Abstract
Vaccination efforts as a mitigation strategy in the corona virus disease 2019 (COVID-19) pandemic are fully underway. A vital component of understanding the optimal clinical use of these vaccines is a thorough investigation of adverse events following vaccination. To date, some limited reports and reviews have discussed ocular adverse events following COVID-19 vaccination, but a systematic review detailing these reports with manifestations and clinical courses as well as proposed mechanisms has yet to be published. This comprehensive review one-year into vaccination efforts against COVID-19 is meant to furnish sound understanding for ophthalmologists and primary care physicians based on the existing body of clinical data. We discuss manifestations categorized into one of the following: eyelid, orbit, uveitis, retina, vascular, neuro-ophthalmology, ocular motility disorders, and other.
1. Introduction
Since the time that the first vaccines against the severe acute respiratory failure coronavirus 2 (SARS-CoV-2) and ensuing corona virus disease2019 (COVID-19) were approved for emergency authorization use by the Food and Drug Administration (FDA) in late 2020, an enormous amount of speculation has surrounded the discourse around vaccination and COVID-19 [1,2,3,4]. It remains the consensus opinion in clinical practice—and the opinion of the authors—that vaccination and subsequent booster administration against COVID-19 is a vital epidemiologic factor in mitigating the devastating effects of the COVID-19 pandemic. It is nevertheless essential that physicians and researchers investigate the possible adverse outcomes due to vaccination against COVID-19.
Previous research has demonstrated a link between COVID-19 infection and ocular complications, direct or indirect [5,6,7,8,9,10,11,12,13]. It has been well-documented that conjunctivitis, scleritis, orbital inflammatory disease, phlyctenular keratoconjunctivitis and retinal involvement may take place in COVID-19 infection. It is thus vital to also investigate the relationship between COVID-19 vaccination and ocular complications. A considerable number of reports and retrospective case studies have reported on possible adverse effects of vaccination against COVID-19 approximately one year into the dissemination of these vaccines [14,15,16]. In this review, we seek to provide a rigorous description of these findings based on a comprehensive review and statistical analysis of the literature.
2. Materials and Methods
We performed a PubMed search for articles of interest using search terms beginning with “coronavirus vaccine” or “COVID vaccine” followed by “ocular”, “palsy”, “cornea”, ”rejection”, “uveitis”, “optic neuritis”, “optic neuropathy” and “retina”. Articles were included if they were case reports or retrospective studies describing adverse ocular manifestations following any vaccination against COVID-19 between December 2020 and December 2021.
We thereafter characterized articles as belonging to one of the following categories of adverse event: eyelid, orbital, corneal, uveitis, retinal, vascular, neuro-ophthalmological, ocular motility disorders and unspecified. When possible, statistical analysis was performed for each category regarding age, sex, visual acuity, and any other pathology-specific characteristics of the categories in question. Continuous variables were reported as mean ± one standard deviation.
3. Adverse Ocular Events: Patient Overview
In total, 58 articles were included in our review. These findings are detailed in Table 1. Of these 58 studies, 28 (48.3%) were case reports, 5 (8.6%) were case series, 22 (37.9%) were letters to the editor, and 3 (5.2%) were photo essays. A total of 94 patients were included. Of 90 patients with documented age information, the mean age at the time of presentation was 46.9 ± 18.4 years. Of 91 patients with documented gender, there were 50 (54.9%) females and 41 (45.1%) males. Of the 87 cases in which vaccine information were present, BNT162b2 mRNA SARS-CoV-2 (BioNTech/Pfizer, Mainz, Germany) was reported 55 (63.2%) times, AZD1222 ChAdO×1 nCoV-19 (AstraZeneca, Cambridge, UK, also marketed as the CoviShield Serum Institute of India vaccine) was reported 20 (22.9%) times, Moderna COVID-19 Vaccine (ModernaTX, Inc., Cambridge, MA, USA) was reported 6 (6.9%) times, BBIBP-CorV (Sinopharm, Beijing, China) was reported 3 (3.4%) times, Corona Vac (Sinovac Biotech Ltd., Beijing, China) was reported 2 (2.3%) times, and Gam-COVID-Vac/Sputnik V (Gamaleya Institute, Moscow, Russia) was reported once (1.1%). Vaccine ordinal dose was reported 81 times; 45 (55.6%) cases were after the first dose, 35 (43.2%) were after the second dose, and one (1.2%) was after a 3rd (booster shot) dose.

Table 1.
Aggregated information on reviewed cases.
In our literature review, we found numerous ophthalmic adverse events following COVID-19 vaccination. Because some phenomena were reported several times and others were reported only once, we primarily discuss mechanisms and clinical considerations for phenomena which have occurred several times. Nevertheless, it is important to note that an important limitation of this analysis is that it is a retrospective review and not a cohort study. Despite the fact that we discuss mechanisms, in the absence of definitive underlying pathophysiologic processes, we must recognize the possibility that some adverse events—particularly those which are especially rare—are due to random chance.
4. Eyelid
In general, reports of eyelid manifestations following vaccination against COVID-19 are limited. Of the 2 reports (6 patients) that we reviewed, 5 of 6 patients (83.3%) were females and the mean age at the time of presentation was 48.7 ± 13.5 years [17,18]. Visual acuities were not reported.
In one study, Austria et al. reported on a series of three women who each presented with unilateral edema more prominent in the upper eyelid following vaccination with the BNT162b2 vaccine [17]. All three patients were middle-aged women (aged 32, 43, and 43) and they were all treated differently. One patient was treated with observation, another with antihistamines, and one with oral steroids. All patients had complete resolution of orbital edema within two days.
Elsewhere, Mazzatenta et al. described a case series of three patients who developed ecchymotic or purpuric lesions on the upper eyelids 1 to 3 weeks following vaccination with the BNT162b2 vaccine [18]. In all three cases, lesions were bilateral and resolved within approximately two weeks.
Regarding the mechanism of these findings, Austria et al. proposed in their report that eyelid changes may be mediated by complement activation which increased complement mediators within the tear duct via leakage of plasma [17,18]. Further investigation is required to support this hypothesis.
5. Orbit
A total of three reports (3 patients, 4 eyes) commented on orbital manifestations following vaccination against COVID-19. These cases are described below.
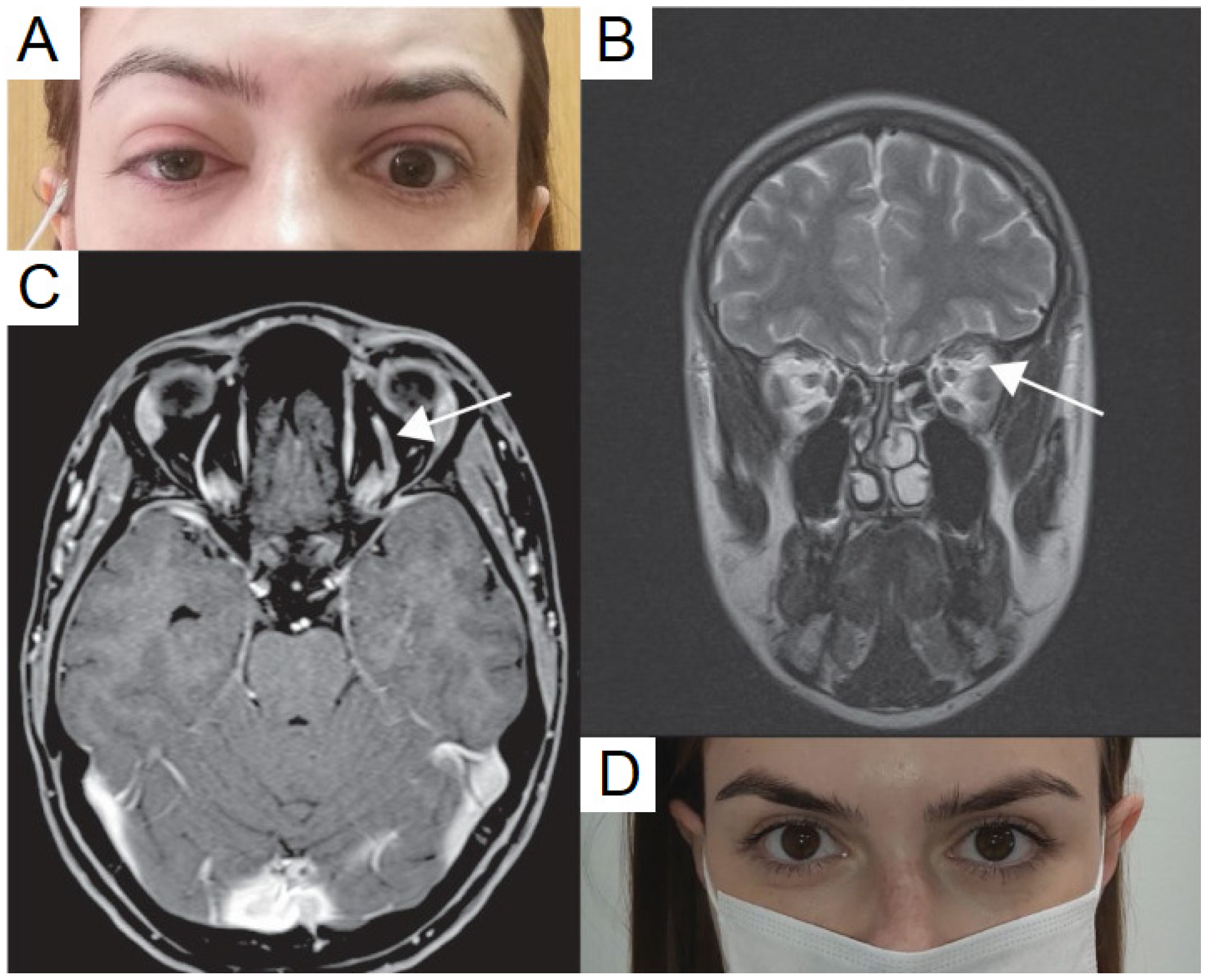
5.1. Superior Ophthalmic Vein Thrombosis
Two cases commented on superior ophthalmic vein thrombosis. Bayas et al. reported a case of a 55-year-old woman who presented with conjunctival injection, retro-orbital pain, and diplopia seven days after getting vaccination with the AZD1222 vaccine [19]. Magnetic resonance imaging (MRI) of brain and orbit with contrast showed superior ophthalmic vein thrombosis with no contrast filling and bilateral T2 signal intensity of the superior ophthalmic vein. Laboratory values revealed secondary immune thrombocytopenia. The patient later developed a transient right-sided hemiparesis and aphasia, and MRI testing demonstrated a left parietal lobe ischemic stroke. Ultimately the patient was treated with anticoagulation and discharged. Elsewhere, Panovska-Stavridis et al. reported on a case of a 29-year-old woman (Figure 1) who developed left orbital swelling, severe headache, and blurred left eye vision 10 days after receiving the AZD1222 vaccine [20]. MRI imaging demonstrated central filling defects and a diagnosis of superior ophthalmic vein thrombosis was made. The patient was treated with intravenous (IV) immunoglobulins 1 g/kg for two days, followed by an oral prednisolone taper. Concurrently, the patient was placed on rivaroxaban 15 mg twice daily for 21 days as well as broad-spectrum antibiotics. The authors reported excellent response within 5 days and the patient’s thrombocytopenia also resolved.
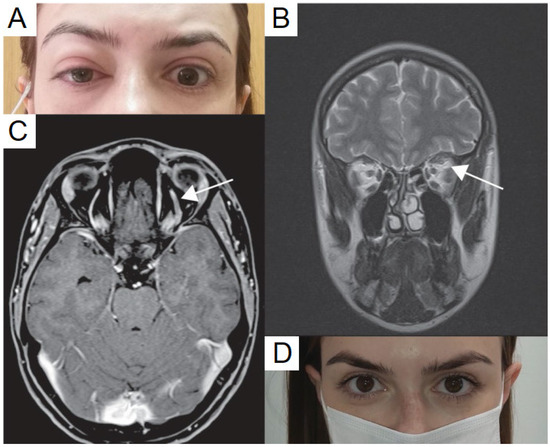
Figure 1.
Clinical presentation of the vaccine-induced prothrombotic immune thrombocytopenic disorder (VIPIT) and superior ophthalmic vein (SOV) thrombosis after ChAdOx1 nCoV-19 vaccination. (A) patient presentation at admission with marked proptosis, (B) contrast enhanced magnetic resonance imaging (MRI) revealed SOV thrombosis (white arrow), presented with widening SOV and filling defects, (C) T2 sequence further confirmed SOV thrombosis with the enhanced signal intensity of SOV (white arrow), (D) no symptoms after five days of treatment, published with patient’s permission. Adapted from Panovska-Stavridis, I.; Pivkova-Veljanovska, A.; Trajkova, S.; Lazarevska, M.; Grozdanova, A.; Filipche, V. A Rare Case of Superior Ophthalmic Vein Thrombosis and Thrombocytopenia Following ChAdOx1 nCoV-19 Vaccine Against SARS-CoV-2. Mediterr. J. Hematol. Infect. Dis. 2021, 13, e2021048; Published 1 March 2021. https://doi.org/10.4084/MJHID.2021.048 [20]. Figure 1, Copyright (2021) with permission from Institute of Hematology, Catholic University, Rome, open access article under the terms of the Creative Commons Attribution License.
5.2. Tolosa-Hunt Syndrome
Chuang et al. reported on a case of a 45-year-old male who developed left eye pain with progressive ptosis, decreased vision, and binocular diplopia seven days after receiving an unspecified COVID-19 vaccine [21]. The patient had an afferent pupillary defect (APD) and complete ophthalmoplegia. Imaging with computed tomography (CT) and MRI of the brain were most consistent with cavernous sinus thrombosis. In the setting of this constellation of findings, the patient was diagnosed with Tolosa–Hunt syndrome.
Diagnostic criteria for Tolosa–Hunt syndrome require unilateral orbital affection with associated paresis of one or more of the 3rd, 4th, and 6th cranial nerves [22]. Cavernous sinus thrombosis with Tolosa–Hunt syndrome has been reported sparingly, but a previous report of it following hepatitis-B vaccination has been described [23]. On our review of other vascular phenomena, we found limited reports of central retinal vein occlusion (CRVO), branch retinal vein occlusion (BRVO), and hemi-retinal vein occlusion (HRVO) (discussed later).
5.3. Mechanisms
The mechanisms underlying a possible hypercoagulable state following vaccination have not yet been completely elucidated. However, Schultz et al. previously reported five cases of severe venous thromboembolism—four of which were cerebral venous thrombosis—following vaccination against COVID-19 [24]. Because all cases resolved with transfusions and had an absence of hemolysis, the authors ruled out thrombotic thrombocytopenic purpura and immune thrombocytopenia. However, in all cases, there was a high level of antibodies to platelet factor-4 (PF4)-polyanion complexes, suggesting a vaccine-related variant of the phenomenon of heparin-induced thrombocytopenia termed vaccine-induced thrombotic thrombocytopenia (VITT) [24]. Indeed, thrombosis and thrombocytopenia has previously been reported following the use of Measles-Mumps-Rubella [25,26,27,28], influenza [29], pneumococcal [30], smallpox [31], and COVID-19 vaccines [24,32,33,34,35], but it is unclear if these would all fall into the category of VITT. Thrombotic microangiopathies have previously been reported following influenza vaccination and linked to thrombotic thrombocytopenic purpura, but these reports are rare [36].
It is our clinical recommendation that any patient presenting with thrombosis—with or without ophthalmic manifestations—should be tested for thrombocytopenia, response to platelet transfusion, and the presence of anti-PF4 complex antibodies.
6. Uveitis
Given the strong association between uveitis and immunologic phenomena, it would be expected that there is some relationship between vaccination against COVID-19 and uveitis. Of the 14 reports we reviewed dealing with uveitis after COVID-19 vaccination, 34 patients (44 eyes) were reported on. Of these 34, 19 (55.9%) were males, 15 (44.1%) were females, and the average age at the time of presentation was 47.6 ± 16.3 years. For the 34 patients, average time from vaccination to development of ophthalmic symptoms was 8.0 ± 8.6 days. Ten patients (29.4%) presented with bilateral manifestations. For the 40 eyes which had presenting visual acuity information, the mean presenting visual acuity was logMAR 0.421 ± 0.455 (20/52 in Snellen notation). For the 35 eyes which had both presenting and final visual acuity at last follow-up, these values were 0.434 ± 0.426 (20/54 in Snellen notation) and 0.085 ± 0.166 (20/24 in Snellen notation), respectively (p < 0.001).
6.1. Uveitis Flares
Previously, we described a case of an 18-year-old girl with a history of antinuclear antibody positive oligoarticular juvenile idiopathic arthritis (JIA) (but no prior history of uveitis) who presented with bilateral anterior uveitis 5 days after the second dose of the Sinopharm COVID-19 vaccine [37]. Examination was notable for anterior uveitis, and optical coherence tomography (OCT) showed hyperreflective dots and circulating cells in the anterior chamber (AC). Uveitis in both eyes resolved gradually after topical steroid treatment without recurrence. Similar to our case, Jain and Kalamkar reported on a 27-year-old man with past medical history of JIA and one previous episode of uveitis who developed a uveitis flare-up in the left eye (OS) two days after receiving the AZD1222 vaccine [38]. Similar to our previous report, the patient demonstrated resolution with topical steroids and cycloplegic drops.
Numerous other reports have been made. Mudie et al. described a case of a 43-year-old woman who presented with eye pain, redness, and photophobia bilaterally 3 days after her second dose of the BNT162b2 [39]. Examination was notable for a thickened choroid and pronounced inflammation in the AC and the vitreous cavity. The patient responded well to oral and topical corticosteroids with a mild recurrence after the initial attempt to taper these drugs. Renisi et al. described a similar case in a 23-year-old man who developed pain, photophobia, and a red eye four days after receiving the second dose of the BNT162b2 vaccine [40]. Examination revealed conjunctival hyperemia, posterior synechiae, and AC cells with keratic precipitates (KP) in the lower quadrants. The patient demonstrated initial improvement on topical dexamethasone and atropine drops daily over 3 weeks, then demonstrated complete resolution at 6 weeks.
Ishay et al. reported a case of a 28-year-old male with past medical history of Behçet’s disease on colchicine twice daily [41]. Ten days after receiving the BNT162b2 vaccine, the patient developed left eye pain, redness, and blurred vision. Examination revealed severe panuveitis. Unlike the previous cases, the patient was successfully treated with five days of pulse-dose IV methylprednisolone followed by oral (PO) corticosteroids and azathioprine.
In a different case, Herbort and Papasavvas reported on a 53-year-old male with pre-existing herpes keratouveitis which was inactive for 18 months without treatment [42]. Five days after receiving the Moderna COVID-19 vaccine, the patient presented with a severe flare-up of disease, including numerous KPs and elevated intraocular pressure to 41 mmHg. The patient was treated with PO valacyclovir 500 mg, topical dexamethasone, dorzolamide, and timolol. Over 6 days of treatment, the patient demonstrated an improvement in flare, and KPs resolved almost completely after 3 weeks.
To date, the largest and only multicenter study investigating a relationship between uveitis and COVID-19 vaccination was conducted by Rabinovitch et al. [43]. In their study, the authors examined 23 eyes of 21 patients (mean age of 51.3 years) who developed uveitis after vaccination against COVID-19 with the BNT162b2 vaccine. These patients presented with uveitis an average of 7.5 ± 7.3 days after vaccination. A total of 8 of the 21 patients had pre-existing uveitis, though average time since last flare was one year, and no patients had recent changes in medication regimen. Eight of 21 patients presented after first dose of vaccination and 13 of 21 presented after second dose of vaccination. Six of the 21 patients had pre-existing uveitis-related diseases, including ankylosing spondylitis, psoriasis, Crohn’s disease, and herpes zoster (VZV) ophthalmicus. Two patients had bilateral disease presentation. Twenty-one of 23 eyes had anterior uveitis and two eyes had multiple evanescent white dot syndrome. Nineteen of 21 patients were treated with steroids, most commonly prednisone or dexamethasone, and all 19 of these patients demonstrated complete resolution of inflammation. Two of 21 patients did not undergo treatment but demonstrated significant improvement, nevertheless.
6.2. Choroiditis
Two reports have been made connecting choroiditis with vaccination against COVID-19. Goyal et al. reported on a 34-year-old male who developed ocular pain and nasal redness OS as well as a floater in the right eye (OD) progressing to severe vision loss 4 days after receiving the AZD1222 vaccine [44]. At presentation, his visual acuity was 20/120 OD and 20/20 OS. The patient’s fundus exam demonstrated multiple bilateral oval lesions at the level of the choroid with serous detachment, consistent with a diagnosis of bilateral multifocal choroiditis. The patient was treated with a PO prednisolone taper to beginning at 100 mg daily and demonstrated significant improvement in inflammation and subretinal fluid after 11 days of treatment. His visual acuity at the last follow-up was 20/20 in both eyes.
Another report by Pan et al. described a 50-year-old woman who developed bilateral blurred vision her 5 days after receiving an unspecified Vero cell-based vaccine in China [45]. Her examination revealed a pale, blurry optic disc, absent foveal reflex, and macular edema. Imaging with fluorescein angiography was consistent with bilateral choroiditis. The patient’s vision and inflammation improved considerably over 5 weeks with periocular triamcinolone acetamide and PO prednisone.
6.3. Vogt–Koyanagi–Harada Disease
Vogt–Koyanagi–Harada (VKH) disease is a T-lymphocyte mediated multi-system disease affecting the auditory system, skin, meninges, and eye [46,47]. Ophthalmologically, it causes a granulomatous panuveitis often affecting young adults, and may also present with exudative retinal detachments and a sunset glow fundus [46,47,48,49]. As it is an autoimmune disease resulting from antibodies against melanocytes-associated antigens, the robust immune response mounted by patients following vaccination against COVID-19 may be of importance to patients living with VKH or other autoimmune diseases.
Papasavvas and Herbort reported on a 43-year-old woman who had a previous history of VKH disease which was under control for 6 years using mycophenolate, cyclosporine, and intermittent infliximab infusions [50]. However, six weeks after the second dose of the BNT162b2 vaccine, the patient presented with severe reactivation of disease. Although her visual acuity remained 20/20 OD and OS, she had severe AC inflammation with 3–4 small mutton-fat KPs as well as bilateral exudative retinal detachments. Several hypofluorescent dark dots were present on indocyanine green angiography (ICGA), which was also observed when the patient was first diagnosed with VKH disease. This flare was ultimately controlled using infliximab. Furthermore, the authors speculated that the flare had occurred with the second dose because the patient’s last infliximab infusion had been performed 3.5 weeks before her first dose of the vaccine but 7.5 weeks before the second dose. This case in particular highlights the possibility that COVID-19 vaccination may be associated with reactivation or exacerbation of pre-existing autoimmune disease.
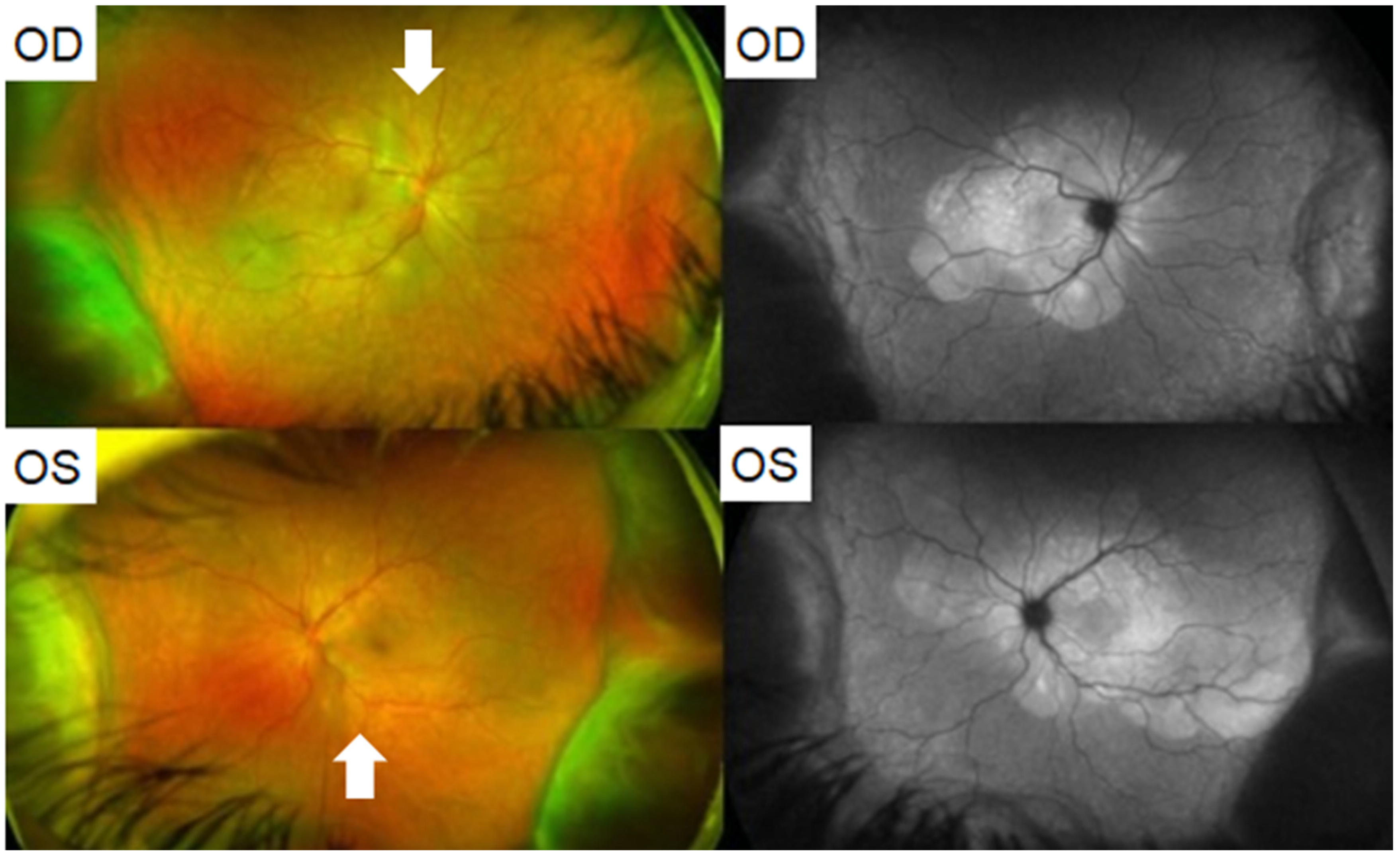
In another report, Saraceno et al. described a 62-year-old female who developed acute bilateral loss of vision two days after receiving the AZD1222 vaccine [51]. She was found to have visual acuity of 20/600 OD and 20/200 OS. On examination, she had 2+ AC cells and 1+ vitreous cells bilaterally. Fundus examination revealed serous retinal detachments and optic disc hyperemia bilaterally (Figure 2). OCT demonstrated subretinal hyperreflective dots. In this case also a diagnosis of VKH was made. The patient was treated with PO prednisone. Intravenous therapy was avoided due to a restriction in available hospital beds. Within four days, the patient’s visual acuity improved to 20/60 OD and 20/80 OS. At a three week follow up, the patient remarkably demonstrated visual acuity of 20/20 in both eyes with no signs of inflammatory activity and resolution of the exudative retinal detachments. Of note, the authors also described a case of VKH which developed in a 37-year-old female patient two weeks after she tested positive for COVID-19 on a polymerase chain reaction (PCR) test—i.e., in the setting of COVID-19 infection—as opposed to after vaccination [51]. Similarly, the patient had vision loss and signs of inflammation: She had KPs OD, mild vitritis bilaterally, and fluorescein angiography demonstrated bilateral optic disc hyperfluorescence due to leakage. The patient had bilateral serous retinal detachments as well. This patient was also treated with PO prednisone with improvement in vision and resolution of retinal detachments. These reports of VKH in the setting of both COVID-19 vaccination and infection suggest that there may be a common immunologic link between vaccination against and infection with COVID-19 which connects them both to the development of VKH.
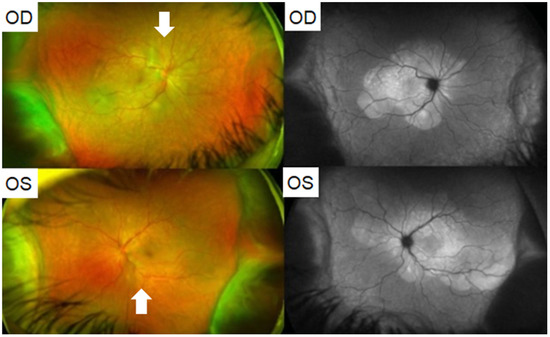
Figure 2.
(Patient 1) Fundus photography and autofluorescence of both eyes showing serous retinal detachment (white arrows) and optic disc hyperemia. Adapted from Saraceno, J.J.F.; Souza, G.M.; Dos Santos Finamor, L.P.; Nascimento, H.M.; Belfort, R., Jr.; Vogt-Koyanagi-Harada Syndrome following COVID-19 and ChAdOx1 nCoV-19 (AZD1222) vaccine. Int. J. Retina Vitreous. 2021, 7, 49; Published 30 August 2021. https://doi.org/10.1186/s40942-021-00319-3 [51]. Figure 1 Copyright (2021) with permission from Springer Nature, open access article under the terms of the Creative Commons Attribution License.
6.4. Acute Retinal Necrosis
Finally, Mishra et al. reported on a 71-year-old man who developed reactivation of VZV OD following his first dose of the AZD1222 vaccine [52]. The patient presented with panuveitis, circumcorneal congestion, multiple fine KPs, vitritis, and widespread acute retinal necrosis. He was successfully treated with 12 weeks of PO valacyclovir 1 g three times daily and a PO prednisolone taper starting at 40 mg.
6.5. Acute Zonal Occult Outer Retinopathy
Maleki et al. reported on a 33-year-old woman who developed bilateral photopsias and a progressive nasal field defect OS 10 days after receiving the second dose of the Moderna COVID-19 vaccine [53]. Imaging with OCT was demonstrative of an outer layer segmental disruption OS. A diagnosis of acute zonal occult outer retinopathy (AZOOR) was made.
6.6. Mechanisms
The primary uveitic phenomenon we encountered on our review was new uveitis or flare-ups of pre-existing disease. Uveitis has previously been documented following numerous vaccines, most commonly the Bacille Calmette–Guerin, hepatitis B, human papillomavirus, influenza, measles-mumps-rubella, and varicella vaccines [54,55,56,57,58]. One review of 276 found that 199 (72.1%) cases were in women [58].
There are several possible mechanisms underpinning the development of post-vaccination uveitis. Fraunfelder et al. previously studied the connection between the hepatitis B vaccine and uveitis and proposed that a delayed-type hypersensitivity reaction and immune complex deposition following vaccination leads to uveitis [56]. The authors also proposed that adjuvants play a role in this immunologic process, though this does not apply to COVID-19 vaccination. Elsewhere, Aguirre et al. reported a uveitic reaction in dogs following vaccination with canine adenovirus 1, which was found to be a type III hypersensitivity reaction involving antigen-antibody complexes present in the aqueous humor [59]. Given the previously established fact that SARS-CoV-2 RNA has been found in human aqueous humor and other ocular tissues, a similar inflammatory reaction involving immune complex deposition is likely [60,61].
In their major review of uveitis following COVID-19 vaccination with the BNT162b2 vaccine, Rabinovitch et al. proposed that the possible causal mechanism is vaccine-induced type I interferon secretion [43]. The authors proposed that the vaccine mRNA activates RNA-sensing molecules including TLR3, TLR7, MDA5, and RIG-I which drive autoimmune processes in these patients. While not mutually exclusive, we favor the phenomenon of immune-complex deposition as the primary driver of COVID-19 vaccine-related uveitis. However, it has been reported that COVID-19 vaccines use the modified nucleobase N1-methylpseudouridine in order to dampen immunostimulatory potential [62]. Further investigation is required to evaluate the extent to which this impacts COVID-19 vaccine-related uveitis.
7. Cornea
A number of studies have reported on adverse events at the level of the ocular surface following vaccination to COVID-19. On our review, 11 reports (15 patients, 18 eyes) described corneal manifestations following vaccination against COVID-19. Of these 15 patients, 9 (66.7%) were female and 6 (33.3%) were male. The mean age at the time of presentation was 61.33 ± 15.5 years, and the average time from vaccination to development of ophthalmic symptoms was 11.8 ± 6.2 days. Three patients (20.0%) presented with bilateral involvement. For the 17 affected eyes which had reported visual acuity, the mean visual acuity was logMAR 1.09 ± 0.858 (20/247 in Snellen notation) at presentation. Only 5 studies (6 patients, 7 eyes) reported on baseline, post-transplantation visual acuity of patients who underwent graft rejection after vaccination. For these patients, baseline visual acuity was logMAR 0.204 ± 0.309 (20/32 in Snellen notation), whereas visual acuity at presentation after vaccination was logMAR 0.871 ± 0.694 (20/149 in Snellen notation). This difference was significant (p = 0.007). For the 13 eyes which had both presenting and final visual acuities reported, the mean visual acuities were 1.215 ± 0.878 (20/328 in Snellen notation) and 0.482 ± 0.793 (20/61 in Snellen notation), respectively (p < 0.001).
7.1. Graft Rejection
Several reports have described complications involving corneal transplant rejection following vaccination to COVID-19. Phylactou et al. reported on a pair of cases [63]. First, they described a 66-year-old woman with Fuchs endothelial corneal dystrophy (FECD) status-post unilateral Descemet’s membrane endothelial keratoplasty (DMEK) transplant in the right eye who received the BNT162b2 vaccine 14 days after DMEK. Seven days after receiving her vaccination, she presented with a visual acuity of 20/120 OD. Examination revealed moderate conjunctival injection, diffuse corneal edema, fine KPs, and 1+ AC cells. Central corneal thickness (CCT) was 652 µm, significantly increased from 525 µm one week after transplantation. She was diagnosed with acute unilateral graft rejection. She was treated with an increase in frequency of topical steroids and one week later demonstrated 20/20 vision OD with a clear cornea and decreased inflammation. The authors also reported on an 83-year-old woman with bilateral DMEK transplants for FECD 3 and 6 years before developing acute bilateral endothelial rejection, 3 weeks after her second dose of the BNT162b2 vaccine. In this case also, the patient was treated with topical steroid drops and demonstrated significant improvement at a one-week follow-up.
Several other reports have also been made. Crnej et al. reported on a 71-year-old patient who underwent DMEK surgery 5 months earlier and developed acute unilateral graft rejection 7 days after receiving his second dose of the BNT162b2 vaccination [64]. In that case, the patient was treated successfully with topical dexamethasone 1 mg/mL every two hours.
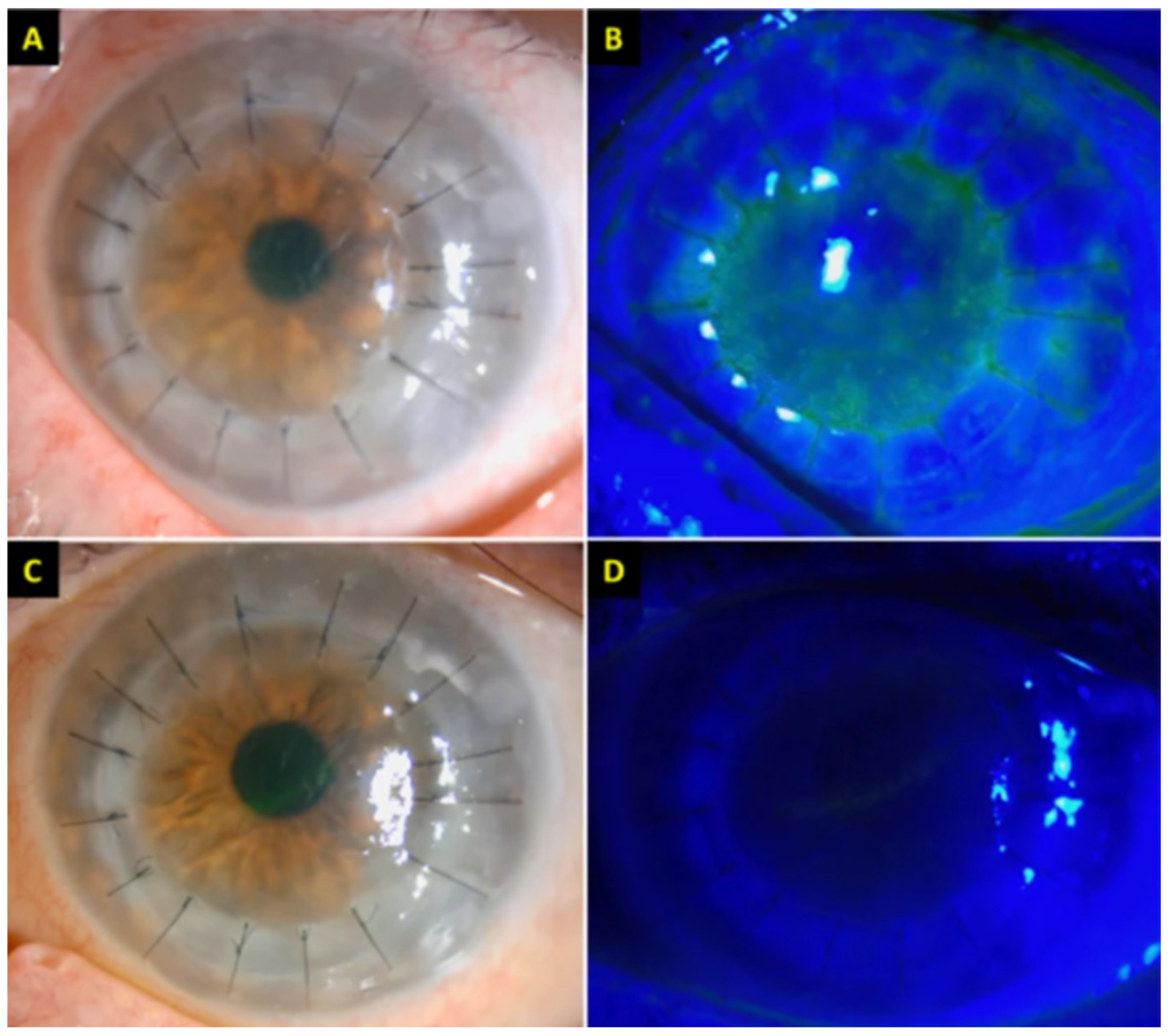
Wasser et al. reported on a pair of men, aged 56 and 73, both with a history of penetrating keratoplasty (PKP) due to keratoconus, who developed acute corneal graft rejection 2 weeks after receiving their first dose of the BNT162b2 vaccine [65]. Similar to other cases of graft rejection, both patients presented with vision loss, corneal edema, and KPs. Of note, the 56-year-old man had pre-existing grafts in both eyes but only his right eye (PKP done 25 years earlier) had rejection, while his left eye (PKP done 7 years earlier) remained intact. Both patients were successfully treated with hourly dexamethasone and oral prednisone 60 mg/day. Rallis et al. reported on a similar case of a 68-year-old woman with previous bilateral lamellar Descemet stripping automated endothelial keratoplasty (DSAEK) for previous FECD and a left re-do PKP for failed DSAEK [66]. She presented with pain and redness and rapid vision loss OS four days after receiving her first dose of the BNT162b2 vaccine. Her examination demonstrated corneal punctuate straining, corneal graft edema, Descemet’s folds, and scattered KPs, all in the left eye only (Figure 3). Similar to the case mentioned in Wasser et al., her pre-existing right eye graft was completely unaffected. At a three-week follow-up, she demonstrated complete resolution of these symptoms following hourly topical dexamethasone 0.1% and a week of PO acyclovir 400 mg five times daily to cover for herpes simplex keratitis.
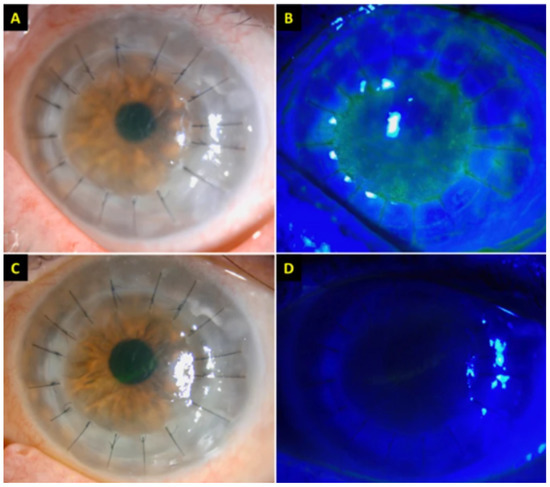
Figure 3.
(A,B) Slit-lamp photography demonstrating conjunctival hyperemia, corneal graft haze, diffuse corneal epithelial, and stromal oedema (within the graft), Descemet’s folds, scattered keratic precipitates (KPs), and 1+ cells in anterior chamber. An unusual distribution of fluorescein staining with coarse punctate epitheliopathy over the corneal graft was observed. The central corneal thickness (CCT) was 730 μm. (C,D) At 3-week post treatment, the corneal graft rejection was successfully treated with considerable improvement in the graft transparency, reduction in epithelial and stromal oedema, and resolution of epitheliopathy and anterior chamber inflammation. The best-corrected visual acuity improved to 6/12, with a CCT of 609 μm. Adapted from Rallis, K.I.; Ting, D.S.J.; Said, D.G.; et al. Corneal graft rejection following COVID-19 vaccine. Eye (2021). https://doi.org/10.1038/s41433-021-01671-2 [65]. Figure 1, Copyright (2021) with permission from Nature Publications, open access article under the terms of the Creative Commons Attribution License.
In comparison, Abousy et al. described a case of a 73-year-old woman with previous bilateral DSEK for FECD who presented with bilateral decreased vision, ocular pain, and photophobia four days after her second dose of the BNT162b2 vaccine [67]. Examination revealed decreased vision to 20/200 OD and 20/40 OS as well as corneal edema OD. Further examination revealed Descemet folds bilaterally. The patient was diagnosed with bilateral graft rejection. The patient was initiated on topical prednisolone acetate 1% four times per day. She had initially persistent and worsening symptoms on this regimen at her 28-day follow-up, so prednisolone frequency was increased to hourly, and Muro ointment was added at bedtime. Prednisolone was tapered with improvement and at a two-month follow-up, the patient’s vision had improved to 20/50 OD and 20/25 OS, with significantly decreased corneal edema bilaterally., Taken together, these cases suggest that graft rejection can be unilateral or bilateral post-COVID-19 vaccination.
Similar cases of post-PKP were reported separately by Ravichandran et al., Nioi et al., and Parmar et al. in adult patients [68,69,70]. Nioi et al. uniquely found that their 44-year-old female patient had severe vitamin D deficiency concurrently with rejection, so the patient was treated with topical dexamethasone and vitamin D supplementation. After initial resolution at four weeks, she again had an episode of rejection concurrently with persistent vitamin D deficiency, and steroid drops were re-started with higher doses of vitamin D, which resulted in sustained resolution. Vitamin D deficiency has previously been demonstrated to play a vital role in adverse effects following solid organ transplantation, namely allograft rejection [71,72,73]. It plays a vital role the expression of IL-2 and interferon-mRNA, downregulates T-cell mediated cytotoxicity, and suppresses major histocompatibility complexes of immunomodulators of dendritic cells [68,74,75]. The authors supported this explanation for their patient.
7.2. Corneal Melting
Khan et al. reported on a 48-year-old man who developed profound vision loss to light perception three weeks after receiving his first dose of the AZD1222 vaccine [76]. He was found to have diffuse conjunctival and ciliary congestion, corneal melting and perforation with diffuse corneal haze, uveal tissue prolapse, and bilateral massive choroidal detachment on B-scan ultrasonography.
7.3. Mechanisms
Our review primarily revealed several cases of corneal graft rejection, both unilateral and bilateral. Corneal transplant rejection has previously been reported—albeit rarely—following influenza, hepatitis B, tetanus, and yellow fever vaccinations [77,78,79,80]. In the setting of this pre-existing precedent, it is not surprising that the highly immunogenic vaccines to COVID-19 present similar risks.
There are several possible mechanisms underlying corneal graft compromise following vaccination. One hypothesis proposed by Steinemann et al. asserts that elevated vascular permeability following vaccination compromises the native-state immunologic privilege possessed by the cornea [77]. This theory is supported by the finding of graft edema, as demonstrated on our review. In the same case series, the Steinemann et al. also proposed that immunization may induce expression of the major histocompatibility complex (MHC) of the cornea, as various organ grafts result in enhancement of MHC antigenic expression after rejection [77]. Donor cells with no MHC expression are thereafter targeted by the host immune cells due to poor immunogenicity [77,81].
Another mechanism for corneal graft rejection proposed in the setting of vaccination to COVID-19 by Abousy et al. revolves around the finding that SARS-CoV-2 RNA is present in the aqueous humor of patients with asymptomatic infections [61,67]. Likewise, Sawant et al. found that SARS-CoV-2 RNA was found in the corneas of postmortem COVID-19 patients [60]. In the setting of vaccination for COVID-19 during ongoing or previous asymptomatic infection, then, it is possible that antibody-antigen complexes would be formed in large quantities with the subsequent development of profound inflammation, again compromising the integrity of corneal grafts.
Regardless of the mechanism, we propose that ophthalmologists consider examining patients with corneal grafts prior to vaccination against COVID-19 in order to evaluate underlying inflammatory processes which may be further exacerbated by the introduction of a profound immunogenic stimulus such as a COVID-19 vaccine. Particularly if we consider the effect of different immune processes to be additive, it may be optimal for patients with corneal grafts to delay COVID-19 vaccination if experiencing a transient inflammatory process around the time of vaccination. However, given the fact that the cases of corneal graft rejection have been successfully managed with topical steroids, whereas COVID-19 infection presents grave individual and epidemiologic risks, we do not recommend that patients avoid receiving the vaccine altogether.
8. Retina
Preliminary reports suggest that retinal adverse events are possible following vaccination against COVID-19. On our review, 12 reports (14 patients, 19 eyes) commented on retinal manifestations following vaccination against COVID-19. One report did not include information on the sex of two patients. Of the remaining 12 patients, 10 (83.3%) were women and 2 (16.7%) were men. The mean age at the time of presentation was 24.8 ± 4.8 years, and the average time from vaccination to development of ophthalmic symptoms was 3.1 ± 2.4 days. Five patients (35.7%) presented with bilateral involvement. For the 19 affected eyes which had presenting visual acuities, the mean visual acuity was logMAR 0.138 ± 0.325 (20/27 in Snellen notation) at presentation. For the 6 eyes which had both presenting and final visual acuities reported, the mean visual acuities were 0.350 ± 0.465 (20/45 in Snellen notation) and 0.030 ± 0.067 (20/21 in Snellen notation), respectively (p = 0.138).
8.1. Acute Macular Neuroretinopathy
Acute macular neuroretinopathy (AMN) is a rare disease, commonly affecting adult females, which frequently presents with the acute onset of paracentral scotomas affecting one or both eyes [82,83,84,85]. Fundus exam may demonstrate reddish-brown petaloid perifoveal lesions with the tip pointed toward the fovea [83,86]. There are no known treatment modalities for AMN, and vision changes may be permanent [85].
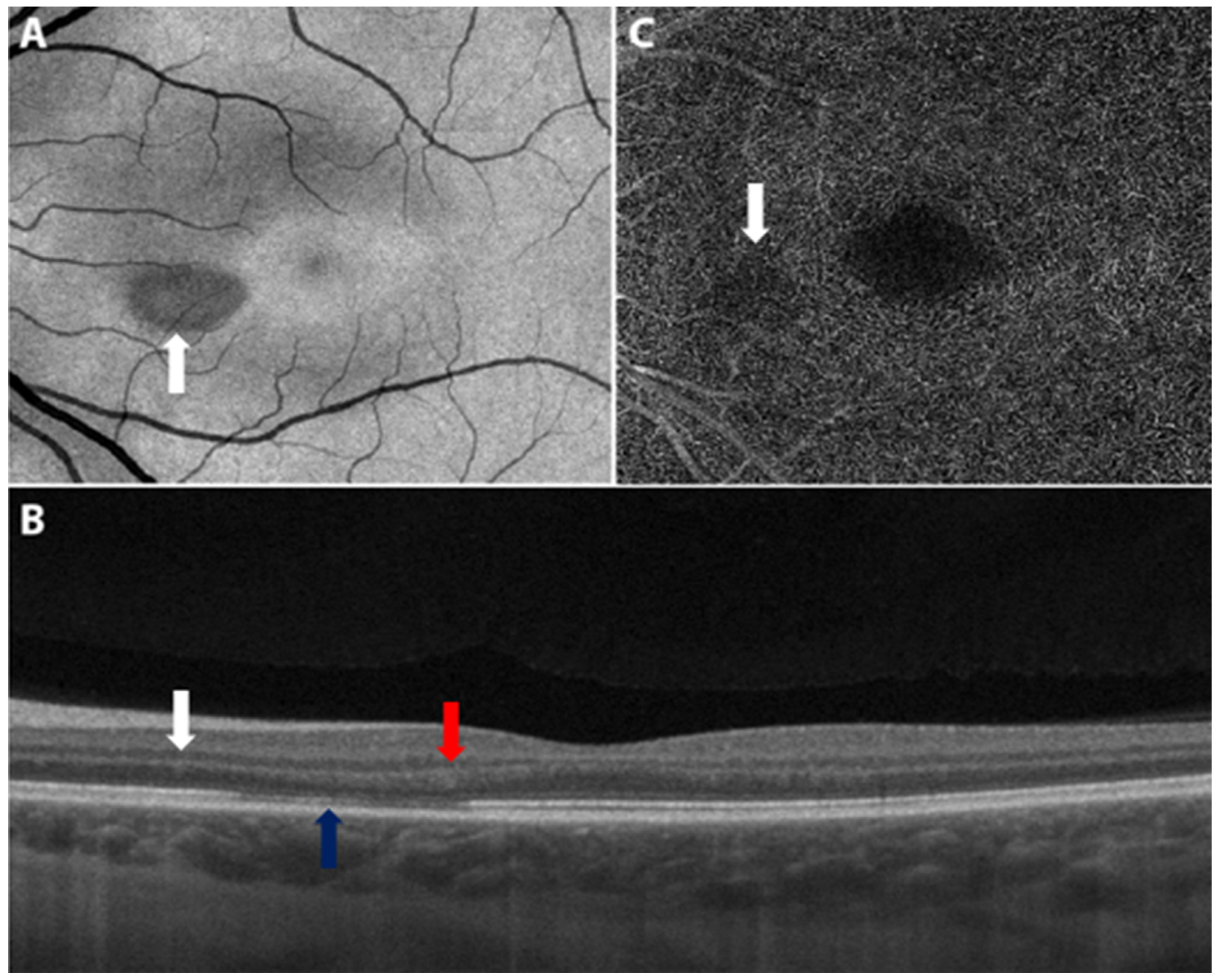
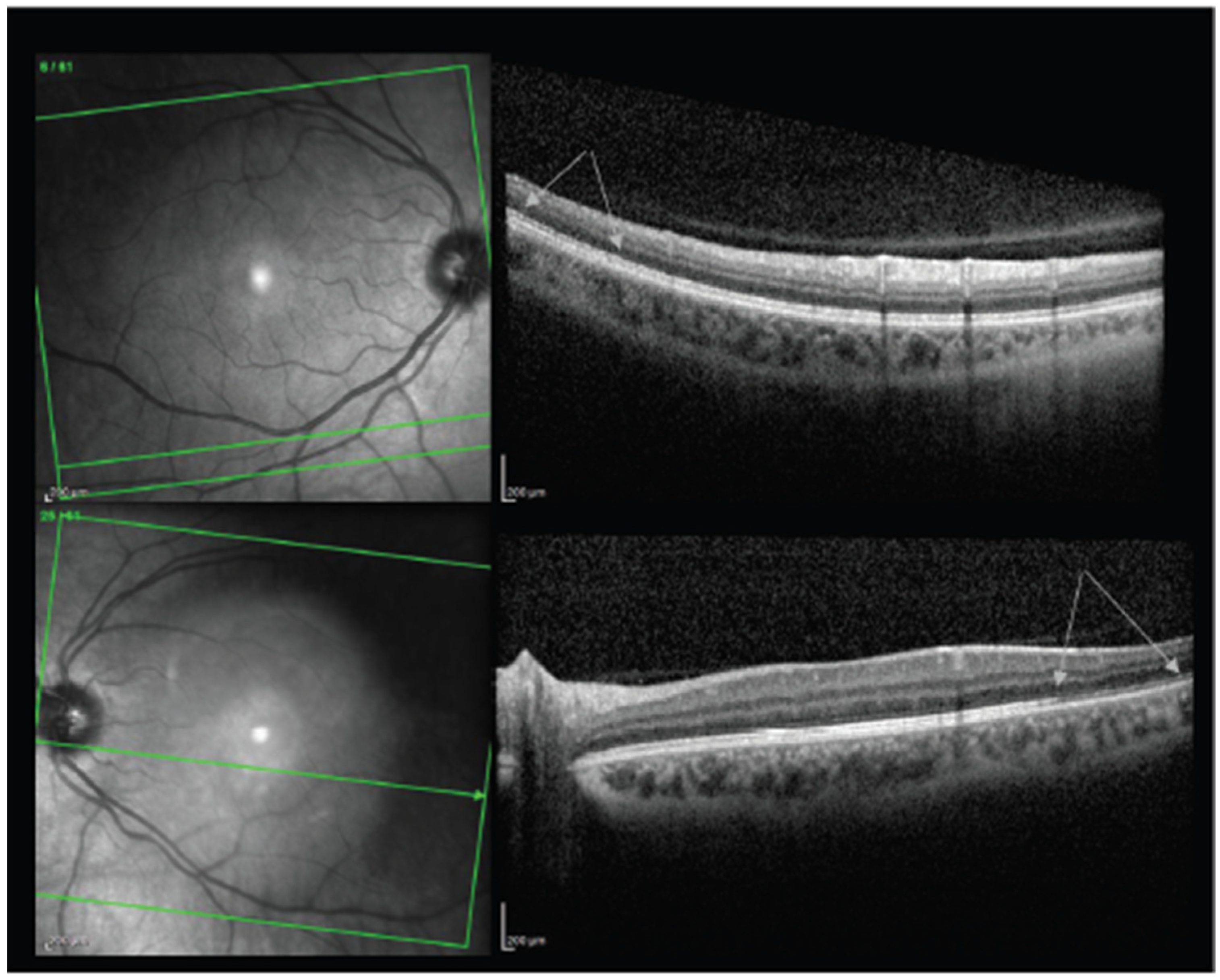
A number of reports suggest that there is an association between vaccination for COVID-19 and development of AMN. Bøhler et al. reported on a 27-year-old female with no past medical history who developed flu-like symptoms followed by a paracentral scotoma OS two days after receiving the AZD1222 vaccine [87]. Examination was notable only for a teardrop-shaped lesion nasal to the fovea. Swept-source OCT revealed slight hyperreflectivity of the outer nuclear and plexiform layers and disruption of the ellipsoid zone (Figure 4). She was diagnosed with unilateral AMN OS. Treatment was not reported. A pair of unilateral AMN cases were likewise reported in women aged 22 and 28 two days following the AZD1222 vaccine by Mambretti et al. [88]. Chen et al. reported a similar case with similar exam findings in a 21-year-old woman who developed paracentral scotomas three days after receiving her first dose of the BNT162b2 vaccine [89].
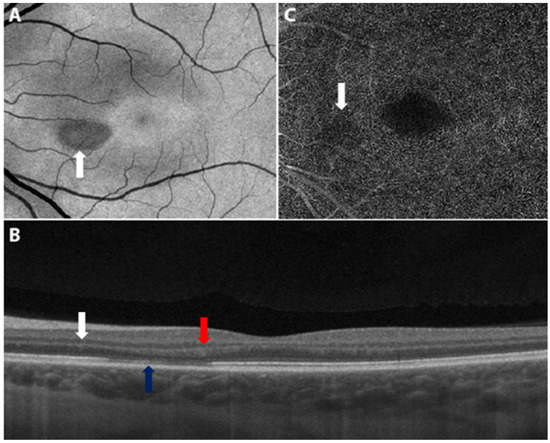
Figure 4.
Swept source optical coherence tomography of the left macula. (A) The en face image displays a teardrop-shaped macular lesion (white arrow) nasally to the fovea. (B) The cross-sectional image displays slight hyperreflectivity of the outer nuclear (white arrow) and plexiform (red arrow) layers and disruption of the ellipsoid zone (blue arrow) corresponding to the lesion. (C) The angiogram indicates subtle dropout (white arrow) in the deep capillary plexus corresponding to the lesion. Adapted from Bøhler, A.D.; Strøm, M.E.; Sandvig, K.U.; et al. Acute macular neuroretinopathy following COVID-19 vaccination. Eye (2021). https://doi.org/10.1038/s41433-021-01610-1 [87]. Figure 2, Copyright (2021) with permission from Springer Nature, open access article under the terms of the Creative Commons Attribution License.
A report made by Pichi et al. regarding unilateral AMN OS was unique in that the patient presented after vaccination with the BBIBP-CorV (Sinopharm) vaccine [90]. Furthermore, the patient presented with visual acuity of 20/400—considerably worse than other cases—despite having similar OCT findings as in previous cases. The authors reported that, with observation only, the patient demonstrated significant improvement back to a baseline visual acuity of 20/30.
Michel et al. reported AMN in a 21-year-old woman two days after receiving the AZD1222 vaccine but reported that the patient initially presented with four central scotomas OS, a greater number than in other reports we reviewed. With observation only, however, there was loss of hyperreflectivity of her lesions four days after presentation and her visual field testing showed improvement four weeks later.
In comparison, Book et al. reported a case of a 21-year-old woman with no past medical history who developed bilateral paracentral scotomas 3 days after receiving the AZD1222 vaccine [91]. Near-infrared imaging and OCT revealed similar lesions as the previous case, but bilaterally. She was diagnosed with bilateral AMN. Druke et al. reported a similar case of a 23-year-old female who developed bilateral paracentral scotomas one day after vaccination with the AZD1222 vaccine [92]. Fundus photography revealed a subtle brownish rimmed lesion parafoveal in the right eye and a blurred lesion nasal to the macula. Near-infrared imaging and OCT imaging confirmed a diagnosis of bilateral AMN. Valenzuela et al. described a similar report of bilateral AMN following vaccination with the second dose BNT162b2 vaccine [93]. In contrast to other reports, the authors reported resolution of symptoms after 7 days with observation only.
8.2. Paracentral Acute Middle Maculopathy
Paracentral acute middle maculopathy (PAMM) is an entity similar yet distinct to AMN [94,95,96]. Rahimy et al. previously described PAMM as a more superficial variant of AMN with similar manifestations such as acute paracentral scotomas and similar imaging findings of hyporeflective macular lesions [97,98]. However, PAMM predominantly affects middle-aged men, whereas AMN predominantly affects young women [84,85,97,98]. Furthermore, PAMM lesions manifest as thinning and atrophy of the inner nerve fiber layer, whereas AMN lesions manifest at the junction of the outer plexiform and outer nerve fiber layers [97,98].
Limited reports suggest that vaccination against COVID-19 may have an association with PAMM as well. Pichi et al. reported on a patient who received the BBIBP-CorV (Sinopharm) vaccine, and 20 min later developed persistent tachycardia, systolic hypertension, and concurrent development of an inferior scotoma OS [90]. The patient’s fundus examination revealed a suprafoveal dot hemorrhage OS. OCTA showed an area of flow disturbance superior to the fovea OS, and en face swept-source OCT showed a round area of hyperreflectivity superior to the fovea. A diagnosis of PAMM was made. The authors did not comment on follow-up.
Another report by Vinzamuri et al. described a 35-year-old man who received the first dose of the AZD1222 vaccine and developed reduced brightness of vision in both eyes over four weeks [99]. After receiving his second dose, his symptoms progressed further, and he was examined by an ophthalmologist. Although his acuity was 20/20 in both eyes, OCT of his macula revealed hyperreflective lesions involving the nerve fiber layer, ganglion cell layer, and outer plexiform layer. There was focal loss of the external limiting membrane in both eyes. He was diagnosed with bilateral PAMM and AMN simultaneously. With observation only, there was improvement in the patient’s symptoms at a three-week follow-up, with significant reduction in the number and size of hyperreflectivity lesions.
8.3. Other Reports
Other reports of retinal phenomena exist but have been reported infrequently. Multiple reports made mention of retinal detachments. Fowler et al. reported on a 33-year-old man who developed blurry vision three days after receiving his first dose of the BNT162b2 vaccine [100]. The patient was found to have a macular serous detachment of the neurosensory retina and OCT revealed a diagnosis of central serous retinopathy. He was successfully treated over three months with spironolactone 50 mg daily. Khochtali et al. reported a case of foveolitis OS in a 24-year-old woman after her first dose of the BNT162b2 vaccine [101]. Imaging showed diffuse retinal vascular leakage, faint foveal hyperfluorescence and late phase hypofluorescence of the foveal lesion, and granular hyperreflective specks in the inner nuclear layer. She demonstrated improvement of her lesions on a six-week PO prednisolone taper and resolution at three months.
8.4. Mechanisms
The most commonly reported retinal adverse event following COVID-19 vaccination on our review was AMN. Previous studies have proposed ischemia of the deep capillary plexus (DCP) in the inner nerve fiber layer as the pathologic mechanism underlying AMN [85,86]. Risk factors for AMN include concurrent viral illness, oral contraceptive use, and vasoactive events such as trauma, dehydration, and shock [85]. Of note, oral contraceptive use was described in all cases of AMN we received.
Reports connecting AMN and vaccination are limited. However, Shah et al. and Liu et al. have previously described AMN following influenza vaccination in women aged 42 and 47, respectively [102,103]. In both cases, there was a demonstration of reduced DCP flow on OCTA imaging at baseline and restoration of flow at follow-up.
Mambretti et al. proposed in their reports of AMN that the pro-inflammatory state following COVID-19 vaccination may have had a compounding effect on the pro-thrombotic effects of oral contraceptives [88]. Furthermore, they proposed that hypovolemia associated with the inflammatory reaction following vaccination may have led to reduced blood flow in the DCP. Only the reports by Bøhler et al. and Pichi et al. commented on imaging findings in the retinal vasculature, but both mentioned compromised flow in the DCP [87,90].
While the exact mechanism remains unclear, Giacuzzo et al. also reported development of bilateral AMN in the setting of COVID-19 infection with reduced flow in the DCP and unusually large, confluent lesions bilaterally compared to the usual smaller, petaloid lesions [104]. Future investigation should examine whether there is a unifying immunologic explanation underlying COVID-19 vaccination, infection, and development of AMN.
9. Vascular
Previous discussion around COVID-19 vaccination has raised the question of whether or not vaccines to COVID-19 confer upon patients a hypercoagulable state [105,106,107]. We reviewed 4 reports (5 patients, 6 eyes) commenting on vascular events following COVID-19 vaccination. Of these 5 patients, 4 (80.0%) were male and 1 (20.0%) was female. The mean age at the time of presentation was 54.6 ± 18.1 years, and the average time from vaccination to development of ophthalmic symptoms was 5.4 ± 6.6 days. One patient (20.0%) presented with bilateral involvement. All 6 eyes had both presenting and final visual acuities reported; the means, respectively, were logMAR 0.676 ± 0.797 (20/95 in Snellen notation) and 0.016 ± 0.036 (20/21) (p = 0.128).
9.1. Central and Hemi-Retinal Vein Occlusion
Two reports of central retinal vein occlusion (CRVO) have been made following vaccination against COVID-19. Bialasiewicz et al. reported on a 50-year-old male who developed immediate bilateral retrobulbar pain, red eye, and vision loss 15 min after receiving the BNT162B2 [108]. Fundus exam revealed a hemorrhagic CRVO with ischemic areas on fluorescein angiography and OCT showed cystoid macular edema. The patient responded well to three days of acetylsalicylic acid 100 mg daily. Elsewhere, Endo et al. reported a similar case of a 52-year-old male developing sudden blurred vision in the left eye 14 days after his first dose of the BNT162b2 vaccine [109]. His visual acuity at presentation was 20/20 OS. On examination, he had dot hemorrhages in the upper quadrants, dilated tortuous veins in four quadrants, and exudates. Fluorescein angiogram was consistent with non-ischemic CRVO. In this case, the patient demonstrated improvement with intravitreal bevacizumab and PO apixaban.
Tanaka et al. also reported on a pair of cases of unilateral branch retinal vein occlusion (BRVO) exacerbation in a 71-year-old woman (OS) and 72-year-old man (OD), both after the BNT162b2 vaccine [110]. Both patients presented with visual disturbance. Ultra-wide-field pseudo-color and OCT imaging demonstrated recurrence of previously resolved BRVO and macular edema. In the former case, the patient was treated with one-time intravitreal aflibercept, and in the latter, the patient received two doses of intravitreal ranibizumab. Both patients demonstrated resolution of symptoms and macular edema.
One report of hemi-retinal vein occlusion (HRVO) has been made following COVID-19 vaccination. Goyal et al. reported on a 28-year-old man who developed visual disturbances OD following his second dose of the Gam-COVID-Vac/Sputnik V vaccine [111]. Examination and imaging revealed a superior HRVO with severe cystoid macular edema. He demonstrated significant resolution of macular edema within one week on a PO prednisolone taper and apixaban twice daily.
9.2. Mechanisms
For a discussion of possible mechanisms underlying hypercoagulable states following vaccination, see Section 5.3.
10. Neuro-Ophthalmology
On our review, 4 reports (5 patients, 8 eyes) have discussed neuro-ophthalmological manifestations following COVID-19 vaccination. All 5 patients were female. The mean age at the time of presentation was 48.0 ± 21.5 years, and the average time from vaccination to development of ophthalmic symptoms was 8.6 ± 8.3 days. Three patients (60.0%) presented with bilateral involvement. For the 8 affected eyes which had presenting visual acuities, the mean visual acuity was logMAR 0.732 ± 0.700 at presentation (20/108 in Snellen notation). For the 4 eyes which had both presenting and final visual acuities reported, the mean visual acuities were 0.490 ± 0.412 and 0.024 ± 0.042, respectively (20/61 and 20/21 in Snellen notation; p = 0.166).
10.1. Optic Neuritis
The majority of the reports that we reviewed dealt with cases on the axis of optic neuritis. Elnahry et al. reported on a pair of cases [112]. A 69-year-old woman presented with blurry vision in both eyes with examination revealing optic nerve head edema bilaterally. OCT showed swelling of the retinal nerve fiber layer in both eyes with intraretinal and subretinal fluid in the right macula. The patient was diagnosed with post-vaccination central nervous system (CNS) inflammatory syndrome leading to neuroretinitis and papillitis. They also reported on a 32-year-old female who similarly presented with left optic neuritis. Both cases demonstrated significant improvement in symptoms and examination with use of IV methylprednisolone.
Pawar et al. reported on a 28-year-old female who developed sudden vision loss OS three weeks after receiving an unspecified COVID-19 vaccination [113]. Examination and imaging were consistent with left optic neuritis. As in the previous cases, the patient developed resolution of symptoms after IV methylprednisolone followed by PO steroids.
Leber et al. reported on a 32-year-old woman who developed rapidly progressive worsening vision and pain with extraocular movements OS [114]. Presenting visual acuity was 20/20 OD and 20/200 OS. Examination revealed and RAPD OS as well as disc swelling OD and OS. MRI revealed bilateral optic neuritis and labs also revealed a thyroid-stimulating hormone (TSH) level of 13.2 mUI/L (reference 0.45–4.5 mUI/L). The patient demonstrated significant improvement in symptoms and examination following five days of IV methylprednisolone 1 g.
10.2. Other Reports
Maleki et al. reported on a neuro-ophthalmologic case as well. A 79-year-old woman presented with bilateral sudden loss of vision 2 days after receiving the BNT162b2 vaccine [53]. Her examination was significant for an APD OD with generalized disc pallor OD and inferior pallor OS (Figure 5). A diagnosis of arteritic anterior ischemic optic neuropathy (AAION) was made.
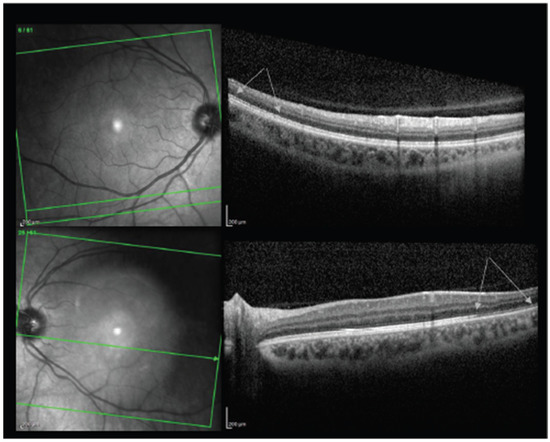
Figure 5.
The upper and lower pictures are macular optical coherence tomography of the right and left eye, respectively. Arrows show the areas of disruption and segmentation of the ellipsoid zone in the right eye and thinning of (absent in some areas) ellipsoid zone in the left eye. Adapted from Maleki A, Look-Why S, Manhapra A, Foster CS. COVID-19 Recombinant mRNA Vaccines and Serious Ocular Inflammatory Side Effects: Real or Coincidence? J. Ophthalmic. Vis. Res. 2021, 16, 490–501; Published 29 July 2021. https://doi.org/10.18502/jovr.v16i3.9443 [53]. Figure 4, Copyright (2021) with permission from KnE Publishing, open access article under the terms of the Creative Commons Attribution License.
10.3. Mechanisms
We have previously discussed the mechanisms underlying optic neuropathy in the setting of vaccination. While the phenomenon is poorly studied, it has been previously posited that molecular mimicry between myelin basic protein and viral particles, epitope spreading, bystander activation, and superantigen activation all may play a role in the development of autoimmune optic neuritis following vaccination [14,115,116,117,118,119].
11. Ocular Motility Disorders
Multiple reports of gaze palsies have been made. On our review, 7 reports (9 patients, 10 eyes) discussed gaze palsies. One case was bilateral. Of these cases, six (66.67%) were male and three (33.3%) were female. The mean age at the time of presentation was 45.3 ± 18.7 years, and the mean time between vaccination and development of ophthalmic symptoms was 8.8 ± 9.4 days. Visual acuities were discussed sparingly.
11.1. Ocular Gaze Palsies
Pawar et al. reported on a series of three cases of gaze palsies [113]. They reported on a 24-year-old woman who developed diplopia 21 days after unspecified COVID-19 vaccination. On examination, she demonstrated restricted elevation of both eyes. MRI and neurological examination were otherwise normal. The patient was diagnosed with bilateral vertical gaze palsy. The patient underwent systemic steroid therapy and demonstrated resolution after 10 days.
Pawar et al. also reported on a case of acute abducens (6th cranial) nerve palsy in the left eye of a 44-year-old male who developed his symptoms 28 days after unspecified vaccination against COVID-19. The patient had normal examination and imaging findings otherwise. The patient was treated with Botox injection into the medial rectus OS and thereafter had only minimal residual esotropia. Finally, they reported on a patient who developed acute onset esotropia OS 6 days after receiving vaccination against COVID-19. The patient previously had recurrent abducens nerve palsy following a chickenpox infection. The authors did not report on treatment. Elsewhere, Reyes-Capo et al. also reported a similar case of abducens nerve palsy in a 59-year-old woman who presented with new esotropia and abduction deficits OD after her first dose of the BNT162b2 vaccine [120]. Examination remained unchanged on follow-up. Kawtharani et al. also reported on a case of abducens nerve palsy OS after the AZD1222 vaccine which resolved with vitamin B12 supplementation and eyeglasses modification, but the patient also went on to develop transverse myelitis and quadriplegia in the ensuing weeks [121].
In another report, Pappaterra et al. reported on an 81-year-old male who developed acute diplopia one day after receiving the first dose of the Moderna COVID-19 vaccine [122]. Examination revealed limited adduction and infraduction OS only with normal motility OD. Further examination revealed an exotropia of 3 prism diopters (PD) in the primary position, decreasing to an exotropia of 2 PD on right gaze and increasing to an exotropia of 10 PD on left gaze, combined with a left hypertropia of 5 PD. Ultimately, the patient was diagnosed with a partial left oculomotor (3rd cranial) nerve palsy. At an 11 day follow up, the patient had full extraocular motility in both eyes with minimal residual exodeviation in the primary position with observation only.
Manea et al. reported on a 29-year-old man who developed multiple cranial neuropathies six days after receiving his first dose of the BNT162b2 vaccine [123]. In particular, he developed incomplete oculomotor (3rd cranial), abducens (6th cranial), and facial (7th cranial) nerve palsies.
Eleiwa et al. reported on a 46-year-old man who developed torsional, binocular diplopia three days after receiving the second dose of the AZD1222 vaccine [14]. Examination was consistent with a diagnosis of right trochlear (4th cranial) nerve palsy.
11.2. Ocular Gaze Palsies
Vaccination-induced cranial nerve palsies have previously been reported following the influenza, hepatitis B, smallpox, and MMR vaccines [124,125,126,127,128,129,130]. While the exact mechanism has not been elucidated, vaccine-induced cranial nerve palsies are believed to be due to immune-mediated damage resulting in demyelination or vascular compromise resulting in reduced blood flow [130,131]. Given the aforementioned links between vaccination and vascular compromise as well as autoimmune phenomena, it is likely that these underlie the development of ocular motility disorders following COVID-19 vaccination.
12. Other Reports
Only one report of scleritis was found on our review. Pichi et al. reported on a patient with unspecified age, gender, and vaccine who presented seven days after vaccination with bilateral eye redness and pain [90]. The patient’s ocular exam was significant for scleral hyperemia and positive phenylephrine test results. No AC cells or flare was present. A diagnosis of scleritis was made. The patient was thereafter successfully treated over one week with a topical steroid taper which resulted in complete resolution.
Jumroendararasame et al. reported on a 42-year-old man who developed blurred vision ten minutes after receiving the Corona Vac [132]. The patient, who was himself an ophthalmologist, described immediate blurred vision centrally which was followed thereafter by obscuration of the visual field OS. Examination and OCT imaging were unrevealing. The patient experienced resolution of his symptoms approximately two hours after the initial event. The authors proposed that acute vasospasm in the vasculature of the postchiasmatic visual pathway was the underlying cause of the event.
Santovito and Pinna previously reported on a male patient who developed sudden darkening of his visual field after receiving the BNT162b2 vaccine but were unable to comment on an etiology [133]. We have previously discussed this case elsewhere, suggesting that it may have been an optic neuropathy [14].
13. Conclusions
Since the introduction of COVID-19 vaccinations, numerous reports have commented on adverse ocular events following vaccination. In this review, we sought to present these in a systematic fashion and offer insights into the mechanisms and clinical considerations surrounding these phenomena. Given the relatively low number of reports per specific phenomenon, more reports and clinical data are needed in order to establish better guidelines and insights. Leading clinical bodies in ophthalmology have not provided official guidelines on the use of COVID-19 boosters in the setting of active ophthalmic complications, yet it is our belief that caution and delay may be warranted in lower-risk groups with active complications. Nevertheless, it is the opinion of the authors that vaccination is a vital public health tool in the management of the COVID-19 pandemic.
Author Contributions
Conceptualization, A.A.H. and A.M.E.; methodology, A.A.H. and A.M.E.; formal analysis, A.A.H. and A.M.E.; investigation, O.S., M.M.A. and A.S.A.O.; resources, O.S., M.M.A. and A.S.A.O.; data curation, O.S. and A.A.H.; writing—original draft preparation, A.A.H. and M.M.A.; writing—review and editing, A.A.H. and A.M.E. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Please refer to suggested Data Availability Statements in section “MDPI Research Data Policies” at https://www.mdpi.com/ethics (accessed on 30 December 2021).
Conflicts of Interest
The authors declare no conflict of interest.
References
- Saied, S.M.; Saied, E.M.; Kabbash, I.A.; Abdo, S.A.E. Vaccine hesitancy: Beliefs and barriers associated with COVID-19 vaccination among Egyptian medical students. J. Med. Virol. 2021, 93, 4280–4291. [Google Scholar] [CrossRef]
- Kadali, R.A.K.; Janagama, R.; Peruru, S.R.; Racherla, S.; Tirumala, R.; Madathala, R.R.; Gajula, V. Adverse effects of COVID-19 messenger RNA vaccines among pregnant women: A cross-sectional study on healthcare workers with detailed self-reported symptoms. Am. J. Obs. Gynecol. 2021, 225, 458–460. [Google Scholar] [CrossRef]
- Meo, S.A.; Fahad Al-Jassir, F.; Al-Qahtani, S.; Albarrak, R.; Usmani, A.M.; Klonoff, D.C. Effect of Pfizer/BioNTech and Oxford/AstraZeneca vaccines against COVID-19 morbidity and mortality in real-world settings at countrywide vaccination campaign in Saudi Arabia. Eur. Rev. Med. Pharm. Sci. 2021, 25, 7185–7191. [Google Scholar] [CrossRef]
- Meo, S.A.; Bukhari, I.A.; Akram, J.; Meo, A.S.; Klonoff, D.C. COVID-19 vaccines: Comparison of biological, pharmacological characteristics and adverse effects of Pfizer/BioNTech and Moderna Vaccines. Eur. Rev. Med. Pharm. Sci. 2021, 25, 1663–1669. [Google Scholar] [CrossRef]
- Singh, S.; Garcia, G.; Shah, R.; Kramerov, A.A.; Wright, R.E., 3rd; Spektor, T.M.; Ljubimov, A.V.; Arumugaswami, V.; Kumar, A. SARS-CoV-2 and its beta variant of concern infect human conjunctival epithelial cells and induce differential antiviral innate immune response. Ocul. Surf. 2021, 23, 184–194. [Google Scholar] [CrossRef] [PubMed]
- Barros, A.; Queiruga-Pineiro, J.; Lozano-Sanroma, J.; Alcalde, I.; Gallar, J.; Fernandez-Vega Cueto, L.; Alfonso, J.F.; Quiros, L.M.; Merayo-Lloves, J. Small fiber neuropathy in the cornea of Covid-19 patients associated with the generation of ocular surface disease. Ocul. Surf. 2021, 23, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Li, Y.; Musch, D.C.; Wei, N.; Qi, X.; Ding, G.; Li, X.; Li, J.; Song, L.; Zhang, Y.; et al. Progression of Myopia in School-Aged Children After COVID-19 Home Confinement. JAMA Ophthalmol. 2021, 139, 293–300. [Google Scholar] [CrossRef] [PubMed]
- Rokohl, A.C.; Grajewski, R.S.; Matos, P.A.W.; Kopecky, A.; Heindl, L.M.; Cursiefen, C. Ocular Involvement in COVID-19: Conjunctivitis and More. Klin. Monbl. Augenheilkd. 2021, 238, 555–560. [Google Scholar] [CrossRef] [PubMed]
- Loffredo, L.; Pacella, F.; Pacella, E.; Tiscione, G.; Oliva, A.; Violi, F. Conjunctivitis and COVID-19: A meta-analysis. J. Med. Virol. 2020, 92, 1413–1414. [Google Scholar] [CrossRef] [PubMed]
- Ahuja, A.S.; Farford, B.A.; Forouhi, M.; Abdin, R.; Salinas, M. The Ocular Manifestations of COVID-19 through Conjunctivitis. Cureus 2020, 12, e12218. [Google Scholar] [CrossRef]
- Elhusseiny, A.M.; Eleiwa, T.K.; Yacoub, M.S.; George, J.; ElSheikh, R.H.; Haseeb, A.; Kwan, J.; Elsaadani, I.A.; Abo Shanab, S.M.; Solyman, O.; et al. Relationship between screen time and dry eye symptoms in pediatric population during the COVID-19 pandemic. Ocul. Surf. 2021, 22, 117–119. [Google Scholar] [CrossRef] [PubMed]
- Eleiwa, T.K.; Elmaghrabi, A.; Helal, H.G.; Abdelrahman, S.N.; ElSheikh, R.H.; Elhusseiny, A.M. Phlyctenular Keratoconjunctivitis in a Patient with COVID-19 Infection. Cornea 2021, 40, 1502–1504. [Google Scholar] [CrossRef] [PubMed]
- Eleiwa, T.; Abdelrahman, S.N.; ElSheikh, R.H.; Elhusseiny, A.M. Orbital inflammatory disease associated with COVID-19 infection. J. AAPOS 2021, 25, 232–234. [Google Scholar] [CrossRef] [PubMed]
- Eleiwa, T.K.; Gaier, E.D.; Haseeb, A.; ElSheikh, R.H.; Sallam, A.B.; Elhusseiny, A.M. Adverse Ocular Events following COVID-19 Vaccination. Inflamm. Res. 2021, 70, 1005–1009. [Google Scholar] [CrossRef]
- Ng, X.L.; Betzler, B.K.; Ng, S.; Chee, S.P.; Rajamani, L.; Singhal, A.; Rousselot, A.; Pavesio, C.E.; Gupta, V.; de Smet, M.D.; et al. The Eye of the Storm: COVID-19 Vaccination and the Eye. Ophthalmol. Ther. 2021, 11, 81–100. [Google Scholar] [CrossRef] [PubMed]
- Sen, M.; Honavar, S.G. After the Storm: Ophthalmic Manifestations of COVID-19 Vaccines. Indian J. Ophthalmol. 2021, 69, 3398–3420. [Google Scholar] [CrossRef] [PubMed]
- Austria, Q.M.; Lelli, G.J.; Segal, K.L.; Godfrey, K.J. Transient Eyelid Edema following COVID-19 Vaccination. Ophthalmic. Plast Reconstr. Surg. 2021, 37, 501–502. [Google Scholar] [CrossRef]
- Mazzatenta, C.; Piccolo, V.; Pace, G.; Romano, I.; Argenziano, G.; Bassi, A. Purpuric lesions on the eyelids developed after BNT162b2 mRNA COVID-19 vaccine: Another piece of SARS-CoV-2 skin puzzle? J. Eur. Acad. Derm. Venereol. 2021, 35, e543–e545. [Google Scholar] [CrossRef]
- Bayas, A.; Menacher, M.; Christ, M.; Behrens, L.; Rank, A.; Naumann, M. Bilateral superior ophthalmic vein thrombosis, ischaemic stroke, and immune thrombocytopenia after ChAdOx1 nCoV-19 vaccination. Lancet 2021, 397, e11. [Google Scholar] [CrossRef]
- Panovska-Stavridis, I.; Pivkova-Veljanovska, A.; Trajkova, S.; Lazarevska, M.; Grozdanova, A.; Filipche, V. A Rare Case of Superior Ophthalmic Vein Thrombosis and Thrombocytopenia following ChAdOx1 nCoV-19 Vaccine against SARS-CoV-2. Mediterr. J. Hematol. Infect Dis. 2021, 13, e2021048. [Google Scholar] [CrossRef] [PubMed]
- Chuang, T.Y.; Burda, K.; Teklemariam, E.; Athar, K. Tolosa-Hunt Syndrome Presenting after COVID-19 Vaccination. Cureus 2021, 13, e16791. [Google Scholar] [CrossRef] [PubMed]
- Dutta, P.; Anand, K. Tolosa-Hunt Syndrome: A Review of Diagnostic Criteria and Unresolved Issues. J. Curr. Ophthalmol. 2021, 33, 104–111. [Google Scholar] [CrossRef] [PubMed]
- Hyer, R.; McGuire, D.K.; Xing, B.; Jackson, S.; Janssen, R. Safety of a two-dose investigational hepatitis B vaccine, HBsAg-1018, using a toll-like receptor 9 agonist adjuvant in adults. Vaccine 2018, 36, 2604–2611. [Google Scholar] [CrossRef] [PubMed]
- Schultz, N.H.; Sorvoll, I.H.; Michelsen, A.E.; Munthe, L.A.; Lund-Johansen, F.; Ahlen, M.T.; Wiedmann, M.; Aamodt, A.H.; Skattor, T.H.; Tjonnfjord, G.E.; et al. Thrombosis and Thrombocytopenia after ChAdOx1 nCoV-19 Vaccination. N. Engl. J. Med. 2021, 384, 2124–2130. [Google Scholar] [CrossRef]
- Owatanapanich, S.; Wanlapakorn, N.; Tangsiri, R.; Poovorawan, Y. Measles-mumps-rubella vaccination induced thrombocytopenia: A case report and review of the literature. Southeast Asian J. Trop. Med. Public Health 2014, 45, 1053–1057. [Google Scholar]
- Kashyape, S.S.; Kashyape, P.S. Thrombocytopenia following MMR vaccination. Indian Pediatr. 2005, 42, 80–82. [Google Scholar]
- Forrest, J.M.; Honeyman, M.C.; Lovric, V.A. Rubella vaccination and thrombocytopenia. Aust. N. Z. J. Med. 1974, 4, 352–355. [Google Scholar] [CrossRef]
- Bartos, H.R. Thrombocytopenia associated with rubella vaccination. N. Y. State J. Med. 1972, 72, 499. [Google Scholar]
- Yamamoto, Y.; Ohara, Y.; Iwai, A.; Hara, R.; Matsuki, T.; Fukushima, K.; Oshitani, Y.; Kagawa, H.; Tsujino, K.; Yoshimura, K.; et al. Influenza Vaccination-associated Acute Thrombocytopenia and Diffuse Alveolar Hemorrhage. Intern. Med. 2020, 59, 1633–1637. [Google Scholar] [CrossRef]
- Moulis, G.; Sailler, L.; Sommet, A.; Lapeyre-Mestre, M.; Adoue, D. Prevalence of pneumococcal vaccination in adult immune thrombocytopenia patients exposed to rituximab or to splenectomy. Eur. J. Haematol. 2013, 90, 438–439. [Google Scholar] [CrossRef]
- Meindersma, T.E. Thrombocytopenia after vaccination against smallpox. Ned. Milit. Geneeskd. Tijdschr. 1961, 14, 199–205. [Google Scholar]
- McCrae, K.R. Thrombotic thrombocytopenia due to SARS-CoV-2 vaccination. Clevel. Clin. J. Med. 2021. [Google Scholar] [CrossRef]
- Lee, E.J.; Cines, D.B.; Gernsheimer, T.; Kessler, C.; Michel, M.; Tarantino, M.D.; Semple, J.W.; Arnold, D.M.; Godeau, B.; Lambert, M.P.; et al. Thrombocytopenia following Pfizer and Moderna SARS-CoV-2 vaccination. Am. J. Hematol. 2021, 96, 534–537. [Google Scholar] [CrossRef]
- Lai, K.Y.; Au, S.Y.; Fong, K.M. Thrombotic Thrombocytopenia after ChAdOx1 nCoV-19 Vaccination. N. Engl. J. Med. 2021, 385, e11. [Google Scholar] [CrossRef]
- Greinacher, A.; Thiele, T.; Warkentin, T.E.; Weisser, K.; Kyrle, P.A.; Eichinger, S. Thrombotic Thrombocytopenia after ChAdOx1 nCov-19 Vaccination. N. Engl. J. Med. 2021, 384, 2092–2101. [Google Scholar] [CrossRef]
- Bitzan, M.; Zieg, J. Influenza-associated thrombotic microangiopathies. Pediatr. Nephrol. 2018, 33, 2009–2025. [Google Scholar] [CrossRef]
- ElSheikh, R.H.; Haseeb, A.; Eleiwa, T.K.; Elhusseiny, A.M. Acute Uveitis following COVID-19 Vaccination. Ocul. Immunol. Inflamm. 2021, 29, 1207–1209. [Google Scholar] [CrossRef]
- Jain, A.; Kalamkar, C. COVID-19 vaccine-associated reactivation of uveitis. Indian J. Ophthalmol. 2021, 69, 2899–2900. [Google Scholar] [CrossRef]
- Mudie, L.I.; Zick, J.D.; Dacey, M.S.; Palestine, A.G. Panuveitis following Vaccination for COVID-19. Ocul. Immunol. Inflamm. 2021, 29, 1–2. [Google Scholar] [CrossRef]
- Renisi, G.; Lombardi, A.; Stanzione, M.; Invernizzi, A.; Bandera, A.; Gori, A. Anterior uveitis onset after bnt162b2 vaccination: Is this just a coincidence? Int. J. Infect. Dis. 2021, 110, 95–97. [Google Scholar] [CrossRef]
- Ishay, Y.; Kenig, A.; Tsemach-Toren, T.; Amer, R.; Rubin, L.; Hershkovitz, Y.; Kharouf, F. Autoimmune phenomena following SARS-CoV-2 vaccination. Int. Immunopharmacol. 2021, 99, 107970. [Google Scholar] [CrossRef]
- Herbort, C.P., Jr.; Papasavvas, I. Effect of SARS-CoV-2 mRNA vaccination on ocular herpes simplex and varicella-zoster virus reactivation: Should preventive antiviral treatment be given in known herpes patients. J. Ophthalmic. Inflamm. Infect. 2021, 11, 33. [Google Scholar] [CrossRef]
- Rabinovitch, T.; Ben-Arie-Weintrob, Y.; Hareuveni-Blum, T.; Shaer, B.; Vishnevskia-Dai, V.; Shulman, S.; Newman, H.; Biadsy, M.; Masarwa, D.; Fischer, N.; et al. Uveitis following the BNT162b2 mRNA vaccination against SARS-CoV-2 infection: A possible association. Retina 2021, 41, 2462–2471. [Google Scholar] [CrossRef]
- Goyal, M.; Murthy, S.I.; Annum, S. Bilateral Multifocal Choroiditis following COVID-19 Vaccination. Ocul. Immunol. Inflamm. 2021, 29, 1–5. [Google Scholar] [CrossRef]
- Pan, L.; Zhang, Y.; Cui, Y.; Wu, X. Bilateral uveitis after inoculation with COVID-19 vaccine: A case report. Int. J. Infect. Dis. 2021, 113, 116–118. [Google Scholar] [CrossRef]
- Read, R.W.; Rao, N.A.; Cunningham, E.T. Vogt-Koyanagi-Harada disease. Curr. Opin. Ophthalmol. 2000, 11, 437–442. [Google Scholar] [CrossRef]
- Read, R.W.; Holland, G.N.; Rao, N.A.; Tabbara, K.F.; Ohno, S.; Arellanes-Garcia, L.; Pivetti-Pezzi, P.; Tessler, H.H.; Usui, M. Revised diagnostic criteria for Vogt-Koyanagi-Harada disease: Report of an international committee on nomenclature. Am. J. Ophthalmol. 2001, 131, 647–652. [Google Scholar] [CrossRef]
- Rao, N.A.; Gupta, A.; Dustin, L.; Chee, S.P.; Okada, A.A.; Khairallah, M.; Bodaghi, B.; Lehoang, P.; Accorinti, M.; Mochizuki, M.; et al. Frequency of distinguishing clinical features in Vogt-Koyanagi-Harada disease. Ophthalmology 2010, 117, 591–599. [Google Scholar] [CrossRef]
- Harada, Y.; Bhat, P.; Munk, M.R.; Goldstein, D.A. Changes in Scleral Architecture in Chronic Vogt-Koyanagi-Harada Disease. Ocul. Immunol. Inflamm. 2017, 25, 85–92. [Google Scholar] [CrossRef]
- Papasavvas, I.; Herbort, C.P., Jr. Reactivation of Vogt-Koyanagi-Harada disease under control for more than 6 years, following anti-SARS-CoV-2 vaccination. J. Ophthalmic. Inflamm. Infect. 2021, 11, 21. [Google Scholar] [CrossRef]
- Saraceno, J.J.F.; Souza, G.M.; Dos Santos Finamor, L.P.; Nascimento, H.M.; Belfort, R., Jr. Vogt-Koyanagi-Harada Syndrome following COVID-19 and ChAdOx1 nCoV-19 (AZD1222) vaccine. Int. J. Retin. Vitr. 2021, 7, 49. [Google Scholar] [CrossRef]
- Mishra, S.B.; Mahendradas, P.; Kawali, A.; Sanjay, S.; Shetty, R. Reactivation of varicella zoster infection presenting as acute retinal necrosis post COVID 19 vaccination in an Asian Indian male. Eur. J. Ophthalmol. 2021. [Google Scholar] [CrossRef] [PubMed]
- Maleki, A.; Look-Why, S.; Manhapra, A.; Foster, C.S. COVID-19 Recombinant mRNA Vaccines and Serious Ocular Inflammatory Side Effects: Real or Coincidence? J. Ophthalmic. Vis. Res. 2021, 16, 490–501. [Google Scholar] [CrossRef]
- Holt, H.D.; Hinkle, D.M.; Falk, N.S.; Fraunfelder, F.T.; Fraunfelder, F.W. Human papilloma virus vaccine associated uveitis. Curr. Drug Saf. 2014, 9, 65–68. [Google Scholar] [CrossRef] [PubMed]
- Heydari-Kamjani, M.; Vante, I.; Uppal, P.; Demory Beckler, M.; Kesselman, M.M. Uveitis Sarcoidosis Presumably Initiated after Administration of Shingrix Vaccine. Cureus 2019, 11, e4920. [Google Scholar] [CrossRef] [PubMed]
- Fraunfelder, F.W.; Suhler, E.B.; Fraunfelder, F.T. Hepatitis B vaccine and uveitis: An emerging hypothesis suggested by review of 32 case reports. Cutan. Ocul. Toxicol. 2010, 29, 26–29. [Google Scholar] [CrossRef] [PubMed]
- Esmaeli-Gutstein, B.; Winkelman, J.Z. Uveitis associated with varicella virus vaccine. Am. J. Ophthalmol. 1999, 127, 733–734. [Google Scholar] [CrossRef]
- Benage, M.; Fraunfelder, F.W. Vaccine-Associated Uveitis. Mo. Med. 2016, 113, 48–52. [Google Scholar]
- Aguirre, G.; Carmichael, L.; Bistner, S. Corneal endothelium in viral induced anterior uveitis. Ultrastructural changes following canine adenovirus type 1 infection. Arch. Ophthalmol. 1975, 93, 219–224. [Google Scholar] [CrossRef]
- Sawant, O.B.; Singh, S.; Wright, R.E., 3rd; Jones, K.M.; Titus, M.S.; Dennis, E.; Hicks, E.; Majmudar, P.A.; Kumar, A.; Mian, S.I. Prevalence of SARS-CoV-2 in human post-mortem ocular tissues. Ocul. Surf. 2021, 19, 322–329. [Google Scholar] [CrossRef]
- Koo, E.H.; Eghrari, A.O.; Dzhaber, D.; Shah, A.; Fout, E.; Dubovy, S.; Maestre-Mesa, J.; Miller, D. Presence of SARS-CoV-2 Viral RNA in Aqueous Humor of Asymptomatic Individuals. Am. J. Ophthalmol. 2021, 230, 151–155. [Google Scholar] [CrossRef] [PubMed]
- Nance, K.D.; Meier, J.L. Modifications in an Emergency: The Role of N1-Methylpseudouridine in COVID-19 Vaccines. ACS Cent. Sci. 2021, 7, 748–756. [Google Scholar] [CrossRef] [PubMed]
- Phylactou, M.; Li, J.O.; Larkin, D.F.P. Characteristics of endothelial corneal transplant rejection following immunisation with SARS-CoV-2 messenger RNA vaccine. Br. J. Ophthalmol. 2021, 105, 893–896. [Google Scholar] [CrossRef] [PubMed]
- Crnej, A.; Khoueir, Z.; Cherfan, G.; Saad, A. Acute corneal endothelial graft rejection following COVID-19 vaccination. J. Fr. Ophtalmol. 2021. [Google Scholar] [CrossRef] [PubMed]
- Wasser, L.M.; Roditi, E.; Zadok, D.; Berkowitz, L.; Weill, Y. Keratoplasty Rejection After the BNT162b2 messenger RNA Vaccine. Cornea 2021, 40, 1070–1072. [Google Scholar] [CrossRef]
- Rallis, K.I.; Ting, D.S.J.; Said, D.G.; Dua, H.S. Corneal graft rejection following COVID-19 vaccine. Eye 2021. [Google Scholar] [CrossRef]
- Abousy, M.; Bohm, K.; Prescott, C.; Bonsack, J.M.; Rowhani-Farid, A.; Eghrari, A.O. Bilateral EK Rejection After COVID-19 Vaccine. Eye Contact Lens 2021, 47, 625–628. [Google Scholar] [CrossRef]
- Nioi, M.; D’Aloja, E.; Fossarello, M.; Napoli, P.E. Dual Corneal-Graft Rejection after mRNA Vaccine (BNT162b2) for COVID-19 during the First Six Months of Follow-Up: Case Report, State of the Art and Ethical Concerns. Vaccines 2021, 9, 1274. [Google Scholar] [CrossRef] [PubMed]
- Parmar, D.P.; Garde, P.V.; Shah, S.M.; Bhole, P.K. Acute graft rejection in a high-risk corneal transplant following COVID-19 vaccination: A case report. Indian J. Ophthalmol. 2021, 69, 3757–3758. [Google Scholar] [CrossRef]
- Ravichandran, S.; Natarajan, R. Corneal graft rejection after COVID-19 vaccination. Indian J. Ophthalmol. 2021, 69, 1953–1954. [Google Scholar] [CrossRef] [PubMed]
- Thiem, U.; Borchhardt, K. Vitamin D in solid organ transplantation with special emphasis on kidney transplantation. Vitam. Horm. 2011, 86, 429–468. [Google Scholar] [CrossRef] [PubMed]
- Stein, E.M.; Shane, E. Vitamin D in organ transplantation. Osteoporos. Int. 2011, 22, 2107–2118. [Google Scholar] [CrossRef]
- Courbebaisse, M.; Souberbielle, J.C.; Thervet, E. Potential nonclassical effects of vitamin D in transplant recipients. Transplantation 2010, 89, 131–137. [Google Scholar] [CrossRef]
- DeLuca, H.F.; Zierold, C. Mechanisms and functions of vitamin D. Nutr. Rev. 1998, 56, S4–S10. [Google Scholar] [CrossRef]
- Lemire, J. 1,25-Dihydroxyvitamin D3—A hormone with immunomodulatory properties. Z. Rheumatol. 2000, 59 (Suppl. 1), 24–27. [Google Scholar] [CrossRef]
- Khan, T.A.; Sidhu, N.; Khan, L.; Sen, S.; Hussain, N.; Tandon, R.; Gupta, N. Bilateral Immune-Mediated Keratolysis after Immunization with SARS-CoV-2 Recombinant Viral Vector Vaccine. Cornea 2021, 40, 1629–1632. [Google Scholar] [CrossRef]
- Steinemann, T.L.; Koffler, B.H.; Jennings, C.D. Corneal allograft rejection following immunization. Am. J. Ophthalmol. 1988, 106, 575–578. [Google Scholar] [CrossRef]
- Vignapiano, R.; Vicchio, L.; Favuzza, E.; Cennamo, M.; Mencucci, R. Corneal Graft Rejection after Yellow Fever Vaccine: A Case Report. Ocul. Immunol. Inflamm. 2021, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Wertheim, M.S.; Keel, M.; Cook, S.D.; Tole, D.M. Corneal transplant rejection following influenza vaccination. Br. J. Ophthalmol. 2006, 90, 925. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Solomon, A.; Frucht-Pery, J. Bilateral simultaneous corneal graft rejection after influenza vaccination. Am. J. Ophthalmol. 1996, 121, 708–709. [Google Scholar] [CrossRef]
- Fabre, J.W.; Milton, A.D.; Spencer, S.; Settaf, A.; Houssin, D. Regulation of alloantigen expression in different tissues. Transpl. Proc. 1987, 19, 45–49. [Google Scholar]
- Steger, B.; Curnow, E.; Cheeseman, R.; Romano, V.; Kaye, A.; Jones, M.; Kaye, S.; National Health Service, B.; Transplant Ocular Tissue Advisory, G.; Contributing, O. Sequential Bilateral Corneal Transplantation and Graft Survival. Am. J. Ophthalmol. 2016, 170, 50–57. [Google Scholar] [CrossRef] [PubMed]
- Fawzi, A.A.; Pappuru, R.R.; Sarraf, D.; Le, P.P.; McCannel, C.A.; Sobrin, L.; Goldstein, D.A.; Honowitz, S.; Walsh, A.C.; Sadda, S.R.; et al. Acute macular neuroretinopathy: Long-term insights revealed by multimodal imaging. Retina 2012, 32, 1500–1513. [Google Scholar] [CrossRef]
- Bos, P.J.; Deutman, A.F. Acute macular neuroretinopathy. Am. J. Ophthalmol. 1975, 80, 573–584. [Google Scholar] [CrossRef]
- Bhavsar, K.V.; Lin, S.; Rahimy, E.; Joseph, A.; Freund, K.B.; Sarraf, D.; Cunningham, E.T., Jr. Acute macular neuroretinopathy: A comprehensive review of the literature. Surv. Ophthalmol. 2016, 61, 538–565. [Google Scholar] [CrossRef]
- Monson, B.K.; Greenberg, P.B.; Greenberg, E.; Fujimoto, J.G.; Srinivasan, V.J.; Duker, J.S. High-speed, ultra-high-resolution optical coherence tomography of acute macular neuroretinopathy. Br. J. Ophthalmol. 2007, 91, 119–120. [Google Scholar] [CrossRef][Green Version]
- Bohler, A.D.; Strom, M.E.; Sandvig, K.U.; Moe, M.C.; Jorstad, O.K. Acute macular neuroretinopathy following COVID-19 vaccination. Eye 2021, 1–2. [Google Scholar] [CrossRef]
- Mambretti, M.; Huemer, J.; Torregrossa, G.; Ullrich, M.; Findl, O.; Casalino, G. Acute Macular Neuroretinopathy following Coronavirus Disease 2019 Vaccination. Ocul. Immunol. Inflamm. 2021, 29, 730–733. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Hodge, C. Comment on: Acute macular neuroretinopathy following COVID-19 vaccination. Eye 2021. [Google Scholar] [CrossRef] [PubMed]
- Pichi, F.; Aljneibi, S.; Neri, P.; Hay, S.; Dackiw, C.; Ghazi, N.G. Association of Ocular Adverse Events with Inactivated COVID-19 Vaccination in Patients in Abu Dhabi. JAMA Ophthalmol. 2021, 139, 1131–1135. [Google Scholar] [CrossRef] [PubMed]
- Book, B.A.J.; Schmidt, B.; Foerster, A.M.H. Bilateral Acute Macular Neuroretinopathy after Vaccination against SARS-CoV-2. JAMA Ophthalmol. 2021, 139, e212471. [Google Scholar] [CrossRef]
- Druke, D.; Pleyer, U.; Hoerauf, H.; Feltgen, N.; Bemme, S. Acute macular neuroretinopathy (AMN) following COVID-19 vaccination. Am. J. Ophthalmol. Case Rep. 2021, 24, 101207. [Google Scholar] [CrossRef]
- Valenzuela, D.A.; Groth, S.; Taubenslag, K.J.; Gangaputra, S. Acute macular neuroretinopathy following Pfizer-BioNTech COVID-19 vaccination. Am. J. Ophthalmol. Case Rep. 2021, 24, 101200. [Google Scholar] [CrossRef]
- Virgo, J.; Mohamed, M. Paracentral acute middle maculopathy and acute macular neuroretinopathy following SARS-CoV-2 infection. Eye 2020, 34, 2352–2353. [Google Scholar] [CrossRef] [PubMed]
- Nemiroff, J.; Kuehlewein, L.; Rahimy, E.; Tsui, I.; Doshi, R.; Gaudric, A.; Gorin, M.B.; Sadda, S.; Sarraf, D. Assessing Deep Retinal Capillary Ischemia in Paracentral Acute Middle Maculopathy by Optical Coherence Tomography Angiography. Am. J. Ophthalmol. 2016, 162, 121–132.e121. [Google Scholar] [CrossRef] [PubMed]
- Sarraf, D.; Rahimy, E.; Fawzi, A.A.; Sohn, E.; Barbazetto, I.; Zacks, D.N.; Mittra, R.A.; Klancnik, J.M., Jr.; Mrejen, S.; Goldberg, N.R.; et al. Paracentral acute middle maculopathy: A new variant of acute macular neuroretinopathy associated with retinal capillary ischemia. JAMA Ophthalmol. 2013, 131, 1275–1287. [Google Scholar] [CrossRef]
- Rahimy, E.; Sarraf, D. Paracentral acute middle maculopathy spectral-domain optical coherence tomography feature of deep capillary ischemia. Curr. Opin. Ophthalmol. 2014, 25, 207–212. [Google Scholar] [CrossRef]
- Rahimy, E.; Kuehlewein, L.; Sadda, S.R.; Sarraf, D. Paracentral Acute Middle Maculopathy: What We Knew Then and What We Know Now. Retina 2015, 35, 1921–1930. [Google Scholar] [CrossRef]
- Vinzamuri, S.; Pradeep, T.G.; Kotian, R. Bilateral paracentral acute middle maculopathy and acute macular neuroretinopathy following COVID-19 vaccination. Indian J. Ophthalmol. 2021, 69, 2862–2864. [Google Scholar] [CrossRef]
- Fowler, N.; Mendez Martinez, N.R.; Pallares, B.V.; Maldonado, R.S. Acute-onset central serous retinopathy after immunization with COVID-19 mRNA vaccine. Am. J. Ophthalmol. Case Rep. 2021, 23, 101136. [Google Scholar] [CrossRef]
- Khochtali, S.; Krifa, H.; Zina, S.; Khairallah, M.; Jelliti, B.; Abroug, N.; Khairallah, M. Multimodal Imaging of Acute Foveolitis following COVID-19 Vaccination. Ocul. Immunol. Inflamm. 2021, 1–4. [Google Scholar] [CrossRef]
- Shah, P.; Zaveri, J.S.; Haddock, L.J. Acute Macular Neuroretinopathy following the Administration of an Influenza Vaccination. Ophthalmic. Surg. Lasers Imaging Retin. 2018, 49, e165–e168. [Google Scholar] [CrossRef]
- Liu, J.C.; Nesper, P.L.; Fawzi, A.A.; Gill, M.K. Acute macular neuroretinopathy associated with influenza vaccination with decreased flow at the deep capillary plexus on OCT angiography. Am. J. Ophthalmol. Case Rep. 2018, 10, 96–100. [Google Scholar] [CrossRef]
- Giacuzzo, C.; Eandi, C.M.; Kawasaki, A. Bilateral acute macular neuroretinopathy following COVID-19 infection. Acta Ophthalmol. 2021, 100, 611–612. [Google Scholar] [CrossRef]
- Premkumar, M.; Bhujade, H.; Karki, T.; Chaluvashetty, S.B.; Kaur, H.; Duseja, A.K.; Singh, V. New Portal Vein Thrombosis in Cirrhosis-is the thrombophilia exacerbated due to Vaccine or COVID-19? J. Clin. Exp. Hepatol. 2021. [Google Scholar] [CrossRef]
- John, N.A.; John, J.; Kamble, P.; Singhal, A.; Daulatabad, V.; Vamshidhar, I.S. COVID 19 vaccine in patients of hypercoagulable disorders: A clinical perspective. Horm. Mol. Biol. Clin. Investig. 2021. [Google Scholar] [CrossRef]
- Tomerak, S.; Khan, S.; Almasri, M.; Hussein, R.; Abdelati, A.; Aly, A.; Salameh, M.A.; Saed Aldien, A.; Naveed, H.; Elshazly, M.B.; et al. Systemic inflammation in COVID-19 patients may induce various types of venous and arterial thrombosis: A systematic review. Scand. J. Immunol. 2021, 94, e13097. [Google Scholar] [CrossRef]
- Bialasiewicz, A.A.; Farah-Diab, M.S.; Mebarki, H.T. Central retinal vein occlusion occurring immediately after 2nd dose of mRNA SARS-CoV-2 vaccine. Int. Ophthalmol. 2021, 41, 3889–3892. [Google Scholar] [CrossRef]
- Endo, B.; Bahamon, S.; Martinez-Pulgarin, D.F. Central retinal vein occlusion after mRNA SARS-CoV-2 vaccination: A case report. Indian J. Ophthalmol. 2021, 69, 2865–2866. [Google Scholar] [CrossRef]
- Tanaka, H.; Nagasato, D.; Nakakura, S.; Tanabe, H.; Nagasawa, T.; Wakuda, H.; Imada, Y.; Mitamura, Y.; Tabuchi, H. Exacerbation of branch retinal vein occlusion post SARS-CoV2 vaccination: Case reports. Medicine 2021, 100, e28236. [Google Scholar] [CrossRef]
- Goyal, M.; Murthy, S.I.; Srinivas, Y. Unilateral retinal vein occlusion in a young, healthy male following Sputnik V vaccination. Indian J. Ophthalmol. 2021, 69, 3793–3794. [Google Scholar] [CrossRef]
- Elnahry, A.G.; Asal, Z.B.; Shaikh, N.; Dennett, K.; Abd Elmohsen, M.N.; Elnahry, G.A.; Shehab, A.; Vytopil, M.; Ghaffari, L.; Athappilly, G.K.; et al. Optic neuropathy after COVID-19 vaccination: A report of two cases. Int. J. Neurosci. 2021, 1–7. [Google Scholar] [CrossRef]
- Pawar, N.; Maheshwari, D.; Ravindran, M.; Padmavathy, S. Ophthalmic complications of COVID-19 vaccination. Indian J. Ophthalmol. 2021, 69, 2900–2902. [Google Scholar] [CrossRef]
- Leber, H.M.; Sant′Ana, L.; Konichi da Silva, N.R.; Raio, M.C.; Mazzeo, T.; Endo, C.M.; Nascimento, H.; de Souza, C.E. Acute Thyroiditis and Bilateral Optic Neuritis following SARS-CoV-2 Vaccination with CoronaVac: A Case Report. Ocul. Immunol. Inflamm. 2021, 29, 1–7. [Google Scholar] [CrossRef]
- Barnaba, V. Viruses, hidden self-epitopes and autoimmunity. Immunol. Rev. 1996, 152, 47–66. [Google Scholar] [CrossRef]
- Hull, T.P.; Bates, J.H. Optic neuritis after influenza vaccination. Am. J. Ophthalmol. 1997, 124, 703–704. [Google Scholar] [CrossRef]
- McCoy, L.; Tsunoda, I.; Fujinami, R.S. Multiple sclerosis and virus induced immune responses: Autoimmunity can be primed by molecular mimicry and augmented by bystander activation. Autoimmunity 2006, 39, 9–19. [Google Scholar] [CrossRef]
- Miller, S.D.; Vanderlugt, C.L.; Begolka, W.S.; Pao, W.; Yauch, R.L.; Neville, K.L.; Katz-Levy, Y.; Carrizosa, A.; Kim, B.S. Persistent infection with Theiler’s virus leads to CNS autoimmunity via epitope spreading. Nat. Med. 1997, 3, 1133–1136. [Google Scholar] [CrossRef]
- Nahill, S.R.; Welsh, R.M. High frequency of cross-reactive cytotoxic T lymphocytes elicited during the virus-induced polyclonal cytotoxic T lymphocyte response. J. Exp. Med. 1993, 177, 317–327. [Google Scholar] [CrossRef]
- Reyes-Capo, D.P.; Stevens, S.M.; Cavuoto, K.M. Acute abducens nerve palsy following COVID-19 vaccination. J. AAPOS 2021, 25, 302–303. [Google Scholar] [CrossRef]
- Kawtharani, A.A.; Fakhry, B.; Serhan, A. Longitudinal extensive transverse myelitis with sixth nerve palsy post ChAdOx1 nCov-19 vaccine: A case report and literature review. World J. Adv. Res. Rev. 2021. [Google Scholar]
- Pappaterra, M.C.; Rivera, E.J.; Oliver, A.L. Transient Oculomotor Palsy Following the Administration of the Messenger RNA-1273 Vaccine for SARS-CoV-2 Diplopia Following the COVID-19 Vaccine. J. Neuroophthalmol. 2021. [Google Scholar] [CrossRef]
- Manea, M.M.; Dragos, D.; Enache, I.; Sirbu, A.G.; Tuta, S. Multiple cranial nerve palsies following COVID-19 vaccination-Case report. Acta Neurol. Scand. 2021, 145, 257–259. [Google Scholar] [CrossRef]
- Essrani, R.; Essrani, R.K.; Mehershahi, S.; Lohana, A.K.; Sudhakaran, A. Oculomotor Nerve Palsy after Influenza Vaccine in Inflammatory Bowel Disease. Cureus 2018, 10, e3759. [Google Scholar] [CrossRef]
- Roger, H.; Poursines, Y.; Roger, J.; Pujol, R. Guillain-Barre syndrome with paralysis of the two external oculomotor muscles after smallpox vaccination. Rev. Otoneuroophtalmol. 1953, 25, 425–427. [Google Scholar]
- Larmande, A.; Margaillan, A. Oculomotor paralysis & jennerian vaccination. Rev. Otoneuroophtalmol. 1956, 28, 431. [Google Scholar]
- Kim, B.Y.; Yung, Y.; Kim, G.S.; Park, H.R.; Lee, J.J.; Song, P.; Cho, J.Y. Complete Oculomotor Palsy after Influenza Vaccination in a Young Healthy Adult: A Case Report. Case Rep. Neurol. 2021, 13, 35–39. [Google Scholar] [CrossRef]
- De Almeida, D.F.; Teodoro, A.T.; Radaeli Rde, F. Transient oculomotor palsy after influenza vaccination: Short report. ISRN Neurol. 2011, 2011, 849757. [Google Scholar] [CrossRef]
- Grewal, D.S.; Zeid, J.L. Isolated abducens nerve palsy following neonatal hepatitis B vaccination. J. AAPOS 2014, 18, 75–76. [Google Scholar] [CrossRef]
- Bourtoulamaiou, A.; Yadav, S.; Nayak, H. Benign Recurrent Sixth (Abducens) Nerve Palsy following Measles-Mumps-Rubella Vaccination. Case Rep. Pediatr. 2015, 2015, 734516. [Google Scholar] [CrossRef]
- Pereima, R.R.; Bonatti, R.; Crotti, F.; Furtado, J.M.; Lopes, M.H.; Yamamoto, J.H.; Kreuz, A.C. Ocular Adverse Events following Yellow Fever Vaccination: A Case Series. Ocul. Immunol. Inflamm. 2021, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Jumroendararasame, C.; Panyakorn, S.; Othong, R.; Jumroendararasame, A.; Srimanan, W.; Tipparut, K. Transient visual field loss after COVID-19 vaccination: Experienced by ophthalmologist, case report. Am. J. Ophthalmol. Case Rep. 2021, 24, 101212. [Google Scholar] [CrossRef] [PubMed]
- Santovito, L.S.; Pinna, G. Acute reduction of visual acuity and visual field after Pfizer-BioNTech COVID-19 vaccine 2nd dose: A case report. Inflamm. Res. 2021, 70, 931–933. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).