Vaccine Hesitancy during the Coronavirus Pandemic in South Tyrol, Italy: Linguistic Correlates in a Representative Cross-Sectional Survey
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Data Collection
2.2. Questionnaire
2.3. Vaccine Hesitancy (Dependent Variable)
2.4. Putative Predictors of Vaccine Hesitancy (Independent Variables)
2.5. Statistical Analysis
3. Results
3.1. Sample Characteristics
3.2. Vaccination Perception
3.2.1. Compulsory Vaccination for Non-Coronaviruses
3.2.2. Vaccination Hesitancy and Attitudes towards COVID-19 Disease, Vaccines, and Vaccination
3.3. Predictors of Vaccine Hesitancy
Trust in Information Sources
3.4. Specific Reasons for Vaccine Hesitancy: Total Scores
3.4.1. Mistrust in Political and Scientific Authorities and Conspiracy Theories
3.4.2. Altruism, Resilience, and Well-Being
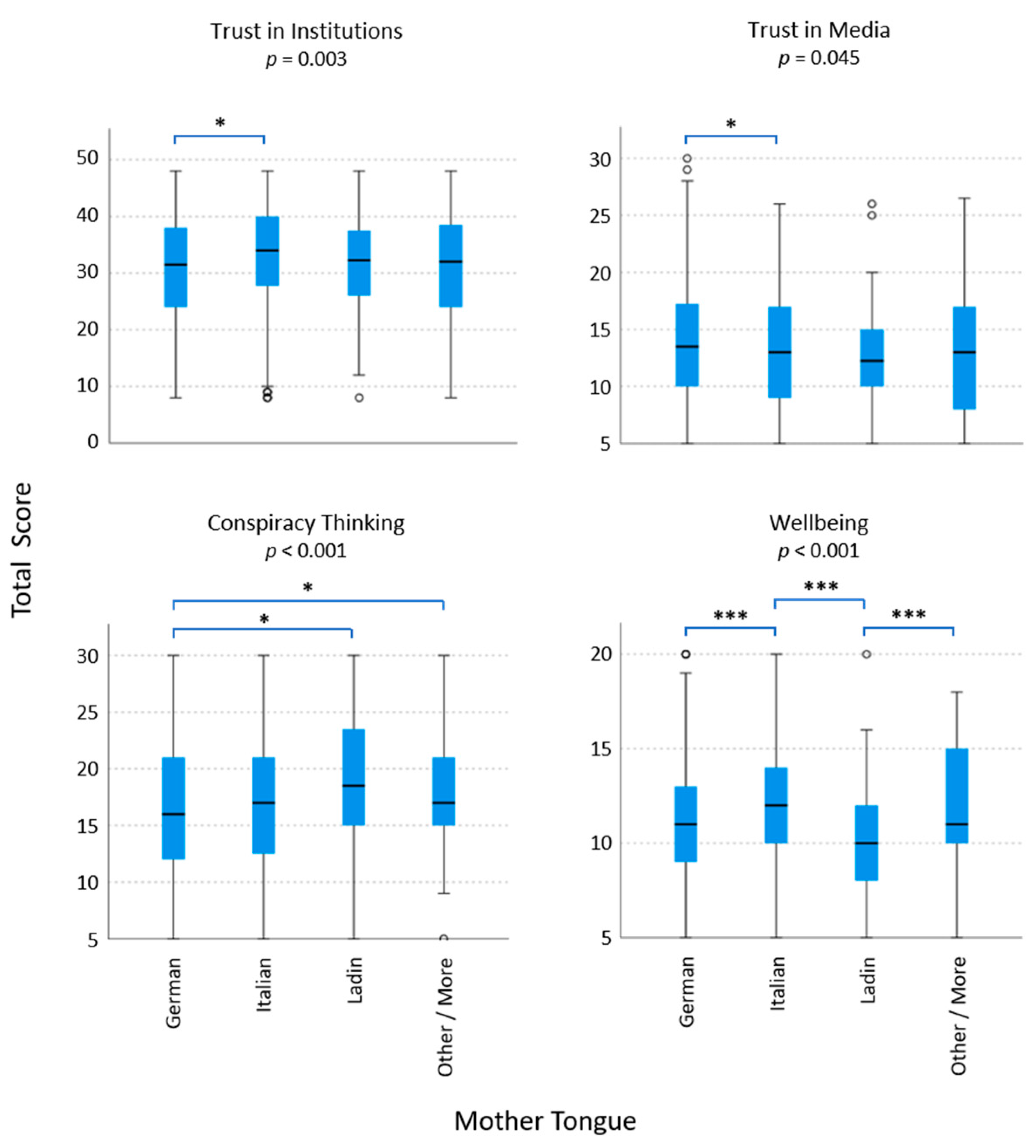
3.5. Hesitancy-Related Attitudes in Mother Tongue Groups
3.6. Multivariable Logistic Regression to Predict Vaccine Hesitancy
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tatar, M.; Faraji, M.R.; Montazeri Shoorekchali, J.; Pagán, J.A.; Wilson, F.A. The Role of Good Governance in the Race for Global Vaccination during the COVID-19 Pandemic. Sci. Rep. 2021, 11, 22440. [Google Scholar] [CrossRef]
- Kwok, K.O.; Li, K.-K.; Wei, W.I.; Tang, A.; Wong, S.Y.S.; Lee, S.S. Influenza Vaccine Uptake, COVID-19 Vaccination Intention and Vaccine Hesitancy among Nurses: A Survey. Int. J. Nurs. Stud. 2020, 114, 103854. [Google Scholar] [CrossRef]
- Webb Hooper, M.; Nápoles, A.M.; Pérez-Stable, E.J. COVID-19 and Racial/Ethnic Disparities. JAMA 2020, 323, 2466–2467. [Google Scholar] [CrossRef]
- Ritchie, H.; Mathieu, E.; Rodés-Guirao, L.; Appel, C.; Giattino, C.; Ortiz-Ospina, E.; Hasell, J.; Macdonald, B.; Beltekian, D.; Roser, M. Coronavirus Pandemic (COVID-19). Our World in Data. 2020. Available online: https://ourworldindata.org/covid-vaccinations?country=JPN~USA (accessed on 15 September 2022).
- Neumann-Böhme, S.; Varghese, N.E.; Sabat, I.; Barros, P.P.; Brouwer, W.; van Exel, J.; Schreyögg, J.; Stargardt, T. Once We Have It, Will We Use It? A European Survey on Willingness to Be Vaccinated against COVID-19. Eur. J. Health Econ. 2020, 21, 977–982. [Google Scholar] [CrossRef]
- Halvorsrud, K.; Shand, J.; Weil, L.G.; Hutchings, A.; Zuriaga, A.; Satterthwaite, D.; Yip, J.L.Y.; Eshareturi, C.; Billett, J.; Hepworth, A.; et al. Tackling Barriers to COVID-19 Vaccine Uptake in London: A Mixed-Methods Evaluation. J. Public Health 2022, fdac038. [Google Scholar] [CrossRef]
- Dong, L.; Bogart, L.M.; Gandhi, P.; Aboagye, J.B.; Ryan, S.; Serwanga, R.; Ojikutu, B.O. A Qualitative Study of COVID-19 Vaccine Intentions and Mistrust in Black Americans: Recommendations for Vaccine Dissemination and Uptake. PLoS ONE 2022, 17, e0268020. [Google Scholar] [CrossRef] [PubMed]
- Benvenuto, O.; Gobbi, G. South Tyrol in Figures 2014; Provincial Statistics Institute ASTAT: Autonomous Province of Bolzano, Italy, 2014. [Google Scholar]
- Ausserhofer, D.; Wiedermann, W.; Becker, U.; Vögele, A.; Piccoliori, G.; Wiedermann, C.J.; Engl, A. Health Information-Seeking Behavior Associated with Linguistic Group Membership: Latent Class Analysis of a Population-Based Cross-Sectional Survey in Italy, August to September 2014. Arch. Public Health 2022, 80, 87. [Google Scholar] [CrossRef]
- Larson, H.J.; Gakidou, E.; Murray, C.J.L. The Vaccine-Hesitant Moment. N. Engl. J. Med. 2022, 387, 58–65. [Google Scholar] [CrossRef]
- Gallè, F.; Sabella, E.A.; Roma, P.; Ferracuti, S.; Da Molin, G.; Diella, G.; Montagna, M.T.; Orsi, G.B.; Liguori, G.; Napoli, C. Knowledge and Lifestyle Behaviors Related to COVID-19 Pandemic in People over 65 Years Old from Southern Italy. Int. J. Environ. Res. Public Health 2021, 18, 10872. [Google Scholar] [CrossRef]
- Tagini, S.; Brugnera, A.; Ferrucci, R.; Priori, A.; Compare, A.; Parolin, L.; Pravettoni, G.; Silani, V.; Poletti, B. Behind the Scenes of COVID-19 Vaccine Hesitancy: Psychological Predictors in an Italian Community Sample. Vaccines 2022, 10, 1158. [Google Scholar] [CrossRef]
- Landesinstitut für Statistik der Autonomen Provinz Bozen—Südtirol. COVID-19: Einstellungen und Verhalten der Bürger. Jänner 2021; astatinfo; Landesverwaltung der Autonomen Provinz Bozen—Südtirol: Bolzano (BZ), Italy, 2021. [Google Scholar]
- WHO Regional Office for Europe. COVID-19 Snapshot MOnitoring (COSMO Standard): Monitoring Knowledge, Risk Perceptions, Preventive Behaviours, and Public Trust in the Current Coronavirus Outbreak—WHO Standard Protocol; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- Caserotti, M.; Gavaruzzi, T.; Girardi, P.; Tasso, A.; Buizza, C.; Candini, V.; Zarbo, C.; Chiarotti, F.; Brescianini, S.; Calamandrei, G.; et al. Who Is Likely to Vacillate in Their COVID-19 Vaccination Decision? Free-Riding Intention and Post-Positive Reluctance. Prev. Med. 2022, 154, 106885. [Google Scholar] [CrossRef] [PubMed]
- Schweitzer, M.E.; Hershey, J.C.; Bradlow, E.T. Promises and Lies: Restoring Violated Trust. Organ. Behav. Hum. Decis. Process. 2006, 101, 1–19. [Google Scholar] [CrossRef]
- Pearson, S.D.; Raeke, L.H. Patients’ Trust in Physicians: Many Theories, Few Measures, and Little Data. J. Gen. Intern. Med. 2000, 15, 509–513. [Google Scholar] [CrossRef]
- Bruder, M.; Haffke, P.; Neave, N.; Nouripanah, N.; Imhoff, R. Measuring Individual Differences in Generic Beliefs in Conspiracy Theories Across Cultures: Conspiracy Mentality Questionnaire. Front. Psychol. 2013, 4, 225. [Google Scholar] [CrossRef] [PubMed]
- Smith, B.W.; Dalen, J.; Wiggins, K.; Tooley, E.; Christopher, P.; Bernard, J. The Brief Resilience Scale: Assessing the Ability to Bounce Back. Int. J. Behav. Med. 2008, 15, 194–200. [Google Scholar] [CrossRef]
- Bhatta, T.R.; Kahana, E.; Lekhak, N.; Kahana, B.; Midlarsky, E. Altruistic Attitudes Among Older Adults: Examining Construct Validity and Measurement Invariance of a New Scale. Innov. Aging 2021, 5, igaa060. [Google Scholar] [CrossRef]
- Gamliel, E.; Peer, E. Attribute Framing Affects the Perceived Fairness of Health Care Allocation Principles. Judgm. Decis. Mak. 2010, 5, 11. [Google Scholar]
- Bujang, M.A.; Sa’at, N.; Sidik, T.M.I.T.A.B.; Joo, L.C. Sample Size Guidelines for Logistic Regression from Observational Studies with Large Population: Emphasis on the Accuracy Between Statistics and Parameters Based on Real Life Clinical Data. Malays. J. Med. Sci. 2018, 25, 122–130. [Google Scholar] [CrossRef]
- Radiotelevisione Italiana Impfkampagne: Wochen-Negativrekord in Südtirol—TGR Tagesschau. Available online: https://www.rainews.it/tgr/tagesschau/articoli/2021/09/tag-Impfkampagne-Wochenbilanz-Suedtirol-20210906-a3614331-14e6-43cd-80eb-447bd32fb552.html (accessed on 17 July 2022).
- Del Riccio, M.; Boccalini, S.; Rigon, L.; Biamonte, M.A.; Albora, G.; Giorgetti, D.; Bonanni, P.; Bechini, A. Factors Influencing SARS-CoV-2 Vaccine Acceptance and Hesitancy in a Population-Based Sample in Italy. Vaccines 2021, 9, 633. [Google Scholar] [CrossRef]
- Reno, C.; Maietti, E.; Fantini, M.P.; Savoia, E.; Manzoli, L.; Montalti, M.; Gori, D. Enhancing COVID-19 Vaccines Acceptance: Results from a Survey on Vaccine Hesitancy in Northern Italy. Vaccines 2021, 9, 378. [Google Scholar] [CrossRef] [PubMed]
- Valckx, S.; Crèvecoeur, J.; Verelst, F.; Vranckx, M.; Hendrickx, G.; Hens, N.; Van Damme, P.; Pepermans, K.; Beutels, P.; Neyens, T. Individual Factors Influencing COVID-19 Vaccine Acceptance in between and during Pandemic Waves (July–December 2020). Vaccine 2022, 40, 151–161. [Google Scholar] [CrossRef]
- Reid, J.A.; Mabhala, M.A. Ethnic and Minority Group Differences in Engagement with COVID-19 Vaccination Programmes—At Pandemic Pace; When Vaccine Confidence in Mass Rollout Meets Local Vaccine Hesitancy. Isr. J. Health Policy Res. 2021, 10, 33. [Google Scholar] [CrossRef]
- Taylor, L. Guatemala’s COVID Vaccine Roll-out Failed: Here’s What Researchers Know. Nature 2022. [Google Scholar] [CrossRef] [PubMed]
- Ochieng, C.; Anand, S.; Mutwiri, G.; Szafron, M.; Alphonsus, K. Factors Associated with COVID-19 Vaccine Hesitancy among Visible Minority Groups from a Global Context: A Scoping Review. Vaccines 2021, 9, 1445. [Google Scholar] [CrossRef] [PubMed]
- Weng, Y.; Lu, D.; Bollyky, J.; Jain, V.; Desai, M.; Lindan, C.; Boothroyd, D.; Judson, T.; Doernberg, S.B.; Holubar, M.; et al. Race-Ethnicity and COVID-19 Vaccination Beliefs and Intentions: A Cross-Sectional Study among the General Population in the San Francisco Bay Area. Vaccines 2021, 9, 1406. [Google Scholar] [CrossRef] [PubMed]
- Bubola, E. In Italy’s Alps, Traditional Medicine Flourishes, as Does COVID. The New York Times, 16 December 2021. [Google Scholar]
- Gruppo Italiano per la Medicina Basata Sulle Evidenze Pandemia Coronavirus. Available online: https://coronavirus.gimbe.org/vaccini.it-IT.html (accessed on 14 December 2021).
- Roberts, H. Italy’s German-Speaking North Caught up in Latest Coronavirus Surge. Politico, 19 November 2021. [Google Scholar]
- Natter, B. Krankheiten Und Impfungen—Anfrage 3293/18 Vom 23.01.2018; Landesrätin für Gesundheit, Sport, Soziales und Arbeit—Autonome Provinz Bozen—Südtirol: Bolzano (BZ), Italy, 2018. [Google Scholar]
- Ferro, A.; Odone, A.; Siddu, A.; Colucci, M.; Anello, P.; Longone, M.; Marcon, E.; Castiglia, P.; Bonanni, P.; Signorelli, C. Monitoring the Web to Support Vaccine Coverage: Results of Two Years of the Portal VaccinarSì. Epidemiol. Prev. 2015, 39, 88–93. [Google Scholar]
- Burioni, R.; Odone, A.; Signorelli, C. Lessons from Italy’s Policy Shift on Immunization. Nature 2018, 555, 30. [Google Scholar] [CrossRef]
- Atz, H. Einstellung von Südtiroler Eltern zu den Pflichtimpfungen für Kinder; Apollis: Bolzano (BZ), Italy, 2017. [Google Scholar]
- Kamal, A.; Hodson, A.; Pearce, J.M. A Rapid Systematic Review of Factors Influencing COVID-19 Vaccination Uptake in Minority Ethnic Groups in the UK. Vaccines 2021, 9, 1121. [Google Scholar] [CrossRef]
- Wang, Y.; Liu, Y. Multilevel Determinants of COVID-19 Vaccination Hesitancy in the United States: A Rapid Systematic Review. Prev. Med. Rep. 2021, 25, 101673. [Google Scholar] [CrossRef]
- Murphy, J.; Vallières, F.; Bentall, R.P.; Shevlin, M.; McBride, O.; Hartman, T.K.; McKay, R.; Bennett, K.; Mason, L.; Gibson-Miller, J.; et al. Psychological Characteristics Associated with COVID-19 Vaccine Hesitancy and Resistance in Ireland and the United Kingdom. Nat. Commun. 2021, 12, 29. [Google Scholar] [CrossRef]
- Legge 31 Luglio 2017, n. 119. Conversione in Legge, con Modificazioni, del Decreto-Legge 7 Giugno 2017, n. 73, Recante Disposizioni Urgenti in Materia di Prevenzione Vaccinale. (17G00132). Gazzetta Ufficiale Serie Generale n. 182 del 05-08-2017. Available online: https://www.gazzettaufficiale.it/eli/id/2017/08/5/17G00132/sg (accessed on 22 January 2022).
- Melot, B.; Bordin, P.; Bertoni, C.; Tralli, V.; Zuccali, M.; Grignolio, A.; Majori, S.; Ferro, A. Knowledge, Attitudes and Practices about Vaccination in Trentino, Italy in 2019. Hum. Vaccines Immunother. 2021, 17, 259–268. [Google Scholar] [CrossRef] [PubMed]
- EpiCentro Copertura Vaccinale in Italia. Available online: https://www.epicentro.iss.it/vaccini/dati_Ita#morbillo (accessed on 22 January 2022).
- Kuznetsova, L.; Cortassa, G.; Trilla, A. Effectiveness of Mandatory and Incentive-Based Routine Childhood Immunization Programs in Europe: A Systematic Review of the Literature. Vaccines 2021, 9, 1173. [Google Scholar] [CrossRef]
- Casula, M.; Toth, F. The 2017 Italian Reform on Mandatory Childhood Vaccinations: Analysis of the Policy Process and Early Implementation. Health Policy 2021, 125, 7–11. [Google Scholar] [CrossRef] [PubMed]
- Decreto—Legge 31 1 Aprile 2021, n. 44. Misure Urgenti Per Il Contenimento Dell’epidemia Da COVID-19, in Materia Di Vaccinazioni Anti SARS-CoV-2, Di Giustizia e Di Concorsi Pubblici. (21G00056) (GU Serie Generale n.79 Del 01-04-2021). Available online: https://www.gazzettaufficiale.it/eli/id/2021/04/01/21G00056/sg (accessed on 22 January 2022).
- Raffetti, E.; Mondino, E.; Di Baldassarre, G. COVID-19 Vaccine Hesitancy in Sweden and Italy: The Role of Trust in Authorities. Scand. J. Public Health 2022, 50, 803–809. [Google Scholar] [CrossRef] [PubMed]
- Gleason, J.L.; Jamison, A.; Freimuth, V.S.; Quinn, S.C. Home Remedy Use and Influenza Vaccination among African American and White Adults: An Exploratory Study. Prev. Med. 2019, 125, 19–23. [Google Scholar] [CrossRef] [PubMed]
- Guay, M.; Gosselin, V.; Petit, G.; Baron, G.; Gagneur, A. Determinants of Vaccine Hesitancy in Quebec: A Large Population-Based Survey. Hum. Vaccines Immunother. 2019, 15, 2527–2533. [Google Scholar] [CrossRef] [PubMed]
- Vögele, A.; Engl, A.; Wiedermann, C. Verwendung von Hausmitteln bei deutsch- und italienischsprachigen Erwachsenen in Südtirol, Italien. In Proceedings of the 51st Kongress für Allgemeinmedizin und Familienmedizin, Düsseldorf, Germany, 5 September 2017; German Medical Science GMS Publishing House: Düsseldorf, Germany, 2017; p. 258. [Google Scholar]



| Characteristics N (%) | Overall 1425 (100) N (%) | Non-Hesitant 1204 (84.4) N (%) | Hesitant 222 (15.6) N (%) | p–Values † |
|---|---|---|---|---|
| Age (years) | <0.001 | |||
| 18–34 | 334 (23.4) | 248 (74.3) | 86 (25.7) | |
| 35–49 | 354 (24.8) | 281 (79.4) | 73 (20.6) | |
| 50–64 | 391 (27.4) | 342 (87.5) | 49 (12.5) | |
| ≥64 | 346 (24.3) | 332 (96) | 14 (4.0) | |
| Gender | n.s. | |||
| Male | 691 (48.5) | 587 (84.9) | 104 (15.1) | |
| Female | 735 (51.5) | 617 (83.9) | 118 (16.1) | |
| Education | 0.001 | |||
| Middle school or lower | 316 (22.2) | 278 (88) | 38 (12) | |
| Vocational school | 411 (28.9) | 335 (81.5) | 76 (18.5) | |
| High school | 410 (28.8) | 332 (81.0) | 78 (19) | |
| University | 287 (20.2) | 258 (89.9) | 29 (10.1) | |
| Residence | 0.013 | |||
| Urban | 602 (42.2) | 525 (87.2) | 77 (12.8) | |
| Rural | 824 (57.8) | 679 (82.4) | 145 (17.6) | |
| Citizenship | n.s. | |||
| Italian | 1307 (91.7) | 1107 (84.7) | 200 (15.3) | |
| Other | 118 (8.3) | 96 (81.4) | 22 (18.6) | |
| Native Language ‡ | <0.001 | |||
| German | 879 (61.7) | 740 (84.2) | 139 (15.8) | |
| Italian | 384 (26.9) | 339 (88.3) | 45 (11.7) | |
| Ladin | 57 (4) | 47 (82.5) | 10 (17.5) | |
| Other/more than one | 106 (7.3) | 78 () | 28 () | |
| Household/Family structure (more than one answer possible) | ||||
| Single | 236 (16.5) | 206 (87.3) | 30 (12.7) | n.s. |
| Children 0–6 years of age | 178 (12.5) | 137 (77.0) | 41 (23.0) | 0.003 |
| Adolescents 7–17 years of age | 276 (19.4) | 223 (85.4) | 168 (14.6) | n.s. |
| Patient at risk of COVID-19 + | 301 (21.1) | 275 (91.4) | 26 (8.6) | <0.001 |
| None of the above | 522 (36.6) | 432 (82.8) | 90 (17.2) | n.s. |
| Working in the health sector | n.s. | |||
| Yes | 85 (6.0) | 76 (89.4) | 9 (10.6) | |
| No | 1340 (94.0) | 1127 (84.4) | 222 (15.6) | |
| Chronic disease(s) | <0.001 | |||
| Yes | 246 (17.3) | 233 (94.7) | 13 (5.3) | |
| No | 1179 (82.7) | 970 (82.3) | 209 (17.7) | |
| COVID-19 infected | 0.003 | |||
| Yes | 251 (17.6) | 197 (78.5) | 54 (21.5) | |
| No | 1173 (82.4) | 1006 (85.8) | 167 (14.2) | |
| Economic situation (last 3 months) | <0.001 | |||
| Better | 43 (3.0) | 43 (100) | 0 (0) | |
| The same | 972 (68.3) | 850 (87.4) | 122 (12.6) | |
| Worse | 375 (26.3) | 285 (76.0) | 90 (24.0) | |
| Don’t know | 34 (2.4) | 25 (73.5) | 9 (26.5) |
| Category | Question | Response (Rather) Agree | Total N = 1425 (100%) N (%) | Non-Hesitant 1 N = 1204 (84.4%) N (%) | Hesitant 1 N = 222 (15.6%) N (%) | Cramér’s V (p–Value) |
|---|---|---|---|---|---|---|
| Decision making | I think that decisions about COVID-19 made by the public authorities are right | Yes | 788 (55) | 761 (97) | 27 (3) | 0.489 (<0.001) |
| No | 575 (40) | 393 (68) | 182 (32) | |||
| I think that decisions about vaccination against COVID-19 made by the public authorities are right | Yes | 992 (70) | 957 (96) | 35 (4) | 0.637 (<0.001) | |
| No | 331 (23) | 162 (49) | 169 (51) | |||
| I think that decisions about compulsory vaccination (not COVID-19) made by the public authorities are right | Yes | 952 (67) | 924 (97) | 28 (3) | 0.658 (<0.001) | |
| No | 348 (24) | 170 (49) | 178 (51) | |||
| Trust in COVID-19 vaccination 2 | I believe vaccination can contain the spread of the virus 1 | Yes | 1227 (86) | 1139 (93) | 89 (7) | 0.65 (<0.001) |
| No | 198 (14) | 65 (33) | 133 (67) | |||
| If I knew that I’d already been infected with the virus, I wouldn’t get vaccinated | Yes | 492 (34) | 326 (66) | 166 (34) | 0.44 (<0.001) | |
| No | 933 (65) | 877 (94) | 56 (6) | |||
| When others are vaccinated against the virus, I don’t need to get vaccinated | Yes | 220 (15) | 101 (6) | 119 (54) | 0.557 (<0.001) | |
| No | 1206 (85) | 1102 (92) | 103 (8) | |||
| If vaccination was recommended to me, I would get vaccinated | Yes | 1174 (82) | 1138 (97) | 36 (3) | 0.789 (<0.001) | |
| No | 251 (18) | 66 (26) | 185 (74) | |||
| If my doctor recommended COVID-19 vaccination, I would get vaccinated | Yes | 1153 (81) | 1116 (97) | 37 (3) | 0.768 (<0.001) | |
| No | 273 (19) | 88 (32) | 185 (68) | |||
| COVID-19 vaccination is not necessary because… | It is not effective | Yes | 197 (14) | 76 (39) | 121 (61) | 0.577 (<0.001) |
| No | 1229 (86) | 1128 (92) | 101 (8) | |||
| …natural herd immunity is achieved with virus spread and that is quite sufficient | Yes | 274 (19) | 141 (12) | 133 (60) | 0.512 (<0.001) | |
| No | 1151 (81) | 1063 (92) | 89 (8) | |||
| …this disease does not exist/is a normal flu | Yes | 150 (10) | 74 (6) | 76 (34) | 0.44 (<0.001) | |
| No | 1276 (90) | 1130 (89) | 146 (11) | |||
| …the whole thing is only a profit for the pharmaceutical industry | Yes | 321 (22) | 159 (49) | 162 (51) | 0.583 (<0.001) | |
| No | 1105 (78) | 1045 (95) | 60 (5) | |||
| COVID-19 vaccination is harmful because… | ...long-term risks are not known | Yes | 665 (47) | 465 (70) | 201 (30) | 0.516 (<0.001) |
| No | 760 (53) | 740 (97) | 20 (3) | |||
| …new vaccines pose additional risks in the RNA | Yes | 306 (21) | 147 (48) | 159 (52) | 0.571 (<0.001) | |
| No | 1119 (79) | 1056 (94) | 63 (6) | |||
| ...there are doctors who advise against it | Yes | 308 (22) | 163 (53) | 145 (47) | 0.497 (0.001) | |
| No | 1117 (78) | 1040 (93) | 77 (7) | |||
| …a compulsory corona vaccination with the prioritization of certain groups will lead to major socio-political discussions | Yes | 512 (36) | 366 (30) | 148 (67) | 0.33 (<0.001) | |
| No | 912 (64) | 838 (92) | 74 (8) |
| Variable 1 | Question | Non-Hesitant 3 N = 1204 N (%) | Hesitant 3 N = 222 N (%) | Cramér’s V (p–Value) 2 | ||
|---|---|---|---|---|---|---|
| More Than Once a Week | More Than Once a Week | |||||
| Frequency of searching for information on COVID-19 | How often do you search for information on the novel coronavirus? | 586 (49) | 42 (19) | 0.323 *** | ||
| (Rather) trust/agree | Do not know | (Rather) trust/agree | Do not know | |||
| General national vaccination schedule | Aside from COVID-19, I think everyone should be vaccinated according to the national vaccination schedule | 993 (83) | n.a. | 51 (23) | n.a. | 0.593 *** |
| Trust—How much do you trust information about COVID-19 and vaccinations from the following sources? | TV | 455 (38) | 56 (4.7) | 19 (9) | 5 (2.4) | 0.406 *** |
| Newspapers/press | 443 (27) | 55 (4.5) | 24 (11) | 11 (5.2) | 0.354 *** | |
| Healthcare workers | 911 (76) | 57 (4.8) | 98 (44) | 13 (6) | 0.365 *** | |
| Social media | 144 (12) | 122 (10.1) | 18 (8) | 12 (5.3) | 0.143 *** | |
| Radio | 512 (43) | 100 (8.3) | 23 (10) | 13 (5.9) | 0.383 *** | |
| Ministry of Health | 788 (65) | 84 (7) | 49 (22) | 18 (7.9) | 0.441 *** | |
| National Institute of Health | 695 (68) | 201 (16.7) | 37 (17) | 35 (15.6) | 0.442 *** | |
| Famous people and influencers | 138 (11) | 152 (12.6) | 6 (3) | 19 (8.5) | 0.166 *** | |
| WHO | 774 (64) | 77 (6.4) | 48 (22) | 16 (7.1) | 0.441 *** | |
| Regional toll-free and emergency numbers | 568 (47) | 338 (28.1) | 48 (2%) | 53 (23.7) | 0.341 *** | |
| Civil protection | 863 (72) | 104 (8.6) | 77 (35) | 23 (10.3) | 0.423 *** | |
| Provincial government | 701 (58) | 42 (35) | 42 (19) | 10 (4.7) | 0.419 *** | |
| Management of the South Tyrolean Health Service | 776 (64) | 41 (3.4) | 48 (22) | 11 (4.9) | 0.386 *** | |
| Conspiracy—CMQ (Conspiracy Mental Questionnaire) | I think that many very important things happen in the world that the public is never informed about | 765 (64) | n.a. | 187 (84) | n.a. | 0.241 *** |
| I think politicians usually do not tell us the true motives for their decisions | 627 (52) | n.a. | 177 (80) | n.a. | 0.308 *** | |
| I think that government agencies closely monitor all citizens | 315 (26) | n.a. | 92 (41) | n.a. | 0.206 *** | |
| I think that events that superficially seem to lack a connection are often the result of secret activities | 320 (27) | n.a. | 105 (48) | n.a. | 0.222 *** | |
| I think that there are secret organizations that greatly influence political decisions | 383 (32) | n.a. | 126 (57) | n.a. | 0.258 *** | |
| Resilience | I have a hard time making it through stressful events | 375 (31) | n.a. | 71 (32) | n.a. | 0.044 (n.s.) |
| It does not take me long to recover from a stressful event | 628 (52) | n.a. | 123 (56) | n.a. | 0.083 (n.s.) | |
| It is hard for me to snap back when something bad happens | 419 (35) | n.a. | 79 (36) | n.a. | 0.08 (n.s.) | |
| Altruism—Altruistic Attitudes Among Older Adults Scale | I enjoy doing things for others | 966 (80) | n.a. | 180 (81) | n.a. | 0.03 (n.s.) |
| I try to help others, even if they do not help me | 933 (77) | n.a. | 152 (68) | n.a. | 0.098 * | |
| Seeing others prosper makes me happy | 1032 (86) | n.a. | 189 (85) | n.a. | 0.074 (n.s.) | |
| I really care about the needs of other people | 903 (75%) | n.a. | 165 (75) | n.a. | 0.073 (n.s.) | |
| I come first and should not have to care so much for others | 187 (16%) | n.a. | 36 (16) | n.a. | 0.032 (n.s.) | |
| Well-being—In the last two weeks … 4 | …I was happy and in a good mood | 797 (66) | n.a. | 138 (62) | n.a. | 0.079 (n.s.) |
| …I was calm and relaxed | 802 (67) | n.a. | 134 (60) | n.a. | 0.052 (n.s.) | |
| …I was active and energetic | 705 (59) | n.a. | 131 (59) | n.a. | 0.042 (n.s.) | |
| …I woke up fresh and rested | 742 (62) | n.a. | 124 (56) | n.a. | 0.094 ** | |
| …my everyday life was full of things that interest me | 688 (57) | n.a. | 109 (49) | n.a. | 0.072 (n.s.) | |
| Characteristic | Hesitancy | German | Italian | Ladin | Other/More Than One | p-Value * | |
|---|---|---|---|---|---|---|---|
| N = 879 % | N = 384 % | N = 57 % | N = 106 | ||||
| Age (median (IQR)) | No | 53 (38;67) | 56 (40;70) | 54 (44;64) | 38 (30;51) | <0.001 | |
| Yes | 36 (28;49) | 47 (35;54) | 44 (31;50) | 43 (30;48) | |||
| Females (%) | No | 54.6 | 44.1 | 42.6 | 56.4 | 0.001 | |
| Yes | 55.4 | 37.8 | 70.0 | 64.3 | |||
| Education (%) | Middle school or lower | No | 23.2 | 23.3 | 19.1 | 23.1 | <0.001 |
| Yes | 15.8 | 15.6 | 10.0 | 32.1 | |||
| Vocational school | No | 32.8 | 18.9 | 34.0 | 16.7 | ||
| Yes | 41.0 | 24.4 | 60.0 | 7.1 | |||
| High school | No | 25.9 | 30.1 | 29.8 | 32.1 | ||
| Yes | 35.3 | 37.8 | 10.0 | 39.3 | |||
| University | No | 18.1 | 27.7 | 17.0 | 28.2 | ||
| Yes | 7.9 | 22.2 | 20.0 | 21.4 | |||
| Italian citizenship (%) | No | 95.4 | 97.6 | 100.0 | 29.9 | <0.001 | |
| Yes | 98.6 | 91.1 | 100.0 | 39.3 | |||
| Household / family structure (%) † | Single | No | 18.5 | 16.5 | 8.5 | 11.7 | n.s. |
| Yes | 14.4 | 13.3 | 10.0 | 4.3 | |||
| Children from 0–6 | No | 11.9 | 8.3 | 8.3 | 22.1 | 0.001 | |
| Yes | 20.1 | 11.1 | 10.0 | 25.0 | |||
| Adolescents from 7–17 | No | 19.2 | 16.5 | 10.4 | 26.9 | n.s. | |
| Yes | 21.6 | 22.2 | 40.0 | 32.1 | |||
| Patient at risk of COVID-19 | No | 23.4 | 23.1 | 25.5 | 15.4 | n.s. | |
| Yes | 13.8 | 11.1 | 10.0 | 3.6 | |||
| None of the above mentioned | No | 34.9 | 38.3 | 50.0 | 26.9 | n.s. | |
| Yes | 39.9 | 44.4 | 44.4 | 35.7 | |||
| Working in the health sector (%) | No | 6.6 | 5.9 | 8.3 | 5.1 | n.s. | |
| Yes | 2.9 | 2.2 | 0 | 10.7 | |||
| Chronic disease(s) (%) | No | 19.5 | 19.8 | 17.0 | 17.9 | n.s. | |
| Yes | 7.9 | 4.4 | 0 | 0 | |||
| Economic situation of the last 3 months (%) | Better | No | 3.4 | 3.8 | 6.4 | 2.6 | <0.001 |
| Yes | 0 | 0 | 0 | 0 | |||
| The same | No | 72.3 | 76.4 | 42.6 | 46.2 | ||
| Yes | 54.7 | 71.1 | 50.0 | 35.7 | |||
| Worse | No | 22.0 | 18.9 | 51.1 | 44.9 | ||
| Yes | 41.7 | 24.4 | 50.0 | 53.6 | |||
| Don’t know | No | 2.3 | 0.9 | 0 | 6.4 | ||
| Yes | 3.6 | 4.4 | 0 | 10.7 | |||
| COVID-19 infected (%) | No | 16.5 | 16.8 | 22.9 | 10.4 | n.s. | |
| Yes | 29.0 | 11.1 | 20.0 | 25.0 | |||
| Urban residence (%) | No | 26.1 | 82.2 | 12.8 | 61.0 | <0.001 | |
| Yes | 19.4 | 77.8 | 10.0 | 50.0 | |||
| Hesitancy (%) | No | 26.1 | 82.2 | 12.8 | 61.0 | 0.002 | |
| Yes | 19.4 | 77.8 | 10.0 | 50.0 | |||
| Conspiracy thinking (median (IQR)) | No | 15 (11;19) | 16 (11;20) | 18 (14;23) | 16 (15;20) | <0.001 | |
| Yes | 21 (16;24) | 23 (19;27) | 20 (19;27) | 20 (18;24) | |||
| Trust in institutions (median (IQR)) | No | 33 (27;38) | 35 (30;40) | 35 (29;39) | 35 (27;43) | 0.003 | |
| Yes | 20 (12;28) | 23 (12;30) | 27 (20;32) | 21 (13;28) | |||
| Trust in media (median (IQR)) | No | 14 (11;18) | 13 (10;17) | 12 (10;15) | 14 (11;19) | 0.045 | |
| Yes | 8 (5;13) | 9 (6;13) | 13 (10;16) | 7 (5;10) | |||
| Trust in the national vaccination plan (median (IQR)) | No | 6 (4;6) | 6 (5;6) | 6 (4;6) | 5 (4;6) | <0.001 | |
| Yes | 2 (1;4) | 2 (1;3) | 2 (1;4) | 3 (1;4) | |||
| Frequency of information search (median (IQR)) | No | 3 (2;5) | 4 (3;6) | 4 (2;6) | 3 (2;5) | <0.001 | |
| Yes | 6 (2;7) | 6 (6;7) | 6 (6;7) | 6 (3;6) |
| Model 0 Nagelkerkes R2 = 0.614 | Model 1 Nagelkerkes R2 = 0.614 | ||||||
|---|---|---|---|---|---|---|---|
| Regression Coefficient B | p-Value | OR (95% CI) | Regression Coefficient B | p-Value | OR (95% CI) | ||
| Constant term | 0.293 | n.s. | 1340 | 2475 | 0.035 | 11,879 | |
| Age | −0.038 | 0.000 | 0.963 (0.963;0.973) | –0.035 | 0.000 | 0.966 (0.952;0.980) | |
| Educational level # | −0.284 | 0.001 | 0.753 (0.641;0.884) | –0.241 | 0.039 | 0.785 (0.624;0.988) | |
| Family and risk patterns | Children 0–6 years | 0.089 | n.s. | 1.093 (0.728;1.641) | 0.352 | n.s. | 1.422 (0.819;2.470) |
| Patient at risk of COVID-19 | −0.392 | n.s. | 0.675 (0.429;1.064) | –0.588 | n.s. | 0.555 (0.289;1.068) | |
| Chronic disease | −0.866 | 0.005 | 0.421 (0.229;0.771) | –1.033 | 0.012 | 0.356 (0.159;0.795) | |
| COVID-19 infected | 0.374 | 0.042 | 1.454 (1.013;2.085) | 0.227 | n.s. | 1.255 (0.769;2.048) | |
| Search for information | 0.210 | 0.001 | 1.234 (1.093;1.393) | ||||
| Altruism | I try to help others, even when they do not help me | 0.046 | n.s. | 1.047 (0.889;1.234) | |||
| Well-being | Feeling fresh an awake | 0.099 | n.s. | 1.104 (0.871;1.399) | |||
| Trust | Agree with national vaccination plan | –0.787 | 0.000 | 0.455 (0.399;0.520) | |||
| Trust in media | –0.024 | n.s. | 0.976 (0.918;1.037) | ||||
| Trust in institutions | –0.066 | 0.000 | 0.936 (0.907;0.966) | ||||
| Urban | −0.236 | n.s. | 0.790 (0.548;1.138) | 0.045 | n.s. | 1.046 (0.621;1.761) | |
| Mother tongue | Italian † | n.s. | n.s. | ||||
| German | 0.000 | n.s. | 1.000 (0.652;1.533) | –0.623 | n.s. | 0.536 (0.286;1.005) | |
| Ladin | 0.025 | n.s. | 1.025 (0.447;2.349) | –0.515 | n.s. | 0.597 (0.197;1.811) | |
| Other/more than one | 0.457 | n.s. | 1.580 (0.891;2.801) | –0.061 | n.s. | 0.941 (0.431;2.053) | |
| Economic situation # | 0.362 | 0.004 | 1.436 (1.124;1.836) | 0.042 | n.s. | 1.043 (0.770;1.413) | |
| Conspiracy thinking | 0.107 | 0.000 | 1.113 (1.071;1.157) | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barbieri, V.; Wiedermann, C.J.; Lombardo, S.; Ausserhofer, D.; Plagg, B.; Piccoliori, G.; Gärtner, T.; Wiedermann, W.; Engl, A. Vaccine Hesitancy during the Coronavirus Pandemic in South Tyrol, Italy: Linguistic Correlates in a Representative Cross-Sectional Survey. Vaccines 2022, 10, 1584. https://doi.org/10.3390/vaccines10101584
Barbieri V, Wiedermann CJ, Lombardo S, Ausserhofer D, Plagg B, Piccoliori G, Gärtner T, Wiedermann W, Engl A. Vaccine Hesitancy during the Coronavirus Pandemic in South Tyrol, Italy: Linguistic Correlates in a Representative Cross-Sectional Survey. Vaccines. 2022; 10(10):1584. https://doi.org/10.3390/vaccines10101584
Chicago/Turabian StyleBarbieri, Verena, Christian J. Wiedermann, Stefano Lombardo, Dietmar Ausserhofer, Barbara Plagg, Giuliano Piccoliori, Timon Gärtner, Wolfgang Wiedermann, and Adolf Engl. 2022. "Vaccine Hesitancy during the Coronavirus Pandemic in South Tyrol, Italy: Linguistic Correlates in a Representative Cross-Sectional Survey" Vaccines 10, no. 10: 1584. https://doi.org/10.3390/vaccines10101584
APA StyleBarbieri, V., Wiedermann, C. J., Lombardo, S., Ausserhofer, D., Plagg, B., Piccoliori, G., Gärtner, T., Wiedermann, W., & Engl, A. (2022). Vaccine Hesitancy during the Coronavirus Pandemic in South Tyrol, Italy: Linguistic Correlates in a Representative Cross-Sectional Survey. Vaccines, 10(10), 1584. https://doi.org/10.3390/vaccines10101584







