Knowledge and Attitudes of Medical Students toward COVID-19 Vaccine in Saudi Arabia
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design, Population, and Sample
2.2. Questionnaire
2.3. Data Collection
2.4. Ethical Consideration
2.5. Statistical Analysis
3. Results
3.1. Sociodemographic Characteristics of Participants
3.2. Knowledge Related to the COVID-19 Vaccine
3.3. Attitude Related to the COVID-19 Vaccine
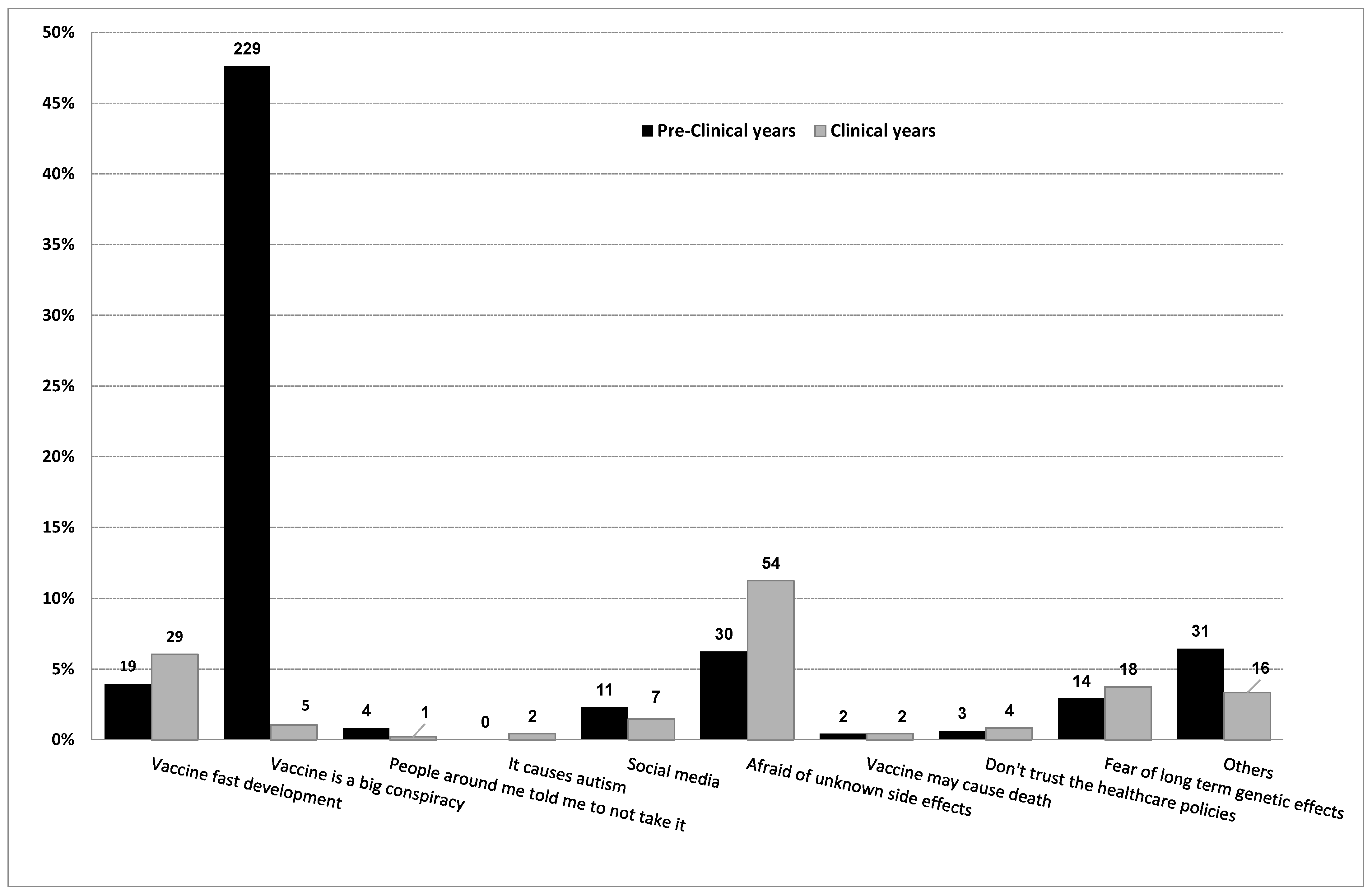
4. Discussion
5. Conclusions
6. Strength and Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wang, C.; Horby, P.W.; Hayden, F.G.; Gao, G.F. A Novel Coronavirus Outbreak of Global Health Concern. Lancet 2020, 395, 470–473. [Google Scholar] [CrossRef] [Green Version]
- Interim Clinical Guidance for Management of Patients with Confirmed 2019 Novel Coronavirus (2019-nCoV) Infection. Available online: https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html (accessed on 1 April 2021).
- COVID-19 Map. Available online: https://coronavirus.jhu.edu/map.html (accessed on 9 March 2022).
- WHO Issues Its First Emergency Use Validation for a COVID-19 Vaccine and Emphasizes Need for Equitable Global Access. Available online: https://www.who.int/news/item/31-12-2020-who-issues-its-first-emergency-use-validation-for-a-covid-19-vaccine-and-emphasizes-need-for-equitable-global-access (accessed on 10 April 2021).
- Forni, G.; Mantovani, A. COVID-19 vaccines: Where we stand and challenges ahead. Cell Death Differ. 2021, 28, 626–639. [Google Scholar] [CrossRef] [PubMed]
- COVID-19 Vaccines. Available online: https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/covid-19-vaccines (accessed on 7 November 2021).
- Interim Guidelines for the Use of SARS-CoV-2 Vaccine. Available online: https://covid19.cdc.gov.sa/professionals-health-workers/interim-guidelines-for-the-use-of-sars-cov-2-vaccine/ (accessed on 16 December 2021).
- Ten Health Issues WHO Will Tackle This Year. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 11 November 2021).
- Halpin, C.; Reid, B. Attitudes and beliefs of healthcare workers about influenza vaccination. Nurs. Older People 2021, 33, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Setbon, M.; Raude, J. Factors in vaccination intention against the pandemic influenza A/H1N1. Eur. J. Public Health 2010, 20, 490–494. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nguyen, T.; Henningsen, K.H.; Brehaut, J.C.; Hoe, E.; Wilson, K. Acceptance of a pandemic influenza vaccine: A systematic review of surveys of the general public. Infect. Drug Resist. 2011, 4, 197. [Google Scholar] [PubMed] [Green Version]
- Lucia, V.C.; Kelekar, A.; Afonso, N.M. COVID-19 vaccine hesitancy among medical students. J. Public Health 2021, 43, 445–449. [Google Scholar] [CrossRef] [PubMed]
- Saied, S.M.; Saied, E.M.; Kabbash, I.A.; Abdo, S.A.E.F. Vaccine hesitancy: Beliefs and barriers associated with COVID-19 vaccination among Egyptian medical students. J. Med. Virol. 2021, 93, 4280–4291. [Google Scholar] [CrossRef] [PubMed]
- Saudi Arabia Requires “Immunization” against the Corona Virus to Enter Facilities and Use Transportation. Available online: https://arabic.cnn.com/health/article/2021/05/18/saudi-arabia-vaccination-condition-facilities (accessed on 7 July 2021).
- Epi InfoTM|CDC. Available online: https://www.cdc.gov/epiinfo/ (accessed on 1 July 2021).
- Saudi Arabian Medical Schools by Student Number 2018/2019. Available online: https://www.statista.com/statistics/608615/saudi-arabian-medical-schools-by-student-number/ (accessed on 1 July 2021).
- MOH Launches New App (Tetamman) to Prevent COVID-19. Available online: https://www.moh.gov.sa/en/Ministry/MediaCenter/News/Pages/News-2020-04-11-004.aspx (accessed on 9 March 2022).
- Bashir, S.; Alsultan, F.; Iqbal, M.; Alabdulkarim, N.; Alammari, K.; Almousa, A.; Alsultan, A.; Almousa, B.; Albaradie, R.; Mir, A.; et al. Healthcare Workers’ Knowledge and Attitudes towards COVID-19 in Saudi Arabia. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 1060–1069. [Google Scholar] [PubMed]
- Madhi, S.A.; Baillie, V.; Cutland, C.L.; Voysey, M.; Koen, A.L.; Fairlie, L.; Padayachee, S.D.; Dheda, K.; Barnabas, S.L.; Bhorat, Q.E. Efficacy of the ChAdOx1 nCoV-19 COVID-19 vaccine against the B. 1.351 variant. N. Engl. J. Med. 2021, 384, 1885–1898. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, T.; Klemis, V.; Schub, D.; Mihm, J.; Hielscher, F.; Marx, S.; Abu-Omar, A.; Ziegler, L.; Guckelmus, C.; Urschel, R. Immunogenicity and reactogenicity of heterologous ChAdOx1 nCoV-19/mRNA vaccination. Nat. Med. 2021, 27, 1530–1535. [Google Scholar] [CrossRef] [PubMed]
- COVID-19 Vaccine Facts. Available online: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/facts.html (accessed on 21 December 2021).
- Aw, J.; Seng, J.J.B.; Seah, S.S.Y.; Low, L.L. COVID-19 vaccine hesitancy—A scoping review of literature in high-income countries. Vaccines 2021, 9, 900. [Google Scholar] [CrossRef] [PubMed]
- Bălan, A.; Bejan, I.; Bonciu, S.; Eni, C.E.; Ruță, S. Romanian Medical Students’ Attitude towards and Perceived Knowledge on COVID-19 Vaccination. Vaccines 2021, 9, 854. [Google Scholar] [CrossRef] [PubMed]
- How Did We Develop a COVID-19 Vaccine So Quickly? Medical News Today. Available online: https://www.medicalnewstoday.com/articles/how-did-we-develop-a-covid-19-vaccine-so-quickly (accessed on 11 December 2021).
- Van Tap Nguyen, M.Q.N.; Le, N.T.; Nguyen, T.N.H.; Huynh, G. Predictors of intention to get a COVID-19 vaccine of health science students: A cross-sectional study. Risk Manag. Healthc. Policy 2021, 14, 4023. [Google Scholar] [CrossRef] [PubMed]
- Islam, M.S.; Kamal, A.-H.M.; Kabir, A.; Southern, D.L.; Khan, S.H.; Hasan, S.M.; Sarkar, T.; Sharmin, S.; Das, S.; Roy, T. COVID-19 vaccine rumors and conspiracy theories: The need for cognitive inoculation against misinformation to improve vaccine adherence. PLoS ONE 2021, 16, e0251605. [Google Scholar] [CrossRef] [PubMed]
- Cavaliere, A.F. Flu and Tdap Maternal Immunization Hesitancy in Times of COVID-19: An Italian Survey on Multiethnic Sample. Vaccines 2021, 9, 1107. [Google Scholar] [CrossRef] [PubMed]
- Vilca, L.M.; Cesari, E.; Tura, A.M.; Di Stefano, A.; Vidiri, A.; Cavaliere, A.F.; Cetin, I. Barriers and Facilitators Regarding Influenza and Pertussis Maternal Vaccination Uptake: A Multi-Center Survey of Pregnant Women in Italy. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 247, 10–15. [Google Scholar] [CrossRef] [PubMed]
| Variables | n = 1445 n (%) |
|---|---|
| Gender | |
| Male | 1282 (88.7) |
| Female | 163 (11.3) |
| Age | |
| 18–20 | 465 (32.2) |
| >20 | 980 (67.8) |
| Nationality | |
| Saudi | 1428 (98.8) |
| Non-Saudi | 17 (1.2) |
| Place of residence | |
| Central region | 1291 (89.3) |
| Others | 154 (10.7) |
| Your university | |
| King Saud University | 802 (55.5) |
| King Saud Bin Abdulaziz University for health science | 316 (21.9) |
| Imam Mohammad Bin Saud Islamic University | 282 (19.5) |
| Others | 45 (3.1) |
| Current year | |
| Pre-Clinical Years | 683 (47.3) |
| Clinical Years | 762 (52.7) |
| Family income | |
| <5000 | 43 (3) |
| 5000–20,000 | 465 (32.2) |
| >20,000 | 937 (64.8) |
| Which vaccine did you receive? | |
| I didn’t get the vaccine | 231 (16) |
| BioNTech/Pfizer and Oxford-AstraZeneca | 376 (26) |
| BioNTech/Pfizer | 625 (43.3) |
| Oxford-AstraZeneca | 189 (13.1) |
| Others | 24 (1.7) |
| Have you ever been infected with COVID-19? | |
| Yes | 217 (15) |
| No | 1150 (79.6) |
| I don’t know | 78 (5.4) |
| Question | Pre-Clinical (n = 683) n (%) | Clinical (n = 762) n (%) | Total (n = 1445) n (%) | p-Value | (95% CI) |
|---|---|---|---|---|---|
| Do you agree on the importance of developing a COVID-19 vaccine to decrease its community spread? | <0.001 | (1.57–1.68) | |||
| Yes | 420 (36.7) | 723 (63.3) | 1143 (79.1) | ||
| No | 238 (91.5) | 22 (8.5) | 260 (18) | ||
| I don’t know | 25 (59.5) | 17 (40.5) | 42 (2.9) | ||
| How does the Pfizer vaccine work? | <0.001 | (2.89–3.1) | |||
| Encapsulated mRNA vaccine | 268 (32.6) | 553 (67.4) | 821 (56.8) | ||
| Virus-like particle vaccine | 20 (38.5) | 32 (61.5) | 52 (3.6) | ||
| Inactivated virus vaccine | 51 (67.1) | 25 (32.9) | 76 (5.3) | ||
| I don’t know | 344 (69.4) | 152 (30.6) | 496 (34.3) | ||
| Is it safe to take two different COVID-19 vaccines from different companies/brands? | <0.001 | (1.8–1.9) | |||
| Yes | 338 (36.8) | 581 (63.2) | 919 (63.6) | ||
| No | 256 (86.2) | 41 (13.8) | 297 (20.6) | ||
| I don’t know | 89 (38.9) | 140 (61.1) | 229 (15.8) | ||
| Can you be infected with COVID-19 via the COVID-19 vaccine? | <0.001 | (1.4–1.5) | |||
| Yes | 359 (67.1) | 176 (32.9) | 535 (37) | ||
| No | 247 (33.5) | 490 (66.5) | 737 (51) | ||
| I don’t know | 77 (44.5) | 96 (55.5) | 173 (12) | ||
| Does the COVID-19 vaccine prevent you from spreading COVID-19? | <0.001 | (1.88–1.9) | |||
| Yes | 215 (35.3) | 394 (64.7) | 609 (42.1) | ||
| No | 394 (57.7) | 289 (42.3) | 683 (47.3) | ||
| I don’t know | 74 (48.4) | 79 (51.6) | 153 (10.6) | ||
| Does the COVID-19 vaccine decrease your immunity? | <0.001 | (2.5–2.7) | |||
| Yes | 35 (57.4) | 26 (42.6) | 61 (4.2) | ||
| No | 345 (35.5) | 628 (64.5) | 973 (67.3) | ||
| I don’t know | 303 (73.7) | 108 (26.3) | 411 (28.4) | ||
| Has anyone gotten COVID-19 after being fully vaccinated? | <0.001 | (2.1–2.3) | |||
| Yes | 335 (34.7) | 630 (65.3) | 965 (66.8) | ||
| No | 28 (49.1) | 29 (50.9) | 57 (3.9) | ||
| I don’t know | 320 (75.7) | 103 (24.3) | 423 (29.3) | ||
| What are your sources of information about the COVID-19 vaccine? * | |||||
| Social media | 292 (38) | 477 (62) | 769 (53.2) | <0.001 | (0.3–0.4) |
| People around you/Friends | 177 (37.1) | 300 (62.9) | 477 (33.01) | <0.001 | (0.20–0.28) |
| WHO (World Health Organisation) | 244 (32.3) | 512 (67.7) | 756 (52.3) | <0.001 | (0.21–0.29) |
| Ministry of health | 355 (35.6) | 641 (64.4) | 996 (68.92) | <0.001 | (0.31–0.39) |
| Radio | 235 (87.4) | 34 (12.6) | 269 (18.61) | <0.001 | (0.44–0.53) |
| Television | 96 (39) | 150 (61) | 246 (17.02) | 0.004 | (0.06–0.12) |
| Newspaper | 1 (25) | 3 (75) | 4 (0.27) | 0.372 | (−0.002–0.006) |
| Others | 8 (22.9) | 27 (77.1) | 35 (2.422) | 0.003 | (0.009–0.04) |
| Question | Pre-Clinical (n = 683) n (%) | Clinical (n = 762) n (%) | Total (n = 1445) n (%) | p-Value | (95% CI) |
|---|---|---|---|---|---|
| Are you concerned about the safety of the COVID-19 vaccine? | <0.001 | (1.23–1.34) | |||
| Yes | 410 (58) | 297 (42) | 707 (48.9) | ||
| No | 236 (36.3) | 414 (63.7) | 650 (45) | ||
| I don’t know | 37 (42) | 51 (58) | 88 (6.1) | ||
| Are you concerned about the efficacy of the COVID-19 vaccine? | <0.001 | (1.22–1.32) | |||
| Yes | 432 (56.8) | 328 (43.2) | 760 (52.6) | ||
| No | 219 (35.7) | 394 (64.3) | 613 (42.4) | ||
| I don’t know | 32 (44.4) | 40 (55.6) | 72 (5) | ||
| Should the COVID-19 vaccine be taken annually? | <0.001 | (2.56–2.68) | |||
| Yes | 87 (39.4) | 134 (60.6) | 221 (15.3) | ||
| No | 147 (33.9) | 287 (66.1) | 434 (30) | ||
| I don’t know | 449 (56.8) | 341 (43.2) | 790 (54.7) | ||
| Do you trust the Ministry of Health when it comes to information about the COVID-19 vaccine? | <0.001 | (1.8–1.9) | |||
| Yes | 382 (37.3) | 642 (62.7) | 1024 (70.9) | ||
| No | 261 (79.8) | 66 (20.2) | 327 (22.6) | ||
| I don’t know | 40 (42.6) | 54 (57.4) | 94 (6.5) | ||
| Do you agree with the government’s decision about the COVID-19 vaccine being a requirement to enter a university facility? | <0.001 | (1.85–1.96) | |||
| Yes | 350 (37.2) | 590 (62.8) | 940 (65) | ||
| No | 273 (70.5) | 114 (29.5) | 387 (26.8) | ||
| I don’t know | 60 (50.8) | 58 (49.2) | 118 (8.2) | ||
| In your opinion, what is the best way to deal with the vaccine? | <0.001 | (1.76–2.02) | |||
| Free choice to take the vaccine or not | 309 (68.1) | 145 (31.9) | 454 (31.4) | ||
| Imposing vaccination on specific groups of people | 38 (39.2) | 59 (60.8) | 97 (6.7) | ||
| Make it mandatory for everyone | 99 (35.4) | 181 (64.6) | 280 (19.4) | ||
| Make it a requirement in transportation and workplace | 168 (36.8) | 289 (63.2) | 457 (31.6) | ||
| I am not sure | 69 (43.9) | 88 (56.1) | 157 (10.9) | ||
| Does the rapid development of the COVID-19 vaccine play any role in the refusal or hesitancy of the population? | <0.001 | (1.73–1.85) | |||
| Yes | 285 (33.2) | 574 (66.8) | 859 (59.4) | ||
| No | 268 (78.8) | 72 (21.2) | 340 (23.5) | ||
| I don’t know | 130 (52.8) | 116 (47.2) | 246 (17) | ||
| If the government canceled the precautions, would you wear the mask even though you received a vaccine? | <0.001 | (1.88–1.98) | |||
| Yes | 214 (36.9) | 366 (63.1) | 580 (40.1) | ||
| No | 393 (56.6) | 301 (43.4) | 694 (48) | ||
| I don’t know | 76 (44.4) | 95 (55.6) | 171 (11.8) | ||
| Do you think people would take the COVID-19 vaccine even if it costs money? | <0.001 | (1.98–2.08) | |||
| Yes | 174 (38.5) | 278 (61.5) | 452 (31.3) | ||
| No | 389 (53.8) | 334 (46.2) | 723 (50) | ||
| I don’t know | 120 (44.4) | 150 (55.6) | 270 (18.7) | ||
| Do you feel anxious about the long-term side effects of the COVID-19 vaccine? | <0.001 | (1.79–1.90) | |||
| Yes | 159 (39.5) | 244 (60.5) | 403 (27.9) | ||
| No | 452 (51.5) | 425 (48.5) | 877 (60.7) | ||
| I don’t know | 72 (43.6) | 93 (56.4) | 165 (11.4) | ||
| Do you think the COVID-19 vaccine will return life to what it was before the pandemic? | <0.001 | (2.02–2.12) | |||
| Yes | 215 (38.7) | 341 (61.3) | 556 (38.5) | ||
| No | 353 (59) | 245 (41) | 598 (41.1) | ||
| I don’t know | 115 (39.5) | 176 (60.5) | 291 (20.1) | ||
| COVID-19 vaccine is a requirement to enter a university facility; if it wasn’t a requirement, would you still take the COVID-19 vaccine? | <0.001 | (2.16–2.23) | |||
| Yes | 340 (35.3) | 624 (64.7) | 964 (66.7) | ||
| No | 293 (76.3) | 91 (23.7) | 384 (26.6) | ||
| I don’t know | 50 (51.5) | 47 (48.5) | 97 (6.7) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Habib, S.S.; Alamri, M.S.; Alkhedr, M.M.; Alkhorijah, M.A.; Jabaan, R.D.; Alanzi, M.K. Knowledge and Attitudes of Medical Students toward COVID-19 Vaccine in Saudi Arabia. Vaccines 2022, 10, 541. https://doi.org/10.3390/vaccines10040541
Habib SS, Alamri MS, Alkhedr MM, Alkhorijah MA, Jabaan RD, Alanzi MK. Knowledge and Attitudes of Medical Students toward COVID-19 Vaccine in Saudi Arabia. Vaccines. 2022; 10(4):541. https://doi.org/10.3390/vaccines10040541
Chicago/Turabian StyleHabib, Syed Shahid, Musab Saleh Alamri, Mudafr Mahmoud Alkhedr, Mohammad Abdullah Alkhorijah, Rayan Dhafer Jabaan, and Mubarak Khalid Alanzi. 2022. "Knowledge and Attitudes of Medical Students toward COVID-19 Vaccine in Saudi Arabia" Vaccines 10, no. 4: 541. https://doi.org/10.3390/vaccines10040541
APA StyleHabib, S. S., Alamri, M. S., Alkhedr, M. M., Alkhorijah, M. A., Jabaan, R. D., & Alanzi, M. K. (2022). Knowledge and Attitudes of Medical Students toward COVID-19 Vaccine in Saudi Arabia. Vaccines, 10(4), 541. https://doi.org/10.3390/vaccines10040541






