Side Effects of COVID-19 Vaccines Primer Doses: Experience of Saudi Healthcare Workers Participating in CoVaST-SA
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Participants
2.3. Instrument
- i.
- Demographic characteristics (age, gender, height, weight, profession, and geographic region).
- ii.
- Medical anamnesis (chronic diseases, medication, smoking and alcohol consumption).
- iii.
- COVID-19-related medical histories (type of vaccine, number of vaccine doses, dates of vaccine doses, previous infection, and date of diagnosis).
- iv.
- Vaccine side effects (local side effects, systemic side effects, onset, and duration).
2.4. Ethics
2.5. Analyses
3. Results
3.1. Demographic Characteristics
3.2. Medical and COVID-19-Related Anamnesis
3.3. Post-Vaccination Side Effects by Sex, Age, and BMI
3.4. Post-Vaccination Side Effects by Dose and Vaccination Schedule
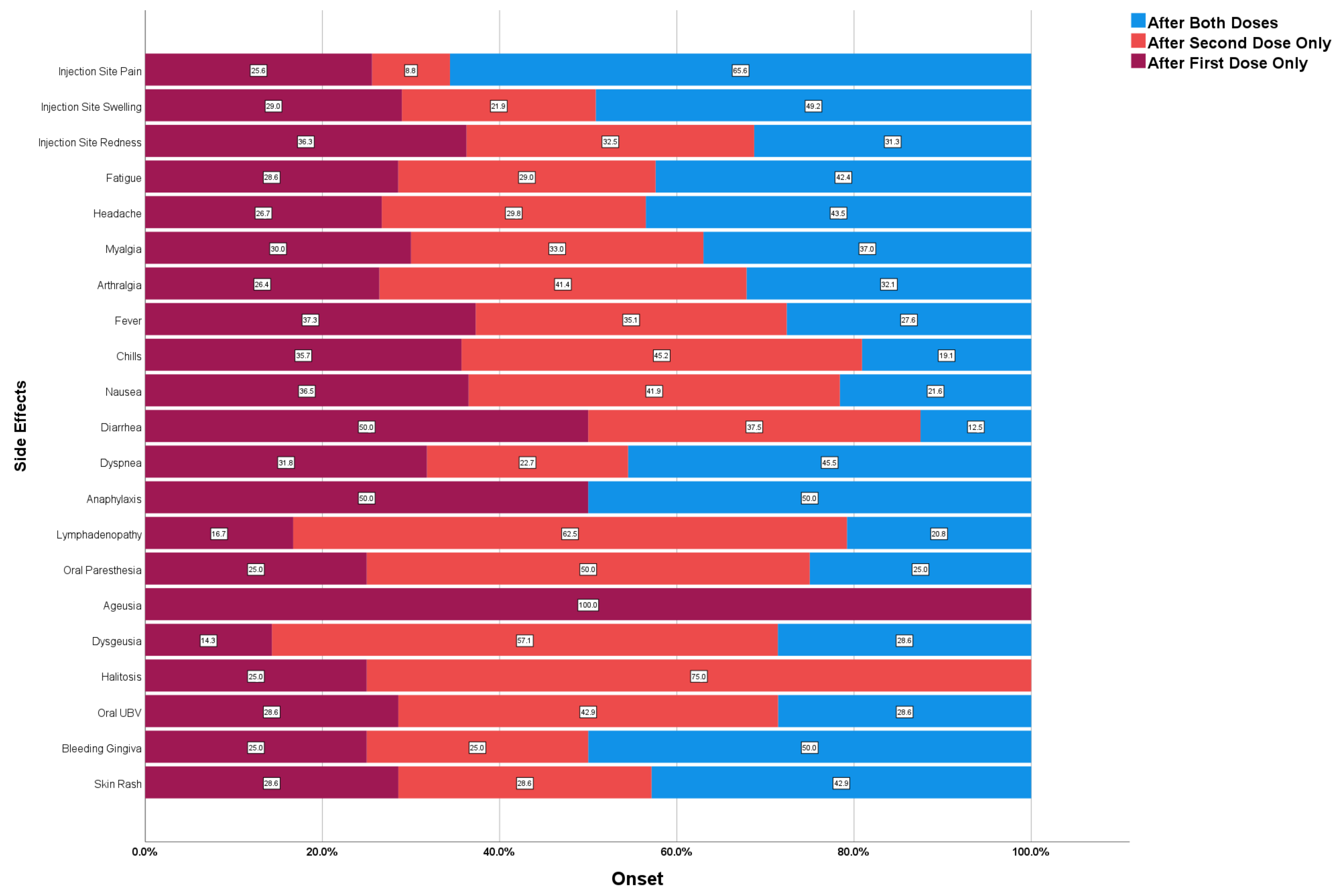
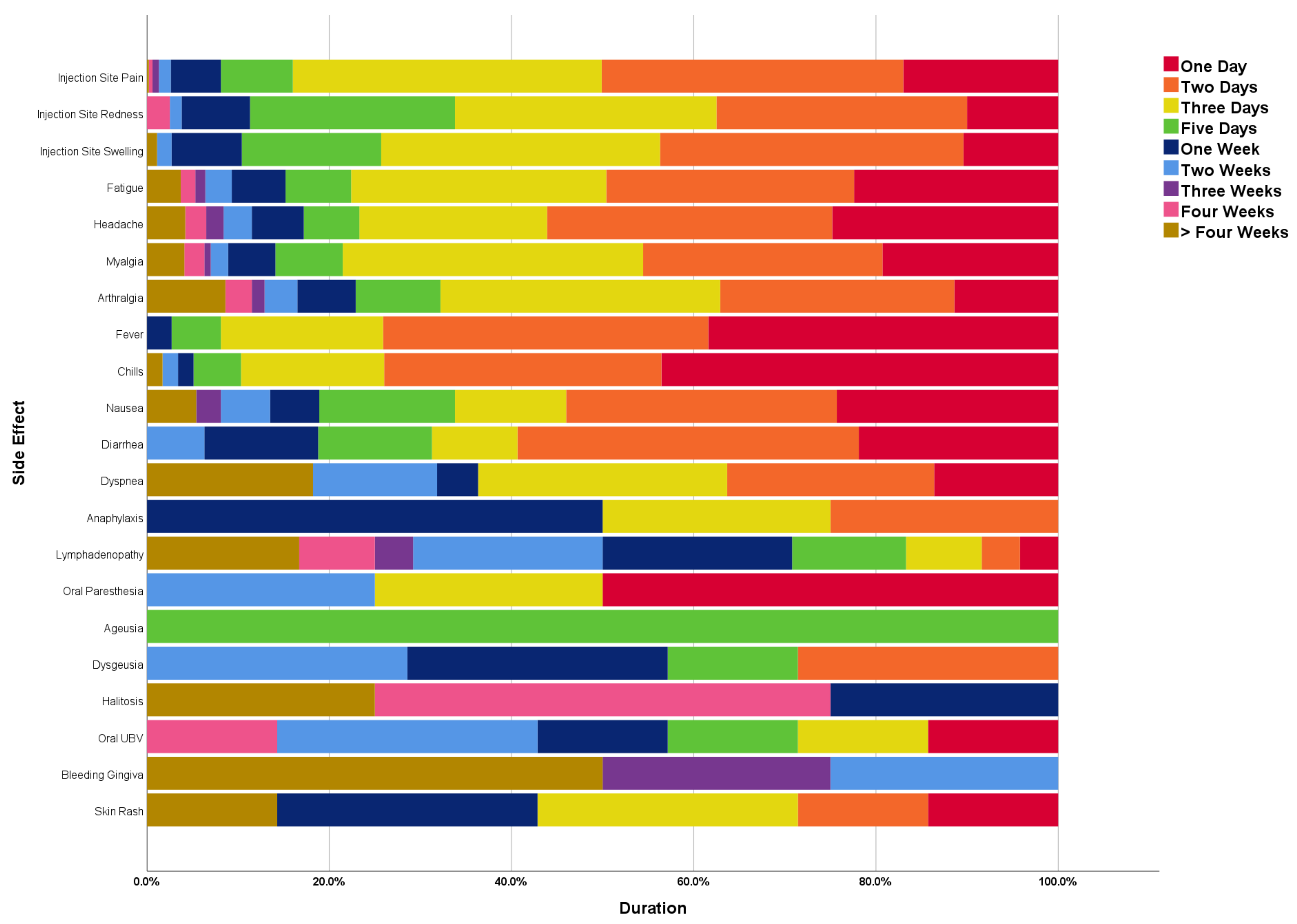
3.5. Onset and Duration of Post-Vaccination Side Effects
3.6. Post-Vaccination Medications
3.7. Risk Factors of Post-Vaccination Side Effects
4. Discussion
4.1. Strengths
4.2. Limitations
4.3. Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Siyal, F.J.; Shaikh, Z.A.; Ahmed, S.Z.; Shahid, M.A.; Agha, F.; Khoso, M.; Unar, A.A.; Unar, K.; Saleem, R.; Shahani, M.P. Anxiety among COVID-19 Physicians during the Pandemic in the Health Care Center of the Rural Region. Arch. Pharm. Pract. 2020, 11, 91–93. [Google Scholar]
- Fadel, H.H.; Ahmed, M.A.E.-R. A Combination of Immunotherapies and Micronutrients May Relieve the Severe Illness in COVID-19 Patients: Review Article. Int. J. Pharm. Phytopharm. Res. 2020, 10, 8–21. [Google Scholar]
- World Health Organization (WHO). Advice for the Public. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public (accessed on 28 October 2022).
- Centers for Disease Control and Prevention (CDC). CDC Streamlines COVID-19 Guidance to Help the Public Better Protect Themselves and Understand Their Risk. Available online: https://www.cdc.gov/media/releases/2022/p0811-covid-guidance.html (accessed on 28 October 2022).
- Orenstein, W.A.; Ahmed, R. Simply Put: Vaccination Saves Lives. Proc. Natl. Acad. Sci. USA 2017, 114, 4031–4033. [Google Scholar] [CrossRef] [PubMed]
- Davis, T.C.; Fredrickson, D.D.; Arnold, C.L.; Cross, J.T.; Humiston, S.G.; Green, K.W.; Bocchini, J.A.J. Childhood Vaccine Risk/Benefit Communication in Private Practice Office Settings: A National Survey. Pediatrics 2001, 107, E17. [Google Scholar] [CrossRef]
- Bond, L.; Nolan, T.; Pattison, P.; Carlin, J. Vaccine Preventable Diseases and Immunisations: A Qualitative Study of Mothers? Perceptions of Severity, Susceptibility, Benefits and Barriers. Aust. N. Z. J. Public Health 1998, 22, 441–446. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, N.E.; Eskola, J.; Liang, X.; Chaudhuri, M.; Dube, E.; Gellin, B.; Goldstein, S.; Larson, H.; Manzo, M.L.; Reingold, A.; et al. Vaccine Hesitancy: Definition, Scope and Determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- Alabdulla, M.; Reagu, S.M.; Al-Khal, A.; Elzain, M.; Jones, R.M. COVID-19 Vaccine Hesitancy and Attitudes in Qatar: A National Cross-Sectional Survey of a Migrant-Majority Population. Influenza Other Respir. Viruses 2021, 15, 361–370. [Google Scholar] [CrossRef]
- Alibrahim, J.; Awad, A. COVID-19 Vaccine Hesitancy among the Public in Kuwait: A Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2021, 18, 8836. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Ten Threats to Global Health in 2019. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 7 May 2021).
- Kaur, S.P.; Gupta, V. COVID-19 Vaccine: A Comprehensive Status Report. Virus Res. 2020, 288, 198114. [Google Scholar] [CrossRef]
- Dal-Ré, R.; Caplan, A.L.; Gluud, C.; Porcher, R. Ethical and Scientific Considerations Regarding the Early Approval and Deployment of a COVID-19 Vaccine. Ann. Intern. Med. 2021, 174, 258–260. [Google Scholar] [CrossRef]
- Tumban, E. Lead SARS-CoV-2 Candidate Vaccines: Expectations from Phase III Trials and Recommendations Post-Vaccine Approval. Viruses 2021, 13, 54. [Google Scholar] [CrossRef] [PubMed]
- Voysey, M.; Clemens, S.A.C.; Madhi, S.A.; Weckx, L.Y.; Folegatti, P.M.; Aley, P.K.; Angus, B.; Baillie, V.L.; Barnabas, S.L.; Bhorat, Q.E.; et al. Safety and Efficacy of the ChAdOx1 NCoV-19 Vaccine (AZD1222) against SARS-CoV-2: An Interim Analysis of Four Randomised Controlled Trials in Brazil, South Africa, and the UK. Lancet 2021, 397, 99–111. [Google Scholar] [CrossRef]
- Centres for Diseases Control and Prevention (CDC). Reactions and Adverse Events of the Pfizer-BioNTech COVID-19 Vaccine; Centres for Diseases Control and Prevention: Atlanta, GA, USA, 2021. [Google Scholar]
- Ministry of Health—Kingdom of Saudi Arabia (MOH-KSA). COVID-19 Vaccine. Available online: https://www.moh.gov.sa/en/awarenessplateform/VariousTopics/Pages/COVID-19Vaccine.aspx (accessed on 1 August 2022).
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Pérez Marc, G.; Moreira, E.D.; Zerbini, C.; et al. Safety and Efficacy of the BNT162b2 MRNA COVID-19 Vaccine. N. Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef]
- Carli, G.; Nichele, I.; Ruggeri, M.; Barra, S.; Tosetto, A. Deep Vein Thrombosis (DVT) Occurring Shortly after the Second Dose of MRNA SARS-CoV-2 Vaccine. Intern. Emerg. Med. 2021, 16, 803–804. [Google Scholar] [CrossRef] [PubMed]
- Harvard Humanitarian Initiative. Welcome to KoBoToolbox. Available online: https://support.kobotoolbox.org/welcome.html (accessed on 4 January 2022).
- El-Shitany, N.A.; Harakeh, S.; Badr-Eldin, S.M.; Bagher, A.M.; Eid, B.G.; Almukadi, H.S.; Alghamdi, B.S.; Alahmadi, A.A.; Hassan, N.A.; Sindi, N.; et al. Minor to Moderate Side Effects of Pfizer-BioNTech COVID-19 Vaccine among Saudi Residents: A Retrospective Cross-Sectional Study. Int. J. Gen. Med. 2021, 14, 1389–1401. [Google Scholar] [CrossRef]
- Ahsan, W.; Syed, N.K.; Alsraeya, A.A.; Alhazmi, H.A.; Najmi, A.; Al Bratty, M.; Javed, S.; Makeen, H.A.; Meraya, A.M.; Albarraq, A.A.; et al. Post-Vaccination Survey for Monitoring the Side Effects Associated with COVID-19 Vaccines among Healthcare Professionals of Jazan Province, Saudi Arabia. Saudi Med. J. 2021, 42, 1341–1352. [Google Scholar] [CrossRef]
- Darraj, M.A.; Al-Mekhlafi, H.M. Prospective Evaluation of Side-Effects Following the First Dose of Oxford/AstraZeneca COVID-19 Vaccine among Healthcare Workers in Saudi Arabia. Vaccines 2022, 10, 223. [Google Scholar] [CrossRef]
- Mohammed, R.A.; Garout, R.M.; Wahid, S.; Ayub, F.; ZinAlddin, L.M.F.; Sultan, I. A Survey on the Side Effects of Pfizer/BioNTech COVID-19 Vaccine among Vaccinated Adults in Saudi Arabia. Cureus 2021, 13, e19222. [Google Scholar] [CrossRef]
- Alghamdi, A.; Ibrahim, A.; Almutairi, R.; Joseph, M.; Alghamdi, G.; Alhamza, A. A Cross-Sectional Survey of Side Effects after COVID-19 Vaccination in Saudi Arabia: Male versus Female Outcomes. J. Adv. Pharm. Educ. Res. 2021, 11, 51–56. [Google Scholar] [CrossRef]
- Alzarea, A.I.; Khan, Y.H.; Alatawi, A.D.; Alanazi, A.S.; Alzarea, S.I.; Butt, M.H.; Almalki, Z.S.; Alahmari, A.K.; Mallhi, T.H.; Alzarea, A.I.; et al. Surveillance of Post-Vaccination Side Effects of COVID-19 Vaccines among Saudi Population: A Real-World Estimation of Safety Profile. Vaccines 2022, 10, 924. [Google Scholar] [CrossRef]
- Alamer, E.; Alhazmi, A.; Qasir, N.A.; Alamer, R.; Areeshi, H.; Gohal, G.; Qadri, M.; Hashem, A.M.; Algaissi, A. Side Effects of COVID-19 Pfizer-BioNTech MRNA Vaccine in Children Aged 12–18 Years in Saudi Arabia. Vaccines 2021, 9, 1297. [Google Scholar] [CrossRef] [PubMed]
- Riad, A.; Pokorná, A.; Attia, S.; Klugarová, J.; Koščík, M.; Klugar, M. Prevalence of COVID-19 Vaccine Side Effects among Healthcare Workers in the Czech Republic. J. Clin. Med. 2021, 10, 1428. [Google Scholar] [CrossRef] [PubMed]
- Riad, A.; Hocková, B.; Kantorová, L.; Slávik, R.; Spurná, L.; Stebel, A.; Havriľak, M.; Klugar, M. Side Effects of MRNA-Based COVID-19 Vaccine: Nationwide Phase IV Study among Healthcare Workers in Slovakia. Pharmaceuticals 2021, 14, 873. [Google Scholar] [CrossRef] [PubMed]
- Klugar, M.; Riad, A.; Mekhemar, M.; Conrad, J.; Buchbender, M.; Howaldt, H.-P.; Attia, S. Side Effects of MRNA-Based and Viral Vector-Based COVID-19 Vaccines among German Healthcare Workers. Biology 2021, 10, 752. [Google Scholar] [CrossRef] [PubMed]
- Yesuf, E.A.; Riad, A.; Sofi-Mahmudi, A.; Sudhakar, M.; Mekonnen, A.; Endalkachew, S.; Mama, F.; Muhidin, S.; Ayele, B.; Yahya, M.; et al. Self-Reported Side Effects of the Oxford AstraZeneca COVID-19 Vaccine among Healthcare Workers in Ethiopia, Africa: A Cross-Sectional Study. Front. Public Health 2022, 10, 937794. [Google Scholar] [CrossRef]
- Riad, A.; Sağıroğlu, D.; Üstün, B.; Pokorná, A.; Klugarová, J.; Attia, S.; Klugar, M. Prevalence and Risk Factors of CoronaVac Side Effects: An Independent Cross-Sectional Study among Healthcare Workers in Turkey. J. Clin. Med. 2021, 10, 2629. [Google Scholar] [CrossRef] [PubMed]
- Dziedzic, A.; Riad, A.; Attia, S.; Klugar, M.; Tanasiewicz, M. Self-Reported Adverse Events of COVID-19 Vaccines in Polish Healthcare Workers and Medical Students. Cross-Sectional Study and Pooled Analysis of CoVaST Project Results in Central Europe. J. Clin. Med. 2021, 10, 5338. [Google Scholar] [CrossRef]
- Lounis, M.; Rais, M.A.; Bencherit, D.; Aouissi, H.A.; Oudjedi, A.; Klugarová, J.; Pokorná, A.; Klugar, M.; Riad, A. Side Effects of COVID-19 Inactivated Virus versus Adenoviral Vector Vaccines: Experience of Algerian Healthcare Workers. Front. Public Health 2022, 10, 896343. [Google Scholar] [CrossRef]
- Green, M.S.; Peer, V.; Magid, A.; Hagani, N.; Anis, E.; Nitzan, D. Gender Differences in Adverse Events Following the Pfizer-BioNTech COVID-19 Vaccine. Vaccines 2022, 10, 233. [Google Scholar] [CrossRef]
- Green, M.S.; Nitzan, D.; Schwartz, N.; Niv, Y.; Peer, V. Sex Differences in the Case-Fatality Rates for COVID-19—A Comparison of the Age-Related Differences and Consistency over Seven Countries. PLoS ONE 2021, 16, e0250523. [Google Scholar] [CrossRef]
- Jacobsen, H.; Klein, S.L. Sex Differences in Immunity to Viral Infections. Front. Immunol. 2021, 12, 3483. [Google Scholar] [CrossRef] [PubMed]
- Klein, S.L.; Pekosz, A. Sex-Based Biology and the Rational Design of Influenza Vaccination Strategies. J. Infect. Dis. 2014, 209, S114. [Google Scholar] [CrossRef] [PubMed]
- Flanagan, K.L.; Fink, A.L.; Plebanski, M.; Klein, S.L. Sex and Gender Differences in the Outcomes of Vaccination over the Life Course. Annu. Rev. Cell Dev. Biol. 2017, 33, 577–599. [Google Scholar] [CrossRef]
- Chen, J.; Cai, Y.; Chen, Y.; Williams, A.P.; Gao, Y.; Zeng, J. Nervous and Muscular Adverse Events after COVID-19 Vaccination: A Systematic Review and Meta-analysis of Clinical Trials. Vaccines 2021, 9, 939. [Google Scholar] [CrossRef]
- Walsh, E.E.; Frenck, R.W.; Falsey, A.R.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Neuzil, K.; Mulligan, M.J.; Bailey, R.; et al. Safety and Immunogenicity of Two RNA-Based COVID-19 Vaccine Candidates. N. Engl. J. Med. 2020, 383, 2439–2450. [Google Scholar] [CrossRef]
- Ledgerwood, J.E.; Pierson, T.C.; Hubka, S.A.; Desai, N.; Rucker, S.; Gordon, I.J.; Enama, M.E.; Nelson, S.; Nason, M.; Gu, W.; et al. A West Nile Virus DNA Vaccine Utilising a Modified Promoter Induces Neutralizing Antibody in Younger and Older Healthy Adults in a Phase I Clinical Trial. J. Infect. Dis. 2011, 203, 1396–1404. [Google Scholar] [CrossRef]
- Iguacel, I.; Maldonado, A.L.; Luna Ruiz-Cabello, A.; Casaus, M.; Moreno, L.A.; Martínez-Jarreta, B.; Apostolopoulos, V.; Homaira, N. Association between COVID-19 Vaccine Side Effects and Body Mass Index in Spain. Vaccines 2021, 9, 1321. [Google Scholar] [CrossRef]
- Zare, H.; Rezapour, H.; Mahmoodzadeh, S.; Fereidouni, M. Prevalence of COVID-19 Vaccines (Sputnik V, AZD-1222, and Covaxin) Side Effects among Healthcare Workers in Birjand City, Iran. Int. Immunopharmacol. 2021, 101, 108351. [Google Scholar] [CrossRef]
- Pellini, R.; Venuti, A.; Pimpinelli, F.; Abril, E.; Blandino, G.; Campo, F.; Conti, L.; de Virgilio, A.; de Marco, F.; Gino Di Domenico, E.; et al. Obesity May Hamper SARS-CoV-2 Vaccine Immunogenicity. medRxiv 2021. Preprint. [Google Scholar] [CrossRef]
- Andrzejczak-Grządko, S.; Czudy, Z.; Donderska, M. Side Effects after COVID-19 Vaccinations among Residents of Poland. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 4418–4421. [Google Scholar] [CrossRef]
- Rzymski, P.; Sikora, D.; Zeyland, J.; Poniedziałek, B.; Kiedik, D.; Falfushynska, H.; Fal, A. Frequency and Nuisance Level of Adverse Events in Individuals Receiving Homologous and Heterologous COVID-19 Booster Vaccine. Vaccines 2022, 10, 754. [Google Scholar] [CrossRef] [PubMed]
- Costa Clemens, S.A.; Weckx, L.; Clemens, R.; Almeida Mendes, A.V.; Ramos Souza, A.; Silveira, M.B.V.; da Guarda, S.N.F.; de Nobrega, M.M.; de Moraes Pinto, M.I.; Gonzalez, I.G.S.; et al. Heterologous versus Homologous COVID-19 Booster Vaccination in Previous Recipients of Two Doses of CoronaVac COVID-19 Vaccine in Brazil (RHH-001): A Phase 4, Non-Inferiority, Single Blind, Randomised Study. Lancet 2022, 399, 521–529. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, T.; Klemis, V.; Schub, D.; Mihm, J.; Hielscher, F.; Marx, S.; Abu-Omar, A.; Schneitler, S.; Becker, S.L.; Gärtner, B.C.; et al. Immunogenicity and Reactogenicity of a Heterologous COVID-19 Prime-Boost Vaccination Compared with Homologous Vaccine Regimens. Nat. Med. 2021, 27, 1530–1535. [Google Scholar] [CrossRef] [PubMed]
- Ooi, E.E.; Dhar, A.; Petruschke, R.; Locht, C.; Buchy, P.; Low, J.G.H. Use of Analgesics/Antipyretics in the Management of Symptoms Associated with COVID-19 Vaccination. NPJ Vaccines 2022, 7, 31. [Google Scholar] [CrossRef] [PubMed]
- Sah, R.; Shrestha, S.; Mehta, R.; Sah, S.K.; Raaban, A.A.; Dharma, K.; Rodriguez-Morales, A.J. AZD1222 (Covishield) Vaccination for COVID-19: Experiences, Challenges, and Solutions in Nepal. Travel. Med. Infect. Dis. 2021, 40, 101989. [Google Scholar] [CrossRef] [PubMed]
- Serwaa, D.; Osei-Boakye, F.; Nkansah, C.; Ahiatrogah, S.; Lamptey, E.; Abdulai, R.; Antwi, M.H.; Wirekoh, E.Y.; Owusu, E.; Buckman, T.A.; et al. Non-Life-Threatening Adverse Reactions from COVID-19 vaccine; a Cross-Sectional Study with Self-Reported Symptoms among Ghanaian Healthcare Workers. Hum. Vaccines Immunother. 2021, 17, 3881–3886. [Google Scholar] [CrossRef] [PubMed]
| Variable | Outcome | Female (n = 729) | Male (n = 310) | Total (n = 1039) | Sig. |
|---|---|---|---|---|---|
| Age | ≤34 years old | 387 (53.2%) | 133 (42.9%) | 520 (50.1%) | <0.002 |
| >34 years old | 341 (46.8%) | 177 (57.1%) | 518 (49.9%) | ||
| µ ± SD | 36.25 ± 18.64 | 36.99 ± 8.86 | 36.47 ± 16.34 | 0.017 | |
| Profession | M.D. | 309 (42.4%) | 151 (48.7%) | 460 (44.3%) | 0.060 |
| D.D.S. | 15 (2.1%) | 9 (2.9%) | 24 (2.3%) | 0.406 | |
| R.N. | 200 (27.4%) | 43 (13.9%) | 243 (23.4%) | <0.001 | |
| Pharmacist | 18 (2.5%) | 17 (5.5%) | 35 (3.4%) | 0.014 | |
| Physiotherapist | 6 (0.8%) | 2 (0.6%) | 8 (0.8%) | 1.000 * | |
| Other | 181 (24.8%) | 88 (28.4%) | 269 (25.9%) | 0.231 | |
| BMI | Underweight (<18.5) | 32 (4.4%) | 0 (0%) | 32 (3.1%) | <0.001 |
| Normal (18.5–24.9) | 342 (47.2%) | 102 (33%) | 444 (42.9%) | <0.001 | |
| Overweight (25–29.9) | 237 (32.7%) | 121 (39.2%) | 358 (34.6%) | 0.045 | |
| Obese (30–34.9) | 74 (10.2%) | 58 (18.8%) | 132 (12.8%) | <0.001 | |
| Extremely Obese (>35) | 40 (5.5%) | 28 (9.1%) | 68 (6.6%) | 0.035 | |
| µ ± SD | 25.59 ± 5.75 | 27.78 ± 5.13 | 26.24 ± 5.66 | <0.001 | |
| Region | Eastern | 670 (91.9%) | 280 (90.3%) | 950 (91.4%) | 0.404 |
| Central | 38 (5.2%) | 23 (7.4%) | 61 (5.9%) | 0.166 | |
| Western | 15 (2.1%) | 4 (1.3%) | 19 (1.8%) | 0.461 | |
| Northern | 2 (0.3%) | 1 (0.3%) | 3 (0.3%) | 1.000 * | |
| Southern | 4 (0.5%) | 2 (0.6%) | 6 (0.6%) | 1.000 * |
| Variable | Outcome | Sex | Sig. | Age | Sig. | BMI | Sig. | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Female (n = 729) | Male (n = 310) | ≤34 years (n = 520) | >34 years (n = 518) | Non-Obese (n = 834) | Obese (n = 200) | ||||||
| Local SE | Injection Site Pain | 589 (80.8%) | 236 (76.1%) | 0.089 | 438 (84.2%) | 386 (74.5%) | <0.001 | 674 (80.8%) | 147 (73.5%) | 0.022 | |
| Injection Site Swelling | 151 (20.7%) | 32 (10.3%) | <0.001 | 87 (16.7%) | 96 (18.5%) | 0.446 | 145 (17.4%) | 38 (19%) | 0.591 | ||
| Injection Site Redness | 69 (9.5%) | 11 (3.5%) | 0.001 | 35 (6.7%) | 45 (8.7%) | 0.237 | 59 (7.1%) | 21 (10.5%) | 0.103 | ||
| Total | 617 (84.6%) | 244 (78.7%) | 0.020 | 455 (87.5%) | 405 (78.2%) | <0.001 | 701 (84.1%) | 156 (78%) | 0.041 | ||
| Systemic SE | Fatigue | 261 (35.8%) | 114 (36.8%) | 0.765 | 189 (36.3%) | 185 (35.7%) | 0.832 | 303 (36.3%) | 71 (35.5%) | 0.826 | |
| Headache | 201 (27.6%) | 61 (19.7%) | 0.007 | 139 (26.7%) | 123 (23.7%) | 0.268 | 218 (26.1%) | 43 (21.5%) | 0.175 | ||
| Myalgia | 191 (26.2%) | 79 (25.5%) | 0.810 | 135 (26%) | 135 (26.1%) | 0.971 | 225 (27%) | 42 (21%) | 0.083 | ||
| Arthralgia | 102 (14%) | 38 (12.3%) | 0.454 | 69 (13.3%) | 71 (13.7%) | 0.837 | 118 (14.1%) | 22 (11%) | 0.242 | ||
| Fever | 130 (17.8%) | 55 (17.7%) | 0.972 | 98 (18.8%) | 87 (16.8%) | 0.388 | 151 (18.1%) | 32 (16%) | 0.483 | ||
| Chills | 83 (11.4%) | 32 (10.3%) | 0.617 | 65 (12.5%) | 50 (9.7%) | 0.144 | 98 (11.8%) | 17 (8.5%) | 0.189 | ||
| Nausea | 63 (8.6%) | 11 (3.5%) | 0.003 | 37 (7.1%) | 37 (7.1%) | 0.986 | 62 (7.4%) | 12 (6%) | 0.480 | ||
| Diarrhoea | 25 (3.4%) | 7 (2.3%) | 0.317 | 12 (2.3%) | 20 (3.9%) | 0.148 | 25 (3%) | 7 (3.5%) | 0.713 | ||
| Dyspnea | 18 (2.5%) | 4 (1.3%) | 0.227 | 10 (1.9%) | 12 (2.3%) | 0.660 | 19 (2.3%) | 3 (1.5%) | 0.784 | ||
| Anaphylaxis | 3 (0.4%) | 1 (0.3%) | 1.000 * | 1 (0.2%) | 3 (0.6%) | 0.373 * | 4 (0.5%) | 0 (0%) | 1.000 * | ||
| Lymphadenopathy | 21 (2.9%) | 3 (1%) | 0.060 | 5 (1%) | 19 (3.7%) | 0.004 | 20 (2.4%) | 4 (2%) | 1.000 * | ||
| Oral Paresthesia | 8 (1.1%) | 0 (0%) | 0.114 * | 4 (0.8%) | 4 (0.8%) | 1.000 * | 6 (0.7%) | 2 (1%) | 0.656 * | ||
| Ageusia | 1 (0.1%) | 0 (0%) | 1.000 * | 0 (0%) | 1 (0.2%) | 0.499 * | 1 (0.1%) | 0 (0%) | 1.000 * | ||
| Dysgeusia | 7 (1%) | 0 (0%) | 0.111 * | 3 (0.6%) | 4 (0.8%) | 0.725 * | 6 (0.7%) | 1 (0.5%) | 1.000 * | ||
| Halitosis | 3 (0.4%) | 1 (0.3%) | 1.000 * | 1 (0.2%) | 3 (0.6%) | 0.373 * | 4 (0.5%) | 0 (0%) | 1.000 * | ||
| Oral UBV | 6 (0.8%) | 1 (0.3%) | 0.681 * | 3 (0.6%) | 4 (0.8%) | 0.725 * | 4 (0.5%) | 3 (1.5%) | 0.136 * | ||
| Bleeding Gingiva | 4 (0.5%) | 0 (0%) | 0.324 * | 1 (0.2%) | 3 (0.6%) | 0.373 * | 4 (0.5%) | 0 (0%) | 1.000 * | ||
| Skin Rash | 6 (0.8%) | 1 (0.3%) | 0.681 * | 6 (1.2%) | 1 (0.2%) | 0.124 * | 7 (0.8%) | 0 (0%) | 0.357 * | ||
| Total | 390 (53.5%) | 153 (49.4%) | 0.221 | 275 (52.9%) | 267 (51.5%) | 0.666 | 441 (52.9%) | 99 (49.5%) | 0.390 | ||
| Variable | Outcome | First Dose | Sig. | Second Dose | Sig. | Schedule | Sig. | Total (n = 1039) | |||
| mRNA (n = 759) | Vector (n = 280) | mRNA (n = 793) | Vector (n = 132) | Homologous (n = 786) | Heterologous (n = 139) | ||||||
| Local SE | Injection Site Pain | 624 (82.2%) | 201 (71.8%) | <0.001 | 646 (81.5%) | 98 (74.2%) | 0.053 | 641 (81.6%) | 103 (74.1%) | 0.041 | 825 (79.4%) |
| Injection Site Swelling | 141 (18.6%) | 42 (15%) | 0.179 | 140 (17.7%) | 25 (18.9%) | 0.721 | 148 (18.8%) | 17 (12.2%) | 0.061 | 183 (17.6%) | |
| Injection Site Redness | 59 (7.8%) | 21 (7.5%) | 0.883 | 58 (7.3%) | 14 (10.6%) | 0.191 | 63 (8%) | 9 (6.5%) | 0.532 | 80 (7.7%) | |
| Total | 650 (85.6%) | 211 (75.4%) | <0.001 | 673 (84.9%) | 105 (79.5%) | 0.121 | 670 (85.2%) | 108 (77.7%) | 0.025 | 861 (82.9%) | |
| Systemic SE | Fatigue | 256 (33.7%) | 119 (42.5%) | 0.009 | 285 (35.9%) | 54 (40.9%) | 0.273 | 288 (36.6%) | 51 (36.7%) | 0.991 | 375 (36.1%) |
| Headache | 171 (22.5%) | 91 (32.5%) | 0.001 | 193 (24.3%) | 41 (31.1%) | 0.100 | 188 (23.9%) | 46 (33.1%) | 0.022 | 262 (25.2%) | |
| Myalgia | 178 (23.5%) | 92 (32.9%) | 0.002 | 203 (25.6%) | 40 (30.3%) | 0.256 | 199 (25.3%) | 44 (31.7%) | 0.118 | 270 (26%) | |
| Arthralgia | 86 (11.3%) | 54 (19.3%) | <0.001 | 99 (12.5%) | 26 (19.7%) | 0.025 | 101 (12.8%) | 24 (17.3%) | 0.160 | 140 (13.5%) | |
| Fever | 108 (14.2%) | 77 (27.5%) | <0.001 | 133 (16.8%) | 36 (27.3%) | 0.004 | 132 (16.8%) | 37 (26.6%) | 0.006 | 185 (17.8%) | |
| Chills | 69 (9.1%) | 46 (16.4%) | <0.001 | 82 (10.3%) | 20 (15.2%) | 0.102 | 83 (10.6%) | 19 (13.7%) | 0.281 | 115 (11.1%) | |
| Nausea | 48 (6.3%) | 26 (9.3%) | 0.100 | 52 (6.6%) | 13 (9.8%) | 0.171 | 48 (6.1%) | 17 (12.2%) | 0.009 | 74 (7.1%) | |
| Diarrhoea | 20 (2.6%) | 12 (4.3%) | 0.172 | 21 (2.6%) | 8 (6.1%) | 0.054 * | 23 (2.9%) | 6 (4.3%) | 0.424 * | 32 (3.1%) | |
| Dyspnea | 13 (1.7%) | 9 (3.2%) | 0.136 | 14 (1.8%) | 5 (3.8%) | 0.173 * | 16 (2%) | 3 (2.2%) | 1.000 * | 22 (2.1%) | |
| Anaphylaxis | 4 (0.5%) | 0 (0%) | 0.579 * | 3 (0.4%) | 0 (0%) | 1.000 * | 3 (0.4%) | 0 (0%) | 1.000 * | 4 (0.4%) | |
| Lymphadenopathy | 19 (2.5%) | 5 (1.8%) | 0.494 | 20 (2.5%) | 1 (0.8%) | 0.342 * | 18 (2.3%) | 3 (2.2%) | 1.000 * | 24 (2.3%) | |
| Oral Paresthesia | 7 (0.9%) | 1 (0.4%) | 0.690 * | 8 (1%) | 0 (0%) | 0.610 * | 7 (0.9%) | 1 (0.7%) | 1.000 * | 8 (0.8%) | |
| Ageusia | 0 (0%) | 1 (0.4%) | 0.269 * | 1 (0.1%) | 0 (0%) | 1.000 * | 0 (0%) | 1 (0.7%) | 0.150 * | 1 (0.1%) | |
| Dysgeusia | 6 (0.8%) | 1 (0.4%) | 0.682 * | 6 (0.8%) | 1 (0.8%) | 1.000 * | 7 (0.9%) | 0 (0%) | 0.603 * | 7 (0.7%) | |
| Halitosis | 2 (0.3%) | 2 (0.7%) | 0.295 * | 2 (0.3%) | 1 (0.8%) | 0.370 * | 2 (0.3%) | 1 (0.7%) | 0.387 * | 4 (0.4%) | |
| Oral UBV | 5 (0.7%) | 2 (0.7%) | 1.000 * | 4 (0.5%) | 1 (0.8%) | 0.538 * | 4 (0.5%) | 1 (0.7%) | 0.558 * | 7 (0.7%) | |
| Bleeding Gingiva | 3 (0.4%) | 1 (0.4%) | 1.000 * | 2 (0.3%) | 1 (0.8%) | 0.370 * | 3 (0.4%) | 0 (0%) | 1.000 * | 4 (0.4%) | |
| Skin Rash | 6 (0.8%) | 1 (0.4%) | 0.682 * | 4 (0.5%) | 1 (0.8%) | 0.538 * | 5 (0.6%) | 0 (0%) | 1.000 * | 7 (0.7%) | |
| Total | 376 (49.5%) | 167 (59.6%) | 0.004 | 411 (51.8%) | 76 (57.6%) | 0.221 | 408 (51.9%) | 79 (56.8%) | 0.284 | 543 (52.3%) | |
| Variable | Outcome | Acetaminophen (n = 594) | Ibuprofen (n = 60) | Diclofenac (n = 10) | Total (n = 649) | Sig. |
|---|---|---|---|---|---|---|
| Sex | Female | 430 (59%) | 43 (5.9%) | 8 (1.1%) | 468 (64.2%) | 0.077 |
| Male | 164 (52.9%) | 17 (5.5%) | 2 (0.6%) | 181 (58.4%) | ||
| Age Group | ≤34 years old | 304 (58.5%) | 26 (5%) | 6 (1.2%) | 331 (63.7%) | 0.451 |
| >34 years old | 290 (56%) | 34 (6.6%) | 4 (0.8%) | 318 (61.4%) | ||
| BMI | Non-obese | 485 (58.2%) | 45 (5.4%) | 10 (1.2%) | 532 (63.8%) | 0.056 |
| Obese | 106 (53%) | 14 (7%) | 0 (0%) | 113 (56.5%) | ||
| Chronic Illnesses | Yes | 116 (61.7%) | 10 (5.3%) | 1 (0.5%) | 123 (65.4%) | 0.354 |
| No | 478 (56.2%) | 50 (5.9%) | 9 (1.1%) | 526 (61.8%) | ||
| Medications | Yes | 152 (59.8%) | 13 (5.1%) | 3 (1.2%) | 166 (65.4%) | 0.274 |
| No | 442 (56.3%) | 47 (6%) | 7 (0.9%) | 483 (61.5%) | ||
| First Dose | mRNA | 402 (53%) | 35 (4.6%) | 7 (0.9%) | 443 (58.4%) | <0.001 |
| Viral Vector | 192 (68.6%) | 25 (8.9%) | 3 (1.1%) | 206 (73.6%) | ||
| Second Dose | mRNA | 443 (55.9%) | 41 (5.2%) | 7 (0.9%) | 478 (60.3%) | <0.001 |
| Viral Vector | 93 (70.5%) | 17 (12.9%) | 1 (0.8%) | 104 (78.8%) | ||
| Schedule | Homologous | 439 (55.9%) | 49 (6.2%) | 7 (0.9%) | 481 (61.2%) | 0.010 |
| Heterologous | 97 (69.8%) | 9 (6.5%) | 1 (0.7%) | 101 (72.7%) | ||
| Local SE | Injection Site Pain | 489 (59.3%) | 53 (6.4%) | 8 (1%) | 538 (65.2%) | <0.001 |
| Injection Site Swelling | 118 (64.5%) | 15 (8.2%) | 2 (1.1%) | 134 (73.2%) | <0.001 | |
| Injection Site Redness | 46 (57.5%) | 8 (10%) | 2 (2.5%) | 53 (66.3%) | 0.467 | |
| Total | 508 (59%) | 57 (6.6%) | 8 (0.9%) | 561 (65.2%) | <0.001 | |
| Systemic SE | Fatigue | 282 (75.2%) | 33 (8.8%) | 4 (1.1%) | 306 (81.6%) | <0.001 |
| Headache | 211 (80.5%) | 26 (9.9%) | 4 (1.5%) | 227 (86.6%) | <0.001 | |
| Myalgia | 203 (75.2%) | 28 (10.4%) | 3 (1.1%) | 221 (81.9%) | <0.001 | |
| Arthralgia | 104 (74.3%) | 14 (10%) | 3 (2.1%) | 118 (84.3%) | <0.001 | |
| Fever | 157 (84.9%) | 22 (11.9%) | 1 (0.5%) | 168 (90.8%) | <0.001 | |
| Chills | 100 (87%) | 15 (13%) | 1 (0.9%) | 104 (90.4%) | <0.001 | |
| Nausea | 53 (71.6%) | 5 (6.8%) | 0 (0%) | 59 (79.7%) | 0.001 | |
| Diarrhea | 23 (71.9%) | 3 (9.4%) | 1 (3.1%) | 27 (84.4%) | 0.009 | |
| Dyspnea | 15 (68.2%) | 0 (0%) | 0 (0%) | 17 (77.3%) | 0.147 | |
| Anaphylaxis | 3 (75%) | 0 (0%) | 0 (0%) | 3 (75%) | 1.000 * | |
| Lymphadenopathy | 12 (50%) | 3 (12.5%) | 0 (0%) | 17 (70.8%) | 0.392 | |
| Oral Paresthesia | 7 (87.5%) | 1 (12.5%) | 0 (0%) | 7 (87.5%) | 0.271 * | |
| Ageusia | 1 (100%) | 0 (0%) | 0 (0%) | 1 (100%) | 1.000 * | |
| Dysgeusia | 7 (100%) | 1 (14.3%) | 0 (0%) | 7 (100%) | 0.050 * | |
| Halitosis | 3 (75%) | 0 (0%) | 0 (0%) | 3 (75%) | 1.000 * | |
| Oral UBV | 4 (57.1%) | 1 (14.3%) | 0 (0%) | 5 (71.4%) | 0.717 * | |
| Bleeding Gingiva | 1 (25%) | 0 (0%) | 0 (0%) | 2 (50%) | 0.634 * | |
| Skin Rash | 4 (57.1%) | 0 (0%) | 0 (0%) | 5 (71.4%) | 0.717 * | |
| Total | 379 (69.8%) | 45 (8.3%) | 6 (1.1%) | 419 (77.2%) | <0.001 |
| Predictor | Local Side Effects | Systemic Side Effects | ||||
|---|---|---|---|---|---|---|
| B (SE) | OR (CI 95%) | Sig. | B (SE) | OR (CI 95%) | Sig. | |
| Sex: Female [n = 729] (vs. Male [n = 310]) | 0.399 (0.173) | 1.490 (1.062–2.090) | 0.021 | 0.166 (0.136) | 1.181 (0.905–1.540) | 0.221 |
| Age Group: ≤34 [n = 520] (vs. >34 y [n = 518]) | 0.669 (0.170) | 1.953 (1.400–2.725) | <0.001 | 0.054 (0.124) | 1.055 (0.827 –1.346) | 0.666 |
| BMI: non-obese [n = 834] (vs. obese [n = 200]) | 0.396 (0.195) | 1.487 (1.014–2.179) | 0.042 | 0.135 (0.158) | 1.145 (0.841–1.559) | 0.391 |
| Infection: No [n = 820] (vs. Yes [n = 219]) | 0.399 (0.189) | 1.490 (1.028–2.159) | 0.035 | 0.265 (0.152) | 1.304 (0.967–1.758) | 0.082 |
| Schedule: Homo- [n = 786] (vs. Heterologous [n = 139]) | 0.506 (0.227) | 1.658 (1.062–2.588) | 0.026 | −0.199 (0.186) | 0.820 (0.570–1.179) | 0.284 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Riad, A.; Alsaad, S.S.; Almurikhi, A.A.; Alzahrani, F.A.; Alghamdi, A.M.; Alzaid, E.H.; Klugar, M. Side Effects of COVID-19 Vaccines Primer Doses: Experience of Saudi Healthcare Workers Participating in CoVaST-SA. Vaccines 2022, 10, 2137. https://doi.org/10.3390/vaccines10122137
Riad A, Alsaad SS, Almurikhi AA, Alzahrani FA, Alghamdi AM, Alzaid EH, Klugar M. Side Effects of COVID-19 Vaccines Primer Doses: Experience of Saudi Healthcare Workers Participating in CoVaST-SA. Vaccines. 2022; 10(12):2137. https://doi.org/10.3390/vaccines10122137
Chicago/Turabian StyleRiad, Abanoub, Safa S. Alsaad, Ali A. Almurikhi, Fayez A. Alzahrani, Ali M. Alghamdi, Esra H. Alzaid, and Miloslav Klugar. 2022. "Side Effects of COVID-19 Vaccines Primer Doses: Experience of Saudi Healthcare Workers Participating in CoVaST-SA" Vaccines 10, no. 12: 2137. https://doi.org/10.3390/vaccines10122137
APA StyleRiad, A., Alsaad, S. S., Almurikhi, A. A., Alzahrani, F. A., Alghamdi, A. M., Alzaid, E. H., & Klugar, M. (2022). Side Effects of COVID-19 Vaccines Primer Doses: Experience of Saudi Healthcare Workers Participating in CoVaST-SA. Vaccines, 10(12), 2137. https://doi.org/10.3390/vaccines10122137







