Vaccine Literacy and Source of Information about Vaccination among Staff of Nursing Homes: A Cross-Sectional Survey Conducted in Tuscany (Italy)
Abstract
:1. Introduction
2. Materials and Methods
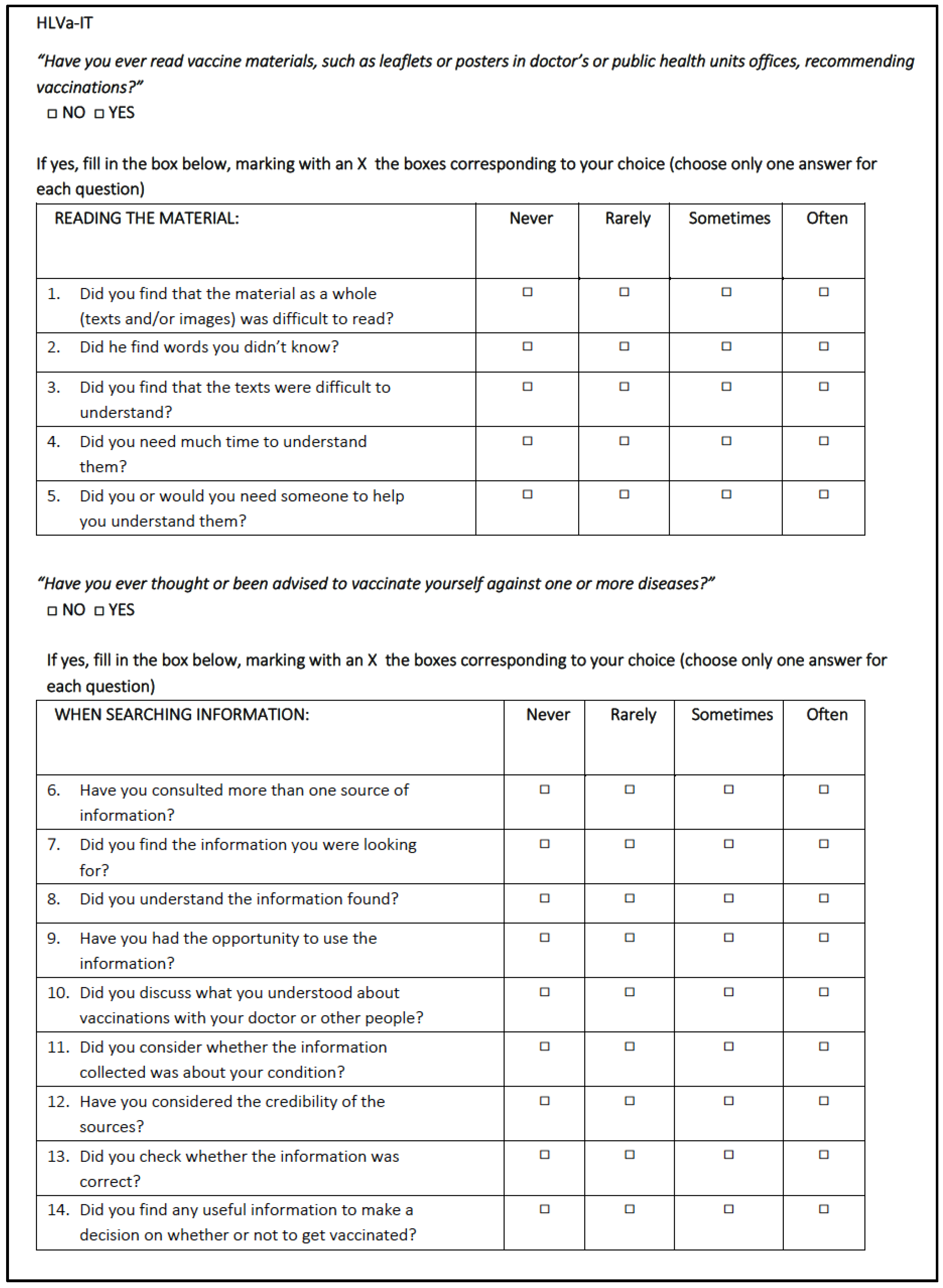
2.1. HLVa-IT
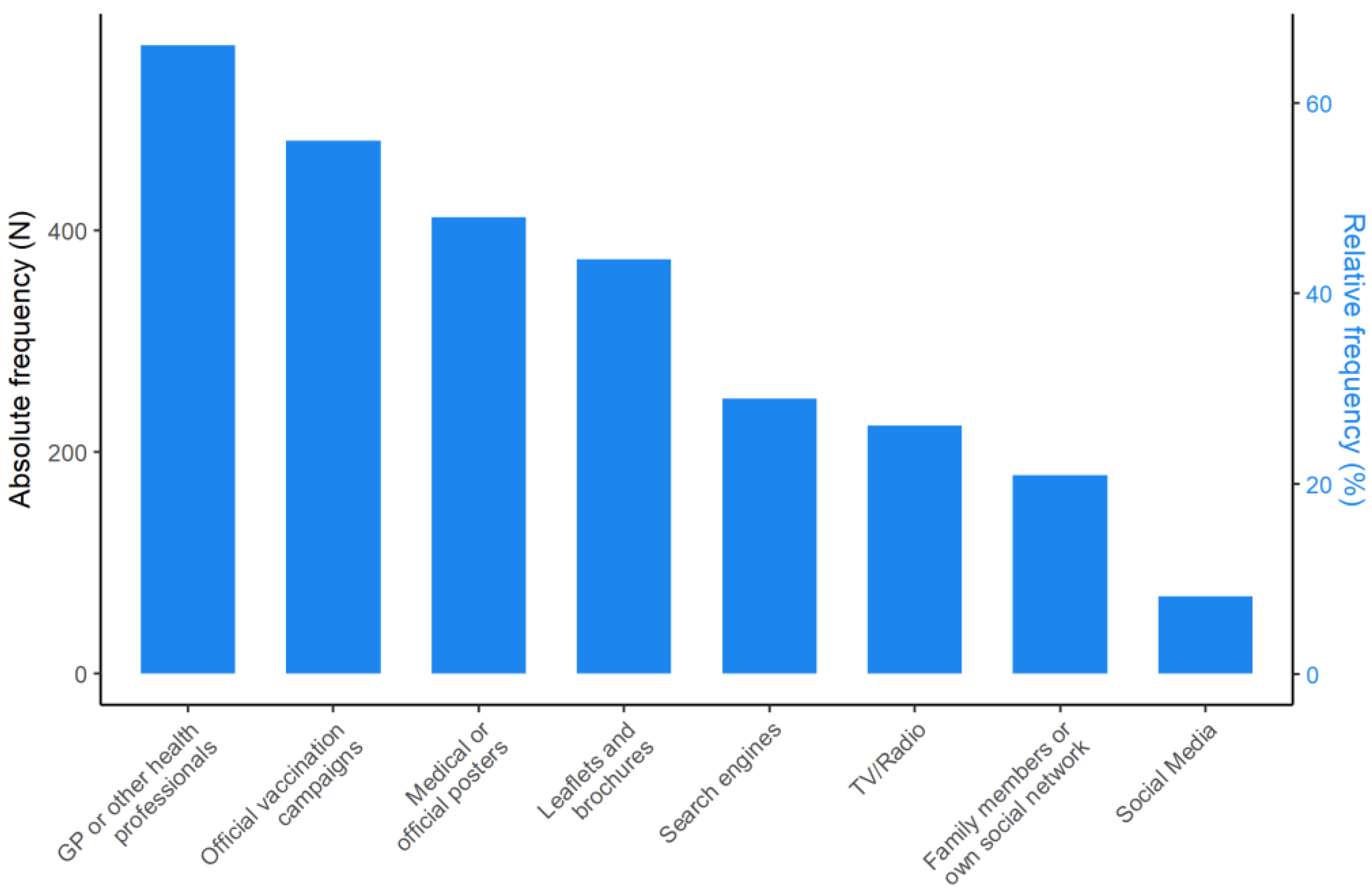
2.2. Sources of Information
2.3. Statistical Analysis
3. Results
3.1. Sample Description
3.2. HLVa-IT: Principal Component Analysis and Internal Consistency
3.3. HLVa-IT: Item Responses and Score Description
3.4. HLVa-IT and Main Sources of Information
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Vaccine and Vaccination. Available online: https://www.who.int/health-topics/vaccines-and-immunization#tab=tab_1 (accessed on 3 March 2022).
- MacDonald, N.E.; SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef] [PubMed]
- Larson, H.J.; Broniatowski, D.A. Volatility of vaccine confidence. Science 2021, 371, 1289. [Google Scholar] [CrossRef] [PubMed]
- Carrieri, V.; Madio, L.; Principe, F. Vaccine hesitancy and (fake) news: Quasi-experimental evidence from Italy. Health Econ. 2019, 28, 1377–1382. [Google Scholar] [CrossRef] [PubMed]
- Bianco, A.; Della Polla, G.; Angelillo, S.; Pelullo, C.P.; Licata, F.; Angelillo, I.F. Parental COVID-19 vaccine hesitancy: A cross-sectional survey in Italy. Expert Rev. Vaccines 2022, 21, 541–547. [Google Scholar] [CrossRef]
- Kieslich, K. Addressing vaccination hesitancy in Europe: A case study in state-society relations. Eur. J. Public Health 2018, 28 (Suppl. S3), 30–33. [Google Scholar] [CrossRef]
- Chirico, F. The new Italian mandatory vaccine Law as a health policy instrument against the anti-vaccination movement. Ann. Ig. 2018, 30, 251–256. [Google Scholar] [PubMed]
- Vergallo, G.M.; Del Rio, A.; Negro, F.; Zaami, S. COVID-19 vaccine mandates: What are the current European public perspectives? Eur. Rev. Med. Pharmacol. Sci. 2022, 26, 643–652. [Google Scholar]
- Ratzan, S.C.; Parker, R.M. Vaccine Literacy-helping Everyone Decide to Accept Vaccination. J. Health Commun. 2020, 25, 750–752. [Google Scholar] [CrossRef] [PubMed]
- Biasio, L.R. Vaccine literacy is undervalued. Hum. Vaccines Immunother. 2019, 15, 2552–2553. [Google Scholar] [CrossRef]
- Allington, D.; McAndrew, S.; Moxham-Hall, V.L.; Duffy, B. Media usage predicts intention to be vaccinated against SARS-CoV-2 in the US and the UK. Vaccine 2021, 39, 2595–2603. [Google Scholar] [CrossRef]
- Callaghan, T.; Motta, M.; Sylvester, S.; Lunz Trujillo, K.; Blackburn, C.C. Parent Psychology and the Decision to Delay Childhood Vaccination. Soc. Sci. Med. 2019, 238, 112407. [Google Scholar] [CrossRef] [PubMed]
- Kata, A. Anti-Vaccine Activists Web 2.0, and the Postmodern Paradigm: An Overview of Tactics and Tropes Used Online by the Anti-Vaccination Movement. Vaccine 2012, 30, 3778–3789. [Google Scholar] [CrossRef] [PubMed]
- Puri, N.; Coomes, E.A.; Haghbayan, H.; Gunaratne, K. Social media and vaccine hesitancy: New updates for the era of COVID-19 and globalized infectious diseases. Hum. Vaccines Immunother. 2020, 16, 2586–2593. [Google Scholar] [CrossRef] [PubMed]
- Basch, C.H.; Zybert, P.; Reeves, R.; Basch, C. What do popular YouTube videos say about vaccines? Child Care Health Dev. 2017, 43, 499–503. [Google Scholar] [CrossRef] [PubMed]
- Guidry, J.P.; Carlyle, K.; Messner, M.; Jin, Y. On pins and needles: How vaccines are portrayed on Pinterest. Vaccine 2015, 33, 5051–5056. [Google Scholar] [CrossRef]
- Lorini, C.; Santomauro, F.; Donzellini, M.; Capecchi, L.; Bechini, A.; Boccalini, S.; Bonanni, P.; Bonaccorsi, G. Health literacy and vaccination: A systematic review. Hum. Vaccines Immunother. 2018, 14, 478–488. [Google Scholar] [CrossRef] [Green Version]
- Biasio, L.R.; Giambi, C.; Fadda, G.; Lorini, C.; Bonaccorsi, G.; D’Ancona, F. Validation of an Italian tool to assess vaccine literacy in adulthood vaccination: A pilot study. Ann. Ig. 2020, 32, 205–222. [Google Scholar] [CrossRef]
- Biasio, L.R.; Bonaccorsi, G.; Lorini, C.; Pecorelli, S. Assessing COVID-19 vaccine literacy: A preliminary online survey. Hum. Vaccines Immunother. 2021, 17, 1304–1312. [Google Scholar] [CrossRef] [PubMed]
- Biasio, L.R.; Bonaccorsi, G.; Lorini, C.; Mazzini, D.; Pecorelli, S. Italian Adults’ Likelihood of Getting COVID-19 Vaccine: A Second Online Survey. Vaccines 2021, 9, 268. [Google Scholar] [CrossRef]
- Costantini, H. COVID-19 Vaccine Literacy of Family Carers for Their Older Parents in Japan. Healthcare 2021, 9, 1038. [Google Scholar] [CrossRef]
- Turhan, Z.; Dilcen, H.Y.; Dolu, İ. The mediating role of health literacy on the relationship between health care system distrust and vaccine hesitancy during COVID-19 pandemic. Curr. Psychol. 2021, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Gusar, I.; Konjevoda, S.; Babić, G.; Hnatešen, D.; Čebohin, M.; Orlandini, R.; Dželalija, B. Pre-Vaccination COVID-19 Vaccine Literacy in a Croatian Adult Population: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 7073. [Google Scholar] [CrossRef] [PubMed]
- Nace, D.A.; Archbald-Pannone, L.R.; Ashraf, M.S.; Drinka, P.J.; Frentzel, E.; Gaur, S.; Mahajan, D.; Mehr, D.R.; Mercer, W.C.; Sloane, P.D.; et al. Pneumococcal Vaccination Guidance for Nursing Home Residents: Recommendations from AMDA’s Infection Advisory Committee. J. Am. Med. Dir. Assoc. 2017, 18, 99–104. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Guiding Principles for Immunization Activities during the COVID-19 Pandemic; WHO: Geneva, Switzerland, 2020. Available online: https://apps.who.int/iris/bitstream/handle/10665/331590/WHO-2019-nCoV-immunization_services-2020.1-eng.pdf (accessed on 3 March 2022).
- Boey, L.; Bosmans, E.; Ferreira, L.B.; Heyvaert, N.; Nelen, M.; Smans, L.; Tuerlinckx, H.; Roelants, M.; Claes, K.; Derdelinckx, I.; et al. Vaccination coverage of recommended vaccines and determinants of vaccination in at-risk groups. Hum. Vaccines Immunother. 2020, 16, 2136–2143. [Google Scholar] [CrossRef] [PubMed]
- Berry, S.D.; Johnson, K.S.; Myles, L.; Herndon, L.; Montoya, A.; Fashaw, S.; Gifford, D. Lessons learned from frontline skilled nursing facility staff regarding COVID-19 vaccine hesitancy. J. Am. Geriatr. Soc. 2021, 69, 1140–1146. [Google Scholar] [CrossRef] [PubMed]
- Unroe, K.T.; Evans, R.; Weaver, L.; Rusyniak, D.; Blackburn, J. Willingness of Long-Term Care Staff to Receive a COVID-19 Vaccine: A Single State Survey. J. Am. Geriatr. Soc. 2021, 69, 593–599. [Google Scholar] [CrossRef]
- Elias, C.; Fournier, A.; Vasiliu, A.; Beix, N.; Demillac, R.; Tillaut, H.; Guillois, Y.; Eyebe, S.; Mollo, B.; Crépey, P. Seasonal influenza vaccination coverage and its determinants among nursing homes personnel in western France. BMC Public Health 2017, 17, 634. [Google Scholar] [CrossRef] [Green Version]
- Lorini, C.; Collini, F.; Gasparini, F.; Paolini, D.; Grazzini, M.; Ierardi, F.; Galletti, G.; Zanobini, P.; Gemmi, F.; Bonaccorsi, G. Health Literacy, Vaccine Confidence and Influenza Vaccination Uptake among Nursing Home Staff: A Cross-Sectional Study Conducted in Tuscany. Vaccines 2020, 8, 154. [Google Scholar] [CrossRef] [Green Version]
- Lorini, C.; Ierardi, F.; Gatteschi, C.; Galletti, G.; Collini, F.; Peracca, L.; Zanobini, P.; Gemmi, F.; Bonaccorsi, G. Promoting Influenza Vaccination among Staff of Nursing Homes According to Behavioral Insights: Analyzing the Choice Architecture during a Nudge-Based Intervention. Vaccines 2020, 8, 600. [Google Scholar] [CrossRef]
- Ishikawa, H.; Takeuchi, T.; Yano, E. Measuring functional, communicative, and critical health literacy among diabetic patients. Diabetes Care 2008, 31, 874–879. [Google Scholar] [CrossRef] [Green Version]
- Nutbeam, D. Health literacy as a public health goal: A challenge for contemporary health education and communication strategies into the 21st century. Health Promot. Int. 2000, 15, 259–267. [Google Scholar] [CrossRef] [Green Version]
- Cadeddu, C.; Regazzi, L.; Bonaccorsi, G.; Rosano, A.; Unim, B.; Griebler, R.; Link, T.; De Castro, P.; D’Elia, R.; Mastrilli, V.; et al. The Determinants of Vaccine Literacy in the Italian Population: Results from the Health Literacy Survey 2019. Int. J. Environ. Res. Public 2022, 19, 4429. [Google Scholar] [CrossRef] [PubMed]
- Correa-Rodríguez, M.; Rueda-Medina, B.; Callejas-Rubio, J.L.; Ríos-Fernández, R.; de la Hera-Fernández, J.; Ortego-Centeno, N. COVID-19 vaccine literacy in patients with systemic autoimmune diseases. Curr. Psychol. 2022, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Aharon, A.A.; Nehama, H.; Rishpon, S.; Baron-Epel, O. Parents with high levels of communicative and critical health literacy are less likely to vaccinate their children. Patient Educ. Couns. 2017, 100, 768–775. [Google Scholar] [CrossRef]
- Catalan-Matamoros, D.; Peñafiel-Saiz, C. How is communication of vaccines in traditional media: A systematic review. Perspect. Public Health 2019, 139, 34–43. [Google Scholar] [CrossRef]
- Rubinelli, S.; Ort, A.; Zanini, C.; Fiordelli, M.; Diviani, N. Strengthening Critical Health Literacy for Health Information Appraisal: An Approach from Argumentation Theory. Int. J. Environ. Res. Public Health 2021, 18, 6764. [Google Scholar] [CrossRef]
- Rowlands, G.; Nutbeam, D. Health literacy and the ‘inverse information law’. Br. J. Gen. Pract. 2013, 63, 120–121. [Google Scholar] [CrossRef] [Green Version]
- Zhang, F.; Or, P.P.; Chung, J.W. The effects of health literacy in influence vaccination competences between Community-Dwelling Elder Adults in Hong Kong. BMC Geriatr. 2020, 20, 103. [Google Scholar] [CrossRef]

| Variables | n | % | |
|---|---|---|---|
| Sex | Female | 744 | 87.0 |
| Male | 106 | 12.0 | |
| NA * | 8 | 1.0 | |
| Language | Italian | 727 | 84.7 |
| Others | 108 | 12.6 | |
| NA * | 23 | 2.7 | |
| Educational level | Less than high school diploma | 220 | 25.6 |
| High school degree | 400 | 46.6 | |
| Bachelor’s degree and higher | 230 | 26.8 | |
| NA * | 8 | 1.0 | |
| Profession | Nurses | 139 | 16.2 |
| Assistants/aides | 503 | 58.6 | |
| Physiotherapists | 41 | 4.9 | |
| Health educators | 34 | 4.0 | |
| Other clinical staff | 52 | 6.1 | |
| Cleaning staff | 34 | 4.0 | |
| Other nonclinical staff | 43 | 5.0 | |
| NA * | 12 | 1.4 | |
| Component | Eigenvalue | Percentage of Explained Variance | Cumulative Variance Percent |
|---|---|---|---|
| Item 1 | 4.88 | 34.87 | 34.87 |
| Item 2 | 3.06 | 21.88 | 56.75 |
| Item 3 | 1.12 | 8.03 | 64.78 |
| Item 4 | 0.80 | 5.72 | 70.50 |
| Item 5 | 0.66 | 4.73 | 75.24 |
| Item 6 | 0.63 | 4.51 | 79.75 |
| Item 7 | 0.52 | 3.75 | 83.49 |
| Item 8 | 0.45 | 3.24 | 86.73 |
| Item 9 | 0.40 | 2.86 | 89.59 |
| Item 10 | 0.36 | 2.61 | 92.20 |
| Item 11 | 0.34 | 2.46 | 94.66 |
| Item 12 | 0.30 | 2.11 | 96.77 |
| Item 13 | 0.26 | 1.87 | 98.64 |
| Item 14 | 0.19 | 1.36 | 100.00 |
| Scale and Subscales | Standardized Cronbach’s Alpha | Omega Total Coefficient |
|---|---|---|
| HLVa-IT | 0.85 | 0.91 |
| HLVa-IT Functional Component | 0.89 | 0.92 |
| HLVa-IT Interactive/Communicative and Critical Component | 0.87 | 0.90 |
| Subscale | Items | Response Options n (%) | Mean ± SD | Median (IQR) | ||||
|---|---|---|---|---|---|---|---|---|
| 1—often | 2—sometimes | 3—rarely | 4—never | Missing | ||||
| Functional subscale “Have you ever read vaccine materials, such as leaflets or posters in doctors’ or public health units’ offices, recommending vaccinations?” If yes… | 1. Did you find that the material as a whole (texts and/or images) was difficult to read? | 39 (4.55) | 208 (24.24) | 271 (31.59) | 281 (32.75) | 59 (6.87) | 2.99 ± 0.90 | 3 (2–4) |
| 2. Did you find words you didn’t know? | 27 (3.15) | 206 (24.01) | 288 (33.57) | 269 (31.35) | 68 (7.92) | 3.01 ± 0.86 | 3 (2–4) | |
| 3. Did you find that the texts were difficult to understand? | 18 (2.10) | 142 (16.55) | 295 (34.38) | 330 (38.46) | 73 (8.51) | 3.19 ± 0.81 | 3 (3–4) | |
| 4. Did you need a lot of time to understand these materials? | 15 (1.75) | 104 (12.12) | 270 (31.47) | 396 (46.15) | 73 (8.51) | 3.33 ± 0.78 | 4 (3–4) | |
| 5. Did you need or would you have needed someone to help you understand them? | 21 (2.45) | 125 (14.57) | 244 (28.44) | 399 (46.50) | 69 (8.04) | 3.29 ± 0.83 | 4 (3–4) | |
| Subscale | Items | 1—never | 2—rarely | 3—sometimes | 4—often | Missing | Mean ± SD | Median (IQR) |
| Interactive/communicative and critical subscale “Have you ever thought or been advised to vaccinate yourself against one or more diseases?” | 6. Have you consulted more than one source of information? | 60 (6.99) | 165 (19.23) | 310 (36.13) | 262 (30.54) | 61 (7.11) | 2.97 ± 0.91 | 3 (2–4) |
| 7. Did you find the information you were looking for? | 20 (2.33) | 112 (13.05) | 334 (38.93) | 327 (38.11) | 65 (7.58) | 3.22 ± 0.78 | 3 (3–4) | |
| 8. Did you understand the information found? | 18 (2.10) | 61 (7.11) | 240 (27.97) | 464 (54.08) | 75 (8.74) | 3.47 ± 0.74 | 4 (3–4) | |
| 9. Have you had the opportunity to use the information? | 39 (4.55) | 85 (9.91) | 340 (39.63) | 324 (37.76) | 70 (8.15) | 3.20 ± 0.82 | 3 (3–4) | |
| 10. Did you discuss what you understood about vaccinations with your doctor or other people? | 78 (9.09) | 130 (15.15) | 319 (37.18) | 267 (31.12) | 64 (7.46) | 2.98 ± 0.95 | 3 (2–4) | |
| 11. Did you consider whether the information collected was about your condition? | 55 (6.41) | 122 (14.22) | 297 (34.62) | 314 (36.60) | 70 (8.15) | 3.10 ± 0.91 | 3 (3–4) | |
| 12. Have you considered the credibility of the sources? | 30 (3.49) | 82 (9.56) | 268 (31.24) | 407 (47.44) | 71 (8.27) | 3.34 ± 0.81 | 4 (3–4) | |
| 13. Did you check whether the information was correct? | 46 (5.36) | 85 (9.91) | 255 (29.72) | 396 (46.15) | 76 (8.86) | 3.28 ± 0.87 | 4 (3–4) | |
| 14. Did you find any useful information to make a decision on whether or not to get vaccinated? | 47 (5.48) | 116 (13.52) | 270 (31.47) | 351 (40.91) | 74 (8.62) | 3.18 ± 0.90 | 3 (3–4) | |
| Outcome Variable—Source of Information | Model 1. Covariate: HLVa-IT Total Score * | Model 2. Covariate: HLVa-IT-F Subscale Score * | Model 3. Covariate: HLVa-IT-ICC Subscale Score * | |||
|---|---|---|---|---|---|---|
| OR [95%CI] | p | OR [95%CI] | p | OR [95%CI] | p | |
| Leaflets and brochures | 1.25 [0.90; 1.76] | 0.190 | 1.09 [0.88; 1.37] | 0.430 | 1.15 [0.88; 1.50] | 0.310 |
| Medical or official posters | 0.81 [0.58; 1.13] | 0.220 | 0.76 [0.61; 0.95] | 0.020 | 0.91 [0.70; 1.18] | 0.470 |
| TV/Radio | 0.70 [0.49–1.02] | 0.060 | 0.75 [0.59; 0.96] | 0.020 | 0.86 [0.65; 1.58] | 0.310 |
| Official vaccination campaigns | 1.47 [1.05; 2.06] | 0.030 | 0.98 [0.78; 1.22] | 0.830 | 1.49 [1.14; 1.95] | 0.003 |
| GP or other health professionals | 2.37 [1.66; 3.43] | <0.001 | 0.82 [0.65; 1.03] | 0.090 | 2.68 [2.01; 3.61] | <0.001 |
| Family members or social networks | 0.85 [0.57; 1.25] | 0.400 | 0.79 [0.61; 1.03] | 0.080 | 1.13 [0.83; 1.55] | 0.450 |
| Social Media | 0.48 [0.27; 0.88] | 0.020 | 1.25 [0.84; 1.90] | 0.280 | 0.46 [0.30; 0.70] | <0.001 |
| Search engines | 1.65 [1.15; 2.40] | 0.010 | 0.95 [0.75; 1.21] | 0.690 | 1.63 [1.21; 2.22] | 0.002 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lorini, C.; Collini, F.; Galletti, G.; Ierardi, F.; Forni, S.; Gatteschi, C.; Gemmi, F.; Stacchini, L.; Papini, S.; Velpini, B.; et al. Vaccine Literacy and Source of Information about Vaccination among Staff of Nursing Homes: A Cross-Sectional Survey Conducted in Tuscany (Italy). Vaccines 2022, 10, 682. https://doi.org/10.3390/vaccines10050682
Lorini C, Collini F, Galletti G, Ierardi F, Forni S, Gatteschi C, Gemmi F, Stacchini L, Papini S, Velpini B, et al. Vaccine Literacy and Source of Information about Vaccination among Staff of Nursing Homes: A Cross-Sectional Survey Conducted in Tuscany (Italy). Vaccines. 2022; 10(5):682. https://doi.org/10.3390/vaccines10050682
Chicago/Turabian StyleLorini, Chiara, Francesca Collini, Giacomo Galletti, Francesca Ierardi, Silvia Forni, Claudia Gatteschi, Fabrizio Gemmi, Lorenzo Stacchini, Sophia Papini, Beatrice Velpini, and et al. 2022. "Vaccine Literacy and Source of Information about Vaccination among Staff of Nursing Homes: A Cross-Sectional Survey Conducted in Tuscany (Italy)" Vaccines 10, no. 5: 682. https://doi.org/10.3390/vaccines10050682
APA StyleLorini, C., Collini, F., Galletti, G., Ierardi, F., Forni, S., Gatteschi, C., Gemmi, F., Stacchini, L., Papini, S., Velpini, B., Biasio, L. R., & Bonaccorsi, G. (2022). Vaccine Literacy and Source of Information about Vaccination among Staff of Nursing Homes: A Cross-Sectional Survey Conducted in Tuscany (Italy). Vaccines, 10(5), 682. https://doi.org/10.3390/vaccines10050682









