Safety and Humoral and Cellular Immunogenicity of the BNT162b2 SARS-CoV-2 Vaccine in Liver-Transplanted Adolescents Compared to Healthy Adolescents
Abstract
:1. Introduction
2. Methods
2.1. Study Design and Target Population
2.2. Adverse Effects
2.3. Immunogenicity Study
2.4. Vitamin D Study
2.5. Statistical Analysis
3. Results
3.1. Baseline Characteristics of the Liver-Transplanted and Healthy Adolescents
3.2. Immunogenicity of the BNT162b2 Vaccine
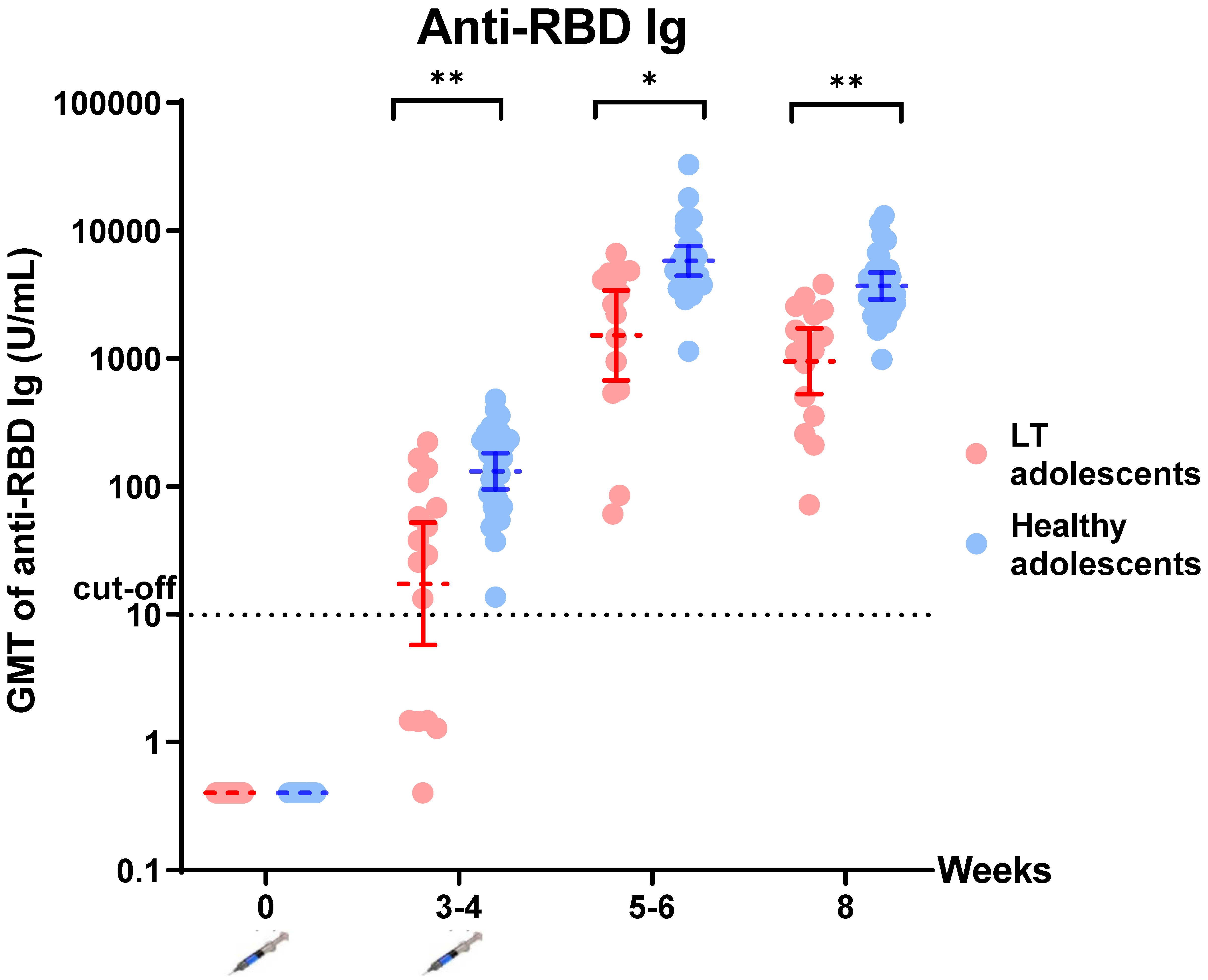
3.2.1. Humoral Response
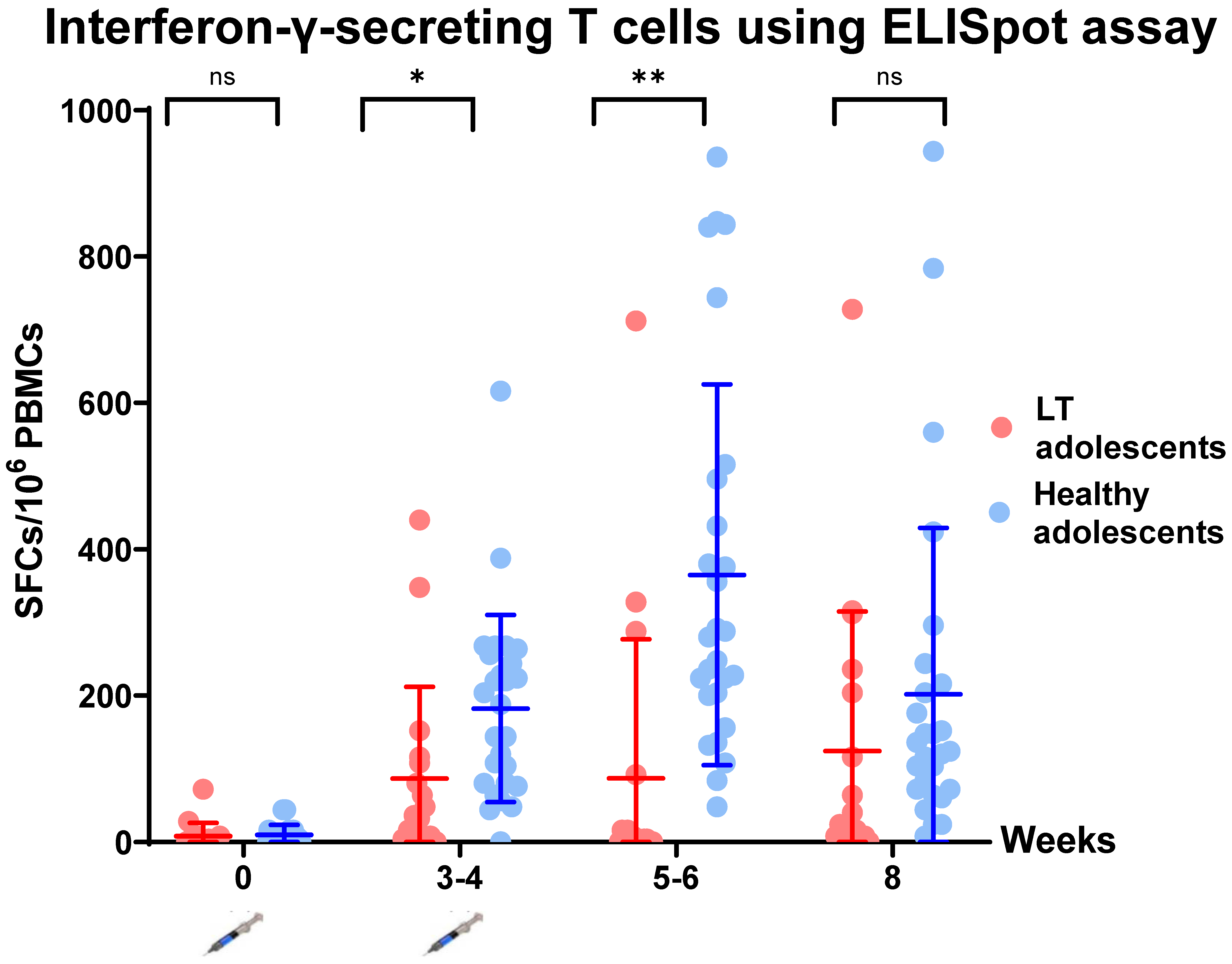
3.2.2. Cellular Response
3.3. Factors Associated with the Immunologic Response to BNT162b2 Administration in Liver-Transplanted Adolescents
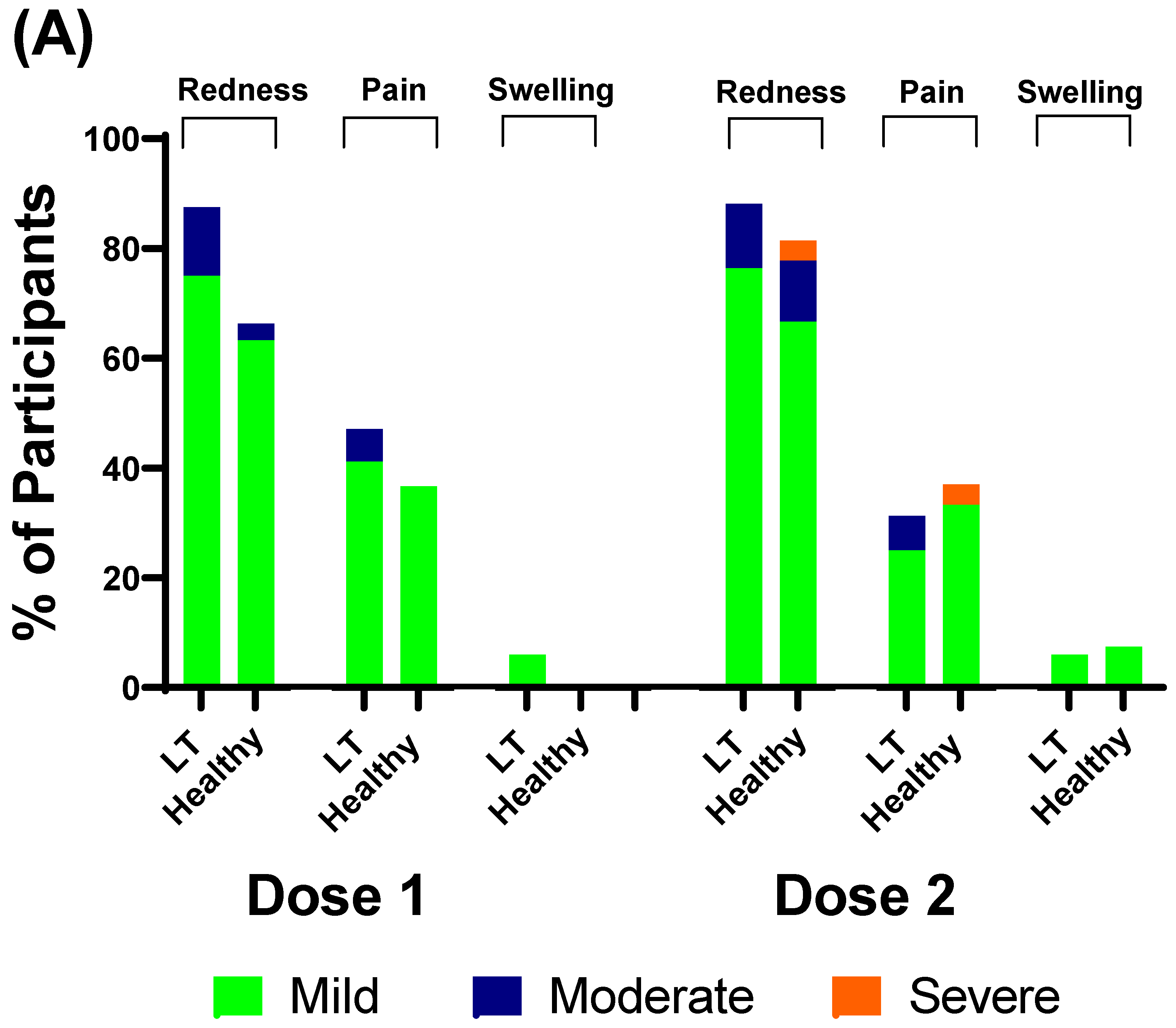
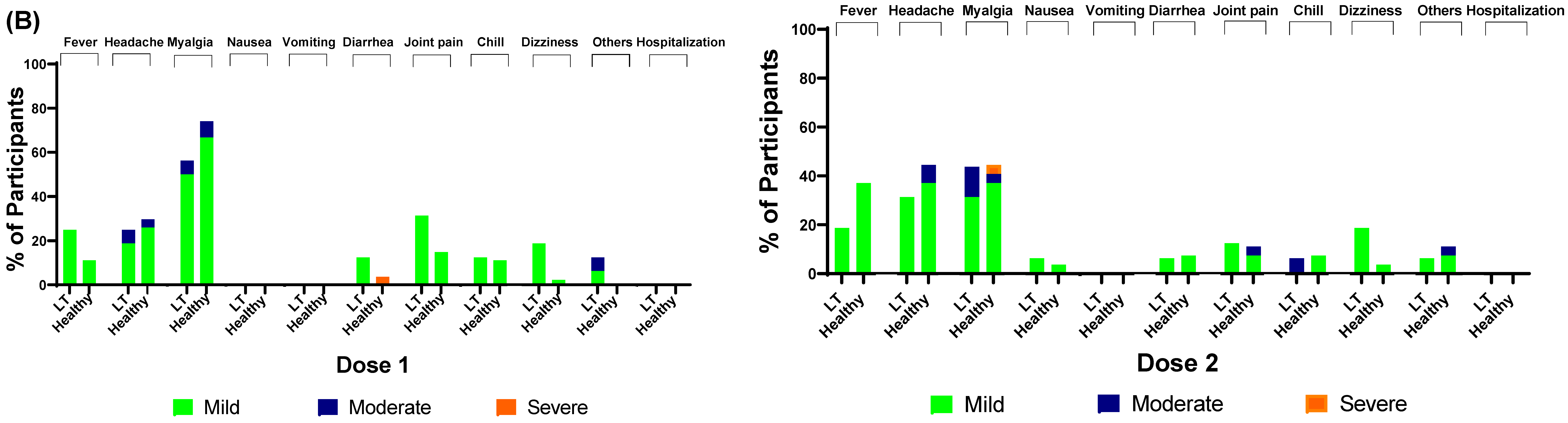
3.4. Safety of BNT162b2
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| LT | liver transplant |
| RBD | receptor-binding domain |
| sVNT | surrogate virus-neutralizing antibody |
| SARS-CoV-2 | Severe acute respiratory syndrome coronavirus 2 |
| anti-N | Anti-nucleocapsid |
| GMT | geometric mean titer |
References
- Bai, Y.; Yao, L.; Wei, T.; Tian, F.; Jin, D.Y.; Chen, L.; Wang, M. Presumed Asymptomatic Carrier Transmission of COVID-19. JAMA 2020, 323, 1406–1407. [Google Scholar] [CrossRef] [PubMed]
- WHO. Archived: WHO Timeline–COVID-19; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- World Health Organization. 2022 S. WHO Coronavirus (COVID-19) Dashboard. 2022. Available online: http://covid19who.int/ (accessed on 5 August 2022).
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Perez Marc, G.; Moreira, E.D.; Zerbini, C.; et al. Safety and Efficacy of the BNT162b2 mRNA COVID-19 Vaccine. N. Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef] [PubMed]
- Pandemic. CC-uFaP-BC-Vfeuiaiaiaifa. News Release of the Food and Drug Administration, Siver Spring, MD. 10 May 2021. Available online: https://wwwfdagov/news-events/press-announcements/coronavirus-covid-19-update-fda-authorizes-pfizer-biontech-covid19-vaccine-emergency-use (accessed on 5 August 2022).
- Spearman, C.W.; Aghemo, A.; Valenti, L.; Sonderup, M.W. COVID-19 and the liver: A 2021 update. Liver Int. 2021, 41, 1988–1998. [Google Scholar] [CrossRef] [PubMed]
- Cornberg, M.; Buti, M.; Eberhardt, C.S.; Grossi, P.A.; Shouval, D. EASL position paper on the use of COVID-19 vaccines in patients with chronic liver diseases, hepatobiliary cancer and liver transplant recipients. J. Hepatol. 2021, 74, 944–951. [Google Scholar] [CrossRef] [PubMed]
- Downes, K.J.; Statler, A.V.; Orscheln, R.C.; Cousino, M.K.; Green, M.; Michaels, M.G.; Muller, W.J.; Sharma, T.S.; Danziger-Isakov, A.L.; Ardura, I.M. Return to School and COVID-19 Vaccination for Pediatric Solid Organ Transplant Recipients in the United States: Expert Opinion for 2021-2022. J. Pediatr. Infect. Dis. Soc. 2021, 11, 43–54. [Google Scholar] [CrossRef]
- Yorsaeng, R.; Suntronwong, N.; Phowatthanasathian, H.; Assawakosri, S.; Kanokudom, S.; Thongmee, T.; Vichaiwattana, P.; Auphimai, C.; Wongsrisang, L. Immunogenicity of a third dose viral-vectored COVID-19 vaccine after receiving two-dose inactivated vaccines in healthy adults. Vaccine 2022, 40, 524–530. [Google Scholar] [CrossRef]
- Kanokudom, S.; Assawakosri, S.; Suntronwong, N.; Auphimai, C.; Nilyanimit, P.; Vichaiwattana, P.; Thongmee, T.; Yorsaeng, R.; Srimuan, D.; Thatsanatorn, T.; et al. Safety and Immunogenicity of the Third Booster Dose with Inactivated, Viral Vector, and mRNA COVID-19 Vaccines in Fully Immunized Healthy Adults with Inactivated Vaccine. Vaccines 2022, 10, 86. [Google Scholar] [CrossRef]
- Rabinowich, L.; Grupper, A.; Baruch, R.; Ben-Yehoyada, M.; Halperin, T.; Turner, D.; Katchman, E.; Levi, S.; Houri, I.; Lubezky, N.; et al. Low immunogenicity to SARS-CoV-2 vaccination among liver transplant recipients. J. Hepatol. 2021, 75, 435–438. [Google Scholar] [CrossRef]
- Davidov, Y.; Tsaraf, K.; Cohen-Ezra, O.; Likhter, M.; Ben Yakov, G.; Levy, I.; Levin, E.G.; Lustig, Y.; Mor, O.; Rahav, G.; et al. Immunogenicity and Adverse Effects of the 2-Dose BNT162b2 Messenger RNA Vaccine Among Liver Transplantation Recipients. Liver Transpl. 2022, 28, 215–223. [Google Scholar] [CrossRef]
- Rashidi-Alavijeh, J.; Frey, A.; Passenberg, M.; Korth, J.; Zmudzinski, J.; Anastasiou, O.; Saner, F.; Jahn, M.; Lange, C.; Willuweit, K. Humoral Response to SARS-CoV-2 Vaccination in Liver Transplant Recipients–A Single-Center Experience. Vaccines 2021, 9, 738. [Google Scholar] [CrossRef]
- Guarino, M.; Esposito, I.; Portella, G.; Cossiga, V.; Loperto, I.; Tortora, R.; Cennamo, M.; Capasso, M.; Terracciano, D.; Lanza, A.G.; et al. Humoral Response to 2-dose BNT162b2 mRNA COVID-19 Vaccination in Liver Transplant Recipients. Clin. Gastroenterol. Hepatol. 2022, 20, 1534–1541.e4. [Google Scholar] [CrossRef] [PubMed]
- Qin, C.X.; Auerbach, S.R.; Charnaya, O.; Danziger-Isakov, L.A.; Ebel, N.H.; Feldman, A.G.; Hsu, E.K.; McAteer, J.; Mohammad, S.; Perito, E.R.; et al. Antibody response to 2-dose SARS-CoV-2 mRNA vaccination in pediatric solid organ transplant recipients. Am. J. Transpl. 2022, 22, 669–672. [Google Scholar] [CrossRef] [PubMed]
- Sadarangani, M.; Marchant, A.; Kollmann, T.R. Immunological mechanisms of vaccine-induced protection against COVID-19 in humans. Nat. Rev. Immunol. 2021, 21, 475–484. [Google Scholar] [CrossRef] [PubMed]
- DiLillo, D.J.; Tan, G.; Palese, P.; Ravetch, J.V. Broadly neutralizing hemagglutinin stalk–specific antibodies require FcγR interactions for protection against influenza virus in vivo. Nat. Med. 2014, 20, 143–151. [Google Scholar] [CrossRef] [PubMed]
- Excler, J.L.; Ake, J.; Robb, M.L.; Kim, J.H.; Plotkin, S.A. Nonneutralizing functional antibodies: A new “old” paradigm for HIV vaccines. Clin. Vaccine Immunol. 2014, 21, 1023–1036. [Google Scholar] [CrossRef]
- Assawasaksakul, T.; Lertussavavivat, T.; Sathitratanacheewin, S.; Oudomying, N.; Vichaiwattana, P.; Wanlapakorn, N.; Poovorawan, Y.; Avihingsanon, Y.; Assawasaksakul, N.; Buranapraditkun, S.; et al. Comparison of Immunogenicity and Safety of Inactivated, Adenovirus-Vectored, and Heterologous Adenovirus-Vectored/mRNA Vaccines in Patients with Systemic Lupus Erythematosus and Rheumatoid Arthritis: A Prospective Cohort Study. Vaccines 2022, 10, 853. [Google Scholar] [CrossRef]
- Buescher, G.; Sebode, M.; Marjot, T.; Webb, G.J.; Moon, A.M.; Barnes, E.; Barritt, A.S., IV; Cananzi, M.; Lohse, A.W.; Jorgensen, M.H.; et al. SARS-CoV-2 in Pediatric Liver Transplant Recipients: The European Experience. J. Pediatr. Gastroenterol. Nutr. 2022, 74, e41–e42. [Google Scholar] [CrossRef]
- Kehar, M.; Ebel, N.; Ng, V.; Lobritto, S.; Martinez, M. Updates from the NASPGHAN/SPLIT SARS-CoV2 International Registry. J. Pediatr. Gastroenterol. Nutr. 2022, 74, e43–e44. [Google Scholar] [CrossRef]
- Frenck, R.W., Jr.; Klein, N.P.; Kitchin, N.; Gurtman, A.; Absalon, J.; Lockhart, S.; Perez, J.L.; Walter, E.B.; Senders, S.; Bailey, R.; et al. Safety, Immunogenicity, and Efficacy of the BNT162b2 COVID-19 Vaccine in Adolescents. N. Engl. J. Med. 2021, 385, 239–250. [Google Scholar] [CrossRef]
- Shroff, H.; Satapathy, S.K.; Crawford, J.M.; Todd, N.J.; VanWagner, L.B. Liver injury following SARS-CoV-2 vaccination: A multicenter case series. J. Hepatol. 2022, 76, 211–214. [Google Scholar] [CrossRef]
- Dumortier, J. Liver injury after mRNA-based SARS-CoV-2 vaccination in a liver transplant recipient. Clin. Res. Hepatol. Gastroenterol. 2022, 46, 101743. [Google Scholar] [CrossRef] [PubMed]
- Merzon, E.; Tworowski, D.; Gorohovski, A.; Vinker, S.; Cohen, A.G.; Green, I.; Frenkel-Morgenstern, M. Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: An Israeli population-based study. FEBS J. 2020, 287, 3693–3702. [Google Scholar] [CrossRef] [PubMed]
- De Smet, D.; De Smet, K.; Herroelen, P.; Gryspeerdt, S.; Martens, G.A. Serum 25(OH)D Level on Hospital Admission Associated With COVID-19 Stage and Mortality. Am. J. Clin. Pathol. 2021, 155, 381–388. [Google Scholar] [CrossRef] [PubMed]
- Laird, E.; Rhodes, J.; Kenny, A.R. Vitamin D and Inflammation: Potential Implications for Severity of COVID-19. Ir. Med. J. 2020, 113, 81. [Google Scholar] [PubMed]
- Lee, M.-D.; Lin, C.-H.; Lei, W.-T.; Chang, H.-Y.; Lee, H.-C.; Yeung, C.-Y.; Chiu, N.-C.; Chi, H.; Liu, J.-M.; Hsu, R.-J.; et al. Does Vitamin D Deficiency Affect the Immunogenic Responses to Influenza Vaccination? A Systematic Review and Meta-Analysis. Nutrients 2018, 10, 409. [Google Scholar] [CrossRef] [PubMed]
- Chiu, S.K.; Tsai, K.W.; Wu, C.C.; Zheng, C.M.; Yang, C.H.; Hu, W.C.; Hou, Y.C.; Lu, K.C.; Chao, Y.C. Putative Role of Vitamin D for COVID-19 Vaccination. Int. J. Mol. Sci. 2021, 22, 8988. [Google Scholar] [CrossRef]
- Keam, S.J. Tixagevimab + Cilgavimab: First approval. Drugs 2022, 82, 1001–1010. [Google Scholar] [CrossRef]
- Machhi, J.; Shahjin, F.; Das, S.; Patel, M.; Abdelmoaty, M.M.; Cohen, J.D.; Singh, P.A.; Baldi, A.; Bajwa, N.; Kumar, R.; et al. Nanocarrier vaccines for SARS-CoV-2. Adv. Drug Deliv. Rev. 2021, 171, 215–239. [Google Scholar] [CrossRef]

| Parameter | Liver-Transplanted Adolescents (n = 16) | Healthy Adolescents (n = 27) | p Value |
|---|---|---|---|
| Age, years (mean ± SD) | 14.59 (1.78) | 14.67 (1.57) | 0.441 |
| Male gender, n (%) | 7 (43.8) | 12 (44.4) | 0.609 |
| Body mass index (kg/m2) (mean ± SD) | 18.59 (2.52) | 19.62 (4.27) | 0.399 |
| Underlying disease for LT, n (%) | - | - | |
| Biliary atresia | 9 (56.25) | ||
| Budd–Chiari syndrome | 1 (6.25) | ||
| Alagille syndrome | 2 (12.5) | ||
| Biliary hypoplasia | 1 (6.25) | ||
| Citrullinemia | 1 (6.25) | ||
| Autoimmune hepatitis | 1 (6.25) | ||
| Cryptogenic cirrhosis | 1 (6.25) | ||
| Time from liver transplant to BNT162b2 vaccination (years) (mean ± SD) | 7.18 (5.12) | - | - |
| History of graft rejection, n (%) | 4 (25) | - | - |
| Type of immunosuppressant, n (%) | - | - | |
| Tacrolimus (calcineurin inhibitor) | 10 (62.5) | ||
| Cyclosporin (calcineurin inhibitor) | 6 (37.5) | ||
| Sirolimus (mTOR) | 1 (6.25) | ||
| MMF (antimetabolite) | 4 (25) | ||
| Prednisolone | 2 (12.5) | ||
| Azathioprine | 1 (6.25) | ||
| Immunosuppressant used (n), n (%) | |||
| 1 | 10 (62.5) | ||
| 2 | 4 (25) | ||
| 3 | 2 (12.5) | ||
| Basic laboratory data (mean ± SD) | - | ||
| Hb (g/L) | 135.12 (22.31) | ||
| WBC (103/µL) | 5.38 (1.69) | ||
| Absolute neutrophil counts | 2830 (910) | ||
| Absolute lymphocyte counts | 2000 (890) | ||
| Platelet (103/microL) | 203.94 (60.86) | ||
| Total bilirubin (µmol/L) | 21.38 (17.96) | ||
| SGOT (U/L) | 47.94 (47.74) | ||
| SGPT (U/L) | 51.88 (43.11) | ||
| GGT (U/L) | 134.62 (213.14) | ||
| Albumin (g/L) | 43.12 (2.82) | ||
| Total 25OH vitamin D level (nmol/L) | 47.92 (38.06, 82.74) | 38.69 (29.2, 52.42) | 0.074 |
| Immunogenic response and duration from first visit (days) | |||
| Visit 1 (1st vaccination) (mean ± SD) | - | - | - |
| GMT of anti-RBD Ig (U/mL) | 0.4 | 0.4 | - |
| IFN-γ-secreting cells (SFCs/106PBMCs) | 8 (−1.197 to 17.197) | 9.63 (4.25 to 15.01) | 0.734 |
| Visit 2 (2nd vaccination), days (mean ± SD) | 21.3 (1.25) | 28 (0) | <0.001 |
| GMT of anti-RBD Ig (U/mL) | 15.85 (5.25–47.87) | 224.74 (126.60–398.93) | 0.001 |
| IFN-γ-secreting cells (SFCs/106PBMCs) | 86.59 (22.174 to 151.003) | 182.37 (131.71 to 233.04) | 0.019 |
| Visit 3, days (mean ± SD) | 34.93 (2.15) | 42.07 (0.55) | <0.001 |
| GMT of anti-RBD Ig (U/mL) | 1511.37 (720.22–3171.59) | 6311.90 (4955.46–8039.64) | 0.009 |
| IFN-γ-secreting cells (SFCs/106PBMCs) | 86.82 (−10.935 to 184.582) | 365.04 (260.134 to 467.94) | <0.001 |
| Visit 4, days (mean ± SD) | 55.75 (1.87) | 56.56 (1.80) | 0.08 |
| GMT of anti-RBD Ig (U/mL) | 948.21 (550.05–1634.59) | 4087.07 (3256.19–5129.97) | <0.001 |
| IFN-γ-secreting cells (SFCs/106PBMCs) | 124.24 (26.105 to 222.366) | 201.92 (227.293 to 291.84) | 0.247 |
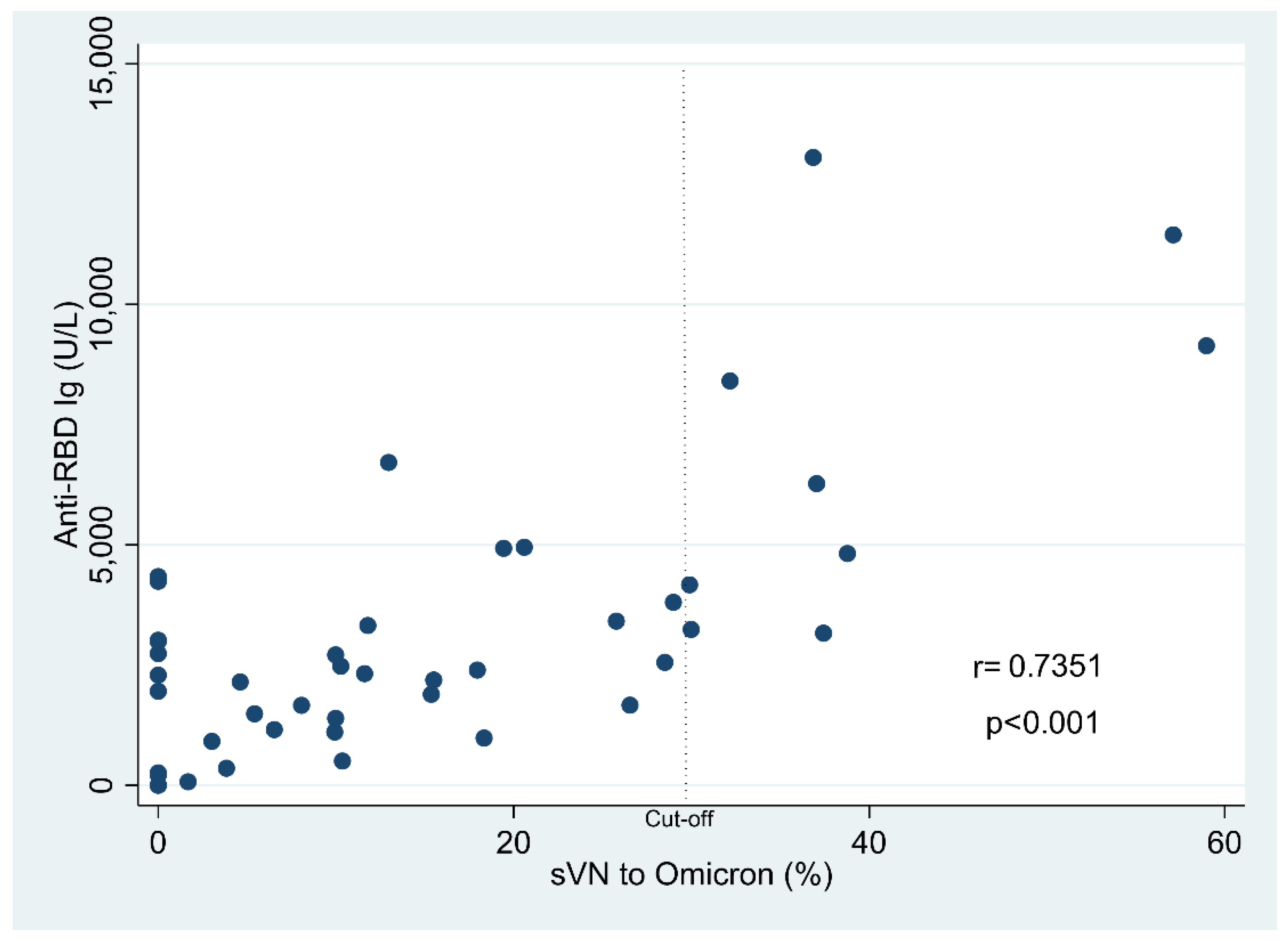
| sVNT to Omicron variant (%) | 8.23 (2.35, 16.73) | 15.36 (4.61, 19.44) | 0.066 |
| positive | 0/16 | 9/27 | 0.016 |
| Anti-N IgG | |||
| positive | 0 | 0 | - |
| Parameter | Liver-Transplanted Adolescents (n = 16) | p Value | |
|---|---|---|---|
| Anti-RBD IgG <550 U/L (n = 4) | Anti-RBD IgG ≥550 U/L | ||
| (n = 12) | |||
| Age, years (mean ± SD) | 15.30 (2.29) | 14.34 (0.46) | 0.368 |
| Male gender, n (%) | 1 (25) | 6 (50) | 0.585 |
| Body mass index (kg/m2) (mean ± SD) | 19.72 (2.71) | 18.31 (2.52) | 0.404 |
| Time from LT to BNT162b2 vaccination (years) (mean ± SD) | 7.99 (4.91) | 7.73 (5.42) | 0.931 |
| History of graft rejection, n (%) | 3 (75) | 1 (8.33) | 0.027 |
| Type of Immunosuppressant, n (%) | |||
| Tacrolimus (calcineurin inhibitor) | 3 (75) | 6 (50) | 0.585 |
| Cyclosporin (calcineurin inhibitor) | 2 (50) | 5 (41.67) | 1 |
| Sirolimus (mTor) | 1 (25) | 0 | - |
| MMF (antimetabolite) | 2 (50) | 2 (16.67) | 0.245 |
| Prednisolone | 3 (75) | 0 (0) | 0.007 |
| Azathioprine | 1 (25) | 1 (8.33) | 0.45 |
| Immunosuppressant used (n), n (%) | 0.003 | ||
| 1 | 0 (0) | 9 (75) | 0.019 |
| 2 | 1 (25) | 3 (25) | 1 |
| 3 | 3 (75) | 0 | 0.007 |
| Basic laboratory data (mean ± SD) | |||
| Hb (g/L) | 124.50 (21.98) | 138.58 (22.23) | 0.29 |
| WBC (103/µL) | 5.52 (1.45) | 5.34 (1.83) | 0.858 |
| Absolute neutrophil counts | 3090.31 (1368.22) | 2744.12 (767.00) | 0.529 |
| Absolute lymphocyte counts | 1920.34 (550.74) | 2030.43 (994.68) | 0.838 |
| Platelet (103/microL) | 220.50 (58.95) | 198.42 (63.01) | 0.548 |
| Total bilirubin (µmol/L) | 15.39 (6.84) | 23.26 (20.18) | 0.467 |
| SGPT (U/L) | 104.5 (46.34) | 34.33 (24.61) | 0.001 |
| SGOT (U/L) | 106.5 (65.40) | 28.42 (16.70) | 0.001 |
| GGT (U/L) | 276.75 (336.96) | 87.25 (145.57) | 0.127 |
| Albumin (g/L) | 42.75 (3.60) | 43.25 (2.67) | 0.769 |
| Total 25OH vitamin D level (nmol/L) | 42.31 (9.86) | 60.85 (25.36) | 0.134 |
| sVNT to Omicron (%) | 1.38 (1.82) | 13.56 (10.00) | 0.033 |
| Factors | Difference * | 95% CI | |
|---|---|---|---|
| Duration from LT to vaccination | |||
| <3 years | Ref | ||
| >3 years | 7.875 | 0.745–15.005 | 0.03 |
| Immunosuppression | |||
| Monotherapy | Ref | ||
| Combined therapy | |||
| 2 drugs | −8.503 | −18.231–1.224 | 0.087 |
| 3 drugs | −14.373 | −26.001–2.747 | 0.015 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sintusek, P.; Buranapraditkun, S.; Khunsri, S.; Saengchaisukhonkit, V.; Vichaiwattana, P.; Srimuan, D.; Thongmee, T.; Poovorawan, Y. Safety and Humoral and Cellular Immunogenicity of the BNT162b2 SARS-CoV-2 Vaccine in Liver-Transplanted Adolescents Compared to Healthy Adolescents. Vaccines 2022, 10, 1324. https://doi.org/10.3390/vaccines10081324
Sintusek P, Buranapraditkun S, Khunsri S, Saengchaisukhonkit V, Vichaiwattana P, Srimuan D, Thongmee T, Poovorawan Y. Safety and Humoral and Cellular Immunogenicity of the BNT162b2 SARS-CoV-2 Vaccine in Liver-Transplanted Adolescents Compared to Healthy Adolescents. Vaccines. 2022; 10(8):1324. https://doi.org/10.3390/vaccines10081324
Chicago/Turabian StyleSintusek, Palittiya, Supranee Buranapraditkun, Siriporn Khunsri, Varattaya Saengchaisukhonkit, Preeyaporn Vichaiwattana, Donchida Srimuan, Thanunrat Thongmee, and Yong Poovorawan. 2022. "Safety and Humoral and Cellular Immunogenicity of the BNT162b2 SARS-CoV-2 Vaccine in Liver-Transplanted Adolescents Compared to Healthy Adolescents" Vaccines 10, no. 8: 1324. https://doi.org/10.3390/vaccines10081324
APA StyleSintusek, P., Buranapraditkun, S., Khunsri, S., Saengchaisukhonkit, V., Vichaiwattana, P., Srimuan, D., Thongmee, T., & Poovorawan, Y. (2022). Safety and Humoral and Cellular Immunogenicity of the BNT162b2 SARS-CoV-2 Vaccine in Liver-Transplanted Adolescents Compared to Healthy Adolescents. Vaccines, 10(8), 1324. https://doi.org/10.3390/vaccines10081324







