Abstract
Vaccines for human use have conventionally been developed by the production of (1) microbial pathogens in eggs or mammalian cells that are then inactivated, or (2) by the production of pathogen proteins in mammalian and insect cells that are purified for vaccine formulation, as well as, more recently, (3) by using RNA or DNA fragments from pathogens. Another approach for recombinant antigen production in the last three decades has been the use of plants as biofactories. Only have few plant-produced vaccines been evaluated in clinical trials to fight against diseases, of which COVID-19 vaccines are the most recent to be FDA approved. In silico tools have accelerated vaccine design, which, combined with transitory antigen expression in plants, has led to the testing of promising prototypes in pre-clinical and clinical trials. Therefore, this review deals with a description of immunoinformatic tools and plant genetic engineering technologies used for antigen design (virus-like particles (VLP), subunit vaccines, VLP chimeras) and the main strategies for high antigen production levels. These key topics for plant-made vaccine development are discussed and perspectives are provided.
1. Introduction
Since the initial comprehension of vaccination by Jenner and Pasteur [1], vaccines for human use have been conventionally developed by the production of (1) microbial pathogens or (2) pathogen proteins in mammalian and insect cells, which are then inactivated and/or purified for final formulations, and, very recently, (3) by using RNA or DNA [2]. Another approach for antigen production is the use of plants as biofactories, which was initially proposed approximately three decades ago [3]). In this period of time, the laboratory-assayed vaccines have reached clinical application. At present, influenza and COVID-19 plant-made vaccines have reached Phase 3 clinical trials, and their results are promising to carry them to commercialization. Ward et al. reported the efficacy, immunogenicity, and safety of a plant-derived, quadrivalent, influenza virus-like particle vaccine in adults and older adults in two Phase 3, multicenter, randomized trials. The results showed that the plant-derived vaccine is protective, well tolerated, and that no major safety signals arose in the participants of the clinical studies [4]. For the influenza virus, the importance of new platforms for vaccine production is due to (1) the humanized virus problem (adaptation to human cell receptors), which minimizes the efficacy of egg-produced vaccines; (2) the use of eggs in case of influenza pandemics could be self-defeating because they commonly originate in birds, so hens could be affected and produce less eggs, and (3), the virus could be lethal in chicken embryos and antigen production could be affected [5].
The emergence of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) has also demanded different strategies for vaccine production. Firstly, RNA and DNA vectors have been used to develop the widely distributed vaccines from Pfizer, Moderna, AstraZeneca, CanSino, and Sputnik [6]. Plant-made vaccines against COVID-19 disease have been also developed, mainly producing VLP-based vaccines, and two companies are bringing them to clinical approval. Medicago (CAN) and Kentucky BioProcessing Inc. (Owensboro, KY, USA) have proceeded to Phase 3 clinical trials and several other plant vaccines based on protein subunits are in the preclinical phase [7,8].
Other strategies in the preclinical phase have used plant vaccines administered orally in prime-boost immunization regimes. In this strategy, an injectable vaccine is applied as a prime-boost vaccine and an edible one as a booster. The main application of this strategy has been to improve the vaccine against poliovirus [9]. In this study, the plant oral vaccine as booster improved IgG- and IgA-level production in immunized mice. Notably, a new approach in generating an oral vaccine for poliovirus was to produce it in the chloroplast of edible lettuce [10].
Methods for genetic plant transformation have been developed to produce heterologous proteins in plant cells in the last 30 years. Initially, plants were genetically engineered by Agrobacterium-mediated nuclear transformation and later by chloroplast via the biolistic method [11,12,13]. These fundamental methods established the developmental basis for a wide number of transformation procedures that nowadays are applied for different designs of vaccines produced in plants (whole organism, specific tissue, and cell culture) and microalgae. An attractive approach is the design and production of virus-like particles (VLPs) in plants as subunit vaccines. This strategy has been useful to produce plant VLPs to fight against infectious diseases even at the industrial scale [8,14].
On the other hand, antigen selection is a key issue for plant-made vaccines. Experimental antigens—for which protective efficacy has been demonstrated at the preclinical or clinical level—have been selected to be produced in plants as a potential low-cost platform option [15,16]. Additionally, antigens can also be selected by immunoinformatic (in silico) approaches such as reverse vaccinology, using computational servers and software that predicts the potential immunogenicity of a given pathogen protein [17].
This review describes the elemental basis of antigen in silico design, plant transformation methods, recent VLP developments, and the most advanced vaccines produced in plant cells, highlighting the main plants used as vaccine biofactories.
2. Genetic Antigen Design for Subunit Vaccine Development
Subunit vaccines (SUV) arise from recombinant DNA and genetic engineering, which provide the opportunity to specifically select one or more immunoprotective antigens and produce them in another organism. Thus, the rapid growth of genomic information in database banks and the possibility of sequencing complete genomes allows the use of bioinformatics tools to quickly explore whether a certain protein pathogen has potential for use as an SUV. These bioinformatic tools can be based on (a) reverse vaccinology (RV), to evaluate the characteristics of multiple antigens of a given genome; (b) immunoinformatics, for the selection of immunogenic peptides from selected antigens; and (c) structural vaccinology, for searching for the best three-dimensional conformations of the vaccine protein (Table 1).

Table 1.
Computational sources for vaccine development (accessed on 26 December 2021).
The main RV computational tools available are New Enhanced Reverse Vaccinology Environment (NERVE) [18], Vaxign [19], VaxiJen [20] Jenner-predict [21], and VacSol [22]. RV emerged in 1997 with the first application of this method with Group B meningococcus (MenB) [23]. Currently, RV is based on (1) searching for the cellular location of pathogen proteins (e.g., LOCATE and LocDB [24,25]), where those that are exposed are usually the most selected for their rapid interaction with the cells of the immune system; (2) adhesin properties, where those pathogen components with the highest ones could be considered more immunogenic (e.g., SPAAN software [17]); (3) antigenicity, where the use of VaxiJen was the first RV software with a machine-learning strategy and a non-alignment approach for antigen prediction based on candidate antigen selection according to protein physicochemical properties [20]; (4) similarity, avoiding the use of sequences too similar to the host [26].
Immunoinformatics is applied to select the most probable immunogenic peptides to design multiepitopic vaccines. The software to be used can be directed to searching for (a) a cellular response by the affinity of peptides to the major histocompatibility complex I (MHC I, specific for cytotoxic T lymphocytes (CTL) [27,28]), or (b) a humoral response by affinity to specific B lymphocytes combining with selected peptides with affinity to the major histocompatibility complex type II (MHC II).
MHC I class molecules consist of heavy chains complexed with β2-microglobulin, which bind in the endoplasmic reticulum to peptides processed by the proteasome, and later display them on the cell surface to CTLs. High affinity at peptide-MHC I binding is difficult to dissociate where the amino-terminal of the peptide binds to pocket A, carboxyl-terminal to pocket F, and the preferred length of the peptide is usually 9 amino acids [29] (Table 1).
MHC II molecules consist of transmembrane chain proteins (α and β), expressed in the membrane of antigen-presenting cells (APC), mainly in dendritic cells (DC) [30] to show antigens to lymphocytes T CD4+. These peptides come from degraded proteins in the endosome, making it possible to respond to extracellular antigens [31]. The peptides that bind to MHC II pockets are usually 15 amino acids long and can extend outward from the peptide–MHC II binding site [29] (Table 1).
On the other hand, the most used servers for predicting epitopes for B cells are: BepiPred-2.0 [32], DiscoTope 2.0 Server [33], ABCpred [34], and COBEpro [35] (Table 1).
Structural vaccinology is used once the epitopes have been selected to organize them in the best way for a correct three-dimensional conformation with the best immunogenic properties for conformational and linear epitopes, which implies estimating tertiary structure. Subsequently, this structure must be refined and finally validated using different software (Table 1) to obtain a better quality model.
A good option to complement the in silico studies for multi-epitope vaccine development is the use of molecular docking to evaluate interaction with a determinate receptor of the immune system of interest. This approach can be explored through the servers PatchDock [36] and Autodock Vina [37]. Molecular dynamics can also be performed with software such as NAMD and VMD [38]. Figure 1 depicts the general route in subunit vaccine design considering the immunoinformatic approach.
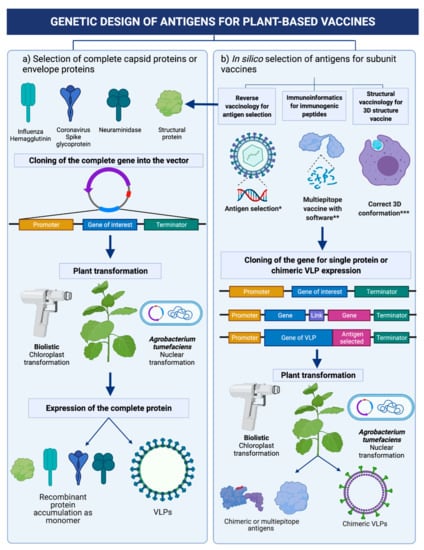
Figure 1.
Strategies for designing and producing subunit vaccines using plants as biofactories. (a) Expression of complete antigenic viral protein (commonly surface proteins), (b) Expression of antigens (fragments of the viral proteins recognized by the immunological system) * Cellular location; adhesin properties; antigenicity; avoid similar host proteins. ** Cellular response by affinity to MHC I or CTL; or humoral response by affinity to MHC II or B lymphocytes. *** Tertiary structure prediction; refinement and validation; molecular docking or dynamics.
3. Virus-Like Particles (VLP) and Chimeric Virus-Like Particles (ChVLP) for Subunit Vaccine Production in Plants
Subunit vaccines tend to have low immunogenicity, making the use of adjuvants, higher doses, or booster schedules necessary. Viral virus-like particles (VLPs) are a model of subunit vaccines that are more immunogenic than the three-dimensional formation of individual antigenic proteins. VLPs are a set of repeated structural viral proteins capable of assembling in sizes from 22–150 nm, where 40-nm size has been considered as optimal for recognition by dendritic cells [39]. VLPs have been considered to be a safer option than killed or inactivated pathogen vaccines since they lack genetic material, allowing them to have up to three different protein forming layers from a single structural antigen [40]. In this sense, VLPs can be enveloped or non-enveloped. Non-enveloped VLPs do not include any components of the producer cell and are the most widely used in clinical trials [15]. On the other hand, enveloped VLPs are more complex, including producer cell membrane components with antigens exposed on the outer surface [41].
Since the first VLP produced by Valenzuela et al. [42] consisted of the HBsAg antigen, multiple VLPs have been produced using various platforms. Vaccine production in plants has the advantages of low production costs, high yields, and complex protein production to allow conformation of VLP structures [15,16]). The production of the first antigen in plants (HbsAg) [3] has led to a wide variety of vaccine antigen prototypes of VLP structures produced in plants [3,43]. The most recent are mentioned in Table 2. As noted, the most recent studies of VLPs in plants have used Nicotiana benthamiana because of its great capacity to form complex structures with high yields [44,45], although Nicotiana tabacum and Arabidopsis thaliana have also been used [46], as well as potato, tomato, and lettuce [10,47,48]. Edible plant-made vaccines are mainly interesting when oral administration is used as the inoculation route.

Table 2.
Main antigens recently expressed as viral virus-like particles (VLPs).
A more recent model of VLPs is focused on the development of chimeric VLPs, which have the advantage of being multivalent, that is, made up of antigens from different pathogens [49,50] and even able to incorporate functional RNA segments [51]. One of the advantages of the chimeric VLP approach is multivalence and the fact that some epitopes or antigens could serve as adjuvants for others. However, some limitations have been identified with the correct folding of the protein, so strategies must be included in the construction design to overcome such problems [52]. Table 2 shows the main antigens recently produced as VLPs.
Another version of chimeric VLP is achieved by inserting immunogenic peptides in the VLP of plant viruses instead of other mammalian viruses. To ensure that the modified capsid protein (CP) of the plant virus shapes the VLP, the added peptide should be located in the surface structure, which is commonly achieved by cloning the antigenic peptide at the N or C terminal of the CP protein [14].
4. Plant Genetic Engineering Transformation Methods for Subunit Vaccine Production
4.1. Stable Nuclear Transformation
Plant cell nuclear transformation was developed four decades ago and has been mainly achieved by Agrobacterium tumefaciens transfection [11,12]. In this method, the DNA containing the transcriptional unit (promoter-gene (antigen)-terminator) for protein expression is cloned in a binary plasmid, commonly pBI121 and pCambia [58]. Then, a plasmid containing the transcriptional unit of the antigen is introduced into A. tumefaciens, usually by electroporation. Next, agrobacterium containing plasmids is co-cultured with plant leaf or stem fragments, followed by a complete transgenic plant regeneration through organogenesis or embryogenesis processes [59]. Finally, transgenes and proteins can be detected in fully regenerated plants to confirm genetic transformation and antigen expression.
Initially, the model plant Nicotiana tabacum was the main plant used for vaccine production [60]. Currently, many other plants have been considered for vaccine production, some of which have advantages for oral vaccine formulation, such as lettuce and carrots [61,62,63,64]. In agrobacterium-mediated nuclear transformation, plasmids contain a fragment between the T borders (right and left) that is genetically recombined with the nuclear genome upon delivery [65,66]. This fragment harbors a gene that codes for a trait of antibiotic resistance to select transformed cells. Those transformed cells are cultured in media with regulators and hormones for full plant regeneration [67,68]. Gene expression and antigen production in transgenic plants is controlled by promoters that can be constitutive or inducible by a substance or physical conditions, e.g., alcohol, NaCl, temperature, or light [69,70,71]. Remarkably, viral genetic elements can be added into the genetic construction to amplify the number of gene copies [72,73] and protein yields.
4.2. Transient Nuclear Transformation
The transient nuclear expression approach is considered when transformed plant cells must be maintained for a short period (two to 10 days). In this case, transgene integration into the nuclear genome is not forced by the antibiotic selection. However, many gene copies are delivered into the nucleus and are capable of producing messenger RNA for high recombinant protein production [74,75]. Transient transformation can be obtained by different strategies where the main aspect is to “infect” a great number of plant cells by using any (or jointly) Agrobacterium tumefaciens or viral vectors containing the gene coding antigen [76]. Transient and stable transformation can also be applied to plant cell culture or to microalgae where antigen production could be more uniform and manufacturing practices more efficient, especially in the containment of genetically modified cells [77].
One of the most known viral vectors used in transient expression was developed using elements of the RNA of the Tobacco mosaic virus (TMV). Icon genetics named this system magnICON© (DENCA, Tokyo, Japan) and the procedures of plant transformation magnifection [78,79]. Currently, a wide repertory of viral vector types is available, and practically any type of virus could be used to design an expression vector. Recently, the Bamboo mosaic virus of the genus potexvirus was used as viral vector to produce Japanese Encephalitis Virus antigens in ^plants [80]. Viral vectors based on plant geminiviruses have been widely used for protein production of biopharmaceutical interest [81,82,83,84]. The mechanism of rolling circle replication allows replicon delivery (copies of transgenes) and can be designed to produce more than one protein in plant cells [85]. Notably, the specific ability of each virus to evade plant immune systems and replicate into the plant cells determines the success of the viral vector in achieving high antigen production.
4.3. Chloroplast Transformation
Chloroplast transformation was the first genetic modification of a green cell, performed approximately three decades ago [13]. Initially, the transformation was conducted to create antibiotic-resistant cells [86]. Chloroplast transformation was first achieved through biolistic procedures [87,88], where gold or tungsten microparticles (~10 µm) are coated with genetic material containing minimal gene expression units and then projected into the target cells for transformation [87,88]. Once in the cell, DNA molecules can be integrated into the chloroplast genome through DNA recombination mechanisms [89]. Other plastid organelles have been transformed, such as chromoplasts (plastids in fruits) and those in tubers [90,91,92]. Currently, antigen production in the chloroplast has advantages including higher recombinant protein production than that of stable nuclear transformation, which is determined by the copy number of chloroplast genomes in a given plant [93]. Thus, the chloroplast could be used to produce proteins for subunit vaccines. However, the chloroplast does not have post-translational modification machinery, which is a disadvantage when a post-translational modified protein is necessary for vaccine production.
5. Main Plants Used as Biofactories in Vaccine Production
Plants have been used as alternatives for low-cost biopharmaceutical production while reducing the threat for contamination by pathogens and exploiting their great industrial potential. The use of plants for protein recombinant production dates to 1990, when human serum albumin was produced in tobacco. Several plant-based vaccines have been produced against both human and animal pathogens. When vaccines are produced in plants, special attention is focused on evaluating the possibility of the vaccines causing allergies [94]. In this regard, each plant-made vaccine, either purified or in whole-raw material, should be evaluated for security as one of the first steps of vaccine development. For instance, Ward et al. demonstrated that plant-made VLPs influenza vaccine had no allergic or hypersensitivity reactions in subjects during Phase I/II clinical trials [95].
Plant species or specific tissues in a particular plant for commercial recombinant protein production have considerable variability. Several plants, including potato, corn, rice, and soybean, among others, have been used to produce recombinant proteins, including the Hepatitis B vaccine produced in lettuce [96]. However, tobacco and alfalfa have been commonly used because of their high biomass and seed yield and short life cycle.
Seeds can be attractive because of their stability in long storage periods compared to other plant materials. For instance, the companies SemBioSys Genetics, and Ventria Biosciences have seed-based recombinant production systems [97]. Proteins of different molecular weights have been expressed in plant seeds [98], and attempts have been made to develop vaccines in seeds. For example, the Hepatitis B virus (HBV) surface antigen (HBsAg) SS1 was produced in rice using the seed-specific Glub-4 promoter. Moreover, mice immunized with this vaccine prototype produced specific antibodies against both S and preS1 epitopes, demonstrating the potential of rice-derived SS1 antigen as an alternative HBV vaccine for Hepatitis B disease [99].
Transgenic potatoes also have been demonstrated to be an excellent expression system. Among the antigens produced in potatoes, the enterotoxigenic Escherichia coli (ETEC) labile toxin B-subunit (LTB) [100], and the Norwalk virus capsid protein (NVCP) [101] were promising candidates in clinical trials. Remarkably, the administration of corn seed-made LTB in clinical trials demonstrated similar outcomes to those of the potato study [102]. Another interesting crop used for vaccine production are tomatoes, which have been genetically modified to produce a rabies vaccine [103].
An important aspect when producing vaccines in plants is the containment of transgenes. In this arena, Murphy [104] has reviewed diverse strategies for biocontainment of transgenes, of which the main ones are using male sterility in transgenic plants, transplastomic plants, inducible and transient expression systems, and plant cell cultures instead of whole plants.
A key topic of plant-based vaccines is the possibility of direct oral delivery. In this aspect, when the vaccine is ingested orally, the antigens are expected to be protected from acids and enzymes in the stomach via bio-encapsulation because human digestive enzymes are incapable of breaking down glycosidic bonds in carbohydrates that make up the plant cell wall. However, when intact plant cells containing the vaccine reach the small intestine, commensal microbes digest the cell wall releasing the antigens. When antigens are fused with suitable transmucosal adjuvants (e.g., cholera toxin non-toxic subunit B (CTB)), they are delivered more efficiently to the immune or circulatory system [105,106].
The edible crops mostly used for generating plant-based vaccines have several advantages when compared with the same products made with other plant species. For example, in tobacco (Nicotiana tabacum or N. benthamiana) plants, the antigen needs to be subsequently purified before being tested, and this process can represent almost 80% of the total vaccine production cost [107].
Moreover, if the vaccine is maintained in lyophilized conditions, cold chain facilities would not be needed to stock and deliver the respective plant material, meaning greater cost efficiency compared to conventional mammalian or fermentation-based vaccines.
6. Plant Vaccines Today and Perspectives
Recently, Ward et al. [4] described Phase 3, (NCT03321968) of a quadrivalent, recombinant, virus-like particle (VLP) influenza vaccine produced in plants. This platform is based on transient protein expression in N. benthamiana and yields VLPs bearing hemagglutinin (HA) protein trimers that are combined in a quadrivalent vaccine (QVLP). These authors showed 96.3% efficacy, since a lot-to-lot study was carried out just prior to two pivotal placebo-controlled efficacy trials of the same plant-derived QVLP vaccine in ~23,000 adult subjects ≥ 18 years of age, and supported earlier findings of the safety profile and immunogenicity of the plant-derived QVLP, demonstrating the consistency with which it can be produced [108].
Although several vaccines against COVID-19 have been already delivered, different companies are developing plant-made vaccines [8] and some of them are in process of clinical trials [109,110].
On the other hand, Medicago (Quebec, Canada), a biopharmaceutical company, recently announced an FDA-approved CoVLP plant-derived vaccine against COVID-19 administered alone or with AS03 or CpG1018 adjuvants from the GSK Company (Brentford, Middlesex, UK). In the preliminary study, the co-primary outcomes were short-term tolerability/safety and immunogenicity of CoVLP formulations assessed by neutralizing antibody (NAb) and cellular responses [111]. Secondary outcomes in this study included safety and immunogenicity assessments up to 12 months after vaccination. Especially in COVID vaccines, Kumar et al. have reviewed the main companies that are working on developing plant-made vaccine platforms. Medicago and Kentucky BioProcessing Inc (Owensboro, KY, USA) have proceeded to the most advanced clinical trials [112].
These examples highlight that plant-made vaccine platforms are a reliable commercial option in the 21st century. Research groups around the globe are mainly working on a major challenge: increasing protein yields. Nevertheless, some specific commercial niches are being covered by plants, such as glucocerebrosidase against Gaucher’s disease [113]. Laere et al. [114] questioned why a commercial plant-produced vaccine had not been made after two decades of plant vaccine development. The authors pointed out three particular challenges: (1) selection of antigen and plant expression hosts; (2) dosage consistency; and (3) vaccine manufacturing, according to good manufacturing practice (GMP) procedures. Today, companies like Medicago and Kentucky BioProcessing have overcome these limitations.
7. Conclusions
Plant-based vaccination is evolving. Improvements and innovations to plant biotechnology platforms have been made by incorporating immunoinformatic tools, genetic engineering methods, and strategies for high yield recombinant vaccine production. Firstly, most of the immunoinformatic tools are free of charge and offer excellent opportunities for novel vaccine designs. In the near future, artificial intelligence will be the central motor for predicting reliable antigens and epitopes for subunit vaccine design. Secondly, it is envisaged that genetic engineering tools can be improved for transient expression as an approach to increase protein yields, with special focus on organic nanoparticles called VLPs to fight against viral diseases. Thirdly, with the fact that industry is involved in the current pandemic challenge and a plant-made vaccine against COVID-19 is now available, new investment for this biotechnological platform could expand in the following years. Future efforts should be directed to moving the experimental success of other plant-made vaccines to clinical applications.
Author Contributions
Conceptualization, B.B.-H. and E.M.-E.; writing—original draft preparation, A.R.-V., E.M.-E., C.A. and B.B.-H.; writing—review and editing, C.A. and B.B.-H.; funding acquisition, E.M.-E. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by CONACYT/México grants that supported this publication (grant CB-A1-S-17585 to EME).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
The authors thank Diana Fischer for English editing.
Conflicts of Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Flemming, A. The origins of vaccination. Nat. Milest. Vaccines 2020, p. S5. Available online: https://media.nature.com/original/magazine-assets/d42859-020-00006-7/d42859-020-00006-7.pdf, (accessed on 4 January 2022).
- Vetter, V.; Denizer, G.; Friedland, L.R.; Krishnan, J.; Shapiro, M. Understanding modern-day vaccines: What you need to know. Ann. Med. 2018, 50, 110–120. [Google Scholar] [CrossRef]
- Mason, H.S.; Lam, D.M.; Arntzen, C.J. Expression of hepatitis B surface antigen in transgenic plants. Proc. Natl. Acad. Sci. USA 1992, 89, 11745–11749. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ward, B.J.; Makarkov, A.; Séguin, A.; Pillet, S.; Trépanier, S.; Dhaliwall, J.; Landry, N. Efficacy, immunogenici-ty, and safety of a plant-derived, quadrivalent, virus-like particle influenza vaccine in adults (18–64 years) and older adults (≥65 years): Two multicentre, randomised phase 3 trials. Lancet 2020, 396, 1491–1503. [Google Scholar] [CrossRef]
- Tregoning, J.S. First human efficacy study of a plant-derived influenza vaccine. Lancet 2020, 396, 1464–1465. [Google Scholar] [CrossRef]
- Zieneldien, T.; Kim, J.; Cao, J.; Cao, C. COVID-19 vaccines: Current conditions and future prospects. Biology 2021, 10, 960. [Google Scholar] [CrossRef] [PubMed]
- Venkataraman, S.; Hefferon, K.; Makhzoum, A.; Abouhaidar, M. Combating human viral diseases: Will plant-based vaccines be the answer? Vaccines 2021, 9, 761. [Google Scholar] [CrossRef]
- Maharjan, P.M.; Choe, S. Plant-based COVID-19 vaccines: Current status, design, and development strategies of candidate vaccines. Vaccines 2021, 9, 992. [Google Scholar] [CrossRef] [PubMed]
- Chan, H.T.; Xiao, Y.; Weldon, W.C.; Oberste, S.M.; Chumakov, K.; Daniell, H. Cold chain and virus-free chloroplast-made booster vaccine to confer immunity against different poliovirus serotypes. Plant Biotechnol. J. 2016, 14, 2190–2200. [Google Scholar] [CrossRef] [PubMed]
- Daniell, H.; Rai, V.; Xiao, Y. Cold chain and virus-free oral polio booster vaccine made in lettuce chloroplasts confers protection against all three poliovirus serotypes. Plant Biotechnol. J. 2018, 17, 1357–1368. [Google Scholar] [CrossRef]
- Bevan, M.W.; Flavell, R.B.; Chilton, M.-D. A chimaeric antibiotic resistance gene as a selectable marker for plant cell transformation. Nat. Cell Biol. 1983, 304, 184–187. [Google Scholar] [CrossRef]
- Gelvin, S.B. Improving plant genetic engineering by manipulating the host. Trends Biotechnol. 2003, 21, 95–98. [Google Scholar] [CrossRef]
- Boynton, J.E.; Gillham, N.W.; Harris, E.H.; Hosler, J.P.; Johnson, A.M.; Jones, A.R.; Randolph-Anderson, B.L.; Robertson, D.; Klein, T.M.; Shark, K.B.; et al. Chloroplast transformation in Chlamydomonas with high velocity microprojectiles. Science 1988, 240, 1534–1538. [Google Scholar] [CrossRef]
- Balke, I.; Zeltins, A. Use of plant viruses and virus-like particles for the creation of novel vaccines. Adv. Drug Deliv. Rev. 2019, 145, 119–129. [Google Scholar] [CrossRef]
- Lua, L.H.L.; Connors, N.K.; Sainsbury, F.; Chuan, Y.P.; Wibowo, N.; Middelberg, A.P.J. Bioengineering virus-like particles as vaccines. Biotechnol. Bioeng. 2014, 111, 425–440. [Google Scholar] [CrossRef]
- Rybicki, E.P. Plant molecular farming of virus-like nanoparticles as vaccines and reagents. WIREs Nanomed. Nanobiotechnol. 2020, 12, e1587. [Google Scholar] [CrossRef] [PubMed]
- Sachdeva, G.; Kumar, K.; Jain, P.; Ramachandran, S. SPAAN: A software program for prediction of adhesins and adhesin-like proteins using neural networks. Bioinformatics 2004, 21, 483–491. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vivona, S.; Bernante, F.; Filippini, F. NERVE: New enhanced reverse vaccinology environment. BMC Biotechnol. 2006, 6, 1–8. [Google Scholar] [CrossRef]
- He, Y.; Xiang, Z.; Mobley, H.L. Vaxign: The first web-based vaccine design program for reverse vaccinology and applications for vaccine development. J. Biomed. Biotechnol. 2010, 2010, 297505. [Google Scholar] [CrossRef] [PubMed]
- Doytchinova, I.A.; Flower, D.R. VaxiJen: A server for prediction of protective antigens, tumour antigens and subunit vaccines. BMC Bioinform. 2007, 8, 4. [Google Scholar] [CrossRef] [Green Version]
- Jaiswal, V.; Chanumolu, S.K.; Gupta, A.; Chauhan, R.S.; Rout, C. Jenner-predict server: Prediction of protein vaccine candidates (PVCs) in bacteria based on host-pathogen interactions. BMC Bioinform. 2013, 14, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Rizwan, M.; Naz, A.; Ahmad, J.; Naz, K.; Obaid, A.; Parveen, T.; Ahsan, M.; Ali, A. VacSol: A high throughput in silico pipeline to predict potential therapeutic targets in prokaryotic pathogens using subtractive reverse vaccinology. BMC Bioinform. 2017, 18, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zollinger, W.D. New and improved vaccines against meningococcal disease. In New Generation Vaccines, 2nd ed.; Levine, M.L., Woodrow, G.C., Kaper, J.B., Cobon, G.S., Eds.; Walter Reed Army Institute of Research: Washington, DC, USA, 1997; pp. 469–488. [Google Scholar]
- LOCATE. Available online: https://bio.tools/locate (accessed on 15 August 2021).
- LocDB. Available online: https://www.rostlab.org/services/locdb/ (accessed on 15 August 2021).
- Altschul, S.F.; Gish, W.; Miller, W.; Myers, E.W.; Lipman, D.J. Basic local alignment search tool. J. Mol. Biol. 1990, 215, 403–410. [Google Scholar] [CrossRef]
- Townsend, A.; Bodmer, H. Antigen recognition by Class I-restricted T lymphocytes. Annu. Rev. Immunol. 1989, 7, 601–624. [Google Scholar] [CrossRef]
- Garrett, T.P.J.; Saper, M.A.; Bjorkman, P.J.; Strominger, J.L.; Wiley, D.C. Specificity pockets for the side chains of peptide antigens in HLA-Aw68. Nat. Cell Biol. 1989, 342, 692–696. [Google Scholar] [CrossRef] [PubMed]
- Wieczorek, M.; Abualrous, E.T.; Sticht, J.; Álvaro-Benito, M.; Stolzenberg, S.; Noé, F.; Freund, C. Major histo-compatibility complex (MHC) class I and MHC class II proteins: Conformational plasticity in antigen presentation. Front. Immunol. 2017, 8, 292. [Google Scholar] [CrossRef] [Green Version]
- Santambrogio, L.; Sato, A.K.; Fischer, F.R.; Dorf, M.E.; Stern, L.J. Abundant empty class II MHC molecules on the surface of immature dendritic cells. Proc. Natl. Acad. Sci. USA 1999, 96, 15050–15055. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Benacerraf, B. Role of MHC gene products in immune regulation. Science 1981, 212, 1229–1238. [Google Scholar] [CrossRef]
- Jespersen, M.C.; Peters, B.; Nielsen, M.; Marcatili, P. BepiPred-2.0: Improving sequence-based B-cell epitope prediction using conformational epitopes. Nucleic Acids Res. 2017, 45, W24–W29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kringelum, J.V.; Lundegaard, C.; Lund, O.; Nielsen, M. Reliable B cell epitope predictions: Impacts of method development and improved benchmarking. PLoS Comput. Biol. 2012, 8, e1002829. [Google Scholar] [CrossRef]
- Saha, S.; Raghava, G.P.S. Prediction of continuous B-cell epitopes in an antigen using recurrent neural net-work. Proteins 2006, 65, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Sweredoski, M.J.; Baldi, P. COBEpro: A novel system for predicting continuous B-cell epitopes. Protein Eng. Des. Sel. 2008, 22, 113–120. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schneidman-Duhovny, D.; Inbar, Y.; Nussinov, R.; Wolfson, H.J. PatchDock and SymmDock: Servers for rigid and symmetric docking. Nucleic Acids Res. 2005, 33, W363–W367. [Google Scholar] [CrossRef] [Green Version]
- Trott, O.; Olson, A.J. AutoDock Vina: Improving the speed and accuracy of docking with a new scoring function, efficient optimization, and multithreading. J. Comput. Chem. 2010, 31, 455–461. [Google Scholar] [CrossRef] [Green Version]
- Humphrey, W.; Dalke, A.; Schulten, K. VMD: Visual molecular dynamics. J. Mol. Graph. 1996, 14, 33–38. [Google Scholar] [CrossRef]
- Fifis, T.; Gamvrellis, A.; Crimeen-Irwin, B.; Pietersz, G.A.; Li, J.; Mottram, P.L.; McKenzie, I.F.C.; Plebanski, M. Size-Dependent Immunogenicity: Therapeutic and Protective Properties of Nano-Vaccines against Tumors. J. Immunol. 2004, 173, 3148–3154. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zeltins, A. Construction and characterization of virus-like particles: A review. Mol. Biotechnol. 2012, 53, 92–107. [Google Scholar] [CrossRef] [PubMed]
- Dai, S.; Wang, H.; Deng, F. Advances and challenges in enveloped virus-like particle (VLP)-based vaccines. J. Immunol. Sci. 2018, 2, 36–41. [Google Scholar]
- Valenzuela, P.; Medina, A.; Rutter, W.J.; Ammerer, G.; Hall, B.D. Synthesis and assembly of hepatitis B virus surface antigen particles in yeast. Nat. Cell Biol. 1982, 298, 347–350. [Google Scholar] [CrossRef]
- Scotti, N.; Rybicki, E. Virus-like particles produced in plants as potential vaccines. Expert Rev. Vaccines 2013, 12, 211–224. [Google Scholar] [CrossRef]
- Veerapen, V.P.; van Zyl, A.R.; Wigdorovitz, A.; Rybicki, E.P.; Meyers, A.E. Novel expression of immunogenic foot-and-mouth disease virus-like particles in Nicotiana benthamiana. Virus Res. 2018, 244, 213–217. [Google Scholar] [CrossRef]
- Marsian, J.; Fox, H.; Bahar, M.W.; Kotecha, A.; Fry, E.E.; Stuart, D.I.; Macadam, A.J.; Rowlands, D.J.; Lomonossoff, G.P. Plant-made polio type 3 stabilized VLPs—A candidate synthetic polio vaccine. Nat. Commun. 2017, 8, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Greco, R.; Michel, M.; Guetard, D.; Cervantes-Gonzalez, M.; Pelucchi, N.; Wain-Hobson, S.; Sala, F.; Sala, M. Production of recombinant HIV-1/HBV virus-like particles in Nicotiana tabacum and Arabidopsis thaliana plants for a bivalent plant-based vaccine. Vaccine 2007, 25, 8228–8240. [Google Scholar] [CrossRef]
- Huang, Z.; Elkin, G.; Maloney, B.J.; Beuhner, N.; Arntzen, C.J.; Thanavala, Y.; Mason, H.S. Virus-like particle expression and assembly in plants: Hepatitis B and Norwalk viruses. Vaccine 2005, 23, 1851–1858. [Google Scholar] [CrossRef]
- Saldaña, S.; Guadarrama, F.E.; Flores, T.D.J.O.; Arias, N.; Lopez, S.; Arias, C.; Ruiz-Medrano, R.; Mason, H.; Mor, T.; Richter, L.; et al. Production of rotavirus-like particles in tomato (Lycopersicon esculentum L.) fruit by expression of capsid proteins VP2 and VP6 and immunological studies. Viral Immunol. 2006, 19, 42–53. [Google Scholar] [CrossRef]
- Gonzalez-Castro, R.; Galindo, G.A.; Salcedo, Y.G.; Campero, L.U.; Perez, V.V.; Carrillo-Tripp, M.; Gevorkian, G.; Lim, M.A.G. Plant-based chimeric HPV-virus-like particles bearing amyloid-β epitopes elicit antibodies able to recognize amyloid plaques in APP-tg mouse and Alzheimer’s disease brains. Inflammopharmacology 2017, 26, 817–827. [Google Scholar] [CrossRef] [PubMed]
- Rutkowska, D.A.; Mokoena, N.; Tsekoa, T.L.; Dibakwane, V.S.; O’Kennedy, M.M. Plant-produced chimeric virus-like particles—A new generation vaccine against African horse sickness. BMC Vet. Res. 2019, 15, 1–15. [Google Scholar] [CrossRef]
- Fang, P.Y.; Gómez Ramos, L.M.; Holguin, S.Y.; Hsiao, C.; Bowman, J.C.; Yang, H.W.; Williams, L.D. Functional RNAs: Combined assembly and packaging in VLPs. Nucleic Acids Res. 2017, 45, 3519–3527. [Google Scholar] [CrossRef] [Green Version]
- Lei, X.; Cai, X.; Yang, Y. Genetic engineering strategies for construction of multivalent chimeric VLPs vaccines. Expert Rev. Vaccines 2020, 19, 235–246. [Google Scholar] [CrossRef] [Green Version]
- Gunter, C.J.; Regnard, G.L.; Rybicki, E.P.; Hitzeroth, I.I. Immunogenicity of plant-produced porcine circovirus-like particles in mice. Plant Biotechnol. J. 2019, 17, 1751–1759. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Makarkov, A.I.; Chierzi, S.; Pillet, S.; Murai, K.K.; Landry, N.; Ward, B.J. Plant-made virus-like particles bearing influenza hemagglutinin (HA) recapitulate early interactions of native influenza virions with human monocytes/macrophages. Vaccine 2017, 35, 4629–4636. [Google Scholar] [CrossRef]
- Lindsay, B.J.; Bonar, M.M.; Costas-Cancelas, I.N.; Hunt, K.; Makarkov, A.I.; Chierzi, S.; Krawczyk, C.M.; Landry, N.; Ward, B.J.; Rouiller, I. Morphological characterization of a plant-made virus-like particle vaccine bearing influenza virus hemagglutinins by electron microscopy. Vaccine 2018, 36, 2147–2154. [Google Scholar] [CrossRef]
- Dennis, S.J.; O’Kennedy, M.M.; Rutkowska, D.; Tsekoa, T.; Lourens, C.W.; Hitzeroth, I.I.; Meyers, A.E.; Rybicki, E.P. Safety and immunogenicity of plant-produced African horse sickness virus-like particles in horses. Vet. Res. 2018, 49, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Malm, M.; Diessner, A.; Tamminen, K.; Liebscher, M.; Vesikari, T.; Blazevic, V. Rotavirus VP6 as an adjuvant for bivalent norovirus vaccine produced in Nicotiana benthamiana. Pharmaceutics 2019, 11, 229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bevan, M. Binary Agrobacterium vectors for plant transformation. Nucleic Acids Res. 1984, 12, 8711–8721. [Google Scholar] [CrossRef] [Green Version]
- Dandekar, A.M.; Fisk, H.J. Plant transformation: Agrobacterium-mediated gene transfer. In Transgenic Plants; Humana Press: Totowana, NJ, USA, 2005; Volume 286, pp. 035–046. [Google Scholar]
- Ganapathi, T.R.; Suprasanna, P.; Rao, P.S.; Bapat, V.A. Tobacco (Nicotiana tabacum L.)—A model system for tissue culture interventions and genetic engineering. Indian J. Biotechnol. 2004, 3, 171–184. [Google Scholar]
- van Eerde, A.; Gottschamel, J.; Bock, R.; Hansen, K.E.A.; Munang’andu, H.M.; Daniell, H.; Liu Clarke, J. Production of tetravalent dengue virus envelope protein domain III-based antigens in lettuce chloroplasts and immunologic analysis for future oral vaccine development. Plant Biotechnol. J. 2019, 17, 1408–1417. [Google Scholar] [CrossRef]
- Lai, H.; He, J.; Engle, M.; Diamond, M.S.; Chen, Q. Robust production of virus-like particles and monoclonal antibodies with geminiviral replicon vectors in lettuce. Plant Biotechnol. J. 2011, 10, 95–104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Monreal-Escalante, E.; Govea-Alonso, D.O.; Hernández, M.; Cervantes, J.; Salazar-González, J.A.; Romero-Maldonado, A.; Rosas, G.; Garate, T.; Fragoso, G.; Sciutto, E.; et al. Towards the development of an oral vaccine against porcine cysticercosis: Expression of the protective HP6/TSOL18 antigen in transgenic carrots cells. Planta 2016, 243, 675–685. [Google Scholar] [CrossRef] [PubMed]
- ZHU, X.Y.; Yu, L.J. The research progress of genetically modified carrots. Hortic. Sci. 2012, 2, 188–190. [Google Scholar]
- Tzfira, T.; Citovsky, V. Agrobacterium-mediated genetic transformation of plants: Biology and biotechnology. Curr. Opin. Biotechnol. 2006, 17, 147–154. [Google Scholar] [CrossRef]
- Tzfira, T.; Li, J.; Lacroix, B.; Citovsky, V. Agrobacterium T-DNA integration: Molecules and models. Trends Genet. 2004, 20, 375–383. [Google Scholar] [CrossRef]
- McCormick, S.; Niedermeyer, J.; Fry, J.; Barnason, A.; Horsch, R.; Fraley, R. Leaf disc transformation of cultivated tomato (L. esculentum) using Agrobacterium tumefaciens. Plant Cell Rep. 1986, 5, 81–84. [Google Scholar] [CrossRef] [PubMed]
- Gallois, P.; Marinho, P. Leaf disk transformation using Agrobacterium tumefaciens-expression of heterologous genes in tobacco. Plant Gene Transf. Expr. Protoc. 1995, 49, 39–48. [Google Scholar] [CrossRef]
- Moore, I.; Samalova, M.; Kurup, S. Transactivated and chemically inducible gene expression in plants. Plant J. 2006, 45, 651–683. [Google Scholar] [CrossRef] [PubMed]
- Borghi, L. Inducible gene expression systems for plants. In Plant Developmental Biology. Methods in Molecular Biology (Methods and Protocols); Hennig, L., Köhler, C., Eds.; Humana Press: Totowa, NJ, USA, 2010; Volume 655, pp. 65–75. [Google Scholar]
- Corrado, G.; Karali, M. Inducible gene expression systems and plant biotechnology. Biotechnol. Adv. 2009, 27, 733–743. [Google Scholar] [CrossRef]
- Dugdale, B.; Mortimer, C.; Kato, M.; James, T.; Harding, R.; Dale, J.L. In Plant Activation: An Inducible, Hyperexpression Platform for Recombinant Protein Production in Plants. Plant Cell 2013, 25, 2429–2443. [Google Scholar] [CrossRef] [Green Version]
- Arevalo-Villalobos, J.I.; Govea-Alonso, D.O.; Bañuelos-Hernández, B.; González-Ortega, O.; Zarazúa, S.; Rosales-Mendoza, S. Inducible expression of antigens in plants: A study focused on peptides related to multiple sclerosis immunotherapy. J. Biotechnol. 2020, 318, 51–56. [Google Scholar] [CrossRef] [PubMed]
- Yusibov, V.; Rabindran, S. Recent progress in the development of plant derived vaccines. Expert Rev. Vaccines 2008, 7, 1173–1183. [Google Scholar] [CrossRef] [PubMed]
- Musiychuk, K.; Stephenson, N.; Bi, H.; Farrance, C.E.; Orozovic, G.; Brodelius, M.; Brodelius, P.; Horsey, A.; Ugulava, N.; Shamloul, A.; et al. A launch vector for the production of vaccine antigens in plants. Influenza Other Respir. Viruses 2007, 1, 19–25. [Google Scholar] [CrossRef]
- Yusibov, V.; Streatfield, S.J.; Kushnir, N.; Roy, G.; Padmanaban, A. Hybrid viral vectors for vaccine and anti-body production in plants. Curr. Pharm. Des. 2013, 19, 5574–5586. [Google Scholar] [CrossRef] [PubMed]
- Massa, S.; Presenti, O.; Benvenuto, E. Engineering plants for the future: Farming with value-added harvest. Prog. Bot. 2018, 80, 65–108. [Google Scholar] [CrossRef]
- Gleba, Y.; Klimyuk, V.; Marillonnet, S. Magnifection—A new platform for expressing recombinant vaccines in plants. Vaccine 2005, 23, 2042–2048. [Google Scholar] [CrossRef] [PubMed]
- Marillonnet, S.; Thoeringer, C.; Kandzia, R.; Klimyuk, V.; Gleba, Y. Systemic Agrobacterium tumefaciens-mediated transfection of viral replicons for efficient transient expression in plants. Nat. Biotechnol. 2005, 23, 718–723. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.-H.; Hu, C.-C.; Liao, J.-T.; Lee, Y.-L.; Huang, Y.-W.; Lin, N.-S.; Lin, Y.-L.; Hsu, Y.-H. Production of Japanese Encephalitis virus antigens in plants using bamboo mosaic virus-based vector. Front. Microbiol. 2017, 8, 788. [Google Scholar] [CrossRef]
- Stanley, J. Geminiviruses: Plant viral vectors. Curr. Opin. Genet. Dev. 1993, 3, 91–96. [Google Scholar] [CrossRef]
- Regnard, G.L.; Halley-Stott, R.P.; Tanzer, F.L.; Hitzeroth, I.I.; Rybicki, E.P. High level protein expression in plants through the use of a novel autonomously replicating geminivirus shuttle vector. Plant Biotechnol. J. 2010, 8, 38–46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, Q.; He, J.; Phoolcharoen, W.; Mason, H.S. Geminiviral vectors based on bean yellow dwarf virus for production of vaccine antigens and monoclonal antibodies in plants. Hum. Vaccines 2011, 7, 331–338. [Google Scholar] [CrossRef] [Green Version]
- Rybicki, E.P.; Martin, D.P. Virus-derived ssDNA vectors for the expression of foreign proteins in plants. Curr. Top. Microbiol. Immunol. 2011, 375, 19–45. [Google Scholar] [CrossRef]
- Huang, Z.; Phoolcharoen, W.; Lai, H.; Piensook, K.; Cardineau, G.; Zeitlin, L.; Whaley, K.J.; Arntzen, C.J.; Mason, H.S.; Chen, Q. High-level rapid production of full-size monoclonal antibodies in plants by a single-vector DNA replicon system. Biotechnol. Bioeng. 2010, 106, 9–17. [Google Scholar] [CrossRef] [Green Version]
- Fischer, N.; Stampacchia, O.; Redding, K.; Rochaix, J.D. Selectable marker recycling in the chloroplast. Mol. Gen. Genom. 1996, 251, 373–380. [Google Scholar] [CrossRef]
- Ye, G.-N.; Daniell, H.; Sanford, J.C. Optimization of delivery of foreign DNA into higher-plant chloroplasts. Plant Mol. Biol. 1990, 15, 809–819. [Google Scholar] [CrossRef]
- Sanford, J.C. The biolistic process. Trends Biotechnol. 1988, 6, 299–302. [Google Scholar] [CrossRef]
- Verma, D.; Daniell, H. Chloroplast vector systems for biotechnology applications. Plant Physiol. 2007, 145, 1129–1143. [Google Scholar] [CrossRef] [Green Version]
- Ruf, S.; Hermann, M.; Berger, I.J.; Carrer, H.; Bock, R. Stable genetic transformation of tomato plastids and expression of a foreign protein in fruit. Nat. Biotechnol. 2001, 19, 870–875. [Google Scholar] [CrossRef] [PubMed]
- Haq, T.A.; Mason, H.S.; Clements, J.D.; Arntzen, C.J. Oral immunization with a recombinant bacterial anti-gen produced in transgenic plants. Science 1995, 268, 714–716. [Google Scholar] [CrossRef] [PubMed]
- Mason, H.S.; Haq, T.A.; Clements, J.D.; Arntzen, C.J. Edible vaccine protects mice against Escherichia coli heat-labile enterotoxin (LT): Potatoes expressing a synthetic LT-B gene. Vaccine 1998, 16, 1336–1343. [Google Scholar] [CrossRef]
- Bock, R. Genetic engineering of the chloroplast: Novel tools and new applications. Curr. Opin. Biotechnol. 2014, 26, 7–13. [Google Scholar] [CrossRef]
- Takeyama, N.; Kiyono, H.; Yuki, Y. Plant-based vaccines for animals and humans: Recent advances in technology and clinical trials. Ther. Adv. Vaccines 2015, 3, 139–154. [Google Scholar] [CrossRef]
- Ward, B.J.; Landry, N.; Trépanier, S.; Mercier, G.; Dargis, M.; Couture, M.; D’Aoust, M.-A.; Vézina, L.-P. Human antibody response to N-glycans present on plant-made influenza virus-like particle (VLP) vaccines. Vaccine 2014, 32, 6098–6106. [Google Scholar] [CrossRef]
- Kapusta, J.; Modelska, A.; Figlerowicz, M.; Pniewski, T.; Letellier, M.; Lisowa, O.; Yusibov, V.; Koprowski, H.; Plucienniczak, A.; Legocki, A.B. A plant-derived edible vaccine against hepatitis B virus. FASEB J. 1999, 13, 1796–1799. [Google Scholar] [CrossRef]
- Cramer, C.L.; Boothe, J.G.; Oishi, K.K. Transgenic plants for therapeutic proteins: Linking upstream and downstream strategies. In Current Topics Microbiology and Immunology, Plant Biotechnology: New Products and Applications; Hammond, J., McGarvey, P., Yusibov, V., Eds.; Springer: Berlin, Germany, 1999; pp. 95–118. [Google Scholar]
- Jilka, J. Have your vaccine and eat it too. In Global Agbiotech Progress Proceedings of the AgBiotech World Forum ’99, Global AG BioTech Progress; Drug and Market Development Publications: Westborough, MA, USA, 1999; pp. 89–95. [Google Scholar]
- Qian, B.; Shen, H.; Liang, W.; Guo, X.; Zhang, C.; Wang, Y.; Li, G.; Wu, A.; Cao, K.; Zhang, D. Immunogenicity of recombinant hepatitis B virus surface antigen fused with preS1 epitopes expressed in rice seeds. Transgenic Res. 2008, 17, 621–631. [Google Scholar] [CrossRef] [PubMed]
- Tacket, C.O.; Mason, H.S.; Losonsky, G.; Clements, J.D.; Levine, M.M.; Arntzen, C.J. Immunogenicity in humans of a recombinant bacterial-antigen delivered in transgenic potato. Nat. Med. 1998, 4, 607–609. [Google Scholar] [CrossRef]
- Tacket, C.O.; Mason, H.S.; Losonsky, G.; Estes, M.K.; Levine, M.M.; Arntzen, C.J. Human immune responses to a novel Norwalk virus vaccine delivered in transgenic potatoes. J. Infect. Dis. 2000, 182, 302–305. [Google Scholar] [CrossRef]
- Tacket, C.O.; Pasetti, M.F.; Edelman, R.; Howard, J.A.; Streatfield, S. Immunogenicity of recombinant LT-B delivered orally to humans in transgenic corn. Vaccine 2004, 22, 4385–4389. [Google Scholar] [CrossRef]
- Twyman, R.M.; Stoeger, E.; Schillberg, S.; Christou, P.; Fischer, R. Molecular farming in plants: Host systems and expression technology. Trends Biotechnol. 2003, 21, 570–578. [Google Scholar] [CrossRef]
- Murphy, D.J. Improving containment strategies in biopharming. Plant Biotechnol. J. 2007, 5, 555–569. [Google Scholar] [CrossRef]
- Rosales-Mendoza, S.; Salazar-González, A.J. Immunological aspects of using plant cells as delivery vehicles for oral vaccines. Expert Rev. Vaccines 2014, 13, 737–749. [Google Scholar] [CrossRef]
- Daniell, H.; Kulis, M.; Herzog, R.W. Plant cell-made protein antigens for induction of Oral tolerance. Biotechnol. Adv. 2019, 37, 107413. [Google Scholar] [CrossRef] [PubMed]
- Kwon, K.-C.; Daniell, H. Low-cost oral delivery of protein drugs bioencapsulated in plant cells. Plant Biotechnol. J. 2015, 13, 1017–1022. [Google Scholar] [CrossRef] [PubMed]
- Ward, B.J.; Séguin, A.; Couillard, J.; Trépanier, S.; Landry, N. Phase III: Randomized observer-blind trial to evaluate lot-to-lot consistency of a new plant-derived quadrivalent virus like particle influenza vaccine in adults 18–49 years of age. Vaccine 2021, 39, 1528–1533. [Google Scholar]
- Gobeil, P.; Pillet, S.; Boulay, I.; Séguin, A.; Makarkov, A.; Heizer, G.; Bhutada, K.; Mahmood, A.; Charland, N.; Trépanier, S.; et al. Phase 2 randomized trial of an AS03 adjuvanted plant-based virus-like particle vaccine for COVID-19 in healthy adults, older adults and adults with comorbidities. medRxiv 2021. Available online: https://www.medrxiv.org/content/10.1101/2021.05.14.21257248v2.full.pdf (accessed on 4 January 2022).
- Available online: https://medicago.com/en/press-release/medicago-and-gsk-announce-positive-phase-3-efficacy-and-safety-results-for-adjuvanted-plant-based-covid-19-vaccine-candidate/ (accessed on 4 January 2022).
- Ward, B.J.; Gobeil, P.; Séguin, A.; Atkins, J.; Boulay, I.; Charbonneau, P.-Y.; Couture, M.; D’Aoust, M.-A.; Dhaliwall, J.; Finkle, C.; et al. Phase 1 randomized trial of a plant-derived virus-like particle vaccine for COVID-19. Nat. Med. 2021, 27, 1071–1078. [Google Scholar] [CrossRef]
- Kumar, A.U.; Kadiresen, K.; Gan, W.C.; Ling, A.P.K. Current updates and research on plant-based vaccines for coronavirus disease 2019. Clin. Exp. Vaccine Res. 2021, 10, 13–23. [Google Scholar] [CrossRef] [PubMed]
- Shaaltiel, Y.; Gingis-Velitski, S.; Tzaban, S.; Fiks, N.; Tekoah, Y.; Aviezer, D. Plant-based oral delivery of β-glucocerebrosidase as an enzyme replacement therapy for Gaucher’s disease. Plant Biotechnol. J. 2015, 13, 1033–1040. [Google Scholar] [CrossRef] [PubMed]
- Laere, E.; Ling, A.P.K.; Wong, Y.P.; Koh, R.Y.; Lila, M.A.M.; Hussein, S. Plant-based vaccines: Production and challenges. J. Bot. 2016, 2016, 4928637. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).