Barriers and Facilitators to Receiving the COVID-19 Vaccination and Development of Theoretically-Informed Implementation Strategies for the Public: Qualitative Study in Hong Kong
Abstract
:1. Introduction
2. Methods
2.1. Identification of Barriers and Facilitators to Receiving COVID-19 Vaccination
2.1.1. Study Sampling
2.1.2. Data Collection
2.1.3. Data Analysis
2.2. Development of Theoretically-Informed Implementation Strategies to Improve Uptake of COVID-19 Vaccination
3. Results
3.1. Identification of Barriers and Facilitators to Receiving COVID-19 Vaccination
3.1.1. Participants
3.1.2. Barriers and Facilitators
3.1.3. Knowledge
3.1.4. Beliefs about Capabilities
3.1.5. Goals
3.1.6. Social Influences
3.1.7. Beliefs about Consequences
3.1.8. Intentions
3.1.9. Reinforcement
3.1.10. Memory, Attention, and Decision Processes
3.1.11. Social/Professional Role and Identity
3.1.12. Optimism
3.1.13. Environmental Context and Resources
3.1.14. Emotion
3.2. Development of Theoretically-Informed Implementation Strategies to Improve Uptake of COVID-19 Vaccination
3.2.1. Providing Reliable COVID-19 Vaccine-Related Information and Scaling up the Promotion of COVID-19 Vaccination
3.2.2. Engaging Healthcare Professionals to Recommend Vaccination for Individuals
3.2.3. Giving Rewards
3.2.4. Using Social Influence Approaches
3.2.5. Allowing Selection of COVID-19 Vaccines According to Individual’s Choice
3.2.6. Increasing Accessibility of the COVID-19 Vaccination
3.2.7. Emphasizing on Social Responsibility
4. Discussion
4.1. Summary of Findings
4.2. Comparison with Current Literature
4.3. Implications
4.4. Providing Reliable COVID-19 Vaccine-Related Information and Scaling up the Promotion of COVID-19 Vaccinations
4.5. Engaging Healthcare Professionals to Recommend Vaccinations for Individuals
4.6. Incentive and Social Influence Approaches
4.7. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Semi-Structured Interview Guide Developed Based on the Theoretical Domains Framework (TDF)
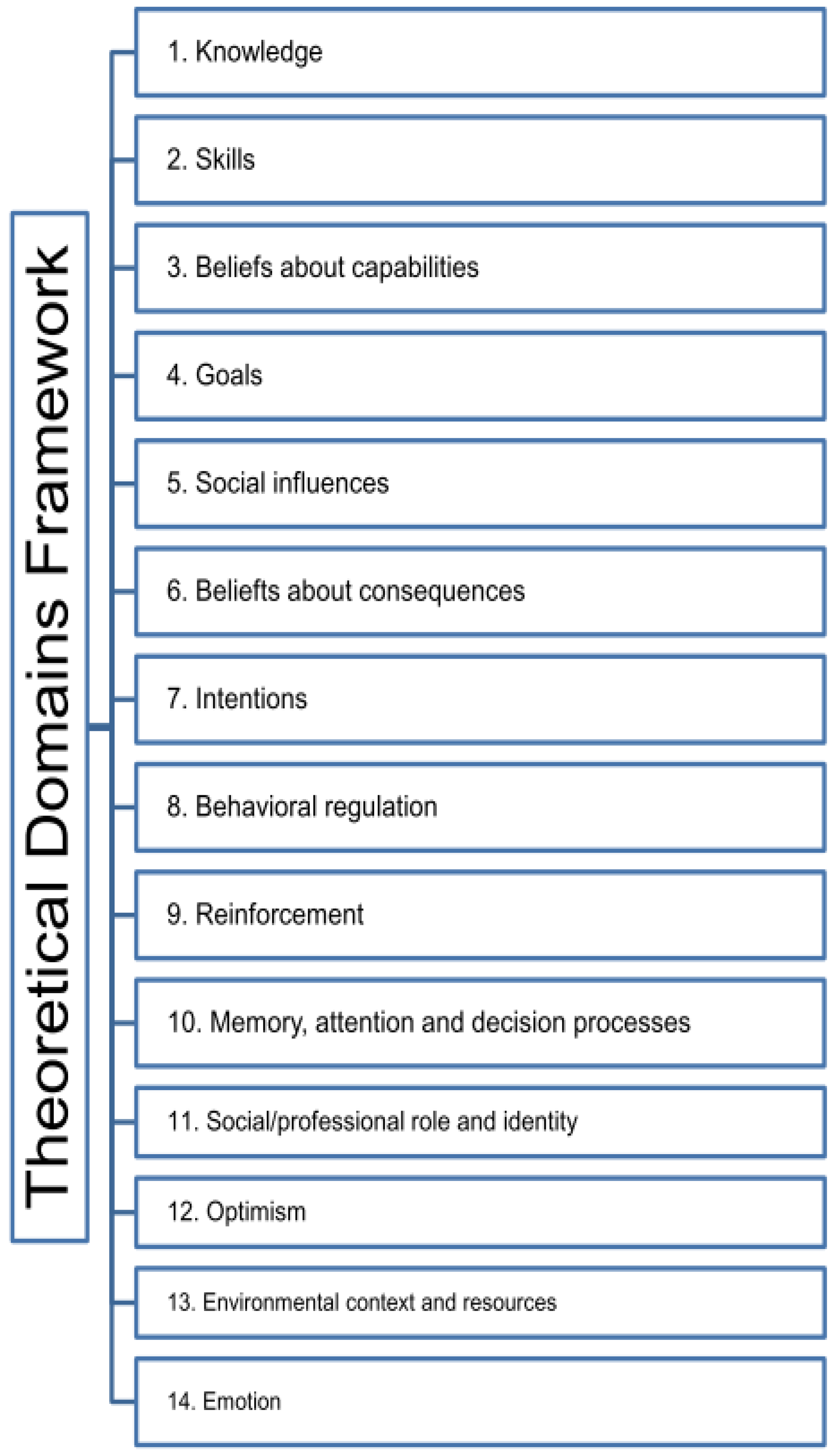
Appendix B. The 14 Domains of TDF
References
- Long, A.; Ascent, D. World Economic Outlook; International Monetary Fund: Washington, DC, USA, 2020. [Google Scholar] [CrossRef]
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard. 2022. Available online: https://covid19.who.int (accessed on 24 February 2022).
- Centers for Disease Control and Prevention. Ensuring COVID-19 Vaccines Work. 2021. Available online: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/effectiveness.html (accessed on 25 June 2021).
- Wouters, O.J.; Shadlen, K.C.; Salcher-Konrad, M.; Pollard, A.J.; Larson, H.J.; Teerawattananon, Y.; Jit, M. Challenges in ensuring global access to COVID-19 vaccines: Production, affordability, allocation, and deployment. Lancet 2021, 397, 1023–1034. [Google Scholar] [CrossRef]
- World Health Organization. Ten Threats to Global Health in 2019. 2021. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 25 June 2021).
- Sethi, S.; Kumar, A.; Mandal, A.; Shaikh, M.; A Hall, C.; Kirk, J.M.W.; Moss, P.; Brookes, M.J.; Basu, S. The UPTAKE study: A cross-sectional survey examining the insights and beliefs of the UK population on COVID-19 vaccine uptake and hesitancy. BMJ Open 2021, 11, e048856. [Google Scholar] [PubMed]
- Chen, M.; Li, Y.; Chen, J.; Wen, Z.; Feng, F.; Zou, H.; Fu, C.; Chen, L.; Shu, Y.; Sun, C. An online survey of the attitude and willingness of Chinese adults to receive COVID-19 vaccination. Hum. Vaccines Immunother. 2021, 17, 2279–2288. [Google Scholar] [CrossRef]
- Wang, K.; Wong, E.L.-Y.; Ho, K.-F.; Cheung, A.W.-L.; Yau, P.S.-Y.; Dong, D.; Wong, S.Y.-S.; Yeoh, E.-K. Change of willingness to accept COVID-19 vaccine and reasons of vaccine hesitancy of working people at different waves of local epidemic in Hong Kong, China: Repeated cross-sectional surveys. Vaccines 2021, 9, 62. [Google Scholar] [CrossRef] [PubMed]
- Wong, M.C.S.; Wong, E.L.Y.; Huang, J.; Cheung, A.W.L.; Law, K.; Chong, M.K.C.; Ng, R.W.Y.; Lai, C.K.C.; Boon, S.S.; Lau, J.T.F.; et al. Acceptance of the COVID-19 vaccine based on the health belief model: A population-based survey in Hong Kong. Vaccine 2021, 39, 1148–1156. [Google Scholar] [CrossRef] [PubMed]
- Hong Kong SAR. Hong Kong Vaccination Dashboard. 2021. Available online: https://www.covidvaccine.gov.hk/en/ (accessed on 28 June 2021).
- Lin, Y.; Hu, Z.; Zhao, Q.; Alias, H.; Danaee, M.; Wong, L.P. Understanding COVID-19 vaccine demand and hesitancy: A nationwide online survey in China. PLoS Negl. Trop. Dis. 2020, 14, e0008961. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Zhang, J.; Wu, W.; Liang, M.; Wu, Q.-S. Willingness to receive future COVID-19 vaccines following the COVID-19 epidemic in Shanghai, China. BMC Public Health 2021, 21, 1103. [Google Scholar] [CrossRef]
- Machida, M.; Nakamura, I.; Kojima, T.; Saito, R.; Nakaya, T.; Hanibuchi, T.; Takamiya, T.; Odagiri, Y.; Fukushima, N.; Kikuchi, H.; et al. Acceptance of a COVID-19 Vaccine in Japan during the COVID-19 Pandemic. Vaccines 2021, 9, 210. [Google Scholar] [CrossRef]
- Reiter, P.L.; Pennell, M.L.; Katz, M.L. Acceptability of a COVID-19 vaccine among adults in the United States: How many people would get vaccinated? Vaccine 2020, 38, 6500–6507. [Google Scholar] [CrossRef]
- Bell, S.; Clarke, R.; Mounier-Jack, S.; Walker, J.L.; Paterson, P. Parents’ and guardians’ views on the acceptability of a future COVID-19 vaccine: A multi-methods study in England. Vaccine 2020, 38, 7789–7798. [Google Scholar] [CrossRef]
- Williams, S.N.; Dienes, K.A. Public attitudes to COVID-19 vaccines: A qualitative study. medRxiv 2021, 21257092. [Google Scholar] [CrossRef]
- Kumari, A.; Ranjan, P.; Chopra, S.; Kaur, D.; Kaur, T.; Kalanidhi, K.B.; Goel, A.; Singh, A.; Baitha, U.; Prakash, B.; et al. What Indians Think of the COVID-19 vaccine: A qualitative study comprising focus group discussions and thematic analysis. Diabetes Metab. Syndr. Clin. Res. Rev. 2021, 15, 679–682. [Google Scholar] [CrossRef] [PubMed]
- Hennink, M.M.; Kaiser, B.N.; Marconi, V.C. Code saturation versus meaning saturation: How many interviews are enough? Qual. Health Res. 2017, 27, 591–608. [Google Scholar] [CrossRef] [PubMed]
- Atkins, L.; Francis, J.; Islam, R.; O’Connor, D.; Patey, A.; Ivers, N.; Foy, R.; Duncan, E.; Colquhoun, H.; Grimshaw, J.M.; et al. A guide to using the Theoretical Domains Framework of behaviour change to investigate implementation problems. Implement. Sci. 2017, 12, 77. [Google Scholar] [CrossRef]
- Elo, S.; Kyngäs, H. The qualitative content analysis process. J. Adv. Nurs. 2008, 62, 107–115. [Google Scholar] [CrossRef]
- MacDonald, N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- Cane, J.; O’Connor, D.; Michie, S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement. Sci. 2012, 7, 37. [Google Scholar] [CrossRef] [Green Version]
- A Wilkinson, S.; Thomas, S.; Phillips, C.J.; Marshall, A.P.; Chaves, N.J.; Jankelowitz, S.K.; Lin, I.B.; Loy, C.T.; Rees, G.; Sakzewski, L.; et al. Experiences of using the Theoretical Domains Framework across diverse clinical environments: A qualitative study. J. Multidiscip. Healthc. 2015, 8, 139. [Google Scholar] [CrossRef] [Green Version]
- Nilsen, P. Making sense of implementation theories, models and frameworks. Implement. Sci. 2015, 10, 53–79. [Google Scholar] [CrossRef] [Green Version]
- Dhakal, K. NVivo. J. Med. Libr. Assoc. 2022, 110, 270. [Google Scholar] [CrossRef]
- Michie, S.; Atkins, L.; West, R. The Behaviour Change Wheel: A Guide to Designing Interventions; Silverback Publishing: Sutton, UK, 2015. [Google Scholar]
- Michie, S.; Richardson, M.; Johnston, M.; Abraham, C.; Francis, J.; Hardeman, W.; Eccles, M.P.; Cane, J.; Wood, C.E. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Ann. Behav. Med. 2013, 46, 81–95. [Google Scholar] [CrossRef] [PubMed]
- Michie, S.; Johnston, M.; Francis, J.; Hardeman, W.; Eccles, M. From theory to intervention: Mapping theoretically derived behavioural determinants to behaviour change techniques. Appl. Psychol. 2008, 57, 660–680. [Google Scholar] [CrossRef]
- Cane, J.; Richardson, M.; Johnston, M.; Ladha, R.; Michie, S. From lists of behaviour change techniques (BCT s) to structured hierarchies: Comparison of two methods of developing a hierarchy of BCT s. Br. J. Health Psychol. 2015, 20, 130–150. [Google Scholar] [CrossRef] [PubMed]
- Taylor, N.; Lawton, R.; Moore, S.J.; Craig, J.; Slater, B.; Cracknell, A.; Wright, J.P.; A Mohammed, M. Collaborating with front-line healthcare professionals: The clinical and cost effectiveness of a theory based approach to the implementation of a national guideline. BMC Health Serv. Res. 2014, 14, 648. [Google Scholar] [CrossRef] [Green Version]
- Debono, D.; Taylor, N.; Lipworth, W.; Greenfield, D.; Travaglia, J.; Black, D.; Braithwaite, J. Applying the theoretical domains framework to identify barriers and targeted interventions to enhance nurses’ use of electronic medication management systems in two Australian hospitals. Implement. Sci. 2017, 12, 42. [Google Scholar] [CrossRef] [Green Version]
- Craig, L.E.; Taylor, N.; Grimley, R.; Cadilhac, D.A.; McInnes, E.; Phillips, R.; Dale, S.; O’Connor, D.; Levi, C.; Fitzgerald, M.; et al. Development of a theory-informed implementation intervention to improve the triage, treatment and transfer of stroke patients in emergency departments using the Theoretical Domains Framework (TDF): The T 3 Trial. Implement. Sci. 2017, 12, 88. [Google Scholar] [CrossRef]
- Chou, W.-Y.S.; Budenz, A. Considering emotion in COVID-19 vaccine communication: Addressing vaccine hesitancy and fostering vaccine confidence. Health Commun. 2020, 35, 1718–1722. [Google Scholar] [CrossRef]
- Griffith, J.; Marani, H.; Monkman, H. COVID-19 Vaccine Hesitancy in Canada: Content Analysis of Tweets Using the Theoretical Domains Framework. J. Med. Internet Res. 2021, 23, e26874. [Google Scholar] [CrossRef]
- Cerda, A.A.; García, L.Y. Hesitation and Refusal Factors in Individuals’ Decision-Making Processes Regarding a Coronavirus Disease 2019 Vaccination. Front. Public Health 2021, 9, 626852. [Google Scholar] [CrossRef]
- Williams, L.; Gallant, A.J.; Rasmussen, S.; Nicholls, L.A.B.; Cogan, N.; Deakin, K.; Young, D.; Flowers, P. Towards intervention development to increase the uptake of COVID-19 vaccination among those at high risk: Outlining evidence-based and theoretically informed future intervention content. Br. J. Health Psychol. 2020, 25, 1039–1054. [Google Scholar] [CrossRef]
- Fabry, P.; Gagneur, A.; Pasquier, J.-C. Determinants of A (H1N1) vaccination: Cross-sectional study in a population of pregnant women in Quebec. Vaccine 2011, 29, 1824–1829. [Google Scholar] [CrossRef] [PubMed]
- Levin-Zamir, D. Communication, Health Literacy and a Systems Approach for Mitigating the COVID-19 Pandemic: The Case for Massive Vaccine Roll-out in Israel. J. Health Commun. 2020, 25, 816–818. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, N.E.; Comeau, J.; Dubé, E.; Bucci, L.; Graham, J.E. A public health timeline to prepare for COVID-19 vaccines in Canada. Can. J. Public Health 2020, 111, 945–952. [Google Scholar] [CrossRef] [PubMed]
- Volpp, K.G.; Loewenstein, G.; Buttenheim, A.M. Behaviorally informed strategies for a national COVID-19 vaccine promotion program. JAMA 2021, 325, 125–126. [Google Scholar] [CrossRef] [PubMed]
- Laine, C.; Cotton, D.; Moyer, D.V. COVID-19 vaccine: Promoting vaccine acceptance. Ann. Intern. Med. 2021, 174, 252–253. [Google Scholar] [CrossRef]
- Ogilvie, G.S.; Gordon, S.; Smith, L.W.; Albert, A.; Racey, C.S.; Booth, A.; Gottschlich, A.; Goldfarb, D.; Murray, M.C.M.; Galea, L.A.M.; et al. Intention to receive a COVID-19 vaccine: Results from a population-based survey in Canada. BMC Public Health 2021, 21, 1017. [Google Scholar] [CrossRef]
- Schmelz, K.; Bowles, S. Overcoming COVID-19 vaccination resistance when alternative policies affect the dynamics of conformism, social norms, and crowding out. Proc. Natl. Acad. Sci. USA 2021, 118, e2104912118. [Google Scholar] [CrossRef]
- Afifi, T.O.; Salmon, S.; Taillieu, T.; Stewart-Tufescu, A.; Fortier, J.; Driedger, S.M. Older adolescents and young adults willingness to receive the COVID-19 vaccine: Implications for informing public health strategies. Vaccine 2021, 39, 3473–3479. [Google Scholar] [CrossRef]
- Buckner, J.H.; Chowell, G.; Springborn, M.R. Dynamic prioritization of COVID-19 vaccines when social distancing is limited for essential workers. Proc. Natl. Acad. Sci. USA 2021, 118, e2025786118. [Google Scholar] [CrossRef]
- Matrajt, L.; Eaton, J.; Leung, T.; Brown, E.R. Vaccine optimization for COVID-19: Who to vaccinate first? Sci. Adv. 2021, 7, eabf1374. [Google Scholar] [CrossRef]
- Giubilini, A.; Savulescu, J.; Wilkinson, D. COVID-19 vaccine: Vaccinate the young to protect the old? J. Law Biosci. 2020, 7, lsaa050. [Google Scholar] [CrossRef] [PubMed]
- Polaha, J.; Johnson, L.; Quinn, M.; Sunderji, N. Lessons from the team care playbook: Recommendations for COVID-19 vaccination dissemination and uptake. Fam. Syst. Health 2020, 38, 341–345. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, J. Populist politics and vaccine hesitancy in Western Europe: An analysis of national-level data. Eur. J. Public Health 2019, 29, 512–516. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.; Lau, J.T.; Lau, M.; Wong, M.; Chan, P.K. Understanding the prevalence and associated factors of behavioral intention of COVID-19 vaccination under specific scenarios combining effectiveness, safety, and cost in the Hong Kong Chinese general population. Int. J. Health Policy Manag. 2021; in press. [Google Scholar] [CrossRef]
- Giubilini, A. Vaccination ethics. Br. Med. Bull. 2021, 137, 4–12. [Google Scholar] [CrossRef] [PubMed]
- Richards, H.M.; Schwartz, L.J. Ethics of qualitative research: Are there special issues for health services research? Fam. Pract. 2002, 19, 135–139. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Quinney, L.; Dwyer, T.; Chapman, Y. Who, where, and how of interviewing peers: Implications for a phenomenological study. Sage Open 2016, 6, 2158244016659688. [Google Scholar] [CrossRef] [Green Version]
- Hong Kong SAR. Census and Statistics Department. Use of Language in Hong Kong in 2018. 2020. Available online: https://www.censtatd.gov.hk/en/data/stat_report/product/FA100270/att/B72001FB2020XXXXB0100.pdf (accessed on 24 April 2022).
- Bergen, N.; Labonté, R. “Everything is perfect, and we have no problems”: Detecting and limiting social desirability bias in qualitative research. Qual. Health Res. 2020, 30, 783–792. [Google Scholar] [CrossRef]
| Sociodemographic Characteristics | Willing (n = 15) | Unwilling (n = 15) | Uncertain (n = 15) | Total (n = 45) |
|---|---|---|---|---|
| Gender | ||||
| 7 | 4 | 6 | 17 |
| 8 | 11 | 9 | 28 |
| Age (years) | ||||
| 5 | 5 | 5 | 15 |
| 5 | 5 | 5 | 15 |
| 5 | 5 | 5 | 15 |
| Chronic disease or not | ||||
| 7 | 5 | 5 | 17 |
| 8 | 10 | 10 | 28 |
| Education | ||||
| 0 | 0 | 2 | 2 |
| 9 | 7 | 5 | 21 |
| 6 | 8 | 8 | 22 |
| Family monthly household income (HKD) | ||||
| 1 | 2 | 0 | 3 |
| 4 | 1 | 4 | 9 |
| 4 | 4 | 2 | 10 |
| 6 | 8 | 9 | 23 |
| Living area | ||||
| 1 | 0 | 1 | 2 |
| 6 | 6 | 4 | 16 |
| 8 | 9 | 10 | 27 |
| Marital status | ||||
| 4 | 4 | 2 | 10 |
| 10 | 10 | 11 | 31 |
| 1 | 1 | 2 | 4 |
| Perceived health status | ||||
| 1 | 5 | 2 | 8 |
| 8 | 4 | 8 | 20 |
| 6 | 6 | 5 | 17 |
| TDF Domain | Facilitators | Barriers |
|---|---|---|
| Knowledge | Knowledge about COVID-19 (n = 19) | Unclear information related to the Hong Kong COVID-19 vaccination program (n = 23) * |
| Professional advice on COVID-19 vaccination are needed (n = 18) | Insufficient data on safety and effectiveness of the COVID-19 vaccines (n = 19) * | |
| Knowledge about COVID-19 vaccines (n = 18) ^ | Knowledge about COVID-19 (n = 9) & | |
| Up-to-date local and international clinical data on safety and effectiveness of COVID-19 vaccines should be provided (n = 18) @ | ||
| Sufficient information related to the Hong Kong COVID-19 vaccination program are needed (n = 13) | ||
| Beliefs about capabilities | Perceived risk of getting COVID-19 among vulnerable population 1 (n = 21) | Perceived high risk of adverse events after receiving the COVID-19 vaccination among vulnerable population 1 (n = 12) & |
| Perceived possible risk of contracting COVID-19 (n = 14) | Perceived low risk of contracting COVID-19 (n = 9) ^ & | |
| Perceived vulnerability of contracting COVID-19 among healthcare professionals (n = 7) | ||
| Goals | Herd immunity against COVID-19 would be considered an incentive (n = 9) | Herd immunity against COVID-19 may not be effective enough to protect the public (n = 3) |
| Social influences | Healthcare professionals’ recommendations on COVID-19 vaccination (n = 34) * | Low level of trust in the government (n = 2) |
| COVID-19 vaccine-related health education delivered by healthcare professionals (n = 33) * | Family members and friends’ suggestions on the COVID-19 vaccination (n = 1) | |
| Healthcare professionals serve as role models for receiving the COVID-19 vaccination (n = 26) | ||
| Family members and friends’ suggestions/their sharing of experiences on receiving the COVID-19 vaccination (n = 17) | ||
| Government leaders serve as role models for receiving the COVID-19 vaccination (n = 14) | ||
| Government’s suggestions on the COVID-19 vaccination (n = 7) | ||
| Social influences (cont.) | COVID-19 vaccine-related health education delivered by government (n = 2) | |
| B eliefs about consequences | Perceived potential in protecting against COVID-19 (n = 16) ^ | Concerns on severe and long-term side effects of COVID-19 vaccines, such as numbness, chest discomfort, Bell’s palsy, stroke, and even death (n = 29) * |
| Beliefs of protecting elderly and chronic disease patients against COVID-19 (n = 7) | Perceived low protection ability against COVID-19 conferred by the vaccines (n = 16) * | |
| Perceived positive expectations on the effectiveness and side effects of COVID-19 vaccines (n = 6) | Concerns on negative impact to family members after receiving the COVID-19 vaccination (n = 3) | |
| Concerns on negative impacts to work after receiving the COVID-19 vaccination (n = 1) | ||
| Intentions | Perceived benefits outweigh risks of mild and short-term side effects of COVID-19 vaccines (n = 30) * | |
| Reinforcement | Easing of travel restrictions and relaxation of social distancing measures as incentives (n = 14) | Easing of travel restrictions and relaxation of social distancing measures as incentives would make public feel negative towards receiving the COVID-19 vaccination (n = 1) |
| Free COVID-19 vaccines as incentives, particularly for people who have financial difficulties (n = 10) | Free COVID-19 vaccines pose concerns on hidden agenda related to promoting vaccination (n = 1) | |
| Cash incentives (n = 1) | Cash incentives would further reduce public’s confidence towards COVID-19 vaccines, as it is perceived as a mean to advance a hidden agenda (n = 1) | |
| Purchase insurance for people who are willing to receive the COVID-19 vaccination as an incentive (n = 1) | ||
| Health Care voucher as incentives (n = 1) | ||
| Memory, attention and decision processes | Have the right to select types of COVID-19 vaccines according to personal wills (n = 27) & @ | Fear of needles and allergic reaction to COVID-19 vaccines (n = 3) |
Criteria for choosing COVID-19 vaccines:
| Previous negative experience of receiving vaccination in chronic disease patients (n = 3) | |
| Social/professional role and identity | Work environment with higher risk of COVID-19 exposure (n = 11) | |
| Organizational commitment to promoting COVID-19 vaccinations (n = 7) | ||
| Leadership/influence on others (n = 3) | ||
| Social responsibility for receiving COVID-19 vaccinations (n = 2) | ||
| Optimism | Hope in resuming normal social life by after full vaccination (n = 31) * | Low confidence in the safety and effectiveness of COVID-19 vaccines due to concerns on their accelerated development. This has reduced the expected benefits of receiving the vaccination (n = 27) * |
| High confidence in the benefits of receiving COVID-19 vaccination (n = 15) ^ | Perceived ineffectiveness in COVID-19 pandemic control despite vaccine availability (n = 9) @ | |
| Perceived effective control of the COVID-19 pandemic with mass vaccination (n = 14) | Perceived low importance of COVID-19 vaccination (n = 2) | |
| Perceived difficulties in the implementation of the COVID-19 vaccination program (n = 1) | ||
| Environmental context and resources | Sources of obtaining COVID-19 vaccine-related information:
| Low trustworthiness of COVID-19 vaccine-related information (n = 6) |
Criteria for determining locations for receiving COVID-19 vaccination:
| ||
| High trustworthiness of COVID-19 vaccine-related information (n = 17) | ||
| Negative impact of COVID-19 pandemic (n = 10) | ||
| Online booking to avoid crowds (n = 8) | ||
| Workplace outreach vaccination program (n = 1) | ||
| Emotion | Impact of the unpleasant feelings caused by the COVID-19 pandemic triggers willingness to be vaccinated (n = 8) | |
| Psychosocial support programs for the public during the COVID-19 pandemic are needed to instill confidence in vaccination (n = 2) |
| Implementation Strategies | Details | Relevant BCTs |
|---|---|---|
| (1) Providing trustworthy COVID-19 vaccine-related information and scaling up the promotion of COVID-19 vaccination | Channels:
|
|
|
| |
|
| |
|
| |
(e.g., newspapers, TV, radio, etc.) |
| |
| (2) Encouraging healthcare professionals to recommend vaccination for individuals |
|
|
| (3) Giving rewards |
|
|
| (4) Using social influence approaches | Healthcare professionals and Hong Kong government leaders
Family members and friends:
|
|
Social support:
|
| |
| (5) Allowing a selection of COVID-19 vaccines according to the individual’s will | Selection criteria include:
|
|
| (6) Increasing accessibility for receiving COVID-19 vaccination | Criteria include:
|
|
| (7) Emphasizing on social responsibility |
|
|
| Facilitators to Implementation | Barriers to Implementation |
|---|---|
| Healthcare professionals’ recommendations on the COVID-19 vaccination (n = 34) | Concerns on severe and long-term side effects caused by COVID-19 vaccines (n = 29) |
| News from TV, radio, and newspapers as main sources for obtaining COVID-19 vaccine-related information (n = 34) | Low confidence in the safety and effectiveness of COVID-19 vaccines due to concerns of their accelerated development, leading to lower expected benefits of receiving the vaccination (n = 27) |
| COVID-19 vaccine-related health education delivered by healthcare professionals (n = 33) | Unclear information on logistical arrangements of the Hong Kong COVID-19 vaccination program (n = 23) |
| Expectation of resuming to a normal social life by getting fully vaccinated (n = 31) | Insufficient data on safety and effectiveness of the COVID-19 vaccines (n = 19) |
| Perceived benefits outweigh the risks of mild and short-term side effects of COVID-19 vaccines (n = 30) | Perceived low protection ability against COVID-19 conferred by the vaccines (n = 16) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wong, C.H.; Zhong, C.C.; Chung, V.C.; Nilsen, P.; Wong, E.L.; Yeoh, E.-k. Barriers and Facilitators to Receiving the COVID-19 Vaccination and Development of Theoretically-Informed Implementation Strategies for the Public: Qualitative Study in Hong Kong. Vaccines 2022, 10, 764. https://doi.org/10.3390/vaccines10050764
Wong CH, Zhong CC, Chung VC, Nilsen P, Wong EL, Yeoh E-k. Barriers and Facilitators to Receiving the COVID-19 Vaccination and Development of Theoretically-Informed Implementation Strategies for the Public: Qualitative Study in Hong Kong. Vaccines. 2022; 10(5):764. https://doi.org/10.3390/vaccines10050764
Chicago/Turabian StyleWong, Charlene Hl, Claire Cw Zhong, Vincent Ch Chung, Per Nilsen, Eliza Ly Wong, and Eng-kiong Yeoh. 2022. "Barriers and Facilitators to Receiving the COVID-19 Vaccination and Development of Theoretically-Informed Implementation Strategies for the Public: Qualitative Study in Hong Kong" Vaccines 10, no. 5: 764. https://doi.org/10.3390/vaccines10050764
APA StyleWong, C. H., Zhong, C. C., Chung, V. C., Nilsen, P., Wong, E. L., & Yeoh, E.-k. (2022). Barriers and Facilitators to Receiving the COVID-19 Vaccination and Development of Theoretically-Informed Implementation Strategies for the Public: Qualitative Study in Hong Kong. Vaccines, 10(5), 764. https://doi.org/10.3390/vaccines10050764






