The Role of Knowledge, Attitude, Confidence, and Sociodemographic Factors in COVID-19 Vaccination Adherence among Adolescents in Indonesia: A Nationwide Survey
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Setting, Design, Participants, and Sampling
2.2. Measures
Translation Process
2.3. Data Collection and Analyses
2.4. Ethical Considerations
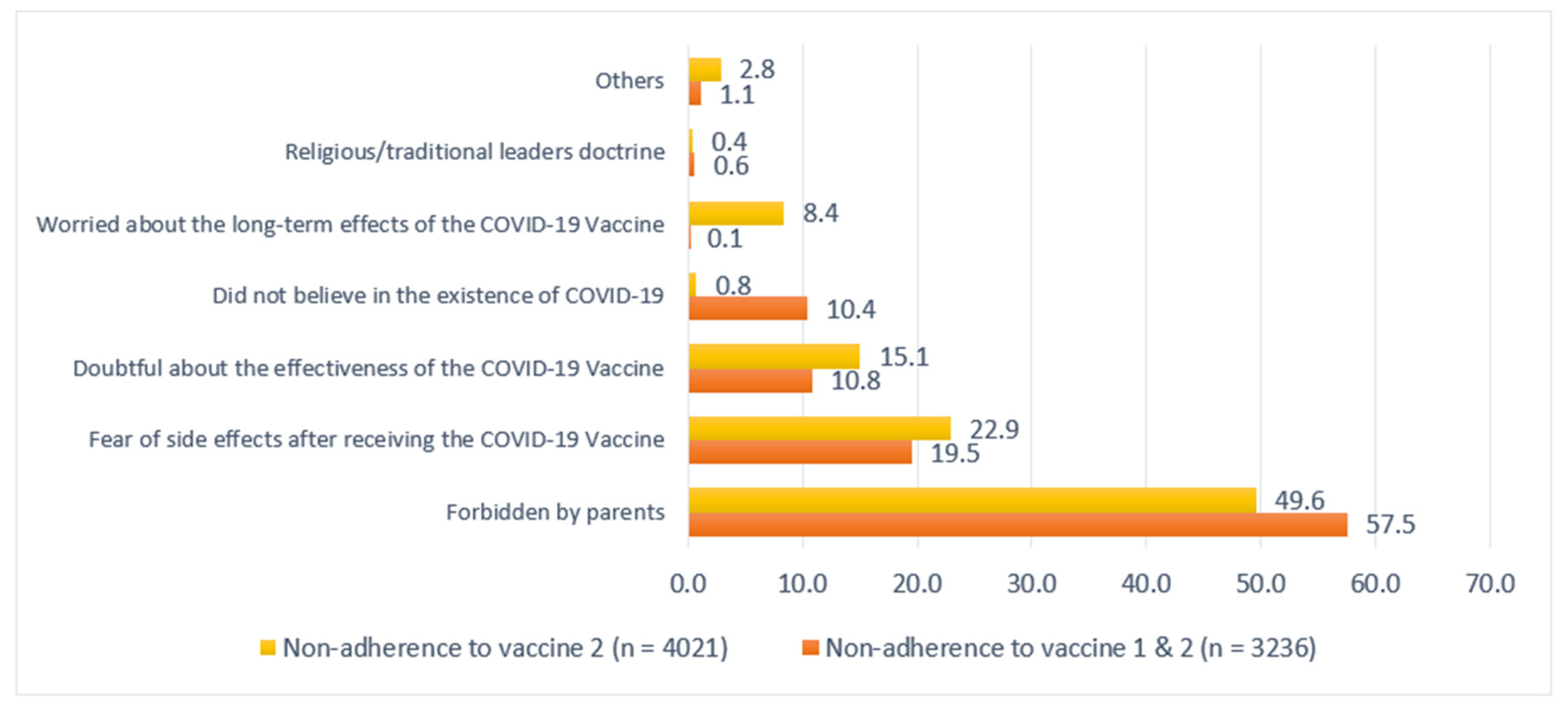
3. Results
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Aschwanden, C. Five Reasons Why COVID Herd Immunity Is Probably Impossible. Nature 2021, 591, 520–522. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. COVID Data Tracker COVID-19 Weekly Cases and Deaths per 100,000 Population by Age, Race/Ethnicity, and Sex. 2022. Available online: https://covid.cdc.gov/covid-data-tracker/#demographicsovertime (accessed on 6 July 2022).
- Afifi, T.O.; Salmon, S.; Taillieu, T.; Stewart-Tufescu, A.; Fortier, J.; Driedger, S.M. Older Adolescents and Young Adults Willingness to Receive the COVID-19 Vaccine: Implications for Informing Public Health Strategies. Vaccine 2021, 39, 3473–3479. [Google Scholar] [CrossRef]
- Delahoy, M.J.; Ujamaa, D.; Whitaker, M.; O’Halloran, A.; Anglin, O.; Burns, E.; Cummings, C.; Holstein, R.; Kambhampati, A.K.; Milucky, J.; et al. Hospitalizations Associated with COVID-19 Among Children and Adolescents–COVID-NET, 14 States, 1 March 2020–14 August 2021. M.M.W.R. Morb. Mortal. Wkly. Rep. 2021, 70, 1255–1260. [Google Scholar] [CrossRef]
- Indonesian Task Force for COVID. Management. Peta Sebaran COVID 2022, 19. Available online: https://covid19.go.id/peta-sebaran (accessed on 6 July 2022).
- Du, Y.; Chen, L.; Shi, Y. Safety, Immunogenicity, and Efficacy of COVID-19 Vaccines in Adolescents, Children, and Infants: A Systematic Review and Meta-analysis. Front. Public Health 2022, 10, 829176. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, N.G.; Moorman, A.C.; Makaretz, A.; Chang, K.T.; Chu, V.T.; Szablewski, C.M.; Yousaf, A.R.; Brown, M.M.; Clyne, A.; DellaGrotta, A.; et al. Adolescent with COVID-19 as the Source of an Outbreak at a 3-Week Family Gathering—Four States, June–July 2020. M.M.W.R. Morb. Mortal. Wkly. Rep. 2020, 69, 1457–1459. [Google Scholar] [CrossRef] [PubMed]
- Harris, R.J.; Hall, J.A.; Zaidi, A.; Andrews, N.J.; Dunbar, J.K.; Dabrera, G. Effect of Vaccination on Household Transmission of SARS-CoV-2 in England. N. Engl. J. Med. 2021, 385, 759–760. [Google Scholar] [CrossRef]
- Singanayagam, A.; Hakki, S.; Dunning, J.; Madon, K.J.; Crone, M.A.; Koycheva, A.; Derqui-Fernandez, N.; Barnett, J.L.; Whitfield, M.G.; Varro, R.; et al. Community Transmission and Viral Load Kinetics of the SARS-CoV-2 Delta (B.1.617.2) Variant in Vaccinated and Unvaccinated Individuals in the UK: A Prospective, Longitudinal, Cohort Study. Lancet Infect. Dis. 2022, 22, 183–195. [Google Scholar] [CrossRef]
- Liu, Y.; Ma, Q.; Liu, H.; Guo, Z. Public Attitudes and Influencing Factors Toward COVID-19 Vaccination for Adolescents/Children: A Scoping Review. Public Health 2022, 205, 169–181. [Google Scholar] [CrossRef]
- Cai, H.; Bai, W.; Liu, S.; Liu, H.; Chen, X.; Qi, H.; Liu, R.; Cheung, T.; Su, Z.; Ng, C.H.; et al. Attitudes Toward COVID-19 Vaccines in Chinese Adolescents. Front. Med. 2021, 8, 691079. [Google Scholar] [CrossRef] [PubMed]
- Wirunpan, M. Knowledge, Attitudes, and Willingness of Adolescents Towards Coronavirus Disease 2019 Vaccine in Bangkok, Thailand. Int. J. Med. Sci. Public Health 2021, 10, 197–204. [Google Scholar] [CrossRef]
- Wong, W.H.S.; Leung, D.; Chua, G.T.; Duque, J.S.R.; Peare, S.; So, H.K.; Chan, S.M.; Kwan, M.Y.W.; Ip, P.; Lau, Y.L. Adolescents’ Attitudes to the COVID-19 Vaccination. Vaccine 2022, 40, 967–969. [Google Scholar] [CrossRef] [PubMed]
- Scherer, A.M.; Gedlinske, A.M.; Parker, A.M.; Gidengil, C.A.; Askelson, N.M.; Petersen, C.A.; Woodworth, K.R.; Lindley, M.C. Acceptability of Adolescent COVID-19 Vaccination Among Adolescents and Parents of Adolescents—United States, April 15–23, 2021. M.M.W.R. Morb. Mortal. Wkly. Rep. 2021, 70, 997–1003. [Google Scholar] [CrossRef] [PubMed]
- Fazel, M.; Puntis, S.; White, S.R.; Townsend, A.; Mansfield, K.L.; Viner, R.; Herring, J.; Pollard, A.J.; Freeman, D. Willingness of Children and Adolescents to Have a COVID-19 Vaccination: Results of a Large Whole Schools Survey in England. eClinicalMedicine 2021, 40, 101144. [Google Scholar] [CrossRef]
- U.N.I.C.E.F. Profil Remaja 2021: Gambaran Umum. U.N.I.C.E.F. 2021, 1–2. Available online: https://www.unicef.org/indonesia/media/9546/file/Profil%20Remaja.pdf (accessed on 6 July 2022).
- Tinsley, H.E.A.; Tinsley, D.J. Uses of Factor Analysis in Counseling Psychology Research. J. Couns. Psychol. 1987, 34, 414–424. [Google Scholar] [CrossRef]
- Ioannou, G.N.; Green, P.; Locke, E.R.; Berry, K. Factors Associated with Early Receipt of COVID-19 Vaccination and Adherence to Second Dose in the Veterans Affairs Healthcare System. PLoS ONE 2021, 16, e0259696. [Google Scholar] [CrossRef] [PubMed]
- Freeman, D.; Loe, B.S.; Chadwick, A.; Vaccari, C.; Waite, F.; Rosebrock, L.; Jenner, L.; Petit, A.; Lewandowsky, S.; Vanderslott, S.; et al. COVID-19 Vaccine Hesitancy in the UK: The Oxford Coronavirus Explanations, Attitudes, and Narratives Survey (Oceans) II. Psychol. Med. 2020, 1–15. [Google Scholar] [CrossRef]
- Mohamed, N.A.; Solehan, H.M.; Mohd Rani, M.D.; Ithnin, M.; Che Isahak, C.I.C. Knowledge, Acceptance and Perception on COVID-19 Vaccine Among Malaysians: A Web-Based Survey. PLoS ONE 2021, 16, e0256110. [Google Scholar] [CrossRef]
- Ministry of Health Republic of Indonesia. Surat Edaran no HK.02.02/I/1727/2021 Tentang Vaksinasi Tahap 3 Bagi Masyarakat Rentan, Masyarakat Umum Lainnya, dan Anak Usia 12–17 Tahun, Ministry of Health Republic of Indonesia. 2021. Available online: https://covid19.go.id/p/regulasi/surat-edaran-no-hk0202i-1727-2021-tentang-vaksinasi-tahap-3-bagi-masyarakat-rentan-serta-masyarakat-umum-lainnya-dan-pelaksanaan-vaksinasi-covid-19-bagi-anak-usia-12-17-tahun (accessed on 11 July 2022).
- Baum, S.G. The Pfizer-BioNTech COVID-19 Vaccine in Adolescents: Balancing Benefits and Risks. Summary and Comments. N. Engl. J. Med. 2021, 1–2. Available online: https://www.jwatch.org/na53931/2021/08/25/pfizer-biontech-covid-19-vaccine-adolescents-balancing (accessed on 6 July 2022).
- Hockenberry, M.; Wilson, D. Wong’s: Nursing Care of Infants and Children, 10th ed.; Elsevier: Amsterdam, The Netherlands, 2015. [Google Scholar]
- Widyastuti, N.N.; Nugraheni, W.J.; Wahyono, T.Y.M.; Yovsyah, Y. Hubungan Status Gizi Terhadap KejadianTuberculosis (TB) Paru Anak Usia 1–5 Tahun Di Indonesia (Analisis Data Riskesdas 2018) = the Association Between Nutritional Status of Children Tuberculosis (TB) Children 1–5 Years in Indonesia (Data Analysis of Riskesdas 2018). Bul. Penelit. Sist. Kesehat. 2021, 24, 89–96. [Google Scholar] [CrossRef]
- Carolina, A.R.; Efendi, D.; Kurniasari, M.D. Determinant Factor of Childhood Basic Immunization Compliance During the COVID-19 Pandemic in Jambi City, Jambi Province, Indonesia. J. Nurs. Pract. 2021, 5, 77–88. [Google Scholar] [CrossRef]
- C.D.C. People with Certain Medical Conditions. U.S. Department of Health & Human Services. 2021. Available online: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html (accessed on 11 July 2022).
- Zahid, H.M.; Alsayb, M.A. Assessing the Knowledge and Attitude Toward COVID-19 Vaccination in Saudi Arabia. Int. J. Environ. Res. Public Health 2021, 18, 8185. [Google Scholar] [CrossRef] [PubMed]
- Harapan, H.; Wagner, A.L.; Yufika, A.; Winardi, W.; Anwar, S.; Gan, A.K.; Setiawan, A.M.; Rajamoorthy, Y.; Sofyan, H.; Mudatsir, M. Acceptance of a COVID-19 Vaccine in Southeast Asia: A Cross-Sectional Study in Indonesia. Front. Public Health 2020, 8, 381. [Google Scholar] [CrossRef] [PubMed]
- Warih, M.P.; Rindarjono, M.G.; Nurhadi, N. The Impact of Parental Education Levels on Digital Skills of Students in Urban Sprawl Impacted Areas. J. Phys. Conf. Ser. 2020, 1469, 012071. [Google Scholar] [CrossRef]
- Sousa, V.D.; Rojjanasrirat, W. Translation, Adaptation and Validation of Instruments or Scales for Use in Cross-Cultural Health Care Research: A Clear and User-Friendly Guideline. J. Eval. Clin. Pract. 2011, 17, 268–274. [Google Scholar] [CrossRef]
- Rias, Y.A.; Rosyad, Y.S.; Chipojola, R.; Wiratama, B.S.; Safitri, C.I.; Weng, S.F.; Yang, C.Y.; Tsai, H.T. Effects of Spirituality, Knowledge, Attitudes, and Practices Toward Anxiety Regarding COVID-19 Among the General Population in Indonesia: A Cross-Sectional Study. J. Clin. Med. 2020, 9, 3798. [Google Scholar] [CrossRef] [PubMed]
- Biddle, N.; Edwards, B.; Gray, M.; Sollis, K. Determinants of COVID-19 Vaccination and Views of Parents About Vaccination of Children in Australia: August 2021 (August); Centre for Social Research & M.E.E.E.E.E.S. (Australian National University): Canberra, Australia, 2021. [Google Scholar] [CrossRef]
- Saelee, R.; Zell, E.; Murthy, B.P.; Castro-Roman, P.; Fast, H.; Meng, L.; Shaw, L.; Gibbs-Scharf, L.; Chorba, T.; Harris, L.Q.; et al. Disparities in COVID-19 Vaccination Coverage Between Urban and Rural Counties—United States, 14 December 2020–31 January 2022. M.M.W.R. Morb. Mortal. Wkly. Rep. 2022, 71, 335–340. [Google Scholar] [CrossRef] [PubMed]
- Wirawan, G.B.S.; Harjana, N.P.A.; Nugrahani, N.W.; Januraga, P.P. Health Beliefs and Socioeconomic Determinants of COVID-19 Booster Vaccine Acceptance: An Indonesian Cross-Sectional Study. Vaccines 2022, 10, 724. [Google Scholar] [CrossRef] [PubMed]
- Hamel, L.; Wu, B.; Brodie, M. The Health Care Views and Experiences of Rural Americans: Findings from the Kaiser Family Foundation/Washington Post Survey of Rural America, (June). Available online: http://files.kff.org/attachment/Report-The-Health-Care-Views-and-Experiences-of-Rural-Americans (accessed on 26 August 2022).
- Arifin, B.; Anas, T. Lessons Learned from COVID-19 Vaccination in Indonesia: Experiences, Challenges, and Opportunities. Hum. Vaccin. Immunother. 2021, 17, 3898–3906. [Google Scholar] [CrossRef] [PubMed]
- Kollamparambil, U.; Oyenubi, A. Behavioural Response to the Covid-19 Pandemic in South Africa. PLoS ONE 2021, 16, e0250269. [Google Scholar] [CrossRef] [PubMed]
- Pogue, K.; Jensen, J.L.; Stancil, C.K.; Ferguson, D.G.; Hughes, S.J.; Mello, E.J.; Burgess, R.; Berges, B.K.; Quaye, A.; Poole, B.D. Influences on Attitudes Regarding Potential COVID-19 Vaccination in the United States. Vaccines 2020, 8, 582. [Google Scholar] [CrossRef]
- Birmingham, W.C.; Macintosh, J.L.B.; Vaughn, A.A.; Graff, T.C. Strength of Belief: Religious Commitment, Knowledge, and HPV Vaccination Adherence. Psychooncology 2019, 28, 1227–1233. [Google Scholar] [CrossRef]
- Rehati, P.; Amaerjiang, N.; Yang, L.; Xiao, H.; Li, M.; Zunong, J.; Wang, L.; Vermund, S.H.; Hu, Y. COVID-19 Vaccine Hesitancy Among Adolescents: Cross-Sectional School Survey in Four Chinese Cities Prior to Vaccine Availability. Vaccines 2022, 10, 452. [Google Scholar] [CrossRef] [PubMed]
- Belingheri, M.; Ausili, D.; Paladino, M.E.; Luciani, M.; Di Mauro, S.; Riva, M.A. Attitudes Towards COVID-19 Vaccine and Reasons for Adherence or Not Among Nursing Students. J. Prof. Nurs. 2021, 37, 923–927. [Google Scholar] [CrossRef] [PubMed]
- Cvjetkovic, S.J.; Jeremic, V.L.; Tiosavljevic, D.V. Knowledge and Attitudes Toward Vaccination: A Survey of Serbian Students. J. Infect. Public Health 2017, 10, 649–656. [Google Scholar] [CrossRef] [PubMed]
- Paul, E.; Steptoe, A.; Fancourt, D. Attitudes Towards Vaccines and Intention to Vaccinate Against COVID-19: Implications for Public Health Communications. Lancet Reg. Health Eur. 2021, 1, 100012. [Google Scholar] [CrossRef] [PubMed]
- O’Leary, S.T.; Middleman, A.B.; Rockwell, P.G. Improving Vaccination Coverage in Children and Adolescents: The Role of Professional Societies. Acad. Pediatr. 2021, 21, S5–S6. [Google Scholar] [CrossRef]
- The Ministry of Health; NITAG; UNICEF; WHO. COVID-19 Vaccine Acceptance Survey in Indonesia 2020. Available online: https://covid19.go.id/storage/app/media/Hasil%20Kajian/2020/November/vaccine-acceptance-survey-en-12-11-2020final.pdf (accessed on 21 February 2022).
- Olick, R.S.; Yang, Y.T.; Shaw, J. Adolescent Consent to COVID-19 Vaccination: The Need for Law Reform. Public Health Rep. 2022, 137, 163–167. [Google Scholar] [CrossRef] [PubMed]
- Middleman, A.B.; Klein, J.; Quinn, J. Vaccine Hesitancy in the Time of COVID-19: Attitudes and Intentions of Teens and Parents Regarding the covid-19 Vaccine. Vaccines 2021, 10, 4. [Google Scholar] [CrossRef]
- Bord, S.; Satran, C.; Schor, A. The Mediating Role of the Perceived COVID-19 Vaccine Benefits: Examining Israeli Parents’ Perceptions Regarding Their Adolescents’ Vaccination. Vaccines 2022, 10, 917. [Google Scholar] [CrossRef] [PubMed]
- Herman, R.; McNutt, L.A.; Mehta, M.; Salmon, D.A.; Bednarczyk, R.A.; Shaw, J. Vaccination Perspectives Among Adolescents and Their Desired Role in the Decision-Making Process. Hum. Vaccin. Immunother. 2019, 15, 1752–1759. [Google Scholar] [CrossRef] [PubMed]
- Abubakar, A.; Van de Vijver, F.J.R.; Suryani, A.O.; Handayani, P.; Pandia, W.S. Perceptions of Parenting Styles and Their Associations with Mental Health and Life Satisfaction Among Urban Indonesian Adolescents. J. Child Fam. Stud. 2015, 24, 2680–2692. [Google Scholar] [CrossRef]
- Magnis-Suseno, F. Etika Jawa: Sebuah Analisa Falsafi Tentang Kebijaksanaan Hidup Jawa [Javanese Ethics: A Philosophical Analysis of Javanese Wisdom]; Gramedia Pustaka Utama: Jakarta, Indonesia, 1991. [Google Scholar]
- Ward, M.K.; Meade, A.W.; Allred, C.M.; Pappalardo, G.; Stoughton, J.W. Careless Response and Attrition as Sources of Bias in Online Survey Assessments of Personality Traits and Performance. Comput. Hum. Behav. 2017, 76, 417–430. [Google Scholar] [CrossRef]

| Variable | n | % |
|---|---|---|
| Vaccination Willingness | 2549 | 34.9 |
| Unwilling | 864 | 11.8 |
| Doubtful | 3886 | 53.3 |
| Ready | ||
| COVID-19 Vaccination Adherence | 3278 | 44.9 |
| Yes | 4021 | 55.1 |
| No | ||
| Island | ||
| Java | 1474 | 20.2 |
| Sumatra | 179 | 2.4 |
| Sulawesi | 863 | 11.8 |
| Borneo | 114 | 1.6 |
| Bali/East and West Nusa Tenggara | 56 | 0.8 |
| Maluku and Papua | 4613 | 63.2 |
| Age | ||
| Early adolescent (12–14 years) | 2014 | 27.6 |
| Middle adolescent (15–17 years) | 5285 | 72.4 |
| Sex | ||
| Male | 2702 | 37 |
| Female | 4597 | 63 |
| Residential Area | 4391 | 60.2 |
| Urban | 2908 | 39.8 |
| Rural | ||
| Distance from House to COVID-19 Vaccination Site | 3680 | 50.4 |
| <4 km | 3619 | 49.6 |
| >4 km | ||
| Housing Status | 5514 | 75.5 |
| Private housing | 1785 | 24.5 |
| Rented housing | ||
| Health Status | 5559 | 76.2 |
| Good | 1629 | 22.3 |
| Fairly good | 111 | 1.5 |
| Poor | ||
| COVID-19 Status | 1653 | 22.6 |
| Prior COVID-19 infection | 5646 | 77.4 |
| No prior COVID-19 infection | ||
| Chronic Disease Status | ||
| Present | 323 | 4.4 |
| Absent | 6976 | 95.6 |
| Congenital Disease Status | 339 | 4.6 |
| Present | 6960 | 95.4 |
| Absent | ||
| COVID-19 Vaccine Information Resources | 5300 | 72.6 |
| Electronic | 1999 | 27.4 |
| Non-electronic | ||
| Parents’ Education Level | 634 | 8.7 |
| Elementary School | 1262 | 17.3 |
| Junior High School | 3110 | 42.6 |
| Senior High School | 2293 | 31.4 |
| College | ||
| Household Income | 6751 | 92.5 |
| <IDR 5,100,000 | 548 | 7.5 |
| ≥5,100,000 | ||
| Financial Problems (During the COVID-19 Pandemic) | 7299 | 100 |
| Yes | 0 | 0 |
| No | ||
| History of Family Members or Friends Infected with COVID-19 | 2013 | 27.6 |
| Yes | 5286 | 72.4 |
| No | ||
| Parents’ Employment Status | 6087 | 83.4 |
| Employed | 1212 | 16.6 |
| Not employed | ||
| Adolescents’ Knowledge Level of COVID-19 Vaccine | 3712 | 50.9 |
| High | 3587 | 49.1 |
| Low | ||
| Attitude Towards COVID-19 Vaccine | 3986 | 54.6 |
| Positive | 3313 | 45.4 |
| Negative | ||
| Confidence in COVID-19 Vaccine | 3615 | 49.5 |
| High | 3684 | 50.5 |
| Low | ||
| Total | 7299 | 100 |
| Variables | Adherence | χ2 | ||||
|---|---|---|---|---|---|---|
| Yes | No | p-Value | ||||
| n | % | n | % | |||
| Willing to Get Vaccinated | 2261.324 *** | 0 | ||||
| Unwilling | 198 | 7.8 | 2351 | 92.2 | ||
| Doubtful | 444 | 51.4 | 420 | 48.6 | ||
| Ready | 2636 | 67.8 | 1250 | 32.2 | ||
| Island | 1681.159 *** | 0 | ||||
| Java | 1267 | 86 | 207 | 14 | ||
| Sumatra | 137 | 76.5 | 42 | 23.5 | ||
| Sulawesi | 381 | 44.1 | 482 | 55.9 | ||
| Borneo | 99 | 86.8 | 15 | 13.2 | ||
| Bali/East and West Nusa Tenggara | 53 | 94.6 | 3 | 5.4 | ||
| Maluku and Papua | 1341 | 29.1 | 3272 | 70.9 | ||
| Age | 462.499 *** | 0 | ||||
| Early adolescent (12–14 years) | 496 | 24.6 | 1518 | 75.4 | ||
| Middle adolescent (15–17 years) | 2782 | 52.6 | 2503 | 47.4 | ||
| Sex | 159.911 *** | 0 | ||||
| Male | 954 | 35.3 | 1748 | 64.7 | ||
| Female | 2324 | 50.6 | 2273 | 49.4 | ||
| Residential Area | 671.199 *** | 0 | ||||
| Urban | 2511 | 57.2 | 1880 | 42.8 | ||
| Rural | 767 | 26.4 | 2141 | 73.6 | ||
| Distance From House to COVID-19 Vaccination Site | 37.611 *** | 0 | ||||
| <4 km | ||||||
| >4 km | 1783 | 48.5 | 1897 | 51.5 | ||
| 1495 | 41.3 | 2124 | 58.7 | |||
| Housing Status | 25.176 *** | 0 | ||||
| Private housing | 2568 | 46.6 | 2946 | 53.4 | ||
| Rented housing | 710 | 39.8 | 1075 | 60.2 | ||
| Health Status | 53.036 *** | 0 | ||||
| Good | 2595 | 46.7 | 2964 | 53.3 | ||
| Fairly good | 664 | 40.8 | 965 | 59.2 | ||
| Poor | 19 | 17.1 | 92 | 82.9 | ||
| COVID-19 Status | 320.934 *** | 0 | ||||
| Prior COVID-19 infection | 1061 | 64.2 | 592 | 35.8 | ||
| No prior COVID-19 infection | 2217 | 39.3 | 3429 | 60.7 | ||
| Chronic Disease Status | 11.736 ** | 0.001 | ||||
| Yes | 175 | 54.2 | 148 | 45.8 | ||
| No | 3103 | 44.5 | 3873 | 55.5 | ||
| Congenital Disease Status | 54.061 *** | 0 | ||||
| Yes | ||||||
| No | 218 | 64.3 | 121 | 35.7 | ||
| 3060 | 44 | 3900 | 56 | |||
| COVID-19 Vaccine Information Resources | 429.541 *** | 0 | ||||
| Electronic | ||||||
| Non-electronic | 2773 | 52.3 | 2527 | 47.7 | ||
| 505 | 25.3 | 1494 | 74.7 | |||
| Parents’ Education Level | 514.483 *** | 0 | ||||
| Elementary School | 206 | 32.5 | 428 | 67.5 | ||
| Junior High School | 294 | 23.3 | 968 | 76.7 | ||
| Senior High School | 1382 | 44.4 | 1728 | 55.6 | ||
| University | 1396 | 60.9 | 897 | 39.1 | ||
| Household Income | 196.290 *** | 0 | ||||
| <IDR 5,100,000 | 2875 | 42.6 | 3876 | 57.4 | ||
| ≥IDR 5,100,000 | 403 | 73.5 | 145 | 26.5 | ||
| History of Family Members or Friends Infected with COVID-19 | 971.529 *** | 0 | ||||
| Yes | ||||||
| No | 1496 | 74.3 | 517 | 25.7 | ||
| 1782 | 33.7 | 3504 | 66.3 | |||
| Parents’ Employment Status | 201.209 *** | 0 | ||||
| Employed | 2958 | 48.6 | 3129 | 51.4 | ||
| Not employed | 320 | 26.4 | 892 | 73.6 | ||
| Adolescents’ Knowledge Level of COVID-19 Vaccine | 2965.669 *** | 0 | ||||
| High | 2824 | 76.1 | 888 | 23.9 | ||
| Low | 454 | 12.7 | 3133 | 87.3 | ||
| Attitude Towards COVID-19 Vaccine | 3562.956 *** | 0 | ||||
| Positive | 3053 | 76.6 | 933 | 23.4 | ||
| Negative | 225 | 6.8 | 3088 | 93.2 | ||
| Confidence in COVID-19 Vaccine | 3066.187 *** | 0 | ||||
| High | 2800 | 77.5 | 815 | 22.5 | ||
| Low | 478 | 13 | 3206 | 87 | ||
| Variables | AOR | p-Value | 95% CI | |
|---|---|---|---|---|
| Lower | Upper | |||
| Willing to Get Vaccinated. | ||||
| Unwilling | 0.159 *** | 0 | 0.13 | 0.195 |
| Doubtful | 0.709 ** | 0.001 | 0.58 | 0.866 |
| Ready | Ref | |||
| Island | ||||
| Java | 1.994 *** | 0 | 1.6 | 2.485 |
| Sumatra | 1.571 | 0.066 | 0.97 | 2.545 |
| Sulawesi | 1.077 | 0.525 | 0.856 | 1.356 |
| Borneo | 1.284 | 0.419 | 0.7 | 2.355 |
| Bali/East and West Nusa Tenggara | 5.168 ** | 0.009 | 1.52 | 17.569 |
| Maluku and Papua | Ref | |||
| Age | ||||
| Early adolescent (12–14 years) | 0.498 *** | 0 | 0.417 | 0.595 |
| Middle adolescent (15–17 years) | Ref | |||
| Sex | ||||
| Male | 0.997 | 0.972 | 0.849 | 1.171 |
| Female | Ref | |||
| Residential Area | ||||
| Urban | 2.007 *** | 0 | 1.701 | 2.368 |
| Rural | Ref | |||
| Distance from House to COVID-19 Vaccination Site | ||||
| <4 km | ||||
| >4 km | 0.974 | 0.729 | 0.839 | 1.131 |
| Ref | ||||
| Housing Status | ||||
| Private housing | 0.555 *** | 0 | 0.46 | 0.67 |
| Rented housing | Ref | |||
| Health Status | ||||
| Good | 3.273 ** | 0.001 | 1.651 | 6.488 |
| Pretty good | 2.030 * | 0.045 | 1.016 | 4.056 |
| Poor | Ref | |||
| COVID-19 Status | ||||
| Prior COVID-19 infection | 0.985 | 0.877 | 0.812 | 1.194 |
| No prior COVID-19 infection | Ref | |||
| Chronic Disease Status | ||||
| Yes | 0.849 | 0.356 | 0.601 | 1.201 |
| No | Ref | |||
| Congenital Disease Status | ||||
| Yes | 1.348 | 0.101 | 0.943 | 1.926 |
| No | Ref | |||
| COVID-19 Vaccine Information Resources | ||||
| Electronic | ||||
| Non-electronic | 0.918 | 0.369 | 0.763 | 1.106 |
| Ref | ||||
| Parents’ Education Level | ||||
| Elementary School | 0.857 | 0.311 | 0.635 | 1.155 |
| Junior High School | 0.396 *** | 0 | 0.312 | 0.502 |
| Senior High School | 0.796 * | 0.011 | 0.667 | 0.949 |
| University | Ref | |||
| Household Income | ||||
| <IDR 5100000 | 0.722 * | 0.036 | 0.532 | 0.979 |
| ≥IDR 5100000 | Ref | |||
| History of Family Members or Friends Infected with COVID-19 | ||||
| Yes | ||||
| No | 1.345 ** | 0.002 | 1.116 | 1.622 |
| Ref | ||||
| Parents’ Employment Status | ||||
| Employed | 1.287 * | 0.02 | 1.04 | 1.592 |
| Not employed | Ref | |||
| Adolescents’ Knowledge Level of COVID-19 Vaccine | ||||
| High | 1.962 *** | 0 | 1.568 | 2.455 |
| Low | Ref | |||
| Attitude Towards COVID-19 Vaccine | ||||
| Positive | 7.072 *** | 0 | 5.652 | 8.849 |
| Negative | Ref | |||
| Confidence in COVID-1 Vaccine | ||||
| High | 1.872 *** | 0 | 1.495 | 2.343 |
| Low | Ref | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Efendi, D.; Rifani, S.R.; Milanti, A.; Efendi, F.; Wong, C.L.; Rustina, Y.; Wanda, D.; Sari, D.; Fabanjo, I.J.; De Fretes, E.D.; et al. The Role of Knowledge, Attitude, Confidence, and Sociodemographic Factors in COVID-19 Vaccination Adherence among Adolescents in Indonesia: A Nationwide Survey. Vaccines 2022, 10, 1489. https://doi.org/10.3390/vaccines10091489
Efendi D, Rifani SR, Milanti A, Efendi F, Wong CL, Rustina Y, Wanda D, Sari D, Fabanjo IJ, De Fretes ED, et al. The Role of Knowledge, Attitude, Confidence, and Sociodemographic Factors in COVID-19 Vaccination Adherence among Adolescents in Indonesia: A Nationwide Survey. Vaccines. 2022; 10(9):1489. https://doi.org/10.3390/vaccines10091489
Chicago/Turabian StyleEfendi, Defi, Sabira Ridha Rifani, Ariesta Milanti, Ferry Efendi, Cho Lee Wong, Yeni Rustina, Dessie Wanda, Dian Sari, Ivonne Junita Fabanjo, Elzina Dina De Fretes, and et al. 2022. "The Role of Knowledge, Attitude, Confidence, and Sociodemographic Factors in COVID-19 Vaccination Adherence among Adolescents in Indonesia: A Nationwide Survey" Vaccines 10, no. 9: 1489. https://doi.org/10.3390/vaccines10091489
APA StyleEfendi, D., Rifani, S. R., Milanti, A., Efendi, F., Wong, C. L., Rustina, Y., Wanda, D., Sari, D., Fabanjo, I. J., De Fretes, E. D., Mohamad, R. W., Sawasemariay, O., Faidiban, R. H., Nur, Q., Tiwery, I. B., Huda, M. H., Mobalen, O., & Nuraidah. (2022). The Role of Knowledge, Attitude, Confidence, and Sociodemographic Factors in COVID-19 Vaccination Adherence among Adolescents in Indonesia: A Nationwide Survey. Vaccines, 10(9), 1489. https://doi.org/10.3390/vaccines10091489







