COVID-19: Impact of Original, Gamma, Delta, and Omicron Variants of SARS-CoV-2 in Vaccinated and Unvaccinated Pregnant and Postpartum Women
Abstract
1. Introduction
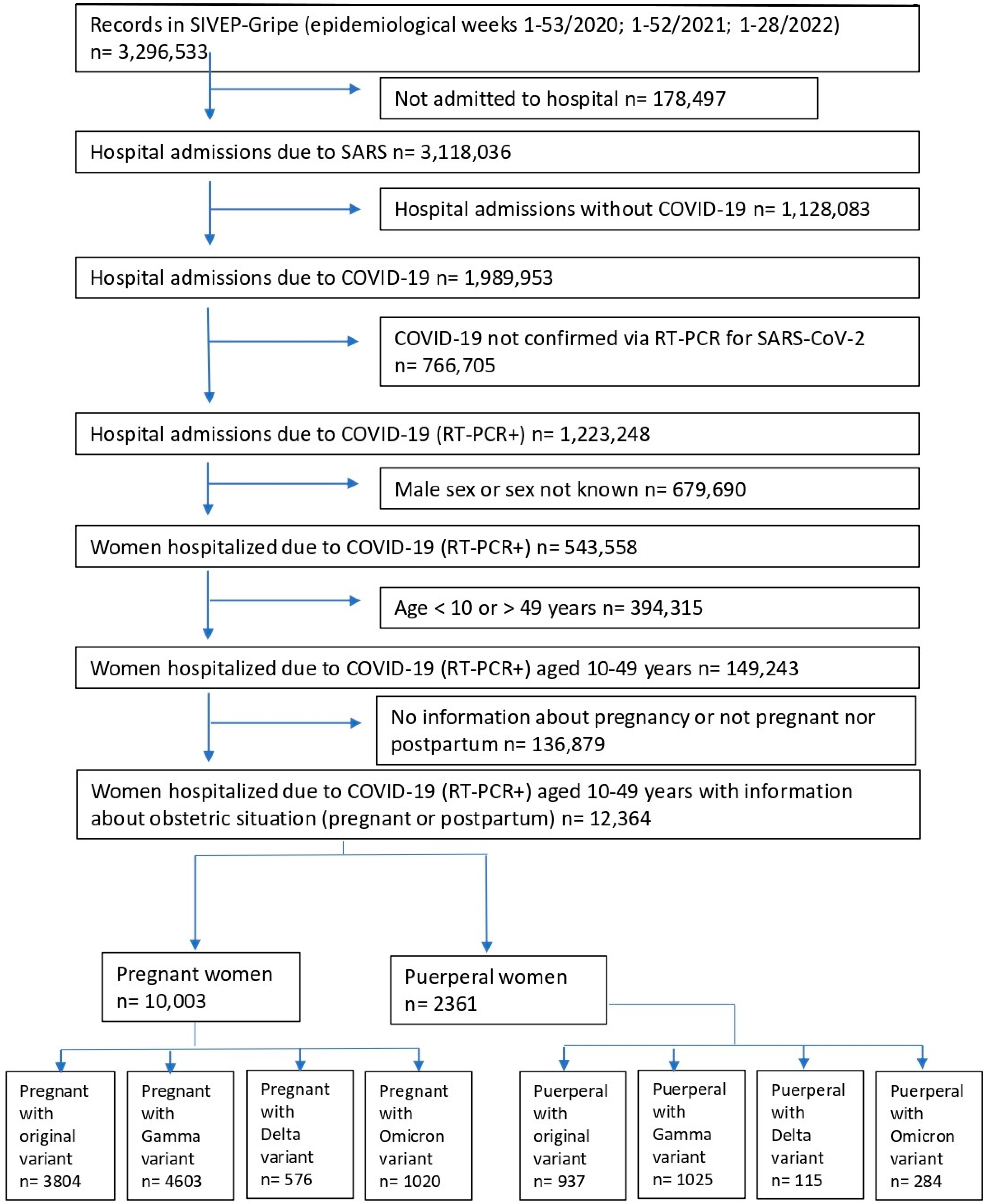
2. Materials and Methods
2.1. Data Analysis
2.2. Patient and Public Involvement
3. Results
4. Discussion
Postpartum Women
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19—11 March 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 23 March 2022).
- World Health Organization. WHO COVID-19 Dashboard. Available online: https://covid19.who.int/ (accessed on 17 October 2022).
- Zaigham, M.; Andersson, O. Maternal and perinatal outcomes with COVID-19: A systematic review of 108 pregnancies. Acta Obstet. Gynecol. Scand. 2020, 99, 823–829. [Google Scholar] [CrossRef] [PubMed]
- Kasraeian, M.; Zare, M.; Vafaei, H.; Asadi, N.; Faraji, A.; Bazrafshan, K.; Roozmeh, S. COVID-19 pneumonia and pregnancy; a systematic review and meta-analysis. J. Matern. Fetal Neonatal Med. 2022, 35, 1652–1659. [Google Scholar] [CrossRef] [PubMed]
- Mullins, E.; Evans, D.; Viner, R.M.; O’Brien, P.; Morris, E. Coronavirus in pregnancy and delivery: Rapid review. Ultrasound Obstet. Gynecol. 2020, 55, 586–592. [Google Scholar] [CrossRef] [PubMed]
- Badr, D.A.; Mattern, J.; Carlin, A.; Cordier, A.G.; Maillart, E.; El Hachem, L.; El Kenz, H.; Andronikof, M.; De Bels, D.; Damoisel, C.; et al. Are clinical outcomes worse for pregnant women at ≥20 weeks’ gestation infected with coronavirus disease 2019? A multicenter case-control study with propensity score matching. Am. J. Obstet. Gynecol. 2020, 223, 764–768. [Google Scholar] [CrossRef] [PubMed]
- Sentilhes, L.; De Marcillac, F.; Jouffrieau, C.; Kuhn, P.; Thuet, V.; Hansmann, Y.; Ruch, Y.; Fafi-Kremer, S.; Deruelle, P. Coronavirus disease 2019 in pregnancy was associated with maternal morbidity and preterm birth. Am. J. Obstet. Gynecol. 2020, 223, 914.e1–914.e15. [Google Scholar] [CrossRef] [PubMed]
- Zambrano, L.D.; Ellington, S.; Strid, P.; Galang, R.R.; Oduyebo, T.; Tong, V.T.; Woodworth, K.R.; Nahabedian, J.F.; Azziz-Baumgartner, E.; Gilboa, S.M.; et al. Update: Characteristics of symptomatic women of reproductive age with laboratory-confirmed SARS-CoV-2 infection by pregnancy status—United States, January 22–October 3, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1641–1647. [Google Scholar] [CrossRef]
- Allotey, J.; Stallings, E.; Bonet, M.; Yap, M.; Chatterjee, S.; Kew, T.; Debenham, L.; Llavall, A.C.; Dixit, A.; Zhou, D.; et al. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: Living systematic review and meta-analysis. BMJ 2020, 370, m3320. [Google Scholar] [CrossRef]
- Martinez-Portilla, R.J.; Sotiriadis, A.; Chatzakis, C.; Torres-Torres, J.; Espino Y Sosa, S.; Sandoval-Mandujano, K.; Castro-Bernabe, D.A.; Medina-Jimenez, V.; Monarrez-Martin, J.C.; Figueras, F.; et al. Pregnant women with SARS-CoV-2 infection are at higher risk of death and pneumonia: Propensity score matched analysis of a nationwide prospective cohort (COV19Mx). Ultrasound Obstet. Gynecol. 2021, 57, 224–231. [Google Scholar] [CrossRef]
- Rozo, N.; Valencia, D.; Newton, S.M.; Avila, G.; Gonzalez, M.A.; Sancken, C.L.; Burkel, V.K.; Ellington, S.R.; Gilboa, S.M.; Rao, C.Y.; et al. Severity of illness by pregnancy status among laboratory-confirmed SARS-CoV-2 infections occurring in reproductive-aged women in Colombia. Paediatr. Perinat. Epidemiol. 2022, 36, 456–465. [Google Scholar] [CrossRef]
- World Health Organization. Tracking SARS-CoV-2 Variants. Available online: http://who.int/en/activities/tracking-SARS-CoV-2-variants/ (accessed on 21 May 2022).
- Fiocruz. Genomic Network. Available online: http://www.genomahcov.fiocruz.br/ (accessed on 22 May 2022).
- Takemoto, M.; Menezes, M.O.; Andreucci, C.B.; Knobel, R.; Sousa, L.; Katz, L.; Fonseca, E.B.; Nakamura-Pereira, M.; Magalhães, C.G.; Diniz, C.; et al. Clinical characteristics and risk factors for mortality in obstetric patients with severe COVID-19 in Brazil: A surveillance database analysis. BJOG Int. J. Obstet. Gynaecol. 2020, 127, 1618–1626. [Google Scholar] [CrossRef]
- Serra, F.E.; Francisco, R.P.V.; de Rossi, P.; de Lourdes Brizot, M.; Rodrigues, A.S. COVID-19 outcomes in hospitalized puerperal, pregnant, and neither pregnant nor puerperal women. PLoS ONE 2021, 16, e0259911. [Google Scholar] [CrossRef] [PubMed]
- Francisco, R.P.V.; Lacerda, L.; Rodrigues, A.S. Obstetric Observatory Brazil—COVID-19: 1031 maternal deaths because of COVID-19 and the unequal access to health care services. Clinics 2021, 76, e3120. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves, B.M.M.; Franco, R.P.V.; Rodrigues, A.S. Maternal mortality associated with COVID-19 in Brazil in 2020 and 2021: Comparison with non-pregnant women and men. PLoS ONE 2021, 16, e0261492. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health of Brazil. Department of Health Surveillance. Department of Immunization and Transmitted Diseases. General Coordination of the National immunization Program: NOTA TÉCNICA Nº 467/2021-CGPNI/DEIDT/SVS/MS. Available online: https://www.gov.br/saude/pt-br/media/pdf/2021/abril/27/nota-tecnica-467-2021-cgpni-deidt-svs-ms.pdf (accessed on 22 May 2022).
- Kalafat, E.; Heath, P.; Prasad, S.; O’Brien, P.; Khalil, A. COVID-19 vaccination in pregnancy. Am. J. Obstet. Gynecol. 2022, 227, 136–147. [Google Scholar] [CrossRef]
- de Freitas Paganoti, C.; Alkmin da Costa, R.; Papageorghiou, A.T.; da Silva Costa, F.; Quintana, S.M.; Graziela de Godoi, L.; Adriana Jiménez Monroy, N.; Sacramento Rodrigues, A.; Pulcineli Vieira Francisco, R. COVID-19 vaccines confer protection in hospitalized pregnant and postpartum women with severe COVID-19: A retrospective cohort study. Vaccines 2022, 10, 749. [Google Scholar] [CrossRef]
- Ministry of Health of Brazil. Definition of Case and Notification. Available online: https://www.gov.br/saude/pt-br/coronavirus/artigos/definicao-e-casos-suspeitos (accessed on 4 April 2021).
- Ministry of Health of Brazil. Notifiable Diseases Information System: Sinan. Epidemiological Calendar 2022. Available online: http://www.portalsinan.saude.gov.br/calendario-epidemiologico (accessed on 30 August 2022).
- R Core Team. R: A Language and Environment for Statistical Computing, version 4.1.3; R Foundation for Statistical Computing: Vienna, Austria, 2020; Available online: https://www.r-project.org/ (accessed on 30 July 2022).
- Chen, H.; Guo, J.; Wang, C.; Luo, F.; Yu, X.; Zhang, W.; Li, J.; Zhao, D.; Xu, D.; Gong, Q.; et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: A retrospective review of medical records. Lancet 2020, 395, 809–815. [Google Scholar] [CrossRef]
- Di Toro, F.; Gjoka, M.; Di Lorenzo, G.; De Santo, D.; De Seta, F.; Maso, G.; Risso, F.M.; Romano, F.; Wiesenfeld, U.; Levi-D’Ancona, R.; et al. Impact of COVID-19 on maternal and neonatal outcomes: A systematic review and meta-analysis. Clin. Microbiol. Infect. 2021, 27, 36–46. [Google Scholar] [CrossRef]
- Elshafeey, F.; Magdi, R.; Hindi, N.; Elshebiny, M.; Farrag, N.; Mahdy, S.; Sabbour, M.; Gebril, S.; Nasser, M.; Kamel, M.; et al. A systematic scoping review of COVID-19 during pregnancy and childbirth. Int. J. Gynaecol. Obstet. 2020, 150, 47–52. [Google Scholar] [CrossRef]
- Huntley, B.J.F.; Huntley, E.S.; Di Mascio, D.; Chen, T.; Berghella, V.; Chauhan, S.P. Rates of maternal and perinatal mortality and vertical transmission in pregnancies complicated by severe acute respiratory syndrome coronavirus 2 (SARS-Co-V-2) infection: A systematic Review. Obstet. Gynecol. 2020, 136, 303–312. [Google Scholar] [CrossRef]
- Hantoushzadeh, S.; Shamshirsaz, A.A.; Aleyasin, A.; Seferovic, M.D.; Aski, S.K.; Arian, S.E.; Pooransari, P.; Ghotbizadeh, F.; Aalipour, S.; Soleimani, Z.; et al. Maternal death due to COVID-19. Am. J. Obstet. Gynecol. 2020, 223, 109.e1–109.e16. [Google Scholar] [CrossRef]
- Collin, J.; Byström, E.; Carnahan, A.; Ahrne, M. Public Health Agency of Sweden’s Brief Report: Pregnant and postpartum women with severe acute respiratory syndrome coronavirus 2 infection in intensive care in Sweden. Acta Obstet. Gynecol. Scand. 2020, 99, 819–822. [Google Scholar] [CrossRef] [PubMed]
- Thaddeus, S.; Maine, D. Too far to walk: Maternal mortality in context. Soc. Sci. Med. 1994, 38, 1091–1110. [Google Scholar] [CrossRef] [PubMed]
- Finlayson, K.; Crossland, N.; Bonet, M.; Downe, S. What matters to women in the postnatal period: A meta-synthesis of qualitative studies. PLoS ONE 2020, 15, e0231415. [Google Scholar] [CrossRef] [PubMed]
- Pacagnella, R.C.; Cecatti, J.G.; Parpinelli, M.A.; Sousa, M.H.; Haddad, S.M.; Costa, M.L.; Souza, J.P.; Pattinson, R.C.; Brazilian Network for the Surveillance of Severe Maternal Morbidity study group. Delays in receiving obstetric care and poor maternal outcomes: Results from a national multicentre cross-sectional study. BMC Pregnancy Childbirth 2014, 14, 159. [Google Scholar] [CrossRef]
- Kamel, H.; Navi, B.B.; Sriram, N.; Hovsepian, D.A.; Devereux, R.B.; Elkind, M.S. Risk of a thrombotic event after the 6-week postpartum period. N. Engl. J. Med. 2014, 370, 1307–1315. [Google Scholar] [CrossRef]
- Helms, J.; Tacquard, C.; Severac, F.; Leonard-Lorant, I.; Ohana, M.; Delabranche, X.; Merdji, H.; Clere-Jehl, R.; Schenck, M.; Fagot Gandet, F.; et al. High risk of thrombosis in patients with severe SARS-CoV-2 infection: A multicenter prospective cohort study. Intensive Care Med. 2020, 46, 1089–1098. [Google Scholar] [CrossRef]
- Tang, N.; Li, D.; Wang, X.; Sun, Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J. Thromb. Haemost. 2020, 18, 844–847. [Google Scholar] [CrossRef]
- Katz, D.; Beilin, Y. Disorders of coagulation in pregnancy. Br. J. Anaesth. 2015, 115 (Suppl. 2), ii75–ii88. [Google Scholar] [CrossRef]
- Sobhy, S.; Arroyo-Manzano, D.; Murugesu, N.; Karthikeyan, G.; Kumar, V.; Kaur, I.; Fernandez, E.; Gundabattula, S.R.; Betran, A.P.; Khan, K.; et al. Maternal and perinatal mortality and complications associated with caesarean section in low-income and middle-income countries: A systematic review and meta-analysis. Lancet 2019, 393, 1973–1982. [Google Scholar] [CrossRef]
- Nahshon, C.; Bitterman, A.; Haddad, R.; Hazzan, D.; Lavie, O. Hazardous postoperative Outcomes of Unexpected COVID-19 Infected Patients: A Call for Global Consideration of Sampling all Asymptomatic Patients Before Surgical Treatment. World J. Surg. 2020, 44, 2477–2481. [Google Scholar] [CrossRef]
- Aminian, A.; Safari, S.; Razeghian-Jahromi, A.; Ghorbani, M.; Delaney, C.P. COVID-19 outbreak and surgical practice: Unexpected fatality in perioperative period. Ann. Surg. 2020, 272, e27–e29. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health of Brazil. DATASUS. Live Birth Information System—SINASC. 2020. Available online: http://tabnet.datasus.gov.br/cgi/tabcgi.exe?sinasc/cnv/nvuf.def (accessed on 23 July 2022).
- Loconsole, D.; Centrone, F.; Morcavallo, C.; Campanella, S.; Accogli, M.; Sallustio, A.; Peccarisi, D.; Stufano, A.; Lovreglio, P.; Chironna, M. Changing features of COVID-19: Characteristics of infections with the SARS-CoV-2 Delta (B.1.617.2) and alpha (B.1.1.7) variants in Southern Italy. Vaccines 2021, 9, 1354. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Zou, X.; Li, Z.; Fu, J.; Fan, H.; Yu, H.; Deng, F.; Huang, H.; Peng, J.; Zhao, K.; et al. Analysis of clinical characteristics and virus strains variation of patients infected with SARS-CoV-2 in Jiangsu Province-A retrospective study. Front. Public Health 2021, 9, 791600. [Google Scholar] [CrossRef]
- Cantón, R.; De Lucas Ramos, P.; García-Botella, A.; García-Lledó, A.; Gómez-Pavón, J.; González Del Castillo, J.; Hernández-Sampelayo, T.; Martín-Delgado, M.C.; Martín Sánchez, F.J.; Martínez-Sellés, M.; et al. New variants of SARS-CoV-2. Rev. Esp. Quimioter. 2021, 34, 419–428. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.; Liu, Y.; Tang, X.; He, D. The disease severity and clinical outcomes of the SARS-CoV-2 variants of concern. Front. Public Health 2021, 9, 775224. [Google Scholar] [CrossRef] [PubMed]
- Gray, K.J.; Bordt, E.A.; Atyeo, C.; Deriso, E.; Akinwunmi, B.; Young, N.; Baez, A.M.; Shook, L.L.; Cvrk, D.; James, K.; et al. Coronavirus disease 2019 vaccine response in pregnant and lactating women: A cohort study. Am. J. Obstet. Gynecol. 2021, 225, 303.e1–303.e17. [Google Scholar] [CrossRef] [PubMed]
- Mackin, D.W.; Walker, S.P. The historical aspects of vaccination in pregnancy. Best Pract. Res. Clin. Obstet. Gynaecol. 2021, 76, 13–22. [Google Scholar] [CrossRef]
- Blakeway, H.; Prasad, S.; Kalafat, E.; Heath, P.T.; Ladhani, S.N.; Le Doare, K.; Magee, L.A.; O’Brien, P.; Rezvani, A.; von Dadelszen, P.; et al. COVID-19 vaccination during pregnancy: Coverage and safety. Am. J. Obstet. Gynecol. 2022, 226, 236.e1–236.e14. [Google Scholar] [CrossRef]
- Lipkind, H.S.; Vazquez-Benitez, G.; DeSilva, M.; Vesco, K.K.; Ackerman-Banks, C.; Zhu, J.; Boyce, T.G.; Daley, M.F.; Fuller, C.C.; Getahun, D.; et al. Receipt of COVID-19 vaccine during pregnancy and preterm or small-for-gestational-age at birth—Eight integrated health care organizations, United States, December 15, 2020–July 22, 2021. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 26–30. [Google Scholar] [CrossRef]
- Ministry of Health of Brazil, Department of Health Surveillance, Department of Immunization and Transmitted Diseases. General Coordination of the National Immunization Program: Nota Técnica Nº 651/2021-CGPNI/DEIDT/SVS/MS. Available online: https://www.gov.br/saude/pt-br/media/pdf/2021/maio/19/nota-tecnica-651-2021-cgpni-deidt-svs-ms.pdf (accessed on 30 July 2022).
- León, T.M.; Dorabawila, V.; Nelson, L.; Lutterloh, E.; Bauer, U.E.; Backenson, B.; Bassett, M.T.; Henry, H.; Bregman, B.; Midgley, C.M.; et al. COVID-19 cases and hospitalizations by COVID-19 vaccination status and previous COVID-19 diagnosis—California and New York, May–November 2021. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 125–131. [Google Scholar] [CrossRef]
- Thompson, M.G.; Natarajan, K.; Irving, S.A.; Rowley, E.A.; Griggs, E.P.; Gaglani, M.; Klein, N.P.; Grannis, S.J.; DeSilva, M.B.; Stenehjem, E.; et al. Effectiveness of a third dose of mRNA vaccines against COVID-19—Associated emergency department and urgent care encounters and hospitalizations among adults during periods of Delta and Omicron variant predominance—VISION Network, 10 states, August 2021–January 2022. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Danza, P.; Koo, T.H.; Haddix, M.; Fisher, R.; Traub, E.; OYong, K.; Balter, S. SARS-CoV-2 Infection and Hospitalization Among Adults Aged ≥18 Years, by Vaccination Status, Before and During SARS-CoV-2 B.1.1.529 (Omicron) Variant Predominance—Los Angeles County, California, November 7, 2021-January 8, 2022. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 177–181. [Google Scholar] [CrossRef] [PubMed]
- Beigi, R.H.; Krubiner, C.; Jamieson, D.J.; Lyerly, A.D.; Hughes, B.; Riley, L.; Faden, R.; Karron, R. The need for inclusion of pregnant women in COVID-19 vaccine trials. Vaccine 2021, 39, 868–870. [Google Scholar] [CrossRef] [PubMed]
| Variant | Age (Years) | Pregnant | Puerperal | p |
|---|---|---|---|---|
| Original (n = 4741) | <20 | 261 (6.9%) | 67 (7.2%) | 0.2567 C |
| 20–34 | 2526 (66.4%) | 596 (63.6%) | ||
| ≥35 | 1017 (26.7%) | 274 (29.2%) | ||
| Gamma (n = 5628) | <20 | 243 (5.3%) | 62 (6.0%) | 0.5902 C |
| 20–34 | 2976 (64.7%) | 662 (64.6%) | ||
| ≥35 | 1384 (30.1%) | 301 (29.4%) | ||
| Delta (n = 691) | <20 | 39 (6.8%) | 11 (9.6%) | 0.5666 C |
| 20–34 | 391 (67.9%) | 75 (65.2%) | ||
| ≥35 | 146 (25.3%) | 29 (25.2%) | ||
| Omicron (n = 1304) | <20 | 85 (8.3%) | 30 (10.6%) | 0.3260 C |
| 20–34 | 722 (70.8%) | 189 (66.5%) | ||
| ≥35 | 213 (20.9%) | 65 (22.9%) | ||
| Variant | Skin color/ethnicity | Pregnant | Puerperal | p |
| Original (n = 3842) | White | 1301 (42.1%) | 289 (38.6%) | 0.07546 F |
| Black | 210 (6.8%) | 52 (6.9%) | ||
| Yellow | 38 (1.2%) | 3 (0.4%) | ||
| Brown | 1531 (49.5%) | 401 (53.5%) | ||
| Indigenous | 13 (0.4%) | 4 (0.5%) | ||
| Gamma (n = 4812) | White | 1917 (48.6%) | 407 (46.8%) | 0.5847 F |
| Black | 230 (5.8%) | 56 (6.4%) | ||
| Yellow | 32 (0.8%) | 6 (0.7%) | ||
| Brown | 1754 (44.5%) | 397 (45.6%) | ||
| Indigenous | 9 (0.2%) | 4 (0.5%) | ||
| Delta (n = 594) | White | 242 (48.8%) | 50 (51.0%) | 0.9395 F |
| Black | 36 (7.3%) | 5 (5.1%) | ||
| Yellow | 3 (0.6%) | 0 (0.0%) | ||
| Brown | 211 (42.5%) | 43 (43.9%) | ||
| Indigenous | 4 (0.8%) | 0 (0.0%) | ||
| Omicron (n = 1176) | White | 610 (65.9%) | 143 (57.0%) | 0.0039 F |
| Black | 50 (5.4%) | 10 (4.0%) | ||
| Yellow | 9 (1.0%) | 0 (0.0%) | ||
| Brown | 255 (27.6%) | 97 (38.6%) | ||
| Indigenous | 1 (0.1%) | 1 (0.4%) | ||
| Variant | Education level | Pregnant | Puerperal | p |
| Original (n = 2002) | No schooling | 7 (0.4%) | 3 (0.8%) | 0.5112 F |
| Up to high school | 394 (24.1%) | 84 (22.7%) | ||
| High school | 898 (55.1%) | 200 (53.9%) | ||
| College | 332 (20.4%) | 84 (22.6%) | ||
| Gamma (n = 2365) | No schooling | 15 (0.8%) | 6 (1.4%) | 0.4348 F |
| Up to high school | 469 (24.3%) | 112 (25.8%) | ||
| High school | 1051 (54.4%) | 236 (54.4%) | ||
| College | 396 (20.5%) | 80 (18.4%) | ||
| Delta (n = 287) | No schooling | 0 (0.0%) | 0 (0.0%) | 0.5912 F |
| Up to high school | 72 (30.1%) | 11 (22.9%) | ||
| High school | 112 (46.9%) | 24 (50.0%) | ||
| College | 55 (23.0%) | 13 (27.1%) | ||
| Omicron (n = 586) | No schooling | 2 (0.4%) | 2 (1.9%) | 0.3158 F |
| Up to high school | 135 (28.2%) | 31 (28.9%) | ||
| High school | 249 (52.0%) | 51 (47.7%) | ||
| College | 93 (19.4%) | 23 (21.5%) | ||
| Comorbidities | Variant | Pregnant | Puerperal | p |
| Chronic cardiovascular disease | Original (n = 1889) | 239/1306 (18.3%) | 89/583 (15.3%) | 0.1230 C |
| Gamma (n = 2084) | 245/1409 (17.4%) | 84/675 (12.4%) | 0.0046 C | |
| Delta (n = 256) | 29/179 (16.2%) | 8/77 (10.4%) | 0.3082 C | |
| Omicron (n = 441) | 49/265 (18.5%) | 13/176 (7.4%) | 0.0017 C | |
| Asthma | Original (n = 1847) | 160/1288 (12.4%) | 34/559 (6.1%) | 0.0001 C |
| Gamma (n = 2040) | 148/1373 (10.8%) | 37/667 (5.5%) | 0.0002 C | |
| Delta (n = 256) | 23/181 (12.7%) | 6/75 (8.0%) | 0.3871 C | |
| Omicron (n = 429) | 26/257 (10.1%) | 6/172 (3.5%) | 0.0176 C | |
| Diabetes | Original (n = 1887) | 274/1319 (20.8%) | 65/568 (11.4%) | <0.0001 C |
| Gamma (n = 2134) | 337/1448 (23.3%) | 77/686 (11.2%) | <0.0001 C | |
| Delta (n = 267) | 48/188 (25.5%) | 8/79 (10.1%) | 0.0079 C | |
| Omicron (n = 446) | 62/268 (23.1%) | 10/178 (5.6%) | <0.0001 C | |
| Obesity | Original (n = 1822) | 181/1263 (14.3%) | 64/559 (11.4%) | 0.1122 C |
| Gamma (n = 2142) | 368/1451 (25.4%) | 111/691 (16.1%) | <0.0001 C | |
| Delta (n = 259) | 39/183 (21.3%) | 8/76 (10.5%) | 0.0610 C | |
| Omicron (n = 425) | 32/249 (12.9%) | 10/176 (5.7%) | 0.0229 C |
| Signs and Symptoms | Variant | Unvaccinated | Vaccinated (at Least One Dose) | ||||
|---|---|---|---|---|---|---|---|
| Pregnant | Puerperal | Puerperal vs. Pregnant OR (95% CI) | Pregnant | Puerperal | Puerperal vs. Pregnant OR (95% CI) | ||
| Fever | Original (n = 4150) | 2283/3345 (68.3%) | 500/805 (62.1%) | 0.76 (0.65–0.90) | - | - | - |
| Gamma (n = 2839) | 1283/1995 (64.3%) | 241/459 (52.5%) | 0.61 (0.50–0.76) | 204/321 (63.6%) | 32/64 (50.0%) | 0.57 (0.32–1.02) | |
| Delta (n = 529) | 131/206 (63.6%) | 30/47 (63.8%) | 1.01 (0.50–2.09) | 146/237 (61.6%) | 20/39 (51.3%) | 0.66 (0.31–1.38) | |
| Omicron (n = 881) | 108/190 (56.8%) | 28/66 (42.4%) | 0.56 (0.30–1.02) | 244/491 (49.7%) | 40/134 (29.9%) | 0.43 (0.28–0.66) | |
| Cough | Original (n = 4272) | 2674/3454 (77.4%) | 576/818 (70.4%) | 0.69 (0.58–0.83) | - | - | - |
| Gamma (n = 2952) | 1689/2079 (81.2%) | 335/473 (70.8%) | 0.56 (0.44–0.71) | 273/331 (82.5%) | 51/69 (73.9%) | 0.60 (0.32–1.17) | |
| Delta (n = 568) | 175/223 (78.5%) | 40/52 (76.9%) | 0.91 (0.43–2.06) | 194/252 (77.0%) | 28/41 (68.3%) | 0.64 (0.30–1.45) | |
| Omicron (n = 953) | 140/205 (68.3%) | 43/68 (63.2%) | 0.80 (0.43–1.49) | 359/529 (67.9%) | 96/151 (63.6%) | 0.83 (0.56–1.23) | |
| Sore throat | Original (n = 3656) | 825/2960 (27.9%) | 182/696 (26.1%) | 0.92 (0.76–1.11) | - | - | - |
| Gamma (n = 2567) | 488/1810 (27.0%) | 96/414 (23.2%) | 0.82 (0.63–1.06) | 71/281 (25.3%) | 13/62 (21.0%) | 0.79 (0.37–1.58) | |
| Delta (n = 486) | 48/186 (25.8%) | 8/45 (17.8%) | 0.62 (0.23–1.48) | 69/222 (31.1%) | 9/33 (27.3%) | 0.83 (0.32–1.97) | |
| Omicron (n = 833) | 70/182 (38.5%) | 15/58 (25.9%) | 0.56 (0.27–1.12) | 177/462 (38.3%) | 40/131 (30.5%) | 0.71 (0.45–1.09) | |
| Dyspnea | Original (n = 4086) | 2024/3305 (61.2%) | 467/781 (59.8%) | 0.94 (0.80–1.11) | - | - | - |
| Gamma (n = 2913) | 1493/2051 (72.8%) | 314/470 (66.8%) | 0.75 (0.60–0.94) | 231/326 (70.9%) | 44/66 (66.7%) | 0.82 (0.45–1.52) | |
| Delta (n = 545) | 149/216 (69.0%) | 36/51 (70.6%) | 1.08 (0.53–2.27) | 147/238 (61.8%) | 20/40 (50.0%) | 0.62 (0.29–1.29) | |
| Omicron (n = 818) | 58/174 (33.3%) | 16/61 (26.2%) | 0.71 (0.35–1.42) | 117/443 (26.4%) | 52/140 (37.1%) | 1.64 (1.07–2.50) | |
| Respiratory discomfort | Original (n = 3882) | 1565/3123 (50.1%) | 413/759 (54.4%) | 1.19 (1.01–1.39) | - | - | - |
| Gamma (n = 2762) | 1143/1944 (58.8%) | 267/448 (59.6%) | 1.03 (0.83–1.28) | 168/303 (55.4%) | 35/67 (52.2%) | 0.88 (0.50–1.55) | |
| Delta (n = 510) | 113/203 (55.7%) | 22/47 (46.8%) | 0.70 (0.35–1.39) | 105/222 (47.3%) | 11/38 (28.9%) | 0.46 (0.19–1.00) | |
| Omicron (n = 807) | 42/170 (24.7%) | 14/60 (23.3%) | 0.92 (0.43–1.92) | 127/438 (29.0%) | 42/139 (30.2%) | 1.06 (0.68–1.63) | |
| SpO2 < 95% | Original (n = 3780) | 1020/3043 (33.5%) | 340/737 (46.1%) | 1.70 (1.44–2.00) | - | - | - |
| Gamma (n = 2780) | 1120/1964 (57.0%) | 264/451 (58.5%) | 1.06 (0.86–1.32) | 163/299 (54.5%) | 34/66 (51.5%) | 0.89 (0.50–1.57) | |
| Delta (n = 517) | 112/205 (54.6%) | 32/47 (68.1%) | 1.77 (0.86–3.74) | 93/227 (41.0%) | 17/38 (44.7%) | 1.16 (0.55–2.46) | |
| Omicron (n = 783) | 31/170 (18.2%) | 12/57 (21.1%) | 1.19 (0.51–2.63) | 67/426 (15.7%) | 35/130 (26.9%) | 1.97 (1.20–3.22) | |
| Diarrhea | Original (n = 3539) | 404/2879 (14.0%) | 74/660 (11.2%) | 0.77 (0.58–1.01) | - | - | - |
| Gamma (n = 2501) | 220/1761 (12.5%) | 37/406 (9.1%) | 0.70 (0.47–1.02) | 25/271 (9.2%) | 7/63 (11.1%) | 1.23 (0.43–3.11) | |
| Delta (n = 472) | 17/183 (9.3%) | 5/44 (11.4%) | 1.25 (0.34–3.82) | 22/212 (10.4%) | 1/33 (3.0%) | 0.27 (0.01–1.80) | |
| Omicron (n = 583) | 13/167 (7.8%) | 2/56 (3.6%) | 0.44 (0.05–2.04) | 22/416 (5.3%) | 7/122 (5.7%) | 1.09 (0.38–2.73) | |
| Vomiting | Original (n = 3539) | 399/2884 (13.8%) | 46/655 (7.0%) | 0.47 (0.33–0.65) | - | - | - |
| Gamma (n = 2510) | 249/1771 (14.1%) | 30/407 (7.4%) | 0.49 (0.32–0.73) | 35/271 (12.9%) | 7/61 (11.5%) | 0.87 (0.31–2.14) | |
| Delta (n = 470) | 21/182 (11.5%) | 1/44 (2.3%) | 0.18 (0.00–1.18) | 24/211 (11.4%) | 2/33 (6.1%) | 0.50 (0.06–2.21) | |
| Omicron (n = 770) | 24/170 (14.1%) | 2/55 (3.6%) | 0.23 (0.03–0.98) | 54/423 (12.8%) | 6/122 (4.9%) | 0.35 (0.12–0.85) | |
| Abdominal pain | Original (n = 1886) | 159/1562 (10.2%) | 26/324 (8.0%) | 0.77 (0.48–1.20) | - | - | - |
| Gamma (n = 2476) | 177/1750 (10.1%) | 35/401 (8.7%) | 0.85 (0.56–1.25) | 29/263 (11.0%) | 3/62 (4.8%) | 0.41 (0.08–1.40) | |
| Delta (n = 466) | 23/181 (12.7%) | 2/44 (4.5%) | 0.33 (0.04–1.42) | 21/208 (10.1%) | 4/33 (12.1%) | 1.23 (0.29–4.02) | |
| Omicron (n = 761) | 18/168 (10.7%) | 3/55 (5.5%) | 0.48 (0.09–1.75) | 56/415 (13.5%) | 9/123 (7.3%) | 0.51 (0.21–1.07) | |
| Fatigue | Original (n = 1933) | 394/1595 (24.7%) | 71/338 (21.0%) | 0.81 (0.60–1.08) | - | - | - |
| Gamma (n = 2576) | 640/1820 (35.2%) | 127/411 (30.9%) | 0.82 (0.65–1.04) | 113/279 (40.5%) | 21/66 (31.8%) | 0.69 (0.37–1.25) | |
| Delta (n = 478) | 52/187 (27.8%) | 17/45 (37.8%) | 1.57 (0.74–3.27) | 62/213 (29.1%) | 7/33 (21.2%) | 0.66 (0.23–1.66) | |
| Omicron (n = 768) | 38/168 (22.6%) | 9/58 (15.5%) | 0.63 (0.25–1.45) | 75/417 (18.0%) | 24/125 (19.2%) | 1.08 (0.62–1.84) | |
| Anosmia | Original (n = 1984) | 442/1636 (27.0%) | 78/348 (22.4%) | 0.78 (0.58–1.03) | - | - | - |
| Gamma (n = 2517) | 373/1778 (21.0%) | 55/401 (13.7%) | 0.60 (0.43–0.82) | 59/275 (21.5%) | 10/63 (15.9%) | 0.69 (0.30–1.48) | |
| Delta (n = 468) | 37/180 (20.6%) | 4/44 (9.1%) | 0.39 (0.09–1.18) | 44/210 (21.0%) | 6/34 (17.6%) | 0.81 (0.26–2.16) | |
| Omicron (n = 748) | 7/164 (4.3%) | 2/54 (3.7%) | 0.86 (0.08–4.73) | 14/407 (3.4%) | 2/123 (1.6%) | 0.46 (0.05–2.07) | |
| Ageusia | Original (n = 1958) | 400/1615 (24.8%) | 66/343 (19.2%) | 0.72 (0.53–0.97) | - | - | - |
| Gamma (n = 2517) | 332/1777 (18.7%) | 55/403 (13.6%) | 0.69 (0.50–0.94) | 64/276 (23.2%) | 8/61 (13.1%) | 0.50 (0.20–1.13) | |
| Delta (n = 468) | 37/178 (20.8%) | 5/44 (11.4%) | 0.49 (0.14–1.37) | 42/211 (19.9%) | 7/35 (20.0%) | 1.01 (0.35–2.57) | |
| Omicron (n = 746) | 7/163 (4.3%) | 1/54 (1.9%) | 0.42 (0.01–3.41) | 18/406 (4.4%) | 3/123 (2.4%) | 0.54 (0.10–1.89) | |
| Outcome | Variant | Unvaccinated | Vaccinated (with at Least One Dose) | ||||
|---|---|---|---|---|---|---|---|
| Pregnant | Puerperal | Puerperal vs. Pregnant OR (95% CI) | Pregnant | Puerperal | Puerperal vs. Pregnant OR (95% CI) | ||
| ICU admission (n = 9202) | Original (n = 4436) | 833/3566 (23.4%) | 310/870 (35.6%) | 1.82 (1.54–2.13) | - | - | - |
| Gamma (n = 3051) | 795/2157 (36.9%) | 235/490 (48.0%) | 1.58 (1.29–1.93) | 91/334 (27.2%) | 28/70 (40.0%) | 1.78 (1.00–3.13) | |
| Delta (n = 579) | 90/225 (40.0%) | 26/51 (51.0%) | 1.56 (0.81–3.01) | 75/256 (29.3%) | 16/47 (34.0%) | 1.24 (0.60–2.51) | |
| Omicron (n = 1136) | 23/257 (8.9%) | 18/88 (20.5%) | 2.61 (1.25–5.38) | 59/623 (9.5%) | 28/168 (16.7%) | 1.91 (1.13–3.17) | |
| Invasive respiratory support (n = 8904) | Original (n = 4237) | 300/3389 (8.9%) | 172/848 (20.3%) | 2.62 (2.13–3.22) | - | - | - |
| Gamma (n = 2964) | 411/2105 (19.5%) | 163/472 (34.5%) | 2.17 (1.75–2.70) | 39/319 (12.2%) | 12/68 (17.6%) | 1.54 (0.76–3.12) | |
| Delta (n = 576) | 34/225 (15.1%) | 11/51 (21.6%) | 1.54 (0.72–3.30) | 20/254 (7.9%) | 4/46 (8.7%) | 1.11 (0.36–3.42) | |
| Omicron (n = 1127) | 8/252 (3.2%) | 8/87 (9.2%) | 3.09 (1.12–8.50) | 16/619 (2.6%) | 12/169 (7.1%) | 2.88 (1.34–6.21) | |
| Death (n = 9206) | Original (n = 4449) | 231/3563 (6.5%) | 130/886 (14.7%) | 2.48 (1.96–3.13) | - | - | - |
| Gamma (n = 3007) | 325/2117 (15.4%) | 128/483 (26.5%) | 1.99 (1.56–2.53) | 22/341 (6.5%) | 10/66 (15.2%) | 2.58 (1.03–6.06) | |
| Delta (n = 559) | 23/222 (10.4%) | 8/48 (16.7%) | 1.73 (0.62–4.36) | 7/243 (2.9%) | 1/46 (2.2%) | 0.75 (0.02–6.07) | |
| Omicron (n = 1191) | 6/267 (2.2%) | 2/94 (2.1%) | 0.95 (0.09–5.41) | 7/659 (1.1%) | 6/171 (3.5%) | 3.38 (0.93–11.93) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Serra, F.E.; Rosa Junior, E.R.; de Rossi, P.; Francisco, R.P.V.; Rodrigues, A.S. COVID-19: Impact of Original, Gamma, Delta, and Omicron Variants of SARS-CoV-2 in Vaccinated and Unvaccinated Pregnant and Postpartum Women. Vaccines 2022, 10, 2172. https://doi.org/10.3390/vaccines10122172
Serra FE, Rosa Junior ER, de Rossi P, Francisco RPV, Rodrigues AS. COVID-19: Impact of Original, Gamma, Delta, and Omicron Variants of SARS-CoV-2 in Vaccinated and Unvaccinated Pregnant and Postpartum Women. Vaccines. 2022; 10(12):2172. https://doi.org/10.3390/vaccines10122172
Chicago/Turabian StyleSerra, Fabiano Elisei, Elias Ribeiro Rosa Junior, Patricia de Rossi, Rossana Pulcineli Vieira Francisco, and Agatha Sacramento Rodrigues. 2022. "COVID-19: Impact of Original, Gamma, Delta, and Omicron Variants of SARS-CoV-2 in Vaccinated and Unvaccinated Pregnant and Postpartum Women" Vaccines 10, no. 12: 2172. https://doi.org/10.3390/vaccines10122172
APA StyleSerra, F. E., Rosa Junior, E. R., de Rossi, P., Francisco, R. P. V., & Rodrigues, A. S. (2022). COVID-19: Impact of Original, Gamma, Delta, and Omicron Variants of SARS-CoV-2 in Vaccinated and Unvaccinated Pregnant and Postpartum Women. Vaccines, 10(12), 2172. https://doi.org/10.3390/vaccines10122172






