A Novel Approach to Vaccine Development: Concomitant Pathogen Inactivation and Host Immune Stimulation by Peroxynitrite
Abstract
:1. Introduction
2. Materials and Methods
2.1. Bacteria
2.2. Peroxynitrite-Induced Bacterial Inactivation
2.3. Formalin-Induced Bacterial Inactivation
2.4. Reduction of Nitrotyrosine Residues of the Peroxynitrite-Inactivated LVS Preparation
2.5. Western Blot Analysis
2.6. Cells
2.7. Cytokine Analysis
2.8. Flow Cytometry
2.9. ELISPOT Assays
2.10. Mice
2.11. Statistical Analysis
3. Results and Discussion
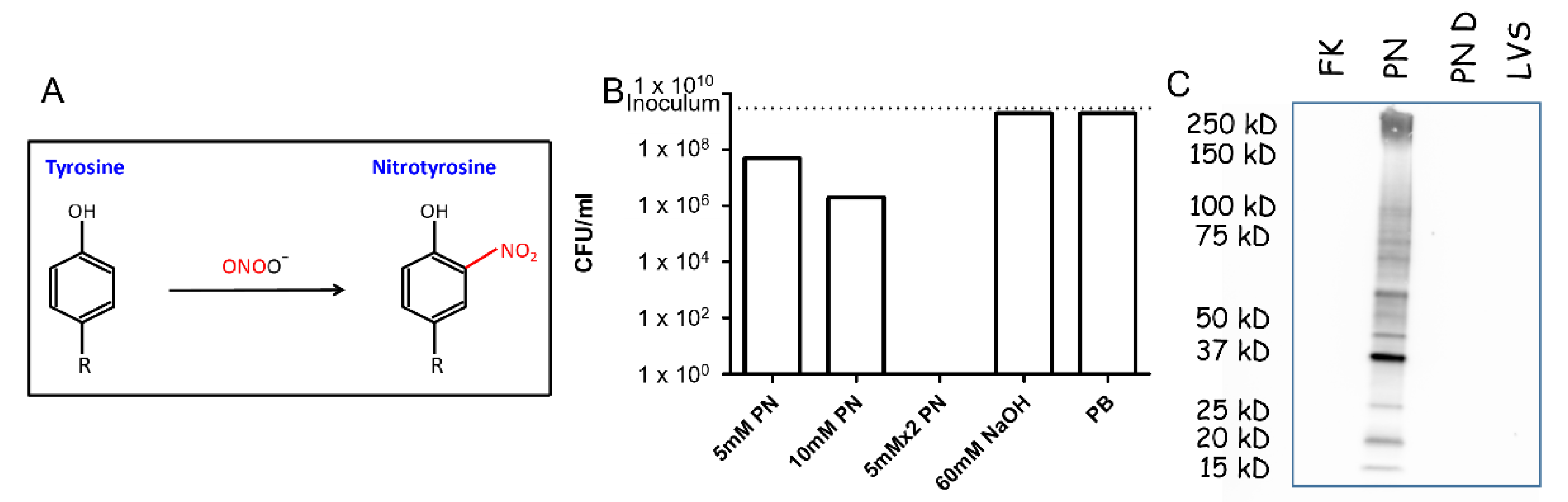
3.1. PN Treatment Results in NT Formation and Inactivation of F. tularensis Bacteria
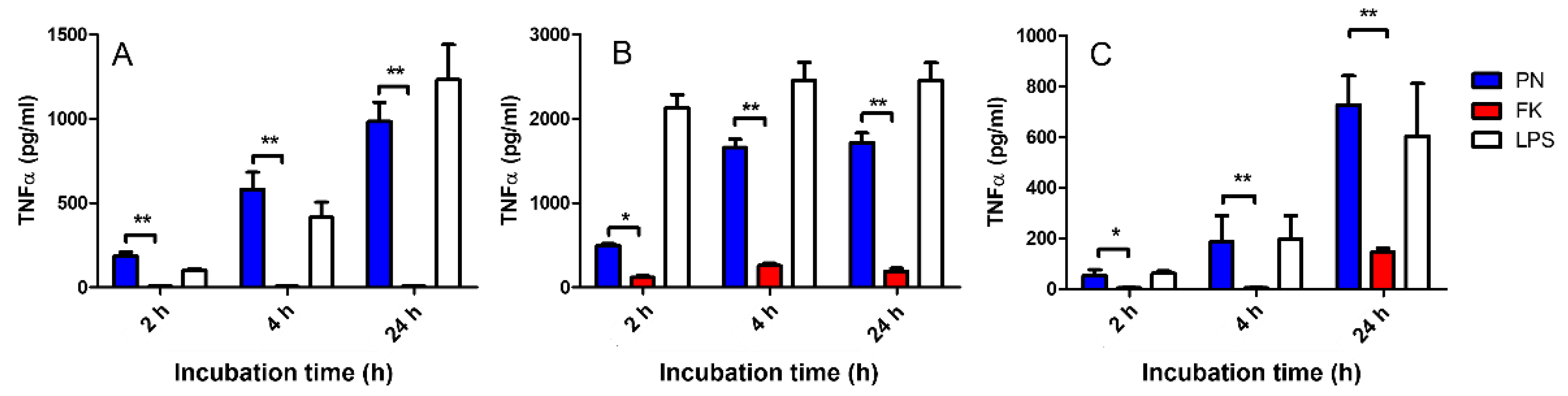
3.2. Activation of Innate Immune Mechanisms by PN-Neutralized Whole Bacteria
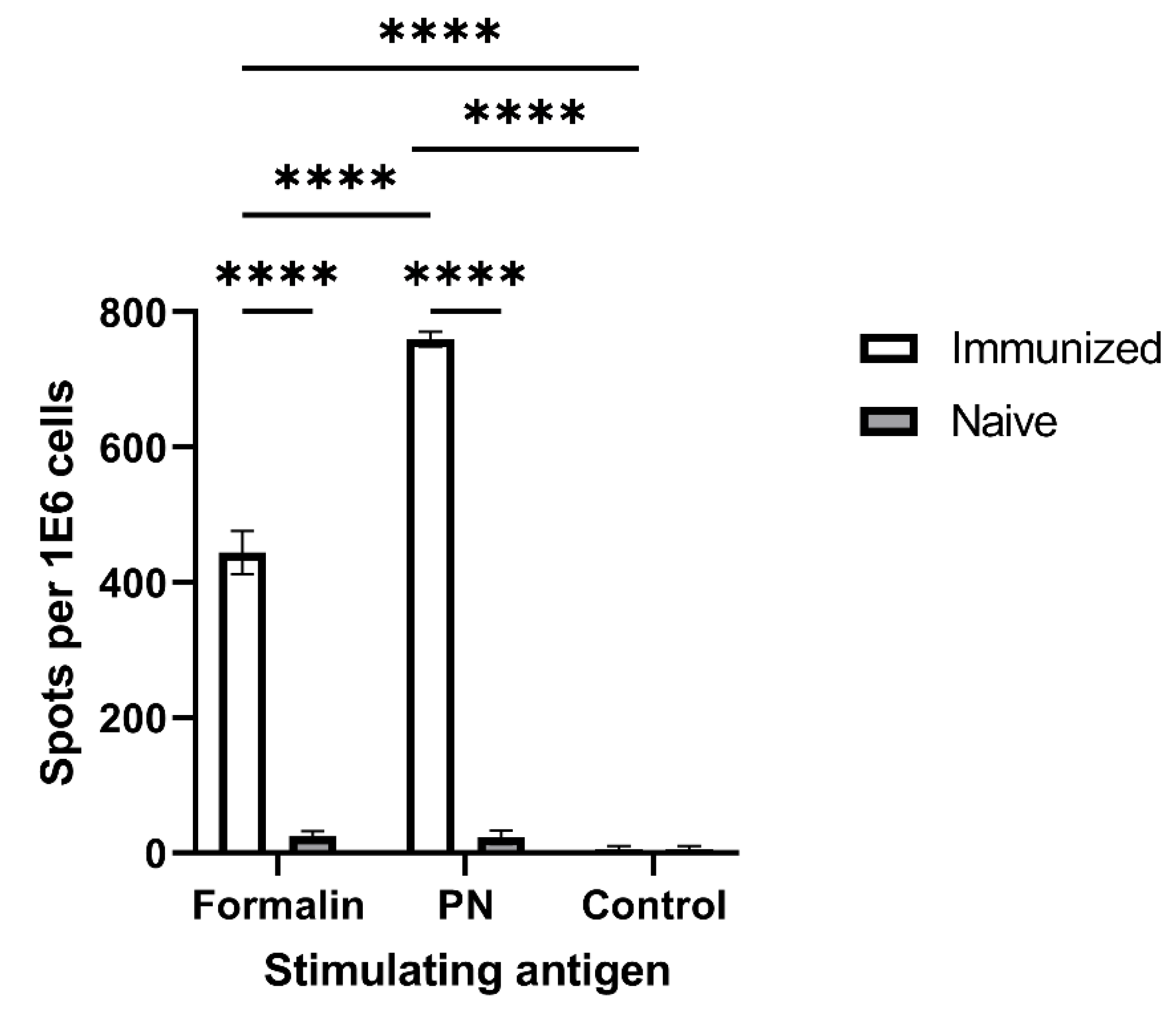
3.3. Antigenicity Assessment of PN-Neutralized F. tularensis by ELISPOT
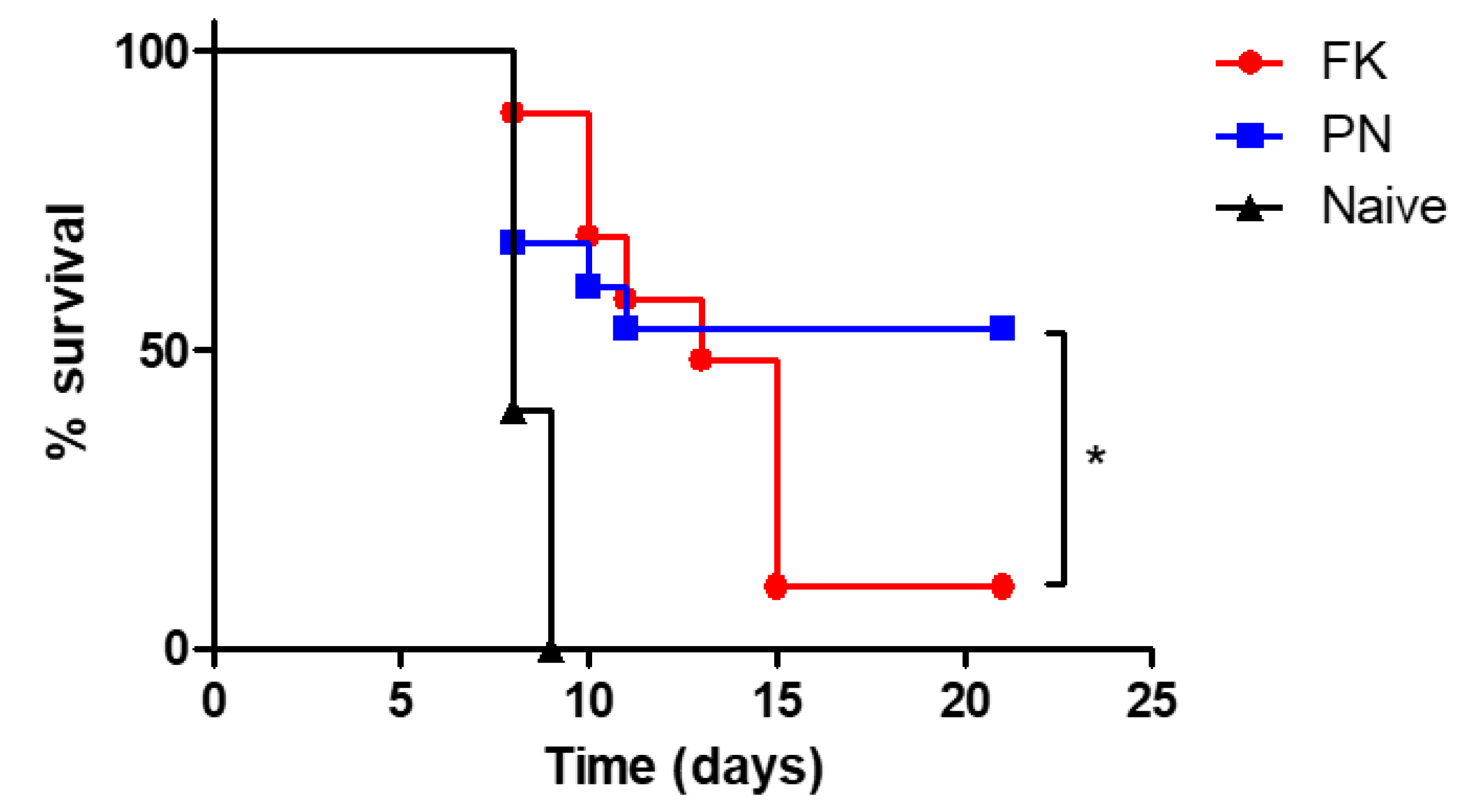
3.4. In Vivo Assessment of Protective Immunity Following Vaccination with Neutralized Bacteria
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tlaxca, J.L.; Ellis, S.; Remmele, R.L. Live Attenuated and Inactivated Viral Vaccine Formulation and Nasal Delivery: Potential and Challenges. Adv. Drug Deliv. Rev. 2015, 93, 56–78. [Google Scholar] [CrossRef] [PubMed]
- Roth, G.A.; Picece, V.C.T.M.; Ou, B.S.; Luo, W.; Pulendran, B.; Appel, E.A. Designing Spatial and Temporal Control of Vaccine Responses. Nat. Rev. Mater. 2022, 7, 174–195. [Google Scholar] [CrossRef] [PubMed]
- Plotkin, S.A.; Plotkin, S.L. The Development of Vaccines: How the Past Led to the Future. Nat. Rev. Microbiol. 2011, 9, 889–893. [Google Scholar] [CrossRef] [PubMed]
- Munoz, F.M.; Cramer, J.P.; Dekker, C.L.; Dudley, M.Z.; Graham, B.S.; Gurwith, M.; Law, B.; Perlman, S.; Polack, F.P.; Spergel, J.M.; et al. Vaccine-Associated Enhanced Disease: Case Definition and Guidelines for Data Collection, Analysis, and Presentation of Immunization Safety Data. Vaccine 2021, 39, 3053–3066. [Google Scholar] [CrossRef] [PubMed]
- Killikelly, A.M.; Kanekiyo, M.; Graham, B.S. Pre-Fusion F Is Absent on the Surface of Formalin-Inactivated Respiratory Syncytial Virus. Sci. Rep. 2016, 6, 34108. [Google Scholar] [CrossRef] [PubMed]
- Gupta, D.; Parthasarathy, H.; Sah, V.; Tandel, D.; Vedagiri, D.; Reddy, S.; Harshan, K.H. Inactivation of SARS-CoV-2 by β-Propiolactone Causes Aggregation of Viral Particles and Loss of Antigenic Potential. Virus Res. 2021, 305, 198555. [Google Scholar] [CrossRef] [PubMed]
- Bogdan, C.; Röllinghoff, M.; Diefenbach, A. Reactive Oxygen and Reactive Nitrogen Intermediates in Innate and Specific Immunity. Curr. Opin. Immunol. 2000, 12, 64–76. [Google Scholar] [CrossRef]
- Beckman, J.S.; Koppenol, W.H. Nitric Oxide, Superoxide, and Peroxynitrite: The Good, the Bad, and Ugly. Am. J. Physiol. 1996, 271, C1424–C1437. [Google Scholar] [CrossRef]
- Kuwahara, H.; Miyamoto, Y.; Akaike, T.; Kubota, T.; Sawa, T.; Okamoto, S.; Maeda, H. Helicobacter pylori Urease Suppresses Bactericidal Activity of Peroxynitrite via Carbon Dioxide Production. Infect. Immun. 2000, 68, 4378–4383. [Google Scholar] [CrossRef]
- Tecder-Unal, M.; Can, F.; Demirbilek, M.; Karabay, G.; Tufan, H.; Arslan, H. The Bactericidal and Morphological Effects of Peroxynitrite on Helicobacter pylori. Helicobacter 2008, 13, 42–48. [Google Scholar] [CrossRef]
- Evans, T.J.; Buttery, L.D.; Carpenter, A.; Springall, D.R.; Polak, J.M.; Cohen, J. Cytokine-Treated Human Neutrophils Contain Inducible Nitric Oxide Synthase That Produces Nitration of Ingested Bacteria. Proc. Natl. Acad. Sci. USA 1996, 93, 9553–9558. [Google Scholar] [CrossRef] [PubMed]
- Alam, M.S.; Akaike, T.; Okamoto, S.; Kubota, T.; Yoshitake, J.; Sawa, T.; Miyamoto, Y.; Tamura, F.; Maeda, H. Role of Nitric Oxide in Host Defense in Murine Salmonellosis as a Function of Its Antibacterial and Antiapoptotic Activities. Infect. Immun. 2002, 70, 3130–3142. [Google Scholar] [CrossRef] [PubMed]
- Satoh, S.; Oishi, K.; Iwagaki, A.; Senba, M.; Akaike, T.; Akiyama, M.; Mukaida, N.; Atsushima, K.M.; Nagatake, T. Dexamethasone Impairs Pulmonary Defence against Pseudomonas aeruginosa through Suppressing INOS Gene Expression and Peroxynitrite Production in Mice. Clin. Exp. Immunol. 2001, 126, 266–273. [Google Scholar] [CrossRef] [PubMed]
- Zhu, L.; Gunn, C.; Beckman, J.S. Bactericidal Activity of Peroxynitrite. Arch. Biochem. Biophys. 1992, 298, 452–457. [Google Scholar] [CrossRef]
- De Groote, M.A.; Granger, D.; Xu, Y.; Campbell, G.; Prince, R.; Fang, F.C. Genetic and Redox Determinants of Nitric Oxide Cytotoxicity in a Salmonella Typhimurium Model. Proc. Natl. Acad. Sci. USA 1995, 92, 6399–6403. [Google Scholar] [CrossRef] [PubMed]
- Shiloh, M.U.; MacMicking, J.D.; Nicholson, S.; Brause, J.E.; Potter, S.; Marino, M.; Fang, F.; Dinauer, M.; Nathan, C. Phenotype of Mice and Macrophages Deficient in Both Phagocyte Oxidase and Inducible Nitric Oxide Synthase. Immunity 1999, 10, 29–38. [Google Scholar] [CrossRef]
- Fang, F.C. Antimicrobial Reactive Oxygen and Nitrogen Species: Concepts and Controversies. Nat. Rev. Microbiol. 2004, 2, 820–832. [Google Scholar] [CrossRef]
- Chakravortty, D.; Hensel, M. Inducible Nitric Oxide Synthase and Control of Intracellular Bacterial Pathogens. Microbes Infect. 2003, 5, 621–627. [Google Scholar] [CrossRef]
- Linares, E.; Giorgio, S.; Augusto, O. Inhibition of in Vivo Leishmanicidal Mechanisms by Tempol: Nitric Oxide down-Regulation and Oxidant Scavenging. Free Radic. Biol. Med. 2008, 44, 1668–1676. [Google Scholar] [CrossRef]
- Ischiropoulos, H.; Al-Mehdi, A.B. Peroxynitrite-Mediated Oxidative Protein Modifications. FEBS Lett. 1995, 364, 279–282. [Google Scholar] [CrossRef] [Green Version]
- Halliwell, B. What Nitrates Tyrosine? Is Nitrotyrosine Specific as a Biomarker of Peroxynitrite Formation in Vivo? FEBS Lett. 1997, 411, 157–160. [Google Scholar] [CrossRef]
- Gauba, V.; Grünewald, J.; Gorney, V.; Deaton, L.M.; Kang, M.; Bursulaya, B.; Ou, W.; Lerner, R.A.; Schmedt, C.; Geierstanger, B.H.; et al. Loss of CD4 T-Cell–Dependent Tolerance to Proteins with Modified Amino Acids. Proc. Natl. Acad. Sci. USA 2011, 108, 12821–12826. [Google Scholar] [CrossRef] [PubMed]
- Birnboim, H.C.; Lemay, A.-M.; Lam, D.K.Y.; Goldstein, R.; Webb, J.R. Cutting Edge: MHC Class II-Restricted Peptides Containing the Inflammation-Associated Marker 3-Nitrotyrosine Evade Central Tolerance and Elicit a Robust Cell-Mediated Immune Response. J. Immunol. 2003, 171, 528–532. [Google Scholar] [CrossRef] [PubMed]
- Madhurantakam, C.; Duru, A.D.; Sandalova, T.; Webb, J.R.; Achour, A. Inflammation-Associated Nitrotyrosination Affects TCR Recognition through Reduced Stability and Alteration of the Molecular Surface of the MHC Complex. PLoS ONE 2012, 7, e32805. [Google Scholar] [CrossRef]
- Khan, M.A.; Dixit, K.; Jabeen, S.; Moinuddin; Alam, K. Impact of Peroxynitrite Modification on Structure and Immunogenicity of H2A Histone. Scand. J. Immunol. 2009, 69, 99–109. [Google Scholar] [CrossRef]
- Gruijthuijsen, Y.K.; Grieshuber, I.; Stöcklinger, A.; Tischler, U.; Fehrenbach, T.; Weller, M.G.; Vogel, L.; Vieths, S.; Pöschl, U.; Duschl, A. Nitration Enhances the Allergenic Potential of Proteins. Int. Arch. Allergy Immunol. 2006, 141, 265–275. [Google Scholar] [CrossRef]
- Telford, S.R.; Goethert, H.K. Ecology of Francisella tularensis. Annu. Rev. Entomol. 2020, 65, 351–372. [Google Scholar] [CrossRef]
- Jia, Q.; Horwitz, M.A. Live Attenuated Tularemia Vaccines for Protection Against Respiratory Challenge with Virulent F. tularensis Subsp. tularensis. Front. Cell. Infect. Microbiol. 2018, 8, 154. [Google Scholar] [CrossRef]
- Steiner, D.J.; Furuya, Y.; Metzger, D.W. Host-Pathogen Interactions and Immune Evasion Strategies in Francisella tularensis Pathogenicity. Infect. Drug Resist. 2014, 7, 239–251. [Google Scholar] [CrossRef]
- Bosio, C.M. The Subversion of the Immune System by Francisella tularensis. Front. Microbiol. 2011, 2, 9. [Google Scholar] [CrossRef] [Green Version]
- Oyston, P.C.F. Francisella tularensis Vaccines. Vaccine 2009, 27, D48–D51. [Google Scholar] [CrossRef] [PubMed]
- Lutz, M.B.; Kukutsch, N.; Ogilvie, A.L.; Rössner, S.; Koch, F.; Romani, N.; Schuler, G. An Advanced Culture Method for Generating Large Quantities of Highly Pure Dendritic Cells from Mouse Bone Marrow. J. Immunol. Methods 1999, 223, 77–92. [Google Scholar] [CrossRef]
- Liu, T.; Zhang, L.; Joo, D.; Sun, S.-C. NF-ΚB Signaling in Inflammation. Signal Transduct. Target. Ther. 2017, 2, 17023. [Google Scholar] [CrossRef] [PubMed]
- Griffin, K.F.; Oyston, P.C.F.; Titball, R.W. Francisella tularensis Vaccines. FEMS Immunol. Med. Microbiol. 2007, 49, 315–323. [Google Scholar] [CrossRef] [PubMed]
- Conlan, J.; Sjöstedt, A.; Gelhaus, H.; Fleming, P.; McRae, K.; Cobb, R.; De Pascalis, R.; Elkins, K. Modern Development and Production of a New Live Attenuated Bacterial Vaccine, SCHU S4 ΔclpB, to Prevent Tularemia. Pathogens 2021, 10, 795. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rotem, S.; Bar-Haim, E.; Elia, U.; Cohen, H.; Lazar, S.; Cohen, O.; Chitlaru, T.; Gal, Y. A Novel Approach to Vaccine Development: Concomitant Pathogen Inactivation and Host Immune Stimulation by Peroxynitrite. Vaccines 2022, 10, 1593. https://doi.org/10.3390/vaccines10101593
Rotem S, Bar-Haim E, Elia U, Cohen H, Lazar S, Cohen O, Chitlaru T, Gal Y. A Novel Approach to Vaccine Development: Concomitant Pathogen Inactivation and Host Immune Stimulation by Peroxynitrite. Vaccines. 2022; 10(10):1593. https://doi.org/10.3390/vaccines10101593
Chicago/Turabian StyleRotem, Shahar, Erez Bar-Haim, Uri Elia, Hila Cohen, Shirley Lazar, Ofer Cohen, Theodor Chitlaru, and Yoav Gal. 2022. "A Novel Approach to Vaccine Development: Concomitant Pathogen Inactivation and Host Immune Stimulation by Peroxynitrite" Vaccines 10, no. 10: 1593. https://doi.org/10.3390/vaccines10101593




