Gender and Race-Based Health Disparities in COVID-19 Outcomes among Hospitalized Patients in the United States: A Retrospective Analysis of a National Sample
Abstract
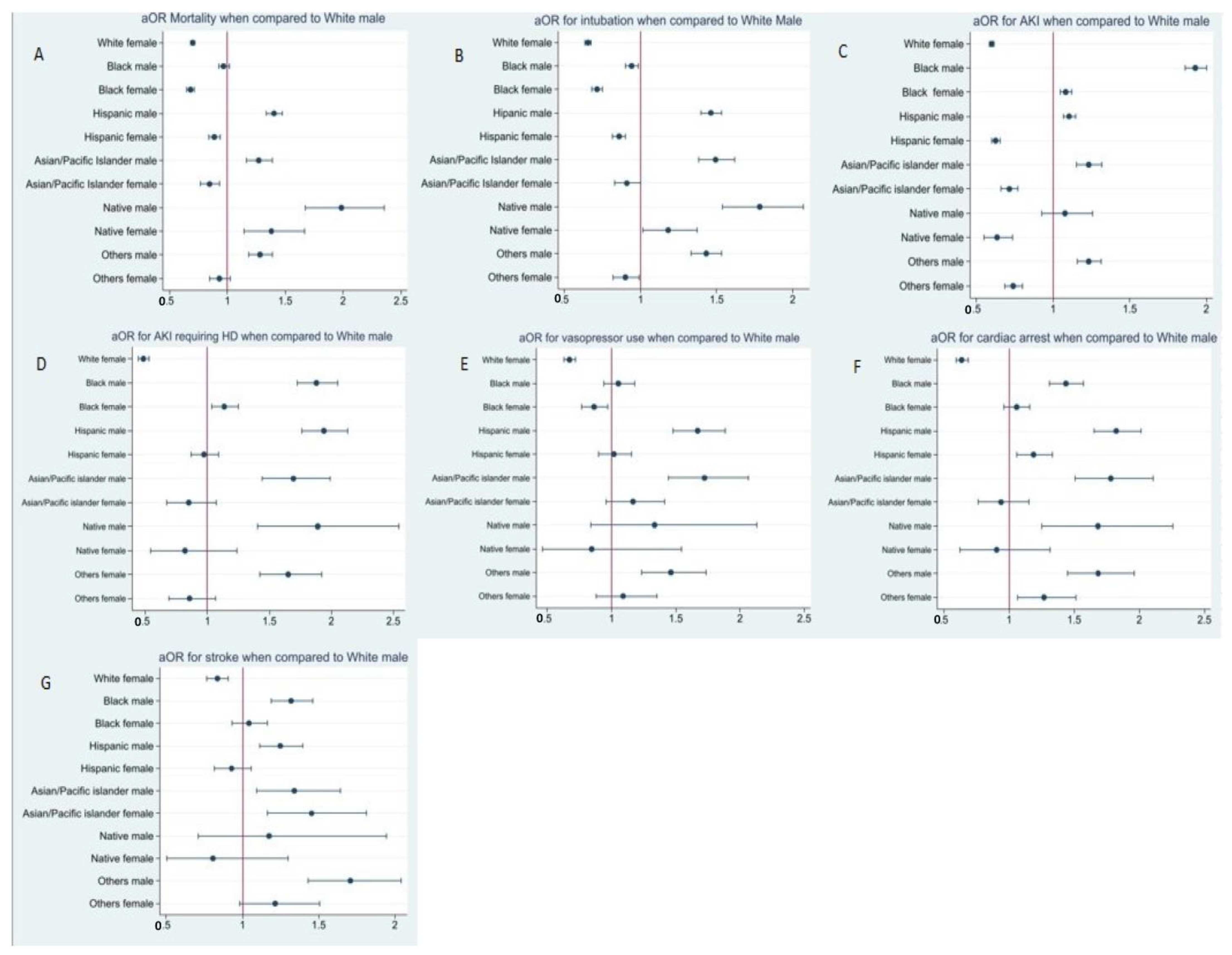
1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Covariates
- a.
- Patient level: Age, comorbidities, insurance status, income in patient’s zip code, disposition.
- b.
- Hospital level: Location, teaching status, bed size, region.
- c.
- Illness severity: Length of stay (LOS), mortality, hospitalization cost, Elixhauser comorbidity score, in-hospital complications, mechanical ventilation, vasopressor use, acute kidney injury (AKI) requiring hemodialysis (HD).
2.3. Study Outcomes
2.4. Statistical Methods
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- CDC. COVID Data Tracker; Centers for Disease Control and Prevention: Atlanta, GA, USA, 28 March 2020. Available online: https://covid.cdc.gov/covid-data-tracker (accessed on 20 October 2022).
- Beydoun, M.A.; Beydoun, H.A.; Mode, N.; Dore, G.A.; Canas, J.A.; Eid, S.M.; Zonderman, A.B. Racial Disparities in Adult All-Cause and Cause-Specific Mortality among Us Adults: Mediating and Moderating Factors. BMC Public Health 2016, 16, 1113. [Google Scholar] [CrossRef]
- U.S. Department of Health and Human Services. Report of the Secretary’s Task Force on Black & Minority Health: Crosscutting Issues in Minority Health; U.S. Department of Health and Human Services: Washington, DC, USA, 1985; ISBN 978-0-16-002806-9. [Google Scholar]
- Riley, W.J. Health Disparities: Gaps in Access, Quality and Affordability of Medical Care. Trans. Am. Clin. Climatol. Assoc. 2012, 123, 167–174. [Google Scholar] [PubMed]
- Rushovich, T.; Boulicault, M.; Chen, J.T.; Danielsen, A.C.; Tarrant, A.; Richardson, S.S.; Shattuck-Heidorn, H. Sex Disparities in COVID-19 Mortality Vary Across US Racial Groups. J. Gen. Intern. Med. 2021, 36, 1696–1701. [Google Scholar] [CrossRef]
- Raine, S.; Liu, A.; Mintz, J.; Wahood, W.; Huntley, K.; Haffizulla, F. Racial and Ethnic Disparities in COVID-19 Outcomes: Social Determination of Health. Int. J. Environ. Res. Public Health 2020, 17, 8115. [Google Scholar] [CrossRef]
- Rockville, M. HCUP National Inpatient Sample (NIS). Healthcare Cost and Utilization Project (HCUP); Agency for Healthcare Research and Quality: Rockville, MD, USA, 2012. [Google Scholar]
- Peckham, H.; de Gruijter, N.M.; Raine, C.; Radziszewska, A.; Ciurtin, C.; Wedderburn, L.R.; Rosser, E.C.; Webb, K.; Deakin, C.T. Male Sex Identified by Global COVID-19 Meta-Analysis as a Risk Factor for Death and ITU Admission. Nat. Commun. 2020, 11, 6317. [Google Scholar] [CrossRef] [PubMed]
- Vahidy, F.S.; Pan, A.P.; Ahnstedt, H.; Munshi, Y.; Choi, H.A.; Tiruneh, Y.; Nasir, K.; Kash, B.A.; Andrieni, J.D.; McCullough, L.D. Sex Differences in Susceptibility, Severity, and Outcomes of Coronavirus Disease 2019: Cross-Sectional Analysis from a Diverse US Metropolitan Area. PLoS ONE 2021, 16, e0245556. [Google Scholar] [CrossRef]
- Finelli, L.; Gupta, V.; Petigara, T.; Yu, K.; Bauer, K.A.; Puzniak, L.A. Mortality Among US Patients Hospitalized with SARS-CoV-2 Infection in 2020. JAMA Netw. Open 2021, 4, e216556. [Google Scholar] [CrossRef]
- Magesh, S.; John, D.; Li, W.T.; Li, Y.; Mattingly-app, A.; Jain, S.; Chang, E.Y.; Ongkeko, W.M. Disparities in COVID-19 Outcomes by Race, Ethnicity, and Socioeconomic Status. JAMA Netw. Open 2021, 4, e2134147. [Google Scholar] [CrossRef]
- Sundaram, S.S.; Melquist, S.; Kalgotra, P.; Srinivasan, S.; Parasa, S.; Desai, M.; Sharma, P. Impact of Age, Sex, Race, and Regionality on Major Clinical Outcomes of COVID-19 in Hospitalized Patients in the United States. BMC Infect. Dis. 2022, 22, 659. [Google Scholar] [CrossRef]
- Qureshi, A.I.; Baskett, W.I.; Huang, W.; Shyu, D.; Myers, D.; Lobanova, I.; Naqvi, S.H.; Thompson, V.S.; Shyu, C.-R. Effect of Race and Ethnicity on In-Hospital Mortality in Patients with COVID-19. Ethn. Dis. 2021, 31, 389–398. [Google Scholar] [CrossRef]
- Musshafen, L.A.; El-Sadek, L.; Lirette, S.T.; Summers, R.L.; Compretta, C.; Dobbs, T.E. In-Hospital Mortality Disparities Among American Indian and Alaska Native, Black, and White Patients with COVID-19. JAMA Netw Open 2022, 5, e224822. [Google Scholar] [CrossRef]
- CDC Cases, Data, and Surveillance. Available online: http://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html (accessed on 21 October 2022).
- Carethers, J.M. Insights into Disparities Observed with COVID-19. J. Intern. Med. 2021, 289, 463–473. [Google Scholar] [CrossRef]
- Garg, S.; Patel, K.; Pham, H.; Whitaker, M.; O’Halloran, A.; Milucky, J.; Anglin, O.; Kirley, P.D.; Reingold, A.; Kawasaki, B.; et al. Clinical Trends Among U.S. Adults Hospitalized with COVID-19, March to December 2020. Ann. Intern. Med. 2021, 174, 1409–1419. [Google Scholar] [CrossRef]
- Wong, M.S.; Haderlein, T.P.; Yuan, A.H.; Moy, E.; Jones, K.T.; Washington, D.L. Time Trends in Racial/Ethnic Differences in COVID-19 Infection and Mortality. Int. J. Environ. Res. Public Health 2021, 18, 4848. [Google Scholar] [CrossRef]
- Charoenngam, N.; Ilori, T.O.; Holick, M.F.; Hochberg, N.S.; Apovian, C.M. Self-Identified Race and COVID-19-Associated Acute Kidney Injury and Inflammation: A Retrospective Cohort Study of Hospitalized Inner-City COVID-19 Patients. J. Gen. Intern. Med. 2021, 36, 3487–3496. [Google Scholar] [CrossRef]
- Hirsch, J.S.; Ng, J.H.; Ross, D.W.; Sharma, P.; Shah, H.H.; Barnett, R.L.; Hazzan, A.D.; Fishbane, S.; Jhaveri, K.D. Acute Kidney Injury in Patients Hospitalized with COVID-19. Kidney Int. 2020, 98, 209–218. [Google Scholar] [CrossRef]
- Chang, M.-H.; Moonesinghe, R.; Truman, B.I. COVID-19 Hospitalization by Race and Ethnicity: Association with Chronic Conditions Among Medicare Beneficiaries, January 1–September 30, 2020. J. Racial Ethn. Health Disparities 2022, 9, 325–334. [Google Scholar] [CrossRef]
- Friedman, D.J.; Pollak, M.R. APOL1 and Kidney Disease: From Genetics to Biology. Annu. Rev. Physiol. 2020, 82, 323–342. [Google Scholar] [CrossRef]
- Ilyas, S.; Henkin, S.; Martinez-Camblor, P.; Suckow, B.D.; Beach, J.M.; Stone, D.H.; Goodney, P.P.; Ebinger, J.E.; Creager, M.A.; Columbo, J.A. Sex-, Race- and Ethnicity-Based Differences in Thromboembolic Events Among Adults Hospitalized with COVID-19. J. Am. Heart Assoc. 2021, 10, e022829. [Google Scholar] [CrossRef]
- Nguyen, N.T.; Chinn, J.; De Ferrante, M.; Kirby, K.A.; Hohmann, S.F.; Amin, A. Male Gender Is a Predictor of Higher Mortality in Hospitalized Adults with COVID-19. PLoS ONE 2021, 16, e0254066. [Google Scholar] [CrossRef]
- Kopel, J.; Perisetti, A.; Roghani, A.; Aziz, M.; Gajendran, M.; Goyal, H. Racial and Gender-Based Differences in COVID-19. Front. Public Health 2020, 8, 418. [Google Scholar] [CrossRef] [PubMed]
- Klein, S.L.; Flanagan, K.L. Sex Differences in Immune Responses. Nat. Rev. Immunol. 2016, 16, 626–638. [Google Scholar] [CrossRef] [PubMed]
- Mikkonen, L.; Pihlajamaa, P.; Sahu, B.; Zhang, F.-P.; Jänne, O.A. Androgen Receptor and Androgen-Dependent Gene Expression in Lung. Mol. Cell. Endocrinol. 2010, 317, 14–24. [Google Scholar] [CrossRef] [PubMed]
| White (820,290) | Black (306,991) | Hispanics (345,935) | Asians (52,326) | Native Americans (16,560) | Others (69,050) | p Value | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | |
| N (%) | 432,293 (52.7%) | 387,997 (47.3%) | 144,900 (47.2%) | 162,091 (52.8%) | 186,113 (53.8%) | 159,822 (46.2%) | 27,628 (52.8%) | 24,698 (47.2%) | 7982 (48.2%) | 8578 (51.8%) | 38,806 (56.2%) | 30,244 (43.8%) | <0.001 |
| Mean Age (SD) | 67.94 (15.08) | 68.29 (17.2) | 60.05 (15.78) | 60.03 (18.1) | 57.01 (16.2) | 54.76 (19.46) | 62.05 (16.2) | 62.58 (18.5) | 56.86 (16.35) | 55.95 (17.26) | 59.33 (16.32) | 58.51 (19.45) | <0.001 |
| Age Groups | |||||||||||||
| ≥18–29 | 8214 (1.9%) | 15,132 (3.9%) | 6231 (4.3%) | 11,995 (7.4%) | 9120 (4.9%) | 21,097 (13.2%) | 884 (3.2%) | 1507 (6.1%) | 439 (5.5%) | 609 (7.1%) | 1630 (4.2%) | 3024 (10.0%) | <0.001 |
| 30–49 | 43,662 (10.1%) | 41,128 (10.6%) | 29,124 (20.1%) | 31,446 (19.4%) | 52,670 (28.3%) | 42,513 (26.6%) | 5387 (19.5%) | 4396 (17.8%) | 2235 (28.0%) | 2453 (28.6%) | 9119 (23.5%) | 6623 (21.9%) | <0.001 |
| 50–69 | 157,355 (36.4%) | 119,503 (30.8%) | 66,944 (46.2%) | 64,998 (40.1%) | 80,401 (43.2%) | 55,139 (34.5%) | 11,991 (43.4%) | 8817 (35.7%) | 3321 (41.6%) | 3526 (41.1%) | 16,842 (43.4%) | 10,737 (35.5%) | <0.001 |
| ≥70 | 223,062 (51.6%) | 212,622 (54.8%) | 42,601 (29.4%) | 53,652 (33.1%) | 44,109 (23.7%) | 41,234 (25.8%) | 9366 (33.9%) | 9978 (40.4%) | 1988 (24.9%) | 1990 (23.2%) | 11,215 (28.9%) | 9860 (32.6%) | <0.001 |
| Median Household Income | |||||||||||||
| <50,000$ | 115,855 (26.8%) | 107,087 (27.6%) | 70,277 (48.5%) | 80,883 (49.9%) | 69,048 (37.1%) | 62,331 (39.0%) | 4227 (15.3%) | 3976 (16.1%) | 4558 (57.1%) | 4975 (58.0%) | 10,400 (26.8%) | 8468 (28.0%) | <0.001 |
| 50,000–64,999$ | 126,230 (29.2%) | 114,459 (29.5%) | 25,502 (17.6%) | 30,959 (19.1%) | 50,623 (27.2%) | 42,832 (26.8%) | 6133 (22.2%) | 5878 (23.8%) | 1796 (22.5%) | 2024 (23.6%) | 9702 (25.0%) | 7349 (24.3%) | <0.001 |
| 65,000–85,999$ | 104,615 (24.2%) | 92,343 (23.8%) | 42,166 (29.1%) | 45,385 (28.0%) | 43,178 (23.2%) | 36,120 (22.6%) | 7984 (28.9%) | 6965 (28.2%) | 1030 (12.9%) | 1089 (12.7%) | 9236 (23.8%) | 7168 (23.7%) | <0.001 |
| >86,000$ | 85,594 (19.8%) | 73,719 (19.0%) | 6955 (4.8%) | 4863 (3.0%) | 23,264 (12.5%) | 18,539 (11.6%) | 9283 (33.6%) | 7903 (32.0%) | 599 (7.5%) | 489 (5.7%) | 9469 (24.4%) | 7259 (24.0%) | <0.001 |
| Insurance status | |||||||||||||
| Medicare | 27,4506 (63.5%) | 257,630 (66.4%) | 72,450 (50.0%) | 85,421 (52.7%) | 63,465 (34.1%) | 53,381 (33.4%) | 11,106 (40.2%) | 10,867 (44.0%) | 3456 (43.3%) | 3689 (43.0%) | 14,746 (38.0%) | 12,370 (40.9%) | <0.001 |
| Medicaid | 28,531 (6.6%) | 29,876 (7.7%) | 33,617 (23.2%) | 36,308 (22.4%) | 46,,342 (24.9%) | 53,700 (33.6%) | 4752 (17.2%) | 5038 (20.4%) | 2355 (29.5%) | 2788 (32.5%) | 8266 (21.3%) | 8015 (26.5%) | <0.001 |
| Private | 119,745 (27.7%) | 94,671 (24.4%) | 23,039 (15.9%) | 24,962 (15.4%) | 58,253 (31.3%) | 41,234 (25.8%) | 10,803 (39.1%) | 8101 (32.8%) | 1924 (24.1%) | 1870 (21.8%) | 12,728 (32.8%) | 8378 (27.7%) | <0.001 |
| Self-pay | 9510 (2.2%) | 6208 (1.6%) | 15,939 (11.0%) | 15,399 (9.5%) | 17,867 (9.6%) | 11,507 (7.2%) | 967 (3.5%) | 692 (2.8%) | 247 (3.1%) | 232 (2.7%) | 3066 (7.9%) | 1482 (4.9%) | <0.001 |
| Hospital bedsize | |||||||||||||
| Small | 110,667 (25.6%) | 101,267 (26.1%) | 34,051 (23.5%) | 38,415 (23.7%) | 41,131 (22.1%) | 33,882 (21.2%) | 5857 (21.2%) | 5458 (22.1%) | 1652 (20.7%) | 2016 (23.5%) | 8110 (20.9%) | 6109 (20.2%) | <0.001 |
| Medium | 123,204 (28.5%) | 111,355 (28.7%) | 41,007 (28.3%) | 45,710 (28.2%) | 56,020 (30.1%) | 48,746 (30.5%) | 7763 (28.1%) | 6915 (28.0%) | 2187 (27.4%) | 2024 (23.6%) | 13,116 (33.8%) | 10,404 (34.4%) | <0.001 |
| Large | 198,422 (45.9%) | 175,375 (45.2%) | 69,842 (48.2%) | 78,128 (48.2%) | 88,962 (47.8%) | 77,354 (48.4%) | 14,007 (50.7%) | 12,324 (49.9%) | 4143 (51.9%) | 4538 (52.9%) | 17,579 (45.3%) | 13,731 (45.4%) | <0.001 |
| Hosptal teaching status | |||||||||||||
| Rural | 59,656 (13.8%) | 55,872 (14.4%) | 9998 (6.9%) | 11,995 (7.4%) | 5583 (3.0%) | 5114 (3.2%) | 470 (1.7%) | 445 (1.8%) | 1373 (17.2%) | 1784 (20.8%) | 1281 (3.3%) | 1089 (3.6%) | <0.001 |
| Urban non-teaching | 87,755 (20.3%) | 79,539 (20.5%) | 20,431 (14.1%) | 23,179 (14.3%) | 37,409 (20.1%) | 31,165 (19.5%) | 5028 (18.2%) | 4470 (18.1%) | 1133 (14.2%) | 1184 (13.8%) | 6403 (16.5%) | 4869 (16.1%) | <0.001 |
| Urban teaching | 284,881 (65.9%) | 252,586 (65.1%) | 114,471 (79.0%) | 126,917 (78.3%) | 143,121 (76.9%) | 123,542 (77.3%) | 22,158 (80.2%) | 19,783 (80.1%) | 5476 (68.6%) | 5601 (65.3%) | 31,161 (80.3%) | 24,286 (80.3%) | <0.001 |
| Comorbidities | |||||||||||||
| CAD | 123,636 (28.6%) | 67,123 (17.3%) | 24,343 (16.8%) | 21,396 (13.2%) | 23,264 (12.5%) | 12,946 (8.1%) | 4559 (16.5%) | 2593 (10.5%) | 1317 (16.5%) | 695 (8.1%) | 6054 (15.6%) | 2813 (9.3%) | <0.001 |
| CHF | 92,511 (21.4%) | 76,823 (19.8%) | 30,284 (20.9%) | 31,446 (19.4%) | 21,031 (11.3%) | 15,023 (9.4%) | 3675 (13.3%) | 2890 (11.7%) | 1317 (16.5%) | 1089 (12.7%) | 4851 (12.5%) | 3539 (11.7%) | <0.001 |
| HTN uncomplicated | 170,323 (39.4%) | 153,647 (39.6%) | 55,931 (38.6%) | 66,457 (41.0%) | 64,953 (34.9%) | 54,180 (33.9%) | 11,079 (40.1%) | 10,052 (40.7%) | 2802 (35.1%) | 2736 (31.9%) | 14,009 (36.1%) | 10,979 (36.3%) | <0.001 |
| HTN complicated | 131,849 (30.5%) | 105,923 (27.3%) | 55,062 (38.0%) | 51,707 (31.9%) | 36,664 (19.7%) | 26,530 (16.6%) | 4780 (17.3%) | 4470 (18.1%) | 1996 (25.0%) | 1819 (21.2%) | 8110 (20.9%) | 5474 (18.1%) | <0.001 |
| DM uncomplicated | 57,927 (13.4%) | 48,888 (12.6%) | 22,749 (15.7%) | 27,880 (17.2%) | 29,964 (16.1%) | 26,690 (16.7%) | 8316 (30.1%) | 6644 (26.9%) | 1301 (16.3%) | 1570 (18.3%) | 6325 (16.3%) | 4839 (16.0%) | <0.001 |
| DM complicated | 111,099 (25.7%) | 82,255 (21.2%) | 48,252 (33.3%) | 49,924 (30.8%) | 54,717 (29.4%) | 41,554 (26.0%) | 6824 (24.7%) | 5359 (21.7%) | 2786 (34.9%) | 2959 (34.5%) | 10,516 (27.1%) | 6835 (22.6%) | <0.001 |
| Renal failure | 101,157 (23.4%) | 74,883 (19.3%) | 47,237 (32.6%) | 39,712 (24.5%) | 31,081 (16.7%) | 21,097 (13.2%) | 5968 (21.6%) | 4446 (18.0%) | 1572 (19.7%) | 1475 (17.2%) | 6830 (17.6%) | 4264 (14.1%) | <0.001 |
| Chronic pulmonary disease | 105,479 (24.4%) | 112,519 (29.0%) | 27,676 (19.1%) | 41,009 (25.3%) | 20,659 (11.1%) | 25,572 (16.0%) | 4365 (15.8%) | 4001 (16.2%) | 1261 (15.8%) | 2024 (23.6%) | 5239 (13.5%) | 5293 (17.5%) | <0.001 |
| Obesity | 98,131 (22.7%) | 99,327 (25.6%) | 35,501 (24.5%) | 58,839 (36.3%) | 47,459 (25.5%) | 47,787 (29.9%) | 3813 (13.8%) | 3606 (14.6%) | 2035 (25.5%) | 2762 (32.2%) | 7645 (19.7%) | 7138 (23.6%) | <0.001 |
| Smoking | 153,464 (35.5%) | 100,103 (25.8%) | 42,456 (29.3%) | 32,580 (20.1%) | 40,945 (22.0%) | 17,421 (10.9%) | 6990 (25.3%) | 2149 (8.7%) | 2315 (29.0%) | 2162 (25.2%) | 8576 (22.1%) | 3508 (11.6%) | <0.001 |
| White (820,290) | Black (306,991) | Hispanics (345,935) | Asians (52,326) | Native (16,560) | Others (69,050) | p Value | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | ||
| Disposition | |||||||||||||
| Home/Routine | 242,516 (56.1%) | 199,430 (51.4%) | 87,809 (60.6%) | 99,524 (61.4%) | 137,165 (73.7%) | 120,825 (75.6%) | 18,842 (68.2%) | 16,449 (66.6%) | 5532 (69.3%) | 6313 (73.6%) | 26,388 (68.0%) | 20,717 (68.5%) | <0.001 |
| SNF/LTAC/Nursing home | 111,532 (25.8%) | 116,787 (30.1%) | 33,907 (23.4%) | 32,094 (19.8%) | 23,450 (12.6%) | 17,421 (10.9%) | 4448 (16.1%) | 4174 (16.9%) | 1477 (18.5%) | 1227 (14.3%) | 6558 (16.9%) | 4960 (16.4%) | <0.001 |
| Home health | 71,761 (16.6%) | 68,675 (17.7%) | 19,562 (13.5%) | 28,366 (17.5%) | 21,961 (11.8%) | 19,658 (12.3%) | 4006 (14.5%) | 3927 (15.9%) | 790 (9.9%) | 884 (10.3%) | 5006 (12.9%) | 4264 (14.1%) | <0.001 |
| AMA | 6052 (1.4%) | 3104 (0.8%) | 3623 (2.5%) | 2107 (1.3%) | 3350 (1.8%) | 1758 (1.1%) | 332 (1.2%) | 123 (0.5%) | 184 (2.3%) | 154 (1.8%) | 776 (2.0%) | 302 (1.0%) | 0.17 |
| AKI | 138,766 (32.1%) | 92,731 (23.9%) | 64,046 (44.2%) | 52,355 (32.3%) | 48,762 (26.2%) | 27,649 (17.3%) | 8758 (31.7%) | 5557 (22.5%) | 2219 (27.8%) | 1673 (19.5%) | 11,758 (30.3%) | 6563 (21.7%) | <0.001 |
| AKI with HD | 9078 (2.1%) | 4268 (1.1%) | 7390 (5.1%) | 5025 (3.1%) | 6700 (3.6%) | 2877 (1.8%) | 995 (3.6%) | 395 (1.6%) | 327 (4.1%) | 163 (1.9%) | 1358 (3.5%) | 514 (1.7%) | <0.001 |
| Cardiac arrest | 10,807 (2.5%) | 6596 (1.7%) | 5941 (4.1%) | 4863 (3.0%) | 7631 (4.1%) | 4155 (2.6%) | 1077 (3.9%) | 519 (2.1%) | 295 (3.7%) | 172 (2.0%) | 1513 (3.9%) | 877 (2.9%) | <0.001 |
| Intubation | 72,193 (16.7%) | 46,948 (12.1%) | 27,096 (18.7%) | 23,827 (14.7%) | 37,781 (20.3%) | 20,937 (13.1%) | 5940 (21.5%) | 3433 (13.9%) | 2099 (26.3%) | 1681 (19.6%) | 8110 (20.9%) | 4355 (14.4%) | <0.001 |
| Vasopressor use | 10,807 (2.5%) | 6596 (1.7%) | 4782 (3.3%) | 4214 (2.6%) | 7072 (3.8%) | 3676 (2.3%) | 1326 (4.8%) | 766 (3.1%) | 216 (2.7%) | 146 (1.7%) | 1475 (3.8%) | 877 (2.9%) | <0.001 |
| Stroke | 6917 (1.6%) | 5044 (1.3%) | 3043 (2.1%) | 2593 (1.6%) | 2978 (1.6%) | 1918 (1.2%) | 525 (1.9%) | 469 (1.9%) | 112 (1.4%) | 77 (0.9%) | 893 (2.3%) | 484 (1.6%) | <0.001 |
| Died | 66,573 (15.4%) | 47,724 (12.3%) | 19,996 (13.8%) | 17,506 (10.8%) | 27,359 (14.7%) | 16,302 (10.2%) | 4476 (16.2%) | 2964 (12.0%) | 1509 (18.9%) | 1209 (14.1%) | 6054 (15.6%) | 3750 (12.4%) | <0.001 |
| Mean LOS | 7.9 | 7.2 | 9.0 | 8.0 | 9.4 | 7.3 | 9.1 | 7.6 | 9.0 | 8.2 | 9.4 | 7.6 | <0.001 |
| Mean TOTCHG | 84,639.4 | 69,127 | 98,138.8 | 82,105.2 | 136,746 | 99,750 | 12,8947.9 | 98,974.5 | 106,172 | 88,653 | 132,199.6 | 101,390.5 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pal, S.; Gangu, K.; Garg, I.; Shuja, H.; Bobba, A.; Chourasia, P.; Shekhar, R.; Sheikh, A.B. Gender and Race-Based Health Disparities in COVID-19 Outcomes among Hospitalized Patients in the United States: A Retrospective Analysis of a National Sample. Vaccines 2022, 10, 2036. https://doi.org/10.3390/vaccines10122036
Pal S, Gangu K, Garg I, Shuja H, Bobba A, Chourasia P, Shekhar R, Sheikh AB. Gender and Race-Based Health Disparities in COVID-19 Outcomes among Hospitalized Patients in the United States: A Retrospective Analysis of a National Sample. Vaccines. 2022; 10(12):2036. https://doi.org/10.3390/vaccines10122036
Chicago/Turabian StylePal, Suman, Karthik Gangu, Ishan Garg, Hina Shuja, Aniesh Bobba, Prabal Chourasia, Rahul Shekhar, and Abu Baker Sheikh. 2022. "Gender and Race-Based Health Disparities in COVID-19 Outcomes among Hospitalized Patients in the United States: A Retrospective Analysis of a National Sample" Vaccines 10, no. 12: 2036. https://doi.org/10.3390/vaccines10122036
APA StylePal, S., Gangu, K., Garg, I., Shuja, H., Bobba, A., Chourasia, P., Shekhar, R., & Sheikh, A. B. (2022). Gender and Race-Based Health Disparities in COVID-19 Outcomes among Hospitalized Patients in the United States: A Retrospective Analysis of a National Sample. Vaccines, 10(12), 2036. https://doi.org/10.3390/vaccines10122036








