The Role of Psychological Factors and Vaccine Conspiracy Beliefs in Influenza Vaccine Hesitancy and Uptake among Jordanian Healthcare Workers during the COVID-19 Pandemic
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Survey Instrument
2.3. Main Study Measures
2.4. Statistical Analysis
3. Results
3.1. General Features of the Study Sample
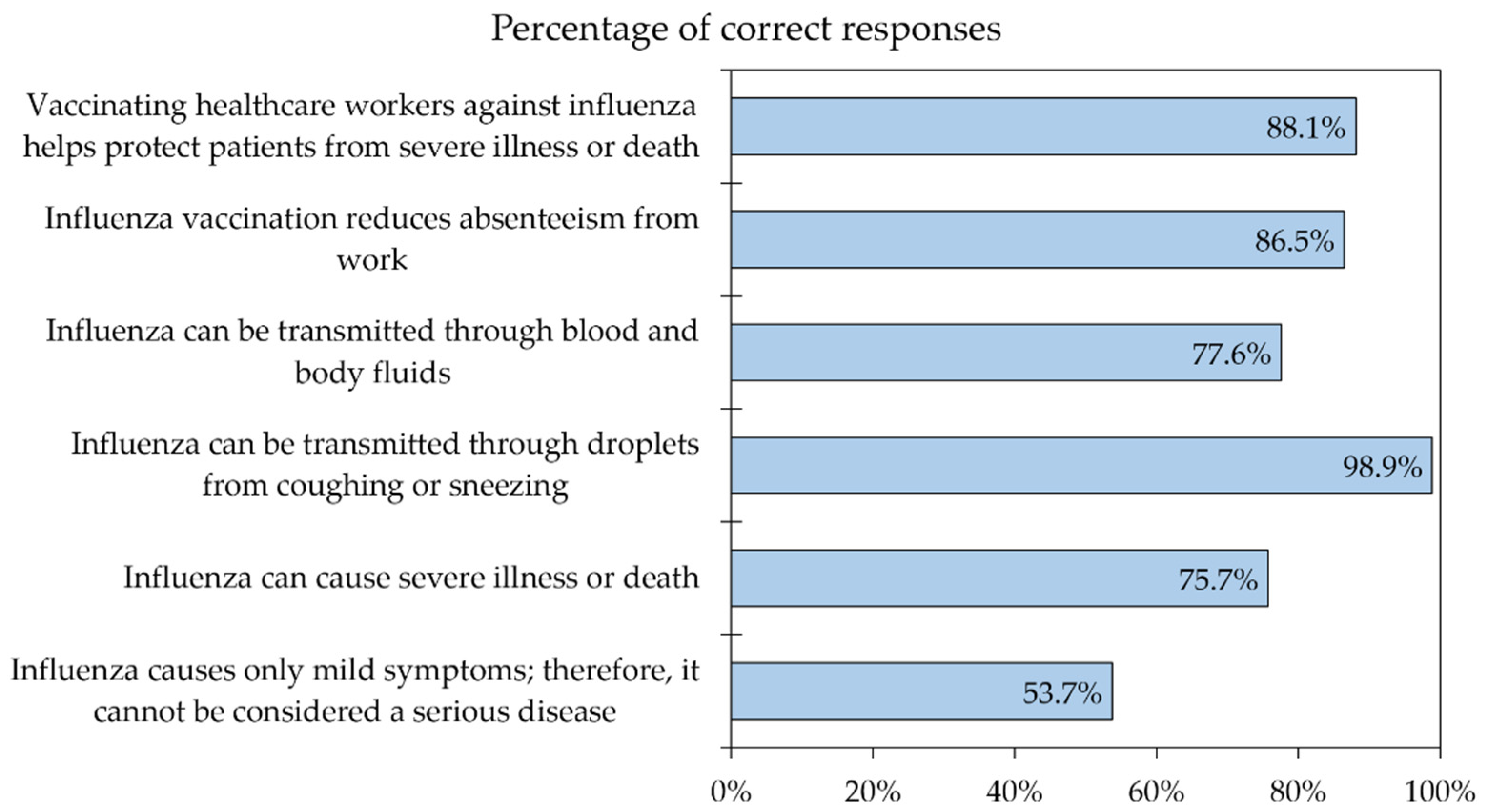
3.2. Knowledge of Influenza and Attitude toward Its Vaccination among the Study Respondents
3.3. About Two-Thirds of the Study Sample Reported Influenza Vaccine Uptake in the Last Season
3.4. Physicians Had the Highest Rate of Vaccine Acceptance, and Nurses Had the Lowest Rate of Willingness to Pay for the Vaccine
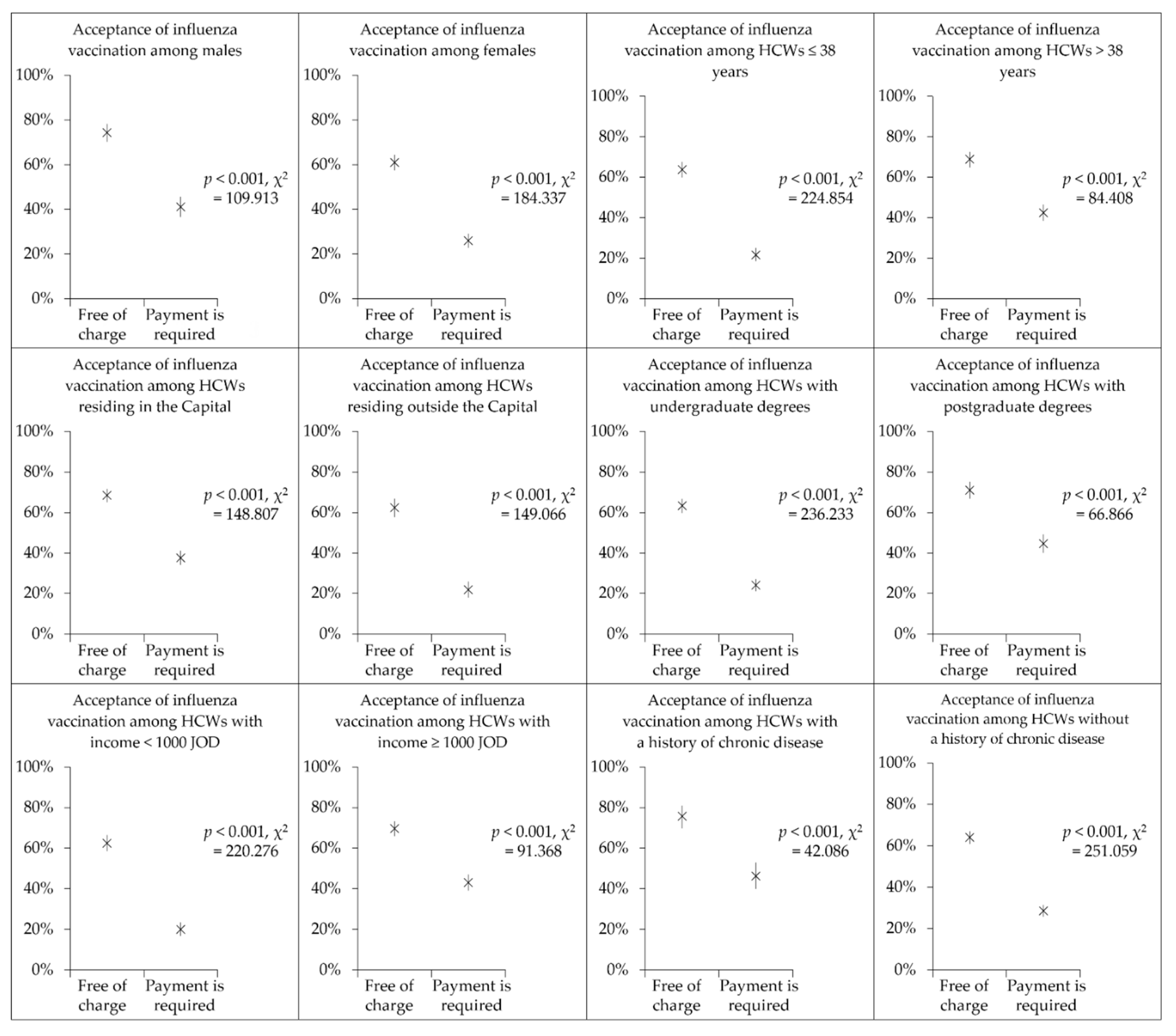
3.5. Influenza Vaccine Acceptance Drops Significantly if Payment Is Required
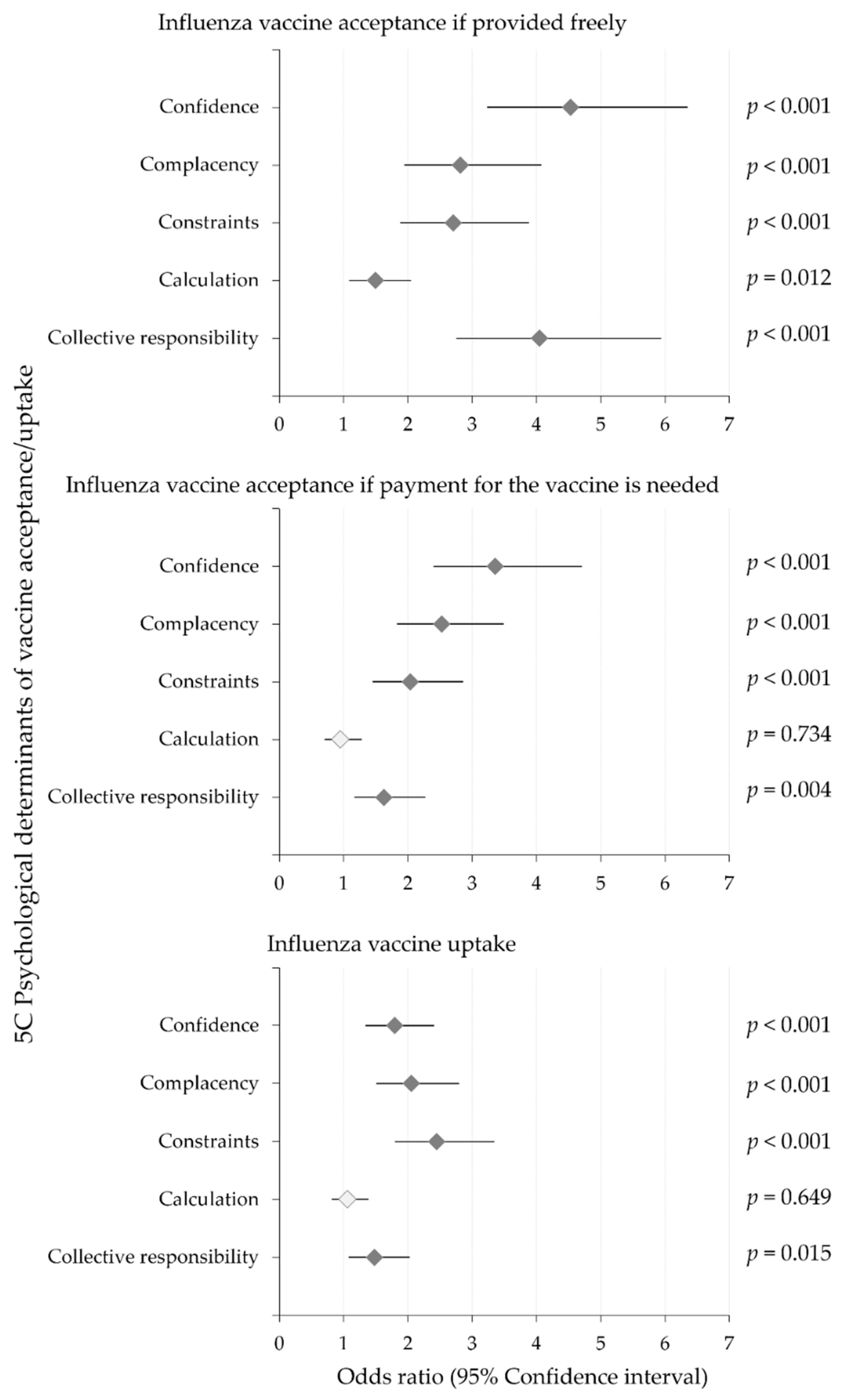
3.6. The 5C Psychological Determinanats Were Associated with Influenza Vaccine Acceptance if Provided Freely
3.7. Confidence, Complacency, Constraints and Collective Responsibility Were Correlated with Willingness to Pay for Influenza Vaccination
3.8. Confidence, Complacency, Constraints, Collective Responsibility and Embrace of Vaccine Conspiracy Beliefs Were Correlated with Influenza Vaccine Uptake
4. Discussion
Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| 5C | Confidence, complacency, constraints, calculation and collective responsibility |
| 7C | Confidence, complacency, constraints, calculation, collective responsibility, conspiracy beliefs and compliance |
| CI | Confidence interval |
| CL | Confidence level |
| COVID-19 | Coronavirus disease 2019 |
| HCW | Healthcare worker |
| IQR | Interquartile range |
| JOD | Jordanian dinar |
| K–W | Kruskal–Wallis test |
| MENA | Middle East and North Africa |
| MSAR | Medical secretaries, administrators and receptionists |
| M–W | Mann–Whitney U test |
| NPI | Non-pharmaceutical intervention |
| OR | Odds ratio |
| P | Proportion |
| VCBS | Vaccine conspiracy beliefs scale |
| WHO | World Health Organization |
| χ2 | Chi-squared test |
References
- Taubenberger, J.K.; Morens, D.M. Influenza: The once and future pandemic. Public Health Rep. 2010, 125, 16–26. [Google Scholar] [CrossRef] [PubMed]
- Troeger, C.E.; Blacker, B.F.; Khalil, I.A.; Zimsen, S.R.M.; Albertson, S.B.; Abate, D.; Abdela, J.; Adhikari, T.B.; Aghayan, S.A.; Agrawal, S.; et al. Mortality, morbidity, and hospitalisations due to influenza lower respiratory tract infections, 2017: An analysis for the Global Burden of Disease Study 2017. Lancet Respir. Med. 2019, 7, 69–89. [Google Scholar] [CrossRef]
- Iuliano, A.D.; Roguski, K.M.; Chang, H.H.; Muscatello, D.J.; Palekar, R.; Tempia, S.; Cohen, C.; Gran, J.M.; Schanzer, D.; Cowling, B.J.; et al. Estimates of global seasonal influenza-associated respiratory mortality: A modelling study. Lancet 2018, 391, 1285–1300. [Google Scholar] [CrossRef]
- Huang, Q.S.; Wood, T.; Jelley, L.; Jennings, T.; Jefferies, S.; Daniells, K.; Nesdale, A.; Dowell, T.; Turner, N.; Campbell-Stokes, P.; et al. Impact of the COVID-19 nonpharmaceutical interventions on influenza and other respiratory viral infections in New Zealand. Nat. Commun. 2021, 12, 1001. [Google Scholar] [CrossRef] [PubMed]
- Piret, J.; Boivin, G. Viral Interference between Respiratory Viruses. Emerg. Infect. Dis. 2022, 28, 273–281. [Google Scholar] [CrossRef]
- Dhanasekaran, V.; Sullivan, S.; Edwards, K.M.; Xie, R.; Khvorov, A.; Valkenburg, S.A.; Cowling, B.J.; Barr, I.G. Human seasonal influenza under COVID-19 and the potential consequences of influenza lineage elimination. Nat. Commun. 2022, 13, 1721. [Google Scholar] [CrossRef]
- Bellizzi, S.; Panu Napodano, C.M.; Pinto, S.; Pichierri, G. COVID-19 and seasonal influenza: The potential 2021–2022 “Twindemic”. Vaccine 2022, 40, 3286–3287. [Google Scholar] [CrossRef]
- Harrington, W.N.; Kackos, C.M.; Webby, R.J. The evolution and future of influenza pandemic preparedness. Exp. Mol. Med. 2021, 53, 737–749. [Google Scholar] [CrossRef]
- Alvarez-Munoz, S.; Upegui-Porras, N.; Gomez, A.P.; Ramirez-Nieto, G. Key Factors That Enable the Pandemic Potential of RNA Viruses and Inter-Species Transmission: A Systematic Review. Viruses 2021, 13, 537. [Google Scholar] [CrossRef]
- Shao, W.; Li, X.; Goraya, M.U.; Wang, S.; Chen, J.L. Evolution of Influenza A Virus by Mutation and Re-Assortment. Int. J. Mol. Sci. 2017, 18, 1650. [Google Scholar] [CrossRef]
- Martini, M.; Gazzaniga, V.; Bragazzi, N.L.; Barberis, I. The Spanish Influenza Pandemic: A lesson from history 100 years after 1918. J. Prev. Med. Hyg. 2019, 60, E64–E67. [Google Scholar] [CrossRef] [PubMed]
- Short, K.R.; Kedzierska, K.; van de Sandt, C.E. Back to the Future: Lessons Learned From the 1918 Influenza Pandemic. Front. Cell. Infect. Microbiol. 2018, 8, 343. [Google Scholar] [CrossRef]
- Piroth, L.; Cottenet, J.; Mariet, A.-S.; Bonniaud, P.; Blot, M.; Tubert-Bitter, P.; Quantin, C. Comparison of the characteristics, morbidity, and mortality of COVID-19 and seasonal influenza: A nationwide, population-based retrospective cohort study. Lancet Respir. Med. 2021, 9, 251–259. [Google Scholar] [CrossRef]
- Buchy, P.; Badur, S. Who and when to vaccinate against influenza. Int. J. Infect. Dis. 2020, 93, 375–387. [Google Scholar] [CrossRef]
- Kuster, S.P.; Shah, P.S.; Coleman, B.L.; Lam, P.-P.; Tong, A.; Wormsbecker, A.; McGeer, A. Incidence of Influenza in Healthy Adults and Healthcare Workers: A Systematic Review and Meta-Analysis. PLoS ONE 2011, 6, e26239. [Google Scholar] [CrossRef] [PubMed]
- Weber, D.J.; Orenstein, W.; Rutala, W.A. How to improve influenza vaccine coverage of healthcare personnel. Isr. J. Health Policy Res. 2016, 5, 61. [Google Scholar] [CrossRef] [PubMed]
- Guillari, A.; Polito, F.; Pucciarelli, G.; Serra, N.; Gargiulo, G.; Esposito, M.R.; Botti, S.; Rea, T.; Simeone, S. Influenza vaccination and healthcare workers: Barriers and predisposing factors. Acta Bio-Med. Atenei Parm. 2021, 92, e2021004. [Google Scholar] [CrossRef]
- Haviari, S.; Bénet, T.; Saadatian-Elahi, M.; André, P.; Loulergue, P.; Vanhems, P. Vaccination of healthcare workers: A review. Hum. Vaccines Immunother. 2015, 11, 2522–2537. [Google Scholar] [CrossRef]
- Ahmed, F.; Lindley, M.C.; Allred, N.; Weinbaum, C.M.; Grohskopf, L. Effect of influenza vaccination of healthcare personnel on morbidity and mortality among patients: Systematic review and grading of evidence. Clin. Infect. Dis. 2014, 58, 50–57. [Google Scholar] [CrossRef]
- Riphagen-Dalhuisen, J.; Burgerhof, J.G.; Frijstein, G.; van der Geest-Blankert, A.D.; Danhof-Pont, M.B.; de Jager, H.J.; Bos, A.A.; Smeets, E.E.; de Vries, M.J.; Gallee, P.M.; et al. Hospital-based cluster randomised controlled trial to assess effects of a multi-faceted programme on influenza vaccine coverage among hospital healthcare workers and nosocomial influenza in the Netherlands, 2009 to 2011. Eurosurveillance 2013, 18, 20512. [Google Scholar] [CrossRef]
- Gianino, M.M.; Politano, G.; Scarmozzino, A.; Stillo, M.; Amprino, V.; Di Carlo, S.; Benso, A.; Zotti, C.M. Cost of Sickness Absenteeism during Seasonal Influenza Outbreaks of Medium Intensity among Health Care Workers. Int. J. Environ. Res. Public Health 2019, 16, 747. [Google Scholar] [CrossRef] [PubMed]
- Karve, S.; Misurski, D.A.; Meier, G.; Davis, K.L. Employer-incurred health care costs and productivity losses associated with influenza. Hum. Vaccines Immunother. 2013, 9, 841–857. [Google Scholar] [CrossRef] [PubMed]
- Thomas, R.E.; Jefferson, T.; Lasserson, T.J. Influenza vaccination for healthcare workers who care for people aged 60 or older living in long-term care institutions. Cochrane Database Syst. Rev. 2016, 2016, CD005187. [Google Scholar] [CrossRef] [PubMed]
- De Serres, G.; Skowronski, D.M.; Ward, B.J.; Gardam, M.; Lemieux, C.; Yassi, A.; Patrick, D.M.; Krajden, M.; Loeb, M.; Collignon, P.; et al. Influenza Vaccination of Healthcare Workers: Critical Analysis of the Evidence for Patient Benefit Underpinning Policies of Enforcement. PLoS ONE 2017, 12, e0163586. [Google Scholar] [CrossRef] [PubMed]
- Nypaver, C.; Dehlinger, C.; Carter, C. Influenza and Influenza Vaccine: A Review. J. Midwifery Women’s Health 2021, 66, 45–53. [Google Scholar] [CrossRef]
- WHO|World Health Organization. Seasonal Influenza Vaccines: An Overview for Decision-Makers. Available online: https://apps.who.int/iris/handle/10665/336951 (accessed on 11 May 2022).
- Kraigsley, A.M.; Moore, K.A.; Bolster, A.; Peters, M.; Richardson, D.; Arpey, M.; Sonnenberger, M.; McCarron, M.; Lambach, P.; Maltezou, H.C.; et al. Barriers and activities to implementing or expanding influenza vaccination programs in low- and middle-income countries: A global survey. Vaccine 2021, 39, 3419–3427. [Google Scholar] [CrossRef]
- Ortiz, J.R.; Neuzil, K.M. Influenza Immunization in Low- and Middle-Income Countries: Preparing for Next-Generation Influenza Vaccines. J. Infect. Dis. 2019, 219, S97–S106. [Google Scholar] [CrossRef]
- Sheldenkar, A.; Lim, F.; Yung, C.F.; Lwin, M.O. Acceptance and uptake of influenza vaccines in Asia: A systematic review. Vaccine 2019, 37, 4896–4905. [Google Scholar] [CrossRef]
- González-Block, M.Á.; Pelcastre-Villafuerte, B.E.; Riva Knauth, D.; Fachel-Leal, A.; Comes, Y.; Crocco, P.; Noboa, L.; Rodríguez Zea, B.; Ruoti, M.; Díaz Portillo, S.P.; et al. Influenza vaccination hesitancy in large urban centers in South America. Qualitative analysis of confidence, complacency and convenience across risk groups. PLoS ONE 2021, 16, e0256040. [Google Scholar] [CrossRef]
- Pavlovic, D.; Sahoo, P.; Larson, H.J.; Karafillakis, E. Factors influencing healthcare professionals’ confidence in vaccination in Europe: A literature review. Hum. Vaccines Immunother. 2022, 18, 2041360. [Google Scholar] [CrossRef]
- Sallam, M.; Al-Sanafi, M.; Sallam, M. A Global Map of COVID-19 Vaccine Acceptance Rates per Country: An Updated Concise Narrative Review. J. Multidiscip. Healthc. 2022, 2022, 21–45. [Google Scholar] [CrossRef] [PubMed]
- Sallam, M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines 2021, 9, 160. [Google Scholar] [CrossRef] [PubMed]
- Dubé, E.; Laberge, C.; Guay, M.; Bramadat, P.; Roy, R.; Bettinger, J. Vaccine hesitancy: An overview. Hum. Vaccines Immunother. 2013, 9, 1763–1773. [Google Scholar] [CrossRef]
- Hassan, W.; Kazmi, S.K.; Tahir, M.J.; Ullah, I.; Ar Royan, H.; Fahriani, M.; Nainu, F.; Rosa, S.G.V. Global acceptance and hesitancy of COVID-19 vaccination: A narrative review. Narra J 2021, 1, e57. [Google Scholar] [CrossRef]
- MacDonald, N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- Geiger, M.; Rees, F.; Lilleholt, L.; Santana, A.P.; Zettler, I.; Wilhelm, O.; Betsch, C.; Böhm, R. Measuring the 7Cs of Vaccination Readiness. Eur. J. Psychol. Assess. 2021, 38, 261–269. [Google Scholar] [CrossRef]
- Betsch, C.; Schmid, P.; Heinemeier, D.; Korn, L.; Holtmann, C.; Böhm, R. Beyond confidence: Development of a measure assessing the 5C psychological antecedents of vaccination. PLoS ONE 2018, 13, e0208601. [Google Scholar] [CrossRef]
- Betsch, C.; Bach Habersaat, K.; Deshevoi, S.; Heinemeier, D.; Briko, N.; Kostenko, N.; Kocik, J.; Böhm, R.; Zettler, I.; Wiysonge, C.S.; et al. Sample study protocol for adapting and translating the 5C scale to assess the psychological antecedents of vaccination. BMJ Open 2020, 10, e034869. [Google Scholar] [CrossRef]
- Böhm, R.; Betsch, C. Prosocial vaccination. Curr. Opin. Psychol. 2022, 43, 307–311. [Google Scholar] [CrossRef]
- Sallam, M.; Dababseh, D.; Eid, H.; Al-Mahzoum, K.; Al-Haidar, A.; Taim, D.; Yaseen, A.; Ababneh, N.A.; Bakri, F.G.; Mahafzah, A. High Rates of COVID-19 Vaccine Hesitancy and Its Association with Conspiracy Beliefs: A Study in Jordan and Kuwait among Other Arab Countries. Vaccines 2021, 9, 42. [Google Scholar] [CrossRef]
- González-Block, M.Á.; Arroyo-Laguna, J.; Rodríguez-Zea, B.; Pelcastre-Villafuerte, B.E.; Gutiérrez-Calderón, E.; Díaz-Portillo, S.P.; Puentes-Rosas, E.; Sarti, E. The importance of confidence, complacency, and convenience for influenza vaccination among key risk groups in large urban areas of Peru. Hum. Vaccines Immunother. 2021, 17, 465–474. [Google Scholar] [CrossRef] [PubMed]
- Schmid, P.; Rauber, D.; Betsch, C.; Lidolt, G.; Denker, M.-L. Barriers of Influenza Vaccination Intention and Behavior—A Systematic Review of Influenza Vaccine Hesitancy, 2005–2016. PLoS ONE 2017, 12, e0170550. [Google Scholar] [CrossRef] [PubMed]
- Youssef, D.; Berry, A.; Youssef, J.; Abou-Abbas, L. Vaccination against influenza among Lebanese health care workers in the era of coronavirus disease 2019. BMC Public Health 2022, 22, 120. [Google Scholar] [CrossRef] [PubMed]
- Luo, Q.; Gan, L.; Xiong, Y.; Li, Q.; Chen, T.; Tang, X. Knowledge, attitudes and practices related to influenza and influenza vaccine among healthcare workers in Chongqing, China-a cross-sectional study. Hum. Vaccines Immunother. 2021, 17, 5500–5508. [Google Scholar] [CrossRef]
- Awaidy, S.T.; KAl Mayahi, Z.; Kaddoura, M.; Mahomed, O.; Lahoud, N.; Abubakar, A.; Zaraket, H. Influenza Vaccination Hesitancy among Healthcare Workers in South Al Batinah Governorate in Oman: A Cross-Sectional Study. Vaccines 2020, 8, 661. [Google Scholar] [CrossRef]
- Scardina, G.; Ceccarelli, L.; Casigliani, V.; Mazzilli, S.; Napoletano, M.; Padovan, M.; Petillo, A.; Sironi, D.; Brilli, C.; Gattini, V.; et al. Evaluation of Flu Vaccination Coverage among Healthcare Workers during a 3 Years’ Study Period and Attitude towards Influenza and Potential COVID-19 Vaccination in the Context of the Pandemic. Vaccines 2021, 9, 769. [Google Scholar] [CrossRef]
- Treanor, J. Flu Vaccine-Too Much of a Good Thing? J. Infect. Dis. 2017, 215, 1017–1019. [Google Scholar] [CrossRef]
- Skowronski, D.M.; Chambers, C.; De Serres, G.; Sabaiduc, S.; Winter, A.-L.; Dickinson, J.A.; Gubbay, J.B.; Fonseca, K.; Drews, S.J.; Charest, H.; et al. Serial Vaccination and the Antigenic Distance Hypothesis: Effects on Influenza Vaccine Effectiveness During A(H3N2) Epidemics in Canada, 2010–2011 to 2014–2015. J. Infect. Dis. 2017, 215, 1059–1099. [Google Scholar] [CrossRef]
- Okoli, G.N.; Racovitan, F.; Abdulwahid, T.; Hyder, S.K.; Lansbury, L.; Righolt, C.H.; Mahmud, S.M.; Nguyen-Van-Tam, J.S. Decline in Seasonal Influenza Vaccine Effectiveness With Vaccination Program Maturation: A Systematic Review and Meta-analysis. Open Forum Infect. Dis. 2021, 8, ofab069. [Google Scholar] [CrossRef]
- Abdou, M.S.; Kheirallah, K.A.; Aly, M.O.; Ramadan, A.; Elhadi, Y.A.M.; Elbarazi, I.; Deghidy, E.A.; El Saeh, H.M.; Salem, K.M.; Ghazy, R.M. The coronavirus disease 2019 (COVID-19) vaccination psychological antecedent assessment using the Arabic 5c validated tool: An online survey in 13 Arab countries. PLoS ONE 2021, 16, e0260321. [Google Scholar] [CrossRef]
- Rosiello, F.; Anwar, S.; Yufika, A.; Adam, R.Y.; Ismaeil, M.I.H.; Ismail, A.Y.; Dahman, N.B.H.; Hafsi, M.; Ferjani, M.; Sami, F.S.; et al. Acceptance of COVID-19 vaccination at different hypothetical efficacy and safety levels in ten countries in Asia, Africa, and South America. Narra J 2021, 1, e55. [Google Scholar] [CrossRef]
- Sallam, M.; Dababseh, D.; Yaseen, A.; Al-Haidar, A.; Taim, D.; Eid, H.; Ababneh, N.A.; Bakri, F.G.; Mahafzah, A. COVID-19 misinformation: Mere harmless delusions or much more? A knowledge and attitude cross-sectional study among the general public residing in Jordan. PLoS ONE 2020, 15, e0243264. [Google Scholar] [CrossRef] [PubMed]
- Sallam, M.; Dababseh, D.; Eid, H.; Hasan, H.; Taim, D.; Al-Mahzoum, K.; Al-Haidar, A.; Yaseen, A.; Ababneh, N.A.; Assaf, A.; et al. Low COVID-19 Vaccine Acceptance Is Correlated with Conspiracy Beliefs among University Students in Jordan. Int. J. Environ. Res. Public Health 2021, 18, 2407. [Google Scholar] [CrossRef] [PubMed]
- Nazer, L.H.; Tuffaha, H. Health Care and Pharmacy Practice in Jordan. Can. J. Hosp. Pharm. 2017, 70, 150–155. [Google Scholar] [CrossRef]
- World Health Organization|Regional Office for the Eastern Mediterranean. Health Workforce Snapshot Jordan. Available online: https://apps.who.int/iris/handle/10665/332429 (accessed on 12 May 2022).
- Epitools-Epidemiological Calculators. Sample Size to Estimate a Simple Proportion (Apparent Prevalence). Available online: https://epitools.ausvet.com.au/oneproportion (accessed on 10 March 2022).
- Sapra, R.L. How to Calculate an Adequate Sample Size? In How to Practice Academic Medicine and Publish from Developing Countries? A Practical Guide; Nundy, S., Kakar, A., Bhutta, Z.A., Eds.; Springer Nature: Singapore, 2022; pp. 81–93. [Google Scholar] [CrossRef]
- Abd ElHafeez, S.; Elbarazi, I.; Shaaban, R.; ElMakhzangy, R.; Ossama Aly, M.; Alnagar, A.; Yacoub, M.; El Saeh, H.M.; Eltaweel, N.; Alqutub, S.T.; et al. Arabic validation and cross-cultural adaptation of the 5C scale for assessment of COVID-19 vaccines psychological antecedents. PLoS ONE 2021, 16, e0254595. [Google Scholar] [CrossRef]
- Shapiro, G.K.; Holding, A.; Perez, S.; Amsel, R.; Rosberger, Z. Validation of the vaccine conspiracy beliefs scale. Papillomavirus Res. 2016, 2, 167–172. [Google Scholar] [CrossRef]
- Abu-Gharbieh, E.; Fahmy, S.; Rasool, B.A.; Khan, S. Influenza Vaccination: Healthcare Workers Attitude in Three Middle East Countries. Int. J. Med. Sci. 2010, 7, 319–325. [Google Scholar] [CrossRef]
- Elawad, K.H.; Farag, E.A.; Abuelgasim, D.A.; Smatti, M.K.; Al-Romaihi, H.E.; Al Thani, M.; Al Mujalli, H.; Shehata, Z.; Alex, M.; Al Thani, A.A.; et al. Improving Influenza Vaccination Rate among Primary Healthcare Workers in Qatar. Vaccines 2017, 5, 36. [Google Scholar] [CrossRef]
- Alhalaseh, L.; Fayoumi, H.; Khalil, B. The Health Belief Model in predicting healthcare workers’ intention for influenza vaccine uptake in Jordan. Vaccine 2020, 38, 7372–7378. [Google Scholar] [CrossRef]
- Assaf, A.M.; Hammad, E.A.; Haddadin, R.N. Influenza Vaccination Coverage Rates, Knowledge, Attitudes, and Beliefs in Jordan: A Comprehensive Study. Viral Immunol. 2016, 29, 516–525. [Google Scholar] [CrossRef]
- Billings, J.; Ching, B.C.F.; Gkofa, V.; Greene, T.; Bloomfield, M. Experiences of frontline healthcare workers and their views about support during COVID-19 and previous pandemics: A systematic review and qualitative meta-synthesis. BMC Health Serv. Res. 2021, 21, 923. [Google Scholar] [CrossRef] [PubMed]
- Dara, S.; Sharma, S.K.; Kumar, A.; Goel, A.D.; Jain, V.; Sharma, M.C.; Gupta, M.K.; Saurabh, S.; Bhardwaj, P.; Misra, S. Awareness, Attitude, and Acceptability of Healthcare Workers About COVID-19 Vaccination in Western India. Cureus 2021, 13, e18400. [Google Scholar] [CrossRef] [PubMed]
- Sani, T.; Morelli, I.; Sarti, D.; Tassinari, G.; Capalbo, M.; Espinosa, E.; Gasperini, B.; Prospero, E. Attitudes of Healthcare Workers toward Influenza Vaccination in the COVID-19 Era. Vaccines 2022, 10, 883. [Google Scholar] [CrossRef] [PubMed]
- Lecce, M.; Biganzoli, G.; Agnello, L.; Belisario, I.; Cicconi, G.; D’Amico, M.; De Giorgi, F.; Ferilli, A.; Ferraguzzi, G.; Guzzardi, F.; et al. COVID-19 and Influenza Vaccination Campaign in a Research and University Hospital in Milan, Italy. Int. J. Environ. Res. Public Health 2022, 19, 6500. [Google Scholar] [CrossRef]
- Marinos, G.; Lamprinos, D.; Georgakopoulos, P.; Oikonomou, E.; Zoumpoulis, G.; Siasos, G.; Schizas, D.; Damaskos, C.; Garmpis, N.; Garmpi, A.; et al. Increased Influenza Vaccination Coverage among Members of the Athens Medical Association Amidst COVID-19 Pandemic. Vaccines 2022, 10, 797. [Google Scholar] [CrossRef] [PubMed]
- Dettori, M.; Arghittu, A.; Deiana, G.; Azara, A.; Masia, M.D.; Palmieri, A.; Spano, A.L.; Serra, A.; Castiglia, P. Influenza Vaccination Strategies in Healthcare Workers: A Cohort Study (2018–2021) in an Italian University Hospital. Vaccines 2021, 9, 971. [Google Scholar] [CrossRef]
- Rachiotis, G.; Papagiannis, D.; Malli, F.; Papathanasiou, I.V.; Kotsiou, O.; Fradelos, E.C.; Daniil, Z.; Gourgoulianis, K.I. Determinants of Influenza Vaccination Coverage among Greek Health Care Workers amid COVID-19 Pandemic. Infect. Dis. Rep. 2021, 13, 71. [Google Scholar] [CrossRef]
- Al Nawas, B. The Jordan Times. Government Halves Cost of Flu Vaccine. Available online: https://jordantimes.com/news/local/government-halves-cost-flu-vaccine (accessed on 21 May 2022).
- To, K.W.; Lai, A.; Lee, K.C.; Koh, D.; Lee, S.S. Increasing the coverage of influenza vaccination in healthcare workers: Review of challenges and solutions. J. Hosp. Infect. 2016, 94, 133–142. [Google Scholar] [CrossRef]
- Black, C.L.; Yue, X.; Ball, S.W.; Fink, R.V.; de Perio, M.A.; Laney, A.S.; Williams, W.W.; Graitcer, S.B.; Fiebelkorn, A.P.; Lu, P.J.; et al. Influenza Vaccination Coverage Among Health Care Personnel—United States, 2017–2018 Influenza Season. MMWR Morb. Mortal. Wkly. Rep. 2018, 67, 1050–1054. [Google Scholar] [CrossRef]
- Hakim, S.A.; Amin, W.; Allam, M.F.; Fathy, A.M.; Mohsen, A. Attitudes, beliefs and practice of Egyptian healthcare workers towards seasonal influenza vaccination. Influenza Other Respir. Viruses 2021, 15, 778–788. [Google Scholar] [CrossRef]
- Yi, H.; Yang, Y.; Zhang, L.; Zhang, M.; Wang, Q.; Zhang, T.; Zhang, Y.; Qin, Y.; Peng, Z.; Leng, Z.; et al. Improved influenza vaccination coverage among health-care workers: Evidence from a web-based survey in China, 2019/2020 season. Hum. Vaccines Immunother. 2021, 17, 2185–2189. [Google Scholar] [CrossRef] [PubMed]
- Korkmaz, N.; Nazik, S.; Gümüştakım, R.; Uzar, H.; Kul, G.; Tosun, S.; Torun, A.; Demirbakan, H.; Seremet Keskin, A.; Kaçmaz, A.B.; et al. Influenza vaccination rates, knowledge, attitudes and behaviours of healthcare workers in Turkey: A multicentre study. Int. J. Clin. Pr. 2021, 75, e13659. [Google Scholar] [CrossRef] [PubMed]
- Principi, N.; Camilloni, B.; Esposito, S. Influenza immunization policies: Which could be the main reasons for differences among countries? Hum. Vaccines Immunother. 2018, 14, 684–692. [Google Scholar] [CrossRef] [PubMed]
- Bock, J.-O.; Hajek, A.; König, H.-H. Psychological determinants of influenza vaccination. BMC Geriatr. 2017, 17, 194. [Google Scholar] [CrossRef]
- Borthwick, C.; O’Connor, R.; Kennedy, L. Psychological predictors of seasonal influenza vaccination uptake among adults with a high-risk physical health condition: A systematic review. Psychol. Health 2021, 36, 214–235. [Google Scholar] [CrossRef]
- Goodwin, R.; Ben-Ezra, M.; Takahashi, M.; Luu, L.-A.N.; Borsfay, K.; Kovács, M.; Hou, W.K.; Hamama-Raz, Y.; Levin, Y. Psychological factors underpinning vaccine willingness in Israel, Japan and Hungary. Sci. Rep. 2022, 12, 439. [Google Scholar] [CrossRef]
- Lorini, C.; Collini, F.; Gasparini, F.; Paolini, D.; Grazzini, M.; Ierardi, F.; Galletti, G.; Zanobini, P.; Gemmi, F.; Bonaccorsi, G. Health Literacy, Vaccine Confidence and Influenza Vaccination Uptake among Nursing Home Staff: A Cross-Sectional Study Conducted in Tuscany. Vaccines 2020, 8, 154. [Google Scholar] [CrossRef]
- Al-Sanafi, M.; Sallam, M. Psychological Determinants of COVID-19 Vaccine Acceptance among Healthcare Workers in Kuwait: A Cross-Sectional Study Using the 5C and Vaccine Conspiracy Beliefs Scales. Vaccines 2021, 9, 701. [Google Scholar] [CrossRef]
- Kwok, K.O.; Li, K.-K.; Wei, W.I.; Tang, A.; Wong, S.Y.S.; Lee, S.S. Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: A survey. Int. J. Nurs. Stud. 2021, 114, 103854. [Google Scholar] [CrossRef]
- Torun, S.D.; Torun, F. Vaccination against pandemic influenza A/H1N1 among healthcare workers and reasons for refusing vaccination in Istanbul in last pandemic alert phase. Vaccine 2010, 28, 5703–5710. [Google Scholar] [CrossRef]
- Oguz, M.M. Improving influenza vaccination uptake among healthcare workers by on-site influenza vaccination campaign in a tertiary children hospital. Hum. Vaccines Immunother. 2019, 15, 1060–1065. [Google Scholar] [CrossRef] [PubMed]
- Kadi, Z.; Atif, M.-L.; Brenet, A.; Izoard, S.; Astagneau, P. Barriers of influenza vaccination in health care personnel in France. Am. J. Infect. Control 2016, 44, 361–362. [Google Scholar] [CrossRef] [PubMed]
- Martinello, R.A.; Jones, L.; Topal, J.E. Correlation Between Healthcare Workers’ Knowledge of Influenza Vaccine and Vaccine Receipt. Infect. Control Hosp. Epidemiol. 2015, 24, 845–847. [Google Scholar] [CrossRef] [PubMed]
- Hollmeyer, H.; Hayden, F.; Mounts, A.; Buchholz, U. Review: Interventions to increase influenza vaccination among healthcare workers in hospitals. Influenza Other Respir. Viruses 2013, 7, 604–621. [Google Scholar] [CrossRef]
- Werk, L.N.; Diaz, M.C.; Cadilla, A.; Franciosi, J.P.; Hossain, M.J. Promoting Adherence to Influenza Vaccination Recommendations in Pediatric Practice. J. Prim. Care Community Health 2019, 10, 2150132719853061. [Google Scholar] [CrossRef]
- Rosen, B.; Waitzberg, R.; Israeli, A.; Hartal, M.; Davidovitch, N. Addressing vaccine hesitancy and access barriers to achieve persistent progress in Israel’s COVID-19 vaccination program. Isr. J. Health Policy Res. 2021, 10, 43. [Google Scholar] [CrossRef]
- Nowak, G.J.; Sheedy, K.; Bursey, K.; Smith, T.M.; Basket, M. Promoting influenza vaccination: Insights from a qualitative meta-analysis of 14 years of influenza-related communications research by U.S. Centers for Disease Control and Prevention (CDC). Vaccine 2015, 33, 2741–2756. [Google Scholar] [CrossRef]
- Zhou, X.; Zhao, X.; Liu, J.; Yang, W. Effectiveness of Educational Intervention on Influenza Vaccine Uptake: A Meta-Analysis of Randomized Controlled Trials. Iran J. Public Health 2020, 49, 2256–2263. [Google Scholar] [CrossRef]
- Yue, M.; Wang, Y.; Low, C.K.; Yoong, J.S.-y.; Cook, A.R. Optimal Design of Population-Level Financial Incentives of Influenza Vaccination for the Elderly. Value Health 2020, 23, 200–208. [Google Scholar] [CrossRef]
- Szőllősi, G.; Al-Tammemi, A.; Harsányi, S.; Garbóczy, S.; Balogh, N.; Simon, I.; Kolozsvári, L. The Impacts of Implementing Primary Care Indicators and Related Financial Incentives on the Trends of Vaccination Coverage Against Influenza Among Elderly People in Hungary. Res. Sq. 2020; 1–11, Preprint. [Google Scholar] [CrossRef]
- Otieno, N.A.; Otiato, F.; Nyawanda, B.; Adero, M.; Wairimu, W.N.; Ouma, D.; Atito, R.; Wilson, A.; Gonzalez-Casanova, I.; Malik, F.A.; et al. Drivers and barriers of vaccine acceptance among pregnant women in Kenya. Hum. Vaccines Immunother. 2020, 16, 2429–2437. [Google Scholar] [CrossRef]
- Bonaccorsi, G.; Santomauro, F.; Porchia, B.R.; Niccolai, G.; Pellegrino, E.; Bonanni, P.; Lorini, C. Beliefs and Opinions of Health Care Workers and Students Regarding Influenza and Influenza Vaccination in Tuscany, Central Italy. Vaccines 2015, 3, 137. [Google Scholar] [CrossRef] [PubMed]
- Ye, L.; Fang, T.; Cui, J.; Zhu, G.; Ma, R.; Sun, Y.; Li, P.; Li, H.; Dong, H.; Xu, G. The intentions to get vaccinated against influenza and actual vaccine uptake among diabetic patients in Ningbo, China: Identifying motivators and barriers. Hum. Vaccines Immunother. 2021, 17, 106–118. [Google Scholar] [CrossRef] [PubMed]
- Rong, H.; Lai, X.; Ma, X.; Hou, Z.; Li, S.; Jing, R.; Zhang, H.; Peng, Z.; Feng, L.; Fang, H. Seasonal Influenza Vaccination and Recommendation: The Difference between General Practitioners and Public Health Workers in China. Vaccines 2020, 8, 265. [Google Scholar] [CrossRef] [PubMed]
- Papini, F.; Mazzilli, S.; Paganini, D.; Rago, L.; Arzilli, G.; Pan, A.; Goglio, A.; Tuvo, B.; Privitera, G.; Casini, B. Healthcare Workers Attitudes, Practices and Sources of Information for COVID-19 Vaccination: An Italian National Survey. Int. J. Environ. Res. Public Health 2022, 19, 733. [Google Scholar] [CrossRef]
- Al-Otaibi, B.; El-Saed, A.; Balkhy, H. Influenza vaccination among healthcare workers at a tertiary care hospital in Saudi Arabia: Facing challenges. Ann. Thorac. Med. 2010, 5, 120–121. [Google Scholar] [CrossRef]
- Rabaan, A.A.; Wyse, R.; Al-Tawfiq, J.A.; Alahmed, S.H.; Aljeldah, M.M.; Bazzi, A.M.; Asseri, A.M.; Binjomah, A.Z.; Haque, S. Influenza vaccine acceptance by healthcare workers in Saudi Arabia: A questionnaire-based analysis. Infez. Med. 2020, 28, 70–77. [Google Scholar]
- Bonaccorsi, G.; Lorini, C.; Santomauro, F.; Guarducci, S.; Pellegrino, E.; Puggelli, F.; Balli, M.; Bonanni, P. Predictive factors associated with the acceptance of pandemic and seasonal influenza vaccination in health care workers and students in Tuscany, Central Italy. Hum. Vaccines Immunother. 2013, 9, 2603–2612. [Google Scholar] [CrossRef]
- Ripp, T.; Röer, J.P. Systematic review on the association of COVID-19-related conspiracy belief with infection-preventive behavior and vaccination willingness. BMC Psychol. 2022, 10, 66. [Google Scholar] [CrossRef]
- Imhoff, R.; Lamberty, P. A Bioweapon or a Hoax? The Link Between Distinct Conspiracy Beliefs About the Coronavirus Disease (COVID-19) Outbreak and Pandemic Behavior. Soc. Psychol. Personal. Sci. 2020, 11, 1110–1118. [Google Scholar] [CrossRef]
- Salali, G.D.; Uysal, M.S. COVID-19 vaccine hesitancy is associated with beliefs on the origin of the novel coronavirus in the UK and Turkey. Psychol. Med. 2020; 1–3, Online ahead of print. [Google Scholar] [CrossRef]
- Sallam, M.; Al-Mahzoum, K.; Dardas, L.A.; Al-Tammemi, A.a.B.; Al-Majali, L.; Al-Naimat, H.; Jardaneh, L.; AlHadidi, F.; Al-Salahat, K.; Al-Ajlouni, E.; et al. Knowledge of Human Monkeypox and Its Relation to Conspiracy Beliefs among Students in Jordanian Health Schools: Filling the Knowledge Gap on Emerging Zoonotic Viruses. Medicina 2022, 58, 924. [Google Scholar] [CrossRef]
- Bierwiaczonek, K.; Kunst, J.R.; Pich, O. Belief in COVID-19 Conspiracy Theories Reduces Social Distancing over Time. Appl. Psychol. Health Well Being 2020, 12, 1270–1285. [Google Scholar] [CrossRef] [PubMed]
- Knight, H.; Jia, R.; Ayling, K.; Bradbury, K.; Baker, K.; Chalder, T.; Morling, J.R.; Durrant, L.; Avery, T.; Ball, J.K.; et al. Understanding and addressing vaccine hesitancy in the context of COVID-19: Development of a digital intervention. Public Health 2021, 201, 98–107. [Google Scholar] [CrossRef] [PubMed]
- Gualano, M.R.; Corradi, A.; Voglino, G.; Catozzi, D.; Olivero, E.; Corezzi, M.; Bert, F.; Siliquini, R. Healthcare Workers’ (HCWs) attitudes towards mandatory influenza vaccination: A systematic review and meta-analysis. Vaccine 2021, 39, 901–914. [Google Scholar] [CrossRef] [PubMed]
- Haridi, H.K.; Salman, K.A.; Basaif, E.A.; Al-Skaibi, D.K. Influenza vaccine uptake, determinants, motivators, and barriers of the vaccine receipt among healthcare workers in a tertiary care hospital in Saudi Arabia. J. Hosp. Infect. 2017, 96, 268–275. [Google Scholar] [CrossRef] [PubMed]
- Akan, H.; Yavuz, E.; Yayla, M.E.; Külbay, H.; Kaspar, E.Ç.; Zahmacıoğlu, O.; Badur, S. Factors affecting uptake of influenza vaccination among family physicians. Vaccine 2016, 34, 1712–1718. [Google Scholar] [CrossRef]
- Wang, T.L.; Jing, L.; Bocchini, J.A., Jr. Mandatory influenza vaccination for all healthcare personnel: A review on justification, implementation and effectiveness. Curr. Opin. Pediatr. 2017, 29, 606–615. [Google Scholar] [CrossRef]
- Rakita, R.M.; Hagar, B.A.; Crome, P.; Lammert, J.K. Mandatory Influenza Vaccination of Healthcare Workers: A 5-Year Study. Infect. Control Hosp. Epidemiol. 2015, 31, 881–888. [Google Scholar] [CrossRef]
- Lytras, T.; Kopsachilis, F.; Mouratidou, E.; Papamichail, D.; Bonovas, S. Interventions to increase seasonal influenza vaccine coverage in healthcare workers: A systematic review and meta-regression analysis. Hum. Vaccines Immunother. 2016, 12, 671–681. [Google Scholar] [CrossRef]
- Maltezou, H.C.; Dounias, G.; Rapisarda, V.; Ledda, C. Vaccination policies for healthcare personnel: Current challenges and future perspectives. Vaccine X 2022, 11, 100172. [Google Scholar] [CrossRef]
- Edmond, M.B. Mandatory Flu Vaccine for Healthcare Workers: Not Worthwhile. Open Forum Infect. Dis. 2019, 6, ofy214. [Google Scholar] [CrossRef]
- Chambon, M.; Kammeraad, W.; van Harreveld, F.; Dalege, J.; Elberse, J.; van der Maas, H. Why COVID-19 vaccination intention is so hard to change: A longitudinal study. PsyArXiv, 2022; preprint. [Google Scholar] [CrossRef]
| Characteristic | Occupational Category n 3 (%) | |||||||
|---|---|---|---|---|---|---|---|---|
| Total (n = 1218) | Nurse (n = 412, 33.8%) | Physician (n = 367, 30.1%) | Dentist (n = 87, 7.1%) | Pharmacist (n = 161, 13.2%) | Technician 4 (n = 182, 14.9%) | MSAR 5 (n = 9, 0.7%) | ||
| Median age (IQR) in years 1 | 38 (31–49) | 36 (33–43) | 49 (30–61) | 45 (37–53) | 37 (32–45) | 34 (28–43) | 37 (27–45) | |
| Sex | Male | 483 (39.7) | 98 (23.8) | 246 (67.0) | 35 (40.2) | 52 (32.3) | 51 (28.0) | 1 (11.1) |
| Female | 735 (60.3) | 314 (76.2) | 121 (33.0) | 52 (59.8) | 109 (67.7) | 131 (72.0) | 8 (88.9) | |
| Region | Amman | 777 (63.8) | 188 (45.6) | 296 (80.7) | 55 (63.2) | 111 (68.9) | 122 (67.0) | 5 (55.6) |
| Outside Amman | 441 (36.2) | 224 (54.4) | 71 (19.3) | 32 (36.8) | 50 (31.1) | 60 (33.0) | 4 (44.4) | |
| Educational level | Undergraduate | 754 (61.9) | 351 (85.2) | 128 (34.9) | 50 (57.5) | 102 (63.4) | 115 (63.2) | 8 (88.9) |
| Postgraduate | 464 (38.1) | 61 (14.8) | 239 (65.1) | 37 (42.5) | 59 (36.6) | 67 (36.8) | 1 (11.1) | |
| Monthly income 2 | JOD < 1000 | 590 (48.4) | 309 (75.0) | 70 (19.1) | 22 (25.3) | 76 (47.2) | 105 (57.7) | 8 (88.9) |
| JOD ≥ 1000 | 628 (51.6) | 103 (25.0) | 297 (80.9) | 65 (74.7) | 85 (52.8) | 77 (42.3) | 1 (11.1) | |
| History of chronic disease | Yes | 231 (19.0) | 53 (12.9) | 118 (32.2) | 15 (17.2) | 25 (15.5) | 18 (9.9) | 2 (22.2) |
| No | 987 (81.0) | 359 (87.1) | 249 (67.8) | 72 (82.8) | 136 (84.5) | 164 (90.1) | 7 (77.8) | |
| Influenza Knowledge/Attitude Item | Response | Occupational Category n 2 (%) | ||||||
|---|---|---|---|---|---|---|---|---|
| Nurse | Physician | Dentist | Pharmacist | Technician 3 | MSAR 4 | p Value 5 | ||
| Influenza causes only mild symptoms; therefore, it cannot be considered a serious disease | Correct | 242 (58.7) | 165 (45.0) | 47 (54.0) | 92 (57.1) | 103 (56.6) | 5 (55.6) | 0.005 |
| Incorrect | 170 (41.3) | 202 (55.0) | 40 (46.0) | 69 (42.9) | 79 (43.4) | 4 (44.4) | ||
| Influenza can cause severe illness or death | Correct | 269 (65.3) | 330 (89.9) | 67 (77.0) | 116 (72.0) | 132 (72.5) | 8 (88.9) | <0.001 |
| Incorrect | 143 (34.7) | 37 (10.1) | 20 (23.0) | 45 (28.0) | 50 (27.5) | 1 (11.1) | ||
| Influenza can be transmitted through droplets from coughing or sneezing | Correct | 407 (98.8) | 365 (99.5) | 85 (97.7) | 157 (97.5) | 181 (99.5) | 9 (100) | 0.368 |
| Incorrect | 5 (1.2) | 2 (0.5) | 2 (2.3) | 4 (2.5) | 1 (0.5) | 0 (0) | ||
| Influenza can be transmitted through blood and body fluids | Correct | 344 (83.5) | 295 (80.4) | 67 (77.0) | 106 (65.8) | 126 (69.2) | 7 (77.8) | <0.001 |
| Incorrect | 68 (16.5) | 72 (19.6) | 20 (23.0) | 55 (34.2) | 56 (30.8) | 2 (22.2) | ||
| Influenza vaccination reduces absenteeism from work | Correct | 343 (83.3) | 350 (95.4) | 77 (88.5) | 139 (86.3) | 139 (76.4) | 5 (55.6) | <0.001 |
| Incorrect | 69 (16.7) | 17 (4.6) | 10 (11.5) | 22 (13.7) | 43 (23.6) | 4 (44.4) | ||
| Vaccinating HCWs against flu helps protect patients from severe illness/death 1 | Correct | 344 (83.5) | 352 (95.9) | 76 (87.4) | 146 (90.7) | 148 (81.3) | 7 (77.8) | <0.001 |
| Incorrect | 68 (16.5) | 15 (4.1) | 11 (12.6) | 15 (9.3) | 34 (18.7) | 2 (22.2) | ||
| In Jordan, vaccination of HCWs against influenza should be mandatory | Yes | 206 (50.0) | 199 (54.2) | 40 (46.0) | 71 (44.1) | 68 (37.4) | 1 (11.1) | 0.001 |
| No | 206 (50.0) | 168 (45.8) | 47 (54.0) | 90 (55.9) | 114 (62.6) | 8 (88.9) | ||
| Characteristic | Would You Be Willing to Get the Influenza Vaccine if It Was Available for Free? | p Value, χ2 | Are You Willing to Pay for Influenza Vaccine if the Cost Does Not Exceed JOD 15? | p Value, χ2 | Have You Received the Influenza Vaccine in the Previous Year? | p Value, χ2 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes | Maybe | No | Yes | Maybe | No | Yes | No | |||||
| Sex | Male | 359 (74.5) | 84 (17.4) | 39 (8.1) | <0.001, 25.930 | 198 (41.1) | 140 (29.0) | 144 (29.9) | <0.001, 37.273 | 330 (68.5) | 152 (31.5) | 0.001, 10.422 |
| Female | 448 (61.6) | 168 (23.1) | 111 (15.3) | 190 (26.1) | 216 (29.7) | 321 (44.2) | 434 (59.7) | 293 (40.3) | ||||
| Age | ≤38 years | 395 (64.4) | 151 (24.6) | 67 (10.9) | 0.004, 10.889 | 134 (21.9) | 201 (32.8) | 278 (45.4) | <0.001, 61.387 | 355 (57.9) | 258 (42.1) | <0.001, 16.047 |
| >38 years | 412 (69.1) | 101 (16.9) | 83 (13.9) | 254 (42.6) | 155 (26.0) | 187 (31.4) | 409 (68.6) | 187 (31.4) | ||||
| HCW category 1 | Nurse | 266 (64.6) | 91 (22.1) | 55 (13.3) | <0.001, 73.611 | 78 (18.9) | 121 (29.4) | 213 (51.7) | <0.001, 134.443 | 292 (70.9) | 120 (29.1) | <0.001, 41.672 |
| Physician | 300 (81.7) | 43 (11.7) | 24 (6.5) | 188 (51.2) | 97 (26.4) | 82 (22.3) | 249 (67.8) | 118 (32.2) | ||||
| Dentist | 62 (71.3) | 16 (18.4) | 9 (10.3) | 43 (49.4) | 20 (23.0) | 24 (27.6) | 52 (59.8) | 35 (40.2) | ||||
| Pharmacist | 90 (55.9) | 44 (27.3) | 27 (16.8) | 40 (24.8) | 54 (33.5) | 67 (41.6) | 85 (52.8) | 76 (47.2) | ||||
| Technician 2 | 89 (48.9) | 58 (31.9) | 35 (19.2) | 39 (21.4) | 64 (35.2) | 79 (43.4) | 86 (47.3) | 96 (52.7) | ||||
| Region | Amman | 532 (68.9) | 144 (18.7) | 96 (12.4) | 0.036, 6.653 | 292 (37.8) | 218 (28.2) | 262 (33.9) | <0.001, 34.520 | 493 (63.9) | 279 (36.1) | 0.539, 0.378 |
| Out capital 3 | 275 (62.9) | 108 (24.7) | 54 (12.4) | 96 (22.0) | 138 (31.6) | 203 (46.5) | 271 (62.0) | 166 (38.0) | ||||
| Educational level | Undergrad | 477 (63.9) | 178 (23.9) | 91 (12.2) | 0.003, 11.868 | 181 (24.3) | 236 (31.6) | 329 (44.1) | <0.001, 58.179 | 447 (59.9) | 299 (40.1) | 0.002, 9.745 |
| Postgrad | 330 (71.3) | 74 (16.0) | 59 (12.7) | 207 (44.7) | 120 (25.9) | 136 (29.4) | 317 (68.5) | 146 (31.5) | ||||
| Monthly income | JOD < 1000 4 | 369 (63.4) | 142 (24.4) | 71 (12.2) | 0.010, 9.297 | 118 (20.3) | 178 (30.6) | 286 (49.1) | <0.001, 85.862 | 357 (61.3) | 225 (38.7) | 0.136, 2.222 |
| JOD ≥ 1000 | 438 (69.9) | 110 (17.5) | 79 (12.6) | 270 (43.1) | 178 (28.4) | 179 (28.5) | 407 (64.9) | 220 (35.1) | ||||
| Chronic disease | Yes | 175 (76.4) | 34 (14.8) | 20 (8.7) | 0.003, 11.512 | 107 (46.7) | 64 (27.9) | 58 (25.3) | <0.001, 31.219 | 171 (74.7) | 58 (25.3) | <0.001, 16.565 |
| No | 632 (64.5) | 218 (22.2) | 130 (13.3) | 281 (28.7) | 292 (29.8) | 407 (41.5) | 593 (60.5) | 387 (39.5) | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sallam, M.; Ghazy, R.M.; Al-Salahat, K.; Al-Mahzoum, K.; AlHadidi, N.M.; Eid, H.; Kareem, N.; Al-Ajlouni, E.; Batarseh, R.; Ababneh, N.A.; et al. The Role of Psychological Factors and Vaccine Conspiracy Beliefs in Influenza Vaccine Hesitancy and Uptake among Jordanian Healthcare Workers during the COVID-19 Pandemic. Vaccines 2022, 10, 1355. https://doi.org/10.3390/vaccines10081355
Sallam M, Ghazy RM, Al-Salahat K, Al-Mahzoum K, AlHadidi NM, Eid H, Kareem N, Al-Ajlouni E, Batarseh R, Ababneh NA, et al. The Role of Psychological Factors and Vaccine Conspiracy Beliefs in Influenza Vaccine Hesitancy and Uptake among Jordanian Healthcare Workers during the COVID-19 Pandemic. Vaccines. 2022; 10(8):1355. https://doi.org/10.3390/vaccines10081355
Chicago/Turabian StyleSallam, Malik, Ramy Mohamed Ghazy, Khaled Al-Salahat, Kholoud Al-Mahzoum, Nadin Mohammad AlHadidi, Huda Eid, Nariman Kareem, Eyad Al-Ajlouni, Rawan Batarseh, Nidaa A. Ababneh, and et al. 2022. "The Role of Psychological Factors and Vaccine Conspiracy Beliefs in Influenza Vaccine Hesitancy and Uptake among Jordanian Healthcare Workers during the COVID-19 Pandemic" Vaccines 10, no. 8: 1355. https://doi.org/10.3390/vaccines10081355
APA StyleSallam, M., Ghazy, R. M., Al-Salahat, K., Al-Mahzoum, K., AlHadidi, N. M., Eid, H., Kareem, N., Al-Ajlouni, E., Batarseh, R., Ababneh, N. A., Sallam, M., Alsanafi, M., Umakanthan, S., Al-Tammemi, A. B., Bakri, F. G., Harapan, H., Mahafzah, A., & Al Awaidy, S. T. (2022). The Role of Psychological Factors and Vaccine Conspiracy Beliefs in Influenza Vaccine Hesitancy and Uptake among Jordanian Healthcare Workers during the COVID-19 Pandemic. Vaccines, 10(8), 1355. https://doi.org/10.3390/vaccines10081355










