COVID-19 Vaccination Trends and Side Effects among Egyptian Hemodialysis Patients: A Multicenter Survey Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
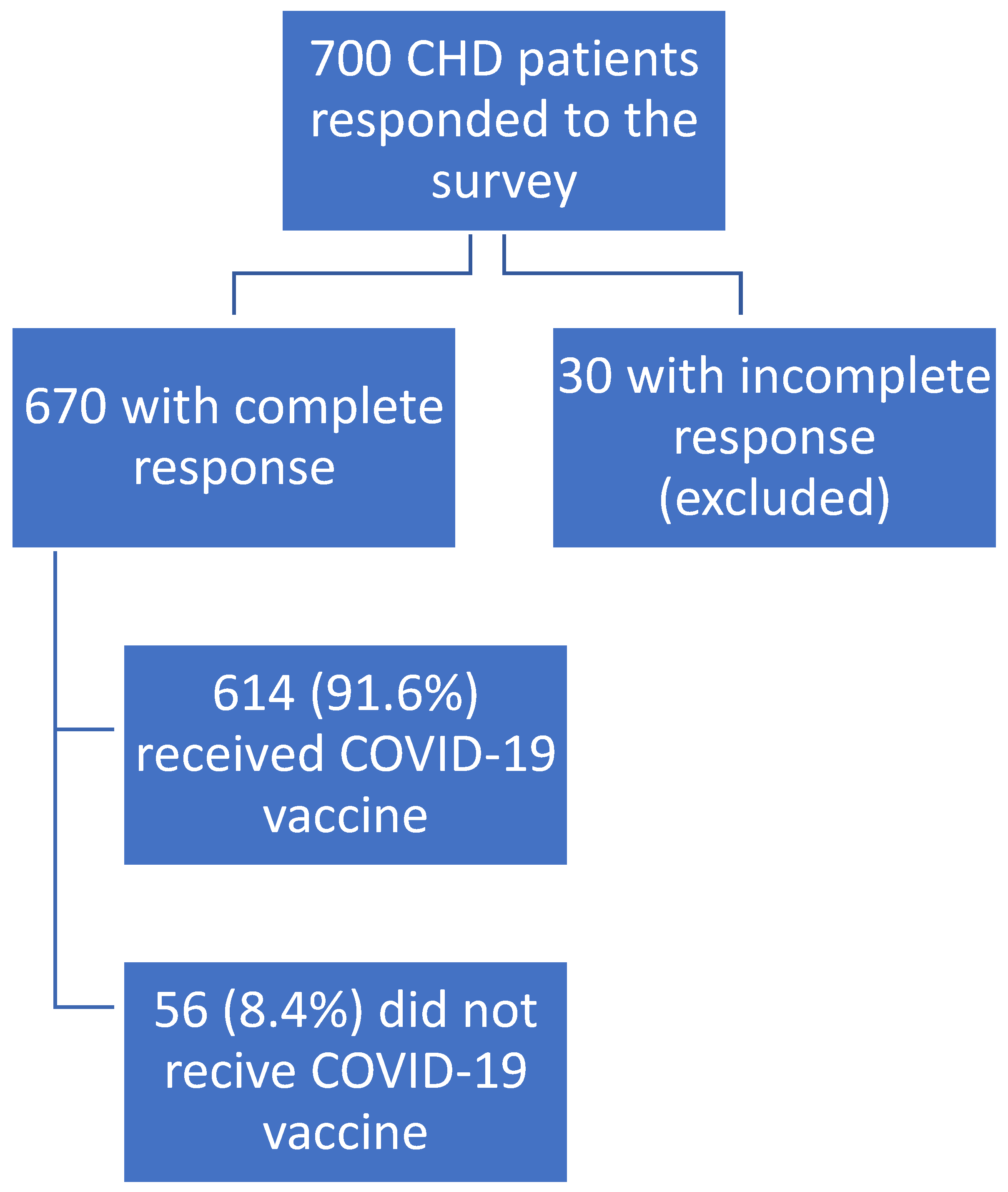
2.2. Participants
2.3. Calculation of Sample Size
2.4. The Questionnaire
Outcome Measures
2.5. Ethical Consideration
2.6. Statistical Analysis
3. Results
3.1. Study Participants’ Demographics and General Characteristics
3.2. Clinical Characteristics of COVID-19 Infection among HD Patients
3.3. COVID-19 Vaccine Related Anamnesis
3.4. COVID-19 Vaccination Status
3.5. Adverse Events of COVID-19 Vaccination
3.6. Other Data about the Adverse Events of COVID-19 Vaccine
3.7. Determinants of Adverse Events Related to COVID-19 Vaccination
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Menges, D.; Ballouz, T.; Anagnostopoulos, A.; Aschmann, H.E.; Domenghino, A.; Fehr, J.S.; Puhan, M.A. Burden of Post-COVID-19 Syndrome and Implications for Healthcare Service Planning: A Population-Based Cohort Study. PLoS ONE 2021, 16, e0254523. [Google Scholar] [CrossRef] [PubMed]
- Francis, A.; Baigent, C.; Ikizler, T.A.; Cockwell, P.; Jha, V. The Urgent Need to Vaccinate Dialysis Patients against Severe Acute Respiratory Syndrome Coronavirus 2: A Call to Action. Kidney Int. 2021, 99, 791–793. [Google Scholar] [CrossRef] [PubMed]
- Meester, J.D.; Bacquer, D.D.; Naesens, M.; Meijers, B.; Couttenye, M.M.; Vriese, A.S.D.; NBVN Kidney Registry Group. Incidence, Characteristics, and Outcome of COVID-19 in Adults on Kidney Replacement Therapy: A Regionwide Registry Study. J. Am. Soc. Nephrol. 2021, 32, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Ng, J.H.; Hirsch, J.S.; Wanchoo, R.; Sachdeva, M.; Sakhiya, V.; Hong, S.; Jhaveri, K.D.; Fishbane, S.; Abate, M.; Andrade, H.P.; et al. Outcomes of Patients with End-Stage Kidney Disease Hospitalized with COVID-19. Kidney Int. 2020, 98, 1530–1539. [Google Scholar] [CrossRef] [PubMed]
- Jager, K.J.; Kramer, A.; Chesnaye, N.C.; Couchoud, C.; Sánchez-Álvarez, J.E.; Garneata, L.; Collart, F.; Hemmelder, M.H.; Ambühl, P.; Kerschbaum, J.; et al. Results from the ERA-EDTA Registry Indicate a High Mortality Due to COVID-19 in Dialysis Patients and Kidney Transplant Recipients across Europe. Kidney Int. 2020, 98, 1540–1548. [Google Scholar] [CrossRef] [PubMed]
- Cherif, A.; Willetts, J.L.; Usvyat, L.; Wang, Y.; Kotanko, P. Comparative Analysis of SARS-CoV-2 Reproduction Rates in the Dialysis and General Populations. J. Am. Soc. Nephrol. 2021, 32, 791–794. [Google Scholar] [CrossRef]
- Nasreen, S.; Chung, H.; He, S.; Brown, K.A.; Gubbay, J.B.; Buchan, S.A.; Fell, D.B.; Austin, P.C.; Schwartz, K.L.; Sundaram, M.E.; et al. Effectiveness of MRNA and ChAdOx1 COVID-19 Vaccines against Symptomatic SARS-CoV-2 Infection and Severe Outcomes with Variants of Concern in Ontario. Nat. Microbiol. 2021, 7, 379–385. [Google Scholar] [CrossRef]
- Marzouk, M.; Elshaboury, N.; Abdel-Latif, A.; Azab, S. Deep Learning Model for Forecasting COVID-19 Outbreak in Egypt. Process Saf. Environ. Prot. 2021, 153, 363–375. [Google Scholar] [CrossRef]
- COVID-19: UN in Egypt Launches Campaign to Curb Online Rumors | United Nations in Egypt. Available online: https://egypt.un.org/en/38825-covid-19-un-egypt-launches-campaign-curb-online-rumors (accessed on 10 October 2022).
- COVID-19 Vaccination Perception and Attitude among Healthcare Workers in Egypt. Available online: https://journals.sagepub.com/doi/epub/10.1177/21501327211013303 (accessed on 10 October 2022).
- Hassaballa, M.; El-Wakil, H.; Elsharkawy, M.; Khamis, S.; El Tantawy, T.; Wahby, W.; Salem, K.; Gawad, M. Egyptian Renal Data System (ERDS) 2020: An Annual Report of End-Stage Kidney Disease Patients on Regular Hemodialysis. J. Egypt. Soc. Nephrol. Transplant. 2022, 22, 1. [Google Scholar] [CrossRef]
- World Medical Association World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA 2013, 310, 2191–2194. [CrossRef]
- El Karoui, K.; De Vriese, A.S. COVID-19 in Dialysis: Clinical Impact, Immune Response, Prevention, and Treatment. Kidney Int. 2022, 101, 883–894. [Google Scholar] [CrossRef]
- Tang, H.; Tu, C.; Xiong, F.; Sun, X.; Tian, J.-B.; Dong, J.-W.; Wang, X.-H.; Lei, C.-T.; Liu, J.; Zhao, Z.; et al. Risk Factors for the Mortality of Hemodialysis Patients with COVID-19: A Multicenter Study from the Overall Hemodialysis Population in Wuhan. Semin. Dial. 2022, 35, 71–80. [Google Scholar] [CrossRef] [PubMed]
- COVID-19 Task Force Committee of the Japanese Association of Dialysis Physicians; Japanese Society for Dialysis Therapy; Japanese Society of Nephrology; Kikuchi, K.; Nangaku, M.; Ryuzaki, M.; Yamakawa, T.; Hanafusa, N.; Sakai, K.; Kanno, Y.; et al. COVID-19 of Dialysis Patients in Japan: Current Status and Guidance on Preventive Measures. Ther. Apher. Dial. 2020, 24, 361–365. [Google Scholar] [CrossRef]
- Dhanda, S.; Osborne, V.; Lynn, E.; Shakir, S. Postmarketing Studies: Can They Provide a Safety Net for COVID-19 Vaccines in the UK? BMJ Evid. Based Med. 2022, 27, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Holt, S.G.; Mahmoud, S.; Ahmed, W.; Acuna, J.M.; Al Madani, A.K.; Eltantawy, I.; Zaher, W.A.; Goodier, G.J.; Al Kaabi, N.A.; Al Obaidli, A.A. An Analysis of Antibody Responses and Clinical Sequalae of the Sinopharm HB02 COVID19 Vaccine in Dialysis Patients in the United Arab Emirates. Nephrology 2022, 27, 260–268. [Google Scholar] [CrossRef] [PubMed]
- Zou, R.; Chen, F.; Chen, D.; Xu, C.-L.; Xiong, F. Clinical Characteristics and Outcome of Hemodialysis Patients with COVID-19: A Large Cohort Study in a Single Chinese Center. Ren. Fail. 2020, 42, 950–957. [Google Scholar] [CrossRef]
- Chen, C.-Y.; Shao, S.-C.; Chen, Y.-T.; Hsu, C.-K.; Hsu, H.-J.; Lee, C.-C.; Sun, C.-Y.; Chen, Y.-C.; Hung, M.-J.; Wu, I.-W. Incidence and Clinical Impacts of COVID-19 Infection in Patients with Hemodialysis: Systematic Review and Meta-Analysis of 396,062 Hemodialysis Patients. Healthc. Basel Switz. 2021, 9, 47. [Google Scholar] [CrossRef]
- Shakeel, C.S.; Mujeeb, A.A.; Mirza, M.S.; Chaudhry, B.; Khan, S.J. Global COVID-19 Vaccine Acceptance: A Systematic Review of Associated Social and Behavioral Factors. Vaccines 2022, 10, 110. [Google Scholar] [CrossRef]
- Sanders, J.-S.F.; Bemelman, F.J.; Messchendorp, A.L.; Baan, C.C.; van Baarle, D.; van Binnendijk, R.; Diavatopoulos, D.A.; Frölke, S.C.; Geers, D.; GeurtsvanKessel, C.H.; et al. The RECOVAC Immune-Response Study: The Immunogenicity, Tolerability, and Safety of COVID-19 Vaccination in Patients With Chronic Kidney Disease, on Dialysis, or Living With a Kidney Transplant. Transplantation 2022, 106, 821–834. [Google Scholar] [CrossRef]
- Al-Muhaiteeb, A.; AlSahow, A.; Al-Yousef, A.; AlHelal, B.; Alrajab, H.; Bahbahani, Y.; Dewidar, N.; Fanous, G.N.M. Response to and Outcomes of the Pfizer BNT162B2 Vaccine in Hemodialysis Patients—A Prospective Observational Study. Hemodial. Int. 2022, 26, 216–222. [Google Scholar] [CrossRef]
- Karlsson, L.C.; Soveri, A.; Lewandowsky, S.; Karlsson, L.; Karlsson, H.; Nolvi, S.; Karukivi, M.; Lindfelt, M.; Antfolk, J. Fearing the Disease or the Vaccine: The Case of COVID-19. Personal. Individ. Differ. 2021, 172, 110590. [Google Scholar] [CrossRef] [PubMed]
- Hatmal, M.M.; Al-Hatamleh, M.A.I.; Olaimat, A.N.; Hatmal, M.; Alhaj-Qasem, D.M.; Olaimat, T.M.; Mohamud, R. Side Effects and Perceptions Following COVID-19 Vaccination in Jordan: A Randomized, Cross-Sectional Study Implementing Machine Learning for Predicting Severity of Side Effects. Vaccines 2021, 9, 556. [Google Scholar] [CrossRef] [PubMed]
- Al Khames Aga, Q.A.; Alkhaffaf, W.H.; Hatem, T.H.; Nassir, K.F.; Batineh, Y.; Dahham, A.T.; Shaban, D.; Al Khames Aga, L.A.; Agha, M.Y.R.; Traqchi, M. Safety of COVID-19 Vaccines. J. Med. Virol. 2021, 93, 6588–6594. [Google Scholar] [CrossRef] [PubMed]
- Alhazmi, A.; Alamer, E.; Daws, D.; Hakami, M.; Darraj, M.; Abdelwahab, S.; Maghfuri, A.; Algaissi, A. Evaluation of Side Effects Associated with COVID-19 Vaccines in Saudi Arabia. Vaccines 2021, 9, 674. [Google Scholar] [CrossRef]
- Kadali, R.A.K.; Janagama, R.; Peruru, S.; Malayala, S.V. Side Effects of BNT162b2 MRNA COVID-19 Vaccine: A Randomized, Cross-Sectional Study with Detailed Self-Reported Symptoms from Healthcare Workers. Int. J. Infect. Dis. 2021, 106, 376–381. [Google Scholar] [CrossRef]
- Kanizsai, A.; Molnar, T.; Varnai, R.; Zavori, L.; Tőkés-Füzesi, M.; Szalai, Z.; Berecz, J.; Csecsei, P. Fever after Vaccination against SARS-CoV-2 with MRNA-Based Vaccine Associated with Higher Antibody Levels during 6 Months Follow-Up. Vaccines 2022, 10, 447. [Google Scholar] [CrossRef]
- Zitt, E.; Davidovic, T.; Schimpf, J.; Abbassi-Nik, A.; Mutschlechner, B.; Ulmer, H.; Benda, M.A.; Sprenger-Mähr, H.; Winder, T.; Lhotta, K. The Safety and Immunogenicity of the MRNA-BNT162b2 SARS-CoV-2 Vaccine in Hemodialysis Patients. Front. Immunol. 2021, 12, 704773. [Google Scholar] [CrossRef]
- Ramos, C.L.; Kelso, J.M. “COVID Arm”: Very Delayed Large Injection Site Reactions to MRNA COVID-19 Vaccines. J. Allergy Clin. Immunol. Pract. 2021, 9, 2480–2481. [Google Scholar] [CrossRef]
- Ursini, F.; Ruscitti, P.; Raimondo, V.; De Angelis, R.; Cacciapaglia, F.; Pigatto, E.; Olivo, D.; Di Cola, I.; Galluccio, F.; Francioso, F.; et al. Spectrum of Short-Term Inflammatory Musculoskeletal Manifestations after COVID-19 Vaccine Administration: A Report of 66 Cases. Ann. Rheum. Dis. 2022, 81, 440–441. [Google Scholar] [CrossRef]
- Chen, J.; Cai, Y.; Chen, Y.; Williams, A.P.; Gao, Y.; Zeng, J. Nervous and Muscular Adverse Events after COVID-19 Vaccination: A Systematic Review and Meta-Analysis of Clinical Trials. Vaccines 2021, 9, 939. [Google Scholar] [CrossRef]
- Terracina, K.A.; Tan, F.K. Flare of Rheumatoid Arthritis after COVID-19 Vaccination. Lancet Rheumatol. 2021, 3, e469–e470. [Google Scholar] [CrossRef]
- An, Q.; Qin, D.; Pei, J. Reactive Arthritis after COVID-19 Vaccination. Hum. Vaccines Immunother. 2021, 17, 2954–2956. [Google Scholar] [CrossRef] [PubMed]
- Ajmera, K.; Bansal, R.; Wilkinson, H.; Goyal, L. Gastrointestinal Complications of COVID-19 Vaccines. Cureus 2022, 14, e24070. [Google Scholar] [CrossRef] [PubMed]
- Bsoul, E.A.; Loomer, P.M. COVID-19 Vaccination Experience among United States Dental Professionals and Students: Safety, Confidence, Concerns, and Side Effects. PLoS ONE 2022, 17, e0264323. [Google Scholar] [CrossRef]
- Kadali, R.A.K.; Janagama, R.; Peruru, S.; Gajula, V.; Madathala, R.R.; Chennaiahgari, N.; Malayala, S.V. Non-Life-Threatening Adverse Effects with COVID-19 MRNA-1273 Vaccine: A Randomized, Cross-Sectional Study on Healthcare Workers with Detailed Self-Reported Symptoms. J. Med. Virol. 2021, 93, 4420–4429. [Google Scholar] [CrossRef]
- El-Shitany, N.A.; Harakeh, S.; Badr-Eldin, S.M.; Bagher, A.M.; Eid, B.; Almukadi, H.; Alghamdi, B.S.; Alahmadi, A.A.; Hassan, N.A.; Sindi, N.; et al. Minor to Moderate Side Effects of Pfizer-BioNTech COVID-19 Vaccine Among Saudi Residents: A Retrospective Cross-Sectional Study. Int. J. Gen. Med. 2021, 14, 1389–1401. [Google Scholar] [CrossRef]
- Abu-Hammad, O.; Alduraidi, H.; Abu-Hammad, S.; Alnazzawi, A.; Babkair, H.; Abu-Hammad, A.; Nourwali, I.; Qasem, F.; Dar-Odeh, N. Side Effects Reported by Jordanian Healthcare Workers Who Received COVID-19 Vaccines. Vaccines 2021, 9, 577. [Google Scholar] [CrossRef]
- Finsterer, J. Neurological Side Effects of SARS-CoV-2 Vaccinations. Acta Neurol. Scand. 2022, 145, 5–9. [Google Scholar] [CrossRef] [PubMed]
- McMurry, R.; Lenehan, P.; Awasthi, S.; Silvert, E.; Puranik, A.; Pawlowski, C.; Venkatakrishnan, A.J.; Anand, P.; Agarwal, V.; O’Horo, J.C.; et al. Real-Time Analysis of a Mass Vaccination Effort Confirms the Safety of FDA-Authorized MRNA COVID-19 Vaccines. Med. N. Y. 2021, 2, 965–978.e5. [Google Scholar] [CrossRef] [PubMed]
- Avcı, H.; Karabulut, B.; Eken, H.D.; Faraşoğlu, A.; Çakil, T.; Çoruk, S.; Özel, H.; Kaya, N.K.; Özbalta, S.Ö. Otolaryngology-Specific Symptoms May Be Highly Observed in Patients With a History of Covid-19 Infection After Inactivated Coronavirus Vaccination. Ear. Nose. Throat. J. 2021, 01455613211028493. [Google Scholar] [CrossRef]
- Bennet, W.M.; Elamin, A.; Newell-Price, J.D. Subacute Thyroiditis Following COVID-19 Vaccination: Case Report and Society for Endocrinology Survey. Clin. Endocrinol. 2022. [Google Scholar] [CrossRef] [PubMed]
- Kaur, R.J.; Dutta, S.; Charan, J.; Bhardwaj, P.; Tandon, A.; Yadav, D.; Islam, S.; Haque, M. Cardiovascular Adverse Events Reported from COVID-19 Vaccines: A Study Based on WHO Database. Int. J. Gen. Med. 2021, 14, 3909–3927. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, L.; Csuth, Á.; Storsaeter, J.; Garvey, L.H.; Jenmalm, M.C. Vaccine Allergy: Evidence to Consider for COVID-19 Vaccines. Curr. Opin. Allergy Clin. Immunol. 2021, 21, 401–409. [Google Scholar] [CrossRef]
- Ripabelli, G.; Tamburro, M.; Buccieri, N.; Adesso, C.; Caggiano, V.; Cannizzaro, F.; Di Palma, M.A.; Mantuano, G.; Montemitro, V.G.; Natale, A.; et al. Active Surveillance of Adverse Events in Healthcare Workers Recipients After Vaccination with COVID-19 BNT162b2 Vaccine (Pfizer-BioNTech, Comirnaty): A Cross-Sectional Study. J. Community Health 2022, 47, 211–225. [Google Scholar] [CrossRef]
- Saeed, B.Q.; Al-Shahrabi, R.; Alhaj, S.S.; Alkokhardi, Z.M.; Adrees, A.O. Side Effects and Perceptions Following Sinopharm COVID-19 Vaccination. Int. J. Infect. Dis. 2021, 111, 219–226. [Google Scholar] [CrossRef] [PubMed]
- Klein, S.L.; Pekosz, A. Sex-Based Biology and the Rational Design of Influenza Vaccination Strategies. J. Infect. Dis. 2014, 209, S114–S119. [Google Scholar] [CrossRef] [Green Version]
- Müller, L.; Andrée, M.; Moskorz, W.; Drexler, I.; Walotka, L.; Grothmann, R.; Ptok, J.; Hillebrandt, J.; Ritchie, A.; Rabl, D.; et al. Age-Dependent Immune Response to the Biontech/Pfizer BNT162b2 Coronavirus Disease 2019 Vaccination. Clin. Infect. Dis. 2021, 73, 2065–2072. [Google Scholar] [CrossRef]
- Naaber, P.; Tserel, L.; Kangro, K.; Sepp, E.; Jürjenson, V.; Adamson, A.; Haljasmägi, L.; Rumm, A.P.; Maruste, R.; Kärner, J.; et al. Dynamics of Antibody Response to BNT162b2 Vaccine after Six Months: A Longitudinal Prospective Study. Lancet Reg. Health Eur. 2021, 10, 100208. [Google Scholar] [CrossRef]


| Variable Mean ± SD, n (%) | HD Patients (n = 670) |
|---|---|
| Demographic data | |
| Gender | |
| Male | 389 (58.1) |
| Female | 281 (41.9) |
| Age (years) | 50.79 ± 15.9 |
| Marital status | |
| Single | 77 (11.5) |
| Married | 523 (78.1) |
| Widowed | 58 (8.7) |
| Divorced | 12 (1.8) |
| Education level | |
| Illiterate | 387 (57.8) |
| Primary | 85 (12.7) |
| High school/diploma | 145 (21.6) |
| College level | 47 (7) |
| Postgraduate (masters/doctorate) | 6 (0.9) |
| Employment status | |
| Unemployed | 513 (76.6) |
| Employed | 83 (12.4) |
| Retired | 68 (10.1) |
| Student | 6 (0.9) |
| Residence | |
| Urban | 416 (62.1) |
| Rural | 254 (37.9) |
| Smoking habit | |
| Non-smoker | 540 (80.6) |
| Smoker | 85 (12.7) |
| Ex-smoker | 45 (6.7) |
| Socioeconomic status | |
| Low | 239 (35.7) |
| Average | 417 (62.2) |
| High | 14 (2.1) |
| Anthropometric measures | |
| Weight (Kg) | 73.94 ± 20.21 |
| Height (m) | 163.07 ± 11.25 |
| BMI (Kg/m2) | 27.76 ± 7.17 |
| Clinical data | |
| Duration of hemodialysis (years) | 5 (2–10) |
| Associated comorbidities | |
| No | 166 (24.8) |
| Diabetes | 64 (9.6) |
| Hypertension | 430 (64.2) |
| Chronic anemia | 178 (26.6) |
| Heart disease | 26 (3.9) |
| Liver disease | 3 (0.4) |
| Chronic respiratory disease | 4 (0.6) |
| Autoimmune disease | 2 (0.3) |
| Cancer | 14 (2.1) |
| Therapeutic data | |
| None | 66 (9.9) |
| Erythropoietin | 522 (77.9) |
| Iron supplementation | 455 (67.9) |
| Calcium supplementation | 479 (71.5) |
| Alpha calcidol | 483 (72.1) |
| Calcimimetics | 26 (3.9) |
| Aluminum hydroxide | 61 (9.1) |
| Antihypertensive drugs | 374 (55.8) |
| Antidiabetic drugs | 37 (5.5) |
| Immunosuppressive drugs | 1 (0.1) |
| Variable | HD Patients with Prior COVID-19 Infection (n = 173) n (%) |
|---|---|
| Prior COVID-19 contact | 34 (19.7) |
| Symptoms associated with COVID-19 infection | |
| Fever | 127 (73.4) |
| Fatigue | 41 (23.7) |
| Cough | 61 (35.3) |
| Skin rash | 2 (1.2) |
| Diarrhea | 20 (11.6) |
| Pneumonia | 18 (10.4) |
| Dyspnea | 29 (16.8) |
| Headache | 30 (17.3) |
| Chest pain | 14 (8.1) |
| Oral ulcers | 5 (2.9) |
| Anorexia/vomiting | 17 (9.8) |
| Joint pain | 18 (10.4) |
| Hospitalization during COVID-19 infection | |
| No, with no need for oxygen | 146 (84.4) |
| No, with a need for oxygen | 3 (1.7) |
| Yes, with no need for oxygen | 19 (11) |
| Yes, with a need for oxygen | 5 (2.9) |
| ICU admission during COVID-19 infection | 6 (3.5) |
| Duration of symptoms related to COVID-19 infection (days) | 3 (2–7) |
| Variable | Vaccinated CHD Patients (n = 614) | ||
|---|---|---|---|
| After the First Dose Only n (%) | After the Second Dose Only n (%) | After the First and Second Doses n (%) | |
| General side effects | |||
| Generalized weakness/fatigue | 344 (56) | 4 (0.7) | 20 (3.3) |
| Headache | 269 (43.8) | 4 (0.7) | 8 (1.3) |
| Fever | 248 (40.4) | 4 (0.7) | 4 (0.7) |
| Localized symptom/s | |||
| Sore arm/pain | 180 (29.3) | 10 (1.6) | 103 (16.8) |
| Localized swelling at the injection site | 32 (5.2) | 9 (1.5) | 2 (0.3) |
| Itching | 22 (3.6) | 1 (0.2) | 4 (0.7) |
| Lymphadenopathy (axillary or regional) | 3 (0.5) | 0 | 0 |
| Rash | 3 (0.5) | 0 | 1 (0.2) |
| Musculoskeletal symptom/s | |||
| Muscle pain/myalgia | 90 (14.7) | 2 (0.3) | 9 (1.5) |
| Arthritis/joint pains | 55 (9) | 2 (0.3) | 3 (0.5) |
| Muscle stiffness/spasm | 0 | 0 | 1 (0.2) |
| Gastrointestinal symptom/s | |||
| Nausea | 25 (4.1) | 1 (0.2) | 2 (0.3) |
| Decreased appetite | 154 (25.1) | 1 (0.2) | 4 (0.7) |
| Diarrhea | 13 (2.1) | 2 (0.3) | 1 (0.2) |
| Abdominal pain | 46 (7.5) | 4 (0.7) | 1 (0.2) |
| Vomiting | 3 (0.5) | 0 | 0 |
| Heartburn | 25 (4.1) | 4 (0.7) | 3 (0.5) |
| Psychological and/or psychiatric symptom/s | |||
| Feelings of joy/relief/gratitude | 7 (1.1) | 0 | 3 (0.5) |
| Anxiety | 156 (25.4) | 1 (0.2) | 3 (0.5) |
| Increase in sleep | 57 (9.3) | 0 | 6 (1) |
| Psychological stress | 79 (12.9) | 0 | 1 (0.2) |
| Decrease in memory | 12 (2) | 0 | 1 (0.2) |
| Neurological symptom/s | |||
| Brain fogging or reduced mental clarity | 10 (1.6) | 0 | 3 (0.5) |
| Tingling | 105 (17.1) | 0 | 4 (0.7) |
| Vertigo-like symptoms | 53 (8.6) | 1 (0.2) | 0 |
| Paralysis/extremity weakness | 24 (3.9) | 0 | 1 (0.2) |
| Incoordination | 64 (10.4) | 0 | 3 (0.5) |
| Reactivation of shingles | 3 (0.5) | 0 | 0 |
| Head/ear/eyes/nose/throat symptom/s | |||
| Nasal stuffiness | 54 (8.8) | 1 (0.2) | 0 |
| Sore throat | 69 (11.2) | 0 | 1 (0.2) |
| Runny nose | 17 (2.8) | 2 (0.3) | 0 |
| Ringing sensation in ears | 4 (0.7) | 1 (0.2) | 1 (0.2) |
| Ear pain | 5 (0.8) | 0 | 0 |
| Eye pain | 5 (0.8) | 1 (0.2) | 1 (0.2) |
| Blurring of vision | 3 (0.5) | 0 | 1 (0.2) |
| Endocrine symptom/s | |||
| Decreased appetite | 138 (22.5) | 1 (0.2) | 6 (1) |
| Heat/cold intolerance | 60 (9.8) | 1 (0.2) | 3 (0.5) |
| Increased thirst | 118 (19.2) | 0 | 6 (1) |
| Increased appetite | 9 (1.5) | 1 (0.2) | 0 |
| Cardiovascular symptom/s | |||
| Palpitations | 47 (7.7) | 1 (0.2) | 2 (0.3) |
| Chest pain | 88 (14.3) | 0 | 5 (0.8) |
| Blood pressure changes | 75 (12.2) | 1 (0.2) | 10 (1.6) |
| Respiratory symptom/s | |||
| Shortness of breath | 91 (14.8) | 2 (0.3) | 4 (0.7) |
| Cough | 6 (1) | 3 (0.5) | 0 |
| Wheezing | 1 (0.2) | 0 | 0 |
| Allergic symptom/s | |||
| Rash | 5 (0.8) | 0 | 3 (0.5) |
| Hives | 4 (0.7) | 0 | 2 (0.3) |
| Swelling in mouth/throat | 2 (0.3) | 0 | 0 |
| Atopic eczema | 2 (0.3) | 0 | 0 |
| Swelling of lips or tongue | 1 (0.2) | 0 | 0 |
| Variable n (%), Median (min–max) | Vaccinated CHD Patients (n = 614) |
|---|---|
| Intensity of symptoms (VAS) | 3 (0–5) |
| Timing of adverse events | |
| Onset of symptoms post-vaccine (days) | 1 (1–2) |
| Timing of maximum symptoms (days after vaccination) | 2 (1–3) |
| Duration of symptoms (days) (patency period) | 3 (1–5) |
| Activity or need for medical attention | |
| Trouble to perform regular daily living activities temporarily | 396 (64.5) |
| Required transient time off from work | 26 (4.2) |
| Required to seek help from outpatient provider | 3 (0.5) |
| Required to seek help from emergency department provider | 1 (0.2) |
| Required hospitalization and subsequent inpatient care | 2 (0.3) |
| Variable | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | |
| Constant | - | 70.586 | 0.000 | |||
| Male gender | 1.848 | 1.242–2.749 | 0.002 * | 0.793 | 0.284–2.215 | 0.658 |
| Age | 0.981 | 0.969–0.993 | 0.003 * | 0.959 | 0.936–0.983 | 0.001 * |
| Weight | 0.996 | 0.987–1.005 | 0.412 | 0.962 | 0.921–1.004 | 0.079 |
| BMI | 1.005 | 0.976–1.034 | 0.759 | 1.156 | 1.029–1.298 | 0.014 * |
| Residence (urban) | 6.629 | 4.408–9.967 | <0.001 * | 0.809 | 0.380–1.724 | 0.583 |
| Smoking | 6.067 | 3.514–10.475 | <0.001 * | 0.203 | 0.081–0.512 | 0.001 * |
| Duration since starting HD | 0.998 | 0.998–0.999 | <0.001 * | 0.999 | 0.998–0.999 | <0.001 * |
| Calcium supplementation | 2.282 | 1.517–3.432 | <0.001 * | 0.415 | 0.178–0.967 | 0.042 * |
| Antihypertensive medications | 3.595 | 2.418–5.344 | <0.001 * | 0.403 | 0.196–0.826 | 0.013 * |
| Associated comorbidities | 2.202 | 1.478–3.281 | <0.001 * | 0.330 | 0.139–0.783 | 0.012 * |
| Prior COVID-19 infection | 3.318 | 1.952–5.642 | <0.001 * | 1.295 | 0.531–3.158 | 0.570 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nassar, M.K.; Salem, K.M.; Elgamal, M.; Abdel-Gawad, S.M.; Tharwat, S. COVID-19 Vaccination Trends and Side Effects among Egyptian Hemodialysis Patients: A Multicenter Survey Study. Vaccines 2022, 10, 1771. https://doi.org/10.3390/vaccines10101771
Nassar MK, Salem KM, Elgamal M, Abdel-Gawad SM, Tharwat S. COVID-19 Vaccination Trends and Side Effects among Egyptian Hemodialysis Patients: A Multicenter Survey Study. Vaccines. 2022; 10(10):1771. https://doi.org/10.3390/vaccines10101771
Chicago/Turabian StyleNassar, Mohammed Kamal, Karem Mohamed Salem, Mohamed Elgamal, Sara M. Abdel-Gawad, and Samar Tharwat. 2022. "COVID-19 Vaccination Trends and Side Effects among Egyptian Hemodialysis Patients: A Multicenter Survey Study" Vaccines 10, no. 10: 1771. https://doi.org/10.3390/vaccines10101771
APA StyleNassar, M. K., Salem, K. M., Elgamal, M., Abdel-Gawad, S. M., & Tharwat, S. (2022). COVID-19 Vaccination Trends and Side Effects among Egyptian Hemodialysis Patients: A Multicenter Survey Study. Vaccines, 10(10), 1771. https://doi.org/10.3390/vaccines10101771






