Vaccine Hesitancy: Contemporary Issues and Historical Background
Abstract
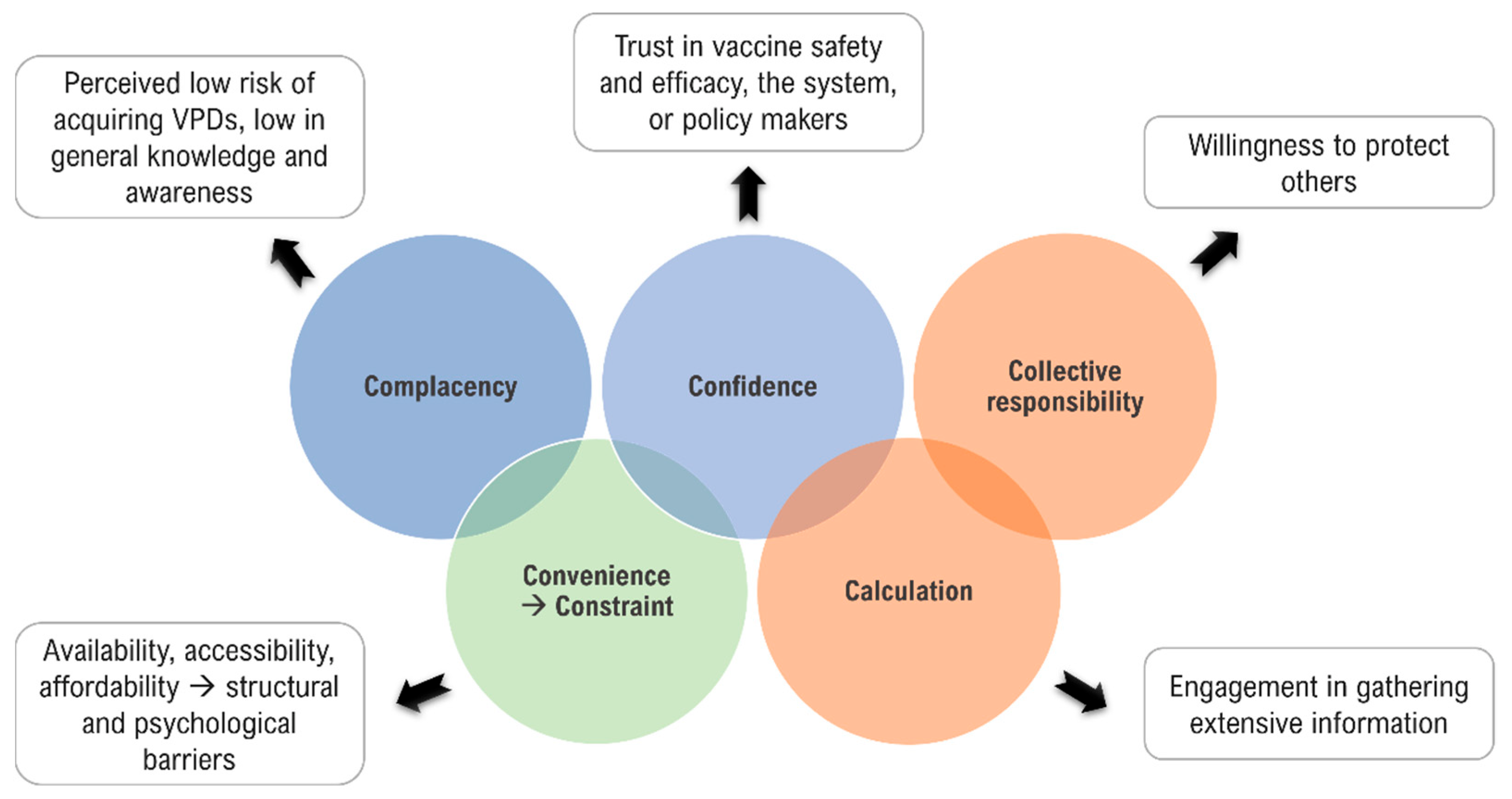
1. Definition and Theoretical Framework
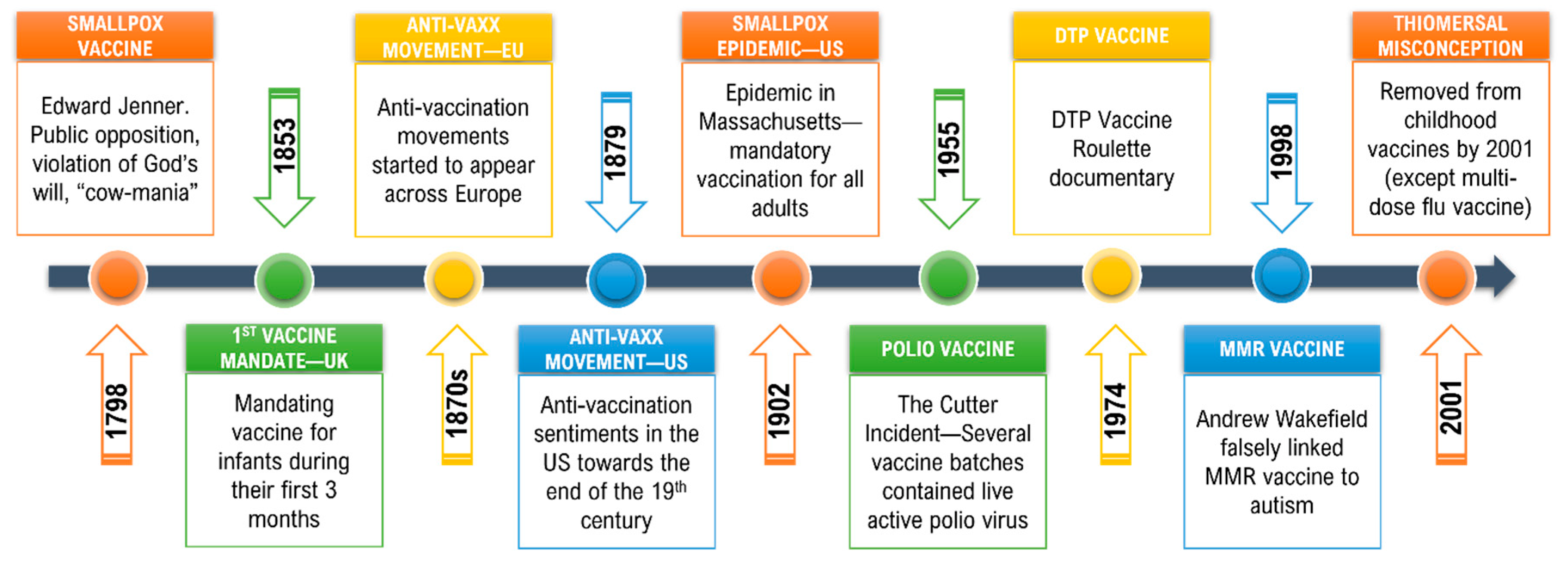
2. Early Vaccine Hesitancy
3. Vaccine Hesitancy and Anti-Vaccine Movement(s) in the Modern Era
3.1. Polio Vaccine: The Cutter Incident and Simian Virus 40 (SV40)
3.2. Swine Flu Vaccine and Guillain-Barré Syndrome (GBS)
3.3. The Diphtheria, Tetanus, and Pertussis (DTP) Vaccine Controversy
3.4. The Measles, Mumps, and Rubella (MMR) Vaccine Controversy
3.5. Thiomersal Controversy
4. Drivers of Vaccine Hesitancy
4.1. Heuristics and Vaccine Hesitancy
4.2. Concerns Regarding Vaccine Safety and Efficacy
4.3. Internet and Social Media Influence
4.4. Mandatory Vaccination and Public Health Policies
4.5. Vaccine Hesitancy in the COVID-19 Era
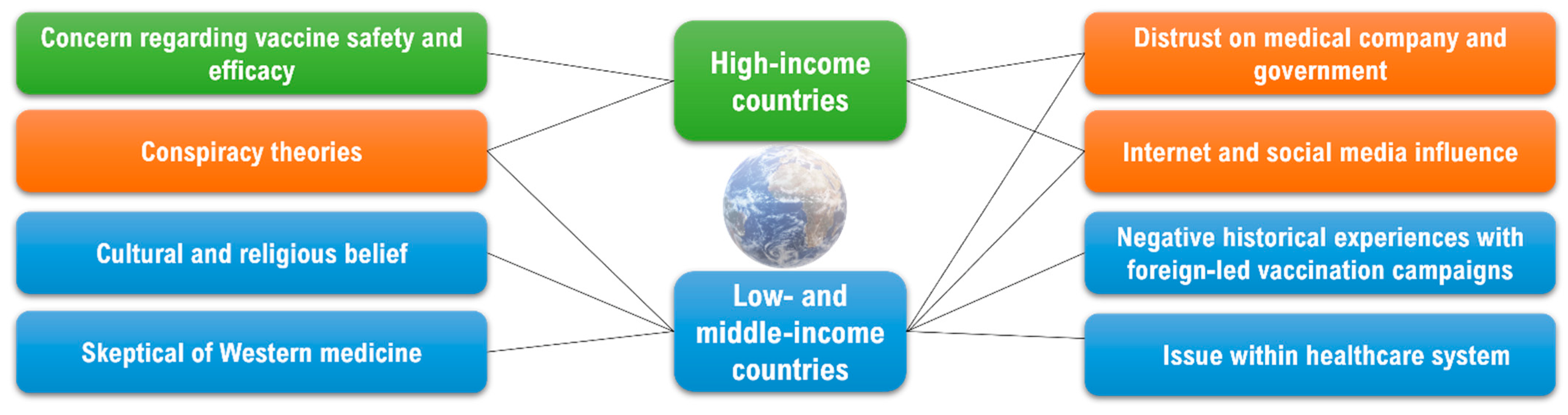
5. Vaccine Hesitancy across Different Countries, Cultures, and Socio-Economic Groups
5.1. Vaccine Hesitancy in High-Income Countries (HICs)
5.2. Vaccine Hesitancy in Low- and Middle-Income Countries (LMICs)
6. Measures to Counteract Vaccine Hesitancy
6.1. Public Education and Communication—Multi-Cultural and Multi-Lingual
6.2. Behavioral Interventions and Catalysts for Change
6.3. Importance of Political Will and Leadership
6.4. Pivotal Input from Healthcare Providers/Clinicians
6.5. Mandatory Vaccinations
7. Conclusions and Future Outlook
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- The COCONEL Group. A future vaccination campaign against COVID-19 at risk of vaccine hesitancy and politicisation. Lancet Infect Dis. 2020, 20, 769–770. [Google Scholar] [CrossRef]
- Dubé, E. Addressing vaccine hesitancy: The crucial role of healthcare providers. Clin. Microbiol. Infect. 2017, 23, 279–280. [Google Scholar] [CrossRef] [PubMed]
- Hou, Z.; Tong, Y.; Du, F.; Lu, L.; Zhao, S.; Yu, K.; Piatek, S.J.; Larson, H.J.; Lin, L. Assessing COVID-19 Vaccine Hesitancy, Confidence, and Public Engagement: A Global Social Listening Study. J. Med. Internet Res. 2021, 23, e27632. [Google Scholar] [CrossRef]
- WHO. Ten Threats to Global Health in 2019. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 1 September 2021).
- WHO. Report of the Strategic Advisory Group of Experts (SAGE) Working Group on Vaccine Hesitancy. Available online: https://www.who.int/immunization/sage/meetings/2014/october/SAGE_working_group_revised_report_vaccine_hesitancy.pdf (accessed on 1 September 2021).
- Wagner, A.L.; Masters, N.B.; Domek, G.J.; Mathew, J.L.; Sun, X.; Asturias, E.J.; Ren, J.; Huang, Z.; Contreras-Roldan, I.L.; Gebremeskel, B.; et al. Comparisons of Vaccine Hesitancy across Five Low- and Middle-Income Countries. Vaccines 2019, 7, 155. [Google Scholar] [CrossRef] [PubMed]
- Thomson, A.; Robinson, K.; Vallée-Tourangeau, G. The 5As: A practical taxonomy for the determinants of vaccine uptake. Vaccine 2016, 34, 1018–1024. [Google Scholar] [CrossRef]
- Betsch, C.; Schmid, P.; Heinemeier, D.; Korn, L.; Holtmann, C.; Böhm, R. Beyond confidence: Development of a measure assessing the 5C psychological antecedents of vaccination. PLoS ONE 2018, 13, e0208601. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, N.E.; Dube, E.; Comeau, J.L. Have vaccine hesitancy models oversimplified a complex problem to our detriment? The Adapted Royal Society of Canada vaccine uptake framework. Vaccine 2022, 40, 3927–3930. [Google Scholar] [CrossRef]
- Dhama, K.; Sharun, K.; Tiwari, R.; Dhawan, M.; Emran, T.B.; Rabaan, A.A.; Alhumaid, S. COVID-19 vaccine hesitancy—Reasons and solutions to achieve a successful global vaccination campaign to tackle the ongoing pandemic. Hum. Vaccines Immunother. 2021, 17, 3495–3499. [Google Scholar] [CrossRef]
- Jacobson, R.M.; St. Sauver, J.L.; Finney Rutten, L.J. Vaccine Hesitancy. Mayo Clin. Proc. 2015, 90, 1562–1568. [Google Scholar] [CrossRef]
- WHO. Coronavirus Disease (COVID-19): Herd Immunity, Lockdowns and COVID-19. Available online: https://www.who.int/news-room/questions-and-answers/item/herd-immunity-lockdowns-and-covid-19 (accessed on 19 January 2022).
- Callender, D. Vaccine hesitancy: More than a movement. Hum. Vaccines Immunother. 2016, 12, 2464–2468. [Google Scholar] [CrossRef]
- Riedel, S. Edward Jenner and the history of smallpox and vaccination. In Baylor University Medical Center Proceedings; Taylor & Francis: Abingdon-on-Thames, UK, 2005; Volume 18, pp. 21–25. [Google Scholar] [CrossRef]
- Best, M.; Neuhauser, D.; Slavin, L. “Cotton Mather, you dog, dam you! I’l inoculate you with this; with a pox to you”: Smallpox inoculation, Boston, 1721. Qual. Saf. Health Care 2004, 13, 82. [Google Scholar] [CrossRef]
- Best, M.; Katamba, A.; Neuhauser, D. Making the right decision: Benjamin Franklin’s son dies of smallpox in 1736. Qual. Saf. Health Care 2007, 16, 478–480. [Google Scholar] [CrossRef] [PubMed]
- Stewart, A.J.; Devlin, P.M. The history of the smallpox vaccine. J. Infect. 2006, 52, 329–334. [Google Scholar] [CrossRef] [PubMed]
- Lantos, J.D.; Jackson, M.A.; Opel, D.J.; Marcuse, E.K.; Myers, A.L.; Connelly, B.L. Controversies in Vaccine Mandates. Curr. Probl. Pediatric Adolesc. Health Care 2010, 40, 38–58. [Google Scholar] [CrossRef]
- Eisen, E.X. “The Mark of the Beast” Georgian Britain’s Anti-Vaxxer Movement. Available online: https://publicdomainreview.org/essay/the-mark-of-the-beast-georgian-britains-anti-vaxxer-movement (accessed on 3 September 2021).
- Durbach, N. ‘They Might As Well Brand Us’: Working-Class Resistance to Compulsory Vaccination in Victorian England. Soc. Hist. Med. 2000, 13, 45–63. [Google Scholar] [CrossRef]
- Prabhu, M. The Long View: Ye Olde Anti-Vaxxers. Available online: https://www.gavi.org/vaccineswork/long-view-ye-olde-anti-vaxxers (accessed on 3 September 2021).
- Grignolio, A.; Rundo, J. Vaccines: Are they Worth a Shot? Springer International Publishing: Berlin, Germany, 2018. [Google Scholar]
- Mariner, W.K.; Annas, G.J.; Glantz, L.H. Jacobson v Massachusetts: It’s not your great-great-grandfather’s public health law. Am. J. Public Health 2005, 95, 581–590. [Google Scholar] [CrossRef] [PubMed]
- Nature. Nature Milestones in Vaccine. Available online: https://www.nature.com/immersive/d42859-020-00005-8/index.html (accessed on 22 September 2021).
- Pennington, M. Vaccine Hesitancy: A Story as Old as Vaccines Themselves. Available online: https://www.criver.com/eureka/vaccine-hesitancy-story-old-vaccines-themselves (accessed on 22 September 2021).
- CDC. Historical Vaccine Safety Concerns. Available online: https://www.cdc.gov/vaccinesafety/concerns/concerns-history.html (accessed on 22 October 2021).
- Boom, J.A.; Cunningham, R.M. Understanding and Managing Vaccine Concerns; Springer International Publishing: Berlin, Germany, 2014; p. 42. [Google Scholar]
- CDC. Guillain-Barré Syndrome and Vaccines. Available online: https://www.cdc.gov/vaccinesafety/concerns/guillain-barre-syndrome.html#:~:text=Over%2045%20million%20people%20were,got%20the%20swine%20flu%20vaccine. (accessed on 19 January 2022).
- Wang, D.J.; Boltz, D.A.; McElhaney, J.; McCullers, J.A.; Webby, R.J.; Webster, R.G. No evidence of a link between influenza vaccines and Guillain-Barre syndrome-associated antiganglioside antibodies. Influenza Other Respir. Viruses 2012, 6, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Ghaderi, S.; Gunnes, N.; Bakken, I.J.; Magnus, P.; Trogstad, L.; Håberg, S.E. Risk of Guillain-Barré syndrome after exposure to pandemic influenza A(H1N1)pdm09 vaccination or infection: A Norwegian population-based cohort study. Eur. J. Epidemiol. 2016, 31, 67–72. [Google Scholar] [CrossRef] [PubMed]
- Baxter, R.; Bakshi, N.; Fireman, B.; Lewis, E.; Ray, P.; Vellozzi, C.; Klein, N.P. Lack of association of Guillain-Barré syndrome with vaccinations. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2013, 57, 197–204. [Google Scholar] [CrossRef]
- Juurlink, D.N.; Stukel, T.A.; Kwong, J.; Kopp, A.; McGeer, A.; Upshur, R.E.; Manuel, D.G.; Moineddin, R.; Wilson, K. Guillain-Barré syndrome after influenza vaccination in adults: A population-based study. Arch. Intern. Med. 2006, 166, 2217–2221. [Google Scholar] [CrossRef]
- Lasky, T.; Terracciano, G.J.; Magder, L.; Koski, C.L.; Ballesteros, M.; Nash, D.; Clark, S.; Haber, P.; Stolley, P.D.; Schonberger, L.B.; et al. The Guillain-Barré syndrome and the 1992–1993 and 1993–1994 influenza vaccines. N. Engl. J. Med. 1998, 339, 1797–1802. [Google Scholar] [CrossRef] [PubMed]
- CDC. Vaccine Information Statement: Influenza Vaccine. Available online: https://www.cdc.gov/vaccines/hcp/vis/vis-statements/flu.pdf (accessed on 20 January 2022).
- Vellozzi, C.; Iqbal, S.; Broder, K. Guillain-Barré Syndrome, Influenza, and Influenza Vaccination: The Epidemiologic Evidence. Clin. Infect. Dis. 2014, 58, 1149–1155. [Google Scholar] [CrossRef] [PubMed]
- Babazadeh, A.; Mohseni Afshar, Z.; Javanian, M.; Mohammadnia-Afrouzi, M.; Karkhah, A.; Masrour-Roudsari, J.; Sabbagh, P.; Koppolu, V.; Vasigala, V.K.; Ebrahimpour, S. Influenza Vaccination and Guillain-Barré Syndrome: Reality or Fear. J. Transl. Int. Med. 2019, 7, 137–142. [Google Scholar] [CrossRef]
- Kulenkampff, M.; Schwartzman, J.S.; Wilson, J. Neurological complications of pertussis inoculation. Arch. Dis. Child. 1974, 49, 46–49. [Google Scholar] [CrossRef] [PubMed]
- Baker, J.P. The pertussis vaccine controversy in Great Britain, 1974–1986. Vaccine 2003, 21, 4003–4010. [Google Scholar] [CrossRef]
- Coulter, H.L.; Fisher, B.L. DPT, a Shot in the Dark; Harcourt Brace Jovanovich: New York, NY, USA, 1985. [Google Scholar]
- Gangarosa, E.J.; Galazka, A.M.; Wolfe, C.R.; Phillips, L.M.; Miller, E.; Chen, R.T.; Gangarosa, R.E. Impact of anti-vaccine movements on pertussis control: The untold story. Lancet 1998, 351, 356–361. [Google Scholar] [CrossRef]
- Vaccine Injury Compensation Programs. Available online: https://www.historyofvaccines.org/content/articles/vaccine-injury-compensation-programs (accessed on 22 October 2021).
- Wakefield, A.J.; Murch, S.H.; Anthony, A.; Linnell, J.; Casson, D.M.; Malik, M.; Berelowitz, M.; Dhillon, A.P.; Thomson, M.A.; Harvey, P.; et al. RETRACTED: Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children. Lancet 1998, 351, 637–641. [Google Scholar] [CrossRef]
- DeStefano, F.; Chen, R.T. Negative association between MMR and autism. Lancet 1999, 353, 1987–1988. [Google Scholar] [CrossRef]
- Taylor, B.; Miller, E.; Lingam, R.; Andrews, N.; Simmons, A.; Stowe, J. Measles, mumps, and rubella vaccination and bowel problems or developmental regression in children with autism: Population study. BMJ 2002, 324, 393. [Google Scholar] [CrossRef]
- Klein, K.C.; Diehl, E.B. Relationship between MMR vaccine and autism. Ann. Pharmacother. 2004, 38, 1297–1300. [Google Scholar] [CrossRef]
- Madsen, K.M.; Hviid, A.; Vestergaard, M.; Schendel, D.; Wohlfahrt, J.; Thorsen, P.; Olsen, J.; Melbye, M. A Population-Based Study of Measles, Mumps, and Rubella Vaccination and Autism. N. Engl. J. Med. 2002, 347, 1477–1482. [Google Scholar] [CrossRef] [PubMed]
- Godlee, F.; Smith, J.; Marcovitch, H. Wakefield’s article linking MMR vaccine and autism was fraudulent. BMJ 2011, 342, c7452 . [Google Scholar] [CrossRef]
- Eggertson, L. Lancet retracts 12-year-old article linking autism to MMR vaccines. Can. Med. Assoc. J. 2010, 182, E199–E200. [Google Scholar] [CrossRef] [PubMed]
- Berger, A. Dispatches. MMR: What They Didn’t Tell You. BMJ 2004, 329, 1293. [Google Scholar] [CrossRef][Green Version]
- Brian Deer’s Film on Andrew Wakefield. Available online: https://briandeer.com/wakefield-deer.htm (accessed on 20 January 2022).
- Deer, B. MMR Doctor Given Legal Aid Thousands. Available online: https://web.archive.org/web/20070223155047/http://www.timesonline.co.uk/tol/newspapers/sunday_times/britain/article1265373.ece (accessed on 20 January 2022).
- Ghebrehewet, S.; Hayhurst, G.; Keenan, A.; Moore, H. Outbreak of measles in Central and Eastern Cheshire, UK, October 2008–February 2009. Epidemiol. Infect. 2013, 141, 1849–1856. [Google Scholar] [CrossRef] [PubMed]
- Omer, S.B. The Discredited Doctor Hailed by the Anti-Vaccine Movement. Available online: https://www.nature.com/articles/d41586-020-02989-9 (accessed on 23 September 2021).
- Quick, J.D.; Larson, H. The Vaccine-Autism Myth Started 20 Years Ago. Here’s Why It Still Endures Today. Available online: https://time.com/5175704/andrew-wakefield-vaccine-autism/ (accessed on 23 September 2021).
- Sutherland, A. The Thimerosal Controversy; Virginia Tech: Blacksburg, VI, USA, 2013. [Google Scholar]
- Targonski, P.V.; Ovsyannikova, I.G.; Tosh, P.K.; Jacobson, R.M.; Poland, G.A. Chapter 91—Vaccines. In Pharmacology and Therapeutics; Waldman, S.A., Terzic, A., Egan, L.J., Elghozi, J.-L., Jahangir, A., Kane, G.C., Kraft, W.K., Lewis, L.D., Morrow, J.D., Zingman, L.V., et al., Eds.; W.B. Saunders: Philadelphia, PA, USA, 2009; pp. 1247–1268. [Google Scholar]
- FDA. Thimerosal in Vaccines Questions and Answers. Available online: https://www.fda.gov/vaccines-blood-biologics/vaccines/thimerosal-vaccines-questions-and-answers#:~:text=As%20a%20vaccine%20preservative%2C%20thimerosal,mercury%20per%200.5%20mL%20dose (accessed on 20 January 2022).
- CDC. Thimerosal in vaccines: A joint statement of the American Academy of Pediatrics and the Public Health Service. MMWR Morb. Mortal. Wkly. Rep. 1999, 48, 563–565. [Google Scholar]
- Offit, P.A. Thimerosal and Vaccines—A Cautionary Tale. N. Engl. J. Med. 2007, 357, 1278–1279. [Google Scholar] [CrossRef]
- Dube, N. Mercury-Free Vaccine Legislation in Other States. Available online: https://www.cga.ct.gov/2010/rpt/2010-R-0352.htm (accessed on 20 January 2022).
- Jarrett, C.; Wilson, R.; O’Leary, M.; Eckersberger, E.; Larson, H.J. Strategies for addressing vaccine hesitancy—A systematic review. Vaccine 2015, 33, 4180–4190. [Google Scholar] [CrossRef]
- Larson, H.J.; Jarrett, C.; Eckersberger, E.; Smith, D.M.D.; Paterson, P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: A systematic review of published literature, 2007–2012. Vaccine 2014, 32, 2150–2159. [Google Scholar] [CrossRef]
- Kennedy, E.B.; Daoust, J.F.; Vikse, J.; Nelson, V. “Until I Know It’s Safe for Me”: The Role of Timing in COVID-19 Vaccine Decision-Making and Vaccine Hesitancy. Vaccines 2021, 9, 1417. [Google Scholar] [CrossRef]
- Azarpanah, H.; Farhadloo, M.; Vahidov, R.; Pilote, L. Vaccine hesitancy: Evidence from an adverse events following immunization database, and the role of cognitive biases. BMC Public Health 2021, 21, 1686. [Google Scholar] [CrossRef] [PubMed]
- Luz, P.M.; Nadanovsky, P.; Leask, J. How heuristics and cognitive biases affect vaccination decisions. Cad. Saude Publica 2020, 36 (Suppl. S2). [Google Scholar] [CrossRef] [PubMed]
- Dubé, E.; Laberge, C.; Guay, M.; Bramadat, P.; Roy, R.; Bettinger, J. Vaccine hesitancy: An overview. Hum. Vaccin. Immunother. 2013, 9, 1763–1773. [Google Scholar] [CrossRef] [PubMed]
- Petrelli, F.; Contratti, C.M.; Tanzi, E.; Grappasonni, I. Vaccine hesitancy, a public health problem. Ann. Ig. 2018, 30, 86–103. [Google Scholar] [CrossRef]
- Spranca, M.; Minsk, E.; Baron, J. Omission and commission in judgment and choice. J. Exp. Soc. Psychol. 1991, 27, 76–105. [Google Scholar] [CrossRef]
- Ritov, I.; Baron, J. Reluctance to vaccinate: Omission bias and ambiguity. J. Behav. Decis. Mak. 1990, 3, 263–277. [Google Scholar] [CrossRef]
- Suarez-Lledo, V.; Alvarez-Galvez, J. Prevalence of Health Misinformation on Social Media: Systematic Review. J. Med. Internet Res. 2021, 23, e17187. [Google Scholar] [CrossRef]
- Brunson, E.K. The Impact of Social Networks on Parents’ Vaccination Decisions. Pediatrics 2013, 131, e1397. [Google Scholar] [CrossRef]
- Betsch, C.; Sachse, K. Jekyll or Mr. Hyde? (How) the Internet influences vaccination decisions: Recent evidence and tentative guidelines for online vaccine communication. Vaccine 2012, 30, 3723–3726. [Google Scholar] [CrossRef]
- Connolly, T.; Reb, J. Toward interactive, Internet-based decision aid for vaccination decisions: Better information alone is not enough. Vaccine 2012, 30, 3813–3818. [Google Scholar] [CrossRef]
- Dubé, È.; Ward, J.K.; Verger, P.; MacDonald, N.E. Vaccine Hesitancy, Acceptance, and Anti-Vaccination: Trends and Future Prospects for Public Health. Annu. Rev. Public Health 2021, 42, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Kata, A. A postmodern Pandora’s box: Anti-vaccination misinformation on the Internet. Vaccine 2010, 28, 1709–1716. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, J.B.; Bell, R.A. Understanding vaccination resistance: Vaccine search term selection bias and the valence of retrieved information. Vaccine 2014, 32, 5776–5780. [Google Scholar] [CrossRef] [PubMed]
- Burki, T. Vaccine misinformation and social media. Lancet Digit. Health 2019, 1, e258–e259. [Google Scholar] [CrossRef]
- Jamison, A.; Broniatowski, D.A.; Smith, M.C.; Parikh, K.S.; Malik, A.; Dredze, M.; Quinn, S.C. Adapting and Extending a Typology to Identify Vaccine Misinformation on Twitter. Am. J. Public Health 2020, 110, S331–S339. [Google Scholar] [CrossRef]
- Loomba, S.; de Figueiredo, A.; Piatek, S.J.; de Graaf, K.; Larson, H.J. Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA. Nat. Hum. Behav. 2021, 5, 337–348. [Google Scholar] [CrossRef]
- Megget, K. Even COVID-19 can’t kill the anti-vaccination movement. BMJ 2020, 369, m2184. [Google Scholar] [CrossRef]
- Pennycook, G.; McPhetres, J.; Zhang, Y.; Lu, J.G.; Rand, D.G. Fighting COVID-19 Misinformation on Social Media: Experimental Evidence for a Scalable Accuracy-Nudge Intervention. Psychol. Sci. 2020, 31, 770–780. [Google Scholar] [CrossRef]
- Fine, P.; Eames, K.; Heymann, D.L. “Herd immunity”: A rough guide. Clin. Infect. Dis. 2011, 52, 911–916. [Google Scholar] [CrossRef]
- Walkinshaw, E. Mandatory vaccinations: The international landscape. Can. Med. Assoc. J. 2011, 183, E1167–E1168. [Google Scholar] [CrossRef]
- Gualano, M.R.; Olivero, E.; Voglino, G.; Corezzi, M.; Rossello, P.; Vicentini, C.; Bert, F.; Siliquini, R. Knowledge, attitudes and beliefs towards compulsory vaccination: A systematic review. Hum. Vaccines Immunother. 2019, 15, 918–931. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, A.M.; Brown, C.J.; Gust, D.A. Vaccine beliefs of parents who oppose compulsory vaccination. Public Health Rep. 2005, 120, 252–258. [Google Scholar] [CrossRef] [PubMed]
- McCoy, C.A. The social characteristics of Americans opposed to vaccination: Beliefs about vaccine safety versus views of U.S. vaccination policy. Crit. Public Health 2020, 30, 4–15. [Google Scholar] [CrossRef]
- Rosenfeld, D.L.; Tomiyama, A.J. Jab my arm, not my morality: Perceived moral reproach as a barrier to COVID-19 vaccine uptake. Soc. Sci. Med. 2022, 294, 114699. [Google Scholar] [CrossRef] [PubMed]
- Bendau, A.; Plag, J.; Petzold, M.B.; Ströhle, A. COVID-19 vaccine hesitancy and related fears and anxiety. Int. Immunopharmacol. 2021, 97, 107724. [Google Scholar] [CrossRef]
- Chevallier, C.; Hacquin, A.-S.; Mercier, H. COVID-19 Vaccine Hesitancy: Shortening the Last Mile. Trends Cogn. Sci. 2021, 25, 331–333. [Google Scholar] [CrossRef]
- Mansour, J.; Pennetier, M.; Savage, C. Video Makes Inaccurate Claims About COVID-19 Shots Harming Children. Available online: https://factcheck.afp.com/http%253A%252F%252Fdoc.afp.com%252F9V36YN-1 (accessed on 7 February 2022).
- Carballo-Carbajal, I. Robert Malone Made Multiple Misleading or Unsubstantiated Claims About COVID-19 and Vaccines on the Joe Rogan Experience Podcast. Available online: https://healthfeedback.org/claimreview/robert-malone-misleading-unsubstantiated-claims-covid-19-safety-efficacy-vaccines-joe-rogan-experience-spotify-podcast/ (accessed on 7 February 2022).
- Yang, M. Menace to Public Health’: 270 Experts Criticise Spotify over Joe Rogan’s Podcast. Available online: https://www.theguardian.com/technology/2022/jan/14/spotify-joe-rogan-podcast-open-letter (accessed on 7 February 2022).
- Suppli, C.H.; Hansen, N.D.; Rasmussen, M.; Valentiner-Branth, P.; Krause, T.G.; Mølbak, K. Decline in HPV-vaccination uptake in Denmark—the association between HPV-related media coverage and HPV-vaccination. BMC Public Health 2018, 18, 1360. [Google Scholar] [CrossRef]
- Hanley, S.J.B.; Yoshioka, E.; Ito, Y.; Kishi, R. HPV vaccination crisis in Japan. Lancet 2015, 385, 2571. [Google Scholar] [CrossRef]
- Larson, H.J.; de Figueiredo, A.; Xiahong, Z.; Schulz, W.S.; Verger, P.; Johnston, I.G.; Cook, A.R.; Jones, N.S. The State of Vaccine Confidence 2016: Global Insights through a 67-Country Survey. EBioMedicine 2016, 12, 295–301. [Google Scholar] [CrossRef]
- Ward, J.K.; Colgrove, J.; Verger, P. Why France is making eight new vaccines mandatory. Vaccine 2018, 36, 1801–1803. [Google Scholar] [CrossRef]
- Duclos, P. Safety of immunization and adverse events following vaccination against hepatitis B. J. Hepatol. 2003, 39, 83–88. [Google Scholar] [CrossRef]
- Ward, J.K.; Peretti-Watel, P.; Bocquier, A.; Seror, V.; Verger, P. Vaccine hesitancy and coercion: All eyes on France. Nat. Immunol. 2019, 20, 1257–1259. [Google Scholar] [CrossRef]
- Finnegan, G. How France Overcame COVID-19 Vaccine Scepticism. Available online: https://www.vaccinestoday.eu/stories/how-france-overcame-covid-19-vaccine-scepticism/ (accessed on 22 September 2021).
- Robinson, E.; Jones, A.; Lesser, I.; Daly, M. International estimates of intended uptake and refusal of COVID-19 vaccines: A rapid systematic review and meta-analysis of large nationally representative samples. Vaccine 2021, 39, 2024–2034. [Google Scholar] [CrossRef] [PubMed]
- RSPH. New Poll Finds Ethnic Minority Groups Less Likely to Want COVID Vaccine. Available online: https://www.rsph.org.uk/about-us/news/new-poll-finds-bame-groups-less-likely-to-want-covid-vaccine.html (accessed on 14 October 2021).
- ONS. Coronavirus and the Social Impacts on Great Britain: 29 January 2021. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthandwellbeing/bulletins/coronavirusandthesocialimpactsongreatbritain/29january2021#attitudes-to-covid-19-vaccination-by-different-sub-groups-of-the-population (accessed on 14 October 2021).
- Robertson, E.; Reeve, K.S.; Niedzwiedz, C.L.; Moore, J.; Blake, M.; Green, M.; Katikireddi, S.V.; Benzeval, M.J. Predictors of COVID-19 vaccine hesitancy in the UK household longitudinal study. Brain Behav. Immun. 2021, 94, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Mills, M.; Rahal, C.; Brazel, D.; Yan, J.; Gieysztor, S. COVID-19 Vaccine Deployment: Behaviour, Ethics, Misinformation and Policy Strategies; The Royal Society & The British Academy: London, UK, 2020. [Google Scholar]
- Razai, M.S.; Kankam, H.K.N.; Majeed, A.; Esmail, A.; Williams, D.R. Mitigating ethnic disparities in covid-19 and beyond. BMJ 2021, 372, m4921. [Google Scholar] [CrossRef]
- Gamble, V.N. Under the shadow of Tuskegee: African Americans and health care. Am. J. Public Health 1997, 87, 1773–1778. [Google Scholar] [CrossRef]
- Razai, M.S.; Osama, T.; McKechnie, D.G.J.; Majeed, A. COVID-19 vaccine hesitancy among ethnic minority groups. BMJ 2021, 372, n513. [Google Scholar] [CrossRef]
- Edwards, B.; Biddle, N.; Gray, M.; Sollis, K. COVID-19 vaccine hesitancy and resistance: Correlates in a nationally representative longitudinal survey of the Australian population. PLoS ONE 2021, 16, e0248892. [Google Scholar] [CrossRef]
- Biddle, N.; Edwards, B.; Gray, M.; Sollis, K. Vaccine Willingness and Concerns in Australia: August 2020 to April 2021; The ANU Centre for Social Research and Methods: Canberra, Australia, 2021. [Google Scholar]
- Read, M. Vaccine Hesitancy Highest in Queensland and WA as Rollouts Lag. Available online: https://www.afr.com/politics/vaccine-hesitancy-highest-in-qld-and-wa-as-rollouts-lag-20211012-p58za9 (accessed on 15 October 2021).
- Vaccine Hesitancy Tracker. Available online: https://melbourneinstitute.unimelb.edu.au/publications/research-insights/ttpn/vaccination-report (accessed on 18 May 2022).
- Qutaiba B Al-lela, O.; Bahari, M.B.; Al-Qazaz, H.K.; Salih, M.R.M.; Jamshed, S.Q.; Elkalmi, R.M. Are parents’ knowledge and practice regarding immunization related to pediatrics’ immunization compliance? a mixed method study. BMC Pediatrics 2014, 14, 20. [Google Scholar] [CrossRef][Green Version]
- Akmatov, M.K.; Mikolajczyk, R.T.; Kretzschmar, M.; Krämer, A. Attitudes and beliefs of parents about childhood vaccinations in post-soviet countries: The example of Kyrgyzstan. Pediatric Infect. Dis. J. 2009, 28, 637–640. [Google Scholar] [CrossRef]
- Obute, J.A.; Arulogun, O.S. Parents’ awareness and perception of the polio eradication programme in Gombe Local Government Area, Gombe State, Nigeria. Int. J. Health Promot. Educ. 2007, 45, 81–86. [Google Scholar] [CrossRef]
- Oladokun, R.E.; Adedokun, B.O.; Lawoyin, T.O. Children not receiving adequate immunization in Ibadan, Nigeria: What reasons and beliefs do their mothers have? Niger. J. Clin. Pract. 2010, 13, 173–178. [Google Scholar]
- Cobos Muñoz, D.; Monzón Llamas, L.; Bosch-Capblanch, X. Exposing concerns about vaccination in low- and middle-income countries: A systematic review. Int. J. Public Health 2015, 60, 767–780. [Google Scholar] [CrossRef]
- Abdulraheem, I.S.; Onajole, A.T.; Oladipo, A. Reasons for incomplete vaccination and factors for missed opportunities among rural Nigerian children. J. Public Health Epidemiol. 2011, 3, 194–203. [Google Scholar]
- Naeem, M.; Adil, M.; Abbas, S.H.; Khan, M.Z.; Naz, S.M.; Khan, A.; Khan, M.U. Coverage and causes of missed oral polio vaccine in urban and rural areas of Peshawar. J. Ayub Med. Coll. Abbottabad 2011, 23, 98–102. [Google Scholar]
- Joseph, N.; Subba, S.H.; Nelliyanil, M.; Kotian, S.M.; Haridath, A.C.; Kishor, N.; Attavar, S.; Poornima, P.; Rane, D.V.; Chaithali, H.; et al. A study of the knowledge and attitude towards pulse polio immunization in semi urban areas of South India. Australas. Med. J. 2011, 4, 81–86. [Google Scholar] [CrossRef]
- Babirye, J.N.; Rutebemberwa, E.; Kiguli, J.; Wamani, H.; Nuwaha, F.; Engebretsen, I.M.S. More support for mothers: A qualitative study on factors affecting immunisation behaviour in Kampala, Uganda. BMC Public Health 2011, 11, 723. [Google Scholar] [CrossRef]
- Sia, D.; Fournier, P.; Sondo, B.K. Local culture of vaccination: The role of central authorities in the health of the rural population in Burkino Faso. Glob. Health Promot. 2011, 18, 68–80. [Google Scholar] [CrossRef]
- Khowaja, A.R.; Khan, S.A.; Nizam, N.; Omer, S.B.; Zaidi, A. Parental perceptions surrounding polio and self-reported non-participation in polio supplementary immunization activities in Karachi, Pakistan: A mixed methods study. Bull. World Health Organ. 2012, 90, 822–830. [Google Scholar] [CrossRef]
- Taylor, S.; Shimp, L. Using Data to Guide Action in Polio Health Communications: Experience From the Polio Eradication Initiative (PEI). J. Health Commun. 2010, 15, 48–65. [Google Scholar] [CrossRef]
- Jegede, A.S. What led to the Nigerian boycott of the polio vaccination campaign? PLoS Med. 2007, 4, e73. [Google Scholar] [CrossRef]
- Larson, H. The CIA’s Fake Vaccination Drive has Damaged the Battle against Polio. Available online: https://www.theguardian.com/commentisfree/2012/may/27/cia-fake-vaccination-polio (accessed on 14 October 2021).
- Lenzer, J. Fake vaccine campaign in Pakistan could threaten plans to eradicate polio. BMJ 2011, 343, d4580. [Google Scholar] [CrossRef] [PubMed]
- Kabir, M.; Afzal, M.S. Epidemiology of polio virus infection in Pakistan and possible risk factors for its transmission. Asian Pac. J. Trop. Med. 2016, 9, 1044–1047. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, J. How Drone Strikes and a Fake Vaccination Program Have Inhibited Polio Eradication in Pakistan: An Analysis of National Level Data. Int. J. Health Serv. 2017, 47, 807–825. [Google Scholar] [CrossRef]
- BBC. Four Kidnapped Polio Workers Are Found Dead in Pakistan. Available online: https://www.bbc.com/news/world-asia-31507217 (accessed on 14 October 2021).
- Fourn, L.; Haddad, S.; Fournier, P.; Gansey, R. Determinants of parents’ reticence toward vaccination in urban areas in Benin (West Africa). BMC Int. Health Hum. Rights 2009, 9 (Suppl. S1). [Google Scholar] [CrossRef] [PubMed][Green Version]
- Etokidem, A.J.; Ndifon, W.; Ogaji, D.; Ebenso, B.; Nsan, E.; Ikpeme, B. Myths and misconceptions as barriers to uptake of immunization services in Nigeria. Ibom Med. J. 2014, 7, 7. [Google Scholar]
- Schwarz, N.; Gysels, M.H.; Pell, C.L.; Gabor, J.J.; Schlie, M.; Issifou, S.; Lell, B.; Kremsner, P.G.; Grobusch, M.P.; Pool, R.J.V. Reasons for non-adherence to vaccination at mother and child care clinics (MCCs) in Lambaréné, Gabon. Vaccine 2009, 27, 5371–5375. [Google Scholar] [CrossRef]
- Solís Arce, J.S.; Warren, S.S.; Meriggi, N.F.; Scacco, A.; McMurry, N.; Voors, M.; Syunyaev, G.; Malik, A.A.; Aboutajdine, S.; Adeojo, O.; et al. COVID-19 vaccine acceptance and hesitancy in low- and middle-income countries. Nat. Med. 2021, 27, 1385–1394. [Google Scholar] [CrossRef]
- Webb Hooper, M.; Nápoles, A.M.; Pérez-Stable, E.J. No Populations Left Behind: Vaccine Hesitancy and Equitable Diffusion of Effective COVID-19 Vaccines. J. Gen. Intern. Med. 2021, 36, 2130–2133. [Google Scholar] [CrossRef]
- Watson, O.J.; Barnsley, G.; Toor, J.; Hogan, A.B.; Winskill, P.; Ghani, A.C. Global impact of the first year of COVID-19 vaccination: A mathematical modelling study. Lancet Infect. Dis. 2022, 22, 1293–1302. [Google Scholar] [CrossRef]
- Vallis, M.; Bacon, S.; Corace, K.; Joyal-Desmarais, K.; Sheinfeld Gorin, S.; Paduano, S.; Presseau, J.; Rash, J.; Mengistu Yohannes, A.; Lavoie, K. Ending the Pandemic: How Behavioural Science Can Help Optimize Global COVID-19 Vaccine Uptake. Vaccines 2021, 10, 7. [Google Scholar] [CrossRef] [PubMed]
- Davis, R.; Campbell, R.; Hildon, Z.; Hobbs, L.; Michie, S. Theories of behaviour and behaviour change across the social and behavioural sciences: A scoping review. Health Psychol. Rev. 2015, 9, 323–344. [Google Scholar] [CrossRef] [PubMed]
- Corace, K.M.; Srigley, J.A.; Hargadon, D.P.; Yu, D.; MacDonald, T.K.; Fabrigar, L.R.; Garber, G.E. Using behavior change frameworks to improve healthcare worker influenza vaccination rates: A systematic review. Vaccine 2016, 34, 3235–3242. [Google Scholar] [CrossRef]
- Madison, A.A.; Shrout, M.R.; Renna, M.E.; Kiecolt-Glaser, J.K. Psychological and Behavioral Predictors of Vaccine Efficacy: Considerations for COVID-19. Perspect. Psychol. Sci. 2021, 16, 191–203. [Google Scholar] [CrossRef] [PubMed]
- West, R.; Michie, S.; Rubin, G.J.; Amlôt, R. Applying principles of behaviour change to reduce SARS-CoV-2 transmission. Nat. Hum. Behav. 2020, 4, 451–459. [Google Scholar] [CrossRef]
- Bavel, J.J.V.; Baicker, K.; Boggio, P.S.; Capraro, V.; Cichocka, A.; Cikara, M.; Crockett, M.J.; Crum, A.J.; Douglas, K.M.; Druckman, J.N.; et al. Using social and behavioural science to support COVID-19 pandemic response. Nat. Hum. Behav. 2020, 4, 460–471. [Google Scholar] [CrossRef] [PubMed]
- Milkman, K.L.; Gandhi, L.; Patel, M.S.; Graci, H.N.; Gromet, D.M.; Ho, H.; Kay, J.S.; Lee, T.W.; Rothschild, J.; Bogard, J.E.; et al. A 680,000-person megastudy of nudges to encourage vaccination in pharmacies. Proc. Natl. Acad. Sci. USA 2022, 119, e2115126119. [Google Scholar] [CrossRef]
- Sääksvuori, L.; Betsch, C.; Nohynek, H.; Salo, H.; Sivelä, J.; Böhm, R. Information nudges for influenza vaccination: Evidence from a large-scale cluster-randomized controlled trial in Finland. PLoS Med. 2022, 19, e1003919. [Google Scholar] [CrossRef]
- Meikle, J. Tony Blair Should Have Gone Public over Leo’s MMR Jab, Says Sir Liam Donaldson. Available online: https://www.theguardian.com/politics/2013/jun/02/liam-donaldson-tony-leo-blair-mmr (accessed on 19 January 2022).
- Phillip, A.; Sun, L.H.; Bernstein, L. Vaccine Skeptic Robert Kennedy Jr. Says Trump Asked Him to Lead Commission on ‘Vaccine Safety’. Available online: https://www.washingtonpost.com/politics/trump-to-meet-with-proponent-of-debunked-tie-between-vaccines-and-autism/2017/01/10/4a5d03c0-d752-11e6-9f9f-5cdb4b7f8dd7_story.html (accessed on 19 January 2022).
- Zhang, E.J.; Chughtai, A.A.; Heywood, A.; MacIntyre, C.R. Influence of political and medical leaders on parental perception of vaccination: A cross-sectional survey in Australia. BMJ Open 2019, 9, e025866. [Google Scholar] [CrossRef]
- Wouters, O.J.; Shadlen, K.C.; Salcher-Konrad, M.; Pollard, A.J.; Larson, H.J.; Teerawattananon, Y.; Jit, M. Challenges in ensuring global access to COVID-19 vaccines: Production, affordability, allocation, and deployment. Lancet 2021, 397, 1023–1034. [Google Scholar] [CrossRef]
- Sabahelzain, M.M.; Hartigan-Go, K.; Larson, H.J. The politics of COVID-19 vaccine confidence. Curr. Opin. Immunol. 2021, 71, 92–96. [Google Scholar] [CrossRef] [PubMed]
- Leask, J.; Willaby, H.W.; Kaufman, J. The big picture in addressing vaccine hesitancy. Hum. Vaccines Immunother. 2014, 10, 2600–2602. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, L. Escaping Catch-22—Overcoming Covid Vaccine Hesitancy. N. Engl. J. Med. 2021, 384, 1367–1371. [Google Scholar] [CrossRef]
- Flanigan, J. A defense of compulsory vaccination. HEC Forum. 2014, 26, 5–25. [Google Scholar] [CrossRef]
- Pierik, R. Mandatory Vaccination: An Unqualified Defence. J. Appl. Philos. 2018, 35, 381–398. [Google Scholar] [CrossRef]
- Boniolo, G. Public Obligation and Individual Freedom: How to Fill the Gap? The Case of Vaccinations. J. Public Health Res. 2016, 5, 732. [Google Scholar] [CrossRef]
- Savulescu, J. Good reasons to vaccinate: Mandatory or payment for risk? J. Med. Ethics 2021, 47, 78. [Google Scholar] [CrossRef]
- Which Countries Have Mandatory Childhood Vaccination Policies? Available online: https://ourworldindata.org/childhood-vaccination-policies#note-2 (accessed on 18 January 2022).
- Ward, J.K.; Gauna, F.; Gagneux-Brunon, A.; Botelho-Nevers, E.; Cracowski, J.-L.; Khouri, C.; Launay, O.; Verger, P.; Peretti-Watel, P. The French health pass holds lessons for mandatory COVID-19 vaccination. Nat. Med. 2022, 28, 232–235. [Google Scholar] [CrossRef]
- Factbox: Countries Making COVID-19 Vaccines Mandatory. Available online: https://www.reuters.com/business/healthcare-pharmaceuticals/countries-making-covid-19-vaccines-mandatory-2021-08-16/ (accessed on 18 January 2022).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nuwarda, R.F.; Ramzan, I.; Weekes, L.; Kayser, V. Vaccine Hesitancy: Contemporary Issues and Historical Background. Vaccines 2022, 10, 1595. https://doi.org/10.3390/vaccines10101595
Nuwarda RF, Ramzan I, Weekes L, Kayser V. Vaccine Hesitancy: Contemporary Issues and Historical Background. Vaccines. 2022; 10(10):1595. https://doi.org/10.3390/vaccines10101595
Chicago/Turabian StyleNuwarda, Rina Fajri, Iqbal Ramzan, Lynn Weekes, and Veysel Kayser. 2022. "Vaccine Hesitancy: Contemporary Issues and Historical Background" Vaccines 10, no. 10: 1595. https://doi.org/10.3390/vaccines10101595
APA StyleNuwarda, R. F., Ramzan, I., Weekes, L., & Kayser, V. (2022). Vaccine Hesitancy: Contemporary Issues and Historical Background. Vaccines, 10(10), 1595. https://doi.org/10.3390/vaccines10101595





