COVID-19 Vaccine Coverage and Sociodemographic, Behavioural and Housing Factors Associated with Vaccination among People Experiencing Homelessness in Toronto, Canada: A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Setting and Design
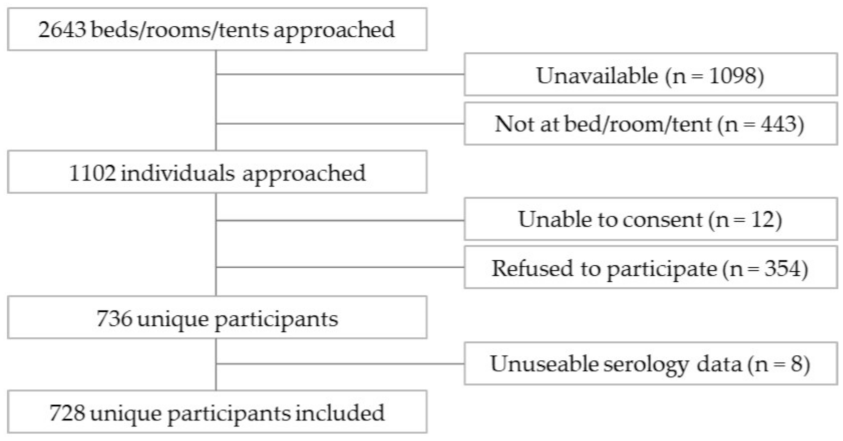
2.2. Participants and Recruitment
2.3. Characteristics of Participants
2.4. Outcome Measures
2.5. Statistical Analysis
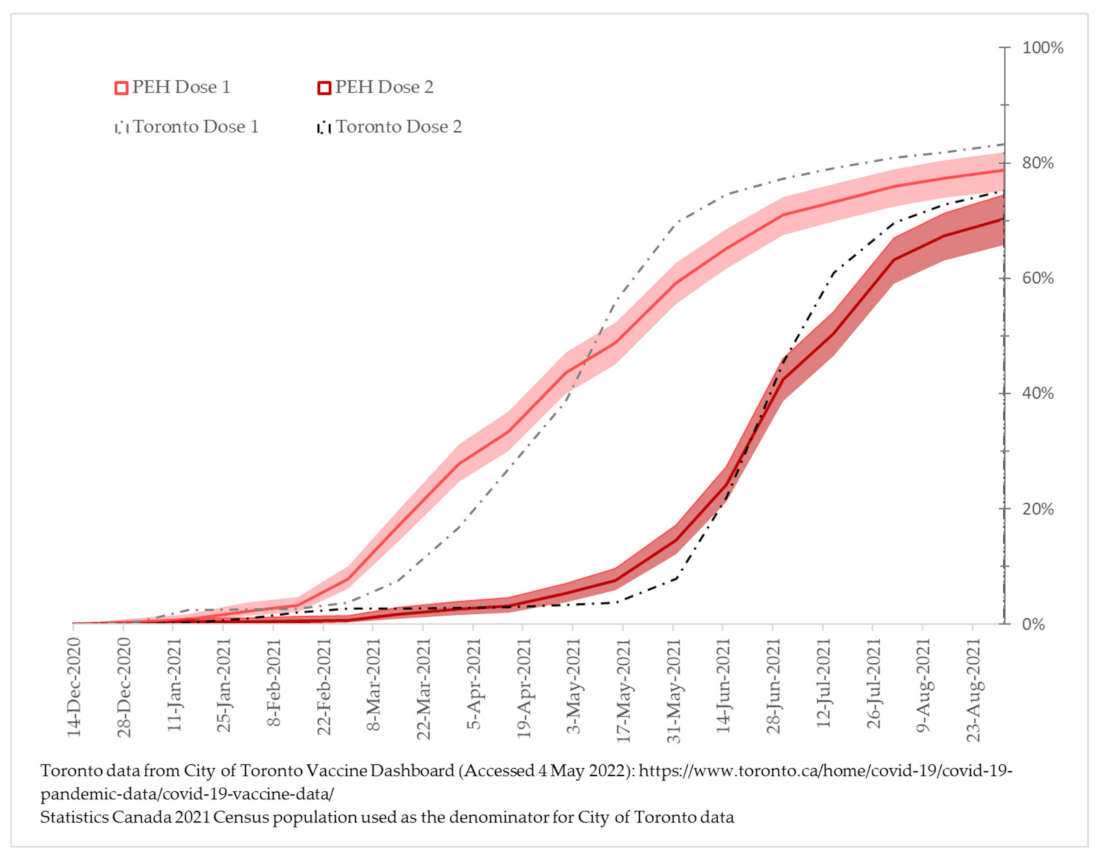
3. Results
4. Discussion
Limitations and Future Research Needs
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Richard, L.; Booth, R.; Rayner, J.; Clemens, K.K.; Forchuk, C.; Shariff, S.Z. Testing, infection and complication rates of COVID-19 among people with a recent history of homelessness in Ontario, Canada: A retrospective cohort study. Can. Med. Assoc. Open Access J. 2021, 9, E1–E9. [Google Scholar] [CrossRef] [PubMed]
- Roederer, T.; Mollo, B.; Vincent, C.; Nikolay, B.; Llosa, A.E.; Nesbitt, R.; Vanhomwegen, J.; Rose, T.; Goyard, S.; Anna, F.; et al. Seroprevalence and risk factors of exposure to COVID-19 in homeless people in Paris, France: A cross-sectional study. Lancet Public Health 2021, 6, e202–e209. [Google Scholar] [CrossRef]
- Fazel, S.; Geddes, J.R.; Kushel, M. The health of homeless people in high-income countries: Descriptive epidemiology, health consequences, and clinical and policy recommendations. Lancet 2014, 384, 1529–1540. [Google Scholar] [CrossRef] [Green Version]
- Liu, M.; Hwang, S.W. Health care for homeless people. Nat. Rev. Dis. Primers 2021, 7, 5. [Google Scholar] [CrossRef] [PubMed]
- Williamson, E.J.; Walker, A.J.; Bhaskaran, K.; Bacon, S.; Bates, C.; Morton, C.E.; Curtis, H.J.; Mehrkar, A.; Evans, D.; Inglesby, P.; et al. OpenSAFELY: Factors associated with COVID-19 death in 17 million patients. Nature 2020, 584, 430. [Google Scholar] [CrossRef] [PubMed]
- Mohsenpour, A.; Bozorgmehr, K.; Rohleder, S.; Stratil, J.; Costa, D. SARS-CoV-2 prevalence, transmission, health-related outcomes and control strategies in homeless shelters: Systematic review and meta-analysis. EClinicalMedicine 2021, 38, 101032. [Google Scholar] [CrossRef] [PubMed]
- Gaetz, S.; Dej, E.; Richter, T.; Redman, M. The State of Homelessness in Canada 2016; Canadian Observatory on Homelessness Press: Toronto, ON, Canada, 2016. [Google Scholar]
- City of Toronto. City of Toronto, Hospital and Community Health Partners to Begin Vaccinating People Experiencing Homelessness and Other Priority Populations as Part of Phase 1 Community Vaccination Plan. Available online: https://www.toronto.ca/news/city-of-toronto-hospital-and-community-health-partners-to-begin-vaccinating-people-experiencing-homelessness-and-other-priority-populations-as-part-of-phase-1-community-vaccination-plan/ (accessed on 28 February 2021).
- Government of Ontario. Ontario’s COVID-19 Vaccination Plan; Queen’s Printer for Ontario: Toronto, ON, Canada, 2021.
- The Homeless Hub. Homeless Hub Community Profiles 2018: Toronto. Available online: https://www.homelesshub.ca/community-profile/toronto (accessed on 31 January 2022).
- Province of Ontario. Help Using the Provincial COVID-19 Vaccine Online System. Available online: Covid-19.Ontario.ca/COVID-19-vaccine-booking-support (accessed on 22 July 2022).
- Paudyal, V.; Racine, M.; Hwang, S.W. COVID-19 vaccination amongst persons experiencing homelessness: Practices and learnings from UK, Canada and the US. Public Health 2021, 199, e2–e3. [Google Scholar] [CrossRef]
- Ghosh, S.M.; Turnbull, J.; MacDonald, N.; Bond, A.; Orkin, A. Key Strategies to Vaccinating Homeless Populations. Available online: https://rsc-src.ca/en/voices/key-strategies-to-vaccinating-homeless-populations (accessed on 4 March 2022).
- City of Toronto. The City of Toronto Continues to Take Significant Action to Assist and Protect People Experiencing Homelessness and Ensure the Safety of the City’s Shelter System. Available online: https://www.toronto.ca/news/the-city-of-toronto-continues-to-take-significant-action-to-assist-and-protect-people-experiencing-homelessness-and-ensure-the-safety-of-the-citys-shelter-system/ (accessed on 4 March 2022).
- City of Toronto. Toronto Public Health Playbook for the COVID-19 Vaccination Program. Available online: https://www.toronto.ca/wp-content/uploads/2021/03/8e7c-TPH-Playbook-for-the-for-COVID-19-Vaccination-Program-Public-Final-F....pdf (accessed on 31 March 2022).
- Casey, L. Vaccination of Toronto’s Homeless Well Underway with about 1000 Getting a Shot. Available online: https://www.cp24.com/news/vaccination-of-toronto-s-homeless-well-underway-with-about-1-000-getting-a-shot-1.5343687?cache=rspnqiqaio%3FclipId%3D89563%3FclipId%3D68597 (accessed on 4 March 2022).
- Sound, D. Pop-Up Clinics Offer Indigenous People in Ontario Easier Access to Vaccinations. Available online: https://www.ctvnews.ca/health/coronavirus/pop-up-clinics-offer-indigenous-people-in-ontario-easier-access-to-vaccinations-1.5361419 (accessed on 4 March 2022).
- Anselmo, A. Community Vaccination Promotion: Increasing Vaccine Confidence and Uptake among Marginalized Individuals and Groups across Canada. Available online: https://www.allianceon.org/blog/Community-Vaccination-Promotion-Increasing-vaccine-confidence-and-uptake-among-marginalised (accessed on 4 March 2022).
- Gibson, V. ‘Now My Body Will be Able to Fight It’: COVID-19 Vaccine Rollout Brings Relief to Downtown Homeless Shelter, Despite Some Lingering Hesitancy. Available online: https://www.thestar.com/news/gta/2021/03/11/now-my-body-will-be-able-to-fight-it-covid-19-vaccine-rollout-brings-relief-to-downtown-homeless-shelter-despite-some-lingering-hesitancy.html (accessed on 4 March 2022).
- Montgomery, M.P.; Meehan, A.A.; Cooper, A.; Toews, K.A.; Ghinai, I.; Schroeter, M.K.; Gibbs, R.; Rehman, N.; Stylianou, K.S.; Yeh, D.; et al. Notes from the Field: COVID-19 Vaccination Coverage Among Persons Experiencing Homelessness—Six U.S. Jurisdictions, December 2020–August 2021. Morb. Mortal. Wkly. Rep. 2021, 70, 1676–1678. [Google Scholar] [CrossRef] [PubMed]
- Shearer, R.D.; Vickery, K.D.; Bodurtha, P.; Drawz, P.E.; Johnson, S.; Jeruzal, J.; Waring, S.; Chamberlain, A.M.; Kharbanda, A.B.; Leopold, J.; et al. COVID-19 Vaccination of People Experiencing Homelessness and Incarceration in Minnesota. Health Aff. 2022, 41, 846–852. [Google Scholar] [CrossRef]
- Balut, M.D.; Chu, K.; Gin, J.L.; Dobalian, A.; Der-Martirosian, C. Predictors of COVID-19 Vaccination among Veterans Experiencing Homelessness. Vaccines 2021, 9, 1268. [Google Scholar] [CrossRef] [PubMed]
- Shariff, S.Z.; Richard, L.; Hwang, S.W.; Kwong, J.C.; Forchuk, C.; Dosani, N.; Booth, R. COVID-19 vaccine coverage and factors associated with vaccine coverage among 23 247 adults with a recent history of homelessness in Ontario, Canada: A population-based cohort study. Lancet Public Health 2022, 7, e366–e377, ISSN 2468-2667. [Google Scholar] [CrossRef]
- Nilsson, S.F.; Laursen, T.M.; Osler, M.; Hjorthøj, C.; Benros, M.E.; Ethelberg, S.; Mølbak, K.; Nordentoft, M. Vaccination against SARS-CoV-2 infection among vulnerable and marginalised population groups in Denmark: A nationwide population-based study. Lancet Reg. Health-Eur. 2022, 16, 100355. [Google Scholar] [CrossRef] [PubMed]
- Bentivegna, E.; Di Meo, S.; Carriero, A.; Capriotti, N.; Barbieri, A.; Martelletti, P. Access to COVID-19 Vaccination during the Pandemic in the Informal Settlements of Rome. Int. J. Environ. Res. Public Health 2022, 19, 719. [Google Scholar] [CrossRef] [PubMed]
- Longchamps, C.; Ducarroz, S.; Crouzet, L.; Vignier, N.; Pourtau, L.; Allaire, C.; Colleville, A.C.; El Aarbaoui, T.; Melchior, M.; ECHO Study Group. COVID-19 vaccine hesitancy among persons living in homeless shelters in France. Vaccine 2021, 39, 3315–3318. [Google Scholar] [CrossRef]
- Knight, K.R.; Duke, M.R.; Carey, C.A.; Pruss, G.; Garcia, C.M.; Lightfoot, M.; Imbert, E.; Kushel, M. COVID-19 testing and vaccine acceptability among homeless-experienced adults: Qualitative data from two samples. J. Gen. Intern. Med. 2022, 37, 823–829. [Google Scholar] [CrossRef] [PubMed]
- Abramovich, A.; Pang, N.; Kunasekaran, S.; Moss, A.; Kiran, T.; Pinto, A.D. Examining COVID-19 vaccine uptake and attitudes among 2SLGBTQ+ youth experiencing homelessness. BMC Public Health 2022, 22, 1–12. [Google Scholar] [CrossRef]
- Kuhn, R.; Henwood, B.; Lawton, A.; Kleva, M.; Murali, K.; King, C.; Gelberg, L. COVID-19 vaccine access and attitudes among people experiencing homelessness from pilot mobile phone survey in Los Angeles, CA. PLoS ONE 2021, 16, e0255246. [Google Scholar] [CrossRef]
- Rogers, J.H.; Cox, S.N.; Hughes, J.P.; Link, A.C.; Chow, E.J.; Fosse, I.; Lukoff, M.; Shim, M.M.; Uyeki, T.M.; Ogokeh, C.; et al. Trends in COVID-19 vaccination intent and factors associated with deliberation and reluctance among adult homeless shelter residents and staff, 1 November 2020 to 28 February 2021–King County, Washington. Vaccine 2022, 40, 122–132. [Google Scholar] [CrossRef] [PubMed]
- City of Toronto. City of Toronto Continues to Prioritize Access to Vaccinations for People Experiencing Homelessness with 154 COVID-19 Vaccination Clinics in January. Available online: https://www.toronto.ca/news/city-of-toronto-continues-to-prioritize-access-to-vaccinations-for-people-experiencing-homelessness-with-154-covid-19-vaccination-clinics-in-january/ (accessed on 31 March 2022).
- Richard, L.; Nisenbaum, R.; Liu, M.; McGeer, A.; Mishra, S.; Gingras, A.C.; Gommerman, J.L.; Sniderman, R.; Pedersen, C.; Spandier, O.; et al. Ku-gaa-gii pimitizi-win, the COVID-19 Prospective Cohort Study of People Experiencing Homelessness in Toronto, Canada: A study protocol. BMJ Open 2022, in press. [Google Scholar]
- Aiello, R. ‘Historic Moment’: Health Canada Approves Pfizer COVID-19 Vaccine. Available online: https://www.ctvnews.ca/health/coronavirus/historic-moment-health-canada-approves-pfizer-covid-19-vaccine-1.5223477 (accessed on 4 March 2022).
- Forani, J. Health Canada Approves ‘Game-Changer’ Moderna COVID-19 Vaccine. Available online: https://www.ctvnews.ca/health/coronavirus/health-canada-approves-game-changer-moderna-covid-19-vaccine-1.5242821 (accessed on 4 March 2021).
- Rabson, M.; Levitz, S. Canada Approves Oxford-AstraZeneca COVID-19 Vaccine for Immediate Use. Available online: https://www.cp24.com/news/canada-approves-oxford-astrazeneca-covid-19-vaccine-for-immediate-use-1.5325449?cache=yxtvsdvfhyq%3FautoPlay%3Dtrue (accessed on 4 March 2022).
- Jones, R.P. Health Canada Approves 4th COVID-19 Vaccine as Pfizer Agrees to Accelerate Deliveries. Available online: https://www.cbc.ca/news/politics/johnson-johnson-covid19-vaccine-approved-1.5937900 (accessed on 4 March 2022).
- Government of Ontario. News Release: Ontario Continues to Expand Eligibility for COVID-19 Vaccines to More Ontarians; Queen’s Printer for Ontario: Toronto, ON, Canada, 2021.
- Tsemberis, S.; McHugo, G.; Williams, V.; Hanrahan, P.; Stefancic, A. Measuring homelessness and residential stability: The residential time-line follow-back inventory. J. Community Psychol. 2007, 35, 29–42. [Google Scholar] [CrossRef] [Green Version]
- Goering, P.N.; Streiner, D.L.; Adair, C.; Aubry, T.; Barker, J.; Distasio, J.; Hwang, S.W.; Komaroff, J.; Latimer, E.; Somers, J.; et al. The At Home/Chez Soi trial protocol: A pragmatic, multi-site, randomized controlled trial of a Housing First intervention for homeless individuals with mental illness in five Canadian cities. BMJ Open 2011, 1, e000323. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Canadian Institute for Health Information. Proposed Standards for Race-Based and Indigenous Identity Data Collection and Health Reporting in Canada; CIHI: Ottawa, ON, Canada, 2020; Available online: www.cihi.ca/sites/default/files/rot/proposed-standard-for-race-based-data-en.pdf (accessed on 22 July 2022).
- Hutchins, H.J.; Wolff, B.; Leeb, R.; Ko, J.Y.; Odom, E.; Willey, J.; Friedman, A.; Bitsko, R.H. COVID-19 Mitigation Behaviors by Age Group–United States, April-June 2020. Morb. Mortal. Wkly. Rep. 2020, 69, 1584–1590. [Google Scholar] [CrossRef] [PubMed]
- Statistics Canada. COVID-19 Vaccination Coverage Survey (CVCS). Available online: https://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=5347#a3 (accessed on 22 July 2022).
- Wyllie, A.L.; Fournier, J.; Casanovas-Massana, A.; Campbell, M.; Tokuyama, M.; Vijayakumar, P.; Warren, J.L.; Geng, B.; Muenker, M.C.; Moore, A.J.; et al. Saliva or Nasopharyngeal Swab Specimens for Detection of SARS-CoV-2. N. Engl. J. Med. 2020, 383, 1283–1286. [Google Scholar] [CrossRef] [PubMed]
- Colwill, K.; Galipeau, Y.; Stuible, M.; Gervais, C.; Arnold, C.; Rathod, B.; Abe, K.T.; Wang, J.H.; Pasculescu, A.; Maltseva, M.; et al. A scalable serology solution for profiling humoral immune responses to SARS-CoV-2 infection and vaccination. Clin. Transl. Immunol. 2022, 11, e1380. [Google Scholar] [CrossRef] [PubMed]
- Agresti, A.; Coull, B.A. Approximate is better than “exact” for interval estimation of binomial proportions. Am. Stat. 1998, 52, 119–126. [Google Scholar]
- City of Toronto Vaccine Dashboard Data. Available online: https://www.toronto.ca/home/covid-19/covid-19-pandemic-data/covid-19-vaccine-data/ (accessed on 4 May 2022).
- Statistics Canada. Population and Dwelling Counts: Canada, Provinces and Territories, Census Metropolitan Areas and Census Agglomerations. Available online: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=9810000501 (accessed on 4 March 2022).
- Rubin, D.B. Multiple Imputation for Nonresponse in Surveys; Wiley-Interscience: New York, NY, USA, 2004. [Google Scholar]
- Swendeman, D.; Norwood, P.; Saleska, J.; Lewis, K.; Ramos, W.; SantaBarbara, N.; Sumstine, S.; Comulada, W.S.; Jimenez, S.; Ocasio, M.A. Vaccine Attitudes and COVID-19 Vaccine Intentions and Prevention Behaviors among Young People At-Risk for and Living with HIV in Los Angeles and New Orleans. Vaccines 2022, 10, 413. [Google Scholar] [CrossRef] [PubMed]
- Ortega, A.N.; Roby, D.H. Ending Structural Racism in the US Health Care System to Eliminate Health Care Inequities. JAMA 2021, 326, 613–615. [Google Scholar] [CrossRef] [PubMed]
- Mathieu, E.; Ritchie, H.; Ortiz-Ospina, E.; Roser, M.; Hasell, J.; Appel, C.; Giattino, C.; Rodés-Guirao, L. A global database of COVID-19 vaccinations. Nat. Hum. Behav. 2021, 5, 947–953. [Google Scholar] [CrossRef]
- City of Toronto. City of Toronto Continues to Protect and Assist People Experiencing Homelessness during the Ongoing COVID-19 Pandemic. Available online: https://www.toronto.ca/news/city-of-toronto-continues-to-protect-and-assist-people-experiencing-homelessness-during-the-ongoing-covid-19-pandemic/ (accessed on 4 March 2022).
- City of Toronto. Street Needs Assessment 2021: Attachment 1. Available online: https://www.toronto.ca/legdocs/mmis/2021/ec/bgrd/backgroundfile-171729.pdf (accessed on 31 January 2022).
- Gelberg, L.; Siecke, N. Accuracy of Homeless Adults’ Self-Reports. Med. Care 1997, 35, 287–290. [Google Scholar] [CrossRef]
- Draaisma, M. Resident of Toronto’s Largest Homeless Shelter Dies with COVID-19 as 50 Shelters Battle Outbreaks. Available online: https://www.cbc.ca/news/canada/toronto/shelter-resident-death-covid-19-outbreaks-toronto-1.6317072 (accessed on 31 January 2022).
- Vella, E. ‘It’s a scary time’: Several COVID-19 Outbreaks Reported at Toronto Shelters. Available online: https://globalnews.ca/news/8471736/covid-outbreaks-toronto-shelters/ (accessed on 31 January 2022).
- Draaisma, M. Toronto Reports COVID-19 Outbreaks at 20 Homeless Shelters, over 300 Cases, 1 Recent Death. Available online: https://www.cbc.ca/news/canada/toronto/toronto-shelters-in-outbreak-unhoused-people-one-death-covid-19-1.6003201 (accessed on 31 January 2022).
| Participant Characteristics | Total (n = 728) | No Dose (n = 143) | 1 + Dose (n = 585) | p-Value | |
|---|---|---|---|---|---|
| Age | Mean (SD) | 46.1 (14.7) | 39.1 (13.8) | 47.8 (14.4) | <0.001 |
| Median (IQR) | 46 (34–58) | 36 (28–48) | 48 (36–58) | <0.001 | |
| Self-reported gender | % Male | 481 (66.1%) | 83 (58.0%) | 398 (68.0%) | 0.07 |
| % Female | 228 (31.3%) | 56 (39.2%) | 172 (29.4%) | ||
| % Other | 17 (2.3%) | 4 (2.8%) | 13 (2.2%) | ||
| Missing 1 | 2 (0.3%) | 0 | 2 (0.3%) | ||
| Identifies as Indigenous | Yes | 75 (10.30%) | 12 (8.39%) | 63 (10.77%) | 0.38 |
| No | 631 (86.68%) | 128 (89.51%) | 503 (85.98%) | ||
| Missing 1 | 22 (3.02%) | 3 (2.10%) | 19 (3.25%) | ||
| Self-reported race | Black | 159 (21.84%) | 47 (32.87%) | 112 (19.15%) | 0.002 |
| Indigenous | 27 (3.71%) | 5 (3.50%) | 22 (3.76%) | ||
| White | 353 (48.49%) | 53 (37.06%) | 300 (51.28%) | ||
| Other/Multiracial | 156 (21.43%) | 31 (21.68%) | 125 (21.37%) | ||
| Missing 1 | 33 (4.53%) | 7 (4.90%) | 26 (4.44%) | ||
| Citizenship status | Citizen | 556 (76.4%) | 112 (78.3%) | 444 (75.9%) | 0.20 |
| Landed Immigrant | 90 (12.4%) | 11 (7.7%) | 79 (13.5%) | ||
| Refugee | 55 (7.6%) | 11 (7.7%) | 44 (7.5%) | ||
| Temporary/Other | 20 (2.8%) | 6 (4.2%) | 14 (2.4%) | ||
| Missing 1 | 7 (1.0%) | 3 (2.1%) | 3 (0.7%) | ||
| Highest level of education completed | Less than high school | 206 (28.3%) | 33 (23.1%) | 173 (29.6%) | 0.01 |
| High school | 251 (34.5%) | 65 (45.5%) | 186 (31.8%) | ||
| Any post-secondary | 262 (36.0%) | 44 (30.8%) | 218 (37.3%) | ||
| Missing 1 | 9 (1.2%) | 1 (0.7%) | 8 (1.4%) | ||
| Engaged in paid work since March 2020 | 165 (22.7%) | 44 (30.8%) | 121 (20.7%) | 0.01 | |
| Primary housing type in past 90 days | Homeless shelter | 287 (39.4%) | 49 (34.3%) | 238 (40.7%) | 0.009 |
| Distancing hotel | 328 (45.1%) | 60 (42.0%) | 268 (45.8%) | ||
| Other setting | 113 (15.5%) | 34 (23.8%) | 79 (13.5%) | ||
| Presence of chronic condition(s) 2 | 350 (48.1%) | 57 (39.9%) | 293 (50.1%) | 0.028 | |
| Body mass index category | Underweight/normal | 333 (45.7%) | 61 (42.7%) | 272 (46.5%) | 0.46 |
| Overweight | 226 (31.0%) | 51 (35.7%) | 175 (29.9%) | ||
| Obese | 140 (19.2%) | 27 (18.9%) | 113 (19.3%) | ||
| Missing 1 | 29 (4.0%) | 4 (2.8%) | 25 (4.3%) | ||
| Influenza vaccine in past season | 217 (29.8%) | 13 (9.1%) | 204 (34.9%) | <0.001 | |
| Following Public Health Guidelines: wear face mask in public | Low (never/rarely/occasionally) | 93 (12.9%) | 30 (21.1%) | 63 (10.8%) | 0.001 |
| High (often/always) | 630 (87.1%) | 112 (78.9%) | 518 (89.2%) | ||
| Missing 1 | 5 (0.7%) | 1 (0.7%) | 4 (0.7%) | ||
| Following Public Health Guidelines: distancing in public places | Low (never/rarely/occasionally) | 103 (14.3%) | 26 (18.4%) | 77 (13.3%) | 0.12 |
| High (often/always) | 615 (85.7%) | 115 (81.6%) | 500 (86.7%) | ||
| Missing 1 | 10 (1.8%) | 2 (1.4%) | 8 (1.4%) | ||
| Following Public Health Guidelines: avoid crowded places or gatherings | Low (never/rarely/occasionally) | 136 (19.1%) | 36 (25.7%) | 100 (17.5%) | 0.026 |
| High (often/always) | 577 (80.9%) | 104 (74.3%) | 473 (82.6%) | ||
| Missing 1 | 15 (2.1%) | 3 (2.1%) | 12 (2.1%) | ||
| Following Public Health Guidelines: wash hands with soap/sanitizer several times per day | Low (never/rarely/occasionally) | 72 (10.0%) | 17 (12.0%) | 55 (9.5%) | 0.37 |
| High (often/always) | 651 (90.0%) | 125 (88.0%) | 526 (90.5%) | ||
| Missing 1 | 5 (0.7%) | 1 (0.7%) | 4 (0.7%) | ||
| Participant Characteristics | Adjusted Rate Ratio | 95% CI | p-Value | |
|---|---|---|---|---|
| Age (per ten years) | 1.05 | 1.03–1.08 | <0.001 | |
| Self-reported gender | Male (ref) | N/A | ||
| Female | 0.92 | 0.85–1.00 | 0.040 | |
| Other | 1.07 | 0.82–1.41 | 0.604 | |
| Self-reported race | White (ref) | N/A | ||
| Black | 0.89 | 0.80–0.99 | 0.033 | |
| Indigenous | 0.99 | 0.83–1.19 | 0.930 | |
| Other/Multiracial | 1.00 | 0.92–1.08 | 0.957 | |
| Received influenza vaccine in past season | No (ref) | N/A | ||
| Yes | 1.19 | 1.11–1.27 | <0.001 | |
| Frequency of masking in public places | Often/Always (ref) | N/A | ||
| Never/Rarely/Occasionally | 0.83 | 0.72–0.95 | 0.009 | |
| Primary housing type in past 90 days | Homeless shelter/Physical distancing hotel (ref) | N/A | ||
| Other settings | 0.93 | 0.82–1.05 | 0.222 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Richard, L.; Liu, M.; Jenkinson, J.I.R.; Nisenbaum, R.; Brown, M.; Pedersen, C.; Hwang, S.W. COVID-19 Vaccine Coverage and Sociodemographic, Behavioural and Housing Factors Associated with Vaccination among People Experiencing Homelessness in Toronto, Canada: A Cross-Sectional Study. Vaccines 2022, 10, 1245. https://doi.org/10.3390/vaccines10081245
Richard L, Liu M, Jenkinson JIR, Nisenbaum R, Brown M, Pedersen C, Hwang SW. COVID-19 Vaccine Coverage and Sociodemographic, Behavioural and Housing Factors Associated with Vaccination among People Experiencing Homelessness in Toronto, Canada: A Cross-Sectional Study. Vaccines. 2022; 10(8):1245. https://doi.org/10.3390/vaccines10081245
Chicago/Turabian StyleRichard, Lucie, Michael Liu, Jesse I. R. Jenkinson, Rosane Nisenbaum, Michael Brown, Cheryl Pedersen, and Stephen W. Hwang. 2022. "COVID-19 Vaccine Coverage and Sociodemographic, Behavioural and Housing Factors Associated with Vaccination among People Experiencing Homelessness in Toronto, Canada: A Cross-Sectional Study" Vaccines 10, no. 8: 1245. https://doi.org/10.3390/vaccines10081245
APA StyleRichard, L., Liu, M., Jenkinson, J. I. R., Nisenbaum, R., Brown, M., Pedersen, C., & Hwang, S. W. (2022). COVID-19 Vaccine Coverage and Sociodemographic, Behavioural and Housing Factors Associated with Vaccination among People Experiencing Homelessness in Toronto, Canada: A Cross-Sectional Study. Vaccines, 10(8), 1245. https://doi.org/10.3390/vaccines10081245





