Internal and External Motivations and Risk Perception toward COVID-19 Vaccination in Adolescents in the U.S.
Abstract
:1. Introduction
2. Methods
2.1. Participants and Data Collection
2.2. Measures
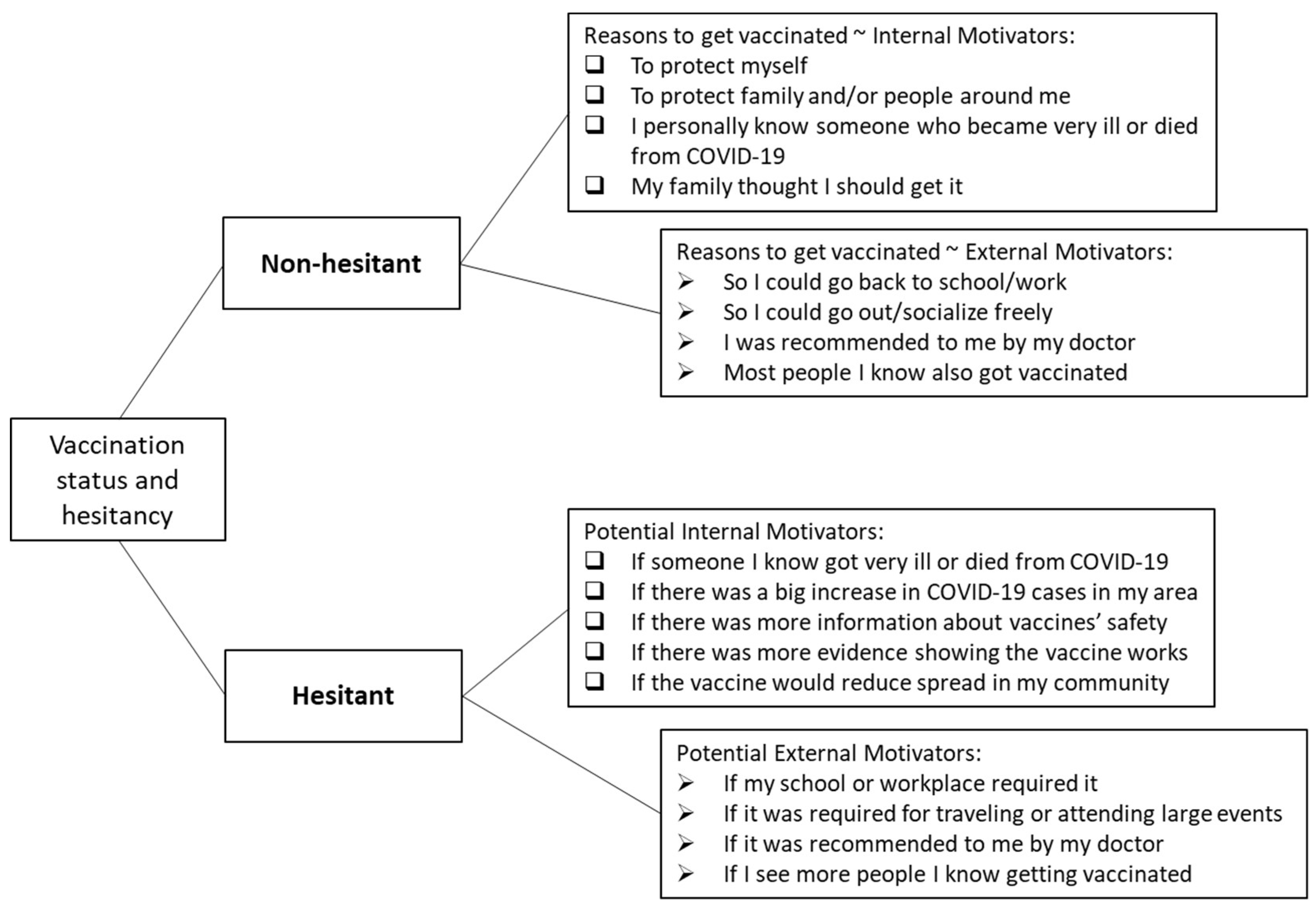
2.2.1. Vaccination Status and Hesitation
2.2.2. Internal vs. External Motivation
2.2.3. Risk Perception
2.2.4. Perceived Knowledge
2.3. Data Analysis
3. Results
3.1. Participant Characteristics
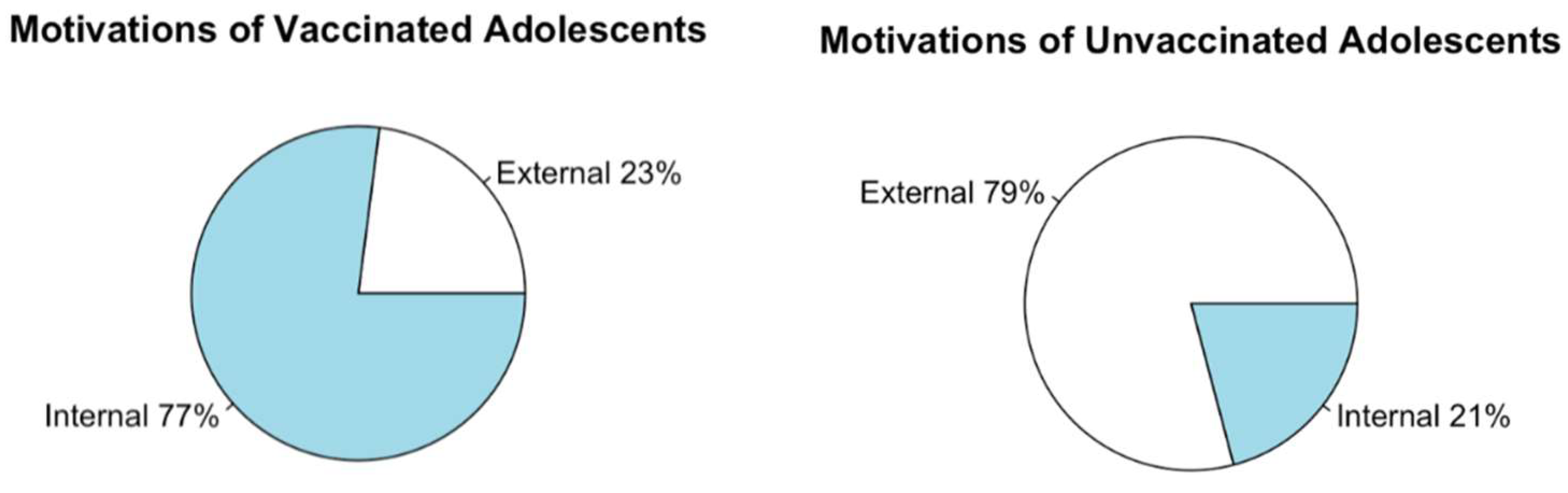
3.2. Motivations across Age Groups
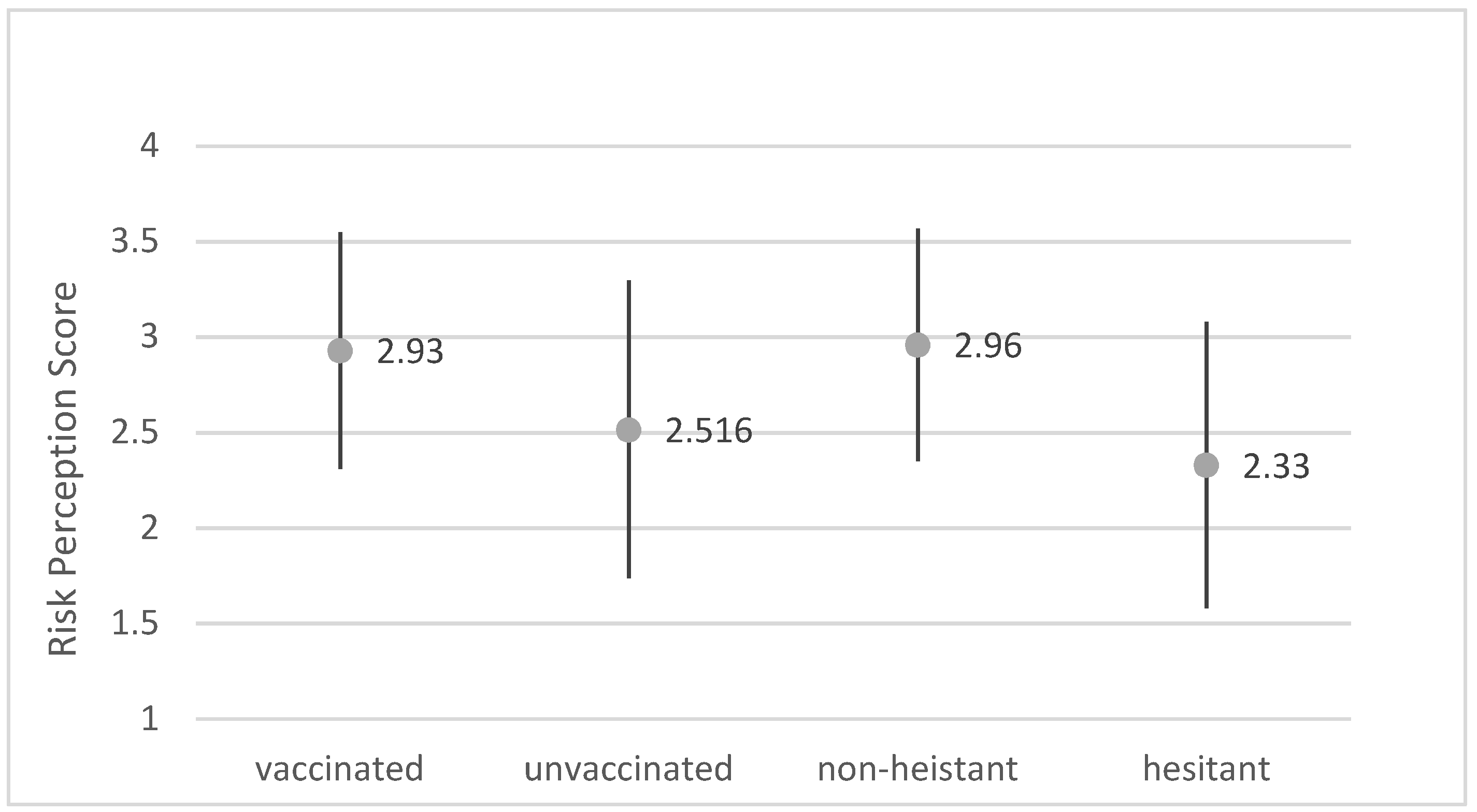
3.3. Risk Perception
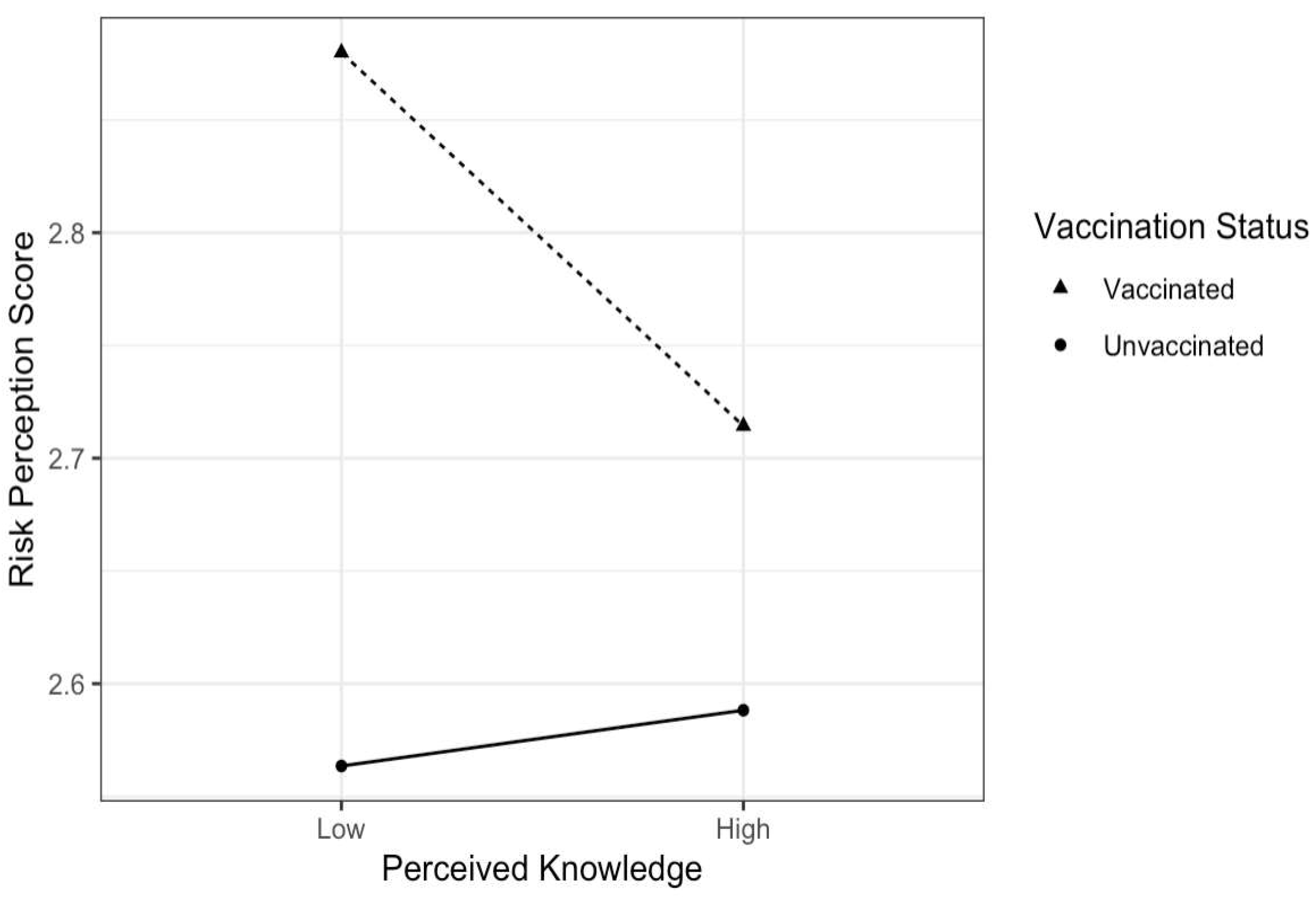
3.4. Perceived Knowledge
3.5. Risk Perception and Motivation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- CDC. COVID Data Tracker—Vaccination and Case Trends of COVID-19 in the US. Available online: https://covid.cdc.gov/covid-data-tracker/#vaccinations-cases-trends (accessed on 15 March 2022).
- Levin, D. The U.S. Is Wasting Vaccine Doses, Even as Cases Rise and Other Countries Suffer Shortages. N. Y. Times. 1 August 2021. Available online: https://www.nytimes.com/2021/08/01/us/covid-us-vaccine-wasted.html (accessed on 15 March 2022).
- MacDonald, N.E. Vaccine Hesitancy: Definition, Scope and Determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef] [PubMed]
- Razai, M.S.; Chaudhry, U.A.R.; Doerholt, K.; Bauld, L.; Majeed, A. COVID-19 Vaccination Hesitancy. BMJ 2021, 373, n1138. [Google Scholar] [CrossRef] [PubMed]
- Jarrett, C.; Wilson, R.; O’Leary, M.; Eckersberger, E.; Larson, H.J.; SAGE Working Group on Vaccine Hesitancy. Strategies for Addressing Vaccine Hesitancy—A Systematic Review. Vaccine 2015, 33, 4180–4190. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brewer, N.T.; Fazekas, K.I. Predictors of HPV Vaccine Acceptability: A Theory-Informed, Systematic Review. Prev. Med. 2007, 45, 107–114. [Google Scholar] [CrossRef]
- Rogers, R.W. A Protection Motivation Theory of Fear Appeals and Attitude Change1. J. Psychol. 1975, 91, 93–114. [Google Scholar] [CrossRef]
- Rogers, R.W.; Mewborn, C.R. Fear Appeals and Attitude Change: Effects of a Threat’s Noxiousness, Probability of Occurrence, and the Efficacy of Coping Responses. J. Pers. Soc. Psychol. 1976, 34, 54–61. [Google Scholar] [CrossRef]
- Eberhardt, J.; Ling, J. Predicting COVID-19 Vaccination Intention Using Protection Motivation Theory and Conspiracy Beliefs. Vaccine 2021, 39, 6269–6275. [Google Scholar] [CrossRef]
- Shmueli, L. Predicting Intention to Receive COVID-19 Vaccine among the General Population Using the Health Belief Model and the Theory of Planned Behavior Model. BMC Public Health 2021, 21, 804. [Google Scholar] [CrossRef]
- Biswas, N.; Mustapha, T.; Khubchandani, J.; Price, J.H. The Nature and Extent of COVID-19 Vaccination Hesitancy in Healthcare Workers. J. Community Health 2021, 46, 1244–1251. [Google Scholar] [CrossRef]
- Betsch, C.; Wicker, S. E-Health Use, Vaccination Knowledge and Perception of Own Risk: Drivers of Vaccination Uptake in Medical Students. Vaccine 2012, 30, 1143–1148. [Google Scholar] [CrossRef]
- Karlsson, L.C.; Soveri, A.; Lewandowsky, S.; Karlsson, L.; Karlsson, H.; Nolvi, S.; Karukivi, M.; Lindfelt, M.; Antfolk, J. Fearing the Disease or the Vaccine: The Case of COVID-19. Personal. Individ. Differ. 2021, 172, 110590. [Google Scholar] [CrossRef] [PubMed]
- Qiao, S.; Tam, C.C.; Li, X. Risk Exposures, Risk Perceptions, Negative Attitudes Toward General Vaccination, and COVID-19 Vaccine Acceptance Among College Students in South Carolina. Am. J. Health Promot. 2021, 36, 08901171211028407. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.-W.; Ahorsu, D.K.; Lin, C.-Y.; Chen, I.-H.; Yen, C.-F.; Kuo, Y.-J.; Griffiths, M.D.; Pakpour, A.H. Motivation to Have COVID-19 Vaccination Explained Using an Extended Protection Motivation Theory among University Students in China: The Role of Information Sources. Vaccines 2021, 9, 380. [Google Scholar] [CrossRef] [PubMed]
- Ezati Rad, R.; Mohseni, S.; Kamalzadeh Takhti, H.; Hassani Azad, M.; Shahabi, N.; Aghamolaei, T.; Norozian, F. Application of the Protection Motivation Theory for Predicting COVID-19 Preventive Behaviors in Hormozgan, Iran: A Cross-Sectional Study. BMC Public Health 2021, 21, 466. [Google Scholar] [CrossRef] [PubMed]
- Huang, P.-C.; Hung, C.-H.; Kuo, Y.-J.; Chen, Y.-P.; Ahorsu, D.K.; Yen, C.-F.; Lin, C.-Y.; Griffiths, M.D.; Pakpour, A.H. Expanding Protection Motivation Theory to Explain Willingness of COVID-19 Vaccination Uptake among Taiwanese University Students. Vaccines 2021, 9, 1046. [Google Scholar] [CrossRef]
- Rosenstock, I.M. The Health Belief Model and Preventive Health Behavior. Health Educ. Monogr. 1974, 2, 354–386. [Google Scholar] [CrossRef]
- Peplak, J.; Klemfuss, J.Z.; Yates, T.M. Parent-Adolescent Conversations About COVID-19 Influence Adolescents’ Empathic Concern and Adherence to Health Protective Behaviors. J. Adolesc. Health 2021, 69, 925–932. [Google Scholar] [CrossRef]
- Wong, L.P.; Alias, H.; Wong, P.-F.; Lee, H.Y.; AbuBakar, S. The Use of the Health Belief Model to Assess Predictors of Intent to Receive the COVID-19 Vaccine and Willingness to Pay. Hum. Vaccines Immunother. 2020, 16, 2204–2214. [Google Scholar] [CrossRef]
- Smail, E.; Schneider, K.E.; DeLong, S.M.; Willis, K.; Arrington-Sanders, R.; Yang, C.; Alexander, K.A.; Johnson, R.M. Health Beliefs and Preventive Behaviors Among Adults During the Early COVID-19 Pandemic in the United States: A Latent Class Analysis. Prev. Sci. 2021, 22, 1013–1022. [Google Scholar] [CrossRef]
- Denman, D.C.; Baldwin, A.S.; Marks, E.G.; Lee, S.C.; Tiro, J.A. Modification and Validation of the Treatment Self Regulation Questionnaire to Assess Parental Motivation for HPV Vaccination of Adolescents. Vaccine 2016, 34, 4985–4990. [Google Scholar] [CrossRef] [Green Version]
- Donadiki, E.M.; Jiménez-García, R.; Hernández-Barrera, V.; Sourtzi, P.; Carrasco-Garrido, P.; López de Andrés, A.; Jimenez-Trujillo, I.; Velonakis, E.G. Health Belief Model Applied to Non-Compliance with HPV Vaccine among Female University Students. Public Health 2014, 128, 268–273. [Google Scholar] [CrossRef] [PubMed]
- Prematunge, C.; Corace, K.; McCarthy, A.; Nair, R.C.; Pugsley, R.; Garber, G. Factors Influencing Pandemic Influenza Vaccination of Healthcare Workers—A Systematic Review. Vaccine 2012, 30, 4733–4743. [Google Scholar] [CrossRef] [PubMed]
- Corace, K.; Prematunge, C.; McCarthy, A.; Nair, R.C.; Roth, V.; Hayes, T.; Suh, K.N.; Balfour, L.; Garber, G. Predicting Influenza Vaccination Uptake among Health Care Workers: What Are the Key Motivators? Am. J. Infect. Control 2013, 41, 679–684. [Google Scholar] [CrossRef] [PubMed]
- Larsman, P.; Eklöf, M.; Törner, M. Adolescents’ Risk Perceptions in Relation to Risk Behavior with Long-Term Health Consequences; Antecedents and Outcomes: A Literature Review. Saf. Sci. 2012, 50, 1740–1748. [Google Scholar] [CrossRef]
- Ramsey, M.A.; Marczinski, C.A. College Students’ Perceptions of H1N1 Flu Risk and Attitudes toward Vaccination. Vaccine 2011, 29, 7599–7601. [Google Scholar] [CrossRef] [Green Version]
- Ramos, V. The Delta Variant Is Detected in 99 Percent of US Cases, CDC Says. N. Y. Times. Available online: https://www.nytimes.com/2021/09/18/health/delta-covid-us-cases-cdc.html (accessed on 18 September 2021).
- Moon, K.; Riege, A.; Gourdon-Kanhukamwe, A.; Vallée-Tourangeau, G. Development and Validation of the Treatmentself-Regulation Questionnaire Assessing Healthcare Professionals’ Motivation for Flu Vaccination (TSRQ-Flu). Psychol. Health 2021, 37, 259–278. [Google Scholar] [CrossRef]
- Park, S.; Oh, S. Factors Associated with Preventive Behaviors for COVID-19 among Adolescents in South Korea. J. Pediatr. Nurs. 2022, 62, e69–e76. [Google Scholar] [CrossRef]
- Fathian-Dastgerdi, Z.; Khoshgoftar, M.; Tavakoli, B.; Jaleh, M. Factors Associated with Preventive Behaviors of COVID-19 among Adolescents: Applying the Health Belief Model. Res. Soc. Adm. Pharm. 2021, 17, 1786–1790. [Google Scholar] [CrossRef]
- Burrai, J.; Barchielli, B.; Cricenti, C.; Borrelli, A.; D’Amato, S.; Santoro, M.; Vitale, M.; Ferracuti, S.; Giannini, A.M.; Quaglieri, A. Older Adolescents Who Did or Did Not Experience COVID-19 Symptoms: Associations with Mental Health, Risk Perception and Social Connection. Int. J. Environ. Res. Public. Health 2021, 18, 5006. [Google Scholar] [CrossRef]
- Fazel, M.; Puntis, S.; White, S.R.; Townsend, A.; Mansfield, K.L.; Viner, R.; Herring, J.; Pollard, A.J.; Freeman, D. Willingness of Children and Adolescents to Have a COVID-19 Vaccination: Results of a Large Whole Schools Survey in England. EClinicalMedicine 2021, 40, 101144. [Google Scholar] [CrossRef]
- United States Census Bureau U.S. Census—Populations and People. Available online: https://data.census.gov/cedsci/profile?q=United%20States&g=0100000US (accessed on 26 October 2021).
- Qualtrics ANOVA Test: Definition & Uses. Available online: https://www.qualtrics.com/experience-management/research/anova/ (accessed on 29 October 2021).
- Gerald, B. A Brief Review of Independent, Dependent and One Sample t-Test. Int. J. Appl. Math. Theor. Phys. 2018, 4, 50. [Google Scholar] [CrossRef] [Green Version]
- Yu, C.; Yao, W. Robust Linear Regression: A Review and Comparison. Commun. Stat.-Simul. Comput. 2017, 46, 6261–6282. [Google Scholar] [CrossRef]
- Kim, T.K. Understanding One-Way ANOVA Using Conceptual Figures. Korean J. Anesthesiol. 2017, 70, 22–26. [Google Scholar] [CrossRef] [Green Version]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020. [Google Scholar]
- Nunnally, J.C.; Bernstein, I.H. Psychometric Theory; McGraw-Hill: New York, NY, USA, 1994; ISBN 978-0-07-047849-7. [Google Scholar]
- DeVellis, R.F. Scale Development: Theory and Applications, 2nd ed.; SAGE: Thousand Oaks, CA, USA, 2003; ISBN 978-0-7619-2605-4. [Google Scholar]
- Moore, R.; Purvis, R.S.; Hallgren, E.; Willis, D.E.; Hall, S.; Reece, S.; CarlLee, S.; Judkins, H.; McElfish, P.A. Motivations to Vaccinate Among Hesitant Adopters of the COVID-19 Vaccine. J. Community Health 2022, 47, 237–245. [Google Scholar] [CrossRef]
- Isler, O.; Isler, B.; Kopsacheilis, O.; Ferguson, E. Limits of the Social-Benefit Motive among High-Risk Patients: A Field Experiment on Influenza Vaccination Behaviour. BMC Public Health 2020, 20, 240. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Towey, R. CNBC Poll Shows Very Little Will Persuade Unvaccinated Americans to Get COVID Shots. Available online: https://www.cnbc.com/2021/09/10/cnbc-poll-shows-very-little-will-persuade-unvaccinated-americans-to-get-covid-shots.html (accessed on 22 November 2021).
- Reyna, V.F.; Broniatowski, D.A.; Edelson, S.M. Viruses, Vaccines, and COVID-19: Explaining and Improving Risky Decision-Making. J. Appl. Res. Mem. Cogn. 2021, 10, 491–509. [Google Scholar] [CrossRef]
- Iorfa, S.K.; Ottu, I.F.A.; Oguntayo, R.; Ayandele, O.; Kolawole, S.O.; Gandi, J.C.; Dangiwa, A.L.; Olapegba, P.O. COVID-19 Knowledge, Risk Perception, and Precautionary Behavior Among Nigerians: A Moderated Mediation Approach. Front. Psychol. 2020, 11, 566773. [Google Scholar] [CrossRef]
- Ning, L.; Niu, J.; Bi, X.; Yang, C.; Liu, Z.; Wu, Q.; Ning, N.; Liang, L.; Liu, A.; Hao, Y.; et al. The Impacts of Knowledge, Risk Perception, Emotion and Information on Citizens’ Protective Behaviors during the Outbreak of COVID-19: A Cross-Sectional Study in China. BMC Public Health 2020, 20, 1751. [Google Scholar] [CrossRef]
- Ursachi, G.; Horodnic, I.A.; Zait, A. How Reliable Are Measurement Scales? External Factors with Indirect Influence on Reliability Estimators. Procedia Econ. Financ. 2015, 20, 679–686. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Ten Threats to Global Health in 2019. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 25 September 2021).
- World Health Organization. Young People and COVID-19: Behavioural Considerations for Promoting Safe Behaviours: Policy Brief; World Health Organization: Geneva, Switzerland, 2021; ISBN 978-92-4-002831-9. [Google Scholar]
- Andrews, J.L.; Foulkes, L.; Blakemore, S.-J. Peer Influence in Adolescence: Public-Health Implications for COVID-19. Trends Cogn. Sci. 2020, 24, 585–587. [Google Scholar] [CrossRef]
- Young, S.D.; Goldstein, N.J. Applying Social Norms Interventions to Increase Adherence to COVID-19 Prevention and Control Guidelines. Prev. Med. 2021, 145, 106424. [Google Scholar] [CrossRef] [PubMed]
| Variables | n (%) * |
|---|---|
| Age (years) | |
| 13–15 | 177 (40.32%) |
| 16–17 | 262 (59.68%) |
| Self-identified Gender | |
| Female | 232 (52.85%) |
| Male | 182 (41.46%) |
| Other/prefer not to answer | 25 (5.60%) |
| Self-reported Race | |
| White | 257 (58.54%) |
| Black/African American | 63 (14.35%) |
| Hispanic/Latino | 46 (10.47%) |
| Asian | 37 (8.42%) |
| Native American | 7 (1.59%) |
| Other | 29 (6.63%) |
| Vaccination Status | |
| Unvaccinated, not planning to get vaccinated | 93 (21.18%) |
| Unvaccinated, unsure (still undecided) whether to get vaccinated | 66 (15.03%) |
| Unvaccinated, planning to get vaccinated | 50 (11.39%) |
| Vaccinated, received one vaccine dose | 14 (3.19%) |
| Vaccinated, received both vaccine doses | 216 (49.20%) |
| Vaccine Hesitancy | |
| Non-hesitant | 275 (62.64%) |
| Hesitant | 164 (37.35%) |
| B | S.E. | Wald | df | Significance p-Value | |
|---|---|---|---|---|---|
| Risk Perception b | −0.982 | 0.128 | 58.641 | 1 | <0.001 |
| Motivation c | 0.366 | 0.087 | 17.729 | 1 | <0.001 |
| Constant | 2.559 | 0.424 | 36.343 | 1 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tu, P.; Kotarba, M.; Bier, B.; Clark, R.; Lin, C. Internal and External Motivations and Risk Perception toward COVID-19 Vaccination in Adolescents in the U.S. Vaccines 2022, 10, 697. https://doi.org/10.3390/vaccines10050697
Tu P, Kotarba M, Bier B, Clark R, Lin C. Internal and External Motivations and Risk Perception toward COVID-19 Vaccination in Adolescents in the U.S. Vaccines. 2022; 10(5):697. https://doi.org/10.3390/vaccines10050697
Chicago/Turabian StyleTu, Pikuei, Michaela Kotarba, Brooke Bier, Rachel Clark, and Cheryl Lin. 2022. "Internal and External Motivations and Risk Perception toward COVID-19 Vaccination in Adolescents in the U.S." Vaccines 10, no. 5: 697. https://doi.org/10.3390/vaccines10050697
APA StyleTu, P., Kotarba, M., Bier, B., Clark, R., & Lin, C. (2022). Internal and External Motivations and Risk Perception toward COVID-19 Vaccination in Adolescents in the U.S. Vaccines, 10(5), 697. https://doi.org/10.3390/vaccines10050697





