Abstract
Providing both personal and social benefits, vaccination may be motivated by collective responsibility (CR). Some previous studies have indicated the relationship between CR and vaccination but could not exclude confounding bias and had little knowledge about the boundary conditions. This study aimed to examine the association between CR and COVID-19 vaccine uptake and its boundary conditions in an extended version of the theory of planned behavior. A cross-sectional survey with 608 participants from six tourism satellite industries in Macao was conducted from 28 July 2021 to 20 August of 2021. Respondentss in CR-lower and CR-higher groups were 1:1 paired using propensity score matching (PSM) to control the potential confounding factors. Results showed participants in the CR-higher group reported significantly higher COVID-19 vaccine uptake than those in the CR-lower group (64.7% vs. 49.7%, p = 0.005). Multivariate logistic regression results indicated a positive association between CR and COVID-19 vaccine uptake (p = 0.012, OR = 2.070, 95% CI= 1.174 to 3.650) and its interaction effect with COVID-19 vaccine attitude (p = 0.019, OR = 0.922, 95% CI = 0.861 to 0.987). Spotlight analysis further illustrated that CR was more effective among individuals with a more negative COVID-19 vaccine attitude. These findings may help promote understanding of vaccine hesitancy, and hence optimize vaccination communication strategies during the COVID-19 pandemic.
1. Introduction
The coronavirus disease 2019 (COVID-19) pandemic has deeply impacted human lives in multiple aspects and resulted in above 6.3 million deaths across 220 countries as of 9th July 2022 [1]. Reliable evidence indicates that vaccination remains the safest and most effective strategy to prevent COVID-19 infections, hospitalizations, and death [2]. However, hesitancy and reluctance about COVID-19 vaccine injections were still observed among some populations worldwide [3,4]. Vaccine hesitancy was listed among the top ten threats to global health by the WHO [5]. Many previous studies have applied health behavior theories, theory of reasoned action (TRA), or theory of planned behavior (TPB) in particular [6,7], attempting to address this problem. In addition, since vaccination not only provides a direct personal benefit to the vaccinated individual but also indirectly provides a social benefit to the unvaccinated such as children and older adults, it can be considered a prosocial behavior and is associated with collective responsibility (defined as the willingness to protect others by one’s own vaccination by means of herd immunity) [8]. A systematic review found that 29 out of 470 studies identified social benefit as a significant influence on influenza vaccine uptake, thus social benefit (e.g., collective responsibility) was added as one of the psychological determinants for vaccine uptake in the extended version of TPB [9]. Collective responsibility, or social accountability, was also proposed by behavioral scientists as an important motivator in COVID-19 vaccination promotion [10,11].
TRA, introduced by Fishben [12], posits that if an individual evaluates a behavior as positive (attitude), and if the individual believes that he or she is expected to perform the behavior (subjective norm), the individual will have more intention to perform the behavior. Subsequently, TRA was extended to TPB by adding the “Perceived Behavioral Control” component (a person’s perception of the ease or difficulty of performing the behavior of interest) to better predict actual behavior [13]. Therefore, according to TPB, attitude, subjective norm, and perceived behavioral control are the three core components that together shape an individual’s intention to take actions, such as vaccination. A meta-analysis also demonstrated that these three components were significant predictors of vaccination intentions [14]. However, most current research on COVID-19 vaccination is overwhelmingly based on evidence of people’s vaccination intention rather than vaccine uptake. Although there is a causal relationship between intention and behavior in most health-related models [15], some studies pointed out that there is a gap between intention and behavior, vaccination intention does not always transfer to vaccine uptake [16].
Collective responsibility was introduced to study health-related behaviors (e.g., reducing sexual transmission of HIV) early [17,18] and was included as a psychological antecedent of vaccination in both the 5C model and the extended 7C model of vaccination intentions recently [19,20]. An increasing number of empirical studies support that people scoring higher in collective responsibility show greater vaccination intentions and report higher vaccine uptake [19,20,21,22]. However, previous studies have little knowledge about the boundary conditions (referring to the ‘who, where, when’ aspects of a theory) of collective responsibility affecting vaccination. Böhm and Betsch [23] proposed that promoting prosocial vaccination (e.g., collective responsibility) may be more effective among individuals with lower vaccination motivation but called for empirical study. This calls into question whether collective responsibility is an independent predictor of vaccine uptake or whether it interacts with other predictors in the extended version of TPB. Additionally, vaccination willingness or behaviors are influenced by many factors [3,9,24,25,26,27,28], and there are potential self-selection or confounding biases when studying vaccination intention or behaviors based on observational samples or data. For example, someone who has higher collective responsibility may also have a more positive attitude or higher subjective norm on vaccination. Studies based on the traditional regression analysis method often cannot address the concerns about self-selection bias or unobservable confounding variables as discussed above [23], whereas the propensity score matching (PSM) method is an effective alternative method to reduce the confounding bias in observational studies [29].
Macao Special Administration Region (SAR) of China is in the western Pearl River Delta by the South China Sea. Featured as a crowded urban setting with high buildings, Macao has a population of about 680,000 and is the most densely populated region in the world [30]. Macao has become a major international resort city and a top destination for gambling tourism, which contributes to 60% of the local GDP and 70% of the local tax revenue. The total number of workers in the six tourism satellite industries (gaming, retail trade, food and beverage, hotel, passenger transportation, and travel agency services) was around 203,000 in 2019, accounting for nearly 50% of the working population in Macao [31]. Up to 7 July 2022, 89.1% of the population of Macao has been fully vaccinated in comparison with the global rate of 61.3% [32]. Workers in tourism satellite industries may generally have a stronger willingness to end the COVID-19 pandemic due to the severe negative impacts on the tourism industry. The government of Macao (SAR) has adopted a variety of strategies to promote COVID-19 vaccination, including promoting residents’ collective responsibility [33]. Therefore, the case of tourism satellite industries in Macao has provided a good research opportunity to study whether CR can play a positive role to reduce vaccine hesitancy. Adopting a PSM technique to reduce self-selection or other potential confounding bias in observational data, this study aims to explore the role of CR in vaccination decision making based on the model of TPB, as well as its boundary conditions.
2. Materials and Methods
2.1. Participants and Study Design
Ethical approval was obtained from the School of Business of Macau University of Science and Technology (Reference number: MUST/MSB/2021/03). A cross-sectional survey using a structured questionnaire was conducted among workers in the six tourism satellite industries (gaming, retail trade, food and beverage, hotel, passenger transportation, and travel agency services) in Macao. The inclusion criteria were full-time adult employees in the studied industries who consented to participate in this study and could answer an online e-questionnaire in the Chinese language. The participants were recruited using convenience sampling. The questionnaire with a written consent form was posted on an online survey platform (Google Forms). A poster with a QR code and a website link of the survey were created, respectively. Both emails and printed posters were used to disseminate the survey information with the assistance of the companies’ human resources departments or heads of the industry associations.
According to the sampling formula (α = 0.05, δ = 0.05, p = 0.5), the minimum sample size was around 400. A quality control question (what year is this year?) was set to detect inattentive samples. Data were collected from 28th July to 20th August of 2021 after a 47-sample pilot study. The progress of the survey was monitored daily. Data were exported from the online survey platform and checked for errors: (i) removed those who did not complete the questionnaire, and (ii) excluded those who answered the quality control question incorrectly. Statistical analyses were performed using SPSS (Version 28,SBAS Ltd., Hong Kong) for Windows.
2.2. Measures
The self-administered questionnaire included (i) COVID-19 vaccine uptake, (ii) COVID-19 vaccine attitude, subjective norm, and perceived behavioral control, (iii) collective responsibility, and (iv) socio-demographic characteristics. In addition, (ii) was designed based on the extended theory of TPB and previous studies. Seven experts in public health were asked to evaluate the content validity, calculating the Item-level Content Validity Index (I-CVI) and Scale-level Content Validity Index (S-CVI). When the experts are no less than 6, the content validity is considered to be good if I-CVI ≥ 0.78 and S-CVI ≥ 0.90 [34]. The exploratory factor analysis (EFA) using principal components analysis (PCA) was performed to test the construct validity. The internal consistency reliability was assessed with Cronbach’s alpha, and it is good when factor analysis is applied and Cronbach’s alpha is between 0.70 and 0.95 [35].
2.2.1. COVID-19 Vaccine Uptake (VU)
COVID-19 VU was reported by a single item: “Have you received COVID-19 vaccine?” The Item was rated on a 5-point scale: 1 = not willing to be vaccinated, 2 = undecided whether to vaccinate, 3 = not yet, but planning to vaccinate, 4 = one dose has been received, and 5 = two doses have been received. Participants answering 1–3 were defined as unvaccinated against COVID-19; others answering 4 or 5 were defined as vaccinated.
2.2.2. COVID-19 Vaccine Attitude (VA)
COVID-19 VA was measured using a belief-based measure [36]. Participants were presented with four paired items of behavioral beliefs and their corresponding outcome evaluation. Behavioral beliefs include “I think getting the COVID-19 vaccine (i) can protect myself from COVID-19 infection, (ii) has additional benefits, such as accessibility, special holidays, etc., (iii) has a safety hazard, (iv) has side effects. The first two beliefs were positive attitudes, and the others were negative attitudes. The corresponding outcome evaluation items are (i) “I value the protection of COVID-19 vaccine”, (ii) “I value the additional benefits, such as accessibility, special holidays, etc.” (iii) “I am scared of safety hazard from COVID-19 vaccine”, (iv) “I am scared of the side effects from COVID-19 vaccine”. Each item was scored on a 5-point unipolar scale ranging from 1 to 5.
A belief-based measure of the COVID-19 VA was calculated as the summation of the four products of the paired behavioral beliefs and outcome evaluations. A higher VA score indicates a more positive attitude. I-CVI of this scale ranged from 0.86 to 1.00, and S-CVI was 0.93. A two-factor solution explaining 63.26% of the total variance (36.96% for positive items, 26.30% for negative items) was obtained by EFA in our sampling (KMO = 0.724, Bartlett’s test χ2 = 1858.616, p < 0.001). Cronbach’s alpha of the two factors was 0.69 (around 0.70) and 0.86. Thus, the scale has sufficient validity and reliability.
2.2.3. Subjective Norm (SN)
SN was also measured using a belief-based measure [36]. Four referents were used in the measure of normative beliefs (i.e., my family, my employer, medical professionals I trust, and associations I trust). Participants were asked to indicate the degree that each referent recommend them to take the COVID-19 vaccine, and the degree that they were motivated to comply with each referent’s recommendation. Each item was scored on a 5-point unipolar scale ranging from 1 to 5. A belief-based measure of SN was calculated as the summation of the four products (normative belief × motivation to comply), with a higher score indicating higher SN. Both I-CVI and S-CVI of the scale were 1.00. One factor explained 64.74% of the total variance using EFA in our sampling (KMO = 0.828, Bartlett’s test χ2 = 3740.009, p < 0.001), and the Cronbach’s alpha was 0.92. Thus, the scale has sufficient validity and reliability.
2.2.4. Perceived Behavioral Control (PBC)
PBC was measured with a single item asking participants to report their perception of the ease or difficulty in getting COVID-19 vaccination [36]. The item was rated on a 5-point scale (1 = very difficult, 5 = very easy).
2.2.5. Collective Responsibility (CR)
CR was measured by the three-item subscale of the 5C scale, a valid brief measure assessing psychological antecedents of vaccination, and the subscale’s Cronbach’s alpha was 0.71 with sufficient reliability [19]. Items were rated on a 5-point scale from 1 = strongly disagree to 5 = strongly agree. One item (‘When everyone is vaccinated, I don’t have to get vaccinated too’) was reversed to be in line with this scoring. A composite variable was computed by averaging the three items, with a higher average score indicating higher CR. The score of the composite variable ranged from 1.67 to 5.00 (mean = 3.72, SD = 0.64). Participants with a score lower than the average were sorted into the CR-lower group, and others were sorted into the CR-higher group.
2.2.6. Socio-Demographic Characteristics
These consisted of gender, age, educational level, marital status, monthly income, whether living with older adults or children or not, and working industries.
2.3. Statistical Analysis
Propensity score matching was performed in this study. Using multivariable logistic regression, a propensity score of each participant being in the CR-higher group was predicted and a 1:1 matching of the scores was performed [37]. The match tolerance was set at 0.02. The following covariates were used for the PSM analysis: COVID-19 VA, SN, PBC, gender, age, educational level, marital status, monthly income, whether living with older adults or children or not, and working industries. Balance-check of the covariates was conducted to confirm the validity of applying this method, using both p-value and standardized mean difference (SMD) as criteria. With potential confounding factors controlled, the association between collective responsibility and COVID-19 vaccine uptake was estimated with multivariable logistic regression analysis. The odds ratio (OR) and 95% confidence interval (CI) were calculated. In the multivariable logistic regression analysis, we also examined the interaction effect between predictors and interpreted the interactions with a spotlight analysis [38]. Significance was accepted at the p-value < 0.05 for all calculations.
3. Results
3.1. Participant Characteristics
A total of 620 questionnaires were collected and 608 (98.06%) were valid for analysis, with 125 (20.56%) from travel agency industry, 167 (27.47%) from food and beverage industry, 178 (29.27%) from gaming industry, and 138 (22.70%) from the other three industries (retail trade, hotel, and passenger transport). Age ranged from 18 to 72 (mean = 38.26, SD = 10.36). As shown in Table 1, more than half of the participants (62.5%) have received COVID-19 vaccine. Figure 1 shows that 268 participants were assigned to the CR-lower group and 340 were assigned to the CR-higher group according to the criteria defined in the 2.2 Measures section, and 173 pairs were selected through PSM treatment according to the criteria defined in the 2.3 Statistical Analysis section.

Table 1.
Demographic characteristics (n = 608).
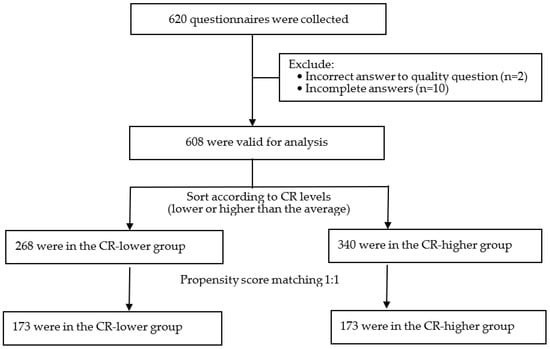
Figure 1.
Flowchart of data processing.
3.2. Baseline Covariates after Propensity Score Matching
The comparisons of baseline characteristics before PSM and after PSM are presented in Table 2. Before PSM treatment, there were significant differences (p < 0.05; SMD > 0.10) among gender, age, working industries, COVID-19 VA, SN, and PBC between the CR-lower and the CR-higher groups. After PSM treatment, there were no significant differences regarding the above-mentioned characteristics between these two groups (p > 0.05; SMD ≤ 0.10).

Table 2.
PSM to balance the participants’ characteristics between the CR-lower and CR-higher groups.
3.3. The Association of Collective Responsibility and COVID-19 Vaccine Uptake
Multivariate logistic regression analysis in Table 3 shows that the significant independent predictors of COVID-19 vaccine uptake were CR (p = 0.012, OR = 2.070, 95% CI = 1.174 to 3.650), COVID-19 VA (p < 0.001, OR = 1.149, 95% CI= 1.086 to 1.216) and PBC (easy or very easy = 1) (p = 0.019, OR = 5.636, 95% CI = 1.330 to 23.882). The model successfully classified 78.3% of cases overall (R2N = 0.465). The results indicated that participants who had higher CR, more positive COVID-19 VA, and perceived getting COVID-19 vaccination as easier would have higher COVID-19 vaccine uptake. Table 3 also shows CR and COVID-19 VA had an interaction effect on COVID-19 vaccine uptake (p = 0.019, OR = 0.922, 95% CI = 0.861 to 0.987).

Table 3.
The logistic regression analysis for COVID-19 vaccine uptake (n = 346).
To better understand the interaction effect between CR and COVID-19 VA, we conducted a spotlight analysis to further interpret the effect of CR on COVID-19 vaccine uptake among participants with more positive (one standard deviation above mean) and more negative (one standard deviation below mean) COVID-19 VA. As shown in Figure 2, CR was moderated by COVID-19 VA, and it was more effective among individuals who had more negative COVID-19 VA. It further illustrates that the CR–COVID-19 vaccine uptake relationship was stronger among participants who had a more negative COVID-19 VA.
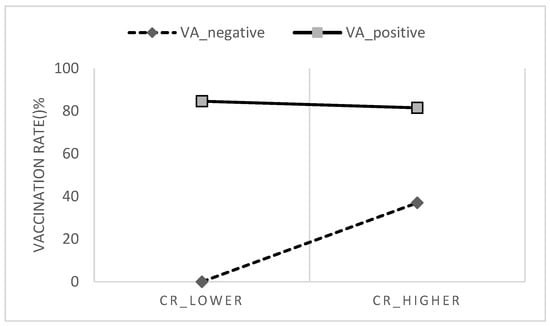
Figure 2.
Collective responsibility moderated by vaccine attitude.
4. Discussion
4.1. Higher Collective Responsibility Predicts Higher COVID-19 Vaccine Uptake
As shown in Table 2, participants in the CR-higher group reported a significantly higher COVID-19 vaccine uptake than those in the CR-lower group (64.7% vs. 49.7%) after PSM. Logistic regression also indicated a positive association between CR and COVID-19 vaccine uptake. Previous studies have already demonstrated that collective responsibility was positively associated with vaccination intentions or vaccine uptake. For example, an online survey in China found participants’ COVID-19 vaccination intention was positively associated with CR [22]; a survey in Hong Kong found nurses scoring higher on CR showed greater influenza vaccine uptake and COVID-19 vaccination intention [21]; another survey in the UK found that a lower sense of CR independently predicted a lack of uptake of influenza, pneumococcal, and shingles vaccine among older adults [39]. Some other studies also found similar results [40,41]. However, vaccine uptake is associated with many factors [3,9,24,25,26]. The present study illustrated that people who have different CR may also have significant differences in terms of COVID-19 VA, SN, and PBC before PSM (Table 2), which may lead to confounding bias. Moreover, previous studies often did not exclude these potentially influential factors as alternative explanations. Compared with these studies, the present study reduced the confounding bias of participants’ COVID-19 VA, SN, PBC, and the socio-demographic characteristics shown in Table 2 with the method of PSM. Thus, this study added better evidence to current research.
Additionally, Table 3 shows that COVID-19 VA and PBC are also positively associated with COVID-19 vaccine uptake, although the association of SN is not significant (p = 0.080). The results were similar to many previous studies [42,43,44,45]. It indicates that the theory of planned behavior can be well applied to study people’s COVID-19 vaccine hesitancy and behaviors. It also proves the necessity of controlling these covariates with PSM in this study.
4.2. Collective Responsibility Is More Effective among Individuals Having More Negative COVID-19 Vaccine Attitude
This study verified that CR and COVID-19 VA had an interaction effect on COVID-19 vaccine uptake, and the spotlight analysis illustrates that the CR –COVID-19 vaccine uptake relationship was stronger among participants who had a more negative COVID-19 VA. On the contrary, participants with a positive vaccine attitude can be motivated to vaccinate by the benefits of vaccines (e.g., protecting themselves), regardless of whether CR is high or low. Figure 2 illustrates that the COVID-19 vaccination rates among participants with positive COVID-19 VA were similarly high in the CR-lower group and the CR-higher group. A meta-analysis study also found that attitude towards vaccine was the strongest predictor of vaccination intention [14]. Conversely, those with negative attitudes towards COVID-19 vaccine may have lower motivation to vaccinate for direct personal benefits, thus whether they value an indirect social benefit is important. The finding supports the hypotheses proposed by Böhm and Betsch [23] that prosocial vaccination (e.g., collective responsibility) may be more effective among individuals with lower vaccination motivation. In addition, it further answered that CR is a predictor of vaccine uptake and will also interact with vaccine attitude in the extended version of TPB.
4.3. Implications
The findings of the present study provide theoretical and practical implications. To begin with, to our knowledge, this is the first study aimed to examine the association between CR and COVID-19 vaccine uptake based on the PSM method. The key findings that higher CR is associated with higher COVID-19 vaccine uptake and that it is more effective among individuals having more negative COVID-19 vaccine attitude emerged, uniquely contributing to our understanding of people’s COVID-19 vaccine hesitancy and behaviors.
These findings may provide policymakers, health educators, and practitioners with insights into vaccination communication. Firstly, CR is an important motivator in COVID-19 vaccination promotion and calls for strategies. People’s vaccine attitudes and behaviors are not immutable. One study found that 60% of those who initially reported some level of hesitancy eventually got vaccinated [46]. Böhm and Betsch [23] proposed that CR can be promoted through communication campaigns regarding awareness of herd immunity and community protection. For example, Macao had been doing well and maintaining several months without new COVID-19 cases before May 2021 [47] despite frequent outbreaks in neighboring cities [48]. To respond to the unprecedented threat, the government of Macao SAR took a series of measures to encourage vaccination, especially, city-wide slogans communicating knowledge about community protection like: ‘we are all guardians, get vaccinated for yourself and others’ and ‘vaccination together to build an immune barrier’ [33]. These promotions may have helped to motivate people’s CR to get COVID-19 vaccination. The vaccination rate in Macao rapidly increased from 15.22% on 27th May to 35.70% on 30th June [32]. Moreover, the government of Macao SAR is currently trying its best to motivate the public’s CR to take measures (e.g., several rounds of city-wide COVID-19 testing) to cope with the latest outbreak involving more than 1000 locally infected cases since 18 June 2022 [33].
Secondly, the present study shows that the CR–COVID-19 VA relationship was stronger among participants who had more negative COVID-19 VA. Hence, educators and practitioners perhaps should focus on CR promotions among people with less positive COVID-19 VA. For example, in Canada, parents using the internet to search for vaccination information often have a negative perception of vaccine risks and safety [49].
4.4. Limitations and Future Research
The present study had some limitations. Firstly, while generally consistent with randomized clinical trials when applied appropriately, the PSM method has its own limitations. Some data information may be lost during the process of propensity score matching because observations without suitable matches are excluded in the final estimation [50]. PSM method may help to alleviate the self-selection bias and the omitted variable bias, but cannot fully address these concerns.
Secondly, this study is a cross-sectional design and the effectiveness of examining causality is limited. Awareness of collective responsibility may vary during stages of the COVID-19 pandemic [51]. Further time sequence studies (e.g., prospective cohort study) are needed to verify the reliability of these results.
Thirdly, the case of Macao may not have high representativeness worldwide, since Macao is an Asian city with the highest population density in the world and its economy heavily depends on tourism. Meanwhile, a US-based study found that prosocial concerns promote vaccination against COVID-19 more in sparsely rather than densely populated areas [52]. The findings of this study should be generalized with caution.
As for study directions in the future, a further investigation of the measurement of CR may help to deepen the understanding of the boundary conditions of CR. As Böhm and Betsch [13] proposed, promoting CR may also be more effective among individuals who have great CR but lack knowledge regarding herd immunity and community protection. Exploring more boundary conditions of CR (e.g., is the role of CR the same in different cultural backgrounds?) and CR communication intervention studies may further demonstrate the application value.
5. Conclusions
Applying the PSM method to control potential confounding bias among observational data, this study found that higher CR predicted higher COVID-19 vaccine uptake. Participants in the CR-higher group in this study reported significantly higher COVID-19 vaccine uptake than those in the CR-lower group (64.7% vs. 49.7%) after PSM treatment. The significant interaction effect of CR and COVID-19 VA indicates that the association is especially strong among those having a negative COVID-19 vaccine attitude. The empirical evidence found in this study hence may help optimize communication strategy to enhance or maintain sustainable COVID-19 vaccine uptakes.
Author Contributions
J.W. composed the proposal, collected data, analyzed data, and was a major contributor to the writing of the manuscript; J.Z. advised and supervised the study, and participated in the study design and manuscript revision; C.H.C. and H.W. reviewed and revised the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by School of Business of Macau University of Science and Technology (Reference number: MUST/MSB/2021/03). No animals were used in the studies that were the basis of this research. All human procedures were carried out in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
All data generated or analyzed during this study are included in the published article and are available from the corresponding author upon reasonable request.
Acknowledgments
We would like to acknowledge the experts from Kiang Wu Nursing College of Macau who evaluated the content validity of the questionnaire, our colleagues who promoted the survey, and Queenie Mak for proofreading the manuscript. We thank the supporting companies, organizations, and participants for the invaluable contributions to the study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Worldometer. COVID-19 Coronavirus Pandemic. 2022. Available online: https://www.worldometers.info/coronavirus/ (accessed on 8 July 2022).
- León, T.M. COVID-19 Cases and Hospitalizations by COVID-19 Vaccination Status and Previous COVID-19 Diagnosis—California and New York, May–November 2021. Morb. Mortal. Wkly. Rep. 2022, 71, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Sallam, M. COVID-19 vaccine hesitancy worldwide: A concise systematic review of vaccine acceptance rates. Vaccines 2021, 9, 160. [Google Scholar] [CrossRef] [PubMed]
- Galanis, P.; Vraka, I.; Katsiroumpa, A.; Siskou, O.; Konstantakopoulou, O.; Katsoulas, T.; Mariolis-Sapsakos, T.; Kaitelidou, D. First COVID-19 Booster Dose in the General Population: A Systematic Review and Meta-Analysis of Willingness and Its Predictors. Vaccines 2022, 10, 1097. [Google Scholar] [CrossRef]
- Friedrich, M. WHO’s top health threats for 2019. JAMA 2019, 321, 1041. [Google Scholar] [CrossRef]
- DiClemente, R.J.; Salazar, L.F.; Crosby, R.A. Health Behavior Theory for Public Health: Principles, Foundations, and Applications; Jones & Bartlett Publishers: Burlington, MA, USA, 2013. [Google Scholar]
- Steptoe, A.; Freedland, K.E.; Jennings, J.R.; Manuck, S.B.; Susman, E.J. Handbook of Behavioral Medicine; Springer: New York, NY, USA, 2010. [Google Scholar]
- Betsch, C.; Böhm, R.; Korn, L. Inviting free-riders or appealing to prosocial behavior? game-theoretical reflections on communicating herd immunity in vaccine advocacy. Health Psychol. 2013, 32, 978–985. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schmid, P.; Rauber, D.; Betsch, C.; Lidolt, G.; Denker, M.L. Barriers of influenza vaccination intention and behavior–a systematic review of influenza vaccine hesitancy, 2005–2016. PLoS ONE 2017, 12, e0170550. [Google Scholar] [CrossRef]
- Volpp, K.G.; Loewenstein, G.; Buttenheim, A.M. Behaviorally informed strategies for a national COVID-19 vaccine promotion program. JAMA 2021, 325, 125–126. [Google Scholar] [CrossRef] [PubMed]
- Costantino, C.; Rizzo, C.; Rosselli, R.; Battista, T.; Conforto, A.; Cimino, L.; Poscia, A.; Fiacchini, D. Ten Actions to Counteract Vaccine Hesitancy Suggested by the Italian Society of Hygiene, Preventive Medicine, and Public Health. Vaccines 2022, 10, 1030. [Google Scholar] [CrossRef]
- Ajzen, I.; Madden, T.J. Prediction of goal-directed behavior: Attitudes, intentions, and perceived behavioral control. J. Exp. Soc. Psychol. 1986, 22, 453–474. [Google Scholar] [CrossRef]
- Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Xiao, X.; Wong, R.M. Vaccine hesitancy and perceived behavioral control: A meta-analysis. Vaccine 2020, 38, 5131–5138. [Google Scholar] [CrossRef] [PubMed]
- Webb, T.L.; Sheeran, P. Does changing behavioral intentions engender behavior change? A meta-analysis of the experimental evidence. Psychol. Bull. 2006, 132, 249. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sheeran, P.; Webb, T.L. The intention–behavior gap. Soc. Personal. Psychol. Compass 2016, 10, 503–518. [Google Scholar] [CrossRef]
- Marks, G.; Burris, S.; Peterman, T.A. Reducing sexual transmission of HIV from those who know they are infected: The need for personal and collective responsibility. AIDS 1999, 13, 297–306. [Google Scholar] [CrossRef] [PubMed]
- Newton, L.H. Collective responsibility in health care. J. Med. Philos. 1982, 7, 11–22. [Google Scholar] [CrossRef] [PubMed]
- Betsch, C.; Schmid, P.; Heinemeier, D.; Korn, L.; Holtmann, C.; Böhm, R. Beyond confidence: Development of a measure assessing the 5C psychological antecedents of vaccination. PLoS ONE 2018, 13, e0208601. [Google Scholar] [CrossRef] [Green Version]
- Geiger, M.; Rees, F.; Lilleholt, L.; Santana, A.P.; Zettler, I.; Wilhelm, O.; Betsch, C.; Böhm, R. Measuring the 7Cs of vaccination readiness. Eur. J. Psychol. Assess. 2021; advance online publication. [Google Scholar] [CrossRef]
- Kwok, K.O.; Li, K.-K.; Wei, W.I.; Tang, A.; Wong, S.Y.S.; Lee, S.S. Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: A survey. Int. J. Nurs. Stud. 2021, 114, 103854. [Google Scholar] [CrossRef]
- Liu, P.L.; Ao, S.H.; Zhao, X.; Zhang, L. Associations between COVID-19 information acquisition and vaccination intention: The roles of anticipated regret and collective responsibility. Health Commun. 2022; Advance online publication. [Google Scholar] [CrossRef]
- Böhm, R.; Betsch, C. Prosocial vaccination. Curr. Opin. Psychol. 2022, 43, 307–311. [Google Scholar] [CrossRef]
- Reiter, P.L.; Pennell, M.L.; Katz, M.L. Acceptability of a COVID-19 vaccine among adults in the United States: How many people would get vaccinated? Vaccine 2020, 38, 6500–6507. [Google Scholar] [CrossRef] [PubMed]
- Al-Amer, R.; Maneze, D.; Everett, B.; Montayre, J.; Villarosa, A.R.; Dwekat, E.; Salamonson, Y. COVID-19 vaccination intention in the first year of the pandemic: A systematic review. J. Clin. Nurs. 2022, 31, 62–86. [Google Scholar] [CrossRef] [PubMed]
- Brewer, N.T.; Chapman, G.B.; Rothman, A.J.; Leask, J.; Kempe, A. Increasing vaccination: Putting psychological science into action. Psychol. Sci. Public Interest 2017, 18, 149–207. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wong, L.P.; Alias, H.; Danaee, M.; Ahmed, J.; Lachyan, A.; Cai, C.Z.; Lin, Y.; Hu, Z.; Tan, S.Y.; Lu, Y.; et al. COVID-19 vaccination intention and vaccine characteristics influencing vaccination acceptance: A global survey of 17 countries. Infect. Dis. Poverty 2021, 10, 122. [Google Scholar] [CrossRef]
- Navin, M.C.; Oberleitner, L.M.-S.; Lucia, V.C.; Ozdych, M.; Afonso, N.; Kennedy, R.H.; Keil, H.; Wu, L.; Mathew, T.A. COVID-19 Vaccine Hesitancy Among Healthcare Personnel Who Generally Accept Vaccines. J. Community Health 2022, 47, 519–529. [Google Scholar] [CrossRef] [PubMed]
- Austin, P.C. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar. Behav. Res. 2011, 46, 399–424. [Google Scholar] [CrossRef] [Green Version]
- Government of Macao Special Administrative Region Statistics and Census Service. Macao in Figures. 2021. Available online: https://www.dsec.gov.mo/en-US/Home/Publication/MacaoInFigures (accessed on 8 July 2022).
- Government of Macao Special Administrative Region Statistics and Census Service. Tourism Satellite Account 2019. 2021. Available online: https://www.dsec.gov.mo/getAttachment/57d1dbb0-2a70-4555-8ef5-88b2858e2525/C_TSA_PUB_2019_Y.aspx (accessed on 8 July 2022).
- Our World in Data. Coronavirus (COVID-19) Vaccinations. Available online: https://ourworldindata.org/covid-vaccinations?country=MAC (accessed on 8 July 2022).
- Macao SAR Government Health Bureau. COVID-19 Vaccine Information Page. Available online: https://www.ssm.gov.mo/apps1/covid19vaccine/ch.aspx#clg18751 (accessed on 8 July 2022).
- Shi, J.; Mo, X.; Sun, Z. Content validity index in scale development. Zhong Nan Da Xue Xue Bao. Yi Xue Ban J. Cent. South University. Med. Sci. 2012, 37, 152–155. [Google Scholar]
- Terwee, C.B.; Bot, S.D.; de Boer, M.R.; van der Windt, D.A.; Knol, D.L.; Dekker, J.; Bouter, L.M.; de Vet, H.C. Quality criteria were proposed for measurement properties of health status questionnaires. J. Clin. Epidemiol. 2007, 60, 34–42. [Google Scholar] [CrossRef] [Green Version]
- Ajzen, I. Constructing a Theory of Planned Behavior Questionnaire. 2006. Available online: https://people.umass.edu/aizen/tpb.html (accessed on 8 July 2022).
- Thoemmes, F. Propensity score matching in SPSS. arXiv 2012, arXiv:1201.6385. [Google Scholar]
- Aiken, L.S.; West, S.G.; Reno, R.R. Multiple Regression: Testing and Interpreting Interactions; Sage: Thousand Oaks, CA, USA, 1991. [Google Scholar]
- Nicholls, L.A.B.; Gallant, A.J.; Cogan, N.; Rasmussen, S.; Young, D.; Williams, L. Older adults’ vaccine hesitancy: Psychosocial factors associated with influenza, pneumococcal, and shingles vaccine uptake. Vaccine 2021, 39, 3520–3527. [Google Scholar] [CrossRef]
- Dorman, C.; Perera, A.; Condon, C.; Chau, C.; Qian, J.; Kalk, K.; DiazDeleon, D. Factors associated with willingness to be vaccinated against COVID-19 in a large convenience sample. J. Community Health 2021, 46, 1013–1019. [Google Scholar] [CrossRef] [PubMed]
- Böhm, R.; Betsch, C.; Korn, L. Selfish-rational non-vaccination: Experimental evidence from an interactive vaccination game. J. Econ. Behav. Organ. 2016, 131, 183–195. [Google Scholar] [CrossRef]
- Fan, C.-W.; Chen, I.-H.; Ko, N.-Y.; Yen, C.-F.; Lin, C.-Y.; Griffiths, M.D.; Pakpour, A.H. Extended theory of planned behavior in explaining the intention to COVID-19 vaccination uptake among mainland Chinese university students: An online survey study. Hum. Vaccines Immunother. 2021, 17, 3413–3420. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, Y.; Romanowich, P.; Hantula, D.A. Predicting Intention to Take a COVID-19 Vaccine in the United States: Application and Extension of Theory of Planned Behavior. Am. J. Health Promot. 2022, 36, 710–713. [Google Scholar] [CrossRef]
- Patwary, M.M.; Bardhan, M.; Disha, A.S.; Hasan, M.; Haque, Z.; Sultana, R.; Hossain, R.; Browning, M.H.E.M.; Alam, A.; Sallam, M. Determinants of COVID-19 vaccine acceptance among the adult population of Bangladesh using the Health Belief Model and the Theory of Planned Behavior Model. Vaccines 2021, 9, 1393. [Google Scholar] [CrossRef]
- Shmueli, L. Predicting intention to receive COVID-19 vaccine among the general population using the health belief model and the theory of planned behavior model. BMC Public Health 2021, 21, 804. [Google Scholar] [CrossRef]
- Willis, D.E.; Selig, J.P.; Andersen, J.A.; Hall, S.; Hallgren, E.; Williams, M.; Bryant-Moore, K.; McElfish, P.A. Hesitant but vaccinated: Assessing COVID-19 vaccine hesitancy among the recently vaccinated. J. Behav. Med. 2022, 1–10, Advance online publication. [Google Scholar] [CrossRef]
- Ieng, S.M.; Cheong, I.H. An overview of epidemiology of COVID-19 in Macau SAR. Front. Public Health 2020, 8, 550057. [Google Scholar] [CrossRef]
- Zhang, M.; Prevention, G.G.P.C.F.D.C.A.; Xiao, J.; Deng, A.; Zhang, Y.; Zhuang, Y.; Hu, T.; Li, J.; Tu, H.; Li, B.; et al. Transmission dynamics of an outbreak of the COVID-19 Delta variant B. 1.617. 2—Guangdong Province, China, May–June 2021. China CDC Wkly. 2021, 3, 584–586. [Google Scholar] [CrossRef]
- Tustin, J.L.; Crowcroft, N.S.; Gesink, D.; Johnson, I.; Keelan, J. Internet exposure associated with Canadian parents’ perception of risk on childhood immunization: Cross-sectional study. JMIR Public Health Surveill. 2018, 4, e8921. [Google Scholar] [CrossRef]
- Ross, M.E.; Kreider, A.R.; Huang, Y.-S.; Matone, M.; Rubin, D.M.; Localio, A.R. Propensity score methods for analyzing observational data like randomized experiments: Challenges and solutions for rare outcomes and exposures. Am. J. Epidemiol. 2015, 181, 989–995. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McRee, A.-L.; Gower, A.L.; Kiss, D.E.; Reiter, P.L. Has the COVID-19 pandemic affected general vaccination hesitancy? Findings from a national study. J. Behav. Med. 2022; advance online publication. [Google Scholar] [CrossRef] [PubMed]
- Jung, H.; Albarracín, D. Concerns for others increase the likelihood of vaccination against influenza and COVID-19 more in sparsely rather than densely populated areas. Proc. Natl. Acad. Sci. USA 2021, 118, e2007538118. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).