Abstract
Vaccination hesitancy (VH) is an important public health issue. The determinants of parental decisions on whether to vaccinate their children are multidimensional and need to be carefully considered in the COVID-19 era. Our study aims to investigate the prevalence of VH among parents, parents’ use of social media, and their attitudes toward the COVID-19 vaccine upon vaccine refusal. Materials and methods: Our participants were the parents of children admitted to hospitals in three different cities in Turkey between September 2021 and December 2021. The parents were asked to complete sociodemographic data and their attitudes toward COVID-19 diseases, the Parental Attitudes Toward Childhood Vaccines (PACV) scale, and the Attitudes Toward COVID-19 Vaccine (ATV-COVID-19) scale. Participants were categorized as “non-hesitant”, with a score of <50, and “hesitant”, with a score of ≥50. Results: A total of 1087 parents with a mean age of 33.66 (SD 9.1) years old participated in the study. VH was noted in 102 (9.38%) parents. Age, gender, education, and income levels did not significantly differ from one another, according to the PACV; however, parents who delayed vaccinating their children and indicated that social media had an impact on vaccination decisions were more hesitant. Parents who were male and had a family member diagnosed with COVID-19 showed more positive attitudes in the ATV-COVID-19. Parents who were hesitant about childhood vaccinations had lower positive attitudes toward the COVID-19 vaccine (2.84 ± 0.97) than parents who were not hesitant (3.77 ± 0.9). A total of 761 (70.14%) parents need more information about childhood immunizations. Conclusion: Parents who are hesitant about childhood immunization programs in Turkey have a less positive attitude toward COVID-19 vaccines and are affected by social media. Parents need information about vaccines, and because the controversy surrounding COVID-19 vaccines can diminish parents’ confidence in routine childhood immunizations, understanding the complex causes behind vaccination hesitancy can help public health policy break through barriers and increase immunization rates.
1. Introduction
Vaccine hesitancy (VH) refers to a delay in accepting or refusing vaccination despite the availability of immunization services, as defined by the Strategic Advisory Group of Experts that work for the WHO [1]. Although VH has been known since the era of widespread vaccine use, it has gained increased acceptance in the last two decades [2]. The need for vaccines and the safety of vaccines are now being questioned as mortality and morbidity rates from vaccinations have declined. For this reason, some people are reluctant to be vaccinated and occasionally choose not to be vaccinated [3]. Vaccination decisions are influenced by a complex interplay of social, psychological, spiritual, political, and personal factors. Furthermore, questioning vaccines and reluctance to vaccinate are exacerbated by social media platforms [4].
Social media and the Internet have become an indispensable part of health-related information behavior today, and the rapid dissemination of health information via social media is a public health opportunity [5]. The Internet and social media are very active in spreading information that questions the safety and efficacy of vaccines, and it is difficult to change the negative attitudes of people exposed to false information about vaccines [4,5]. Some platforms, such as Facebook, Instagram, YouTube, and Twitter, have taken various enforcement actions by removing posts or suspending accounts to prevent the spread of vaccine misinformation [6,7].
In Turkey, vaccine hesitancy–refusal has increased over the past decade. Previously, cases of vaccination refusal were very rare but have increased rapidly since 2015 after the victory of a lawsuit for “obtaining parental consent for vaccination”, as well as frequent arguments against vaccination in the media. The number of families who refused to vaccinate their children was 183 in 2011, which increased to 980 in 2013, 5400 in 2015, 12,000 in 2016, and 23,000 in 2018 [8].
The aim of our study is to investigate the prevalence of VH and the attitudes of parents toward the COVID-19 vaccine and related barriers and facilitators. In addition, our study aims to evaluate the association between parents’ use of social media and their attitudes towards the COVID-19 vaccine and vaccine hesitancy.
2. Materials and Methods
2.1. Study Design, Setting, and Participants
This cross-sectional study was prepared according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines [9]. The study was conducted with parents of children aged 0–60 months. The study was created with convenience samples obtained from three different hospitals: Gulhane Training and Research Hospital; Mersin City Training and Research Hospital, Department of Pediatrics; and Afyon Çay State Hospital. The research was completed between September 2021 and December 2021. The first two hospitals were second- and third-level care hospitals, while the other was a primary care hospital. General pediatric outpatient clinics in hospitals in Turkey provide primary care services to pediatric patients who are between 0–18 years old. These hospitals are by direct referral and do not require a referral chain; a general pediatrician may refer the patient to a pediatric subspecialist when deemed necessary. Patients who were being treated for chronic diseases and presented to outpatient clinics in the subdivisions were excluded from the study.
Before their appointment at a pediatric outpatient clinic, the parents or caregivers of the child in the waiting room were asked to complete the questionnaire. The parents who applied to general pediatric outpatient clinics were consecutively selected for our study. If a child was accompanied by more than one parent, only one parent was asked to participate. The questionnaires were completed without assistance, unless requested. During the study period, parents over 18 years of age were voluntarily included. The present study was approved by the Clinical Research Ethics Committee of Gulhane Training and Research Hospital (Decision Number: 2021/62). Permission was obtained from the three centers where the study was conducted.
2.2. Variables
To examine this, we used the Parents’ Attitudes Toward Childhood Vaccines (PACV) scale and Attitudes Toward COVID-19 Vaccine (ATV-COVID-19) scale. The questionnaire for the study consisted of a 15-item PACV, a 9-item attitude scale about the COVID-19 vaccine, demographic questions, self-report questions about COVID-19 vaccination status/intention, and vaccine-specific concerns about side effects. The questionnaire was adapted after a pilot study with 15 parents/caregivers who met the inclusion criteria.
The questionnaire was divided into six parts. The first part consisted of seven questions on sociodemographic and economic factors (age, sex, occupation, marital status, monthly income, education level, and social security). In the second section, parents were questioned about where their children received their childhood vaccinations, whether there were any delays or vaccinations that were missed, and whether they needed any information. In the third section, the participants were asked if they had ever been vaccinated for COVID-19, had a family history of death as a result of COVID-19 infection, if they had received the COVID-19 vaccine, and their preferences for and side effects from the COVID-19 vaccine. The fourth section consisted of seven questions about social media use and the influence of social media on parents’ decisions to have their children vaccinated.
In the fifth part, the PACV scale developed by Opel et al. was used [10]. Its validity and reliability adaptation to Turkish were performed by Çevik et al. [11]. The floor and ceiling effects of the scale were within the desired limits. The Cronbach‘s alpha value of the scale was 0.676, the test–retest results were good (ICC: 0.93, p: 0.001), and the scale was found to be discriminant according to the validity of the known groups [10].
The PACV is a 15-item questionnaire divided into 3 domains: behavior (2 items), safety and effectiveness (4 items), and general attitude and trust (9 items). In PACV, there are three response options: binary, 5-point Likert scale, and 11-point scale (e.g., from “0, I am not quite sure” to “10, I am quite sure”). All responses were assigned a numerical value. In evaluating the scale, 2 points were awarded for hesitant responses, 1 point for “I do not know, or I am not sure,” and 0 points for non-hesitant responses; the participants were categorized as “non-hesitant” with a score of <50 and “hesitant” with a score of ≥50, which is consistent with previous research.
The sixth and final part was the Attitudes Toward COVID-19 Vaccine Scale (ATV-COVID19), which was first developed by Geniş et al. (2020). [12]. This scale also has nine items and consists of two domains: positive (4 items) and negative (5 items). The statements in the scale were evaluated on a 5-point Likert-style scale; the statements include: “I strongly disagree (1)”, “I do not agree (2)”, “I neither agree nor disagree (3)”, “I agree (4)”, and “I strongly agree (5).” A value between 1 and 5 can be obtained by dividing the total score obtained by the sum of the item scores in the scale subdimension by the number of items in that subdimension. High scores from the positive attitude subdimension indicated that the attitude toward vaccination was positive. In the original study, two subdimensions (positive and negative attitudes) were used; however, in this study, only one subdimension is evaluated.
2.3. Statistical Analysis
The descriptive statistics of the data obtained from the study have been reported with the mean and standard deviation for the numerical variables and with a frequency and percentage analysis for the categorical variables. To compare the values obtained from the scales, the z-test was used for a quantitative analysis across the two groups, and an analysis of variance was used for categorical variables with three or more groups. The Tukey multiple comparison test was used to determine the difference between the groups as a result of the analysis of variance. Analyses were performed using the SPSS 22.0 statistical package (IBM Co., New York, NY, USA). The significance level was set at p < 0.05.
3. Results
A total of 1087 participants were included in the study (1276/1087 = 85.2%), and parents under 18 years of age (11) and participants with missing markers on the scales (178) were excluded (Table 1).

Table 1.
Descriptive Characteristics of the Participants.
3.1. Sociodemographic Data
Of the participants, 779 (72.1%) were female and 308 (27.9%) were male. The mean age of the participants was 33.66 ± 9.1 years (minimum–maximum: 18–64). Of the participants, 993 (92.18%) were married and 358 (33.52%) were housewives. A total of 327 (30.63%) of the participants had a university degree, while 363 (33.9%) had a high school diploma. The income of 414 (38.14%) of the participants was TRY 4000 or less, and 28.21% ıwere between TR 4000 and 6000; there were 117 (10.97%) participants with the highest household income of TRY 10,000 and above (Table 1).
3.2. Hesitancy towards Childhood Vaccinations
Of the participating parents, 958 (89.78%) had their children vaccinated at the Family Health Centers. There were 108 (10.14%) participants where social media influenced their decision about childhood vaccinations, and 161 (15.10%) participants were affected by COVID-19 vaccine decisions. The participants were most likely to use Facebook (n = 380; 44.03%) for vaccination information. In addition, 38 (3.56%) of the participating parents postponed or did not have their children vaccinated and 761 (70.14%) parents indicated they needed more information about childhood immunizations (Table 1).
3.3. COVID-19-Related Variables
A total of 408 (37.92%) of the participants and 504 (46.93%) of their family members were infected with COVID-19. In addition, 105 (9.79%) participants lost one of their family members to COVID-19 infection, and 882 (82.12%) participants who were vaccinated against COVID-19 preferred the mRNA vaccine. Approximately half of the participants (n = 519; 51.08%) were exposed to COVID-19 vaccine side effects (Table 1).
3.4. PACV Scale
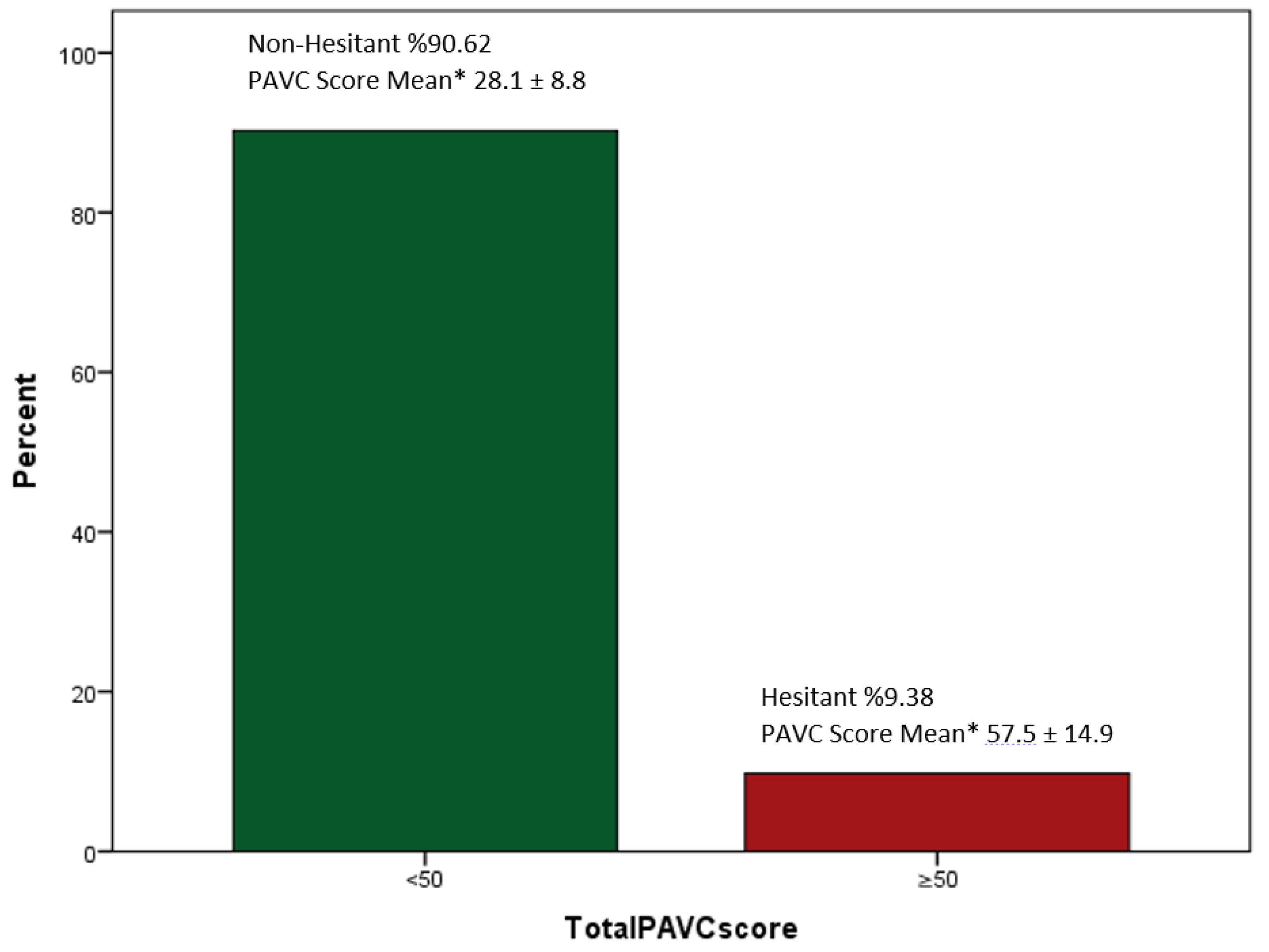
The average PACV score was 30.96 (SD 12.9), and the distribution of scores is shown in Figure 1. VH was noted in 102 (9.38%) parents. There was no significant difference between the age group, gender, education, or income level of the participants. Although there was no statistically significant difference, those who are not hesitant were mostly high school graduates (n = 341; 35.08%), and those who are hesitant were most often college graduates (n = 39; 38.24%). Those who were influenced by social media regarding their vaccination decisions were more hesitant (n = 27; 26.73%) than those who were not hesitant (n = 134; 13.8%) (p < 0.001). Those who used Facebook for vaccination information were less hesitant than those who used other social media (p < 0.001). On the other hand, those who used Instagram have more VH (56.16%). Those who postponed vaccinating their children were more hesitant (7.92%; <0.013) (Table 2).
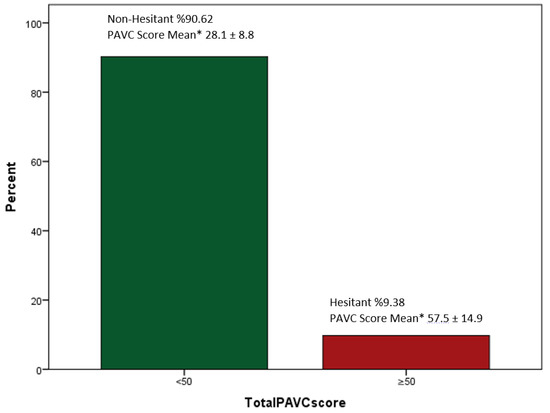
Figure 1.
Participant Parent Attitudes about Childhood Vaccine (PACV) Scores Non-Hesitant/Hesitant. Mean ± SD: Average, standard deviation.

Table 2.
The Relationship between Parental Attitudes about Childhood Vaccines and Characteristics of Participating Parents.
3.5. Attitudes toward the COVID-19 Vaccine (ATV-COVID-19)
When the participants’ ratings on the Attitudes Toward the COVID-19 Vaccine scale were analyzed, the mean score for a positive attitude was 3.69 ± 0.95. Although there was no significant difference in positive attitudes toward the COVID-19 vaccine between age groups, the positive attitude scores of males were higher than those of females (p < 0.022,). When comparing marital status, education level, and monthly income, the mean values of the positive attitude scales did not differ. Those who had a family member with a COVID-19 diagnosis (3.77 ± 0.89) had higher positive attitude scores than those who did not (3.62 ± 0.99) (p < 0.007). There was no significant difference between the mean scores of positive attitudes among those who had received the COVID-19 vaccine, who had experienced COVID-19 vaccine side effects, and those who had lost a family member to COVID-19. In addition, there was no difference between the positive attitudes of parents who had or had not deferred their childhood vaccinations (Table 3).

Table 3.
Descriptive Statistics and Determination of the Factors that Affect Positive Attitudes Based on Demographic Characteristics.
3.6. PACV Scale and ATV-COVID-19
The participants who indicated that social media did not influence their decision to get their child vaccinated had higher positive scores than those who indicated that it did (p < 0.001). Among the social groups, the most positive attitude was found on Facebook (3.97 ± 0.46), (p < 0.001). A statistically significant difference was found between the positive attitudes of parents who were hesitant and not hesitant about childhood vaccines (p < 0.001). Parents who are hesitant to childhood vaccinations (2.84 ± 0.97) have lower positive attitudes towards the COVID-19 vaccine than those who are non-hesitant (3.77 ± 0.9).
4. Discussion
This is the first multicenter study with a large sample using the PACV scale to determine VH in Turkey. Our study has shown that parents who were hesitant about childhood vaccines also displayed less positive attitudes toward the COVID-19 vaccine. In addition, VH, as identified by a high PACV score, was associated with non-vaccination or vaccination delay. The present study showed that people influenced by social media had hesitant attitudes toward childhood vaccines and less positive attitudes toward COVID-19 vaccines when making decisions about childhood vaccines and COVID-19 vaccines. In addition, the presence of a COVID-19 diagnosis in the family led to a positive attitude toward the COVID-19 vaccine, whereas the absence of such a diagnosis was associated with VH.
In the current study, the hesitancy toward childhood vaccines did not change based on age, education, and income level. A study in Turkey found that women who lived in developed regions and had a higher income and higher education levels were more hesitant and more likely to refuse vaccination [13].
In our study, 9.38% of participants are VH. In the literature, the prevalence of VH in PACV varied from 5% to 34.7% in different countries (using the conventional PACV cut-off) [14,15]. Hence, there is a need to conduct studies at different time points in different regions to predict vaccination hesitancy in Turkey.
We found that hesitant parents were more likely to delay or not vaccinate their children. The literature has shown that parents with a PACV score of ≥50 were at higher risk of postponing or not having their children immunized [16,17]. It has been noted that hesitancy around measles vaccination, as identified by PACV in Sudan, was found to have a direct impact on measles vaccine administration [18]. Screening parents who are hesitant to vaccinate can be done with the PACV and may be a useful tool that can be used to support vaccination throughout childhood.
Another finding of the present study was that women have less positive attitudes toward the COVID-19 vaccine than men. In studies of COVID-19 vaccines, it has been observed that men were more willing to be vaccinated [19,20,21]. Research has shown that women in Turkey were hesitant toward the COVID-19 vaccine [13,19,20].
Parents whose families had not been diagnosed with SARS-CoV-2 infection were more reluctant to have their children vaccinated. In their study, Goldman et al. showed that parents’ intention to vaccinate their children against influenza increased after the COVID-19 pandemic [21]. Another study from Indonesia found that knowledge of Zika was significantly associated with lower vaccination compliance among children [22]. Similarly, Opel et al.’s study supported the hypothesis that the pandemic may have positively influenced parents’ general attitudes toward childhood vaccination [23]. In our study, when a family member was diagnosed with SARS-CoV-2, positive attitudes toward COVID-19 vaccines were higher than among those who did not have the disease.
In India, Mohan et al. showed that parents with SARS-CoV-2 had more positive attitudes toward COVID-19 vaccines [24]. One of the many international studies covering all 27 EU member states showed that vaccination readiness was lower among people who tested positive for SARS-CoV-2 than among those who had not [25]. Our study is in line with the findings of Mertens et al., who found that increased anxiety during the COVID-19 pandemic was associated with perceived risks to family members and health anxiety [26]. Infection of relatives of parents may have positively affected parents’ attitudes toward vaccines by increasing their perception of the value of vaccines in preventing communicable diseases.
Our study found that those who reported being influenced by social media regarding their children and their vaccination decisions were more hesitant about routine childhood vaccinations than those who were not. Accessing vaccine-critical websites within 5–10 min has been shown to increase perceptions of vaccination risk, decrease perceptions of risk of not being vaccinated, and decrease the intentions to be vaccinated [3].
Parents not influenced by social media for the COVID-19 vaccine have been found to have more positive attitudes toward vaccination. Along with the pandemic, many studies on this topic have supported our work [25,26,27,28].
Those participants who used social media for vaccine information mainly used Facebook and Instagram. Facebook was the most used social media platform by parents who were not hesitant about childhood vaccines and who had a positive attitude toward the COVID-19 vaccine in this study. In their study of social media use and influenza vaccination among adults, Ahmet et al. found that those who used Facebook as a source of health information were more likely to be vaccinated [29]. Facebook is a powerful platform for finding and sharing health-related content and providing social support [30]. This may be because of the ban on anti-vaxx ads on Facebook, which have prevented the spread of vaccines and resulted in vaccine misinformation [31]. This question can be answered by a new study that examines the factors that help explain the content of the vaccination discourse on Facebook pages, along with what drives and generates that discourse.
Instagram is the most widely used social media for those hesitant about childhood vaccinations. Some posts have described some vaccine-related side effects and the harms of the vaccine, but these were usually presented with a narrative and visuals, thereby triggering anxiety in parents [32]. They continued to spread antivaccine sentiments by creating new antivaccine tags to replace closed accounts or by using pro-vaccine tags. With recent changes, posts on Instagram can now be reported for “false information” [33].
Another important finding of our study was that 70% of the parents reported that they needed information about vaccines. In various studies conducted with parents in Turkey, a lack of knowledge was cited as a cause of incomplete vaccinations and postponement of vaccinations [34,35]. Similar to our study, in the Canadian Immunization Research Network survey, 68% of parents with 24–59-month-old children across Canada reported that they frequently needed to research or obtain information about vaccines [36]. In the future, it is important to meet the need for information to prevent the escalation of vaccination refusal and denial [3].
Parents who are VH, as determined by the PACV scale, have a less positive attitude toward the COVID-19 vaccine. In their study about the acceptability of COVID-19 vaccination among children in India, Mohan et al. found that parents whose children were routinely vaccinated were willing to have their children vaccinated against COVID-19 [24]. This was also noted by Altulaihi et al., who reported that parents who were very receptive to seasonal influenza vaccination were also willing to accept the COVID-19 vaccine for their children [37]. El-Elimat et al. found that participants who had received an influenza vaccination were more likely to accept the COVID-19 vaccine compared to those who had not received an influenza vaccination [38].
The present study has shown that, in Turkey, the parental attitude toward childhood vaccination and use of social media leads to hesitant and uncertain vaccination decisions and results in parents needing information about vaccinations. Developing continuing education programs that provide information for health professionals to appropriately address concerns about vaccination, as well as communication strategies to help them confidently recommend vaccinations, will support the efforts in this area.
One of the strengths of the present study was the use of previously approved survey instruments (PACV and ATV-COVID-19) to determine parental hesitancy toward vaccination. In addition, the large sample size was one of the strengths of our study.
A possible limitation was the current study’s nature: the participants were in hospitals, which may have increased the potential for higher vaccine acceptance. In addition, it is possible that those individuals who were hesitant at the time of participant selection may have been less likely to participate in the survey. This was a cross-sectional survey that provided information or shed light on the situation in a snapshot, and the timing of the cross-sectional snapshot may be unrepresentative of the behavior of the group as a whole. This means that parents who do not regularly see providers or have access to healthcare may not be included, thereby creating selection bias; hence, the results may not be representative of Turkey as a whole.
However, the sociodemographic data of the participants in this study show similarities with the Turkish population. According to 2018 data from the Institute for Population Studies at Hacettepe University, one-third of women and men in the Turkish population have a primary school degree, and 26% of women and 33% of men have a high school degree, which is similar to the participants in our study [39]. The average age of the Turkish population is 33.1 years, which is similar to that of our participants [40]. Furthermore, since there is no referral chain in Turkey, patients can contact hospitals directly. In addition, 76.7% of the population prefers state hospitals for medical care [41]. For these reasons, our study can provide helpful information about VH in Turkey.
5. Conclusions
Vaccine hesitancy is a serious threat to effective vaccination programs against COVID-19 and childhood vaccination. In this study, parents who were hesitant about childhood vaccines also showed a less positive attitude toward COVID-19 vaccines. Our analysis shows that VH and attitudes toward COVID-19 vaccines were influenced by social media use. These findings suggest that public health interventions that use social media may be effective in promoting vaccine uptake and preventing hesitant attitudes toward vaccination in Turkey. Furthermore, parents need information about vaccinations. A total of 89.78% of participating parents had their children vaccinated at family health centers, and we recommend the development and use of health education about vaccinations and vaccine-preventable diseases here. Considering these findings, the national government and professionals, pediatricians, and public health experts must implement reliable strategies to address the detrimental effects of misinformation, which can escalate vaccine hesitancy. In addition, it is important to study the factors that contribute to vaccine hesitancy in different Turkish regions. The controversy surrounding the COVID-19 vaccines may diminish parents’ confidence in routine childhood immunizations. Understanding the complex causes of vaccine hesitancy can help public health policy overcome barriers and increase vaccination rates.
Author Contributions
Conceptualization, N.D. and E.Ö.; methodology, N.D. and M.E.; software, N.D.; validation, N.D., M.S., M.E. and E.Ö.; formal analysis, N.D.; investigation, N.D. and M.S.; resources, N.D.; data curation, N.D. and M.S.; writing—original draft preparation, N.D.; writing—review and editing, N.D. and E.Ö. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Ethics Committee of Clinical Research Ethics Committee of Gulhane Training and Research Hospital (protocol code 2021/62 and date of approval 29 September 2021).
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- MacDonald, N.E.; Eskola, J.; Liang, X.; Chaudhuri, M.; Dube, E.; Gellin, B.; Goldstein, S.; Larson, H.; Manzo, M.L.; Reingold, A.; et al. SAGE Working Group on Vaccine Hesitancy Vaccine Hesitancy: Definition, Scope and De-terminants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef] [PubMed]
- Dubé, E.; Vivion, M.; MacDonald, N.E. Vaccine Hesitancy, Vaccine Refusal and the Anti-Vaccine Movement: Influence, Impact and Implications. Expert Rev. Vaccines 2015, 14, 99–117. [Google Scholar] [CrossRef] [PubMed]
- Williams, S.E. What Are the Factors That Contribute to Parental Vaccine-Hesitancy and What Can We Do about It? Hum. Vaccines Immunother. 2014, 10, 2584–2596. [Google Scholar] [CrossRef]
- Kata, A. Anti-Vaccine Activists, Web 2.0, and the Postmodern Paradigm—An Overview of Tactics and Tropes Used Online by the Anti-Vaccination Movement. Vaccine 2012, 30, 3778–3789. [Google Scholar] [CrossRef] [PubMed]
- Betsch, C.; Renkewitz, F.; Betsch, T.; Ulshöfer, C. The Influence of Vaccine-critical Websites on Perceiving Vaccination Risks. J. Health Psychol. 2010, 15, 446–455. Available online: https://journals.sagepub.com/doi/10.1177/1359105309353647 (accessed on 20 September 2022). [CrossRef] [PubMed]
- Krishnan, N.; Gu, J.; Tromble, R.; Abroms, L. Research note: Examining how various social media platforms have responded to COVID-19 misinformation. Harv. Kennedy Sch. Misinformation Rev. 2021, 2, 1–25. [Google Scholar] [CrossRef]
- Durmaz, N.; Hengirmen, E. The Dramatic Increase in Anti-Vaccine Discourses during the COVID-19 Pandemic: A Social Network Analysis of Twitter. Hum. Vaccines Immunother. 2022, 18, 2025008. [Google Scholar] [CrossRef] [PubMed]
- Aşılar 1. Baskı; Gür, E., Kararsızlığı, A., Gökçay, G., Eds.; Türkiye Klinikleri: Ankara, Turkey, 2021; pp. 28–33. [Google Scholar]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies*. Bull. World Health Organ. 2007, 85, 867–872. [Google Scholar] [CrossRef]
- Opel, D.J.; Mangione-Smith, R.; Taylor, J.A.; Korfiatis, C.; Wiese, C.; Catz, S.; Martin, D.P. Development of a Survey to Identify Vaccine-Hesitant Parents. Hum. Vaccines 2011, 7, 419–425. [Google Scholar] [CrossRef]
- Çevik, C.; Güneş, S.; Eser, S.; Eser, E. Ebeveynlerin Çocukluk Aşilarina Yönelik Tutumlari (Pacv) Ölçeğinin Türkçe Sürümünün Psikometrik Özellikleri. Güncel Pediatri 2020, 18, 153–167. Available online: https://dergipark.org.tr/tr/pub/pediatri/issue/56218/775236 (accessed on 1 August 2022). [CrossRef]
- Geniş, B. Development of Perception And Attitude Scales Related with Covid-19 Pandemia. Pearson J. Soc. Sci. Humanit. 2020, 7, 306–328. [Google Scholar] [CrossRef]
- Özceylan, G.; Toprak, D.; Esen, E.S. Vaccine Rejection and Hesitation in Turkiye. Hum. Vaccines Immunother. 2020, 16, 1034–1039. [Google Scholar] [CrossRef] [PubMed]
- Napolitano, F.; D’Alessandro, A.; Angelillo, I.F. Investigating Italian Parents’ Vaccine Hesitancy: A Cross-Sectional Survey. Hum. Vaccines Immunother. 2018, 14, 1558–1565. [Google Scholar] [CrossRef] [PubMed]
- Henrikson, N.B.; Anderson, M.L.; Opel, D.J.; Dunn, J.; Marcuse, E.K.; Grossman, D.C. Longitudinal Trends in Vaccine Hesitancy in a Cohort of Mothers Surveyed in Washington State, 2013–2015. Public Health Rep. 2017, 132, 451–454. [Google Scholar] [CrossRef]
- Napolitano, F.; del Giudice, G.M.; Angelillo, S.; Fattore, I.; Licata, F.; Pelullo, C.P.; Giuseppe, G.D. Hesitancy towards Childhood Vaccinations among Parents of Children with Underlying Chronic Medical Conditions in Italy. Vaccines 2022, 10, 1254. [Google Scholar] [CrossRef]
- Strelitz, B.; Gritton, J.; Klein, E.J.; Bradford, M.C.; Follmer, K.; Zerr, D.M.; Englund, J.A.; Opel, D.J. Parental Vaccine Hesitancy and Acceptance of Seasonal Influenza Vaccine in the Pediatric Emergency Department. Vaccine 2015, 33, 1802–1807. [Google Scholar] [CrossRef]
- Sabahelzain, M.M.; Moukhyer, M.; van den Borne, B.; Bosma, H. Vaccine Hesitancy among Parents and Its Association with the Uptake of Measles Vaccine in Urban Settings in Khartoum State, Sudan. Vaccines 2022, 10, 205. [Google Scholar] [CrossRef]
- Kilic, M.; Ustundag Ocal, N.; Uslukilic, G. The Relationship of Covid-19 Vaccine Attitude with Life Satisfaction, Religious Attitude and Covid-19 Avoidance in Turkiye. Hum. Vaccines Immunother. 2021, 17, 3384–3393. [Google Scholar] [CrossRef]
- Salali, G.D.; Uysal, M.S. COVID-19 vaccine hesitancy is associated with beliefs on the origin of the novel coronavirus in the UK and Turkey. Psychol. Med. 2020, 1–3. [Google Scholar] [CrossRef]
- Goldman, R.D.; McGregor, S.; Marneni, S.R.; Katsuta, T.; Griffiths, M.A.; Hall, J.E.; Seiler, M.; Klein, E.J.; Cotanda, C.P.; Gelernter, R.; et al. Willingness to Vaccinate Children against Influenza after the Coronavirus Disease 2019 Pandemic. J. Pediatr. 2021, 228, 87–93.e2. [Google Scholar] [CrossRef]
- Yufika, A.; Wagner, A.L.; Nawawi, Y.; Wahyuniati, N.; Anwar, S.; Yusri, F.; Haryanti, N.; Wijayanti, N.P.; Rizal, R.; Fitriani, D.; et al. Parents’ Hesitancy towards Vaccination in Indonesia: A Cross-Sectional Study in Indonesia. Vaccine 2020, 38, 2592–2599. [Google Scholar] [CrossRef] [PubMed]
- Opel, D.J.; Furniss, A.; Zhou, C.; Rice, J.D.; Spielvogle, H.; Spina, C.; Perreira, C.; Giang, J.; Dundas, N.; Dempsey, A.; et al. Parent Attitudes Towards Childhood Vaccines After the Onset of SARS-CoV-2 in the United States. Acad. Pediatr. 2022, 22, 1407–1413. [Google Scholar] [CrossRef] [PubMed]
- Mohan, R.; Pandey, V.; Kumar, A.; Gangadevi, P.; Goel, A.D.; Joseph, J.; Kurien, N. Acceptance and Attitude of Parents Regarding COVID-19 Vaccine for Children: A Cross-Sectional Study. Cureus 2022, 14, e24518. [Google Scholar] [CrossRef] [PubMed]
- Mascherini, M.; Nivakoski, S. Social Media Use and Vaccine Hesitancy in the European Union. Vaccine 2022, 40, 2215–2225. [Google Scholar] [CrossRef] [PubMed]
- Mertens, G.; Gerritsen, L.; Duijndam, S.; Salemink, E.; Engelhard, I.M. Fear of the Coronavirus (COVID-19): Predictors in an Online Study Conducted in March 2020. J. Anxiety Disord. 2020, 74, 102258. [Google Scholar] [CrossRef]
- Oruç, M.A.; Öztürk, O. Attitudes of Health Care Professionals towards COVID-19 Vaccine-a Sequence from Turkey. Hum. Vaccines Immunother. 2021, 17, 3377–3383. [Google Scholar] [CrossRef]
- Wilson, S.L.; Wiysonge, C. Social Media and Vaccine Hesitancy. BMJ Glob. Health 2020, 5, e004206. [Google Scholar] [CrossRef]
- Ahmed, N.; Quinn, S.C.; Hancock, G.R.; Freimuth, V.S.; Jamison, A. Social Media Use and Influenza Vaccine Uptake among White and African American Adults. Vaccine 2018, 36, 7556–7561. [Google Scholar] [CrossRef]
- Oh, H.J.; Lauckner, C.; Boehmer, J.; Fewins-Bliss, R.; Li, K. Facebooking for Health: An Examination into the Solicitation and Effects of Health-Related Social Support on Social Networking Sites. Comput. Hum. Behav. 2013, 29, 2072–2080. [Google Scholar] [CrossRef]
- Wong, J.C. How Facebook and YouTube Help Spread Anti-Vaxxer Propaganda. Guardian 2019, 1. [Google Scholar]
- Taşcı, Ö.; Gökler, M.E. Examining the Social Media Posts of Anti-vaccine People: An Instagram. Med. Res. Rep. 2021, 4, 23–30. [Google Scholar]
- Hard Questions: How Is Facebook’s Fact-Checking Program Working? Facebook Newsroom. 2018. Available online: https://about.fb.com/news/2018/06/hard-questions-fact-checking/ (accessed on 2 September 2022).
- Çatiker, A.; Özkan, Ö. Vaccination status of children and barriers for vaccination in Bolu. J. Contin. Med. Educ. 2006, 15, 171–178. [Google Scholar]
- Bulut, A.; Babadağli, F.; Ertem, H.V.; Gökçay, G. Delayed and lack of immunization and risk factors among children aged 12–36 months attending a state hospital in Turkey. J. Child 2007, 7, 233–239. [Google Scholar]
- McGregor, S.; Goldman, R.D. Determinants of Parental Vaccine Hesitancy. Can. Fam. Physician 2021, 67, 339–341. [Google Scholar] [CrossRef]
- Altulaihi, B.A.; Alaboodi, T.; Alharbi, K.G.; Alajmi, M.S.; Alkanhal, H.; Alshehri, A. Perception of Parents Towards COVID-19 Vaccine for Children in Saudi Population. Cureus 2021, 13, e18342. [Google Scholar] [CrossRef]
- El-Elimat, T.; AbuAlSamen, M.M.; Almomani, B.A.; Al-Sawalha, N.A.; Alali, F.Q. Acceptance and attitudes toward COVID-19 vaccines: A cross-sectional study from Jordan. PLoS ONE 2021, 16, e0250555. [Google Scholar] [CrossRef]
- Hacettepe University Institute of Population Studies. Turkey Demographic and Health Survey; Hacettepe University Institute of Population Studies: Ankara, Turkey, 2018; pp. 12–13. [Google Scholar]
- Turkish Statistical Institute. The Results of Address Based Population Registration System; National Data Release: Ankara, Turkey, 2020. [Google Scholar]
- Bektemur, G.; Arıca, S.; Gençer, M.Z. How Should Referral Chain be Implemented in Family Medicine in Turkey? Ankara Med. J. 2018, 3, 256–266. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).