Exploring Critical Factors Associated with Completion of Childhood Immunisation in the Eastern Province of Saudi Arabia
Abstract
1. Introduction
2. Literature Review
2.1. Literature Review Questions
- What are the rates of immunisation compliance in Saudi Arabia?
- What are the factors that contribute to parents’ immunisation compliance in Saudi Arabia?
2.1.1. Search Strategy
2.1.2. Inclusion Criteria
2.1.3. Exclusion Criteria
2.1.4. Search Outcomes
2.2. Findings of the Literature Review
2.2.1. Rates of Immunisation Compliance
2.2.2. Factors That Impact Completion of Childhood Immunisation
| Study (Region) | Sample Size | Age of Children | Vaccine of Inquiry | Conclusion |
|---|---|---|---|---|
| [8] (Riyadh) | 384 | <14 years | National Childhood Immunisation Programme | Most parents showed adequate confidence in the efficacy of vaccines. Only a tiny proportion showed doubts. |
| [24] (Riyadh) | 500 | 2 m–7 years | A small proportion of parents showed vaccine hesitancy. | |
| [27] (Jeddah) | 351 | <3 years | Adherence to immunisation was common but some parents reported delays. | |
| [16] (Hail region) | 467 | <5 years | Most parents demonstrated a good amount of confidence in and acceptance of vaccines. | |
| [27] (Taif) | 731 | 0–12 years | Most parents had good knowledge of and a positive attitude towards vaccines. |
2.2.3. Discussion of the Literature Review
2.3. Conclusion of the Literature Review
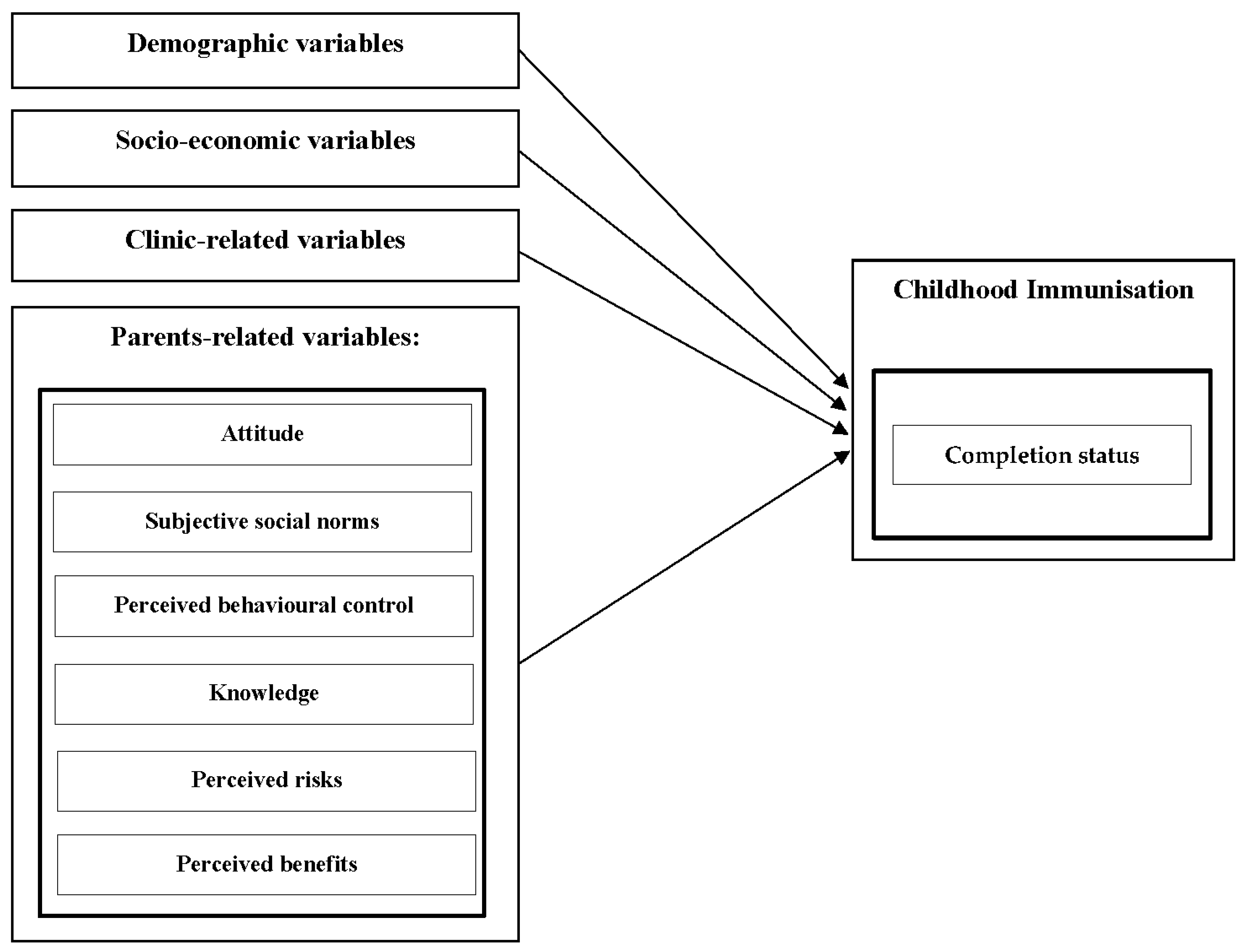
3. Conceptual Framework and Hypotheses
- Demographic Variables
- a.
- Hypothesis 1 (H1):Demographic variables (e.g., age, gender, etc.) are associated with childhood immunisation completion status.
- Socio-economic Variables
- b.
- Hypothesis 2 (H2):Socioeconomic variables (e.g., place of residence, level of education, etc.) are associated with childhood immunisation completion status.
- Clinic-related Variables
- c.
- Hypothesis 3 (H3):Clinic-related variables (e.g., distance to PHC centre, waiting time at immunisation clinic, etc.) are associated with childhood immunisation completion status.
- Parents-related Variables
- d.
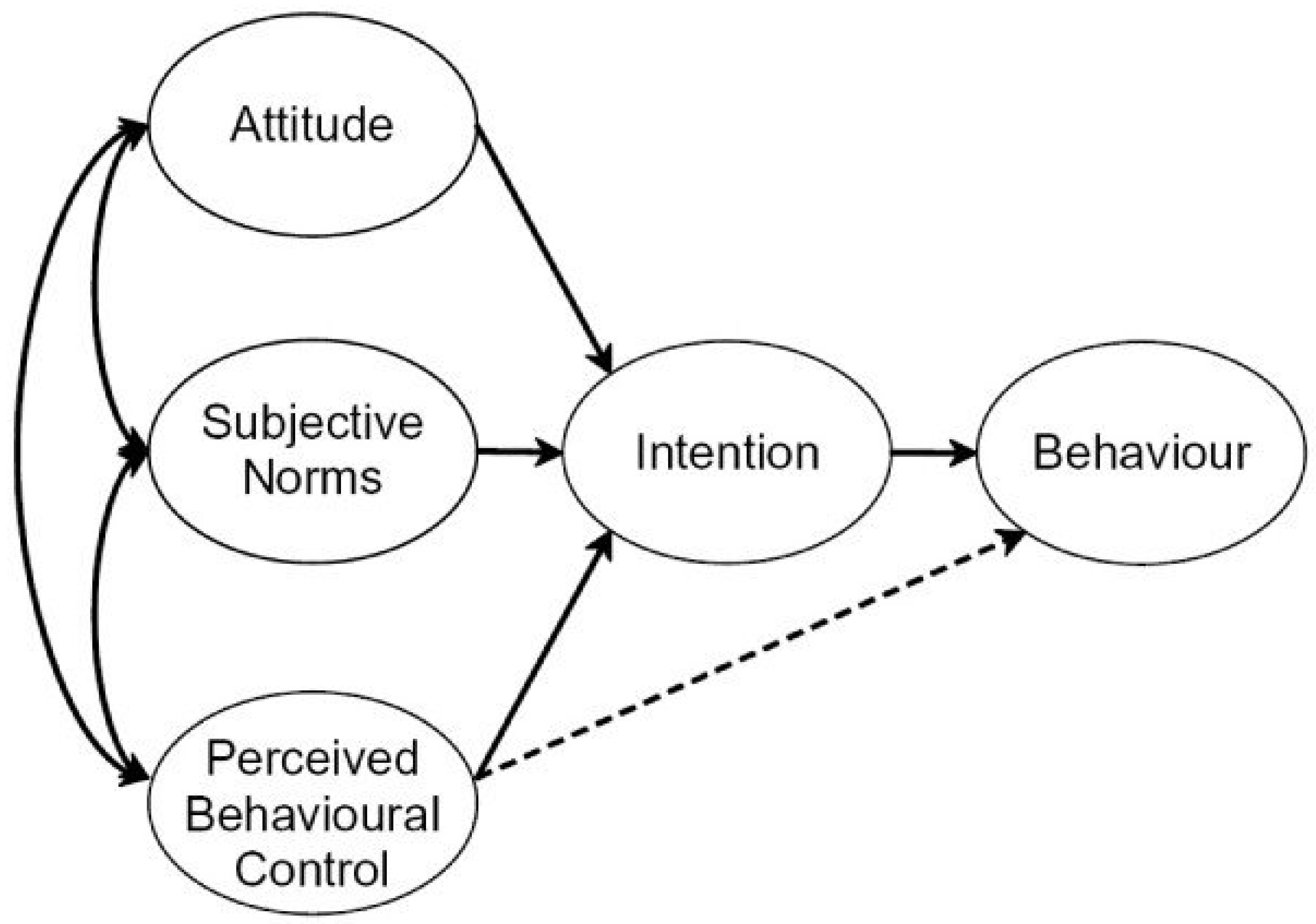
- Theory of Planned Behaviour
- Hypothesis 4 (H4):A positive attitude toward immunisation is associated with childhood immunisation completion status.
- Hypothesis 5 (H5):Subjective social norms toward immunisation are positively associated with childhood immunisation completion status.
- Hypothesis 6 (H6):Perceived behavioural control toward immunisation is positively associated with childhood immunisation completion status.
- e.
- Knowledge
- Hypothesis 7 (H7):Higher knowledge about immunisation is positively associated with childhood immunisation completion status.
- f.
- Trade-offs (Perceived Benefits and Risks)
- Hypothesis 8 (H8):Higher perceived risks of immunisation are negatively associated with childhood immunisation completion status.
- Hypothesis 9 (H9):Higher perceived benefits of immunisation are positively associated with childhood immunisation completion status.
4. Methodology
4.1. Study Area
4.2. Study Design and Sample Size Determination
4.3. Recruitment and Data Collection
4.4. Method of Data Analysis
5. Measurements
6. Results
6.1. Correlation Analysis
6.2. Hypothesis Testing and Regression Analysis
7. Discussion
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pedersen, K.B.; Holck, M.E.; Jensen, A.K.G.; Suppli, C.H.; Benn, C.S.; Krause, T.G.; Sorup, S. How are children who are delayed in the Childhood Vaccination Programme vaccinated: A nationwide register-based cohort study of Danish children aged 15–24 months and semi-structured interviews with vaccination providers. Scand. J. Public Health 2020, 48, 96–105. [Google Scholar] [CrossRef] [PubMed]
- Torres, I.; Artaza, O.; Profeta, B.; Alonso, C.; Kang, J. Realigning global health governance: WHO at a crossroads. Int. J. Equity Health 2020, 19, 186. [Google Scholar] [CrossRef] [PubMed]
- Nesti, M.M.; Goldbaum, M. Infectious diseases and daycare and preschool education. J. Pediatr. 2007, 83, 299–312. [Google Scholar] [CrossRef] [PubMed]
- Bhutta, Z.A.; Sommerfeld, J.; Lassi, Z.S.; Salam, R.A.; Das, J.K. Global burden, distribution, and interventions for infectious diseases of poverty. Infect. Dis. Poverty 2014, 3, 1–7. [Google Scholar] [CrossRef]
- Kyu, H.H.; Mumford, J.E.; Stanaway, J.D.; Barber, R.M.; Hancock, J.R.; Vos, T.; Murray, C.J.; Naghavi, M. Mortality from tetanus between 1990 and 2015: Findings from the global burden of disease study 2015. BMC Public Health 2017, 17, 1–17. [Google Scholar] [CrossRef]
- Powell-Jackson, T.; Fabbri, C.; Dutt, V.; Tougher, S.; Singh, K. Effect and cost-effectiveness of educating mothers about childhood DPT vaccination on immunisation completion status, knowledge, and perceptions in Uttar Pradesh, India: A randomised controlled trial. PLoS Med. 2018, 15, e1002519. [Google Scholar] [CrossRef] [PubMed]
- MOH. Health Awareness—Immunization (Vaccines). 2020. Available online: https://www.moh.gov.sa/en/HealthAwareness/EducationalContent/vaccination/Pages/003.aspx (accessed on 7 December 2022).
- AlGoraini, Y.M.; AlDujayn, N.N.; AlRasheed, M.A.; Bashawri, Y.E.; Alsubaie, S.S.; AlShahrani, D.A. Confidence toward vaccination as reported by parents of children admitted to a tertiary care hospital in Riyadh, Saudi Arabia: A cross sectional study. Vacunas 2020, 21, 95–104. [Google Scholar] [CrossRef]
- Bangura, J.B.; Xiao, S.; Qiu, D.; Ouyang, F.; Chen, L. Barriers to childhood immunization in sub-Saharan Africa: A systematic review. BMC Public Health 2020, 20, 1108. [Google Scholar] [CrossRef]
- Alruwaili, A.A.S.; Abo El-fetoh, N.M.; Alruwaili, T.A.S.; Alanazi, W.A.S.; Alhazmi, H.H.R.; Alanazi, N.A.B.; Alshammari, H.A.B.; Alshammari, A.A.A.; Alrwaili, A.H. Knowledge, attitude and practice of the parents regarding child vaccinations in Arar, Northern Saudi Arabia. Egypt. J. Hosp. Med. 2018, 72, 5178–5182. [Google Scholar] [CrossRef]
- Alabadi, M.; Aldawood, Z. Parents’ Knowledge, Attitude and Perceptions on Childhood Vaccination in Saudi Arabia: A Systematic Literature Review. Vaccines 2020, 8, 750. [Google Scholar] [CrossRef]
- Fernbach, A. Parental rights and decision making regarding vaccinations: Ethical dilemmas for the primary care provider. J. Am. Acad. Nurse Pract. 2011, 23, 336–345. [Google Scholar] [CrossRef] [PubMed]
- Whyte, M.D.; Whyte IV, J.; Cormier, E.; Eccles, D.W. Factors influencing parental decision making when parents choose to deviate from the standard pediatric immunization schedule. J. Community Health Nurs. 2011, 28, 204–214. [Google Scholar] [CrossRef] [PubMed]
- Benin, A.L.; Wisler-Scher, D.J.; Colson, E.; Shapiro, E.D.; Holmboe, E.S. Qualitative analysis of mothers’ decision-making about vaccines for infants: The importance of trust. Pediatrics 2006, 117, 1532–1541. [Google Scholar] [CrossRef] [PubMed]
- Fredrickson, D.D.; Davis, T.C.; Arnould, C.L.; Kennen, E.M.; Hurniston, S.G.; Cross, J.T.; Bocchini, J.A., Jr. Childhood immunization refusal: Provider and parent perceptions. Fam. Med. 2004, 36, 431–439. [Google Scholar] [PubMed]
- Alshammari, T.M.; Subaiea, G.M.; Hussain, T.; Moin, A.; Yusuff, K.B. Parental perceptions, attitudes and acceptance of childhood immunization in Saudi Arabia: A cross sectional study. Vaccine 2018, 36, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Mahrous, M.S. Key role players in health care quality: Who are they and what do they think? An experience from Saudi Arabia. East Mediterr. Health J. 2013, 19, 788–793. [Google Scholar] [CrossRef]
- Alabbad, A.A.; Alsaad, A.K.; Al Shaalan, M.A.; Alola, S.; Albanyan, E.A. Prevalence of influenza vaccine hesitancy at a tertiary care hospital in Riyadh, Saudi Arabia. J. Infect. Public Health 2018, 11, 491–499. [Google Scholar] [CrossRef]
- Rashid, A.K.M.H. Childhood immunization status related to social and educational status of parents in a peripheral northern town of Saudi Arabia. Ann. Saudi Med. 1993, 13, 335–339. [Google Scholar] [CrossRef]
- Alyami, A.R.; Alhashan, G.; Nasser, I.; Alyami, S.R.; Mardhamah, N.; Alyami, M.H.; Alyami, A.; Alqahtani, M.; Alwadei, B.M.; Alanazi, A.M. Knowledge, Beliefs and Practices of Parents towards Childhood. Egypt. J. Hosp. Med. 2018, 70, 1–7. [Google Scholar] [CrossRef]
- Alsuhaibani, M.; Alaqeel, A. Impact of the COVID-19 Pandemic on Routine Childhood Immunization in Saudi Arabia. Vaccines 2020, 8, 581. [Google Scholar] [CrossRef]
- Barchielli, B.; Cricenti, C.; Gallè, F.; Sabella, E.A.; Liguori, F.; Da Molin, G.; Liguori, G.; Orsi, G.B.; Giannini, A.M.; Ferracuti, S. Climate Changes, Natural Resources Depletion, COVID-19 Pandemic, and Russian-Ukrainian War: What Is the Impact on Habits Change and Mental Health? Int. J. Environ. Res. Public Health 2022, 19, 11929. [Google Scholar] [CrossRef] [PubMed]
- WHO. WHO Vaccine-Preventable Diseases: Monitoring System. 2019 Global Summary; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- Alsubaie, S.S.; Gosadi, I.M.; Alsaadi, B.M.; Albacker, N.B.; Bawazir, M.A.; Bin-Daud, N.; Almanie, W.B.; Alsaadi, M.M.; Alzamil, F.A. Vaccine hesitancy among Saudi parents and its determinants. Saudi Med. J. 2019, 40, 1242. [Google Scholar] [CrossRef] [PubMed]
- Rogers, K.M. Immunization Noncompliance: Gauging the Cause, Effect, and Management in the School Setting. NASN Sch. Nurse 2019, 34, 140–144. [Google Scholar] [CrossRef] [PubMed]
- Yousif, M.; Albarraq, A.A.; Abdallah, M.A.; Elbur, A. Parents’ knowledge and attitudes on childhood immunization, Taif, Saudi. J. Vaccines Vaccin 2013, 5, 2. [Google Scholar]
- Banjari, M.A.; Alamri, A.A.; Algarni, A.Y.; Abualjadayel, M.H.; Alshardi, Y.S.; Alahmadi, T.S. How often do children receive their vaccinations late, and why? Saudi Med. J. 2018, 39, 347. [Google Scholar]
- Alolayan, A.; Almotairi, B.; Alshammari, S.; Alhearri, M.; Alsuhaibani, M. Seasonal influenza vaccination among Saudi children: Parental barriers and willingness to vaccinate their children. Int. J. Environ. Res. Public Health 2019, 16, 4226. [Google Scholar] [CrossRef]
- Al-Jabban, T.M. Factors Influencing Immunisation Completion status in Childhood in Saudi Arabia. Ph.D. Thesis, University of Wales Swansea, Swansea, UK, 2002. [Google Scholar]
- Robinson, C.L.; Romero, J.R.; Kempe, A.; Pellegrini, C.; Szilagyi, P. Advisory committee on immunization practices recommended immunization schedule for children and adolescents aged 18 years or younger—United States, 2018. Morb. Mortal. Wkly. Rep. 2018, 67, 156. [Google Scholar] [CrossRef]
- Holton, A.; Weberling, B.; Clarke, C.E.; Smith, M.J. The blame frame: Media attribution of culpability about the MMR–autism vaccination scare. Health Commun. 2012, 27, 690–701. [Google Scholar] [CrossRef]
- McCoy, J.D.; Painter, J.E.; Jacobsen, K.H. Perceptions of vaccination within a Christian homeschooling community in Pennsylvania. Vaccine 2019, 37, 5770–5776. [Google Scholar] [CrossRef]
- Li, J.-Y.; Wen, T.J.; McKeever, R.; Kim, J.K. Uncertainty and negative emotions in parental decision-making on childhood vaccinations: Extending the theory of planned behavior to the context of conflicting health information. J. Health Commun. 2021, 26, 215–224. [Google Scholar]
- Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Armitage, C.J.; Conner, M. Efficacy of the theory of planned behaviour: A meta-analytic review. Br. J. Soc. Psychol. 2001, 40, 471–499. [Google Scholar] [CrossRef] [PubMed]
- Ritchie, D.; Van den Broucke, S.; Van Hal, G. The health belief model and theory of planned behavior applied to mammography screening: A systematic review and meta-analysis. Public Health Nurs. 2021, 38, 482–492. [Google Scholar] [CrossRef]
- Wiemken, T.L.; Carrico, R.M.; Kelley, R.R.; Binford, L.E.; Peyrani, P.; Ford, K.D.; Welch, V.; Ramirez, J.A. Understanding why low-risk patients accept vaccines: A socio-behavioral approach. BMC Res. Notes 2015, 8, 813. [Google Scholar] [CrossRef] [PubMed]
- Askelson, N.M.; Campo, S.; Lowe, J.B.; Smith, S.; Dennis, L.K.; Andsager, J. Using the theory of planned behavior to predict mothers’ intentions to vaccinate their daughters against HPV. J. Sch. Nurs. 2010, 26, 194–202. [Google Scholar] [CrossRef]
- Leech, N.L.; Barrett, K.C.; Morgan, G.A. IBM SPSS for Intermediate Statistics: Use and Interpretation; Routledge: New York, NY, USA, 2014. [Google Scholar]
- Wooldridge, J.M. Introductory Econometrics: A Modern Approach; Cengage Learning: Boston, MA, USA, 2015. [Google Scholar]
- Sinuraya, R.K.; Kusuma, A.S.W.; Pardoel, Z.E.; Postma, M.J.; Suwantika, A.A. Parents' Knowledge, Attitude, and Practice on Childhood Vaccination During the COVID-19 Pandemic in Indonesia. Patient Prefer. Adherence 2022, 16, 105–112. [Google Scholar] [CrossRef]
- Matta, P.; El Mouallem, R.; Akel, M.; Hallit, S.; Fadous Khalife, M.-C. Parents’ knowledge, attitude and practice towards children’s vaccination in Lebanon: Role of the parent-physician communication. BMC Public Health 2020, 20, 1–9. [Google Scholar] [CrossRef]
- Kundi, M.; Obermeier, P.; Helfert, S.; Oubari, H.; Fitzinger, S.; Yun, J.A.; Brix, M.; Rath, B. The impact of the parent-physician relationship on parental vaccine safety perceptions. Curr. Drug Saf. 2015, 10, 16–22. [Google Scholar] [CrossRef]
- Kurosky, S.K.; Davis, K.L.; Krishnarajah, G. Completion and compliance of childhood vaccinations in the United States. Vaccine 2016, 34, 387–394. [Google Scholar] [CrossRef]
- Chen, F.; He, Y.; Shi, Y. Parents’ and Guardians’ Willingness to Vaccinate Their Children against COVID-19: A Systematic Review and Meta-Analysis. Vaccines 2022, 10, 179. [Google Scholar] [CrossRef]
- Ali, M.; Ahmed, S.; Bonna, A.S.; Sarkar, A.S.; Islam, M.A.; Urmi, T.A.; Proma, T.S. Parental coronavirus disease vaccine hesitancy for children in Bangladesh: A cross-sectional study. F1000Research 2022, 11, 90. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Elam-Evans, L.D.; Hill, H.A.; Yankey, D. Employment and Socioeconomic Factors Associated with Children's Up-to-Date Vaccination Status. Clin. Pediatr. 2017, 56, 348–356. [Google Scholar] [CrossRef] [PubMed]
- Shati, A.A.; Al-Qahtani, S.M.; Alsabaani, A.A.; Mahmood, S.E.; Alqahtani, Y.A.; AlQahtani, K.M.; Aldarami, M.S.; AlAmri, F.D.; Alqahtani, A.S.; AlHadi, A.M.; et al. Perceptions of Parents towards COVID-19 Vaccination in Children, Aseer Region, Southwestern Saudi Arabia. Vaccines 2022, 10, 1222. [Google Scholar] [CrossRef] [PubMed]
- Zhang, K.C.; Fang, Y.; Cao, H.; Chen, H.; Hu, T.; Chen, Y.Q.; Zhou, X.; Wang, Z. Parental Acceptability of COVID-19 Vaccination for Children Under the Age of 18 Years: Cross-Sectional Online Survey. JMIR Pediatr. Parent 2020, 3, e24827. [Google Scholar] [CrossRef] [PubMed]
- Stockwell, M.S.; Irigoyen, M.; Martinez, R.A.; Findley, S. How parents' negative experiences at immunization visits affect child immunization status in a community in New York City. Public Health Rep. 2011, 126 (Suppl. S2), 24–32. [Google Scholar] [CrossRef]
- Daley, M.F.; Crane, L.A.; Chandramouli, V.; Beaty, B.L.; Barrow, J.; Allred, N.; Berman, S.; Kempe, A. Misperceptions about influenza vaccination among parents of healthy young children. Clin. Pediatr. 2007, 46, 408–417. [Google Scholar] [CrossRef]

| Completion Status of Childhood Immunisation | no = 29.70% yes = 70.30% | Have you completed the required immunisation for your child presented in the clinic today as of now (as per the immunisation schedule)? |
| Demographic Variables | ||
| Gender | female = 55.00%; male = 45.00% | What is your gender (parent filling this questionnaire)? |
| Age | mean = 33.65; s.d. = 7.04; min = 19; max = 60 | What is your age (parent filling this questionnaire)? |
| Age (other parent) | mean = 33.80; s.d. = 7.19; min = 19; max = 56 | What is the other parent’s age? |
| Child Age (in months) | mean = 16.33; s.d. = 11.75; min = 1; max = 96 | What is the age of your child? |
| Child Gender | female = 45.60% | What is the gender of your child? |
| Child Order | 1st–2nd = 51.80% 3rd–4th = 37.40% 5th–6th = 7.90% 7th–8th = 2.00% 9th and over = 0.80% | What’s the order of your child in the family? |
| Socio-economic Variables | ||
| Number of Children | mean = 2.72; s.d. = 1.54; min = 0; max = 9 | What is the number of children in the family? |
| Place of Residence | urban = 43.30 rural = 56.70% | What is the place of your residence? |
| Father Education | less than university = 14.40% university or higher = 85.60% | What is the highest level of education (father of child)? |
| Mother Education | less than university = 28.00% university or higher = 72.00% | What is the highest level of education (mother of child)? |
| Father Employment | student, not employed, or other = 7.10% government employee = 34.00% private sector employee = 58.90% | What is the employment status (father of child)? |
| Mother Employment | student, not employed, or other = 50.40% government employee = 31.70% private sector employee = 17.80% | What is the employment status (mother of child)? |
| Family Income | Less than 5000 SAR = 7.90% 5001–10,000 SAR = 26.90% 10,001–15, 000 SAR = 25.50% 15,001–20,000 SAR = 16.70% More than 20,000 SAR = 22.90% | What is the family of child monthly income? |
| Number of People Living in Household | mean = 4.95; s.d. = 2.31; min = 1; max = 20 | How many do people live in the household? |
| Housing Type | villa = 31.70% flat = 65.70% mud house or alike = 2.50% | Select the style of housing that the child and family live at. |
| Accommodation Type | owned = 64.30% rent = 35.70% | What is the accommodation type? |
| Clinic-related Variables | ||
| Distance to PHC Centre (in km) | mean = 2.50; s.d. = 1.41; min = 1; max = 6 | Distance to PHC centre (in kilometre). |
| Transportation Type | car = 69.40% walk = 12.70% car and walk = 17.80% | Mode of transport (traveling type). |
| Waiting Time | Less than 15 min = 15.60% 15–30 min = 42.50% 30–45 min = 19.00% 45–60 min = 12.50% More than 60 min = 10.50% | Waiting time at the immunisation clinic. |
| Clinic Rating | mean = 2.52; s.d. = 1.00; min = 1; max = 4 | How do you rate the immunisation clinic facilities? (poor; fair; good; excellent) |
| Reminder System | not available = 37.70% available = 62.30% | Immunisation Reminder System (Does your clinic send you a reminder when your child is due for their next immunisation?) |
| Parents-related Variables | ||
| Attitude | mean = 5.73; s.d. = 1.56; min = 1; max = 7 | 6 items; 7-point semantic scale |
| Social Norms | mean = 5.95; s.d. = 1.20; min = 1; max = 7 | 3 items; 7-point Likert scale |
| Behavioural Control | mean = 4.96; s.d. = 1.97; min = 1; max = 7 | 3 items; 7-point Likert scale |
| Knowledge | mean = 4.80; s.d. = 1.70; min = 1; max = 7 | 4 items; 7-point Likert scale |
| Perceived Risks | mean = 3.05; s.d. = 2.05; min = 1; max = 7 | 4 items; 7-point Likert scale |
| Perceived Benefits | mean = 5.78; s.d. = 1.49; min = 1; max = 7 | 4 items; 7-point Likert scale |
| PHC | Frequency | Percent |
|---|---|---|
| Saihat 1 | 11 | 3.1% |
| Saihat 2 | 12 | 3.4% |
| Albustan | 4 | 1.1% |
| Qudaih | 12 | 3.4% |
| Aum Alhamam | 11 | 3.1% |
| Alnasrah | 21 | 5.9% |
| Alnabiah | 2 | 0.6% |
| Albuhari | 9 | 2.5% |
| Qatif 3 | 32 | 9.1% |
| Shuwaikha | 8 | 2.3% |
| Dareen | 13 | 3.7% |
| Rabiaa | 6 | 1.7% |
| Sanabis | 15 | 4.2% |
| Tarut | 32 | 9.1% |
| Mahdood | 11 | 3.1% |
| Auwammiah | 26 | 7.4% |
| Tubi | 6 | 1.7% |
| Khuwildiah | 7 | 2.0% |
| Hilah | 11 | 3.1% |
| Malahah | 5 | 1.4% |
| Jish | 13 | 3.7% |
| Muneera | 20 | 5.7% |
| Majidiah | 17 | 4.8% |
| Qudaih 2 | 9 | 2.5% |
| Ridah | 5 | 1.4% |
| Saihat 3 | 7 | 2.0% |
| Reef | 1 | 0.3% |
| Aljaroodia | 27 | 7.6% |
| Total | 353 | 100.00% |
| Factor | |||||||
|---|---|---|---|---|---|---|---|
| α = 0.967 | α = 0.966 | α = 0.945 | α = 0.829 | α = 0.887 | α = 0.878 | ||
| Attitude 1 | (bad … good) | 0.824 | −0.162 | 0.232 | 0.066 | 0.065 | 0.177 |
| Attitude 2 | (foolish … wise) | 0.823 | −0.174 | 0.255 | 0.022 | 0.072 | 0.113 |
| Attitude 3 | (unfavourable … favourable) | 0.793 | −0.207 | 0.266 | 0.002 | 0.052 | 0.204 |
| Attitude 4 | (useless … useful) | 0.843 | −0.235 | 0.218 | −0.005 | 0.040 | 0.117 |
| Attitude 5 | (detrimental … beneficial) | 0.875 | −0.204 | 0.185 | −0.043 | 0.062 | 0.130 |
| Attitude 6 | (unhealthy … healthy) | 0.875 | −0.194 | 0.179 | −0.005 | 0.052 | 0.161 |
| Perceived Risks 1 | I am worried that immunisations might not be safe. | −0.255 | 0.878 | −0.188 | −0.010 | 0.037 | −0.053 |
| Perceived Risks 2 | I am worried that immunisations might have serious side effects. | −0.237 | 0.930 | −0.166 | −0.037 | −0.018 | −0.115 |
| Perceived Risks 3 | I am worried that immunisations might have serious future risks. | −0.203 | 0.897 | −0.177 | −0.039 | −0.013 | −0.136 |
| Perceived Risks 4 | I am worried that immunisations might not prevent infectious diseases. | −0.222 | 0.827 | −0.174 | −0.001 | 0.044 | −0.107 |
| Perceived Benefits 1 | Immunisations have a positive impact on public health. | 0.286 | −0.207 | 0.663 | 0.155 | −0.036 | 0.113 |
| Perceived Benefits 2 | Immunisations are important for the prevention of infectious diseases that can have very serious effects. | 0.372 | −0.236 | 0.777 | 0.171 | −0.025 | 0.232 |
| Perceived Benefits 3 | Immunisations are important to protect the health of our community. | 0.339 | −0.228 | 0.836 | 0.154 | 0.012 | 0.221 |
| Perceived Benefits 4 | I would feel safe if my child gets vaccinated. | 0.349 | −0.266 | 0.781 | 0.101 | 0.041 | 0.263 |
| Knowledge 1 | I have good knowledge about immunisations. | −0.085 | −0.023 | 0.012 | 0.913 | −0.013 | 0.003 |
| Knowledge 2 | I know which immunisations my child needs. | −0.073 | −0.035 | 0.062 | 0.927 | 0.003 | 0.022 |
| Knowledge 3 | Unvaccinated children are more resistant to infections diseases. | 0.153 | −0.007 | 0.321 | 0.477 | −0.036 | 0.247 |
| Knowledge 5 | Serious side effects of immunisations are very rare. | 0.100 | −0.003 | 0.246 | 0.543 | 0.000 | 0.265 |
| Perceived Behavioural Control 1 | It is completely up to me whether or not I get my children vaccinated. | 0.096 | 0.010 | 0.009 | −0.026 | 0.880 | −0.056 |
| Perceived Behavioural Control 2 | If I wanted to, I could get my children vaccinated. | 0.031 | 0.027 | −0.009 | 0.032 | 0.835 | 0.010 |
| Perceived Behavioural Control 3 | It is completely up to me if I want to get my children vaccinated. | 0.067 | −0.001 | −0.014 | −0.037 | 0.833 | −0.057 |
| Subjective Social Norms 1 | In my community, most parents like me have their children vaccinated with all the recommended vaccines. | 0.293 | −0.125 | 0.254 | 0.195 | −0.136 | 0.626 |
| Subjective Social Norms 2 | Most parents like me think that it’s important to get their children vaccinated. | 0.382 | −0.264 | 0.410 | 0.141 | 0.021 | 0.650 |
| Subjective Social Norms 3 | Most people who are important to me (family, friends) think that I should give my children the required immunisations as indicated in the national immunisation card. | 0.351 | −0.229 | 0.343 | 0.196 | −0.070 | 0.630 |
| Correlation Matrix | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 |
| 1-Completion Status of Childhood Immunisation | 1 | −0.082 | −0.008 | −0.028 | 0.058 | −0.052 | 0.025 | 0.023 | −0.069 | −0.040 | 0.065 | 0.081 | 0.078 | −0.125 * | 0.200 ** | −0.371 ** | 0.276 ** | 0.041 | 0.333 ** | 0.356 ** | −0.095 | −0.143 ** | −0.245 ** | 0.300 ** |
| 2-Gender (female) | −0.082 | 1 | −0.293 ** | 0.267 ** | −0.094 | 0.028 | −0.036 | −0.015 | −0.056 | −0.099 | −0.031 | −0.248 ** | −0.042 | 0.139 ** | −0.100 | −0.083 | 0.037 | 0.127 * | −0.160 ** | −0.056 | −0.012 | 0.131 * | 0.111 * | −0.034 |
| 3-Age | −0.008 | −0.293 ** | 1 | 0.729 ** | 0.122 * | 0.012 | 0.598 ** | 0.620 ** | 0.181 ** | −0.081 | 0.031 | 0.310 ** | 0.429** | −0.120 * | 0.120 * | 0.033 | 0.002 | −0.159 ** | −0.029 | 0.065 | −0.096 | 0.177 ** | 0.069 | 0.014 |
| 4-Age (other parent) | −0.028 | 0.267 ** | 0.729 ** | 1 | 0.063 | 0.043 | 0.556 ** | 0.610 ** | 0.199 ** | −0.158 ** | 0.049 | 0.147 ** | 0.404** | −0.035 | 0.058 | 0.032 | −0.034 | −0.107 * | −0.120 * | 0.043 | −0.106 * | 0.254 ** | 0.154 ** | −0.021 |
| 5-Child Age (in months) | 0.058 | −0.094 | 0.122 * | 0.063 | 1 | −0.007 | 0.051 | 0.115 * | 0.052 | 0.088 | 0.014 | 0.036 | 0.127* | −0.003 | 0.026 | 0.135 * | −0.019 | 0.019 | 0.023 | −0.042 | 0.154 ** | 0.008 | −0.003 | −0.033 |
| 6-Child Gender (female) | −0.052 | 0.028 | 0.012 | 0.043 | −0.007 | 1 | 0.089 | 0.027 | 0.084 | 0.020 | 0.009 | −0.017 | −0.050 | −0.012 | −0.041 | −0.073 | 0.063 | −0.016 | 0.000 | −0.013 | −0.012 | 0.097 | 0.043 | 0.005 |
| 7-Child Order | 0.025 | −0.036 | 0.598 ** | 0.556 ** | 0.051 | 0.089 | 1 | 0.788 ** | 0.203 ** | −0.123 * | −0.075 | 0.215 ** | 0.540** | −0.028 | 0.045 | −0.014 | 0.038 | −0.084 | 0.011 | 0.055 | −0.032 | 0.122 * | 0.090 | 0.059 |
| 8-Number of Children | 0.023 | −0.015 | 0.620 ** | 0.610 ** | 0.115 * | 0.027 | 0.788 ** | 1 | 0.197 ** | −0.151 ** | −0.130 * | 0.112 * | 0.686** | −0.028 | 0.019 | −0.035 | 0.085 | −0.072 | −0.014 | 0.047 | −0.046 | 0.096 | 0.150 ** | 0.044 |
| 9-Place of Residence (rural) | −0.069 | −0.056 | 0.181 ** | 0.199 ** | 0.052 | 0.084 | 0.203 ** | 0.197 ** | 1 | −0.181 ** | −0.108 * | −0.184 ** | 0.184** | 0.050 | −0.110 * | 0.026 | 0.010 | −0.126 * | −0.086 | 0.086 | −0.079 | 0.157 ** | 0.034 | 0.052 |
| 10-Father Education (university or higher) | −0.040 | −0.099 | −0.081 | −0.158 ** | 0.088 | 0.020 | −0.123 * | −0.151 ** | −0.181 ** | 1 | 0.338 ** | 0.326 ** | −0.141** | 0.003 | 0.062 | 0.178 ** | −0.109 * | −0.022 | 0.036 | −0.072 | 0.139 ** | −0.049 | −0.007 | 0.004 |
| 11-Mother Education (university or higher) | 0.065 | −0.031 | 0.031 | 0.049 | 0.014 | 0.009 | −0.075 | −0.130 * | −0.108 * | 0.338 ** | 1 | 0.413 ** | −0.100 | −0.028 | 0.135 * | 0.023 | −0.096 | −0.120 * | −0.087 | −0.068 | −0.027 | −0.061 | 0.076 | −0.080 |
| 12-Family Income | 0.081 | −0.248 ** | 0.310 ** | 0.147 ** | 0.036 | −0.017 | 0.215 ** | 0.112 * | −0.184 ** | 0.326 ** | 0.413 ** | 1 | 0.044 | −0.138 ** | 0.208 ** | 0.091 | −0.118 * | −0.072 | 0.080 | 0.023 | 0.037 | −0.116 * | −0.011 | 0.030 |
| 13-Number of People Living in Household | 0.078 | −0.042 | 0.429 ** | 0.404 ** | 0.127 * | −0.050 | 0.540 ** | 0.686 ** | 0.184 ** | −0.141 ** | −0.100 | 0.044 | 1 | −0.096 | 0.056 | −0.052 | 0.124 * | −0.120 * | 0.034 | 0.069 | −0.111* | 0.110* | 0.094 | 0.094 |
| 14-Accommodation Type (rent) | −0.125 * | 0.139 ** | −0.120 * | −0.035 | −0.003 | −0.012 | −0.028 | −0.028 | 0.050 | 0.003 | −0.028 | −0.138 ** | −0.096 | 1 | −0.122 * | 0.047 | −0.058 | 0.004 | −0.071 | −0.104 | −0.037 | −0.056 | 0.037 | −0.080 |
| 15-Distance to PHC Centre (in km) | 0.200 ** | −0.100 | 0.120 * | 0.058 | 0.026 | −0.041 | 0.045 | 0.019 | −0.110 * | 0.062 | 0.135 * | 0.208 ** | 0.056 | −0.122 * | 1 | −0.042 | 0.003 | −0.059 | 0.018 | −0.005 | −0.114 * | −0.152 ** | −0.068 | 0.054 |
| 16-Waiting Time | −0.371 ** | −0.083 | 0.033 | 0.032 | 0.135 * | −0.073 | −0.014 | −0.035 | 0.026 | 0.178 ** | 0.023 | 0.091 | −0.052 | 0.047 | −0.042 | 1 | −0.668 ** | −0.043 | 0.076 | −0.095 | 0.202 ** | −0.083 | 0.011 | −0.021 |
| 17-Clinic Rating | 0.276 ** | 0.037 | 0.002 | −0.034 | −0.019 | 0.063 | 0.038 | 0.085 | 0.010 | −0.109 * | −0.096 | −0.118 * | 0.124* | −0.058 | 0.003 | −0.668 ** | 1 | 0.181 ** | 0.113 * | 0.158 ** | −0.048 | 0.184 ** | −0.153 ** | 0.167 ** |
| 18-Reminder System (available) | 0.041 | 0.127 * | −0.159 ** | −0.107 * | 0.019 | −0.016 | −0.084 | −0.072 | −0.126 * | −0.022 | −0.120 * | −0.072 | −0.120 * | 0.004 | −0.059 | −0.043 | 0.181 ** | 1 | 0.036 | −0.018 | 0.138 ** | −0.104 | −0.048 | −0.031 |
| 19-Attitude | 0.333 ** | −0.160 ** | −0.029 | −0.120 * | 0.023 | 0.000 | 0.011 | −0.014 | −0.086 | 0.036 | −0.087 | 0.080 | 0.034 | −0.071 | 0.018 | 0.076 | 0.113 * | 0.036 | 1 | 0.599 ** | 0.118 * | 0.131 * | −0.476 ** | 0.619 ** |
| 20-Social Norms | 0.356 ** | −0.056 | 0.065 | 0.043 | −0.042 | −0.013 | 0.055 | 0.047 | 0.086 | −0.072 | −0.068 | 0.023 | 0.069 | −0.104 | −0.005 | −0.095 | 0.158 ** | −0.018 | 0.599 ** | 1 | −0.068 | 0.385 ** | −0.456 ** | 0.696 ** |
| 21-Behavioural Control | −0.095 | −0.012 | −0.096 | −0.106 * | 0.154 ** | −0.012 | −0.032 | −0.046 | −0.079 | 0.139 ** | −0.027 | 0.037 | −0.111 * | −0.037 | −0.114 * | 0.202 ** | −0.048 | 0.138 ** | 0.118 * | −0.068 | 1 | −0.031 | 0.009 | 0.011 |
| 22-Knowledge | −0.143 ** | 0.131 * | 0.177 ** | 0.254 ** | 0.008 | 0.097 | 0.122 * | 0.096 | 0.157 ** | −0.049 | −0.061 | −0.116 * | 0.110 * | −0.056 | −0.152 ** | −0.083 | 0.184 ** | −0.104 | 0.131 * | 0.385 ** | −0.031 | 1 | −0.104 | 0.365 ** |
| 23-Perceived risks | −0.245 ** | 0.111 * | 0.069 | 0.154 ** | −0.003 | 0.043 | 0.090 | 0.150 ** | 0.034 | −0.007 | 0.076 | −0.011 | 0.094 | 0.037 | −0.068 | 0.011 | −0.153 ** | −0.048 | −0.476 ** | −0.456 ** | 0.009 | −0.104 | 1 | −0.499 ** |
| 24-Perceived Benefits | 0.300 ** | −0.034 | 0.014 | −0.021 | −0.033 | 0.005 | 0.059 | 0.044 | 0.052 | 0.004 | −0.080 | 0.030 | 0.094 | −0.080 | 0.054 | −0.021 | 0.167 ** | −0.031 | 0.619 ** | 0.696 ** | 0.011 | 0.365 ** | −0.499 ** | 1 |
| OLS Regression | Logistic Regression | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
| Dependent Variable: Completion Status of Childhood Immunisation | β | β | β | β | β | β | β | β | β | β |
| (robust s.e.) | (robust s.e.) | (robust s.e.) | (robust s.e.) | (robust s.e.) | (robust s.e.) | (robust s.e.) | (robust s.e.) | (robust s.e.) | (robust s.e.) | |
| Demographic Variables | ||||||||||
| Gender (female) | −0.135 * | −0.101 | −0.163 ** | −0.0996 * | - | −0.657 * | −0.660 | −1.160 ** | −0.781 | - |
| (0.0752) | (0.0781) | (0.0646) | (0.0552) | - | (0.368) | (0.424) | (0.451) | (0.503) | - | |
| Age | −0.0109 | −0.0126 | −0.0205 *** | −0.0147 ** | −0.00886 ** | −0.0528 | −0.0846 * | −0.158*** | −0.161 *** | −0.0975 ** |
| (0.00817) | (0.00811) | (0.00655) | (0.00598) | (0.00418) | (0.0389) | (0.0454) | (0.0492) | (0.0616) | (0.0387) | |
| Age (other parent) | 0.00590 | 0.00461 | 0.0137 ** | 0.0165 *** | 0.00982 ** | 0.0283 | 0.0345 | 0.101 ** | 0.166 *** | 0.100 *** |
| (0.00746) | (0.00756) | (0.00639) | (0.00559) | (0.00406) | (0.0356) | (0.0408) | (0.0439) | (0.0527) | (0.0349) | |
| Child Age (in months) | 0.00214 | 0.00223 | 0.00359 * | 0.00459 ** | 0.00425 ** | 0.0111 | 0.0134 | 0.0297 | 0.0474 * | 0.0440 * |
| (0.00186) | (0.00204) | (0.00206) | (0.00192) | (0.00182) | (0.0104) | (0.0122) | (0.0186) | (0.0243) | (0.0238) | |
| Child Gender (female) | −0.0508 | −0.0499 | −0.0702 | −0.0485 | - | −0.245 | −0.271 | −0.510 * | −0.709 * | - |
| (0.0498) | (0.0493) | (0.0444) | (0.0393) | - | (0.239) | (0.259) | (0.299) | (0.362) | - | |
| Child Order | 0.0407 | 0.0318 | 0.0355 | 0.0318 | - | 0.204 | 0.143 | 0.217 | 0.253 | - |
| (0.0335) | (0.0440) | (0.0354) | (0.0315) | - | (0.174) | (0.234) | (0.227) | (0.291) | - | |
| Socio-economic Variables | ||||||||||
| Number of Children | −0.0117 | −0.0105 | −0.0174 | - | −0.148 | −0.124 | −0.141 | - | ||
| (0.0258) | (0.0217) | (0.0202) | - | (0.147) | (0.150) | (0.221) | - | |||
| Place of Residence (rural) | −0.0203 | −0.0203 | −0.0202 | - | −0.0902 | −0.192 | −0.270 | - | ||
| (0.0558) | (0.0518) | (0.0461) | - | (0.286) | (0.353) | (0.469) | - | |||
| Father Education (university or higher) | −0.140 * | −0.0633 | −0.0245 | - | −0.762 * | −0.461 | 0.0932 | - | ||
| (0.0750) | (0.0676) | (0.0629) | - | (0.414) | (0.461) | (0.623) | - | |||
| Mother Education (university or higher) | 0.0592 | −0.00391 | 0.0532 | - | 0.326 | 0.0212 | 0.706 | - | ||
| (0.0679) | (0.0577) | (0.0487) | - | (0.340) | (0.371) | (0.452) | - | |||
| Father Employment (government employee) | 0.153 | 0.160 | 0.123 | 0.122 | 0.730 | 1.115* | 1.291 * | 1.094 | ||
| (0.110) | (0.102) | (0.0912) | (0.0857) | (0.495) | (0.594) | (0.756) | (0.695) | |||
| Father Employment (private sector employee) | 0.225 ** | 0.186 * | 0.153 * | 0.150 * | 1.120 ** | 1.297 ** | 1.466 ** | 1.262 * | ||
| (0.106) | (0.0992) | (0.0865) | (0.0825) | (0.484) | (0.581) | (0.704) | (0.653) | |||
| Mother Employment (government employee) | −0.00711 | −0.00460 | −0.0295 | - | −0.0685 | −0.0269 | −0.509 | - | ||
| (0.0706) | (0.0629) | (0.0536) | - | (0.363) | (0.410) | (0.504) | - | |||
| Mother Employment (private sector employee) | 0.137 * | 0.117* | 0.0488 | - | 0.869 * | 0.904 * | 0.387 | - | ||
| (0.0734) | (0.0670) | (0.0578) | - | (0.471) | (0.526) | (0.636) | - | |||
| Family Income | 0.00198 | 0.00868 | −0.0178 | - | 0.00858 | 0.0297 | −0.271 | - | ||
| (0.0247) | (0.0236) | (0.0195) | - | (0.131) | (0.151) | (0.180) | - | |||
| Number of People Living in Household | 0.0201 ** | 0.00585 | 0.00349 | - | 0.204 ** | 0.117 | 0.140 | - | ||
| (0.00957) | (0.00789) | (0.00745) | - | (0.0828) | (0.0826) | (0.145) | - | |||
| Housing Type (flat) | −0.164 *** | −0.114 ** | −0.0810 * | −0.0811 ** | −1.046 *** | −0.920 ** | −0.910 * | −0.612 | ||
| (0.0589) | (0.0545) | (0.0462) | (0.0383) | (0.343) | (0.413) | (0.533) | (0.394) | |||
| Housing Type (mud house or alike) | −0.171 | 0.120 | 0.0115 | 0.0109 | −1.050 | 0.591 | −0.240 | 0.231 | ||
| (0.158) | (0.135) | (0.121) | (0.113) | (0.756) | (0.839) | (1.180) | (1.337) | |||
| Accommodation Type (rent) | −0.0379 | −0.00106 | −0.00562 | - | −0.170 | 0.00293 | −0.0558 | - | ||
| (0.0596) | (0.0510) | (0.0440) | - | (0.279) | (0.316) | (0.408) | - | |||
| Clinic-related Variables | ||||||||||
| Distance to PHC Centre (in km) | 0.0123 | −0.00482 | - | 0.0289 | −0.115 | - | ||||
| (0.0166) | (0.0144) | - | (0.132) | (0.157) | - | |||||
| Transportation Type (walking) | −0.364 *** | −0.339 *** | −0.351 *** | −2.082 *** | −2.870 *** | −2.672 *** | ||||
| (0.0783) | (0.0653) | (0.0606) | (0.465) | (0.616) | (0.511) | |||||
| Transportation Type (walking and driving) | −0.181 *** | −0.218 *** | −0.215 *** | −1.059 *** | −1.752 *** | −1.547 *** | ||||
| (0.0633) | (0.0591) | (0.0562) | (0.373) | (0.541) | (0.445) | |||||
| Waiting Time | −0.0984 *** | −0.122 *** | −0.123 *** | −0.554 *** | −0.990 *** | −0.913 *** | ||||
| (0.0253) | (0.0222) | (0.0156) | (0.162) | (0.235) | (0.170) | |||||
| Clinic Rating | 0.0377 | 0.00446 | - | 0.280 | 0.0619 | - | ||||
| (0.0288) | (0.0255) | - | (0.184) | (0.230) | - | |||||
| Reminder System (available) | −0.00754 | −0.0157 | - | −0.157 | −0.291 | - | ||||
| (0.0477) | (0.0429) | - | (0.327) | (0.433) | - | |||||
| Parents-related Variables | ||||||||||
| Attitude | 0.0510 *** | 0.0507 *** | 0.371 *** | 0.337 *** | ||||||
| (0.0182) | (0.0176) | (0.109) | (0.106) | |||||||
| Social Norms | 0.0836 *** | 0.0903 *** | 0.653 *** | 0.672 *** | ||||||
| (0.0233) | (0.0219) | (0.197) | (0.185) | |||||||
| Behavioural Control | −0.00486 | − | −0.0126 | − | ||||||
| (0.0104) | − | (0.0991) | − | |||||||
| Knowledge | −0.0810 *** | −0.0848 *** | −0.726 *** | −0.714 *** | ||||||
| (0.0117) | (0.0102) | (0.162) | (0.134) | |||||||
| Perceived Risks | −0.00260 | − | −0.0526 | - | ||||||
| (0.0121) | − | (0.109) | - | |||||||
| Perceived Benefits | 0.0486 ** | 0.0468 ** | 0.390 ** | 0.379 *** | ||||||
| (0.0202) | (0.0191) | (0.159) | (0.132) | |||||||
| Constant | 0.863 *** | 0.895 *** | 1.079 *** | 0.352 | 0.232 | 1.647 ** | 2.303 ** | 3.765 *** | −0.525 | −1.815 |
| (0.148) | (0.203) | (0.234) | (0.237) | (0.167) | (0.726) | (1.028) | (1.455) | (2.039) | (1.464) | |
| Observations | 351 | 351 | 351 | 351 | 351 | 351 | 351 | 351 | 351 | 351 |
| R-squared (Pseudo R-squared) | 0.019 | 0.107 | 0.314 | 0.509 | 0.494 | (0.015) | (0.100) | (0.280) | (0.499) | (0.473) |
| Adjusted R-squared | 0.001 | 0.055 | 0.260 | 0.460 | 0.473 | - | - | - | - | - |
| F-value (Wald Chi-squared) | 1.11 | 3.12 *** | 10.03 *** | 22.09 *** | 38.81 *** | (6.14) | (41.55 ***) | (83.62 ***) | (104.66 ***) | (88.05 ***) |
| Hypothesis | Support |
|---|---|
| H1:Demographic variables (e.g., age, gender, etc.) are associated with childhood immunisation completion status. | Supported for parental age, age of the other parent, and age of the child |
| H2:Socioeconomic variables (e.g., place of residence, level of education, etc.) are associated with childhood immunisation completion status. | Supported for father employment and housing type |
| H3:Clinic-related variables (e.g., distance to PHC centre, waiting time at immunisation clinic, etc.) are associated with childhood immunisation completion status. | Supported for transportation type and waiting time |
| H4:A positive attitude toward immunisation is associated with childhood immunisation completion status. | Supported |
| H5:Subjective social norms toward immunisation are positively associated with childhood immunisation completion status. | Supported |
| H6:Perceived behavioural control toward immunisation is positively associated with childhood immunisation completion status. | Not supported |
| H7:Higher knowledge about immunisation is positively associated with childhood immunisation completion status. | Not supported but significant in the opposite direction |
| H8:Higher perceived risks of immunisation are negatively associated with childhood immunisation completion status. | Not supported |
| H9:Higher perceived benefits of immunisation are positively associated with childhood immunisation completion status. | Supported |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alabadi, M.; Alashoor, T.; Aldawood, O.; Qanbar, Z.; Aldawood, Z. Exploring Critical Factors Associated with Completion of Childhood Immunisation in the Eastern Province of Saudi Arabia. Vaccines 2022, 10, 2147. https://doi.org/10.3390/vaccines10122147
Alabadi M, Alashoor T, Aldawood O, Qanbar Z, Aldawood Z. Exploring Critical Factors Associated with Completion of Childhood Immunisation in the Eastern Province of Saudi Arabia. Vaccines. 2022; 10(12):2147. https://doi.org/10.3390/vaccines10122147
Chicago/Turabian StyleAlabadi, Marwa, Tawfiq Alashoor, Omran Aldawood, Zainab Qanbar, and Zakariya Aldawood. 2022. "Exploring Critical Factors Associated with Completion of Childhood Immunisation in the Eastern Province of Saudi Arabia" Vaccines 10, no. 12: 2147. https://doi.org/10.3390/vaccines10122147
APA StyleAlabadi, M., Alashoor, T., Aldawood, O., Qanbar, Z., & Aldawood, Z. (2022). Exploring Critical Factors Associated with Completion of Childhood Immunisation in the Eastern Province of Saudi Arabia. Vaccines, 10(12), 2147. https://doi.org/10.3390/vaccines10122147






