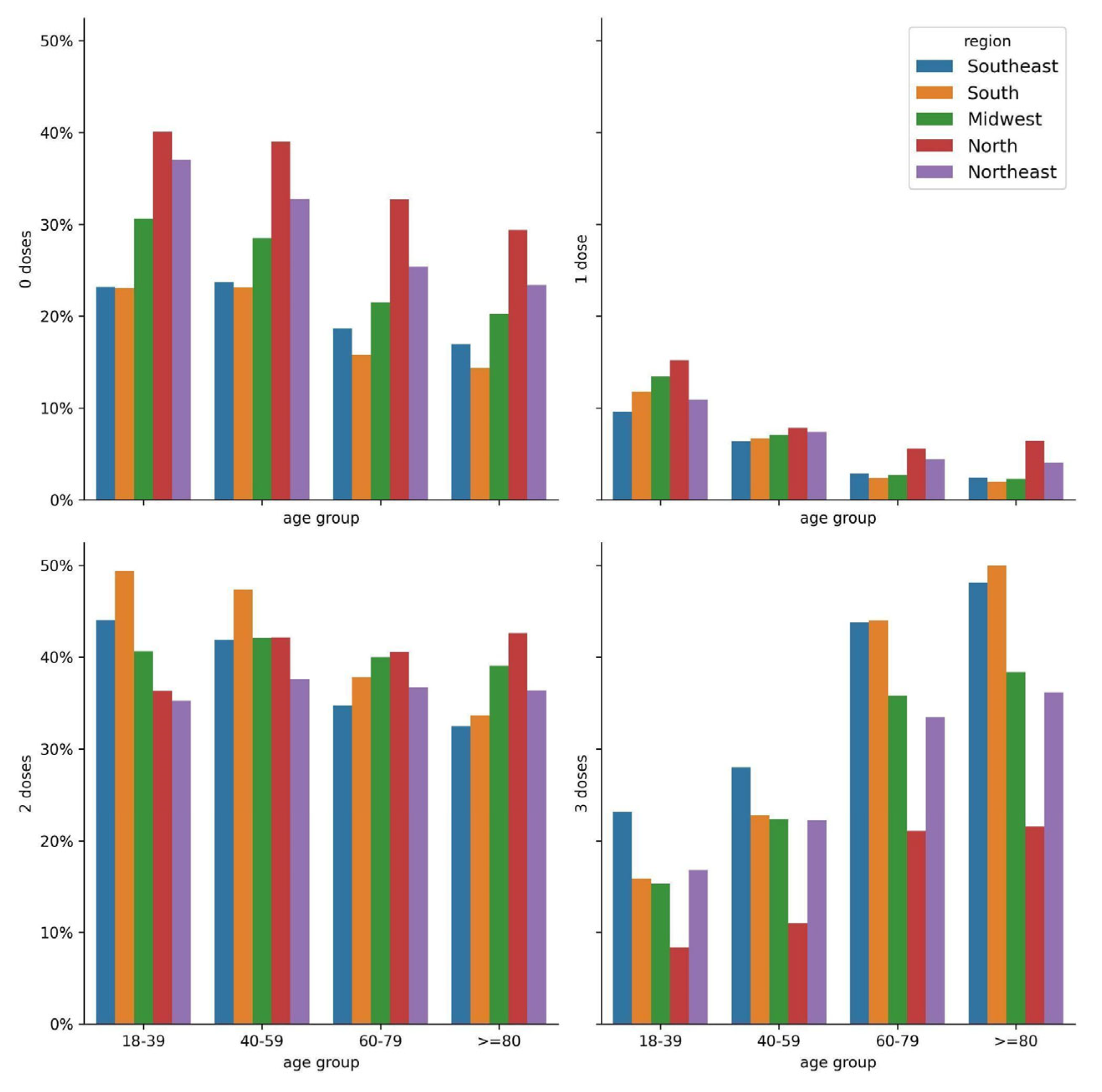
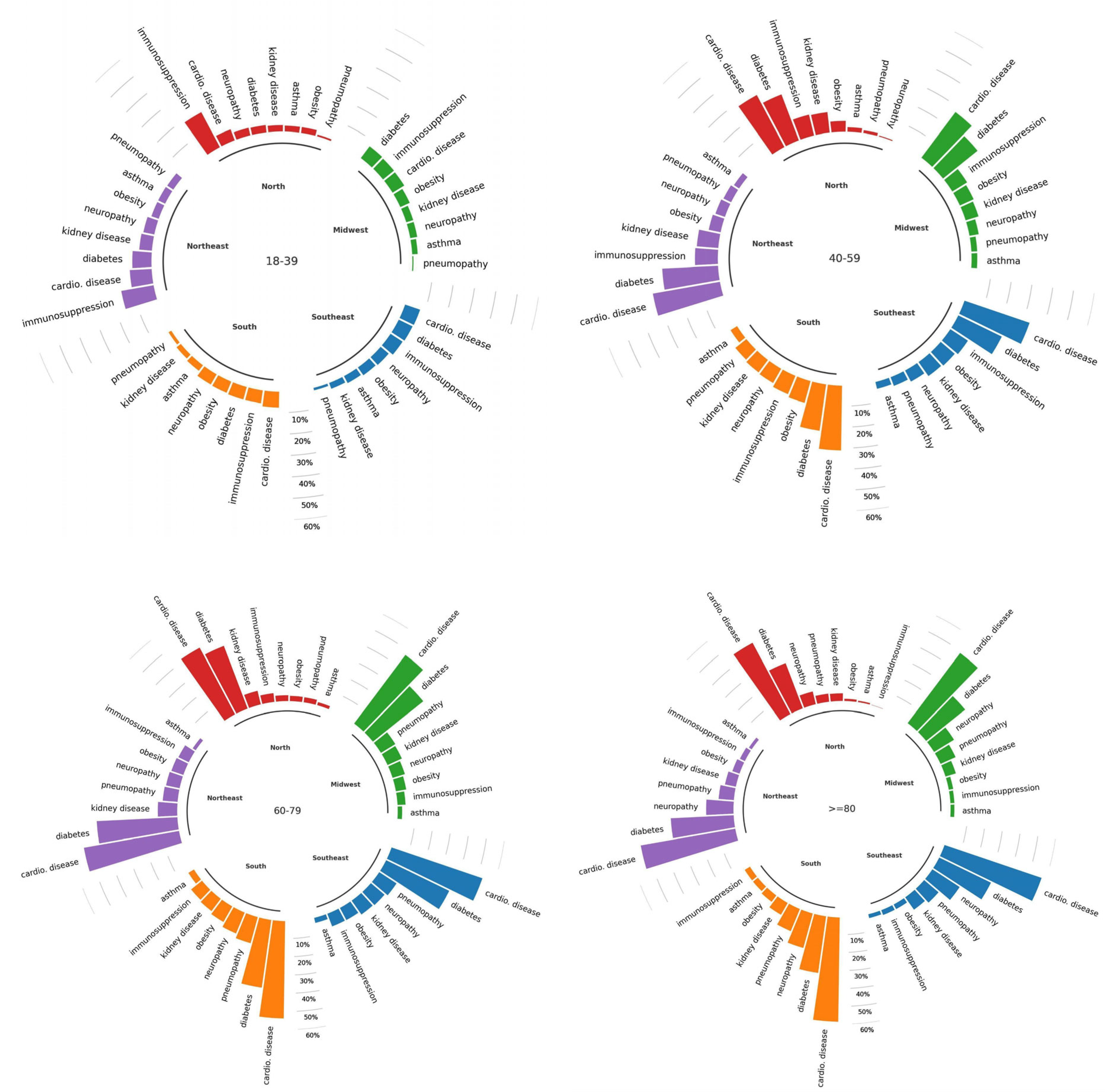
3.1. Description of the Participants
3.2. Analysis of Outcomes and Comorbidities
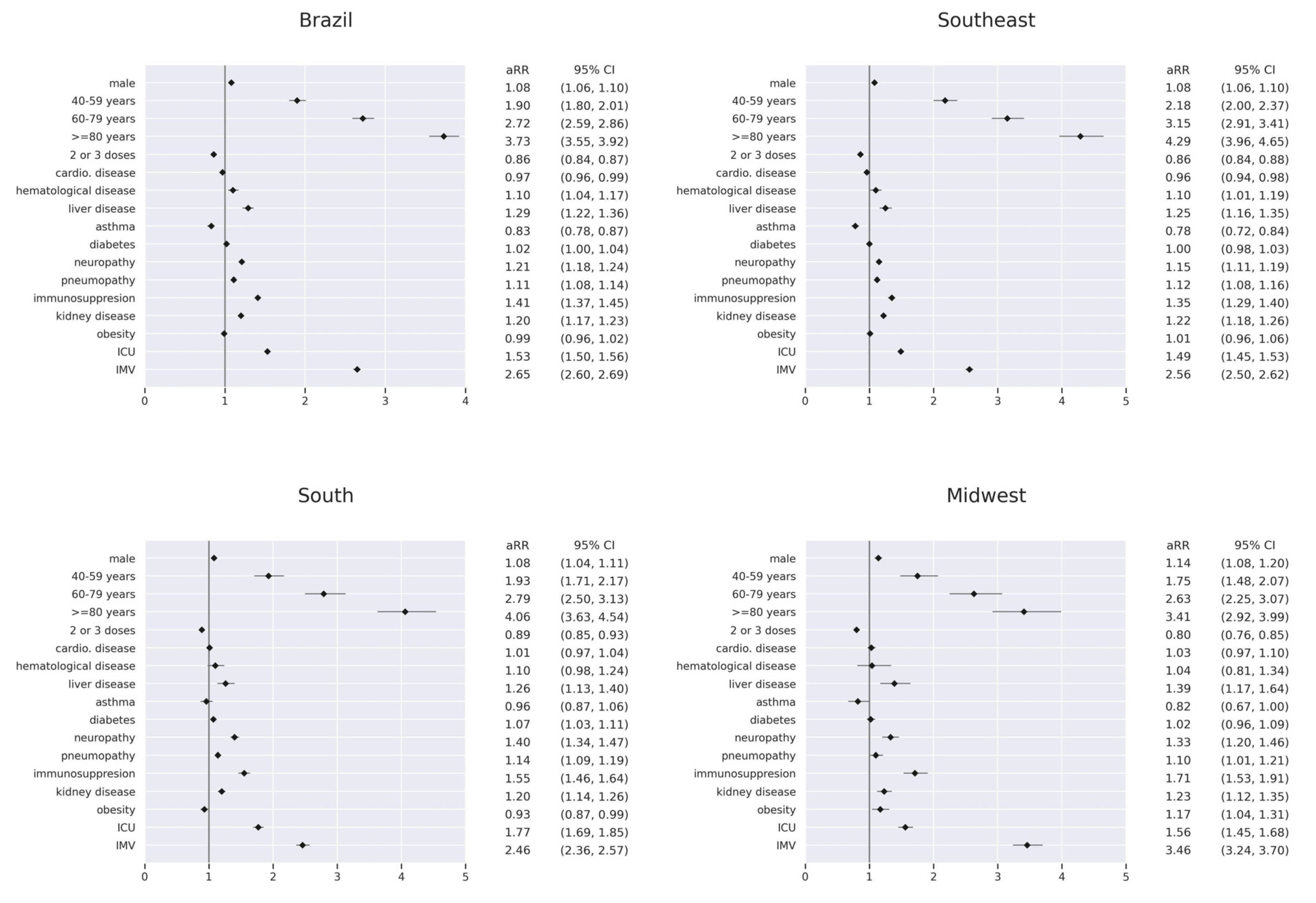
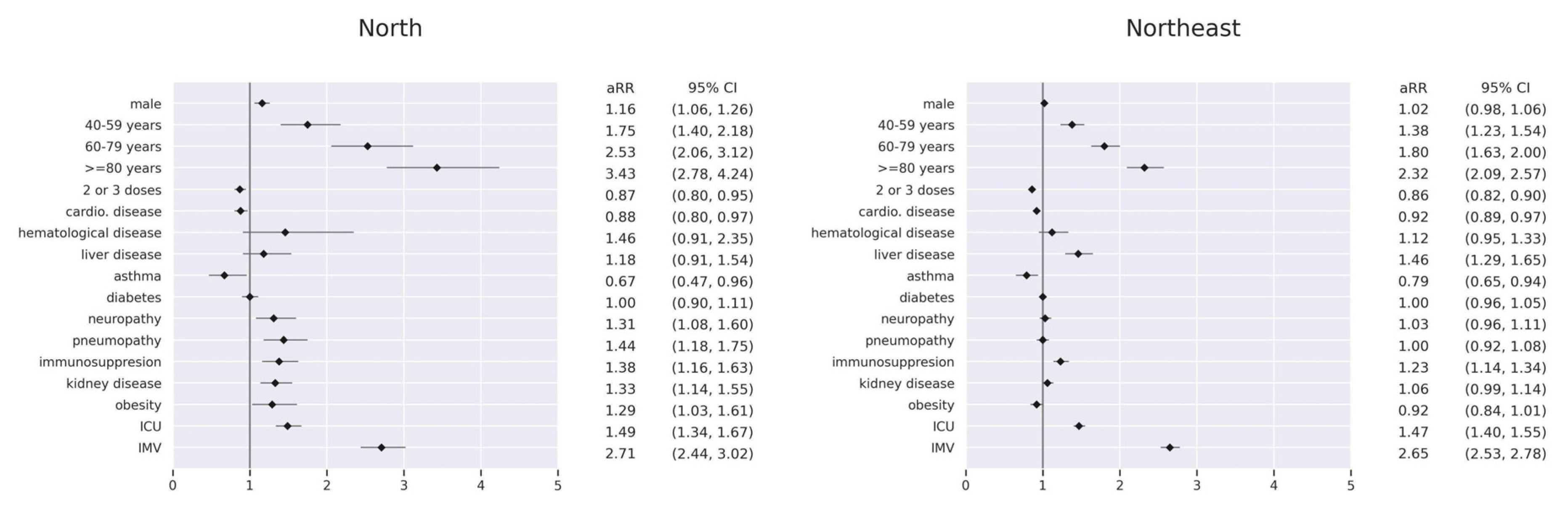
3.3. Risk Factors for In-Hospital Death by Region
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Tracking SARS-CoV-2 Variants. 2022. Available online: www.who.int/en/activities/tracking-SARS-CoV-2-variants (accessed on 6 March 2023).
- Sabino, E.C.; Buss, L.F.; Carvalho, M.P.S.; Prete, C.A., Jr.; Crispim, M.A.E.; Fraiji, N.A.; Pereira, R.H.M.; Parag, K.V.; da Silva Peixoto, P.; Kraemer, M.U.G.; et al. Resurgence of COVID-19 in Manaus, Brazil, despite high seroprevalence. Lancet 2021, 397, 452–455. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Beltran, W.F.; Lam, E.C.; St Denis, K.; Nitido, A.D.; Garcia, Z.H.; Hauser, B.M.; Feldman, J.; Pavlovic, M.N.; Gregory, D.J.; Poznansky, M.C.; et al. Multiple SARS-CoV-2 variants escape neutralization by vaccine-induced humoral immunity. Cell 2021, 184, 2372–2383.e9. [Google Scholar] [CrossRef]
- Cerqueira-Silva, T.; Oliveira, V.d.A.; Paixão, E.S.; Florentino, P.T.V.; Penna, G.O.; Pearce, N.; Werneck, G.L.; Barreto, M.L.; Boaventura, V.S.; Barral-Netto, M. Vaccination plus previous infection: Protection during the omicron wave in Brazil. Lancet Infect. Dis. 2022, 22, 945–946. [Google Scholar] [CrossRef] [PubMed]
- Brasil. Ministério Da Saúde Lança Campanha “Mega Vacinação” Para Reforçar Imunização Dos Brasileiros Contra COVID-19. 2021. Available online: www.gov.br/pt-br/noticias/saude-e-vigilancia-sanitaria/2021/11/governo-federal-lanca-campanha-201cmega-vacinacao201d-para-reforcar-imunizacao-dos-brasileiros-contra-covid-19 (accessed on 6 March 2023).
- Liu, L.; Iketani, S.; Guo, Y.; Chan, J.F.-W.; Wang, M.; Liu, L.; Luo, Y.; Chu, H.; Huang, Y.; Nair, M.S.; et al. Striking antibody evasion manifested by the Omicron variant of SARS-CoV-2. Nature 2022, 602, 676–681. [Google Scholar] [CrossRef] [PubMed]
- Planas, D.; Saunders, N.; Maes, P.; Guivel-Benhassine, F.; Planchais, C.; Buchrieser, J.; Bolland, W.H.; Porrot, F.; Staropoli, I.; Lemoine, F.; et al. Considerable escape of SARS-CoV-2 Omicron to antibody neutralization. Nature 2022, 602, 671–675. [Google Scholar] [CrossRef]
- Campos, G.S.; Giovanetti, M.; de Moraes, L.; da Hora, H.S.; Bandeira, A.C.d.A.; De Alcantara, K.V.O.M.; Sardi, S.I. Genomic monitoring unveils a high prevalence of severe acute respiratory syndrome coronavirus 2 Omicron variant in vaccine breakthrough cases in Bahia, Brazil. Rev. Da Assoc. Médica Bras. 2023, 69, 257–261. [Google Scholar] [CrossRef]
- Fundação Oswaldo Cruz. SARS-CoV-2 Genomic Surveillance in Brazil. Dashboard Genomic Network. 2022. Available online: https://www.genomahcov.fiocruz.br/dashboard-en/ (accessed on 6 March 2023).
- De Souza, F.S.H.; Hojo-Souza, N.S.; da Silva, C.M.; Guidoni, D.L. Second wave of COVID-19 in Brazil: Younger at higher risk. Eur. J. Epidemiol. 2021, 36, 441–443. [Google Scholar] [CrossRef]
- De Souza, F.S.H.; Hojo-Souza, N.S.; de Oliveira, D.C.R.; da Silva, C.M.; Guidoni, D.L. An overview of Brazilian working age adults vulnerability to COVID-19. Sci. Rep. 2022, 12, 2798. [Google Scholar] [CrossRef]
- Birhane, M.; Bressler, S.; Chang, G.; Clark, T.; Dorough, L.; Fischer, M.; Watkins, L.; Goldstein, J.M.; Kugeler, K.; Langley, G.; et al. COVID-19 Vaccine Breakthrough Infections Reported to CDC—United States, January 1–April 30, 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 792–793. [Google Scholar]
- Lipsitch, M.; Krammer, F.; Regev-Yochay, G.; Lustig, Y.; Balicer, R.D. SARS-CoV-2 breakthrough infections in vaccinated individuals: Measurement, causes and impact. Nat. Rev. Immunol. 2021, 22, 57–65. [Google Scholar] [CrossRef]
- Bosch, W.; Cowart, J.B.; Bhakta, S.; Carter, R.E.; Wadei, H.M.; Shah, S.Z.; Sanghavi, D.K.; Pollock, B.D.; Neville, M.R.; Oman, S.P.; et al. Coronavirus Disease 2019 Vaccine-Breakthrough Infections Requiring Hospitalization in Mayo Clinic Florida Through August 2021. Clin. Infect. Dis. 2021, 75, e892–e894. [Google Scholar] [CrossRef] [PubMed]
- De Jesus, M.A.S.; Hojo-Souza, N.S.; Moraes, T.R.; Guidoni, D.L.; de Souza, F.S.H. Profile of Brazilian inpatients with COVID-19 vaccine breakthrough infection and risk factors for unfavorable outcome. Rev. Panam. De Salud Pública 2022, 46, e106. [Google Scholar] [CrossRef] [PubMed]
- Koelle, K.; Martin, M.A.; Antia, R.; Lopman, B.; Dean, N.E. The changing epidemiology of SARS-CoV-2. Science 2022, 375, 1116–1121. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/region/amro/country/br (accessed on 2 September 2023).
- Centers for Disease Control and Prevention. SARS-CoV-2 Variant Classifications and Definitions. Available online: https://www.cdc.gov/coronavirus/2019-ncov/variants/variant-classifications.html (accessed on 1 September 2023).
- Castro, M.C.; Massuda, A.; Almeida, G.; Menezes-Filho, N.A.; Andrade, M.V.; de Souza Noronha, K.V.M.; Rocha, R.; Macinko, J.; Hone, T.; Tasca, R.; et al. Brazil’s unified health system: The first 30 years and prospects for the future. Lancet 2019, 394, 345–356. [Google Scholar] [CrossRef]
- Palamim, C.V.; Marson, F.A. COVID-19—The availability of ICU Beds in Brazil during the onset of pandemic. Ann. Glob. Health 2020, 86, 100. [Google Scholar] [CrossRef]
- De Andrade, C.L.T.; de Pereira, C.C.A.; Martins, M.; Lima, S.M.L.; Portela, M.C. COVID-19 hospitalizations in Brazil’s Unified Health System (SUS). PLoS ONE 2020, 15, e0243126. [Google Scholar] [CrossRef]
- Baqui, P.; Bica, I.; Marra, V.; Ercole, A.; van der Schaar, M. Ethnic and regional variations in hospital mortality from COVID-19 in Brazil: A cross-sectional observational study. Lancet Glob Health 2020, 8, e1018–e1026. [Google Scholar] [CrossRef]
- Liu, Y.; Wang, K.; Yang, L.; He, D. Regional heterogeneity of in-hospital mortality of COVID-19 in Brazil. Infect. Dis. Model. 2022, 7, 364–373. [Google Scholar] [CrossRef]
- Portela, M.C.; Pereira, C.C.D.A.; Lima, S.M.L.; Andrade, C.L.T.D.; Soares, F.R.G.; Martins, M. Nota Técnica. Limites E Possibilidades Dos Municípios Brasileiros Para O Enfrentamento Dos Casos Graves De COVID-19. 2020. Available online: https://portal.fiocruz.br/sites/portal.fiocruz.br/files/documentos/nt_1_portela_et_al_limites_e_possibilidades_dos_municipios_brasileiros_na_covid-19_1.pdf (accessed on 2 September 2023).
- Willett, B.J.; Grove, J.; MacLean, O.A.; Wilkie, C.; De Lorenzo, G.; Furnon, W.; Cantoni, D.; Scott, S.; Logan, N.; Ashraf, S.; et al. SARS-CoV-2 Omicron is an immune escape variant with an altered cell entry pathway. Nat. Microbiol. 2022, 7, 1161–1179. [Google Scholar] [CrossRef]
- Wang, Q.; Guo, Y.; Iketani, S.; Nair, M.S.; Li, Z.; Mohri, H.; Wang, M.; Yu, J.; Bowen, A.D.; Chang, J.Y.; et al. Antibody evasion by SARS-CoV-2 Omicron subvariants BA.2.12.1, BA.4 and BA.5. Nature 2022, 608, 603–608. [Google Scholar] [CrossRef]
- Tan, S.T.; Kwan, A.T.; Rodríguez-Barraquer, I.; Singer, B.J.; Park, H.J.; Lewnard, J.A.; Lo, N.C. Infectiousness of SARS-CoV-2 breakthrough infections and reinfections during the Omicron wave. Nat. Med. 2023, 29, 358–365. [Google Scholar] [CrossRef]
- Feikin, D.R.; Higdon, M.M.; Abu-Raddad, L.J.; Andrews, N.; Araos, R.; Goldberg, Y.; Groome, M.J.; Huppert, A.; O’Brien, K.L.; Smith, P.G.; et al. Duration of effectiveness of vaccines against SARS-CoV-2 infection and COVID-19 disease: Results of a systematic review and meta-regression. Lancet 2022, 399, 924–944. [Google Scholar] [CrossRef]
- Menni, C.; May, A.; Polidori, L.; Louca, P.; Wolf, J.; Capdevila, J.; Hu, C.; Ourselin, S.; Steves, C.J.; Valdes, A.M.; et al. COVID-19 vaccine waning and effectiveness and side-effects of boosters: A prospective community study from the ZOE COVID Study. Lancet Infect. Dis. 2022, 22, 1002–1010. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, H.; Pham-Tran, D.D.; Yeoh, Z.Y.M.; Wang, B.; McMillan, M.; Andraweera, P.H.; Marshall, H.S. A Systematic Review and Meta-Analysis on the Real-World Effectiveness of COVID-19 Vaccines against Infection, Symptomatic and Severe COVID-19 Disease Caused by the Omicron Variant (B.1.1.529). Vaccines 2023, 11, 224. [Google Scholar] [CrossRef] [PubMed]
- Andrews, N.; Stowe, J.; Kirsebom, F.; Toffa, S.; Sachdeva, R.; Gower, C.; Ramsay, M.; Bernal, J.L. Effectiveness of COVID-19 booster vaccines against COVID-19-related symptoms, hospitalization and death in England. Nat. Med. 2022, 28, 831–837. [Google Scholar] [CrossRef] [PubMed]
- Ministério da Saúde; Secretaria de Vigilância em Saúde; Departamento de Imunização e Doenças Transmissíveis. Plano Nacional de Operacionalização da Vacinação Contra a COVID-19. 12. ed.—Brasília: Ministério da Saúde; 2022. Available online: https://www.gov.br/saude/pt-br/coronavirus/publicacoes-tecnicas/guias-e-planos/plano-nacional-de-operacionalizacao-da-vacinacao-contra-covid-19.pdf (accessed on 1 September 2023).
- Guimarães, R.A.; Pinheiro, R.S.; Paula, H.D.; Araújo, L.A.; Gonçalves, I.A.; Pedroso, C.F.; Guilarde, A.O.; Oliveira, G.A.; Batista, K.D. Mortality Risk Factors for Coronavirus Infection in Hospitalized Adults in Brazil: A Retrospective Cohort Study. Int. J. Environ. Res. Public Health 2022, 19, 14074. [Google Scholar] [CrossRef] [PubMed]
- Sardinha, D.M.; Ferreira, A.L.; Guimarães, R.J.; Lima, K.V.; Lima, L.N. Clinical characteristics and outcomes among vaccinated and unvaccinated patients with cardiovascular disease who were hospitalized for COVID-19 in Brazil: Retrospective cohort. Vaccines 2023, 11, 861. [Google Scholar] [CrossRef]
- Zhang, D.; Zhong, J.; Xiong, H.; Li, Y.; Guo, T.; Peng, B.; Fang, C.; Kang, Y.; Tan, J.; Ma, Y. Protective Effect of Inactivated COVID-19 Vaccines against Omicron BA.2 Infection in Guangzhou: A Test-Negative Case-Control Real-World Study. Vaccines 2023, 11, 566. [Google Scholar] [CrossRef]
- Lu, P.J.; Zhou, T.; Santibanez, T.A.; Jain, A.; Black, C.L.; Srivastav, A.; Singleton, J.A. COVID-19 Bivalent Booster Vaccination Coverage and Intent to Receive Booster Vaccination Among Adolescents and Adults—United States, November–December 2022. Morb. Mortal. Wkly. Rep. 2023, 72, 190. [Google Scholar] [CrossRef]
- Johnson, A.G.; Linde, L.; Ali, A.R.; DeSantis, A.; Shi, M.; Adam, C.; Scobie, H.M. COVID-19 incidence and mortality among unvaccinated and vaccinated persons aged ≥ 12 years by receipt of bivalent booster doses and time since vaccination—24 US jurisdictions, October 3, 2021–December 24, 2022. Morb. Mortal. Wkly. Rep. 2023, 72, 145. [Google Scholar] [CrossRef]
- Levin, E.G.; Lustig, Y.; Cohen, C.; Fluss, R.; Indenbaum, V.; Amit, S.; Doolman, R.; Asraf, K.; Mendelson, E.; Ziv, A.; et al. Waning Immune Humoral Response to BNT162b2 COVID-19 Vaccine over 6 Months. N. Engl. J. Med. 2021, 385, e84. [Google Scholar] [CrossRef] [PubMed]
- Colnago, M.; Benvenuto, G.A.; Casaca, W.; Negri, R.G.; Fernandes, E.G.; Cuminato, J.A. Risk Factors Associated with Mortality in Hospitalized Patients with COVID-19 during the Omicron Wave in Brazil. Bioengineering 2022, 9, 584. [Google Scholar] [CrossRef] [PubMed]
- Thaweethai, T.; Jolley, S.E.; Karlson, E.W.; Levitan, E.B.; Levy, B.; McComsey, G.A.; Donohue, S.E. Development of a Definition of Postacute Sequelae of SARS-CoV-2 Infection. JAMA 2023, 329, 1934–1946. [Google Scholar] [CrossRef] [PubMed]


| Age Group | Southeast | South | Midwest | North | Northeast | All |
|---|---|---|---|---|---|---|
| 18–39 years | 5788 (9.11%) | 2785 (10.54%) | 1348 (13.02%) | 539 (16.68%) | 1220 (10.10%) | 11,680 (10.10%) |
| 40–59 years | 10,166 (15.99%) | 4405 (16.67%) | 1997 (19.30%) | 700 (21.66%) | 2061 (17.06%) | 19,329 (16.71%) |
| 60–79 years | 25,223 (39.69%) | 10,967 (41.50%) | 4046 (39.09%) | 1213 (37.54%) | 4641 (38.42%) | 46,090 (39.86%) |
| ≥80 years | 22,374 (35.21%) | 8271 (31.30%) | 2958 (28.58%) | 779 (24.11%) | 4157 (34.41%) | 38,539 (33.33%) |
| All | 63,551 (100%) | 26,428 (100%) | 10,349 (100%) | 3231 (100%) | 12,079 (100%) | 115,638 (100%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Drummond, P.D.; de Salles, D.B.; de Souza, N.S.H.; Oliveira, D.C.R.; Guidoni, D.L.; de Souza, F.S.H. Profile and Outcomes of Hospitalized COVID-19 Patients during the Prevalence of the Omicron Variant According to the Brazilian Regions: A Retrospective Cohort Study from 2022. Vaccines 2023, 11, 1568. https://doi.org/10.3390/vaccines11101568
Drummond PD, de Salles DB, de Souza NSH, Oliveira DCR, Guidoni DL, de Souza FSH. Profile and Outcomes of Hospitalized COVID-19 Patients during the Prevalence of the Omicron Variant According to the Brazilian Regions: A Retrospective Cohort Study from 2022. Vaccines. 2023; 11(10):1568. https://doi.org/10.3390/vaccines11101568
Chicago/Turabian StyleDrummond, Pedro Dutra, Daniel Bortot de Salles, Natália Satchiko Hojo de Souza, Daniela Carine Ramires Oliveira, Daniel Ludovico Guidoni, and Fernanda Sumika Hojo de Souza. 2023. "Profile and Outcomes of Hospitalized COVID-19 Patients during the Prevalence of the Omicron Variant According to the Brazilian Regions: A Retrospective Cohort Study from 2022" Vaccines 11, no. 10: 1568. https://doi.org/10.3390/vaccines11101568
APA StyleDrummond, P. D., de Salles, D. B., de Souza, N. S. H., Oliveira, D. C. R., Guidoni, D. L., & de Souza, F. S. H. (2023). Profile and Outcomes of Hospitalized COVID-19 Patients during the Prevalence of the Omicron Variant According to the Brazilian Regions: A Retrospective Cohort Study from 2022. Vaccines, 11(10), 1568. https://doi.org/10.3390/vaccines11101568







