Satisfaction with COVID-19 Vaccines in Health Care Workers and the General Population: A Cross-Sectional Study in Urban Bangkok, Thailand
Abstract
:1. Introduction
2. Methods
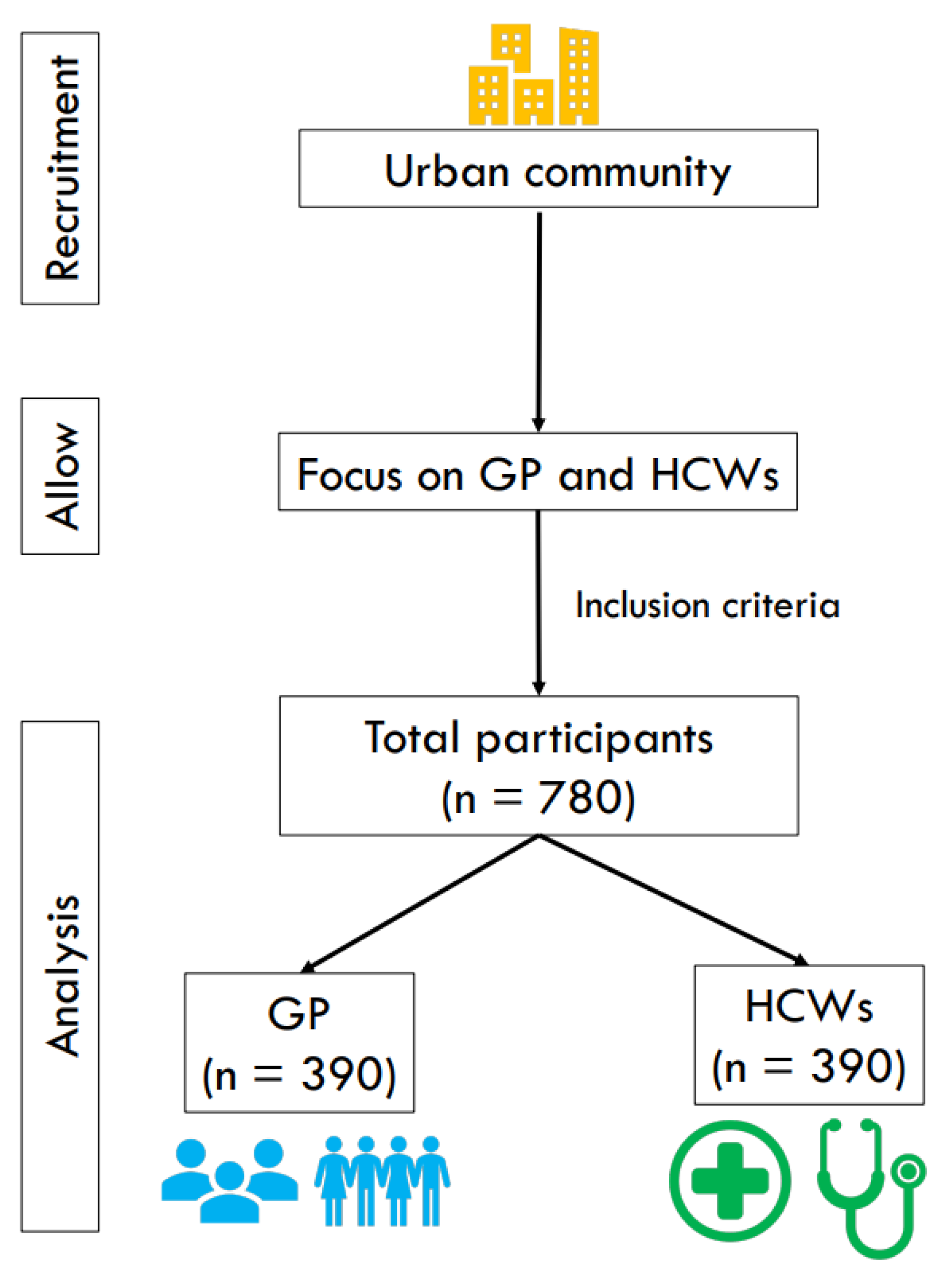
2.1. Study Design
2.2. Participants
2.3. Data Collection
2.4. Questionnaire
2.5. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Vaccine Satisfaction Scores
3.3. Comparison of Total Vaccine Satisfaction Scores
3.4. Comparison of Satisfaction with Vaccine Types
3.5. Association between Participant Characteristics and Satisfaction with COVID-19 Vaccines
4. Discussion
4.1. Vaccine Satisfaction Scores among GP and HCWs
4.2. Comparison of Total Vaccine Satisfaction Scores
4.3. Comparison of Satisfaction with Vaccine Types
4.4. Association between Participant Characteristics and Vaccine Satisfaction
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Kunno, J.; Supawattanabodee, B.; Sumanasrethakul, C.; Wiriyasivaj, B.; Kuratong, S.; Kaewchandee, C. Comparison of Different Waves during the COVID-19 Pandemic: Retrospective Descriptive Study in Thailand. Adv. Prev. Med. 2021, 2021, 5807056. [Google Scholar] [CrossRef] [PubMed]
- Fine, P.; Eames, K.; Heymann, D.L. “Herd Immunity”: A Rough Guide. Clin. Infect. Dis. 2011, 52, 911–916. [Google Scholar] [CrossRef]
- Klugar, M.; Riad, A.; Mekhemar, M.; Conrad, J.; Buchbender, M.; Howaldt, H.P.; Attia, S. Side Effects of mRNA-Based and Viral Vector-Based COVID-19 Vaccines among German Healthcare Workers. Biology 2021, 10, 752. [Google Scholar] [CrossRef] [PubMed]
- Kilic, M.; Ustundag Ocal, N.; Uslukilic, G. The relationship of Covid-19 vaccine attitude with life satisfaction, religious attitude and Covid-19 avoidance in Turkey. Hum. Vaccines Immunother. 2021, 17, 3384–3393. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Vaccines and Immunization. 2020. Available online: https://www.who.int/health-topics/vaccines-and-immunization#tab=tab_1. (accessed on 1 January 2020).
- Klugar, M.; Riad, A.; Mohanan, L.; Pokorná, A. COVID-19 Vaccine Booster Hesitancy (VBH) of Healthcare Workers in Czechia: National Cross-Sectional Study. Vaccines 2021, 9, 1437. [Google Scholar] [CrossRef] [PubMed]
- Control, D.o.D. Progress Report on COVID-19 Vaccination Service; Ministry of Public Health: Nonthaburi, Thailand, 2020; Available online: https://ddc.moph.go.th/vaccine-covid19/pages/ (accessed on 1 January 2020).
- Atwell, J.E.; Salmon, D.A. Pertussis resurgence and vaccine uptake: Implications for reducing vaccine hesitancy. Pediatrics 2014, 134, 602–604. [Google Scholar] [CrossRef]
- Rzymski, P.; Poniedziałek, B.; Fal, A. Willingness to Receive the Booster COVID-19 Vaccine Dose in Poland. Vaccines 2021, 9, 1286. [Google Scholar] [CrossRef]
- Cines, D.B.; Bussel, J.B. SARS-CoV-2 vaccine–induced immune thrombotic thrombocytopenia. Mass. Med. Soc. 2021, 384, 2254–2256. [Google Scholar] [CrossRef]
- Al-Jayyousi, G.F.; Sherbash, M.A.M.; Ali, L.A.M.; El-Heneidy, A.; Alhussaini, N.W.Z.; Elhassan, M.E.A.; Nazzal, M.A. Factors Influencing Public Attitudes towards COVID-19 Vaccination: A Scoping Review Informed by the Socio-Ecological Model. Vaccines 2021, 9, 548. [Google Scholar] [CrossRef]
- Opel, D.J.; Mangione-Smith, R.; Taylor, J.A.; Korfiatis, C.; Wiese, C.; Catz, S.; Martin, D.P. Development of a survey to identify vaccine-hesitant parents: The parent attitudes about childhood vaccines survey. Hum. Vaccines 2011, 7, 419–425. [Google Scholar] [CrossRef]
- Dubé, E.; Laberge, C.; Guay, M.; Bramadat, P.; Roy, R.; Bettinger, J. Vaccine hesitancy: An overview. Hum. Vaccines Immunother. 2013, 9, 1763–1773. [Google Scholar] [CrossRef] [PubMed]
- Gewirtz-Meydan, A.; Mitchell, K.; Shlomo, Y.; Heller, O.; Grinstein-Weiss, M. COVID-19 Among Youth in Israel: Correlates of Decisions to Vaccinate and Reasons for Refusal. J. Adolesc. Health 2022, 70, 396–402. [Google Scholar] [CrossRef] [PubMed]
- Symons, X.; Matthews, S.; Tobin, B. Why should HCWs receive priority access to vaccines in a pandemic? BMC Med. Ethics 2021, 22, 79. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, L.H.; Drew, D.A.; Graham, M.S.; Joshi, A.D.; Guo, C.G.; Ma, W.; Mehta, R.S.; Warner, E.T.; Sikavi, D.R.; Lo, C.H.; et al. Risk of COVID-19 among front-line health-care workers and the general community: A prospective cohort study. Lancet Public Health 2020, 5, e475–e483. [Google Scholar] [CrossRef]
- Benjamanukul, S.; Traiyan, S.; Yorsaeng, R.; Vichaiwattana, P.; Sudhinaraset, N.; Wanlapakorn, N.; Poovorawan, Y. Safety and immunogenicity of inactivated COVID-19 vaccine in health care workers. J. Med. Virol. 2022, 94, 1442–1449. [Google Scholar] [CrossRef] [PubMed]
- Giannakou, K.; Kyprianidou, M.; Christofi, M.; Kalatzis, A.; Fakonti, G. Mandatory COVID-19 Vaccination for Healthcare Professionals and Its Association with General Vaccination Knowledge: A Nationwide Cross-Sectional Survey in Cyprus. Front. Public Health 2022, 10, 897526. [Google Scholar] [CrossRef] [PubMed]
- Giannakou, K.; Kyprianidou, M.; Heraclides, A. Attitudes and Determinants of Mandatory Vaccination against COVID-19 among the General Population of Cyprus: A Nationwide Cross-Sectional Study. Vaccines 2022, 10, 438. [Google Scholar] [CrossRef]
- Azak, E.; Karadenizli, A.; Uzuner, H.; Karakaya, N.; Canturk, N.Z.; Hulagu, S. Comparison of an inactivated Covid19 vaccine-induced antibody response with concurrent natural Covid19 infection. Int. J. Infect. Dis. 2021, 113, 58–64. [Google Scholar] [CrossRef]
- Dong, Y.; Dai, T.; Wei, Y.; Zhang, L.; Zheng, M.; Zhou, F. A systematic review of SARS-CoV-2 vaccine candidates. Signal Transduct. Target. Ther. 2020, 5, 237. [Google Scholar] [CrossRef]
- Kreps, S.; Prasad, S.; Brownstein, J.S.; Hswen, Y.; Garibaldi, B.T.; Zhang, B.; Kriner, D.L. Factors Associated with US Adults’ Likelihood of Accepting COVID-19 Vaccination. JAMA Netw. Open 2020, 3, e2025594. [Google Scholar] [CrossRef]
- Peters, M.D.J. Addressing vaccine hesitancy and resistance for COVID-19 vaccines. Int. J. Nurs. Stud. 2022, 131, 104241. [Google Scholar] [CrossRef]
- Temsah, M.H.; Barry, M.; Aljamaan, F.; Alhuzaimi, A.; Al-Eyadhy, A.; Saddik, B.; Alrabiaah, A.; Alsohime, F.; Alhaboob, A.; Alhasan, K.; et al. Adenovirus and RNA-based COVID-19 vaccines’ perceptions and acceptance among healthcare workers in Saudi Arabia: A national survey. BMJ Open 2021, 11, e048586. [Google Scholar] [CrossRef]
- Lin, Y.W.; Lin, C.H.; Lin, M.H. Vaccination distribution by community pharmacists under the COVID-19 vaccine appointment system in Taiwan. Cost Eff. Resour. Alloc. 2021, 19, 76. [Google Scholar] [CrossRef]
- Pfizer, B. Pfizer and BioNTech Announce Vaccine Candidate against COVID-19 Achieved Success in First Interim Analysis from Phase 3 Study; Pfizer: New York, NY, USA, 2020. [Google Scholar]
- Okubo, T.; Inoue, A.; Sekijima, K. Who Got Vaccinated for COVID-19? Evidence from Japan. Vaccines 2021, 9, 1505. [Google Scholar] [CrossRef]
- Alhasan, K.; Aljamaan, F.; Temsah, M.H.; Alshahrani, F.; Bassrawi, R.; Alhaboob, A.; Assiri, R.; Alenezi, S.; Alaraj, A.; Alhomoudi, R.I.; et al. COVID-19 Delta Variant: Perceptions, Worries, and Vaccine-Booster Acceptability among Healthcare Workers. Healthcare 2021, 9, 1566. [Google Scholar] [CrossRef]
- Lavallee, L.F.; Hatch, P.M.; Michalos, A.C.; McKinley, T. Development of the Contentment with Life Assessment Scale (CLAS): Using daily life experiences to verify levels of self-reported life satisfaction. Soc. Indic. Res. 2007, 83, 201–244. [Google Scholar] [CrossRef]
- Yang, J.; Liao, Y.; Hua, Q.; Lv, H. A Survey of Awareness of COVID-19 Knowledge, Willingness and Influencing Factors of COVID-19 Vaccination. Vaccines 2022, 10, 524. [Google Scholar] [CrossRef]
- Fobiwe, J.P.; Martus, P.; Poole, B.D.; Jensen, J.L.; Joos, S. Influences on Attitudes Regarding COVID-19 Vaccination in Germany. Vaccines 2022, 10, 658. [Google Scholar] [CrossRef]
- Wang, K.; Wong, E.L.; Ho, K.F.; Cheung, A.W.; Yau, P.S.; Dong, D.; Wong, S.Y.; Yeoh, E.K. Change of Willingness to Accept COVID-19 Vaccine and Reasons of Vaccine Hesitancy of Working People at Different Waves of Local Epidemic in Hong Kong, China: Repeated Cross-Sectional Surveys. Vaccines 2021, 9, 62. [Google Scholar] [CrossRef]
- Zhang, K.; Fang, Y.; Chan, P.S.; Cao, H.; Chen, H.; Hu, T.; Chen, Y.; Zhou, X.; Wang, Z. Behavioral Intention to Get a Booster Dose of COVID-19 Vaccine among Chinese Factory Workers. Int. J. Env. Res. Public Health 2022, 19, 5245. [Google Scholar] [CrossRef]
- Rahman, M.M.; Chisty, M.A.; Alam, M.A.; Sakib, M.S.; Quader, M.A.; Shobuj, I.A.; Halim, M.A.; Rahman, F. Knowledge, attitude, and hesitancy towards COVID-19 vaccine among university students of Bangladesh. PLoS ONE 2022, 17, e0270684. [Google Scholar] [CrossRef] [PubMed]
- Alhassan, R.K.; Aberese-Ako, M.; Doegah, P.T.; Immurana, M.; Dalaba, M.A.; Manyeh, A.K.; Klu, D.; Acquah, E.; Ansah, E.K.; Gyapong, M. COVID-19 vaccine hesitancy among the adult population in Ghana: Evidence from a pre-vaccination rollout survey. Trop. Med. Health 2021, 49, 96. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, A.E.; Allen, K.R.; Smith, J.Z. Divorced and separated parents during the COVID-19 pandemic. Fam. Process 2021, 60, 866–887. [Google Scholar] [CrossRef] [PubMed]
- Gallè, F.; Sabella, E.A.; Roma, P.; Da Molin, G.; Diella, G.; Montagna, M.T.; Ferracuti, S.; Liguori, G.; Orsi, G.B.; Napoli, C. Acceptance of COVID-19 Vaccination in the Elderly: A Cross-Sectional Study in Southern Italy. Vaccines 2021, 9, 1222. [Google Scholar] [CrossRef]
- Zhang, H.; Li, Y.; Peng, S.; Jiang, Y.; Jin, H.; Zhang, F. The effect of health literacy on COVID-19 vaccine hesitancy among community population in China: The moderating role of stress. Vaccine 2022, 40, 4473–4478. [Google Scholar] [CrossRef]
| Sociodemographic | GP N = 390 | HCWs N = 390 | |
|---|---|---|---|
| n (%) or median ± SD | n (%) or median ± SD | ||
| Age (Years) | 55.14 ± 17.35 | 35.13 ± 11.28 | |
| Sex | |||
| Male | 179(45.1) | 12(3.1) | |
| Female | 214(54.9) | 378(96.9) | |
| Status | |||
| Single | 132(33.8) | 267(68.5) | |
| Married | 199(51.1) | 110(28.2) | |
| Divorced | 59(15.1) | 13(3.3) | |
| Education | |||
| Primary school | 36(9.3) | 1(0.3) | |
| High school | 70(17.9) | 18(4.6) | |
| Diploma | 62(15.9) | 28(7.2) | |
| Bachelors | 169(43.3) | 307(78.7) | |
| Above Bachelors | 53(13.6) | 36(9.2) | |
| Occupation | |||
| HCWs | - | 390(100) | |
| Government office | 137(35.2) | - | |
| Private office | 70(17.9) | - | |
| Non-office employee | 32(8.2) | - | |
| Entrepreneur | 75(19.2) | - | |
| Housewife | 76(19.5) | - | |
| Risk of contracting COVID-19 | |||
| Risk exposure: isolation | 34(8.7) | 181(46.4) | |
| Risk exposure: no isolation | 30(7.7) | 117(30.0) | |
| Not sure | 53(13.6) | 26(6.7) | |
| Never at risk | 273(70.0) | 66(16.9) | |
| Vaccination history | |||
| 1st dose | |||
| Inactivated vaccine | 25(6.4) | 324(83.1) | |
| Viral vector vaccine | 364(93.3) | 48(12.3) | |
| mRNA vaccine | 1(0.3) | 18(4.6) | |
| 2nd dose | |||
| None | 19(4.9) | 2(0.5) | |
| Inactivated vaccine | 26(6.6) | 323(82.8) | |
| Viral vector vaccine | 345(88.5) | 41(10.5) | |
| mRNA vaccine | 0 | 24(6.2) | |
| 3rd dose | |||
| None | 350(89.7) | 64(16.4) | |
| Inactivated vaccine | 15(3.8) | 6(1.5) | |
| Viral vector vaccine | 18(4.7) | 102(26.2) | |
| mRNA vaccine | 7(1.8) | 218(55.9) | |
| Satisfaction Items | GP | HCWs |
|---|---|---|
| Median ± SD | Median ± SD | |
| Vaccination booster type | ||
| 1. I am satisfied with inactivated vaccine. | 1.25 ± 0.92 | 1.39 ± 0.60 |
| 2. I am satisfied with the viral vector vaccine. | 2.14 ± 1.00 | 1.83 ± 0.63 |
| 3. I have confidence in the quality of the available vaccines. | 1.92 ± 1.05 | 1.65 ± 0.65 |
| 4. I have a good knowledge and understanding of vaccines that have been determined to be of good quality. | 1.91 ± 0.99 | 2.05 ± 0.65 |
| 5. If possible, I will select a viral vector vaccine | 2.09 ± 1.14 | 2.14 ± 0.78 |
| Vaccination booster management | ||
| 6. There are sufficient inactivated vaccine doses for the Thai population | 1.52 ± 1.01 | 1.75 ± 0.73 |
| 7. There are sufficient viral vector vaccine doses for the Thai population | 1.73 ± 1.01 | 1.60 ± 0.65 |
| 8. The registration for injection of inactivated vaccine will be conducted on time (No delay) | 1.50 ± 1.00 | 1.72 ± 0.70 |
| 9. The registration for injection of viral vector vaccine will be conducted on time (No delay) | 1.92 ± 1.08 | 1.71 ± 0.65 |
| 10. Each vaccine allocation is distributed across all areas. | 1.52 ± 0.98 | 1.47 ± 0.60 |
| 11. The government’s credibility in procuring and administering vaccines | 1.48 ± 1.16 | 1.43 ± 0.60 |
| Satisfactions with vaccine booster | ||
| 12. I am satisfied with the type and efficacy of the inactivated vaccine. | 1.58 ± 1.01 | 1.72 ± 0.63 |
| 13. I am satisfied with the type and efficacy of the viral vector vaccine | 1.85 ± 1.11 | 2.50 ± 0.64 |
| 14. I am satisfied with the type and efficacy of the mRNA vaccine. | 1.73 ± 1.09 | 2.37 ± 0.63 |
| 15. I am satisfied with the vaccine cost | 1.45 ± 0.95 | 1.71 ± 0.63 |
| Population | Satisfactions on COVID-19 Vaccine Booster | |||
|---|---|---|---|---|
| Median ± SD | t | p | 95% CI | |
| GP | 25.65 ± 12.36 | −2.091 | 0.037 | −2.80, −0.087 |
| HCWs | 27.10 ± 5.85 | |||
| Vaccine Types | Satisfaction Scores | |||||
|---|---|---|---|---|---|---|
| GP | HCWs | t | p | 95% CI | ||
| Median ± SD | Median ± SD | |||||
| 1st dose vaccination | ||||||
| No vaccine | - | - | - | - | - | |
| Inactivated vaccine | 26.16 ± 11.93 | 27.17 ± 5.79 | −0.422 | 0.677 | −5.97, 3.94 | |
| Viral vector vaccine | 25.65 ± 12.40 | 27.16 ± 5.80 | −1.422 | 0.158 | −3.60, 0.59 | |
| mRNA vaccine | - | - | - | - | - | |
| 2nd dose vaccination booster | ||||||
| No vaccine | 30.15 ± 9.63 | 27.50 ± 14.84 | 0.248 | 0.843 | −109.63, 114.950 | |
| Inactivated vaccine | 26.11 ± 12.22 | 27.15 ± 5.75 | −0.431 | 0.670 | −6.015, 3.93 | |
| Viral vector vaccine | 25.37 ± 12.48 | 27.56 ± 5.83 | −1.93 | 0.056 | −4.43, 0.058 | |
| mRNA vaccine | - | - | - | - | - | |
| 3rd dose vaccination booster | ||||||
| No vaccine | 25.54 ± 12.42 | 27.03 ± 6.42 | −1.422 | 0.157 | −3.54, 0.57 | |
| Inactivated vaccine | 24.80 ± 14.87 | 29.00 ± 7.23 | −0.867 | 0.398 | −14.38, 5.98 | |
| Viral vector vaccine | 27.33 ± 11.76 | 30.28 ± 5.63 | −1.043 | 0.310 | −8.88, 2.98 | |
| mRNA vaccine | 28.42 ± 1.51 | 25.58 ± 5.12 | 4.256 | 0.001 | 1.37, 4.31 | |
| Variable | GP | HCWs | |||
|---|---|---|---|---|---|
| β (95% CI) | p | β (95% CI) | p | ||
| Sex | |||||
| Male | Ref. | Ref. | |||
| Female | −0.025 (−3.167, 1.924) | 0.631 | −0.019 (−3.861, 2.605) | 0.703 | |
| Status | |||||
| Single | Ref. | Ref. | |||
| Married | 0.047 (−1.653, 3.979) | 0.417 | 0.157 (0.794, 3.278) | 0.001 | |
| Divorced | −0.068 (−6.252, 1.556) | 0.238 | 0.198 (3.303, 9.596) | <0.001 | |
| Education | |||||
| ≥ Bachelor’s degree | Ref. | Ref. | |||
| < Bachelor’s degree | −0.042 (−3.59, 1.517) | 0.424 | 0.070 (−0.479, 2.989) | 0.155 | |
| Risk of contracting COVID-19 | |||||
| Never at risk | Ref. | Ref. | |||
| Not sure | −0.008 (−3.839, 3.406) | 0.906 | −0.031 (−3.028, 2.066) | 0.711 | |
| Risk exposure: no isolation | −0.159 (−12.867, −1.877) | 0.009 | −0.206 (−5.013, −0.242) | 0.031 | |
| Risk exposure: isolation | 0.045 (−3.386, 7.334) | 0.469 | −0.282 (−5.627, −0.990) | 0.005 | |
| Vaccination history | |||||
| 1st dose | Ref. | Ref. | |||
| 2nd dose | −0.304 (−1.303, 0.694) | 0.549 | −0.510 (−1.391, 0.371) | 0.256 | |
| 3rd dose | 0.180 (−0.645, 1.005) | 0.668 | −0.844 (−1.177, −0.512) | <0.001 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kunno, J.; Yubonpunt, P.; Sumanasrethakul, C.; Kaewchandee, C.; Robson, M.G.; Wanichnopparat, W.; Prasittichok, K.; Luangwilai, T.; Chaichan, C.; Krainara, P.; et al. Satisfaction with COVID-19 Vaccines in Health Care Workers and the General Population: A Cross-Sectional Study in Urban Bangkok, Thailand. Vaccines 2022, 10, 1345. https://doi.org/10.3390/vaccines10081345
Kunno J, Yubonpunt P, Sumanasrethakul C, Kaewchandee C, Robson MG, Wanichnopparat W, Prasittichok K, Luangwilai T, Chaichan C, Krainara P, et al. Satisfaction with COVID-19 Vaccines in Health Care Workers and the General Population: A Cross-Sectional Study in Urban Bangkok, Thailand. Vaccines. 2022; 10(8):1345. https://doi.org/10.3390/vaccines10081345
Chicago/Turabian StyleKunno, Jadsada, Pataraporn Yubonpunt, Chavanant Sumanasrethakul, Chuthamat Kaewchandee, Mark Gregory Robson, Wachiraporn Wanichnopparat, Krit Prasittichok, Titaporn Luangwilai, Chonlawat Chaichan, Patcharaporn Krainara, and et al. 2022. "Satisfaction with COVID-19 Vaccines in Health Care Workers and the General Population: A Cross-Sectional Study in Urban Bangkok, Thailand" Vaccines 10, no. 8: 1345. https://doi.org/10.3390/vaccines10081345
APA StyleKunno, J., Yubonpunt, P., Sumanasrethakul, C., Kaewchandee, C., Robson, M. G., Wanichnopparat, W., Prasittichok, K., Luangwilai, T., Chaichan, C., Krainara, P., & Supawattanabodee, B. (2022). Satisfaction with COVID-19 Vaccines in Health Care Workers and the General Population: A Cross-Sectional Study in Urban Bangkok, Thailand. Vaccines, 10(8), 1345. https://doi.org/10.3390/vaccines10081345







