Looking Back at the Early Stages of Redox Biology
Abstract
1. Introduction
2. The Hydrogen Peroxide/Heme Period
3. Selenium Conquering the Stage
4. Non-Se Glutathione Peroxidases, Peroxiredoxins and Other Super-Reactive Cysteine Residues
4.1. Cysteine-Containing Homologues of GPx
4.2. Peroxiredoxins
4.3. Other Proteins with CP-Like Reactivity
5. The Biological Radicals
5.1. The Superoxide Radical
5.2. The Nitrogen Monoxide Radical
- •NO itself is a benign radical. Its biological effects are overwhelmingly beneficial. Its radical character, however, implies that it can react with a large variety of molecules and these down-stream processes may cause adverse effects. Fortunately, the history of nitrogen oxides can be traced back to Joseph Priestley (1733–1804), and a lot of the chemistry of •NO had been worked out before its presence in biological systems was detected [268]. The chemistry of the interaction of •NO with oxygen, thiols and other molecules is, however, very complex, and the relevance to biological systems still appears to be debated. Like •O2–, •NO can act as a reductant and as an oxidant.
- A prominent characteristic of •NO is its affinity to metal complexes. It is the basis of its physiological function as activator of guanylyl cyclase, but also of adverse effects resulting from binding to cytochrome P450 in the endoplasmic reticulum or to the cytochromes of the respiratory chain. The interaction of •NO with b-type cytochromes in complex III appeared to mimick antimycin A in triggering superoxide production (see above), which implies the formation of peroxynitrite (ONOO−) due to the simultaneous presence of •NO and •O2– and, in consequence, mitochondrial dysfunction [269].
- Nitrosothiol in proteins or low molecular compounds such as GSH is commonly considered as a hallmark of “nitrosative stress”. Of course, these derivatives could be formed by a reaction of •NO with thiyl radicals, yet the steady state concentration of thiyl radicals is too low to be of physiological relevance. Most likely, S-nitrosation is achieved by N2O3, the latter being built from •NO and •NO2, with a rate constant of 1.1 × 109 M−1 s−1 [268]. However, also other mechanisms are being discussed [270].
- In the context of lipid peroxidation, •NO can adopt controversial roles. Being a radical, it can terminate free radical chains, e.g., by interacting with an ROO• [273]. Its oxidation products, however, may also initiate a free radical chain by hydrogen abstraction from a poly-unsaturated fatty acid residue [272].
- The most important pathogenic reaction of •NO is probably its combination with •O2− to form peroxynitrite. This reaction of two radicals proceeds with a rate constant of 1.9 × 1010 M−1 s−1, which implies that it is limited by diffusion [270,274]. Peroxynitrite, although it is not a radical, is a highly aggressive oxidant, which prompted Beckmann and Koppenol to describe this reaction as one of the “good” (•NO) with the “bad” (•O2−) to make the “ugly” (peroxynitrite) [275].
- •O2−, by reacting with •NO to peroxynitrite, inhibits the beneficial effects of •NO, e.g., on the circulation [279,280], and simultaneously causes oxidative damage. In retrospect, therefore, the surprising results seen with SOD infusion in models of reperfusion injury and septicemia [246] may be re-interpreted as resulting from •NO salvage and inhibition of the formation of peroxynitrite.
6. Changing Paradigms: From Tissue Damage to Redox Regulation
7. Now the Language Problem
8. Conclusions
Funding
Acknowledgments
Conflicts of Interest
References
- Thénard, L.J. Observations sur les combinations nouvelle entre l’oxygen et divers acides. Ann. Chim. Phys. 1818, 8, 306–312. [Google Scholar]
- Schönbein, C.F. Ueber die katalytische Wirksamkeit organischer Materien und deren Verbreitung in der Pflanzen-und Thierwelt. J. Prakt. Chem. 1863, 98, 323–344. [Google Scholar] [CrossRef]
- Loew, O. A new enzyme of general occurrence in organisms. Science 1900, 11, 701–702. [Google Scholar] [CrossRef] [PubMed]
- Warburg, O. Iron, the oxygen-carrier of respiration-ferment. Science 1925, 61, 575–582. [Google Scholar] [CrossRef] [PubMed]
- Keilin, D. The History of Cell Respiration and Cytochome; Cambridge University Press: Cambridge, UK, 1966. [Google Scholar]
- Zamocky, M.; Koller, F. Understanding the structure and function of catalases: Clues from molecular evolution and in vitro mutagenesis. Prog. Biophys. Mol. Biol. 1999, 72, 19–66. [Google Scholar] [CrossRef]
- Zeile, K. Über die aktive Gruppe der Katalase. II. Hoppe Seyler Z. Physiol. Chem. 1931, 195, 39–48. [Google Scholar] [CrossRef]
- Zeile, K.; Hellström, H. Über die aktive Gruppe der Leberkatalase. Hoppe Seyler Z. Physiol. Chem. 1930, 192, 171–192. [Google Scholar] [CrossRef]
- Sumner, J.B.; Dounce, A.L. Crystalline catalase. Science 1937, 85, 366–367. [Google Scholar] [CrossRef]
- Stern, K.G. Structure and action-mechanism of hematin-containing enzymes. Yale J. Biol. Med. 1937, 10, 161–178. [Google Scholar]
- Stern, K.G. Constitution of the prosthetic group of catalase. Nature 1935, 136, 302. [Google Scholar] [CrossRef]
- Stern, K.G. Spectroscopy of catalase. J. Gen. Physiol. 1937, 20, 631–648. [Google Scholar] [CrossRef] [PubMed]
- Chance, B. The primary and secondary compounds of catalase and methy or ethyl hydroperoxide; kinetics and activity. J. Biol. Chem. 1949, 179, 1341–1369. [Google Scholar] [PubMed]
- Schonbaum, G.R.; Chance, B. Catalase. In The Enzymes; Boyer, P.D., Ed.; Acad. Press: New York, NY, USA, 1976; Volume 13, pp. 363–408. [Google Scholar]
- Theorell, H.; Ehrenberg, A.; Chance, B. Electronic structure of the peroxidase-peroxide complexes. Arch. Biochem. Biophys. 1952, 37, 237–239. [Google Scholar] [CrossRef]
- Chance, B. An intermediate compound in the catalse-hydrogenperoxide reaction. Acta Chem. Scand. 1947, 1, 236–267. [Google Scholar] [CrossRef]
- Vidossich, P.; Alfonso-Prietro, M.; Carpena, X.; Fita, I.; Loewen, P.C.; Rovira, C. The dynamic role of distal side residues in heme hydroperoxidase catalysis. Interplay between x-ray crystallography and ab initio md simulations. Arch. Biochem. Biophys. 2010, 500, 37–44. [Google Scholar]
- Chance, B.; Sies, H.; Boveris, A. Hydroperoxide metabolism in mammalian organs. Physiol. Rev. 1979, 59, 527–605. [Google Scholar] [CrossRef]
- Chance, B. The state of catalase in the respiring bacterial cell. Science 1952, 116, 202–203. [Google Scholar] [CrossRef]
- Baudhuin, P.; Mueller, M.; Poole, B.; Deduve, C. Non-mitochondrial oxidizing particles (microbodies) in rat liver and kidney and in tetrahymena pyriformis. Biochem. Biophys. Res. Commun. 1965, 20, 53–59. [Google Scholar] [CrossRef]
- De Duve, C. Exploring cells with a centrifuge. Nobel Lect. Physiol. Med. 1974, 152–170. Available online: https://www.nobelprize.org/prizes/medicine/1974/duve/facts/ (accessed on 1 December 2020).
- Sies, H.; Chance, B. The steady state level of catalase compound I in isolated hemoglobin-free perfused rat liver. FEBS Lett. 1970, 11, 172–176. [Google Scholar] [CrossRef]
- Andreae, W.A. A sensitive method for the estimation of hydrogen peroxide in biological materials. Nature 1955, 175, 859–860. [Google Scholar] [CrossRef] [PubMed]
- Loschen, G.; Flohé, L.; Chance, B. Respiratory chain linked H2O2 production in pigeon heart mitochondria. FEBS Lett. 1971, 18, 261–264. [Google Scholar] [CrossRef]
- Boveris, A.; Oshino, N.; Chance, B. The cellular production of hydrogen peroxide. Biochem. J. 1972, 128, 617–630. [Google Scholar] [CrossRef] [PubMed]
- Pandey, V.P.; Awasthi, M.; Singh, S.; Tiwari, S.; Dwivedi, U.N. A comprehensive review on function and application of plant peroxidases. Biochem. Anal. Biochem. 2017, 6, 1–16. [Google Scholar] [CrossRef]
- Kim, M.J.; Ciani, S.; Schachtman, D.P. A peroxidase contributes to ROS production during arabidopsis roote response to potassium deficiency. Mol. Plant 2010, 3, 420–427. [Google Scholar] [CrossRef]
- Lehtonen, M.T.; Akita, M.; Frank, W.; Reski, R.; Valkonen, J.P. Involvement of a class III peroxidase and the mitochondrial protein TSPO in oxidative burst upon treatment of moss plants with a fungal elicitor. Mol. Plant Microbe Interact. 2012, 25, 363–371. [Google Scholar] [CrossRef]
- Juttawuttipoka, T.; Buranajitpakorn, S.; Vattanaviboon, P.; Mongkolsuk, S. The catalase-peroxidase KatG is required for virulence of Xanthomonas campestris pv. campestris in a host plant by providing protection against low level of H2O2. J. Bacteriol. 2009, 191, 7372–7377. [Google Scholar] [CrossRef]
- Anjum, N.A.; Sharma, P.; Gill, S.S.; Hasanuzzaman, M.; Khan, E.A.; Kachhap, K.; Mohamed, A.A.; Thangavel, P.; Devi, G.D.; Vasudhevan, P.; et al. Catalase and ascorbate peroxidase-representative H2O2-detoxifying heme enzymes in plants. Environ. Sci. Pollut. Res. Int. 2016, 23, 19002–19029. [Google Scholar] [CrossRef]
- Boveris, A.; Sies, H.; Martino, E.E.; Docampo, R.; Turrens, J.F.; Stoppani, A.O. Deficient metabolic utilization of hydrogen peroxide in Trypanosoma cruzi. Biochem. J. 1980, 188, 643–648. [Google Scholar] [CrossRef]
- Zhang, Z.; Zhang, Q.; Wu, J.; Zheng, X.; Zheng, S.; Sun, X.; Qiu, Q.; Lu, T. Gene knockout study reveals that cytosolic ascorbate peroxidase 2(OsAPX2) plays a critical role in growth and reproduction in rice under drought, salt and cold stresses. PLoS ONE 2013, 8, e57472. [Google Scholar] [CrossRef]
- Shigeto, J.; Tsutsumi, Y. Diverse functions and reactions of class III peroxidases. New Phytol. 2016, 209, 1395–1402. [Google Scholar] [CrossRef] [PubMed]
- Zamocky, M.; Gasselhuber, B.; Furtmuller, P.G.; Obinger, C. Molecular evolution of hydrogen peroxide degrading enzymes. Arch. Biochem. Biophys. 2012, 525, 131–144. [Google Scholar] [CrossRef] [PubMed]
- Veitch, N.C. Horseradish peroxidase: A modern view of a classic enzyme. Phytochemistry 2004, 65, 249–259. [Google Scholar] [CrossRef]
- Brill, A.S. Peroxidases and catalase. In Comprehensive Biochemistry; Florkin, M., Stotz, E.H., Eds.; Elsevier: Amsterdam, The Netherlands, 1966; Volume 14, pp. 447–479. [Google Scholar]
- Yonetani, T. Cytochrome c peroxidase. In The Enzymes, 3rd ed.; Boyer, P.D., Ed.; Academic Press: New York, NY, USA, 1976; pp. 345–361. [Google Scholar]
- Grasso, R. Acción de la tiourea y de las sulfonamidas sobre las peroxidasas de la glándula tiroides. Arch. Soc. Biol. Montev. 1945, 12, 173–185. [Google Scholar] [PubMed]
- Kootstra, P.R.; Wever, R.; De Vijlder, J.J. Thyroid peroxidase: Kinetics, pH optima and substrate dependency. Acta Endocrinol. 1993, 129, 328–331. [Google Scholar] [CrossRef]
- Heyland, A.; Price, D.A.; Bodnarova-Buganova, M.; Moroz, L.L. Thyroid hormone metabolism and peroxidase function in two non-chordate animals. J. Exp. Zool. Part B Mol. Dev. Evol. 2006, 306, 551–566. [Google Scholar] [CrossRef] [PubMed]
- Hosoya, T.; Morrison, M. The peroxidase and other hemoproteins of thyroid microsomes. Biochem. Biophys. Res. Commun. 1965, 20, 27–32. [Google Scholar]
- Zhang, X.Y.; Elfarra, A.A. Potential roles of myeloperoxidase and hypochlorous acid in metabolism and toxicity of alkene hydrocarbons and drug molecules containing olefinic moieties. Expert Opin. Drug Metab. Toxicol. 2017, 13, 513–524. [Google Scholar] [CrossRef]
- Winterbourn, C.C.; Kettle, A.J. Reactions of superoxide with myeloperoxidase and its products. Jpn. J. Infect. Dis. 2004, 57, S31–S33. [Google Scholar]
- Winterbourn, C.C.; Kettle, A.J.; Hampton, M.B. Reactive oxygen species and neutrophil function. Annu. Rev. Biochem. 2016, 85, 765–792. [Google Scholar] [CrossRef]
- Gorman, A.A. Singlet oxygen: Current mechanistic aspects of photo-oxidation. In Oxygen Radicals in Biology and Medicine; Simic, M.G., Taylor, K.A., Ward, J.F., Von Sonntag, C., Eds.; Plenum Press: New York, NY, USA; London, UK, 1988; Volume 49, pp. 101–104. [Google Scholar]
- Pollock, J.S.; Nakane, M.; Förstermann, U.; Murad, F. Particulate and soluble bovine endothelial nitric oxide synthases are structurally similar proteins yet different from soluble brain nitric oxide synthase. J. Cardiovasc. Pharmacol. 1992, 20, S50–S53. [Google Scholar] [CrossRef] [PubMed]
- Reiter, B. The lactoperoxidase-thiocyanate-hydrogen peroxide antibacterium system. Ciba Found. Symp. 1979, 65, 285–294. [Google Scholar] [CrossRef]
- Agner, K. Verdoperoxidase. A ferment isolated from leukocytes. Acta Chem. Scand. 1941, 2, 1–68. [Google Scholar]
- Klebanoff, S.J.; Rosen, H. The role of myeloperoxidase in the microbicidal activity of polymorphonuclear leukocytes. Ciba Found. Symp. 1979, 65, 263–284. [Google Scholar] [CrossRef]
- Klebanoff, S.J. Myeloperoxidase: Friend and foe. J. Leukoc. Biol. 2005, 77, 598–625. [Google Scholar] [CrossRef]
- Ndrepepa, G. Myeloperoxidase—A bridge linking inflammation and oxidative stress with cardiovascular disease. Clin. Chim. Acta Int. J. Clin. Chem. 2019, 493, 36–51. [Google Scholar] [CrossRef]
- Palladino, E.N.D.; Hartman, C.L.; Albert, C.J.; Ford, D.A. The chlorinated lipidome originating from myeloperoxidase-derived HOCl targeting plasmalogens: Metabolism, clearance, and biological properties. Arch. Biochem. Biophys. 2018, 641, 31–38. [Google Scholar] [CrossRef]
- Panasenko, O.M.; Torkhovskaya, T.I.; Gorudko, I.V.; Sokolov, A.V. The role of halogenative stress in atherogenic modification of low-density lipoproteins. Biochem. Biokhimiia 2020, 85, S34–S55. [Google Scholar] [CrossRef]
- Vanhamme, L.; Zouaoui Boudjeltia, K.; Van Antwerpen, P.; Delporte, C. The other myeloperoxidase: Emerging functions. Arch. Biochem. Biophys. 2018, 649, 1–14. [Google Scholar] [CrossRef]
- Strzepa, A.; Pritchard, K.A.; Dittel, B.N. Myeloperoxidase: A new player in autoimmunity. Cell. Immunol. 2017, 317, 1–8. [Google Scholar] [CrossRef]
- Bonaventura, A.; Liberale, L.; Carbone, F.; Vecchie, A.; Diaz-Canestro, C.; Camici, G.G.; Montecucco, F.; Dallegri, F. The pathophysiological role of neutrophile extracellular traps in inflammatory diseases. Thromb. Haemost. 2018, 118, 6–27. [Google Scholar] [PubMed]
- Chami, B.; Martin, N.J.J.; Dennis, J.M.; Witting, P.K. Myeloperoxidase in the inflamed colon: A novel target for treating inflammatory bowel disease. Arch. Biochem. Biophys. 2018, 645, 61–71. [Google Scholar] [CrossRef] [PubMed]
- Izuhara, K.; Suzuki, S.; Ogawa, M.; Nunomura, S.; Nanri, Y.; Mitamura, Y.; Yoshihara, T. The significance of hypothiocyanite production via the pendrin/duox/peroxidase pathway in the pathogenesis of Asthma. Oxid. Med. Cell. Longev. 2017, 1–7. [Google Scholar] [CrossRef]
- Berzelius, J.J. Ein neues mineralisches Alkali und ein neues Metall. J. Für Chem. Und Phys. 1817, 21, 342–344. [Google Scholar]
- Klayman, D.L.; Günther, W.H.H. Organic Selenium Compounds: Their Chemistry and Biology; Wiley: New York, NY, USA, 1973. [Google Scholar]
- Flohé, L. The labour pains of biochemical selenology: The history of selenoprotein biosynthesis. Biochim. Biophys. Acta 2009, 1790, 1389–1403. [Google Scholar] [CrossRef] [PubMed]
- Pinsent, J. The need for selenite and molybdate in the formation of formic dehydrogenase by members of the coli-aerogenes group of bacteria. Biochem. J. 1954, 57, 10–16. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, K. Factor 3, selenium and vitamin e. Nutr. Rev. 1960, 18, 193–197. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, K.; Foltz, C.M. Selenium as an integral part of factor 3 against dietary necrotic liver degeneration. J. Proc. Am. Chem. Soc. 1957, 79, 3292–3293. [Google Scholar] [CrossRef]
- Rotruck, J.T.; Hoekstra, W.G.; Pope, A.L.; Ganther, H.E.; Swanson, A.; Hafemann, D. Relationship of selenium to GSH peroxidase. Fed. Proc. 1972, 31, 691. [Google Scholar]
- Flohé, L.; Günzler, W.A.; Schock, H.H. Glutathione peroxidase: A selenoenzyme. FEBS Lett. 1973, 32, 132–134. [Google Scholar] [CrossRef]
- Flohé, L.; Loschen, G.; Günzler, W.A.; Eichele, E. Glutathione peroxidase, V. The kinetic mechanism. Hoppe Seylers Z. Physiol. Chem. 1972, 353, 987–999. [Google Scholar] [CrossRef]
- Mills, G.C. Hemoglobin catabolism. I. Glutathione peroxidase, an erythrocyte enzyme which protects hemoglobin from oxidative breakdown. J. Biol. Chem. 1957, 229, 189–197. [Google Scholar]
- Wendel, A.; Kerner, B.; Graupe, k. The selenium moiety of glutathione peroxidase. In Functions of Glutathione in Liver and Kidney; Siess, H., Wendel, A., Eds.; Springer: Heidelberg, Germany, 1978; pp. 107–113. [Google Scholar]
- Forstrom, J.W.; Zakowski, J.J.; Tappel, A.L. Identification of the catalytic site of rat liver glutathione peroxidase as selenocysteine. Biochemistry 1978, 17, 2639–2644. [Google Scholar] [CrossRef]
- Flohé, L.; Eisele, B.; Wendel, A. Glutathion peroxidase. I. Isolation and determinations of molecular weight. Hoppe Seylers Z. Physiol. Chem. 1971, 352, 151–158. [Google Scholar] [CrossRef] [PubMed]
- Sies, H.; Gerstenecker, C.; Summer, K.H.; Menzel, H.; Flohé, L. Glutathione-dependent hydroperoxide metabolism and associated transitions in hemoglobin-free perfused rat liver. In Glutathione; Flohé, L., Benöhr, H.C., Sies, H.W., Waller, H.D., Wendel, A., Eds.; Thieme: Stuttgart, Germany, 1974; pp. 261–276. [Google Scholar]
- Sies, H.; Gerstenecker, C.; Menzel, H.; Flohé, L. Oxidation in the NADP system and release of GSSG from hemoglobin-free perfused rat liver during peroxidatic oxidation of glutathione by hydroperoxides. FEBS Lett. 1972, 27, 171–175. [Google Scholar] [CrossRef]
- Flohé, L. Helmut Sies and the compartmentation of hydroperoxide metabolism. Arch. Biochem. Biophys. 2016, 595, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Ursini, F.; Maiorino, M.; Gregolin, C. The selenoenzyme phospholipid hydroperoxide glutathione peroxidase. Biochim. Biophys. Acta 1985, 839, 62–70. [Google Scholar] [CrossRef]
- Brigelius-Flohé, R.; Aumann, K.D.; Blöcker, H.; Gross, G.; Kiess, M.; Klöppel, K.D.; Maiorino, M.; Roveri, A.; Schuckelt, R.; Ursini, F.; et al. Phospholipid-hydroperoxide glutathione peroxidase. Genomic DNA, cDNA, and deduced amino acid sequence. J. Biol. Chem. 1994, 269, 7342–7348. [Google Scholar]
- Günzler, W.A.; Steffens, G.J.; Grossmann, A.; Kim, S.M.; Ötting, F.; Wendel, A.; Flohé, L. The amino-acid sequence of bovine glutathione peroxidase. Hoppe Seylers Z. Physiol. Chem. 1984, 365, 195–212. [Google Scholar] [CrossRef]
- Günzler, W.A.; Vergin, H.; Müller, I.; Flohé, L. glutathione peroxidase VI: The reaction of glutahione peroxidase with various hydroperoxides. Hoppe Seylers Z. Physiol. Chem. 1972, 353, 1001–1004. [Google Scholar]
- Cozza, G.; Rossetto, M.; Bosello-Travain, V.; Maiorino, M.; Roveri, A.; Toppo, S.; Zaccarin, M.; Zennaro, L.; Ursini, F. Glutathione peroxidase 4-catalyzed reduction of lipid hydroperoxides in membranes: The polar head of membrane phospholipids binds the enzyme and addresses the fatty acid hydroperoxide group toward the redox center. Free Radic. Biol. Med. 2017, 112, 1–11. [Google Scholar] [CrossRef]
- Ursini, F.; Maiorino, M.; Valente, M.; Ferri, L.; Gregolin, C. Purification from pig liver of a protein which protects liposomes and biomembranes from peroxidative degradation and exhibits glutathione peroxidase activity on phosphatidylcholine hydroperoxides. Biochim. Biophys. Acta 1982, 710, 197–211. [Google Scholar] [CrossRef]
- Maiorino, M.; Roveri, A.; Ursini, F. Gpx4. From prevention of lipid peroxidation to spermatogenesis and back. In Glutathione; Flohé, L., Ed.; CRC Press: Boca Raton, FL, USA, 2019; pp. 111–127. [Google Scholar]
- Ursini, F.; Heim, S.; Kiess, M.; Maiorino, M.; Roveri, A.; Wissing, J.; Flohé, L. Dual function of the selenoprotein PHGPx during sperm maturation. Science 1999, 285, 1393–1396. [Google Scholar] [CrossRef] [PubMed]
- Conrad, M.; Moreno, S.G.; Sinowatz, F.; Ursini, F.; Kolle, S.; Roveri, A.; Brielmeier, M.; Wurst, W.; Maiorino, M.; Bornkamm, G.W. The nuclear form of phospholipid hydroperoxide glutathione peroxidase is a protein thiol peroxidase contributing to sperm chromatin stability. Mol. Cell. Biol. 2005, 25, 7637–7644. [Google Scholar] [CrossRef] [PubMed]
- Godeas, C.; Tramer, F.; Micali, F.; Roveri, A.; Maiorino, M.; Nisii, C.; Sandri, G.; Panfili, E. Phospholipid hydroperoxide glutathione peroxidase (PHGPx) in rat testis nuclei is bound to chromatin. Biochem. Mol. Med. 1996, 59, 118–124. [Google Scholar] [CrossRef]
- Godeas, C.; Tramer, F.; Micali, F.; Soranzo, M.; Sandri, G.; Panfili, E. Distribution and possible novel role of phospholipid hydroperoxide glutathione peroxidase in rat epididymal spermatozoa. Biol. Reprod. 1997, 57, 1502–1508. [Google Scholar] [CrossRef][Green Version]
- Schnurr, K.; Belkner, J.; Ursini, F.; Schewe, T.; Kühn, H. The selenoenzyme phospholipid hydroperoxide glutathione peroxidase controls the activity of the 15-lipoxygenase with complex substrates and preserves the specificity of the oxygenation products. J. Biol. Chem. 1996, 271, 4653–4658. [Google Scholar]
- Sies, H.; Sharov, V.S.; Klotz, L.O.; Briviba, K. Glutathione peroxidase protects against peroxynitrite-mediated oxidations. A new function for selenoproteins as peroxynitrite reductase. J. Biol. Chem. 1997, 272, 27812–27817. [Google Scholar] [CrossRef]
- Briviba, K.; Kissner, R.; Koppenol, W.H.; Sies, H. Kinetic study of the reaction of glutathione peroxidase with peroxynitrite. Chem. Res. Toxicol. 1998, 11, 1398–1401. [Google Scholar] [CrossRef]
- Lei, X.G.; Zhu, J.H.; Cheng, W.H.; Bao, Y.; Ho, Y.S.; Reddi, A.R.; Holmgren, A.; Arner, E.S. Paradoxical roles of antioxidant enzymes: Basic mechanisms and health implications. Physiol. Rev. 2016, 96, 307–364. [Google Scholar] [CrossRef]
- Imai, H.; Hirao, F.; Sakamoto, T.; Sekine, K.; Mizukura, Y.; Saito, M.; Kitamoto, T.; Hayasaka, M.; Hanaoka, K.; Nakagawa, Y. Early embryonic lethality caused by targeted disruption of the mouse phgpx gene. Biochem. Biophys. Res. Commun. 2003, 305, 278–286. [Google Scholar] [CrossRef]
- Yang, W.S.; Stockwell, B.R. Synthetic lethal screening identifies compounds activating iron-dependent, nonapoptotic cell death in oncogenic-ras-harboring cancer cells. Chem. Biol. 2008, 15, 234–245. [Google Scholar] [CrossRef] [PubMed]
- Vuckovic, A.M.; Bosello Travain, V.; Bordin, L.; Cozza, G.; Miotto, G.; Rossetto, M.; Toppo, S.; Venerando, R.; Zaccarin, M.; Maiorino, M.; et al. Inactivation of the glutathione peroxidase GPx4 by the ferroptosis-inducing molecule rsl3 requires the adaptor protein 14-3-3 epsilon. FEBS Lett. 2020, 594, 611–624. [Google Scholar] [CrossRef] [PubMed]
- Galluzzi, L.; Bravo-San Pedro, J.M.; Vitale, I.; Aaronson, S.A.; Abrams, J.M.; Adam, D.; Alnemri, E.S.; Altucci, L.; Andrews, D.; Annicchiarico-Petruzzelli, M.; et al. Essential versus accessory aspects of cell death: Recommendations of the NCCD 2015. Cell Death Differ. 2015, 22, 58–73. [Google Scholar] [CrossRef]
- Conrad, M.; Pratt, D.A. The chemical basis of ferroptosis. Nat. Chem. Biol. 2019, 15, 1137–1147. [Google Scholar] [CrossRef]
- Conrad, M.; Proneth, B. Selenium: Tracing another essential element of ferroptotic cell death. Cell Chem. Biol. 2020, 27, 409–419. [Google Scholar] [CrossRef]
- Ladenstein, R.; Wendel, A. Crystallographic data of the selenoenzyme glutathione peroxidase. J. Mol. Biol. 1976, 104, 877–882. [Google Scholar] [CrossRef]
- Maiorino, M.; Aumann, K.D.; Brigelius-Flohé, R.; Doria, D.; van den Heuvel, J.; McCarthy, J.; Roveri, A.; Ursini, F.; Flohé, L. Probing the presumed catalytic triad of selenium-containing peroxidases by mutational analysis of phospholipid hydroperoxide glutathione peroxidase (phgpx). Biol. Chem. Hoppe Seyler 1995, 376, 651–660. [Google Scholar] [CrossRef]
- Tosatto, S.C.; Bosello, V.; Fogolari, F.; Mauri, P.; Roveri, A.; Toppo, S.; Flohé, L.; Ursini, F.; Maiorino, M. The catalytic site of glutathione peroxidases. Antioxid. Redox Signal. 2008, 10, 1515–1526. [Google Scholar] [CrossRef]
- Orian, L.; Mauri, P.; Roveri, A.; Toppo, S.; Benazzi, L.; Bosello-Travain, V.; De Palma, A.; Maiorino, M.; Miotto, G.; Zaccarin, M.; et al. Selenocysteine oxidation in glutathione peroxidase catalysis: An ms-supported quantum mechanics study. Free Radic. Biol. Med. 2015, 87, 1–14. [Google Scholar] [CrossRef]
- Gladyshev, V.N. Identity, evolution and function of selenoproteins and selenoprotein genes. In Selenium. Its Molecular Biology and Role in Human Health, 1st ed.; Hatfiel, D.L., Ed.; Kluwer Academic Publisher: Boston, UK; Dordrecht, The Netherlands; London, UK, 2001; pp. 99–114. [Google Scholar]
- Brigelius-Flohé, R.; Flohé, L. Regulatory phenomena in the glutathione peroxidase superfamily. Antioxid. Redox Signal. 2019, 33, 498–516. [Google Scholar] [CrossRef] [PubMed]
- Hatfield, D.L. Selenium. Its Molecular Biology and Role in Human Health; Kluwer Academic Publishers: Boston, UK; Dordrecht, The Netherlands; London, UK, 2001. [Google Scholar]
- Hatfield, D.L.; Berry, M.; Gladyshev, V.N. Selenium. Its Molecular Biology and Role in Human Health, 2nd ed.; Springer: New Yok, NY, USA, 2006. [Google Scholar]
- Hatfield, D.L.; Berry, M.J.; Gladyshev, V.N. Selenium. Its Molecular Biology and Role in Human Health, 3rd ed.; Springer: New York, NY, USA, 2012. [Google Scholar]
- Hatfield, D.L.; Schweizer, U.; Tsuji, P.A.; Gladyshev, V.N. Selenium. Its Molecular Biolgy and Role in Human Health, 4th ed.; Springer: New York, NY, USA, 2016. [Google Scholar]
- Rocher, C.; Lalanne, J.L.; Chaudiere, J. Purification and properties of a recombinant sulfur analog of murine selenium-glutathione peroxidase. Eur. J. Biochem. 1992, 205, 955–960. [Google Scholar] [CrossRef] [PubMed]
- Winterbourn, C.C. The biological chemistry of hydrogen peroxide. Methods Enzymol. 2013, 528, 3–25. [Google Scholar] [PubMed]
- Maiorino, M.; Ursini, F.; Bosello, V.; Toppo, S.; Tosatto, S.C.; Mauri, P.; Becker, K.; Roveri, A.; Bulato, C.; Benazzi, L.; et al. The thioredoxin specificity of drosophila GPx: A paradigm for a peroxiredoxin-like mechanism of many glutathione peroxidases. J. Mol. Biol. 2007, 365, 1033–1046. [Google Scholar] [CrossRef] [PubMed]
- Sztajer, H.; Gamain, B.; Aumann, K.D.; Slomianny, C.; Becker, K.; Brigelius-Flohé, R.; Flohé, L. The putative glutathione peroxidase gene of plasmodium falciparum codes for a thioredoxin peroxidase. J. Biol. Chem. 2001, 276, 7397–7403. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, R.A.; Burk, R.F. Glutathione peroxidase activity in selenium-deficient rat liver. Biochem. Biophys. Res. Commun. 1976, 71, 952–958. [Google Scholar] [CrossRef]
- Burk, R.F.; Lawrence, R.A. Non-selenium-dependent glutathione peroxidase. In Functions of Glutathione in Liver and Kidney; Sies, H., Wendel, A., Eds.; Springer: Berlin/Heidelberg, Germany; New York, NY, USA, 1978; pp. 114–119. [Google Scholar]
- Harris, J.R. Release of a macromolecular protein component from human erythrocyte ghosts. Biochim. Biophys. Acta 1968, 150, 534–537. [Google Scholar] [CrossRef]
- Harris, J.R. Torin and cylindrin, two extrinsic proteins of the erythrocyte membrane: A review. Nouv. Rrevue Francaise d Hematol. 1980, 22, 411–448. [Google Scholar]
- Flohé, L.; Harris, J.R. Introduction. History of the peroxiredoxins and topical perspectives. Sub Cell. Biochem. 2007, 44, 1–25. [Google Scholar]
- Tartaglia, L.A.; Storz, G.; Brodsky, M.H.; Lai, A.; Ames, B.N. Alkyl hydroperoxide reductase from Salmonella typhimurium. Sequence and homology to thioredoxin reductase and other flavoprotein disulfide oxidoreductases. J. Biol. Chem. 1990, 265, 10535–10540. [Google Scholar]
- Kim, K.; Kim, I.H.; Lee, K.Y.; Rhee, S.G.; Stadtman, E.R. The isolation and purification of a specific “protector” protein which inhibits enzyme inactivation by a thiol/Fe(III)/O2 mixed-function oxidation system. J. Biol. Chem. 1988, 263, 4704–4711. [Google Scholar] [PubMed]
- Chae, H.Z.; Kim, I.H.; Kim, K.; Rhee, S.G. Cloning, sequencing, and mutation of thiol-specific antioxidant gene of Saccharomyces cerevisiae. J. Biol. Chem. 1993, 268, 16815–16821. [Google Scholar] [PubMed]
- Chae, H.Z.; Robison, K.; Poole, L.B.; Church, G.; Storz, G.; Rhee, S.G. Cloning and sequencing of thiol-specific antioxidant from mammalian brain: Alkyl hydroperoxide reductase and thiol-specific antioxidant define a large family of antioxidant enzymes. Proc. Natl. Acad. Sci. USA 1994, 91, 7017–7021. [Google Scholar] [CrossRef] [PubMed]
- Chae, H.Z.; Chung, S.J.; Rhee, S.G. Thioredoxin-dependent peroxide reductase from yeast. J. Biol. Chem. 1994, 269, 27670–27678. [Google Scholar]
- Netto, L.E.S.; Chae, H.Z.; Kang, S.W.; Rhee, S.G.; Stadtman, E.R. Removal of hydrogen peroxide by thiol-specific antioxidant enzyme (TSA) is involved with its antioxidant properties. TSA possesses thiol peroxidase activity. J. Biol. Chem. 1996, 271, 15315–15321. [Google Scholar] [CrossRef]
- Nogoceke, E.; Gommel, D.U.; Kiess, M.; Kalisz, H.M.; Flohé, L. A unique cascade of oxidoreductases catalyses trypanothione-mediated peroxide metabolism in Crithidia fasciculata. Biol. Chem. 1997, 378, 827–836. [Google Scholar] [CrossRef]
- Gommel, D.U.; Nogoceke, E.; Morr, M.; Kiess, M.; Kalisz, H.M.; Flohé, L. Catalytic characteristics of tryparedoxin. Eur. J. Biochem. 1997, 248, 913–918. [Google Scholar] [CrossRef]
- Castro, H.; Tomas, A.M. Peroxidases of trypanosomatids. Antioxid. Redox Signal. 2008, 10, 1593–1606. [Google Scholar] [CrossRef]
- Ellis, H.R.; Poole, L.B. Roles for the two cysteine residues of ahpc in catalysis of peroxide reduction by alkyl hydroperoxide reductase from Salmonella typhimurium. Biochemistry 1997, 36, 13349–13356. [Google Scholar] [CrossRef]
- Montemartini, M.; Kalisz, H.M.; Hecht, H.J.; Steinert, P.; Flohé, L. Activation of active-site cysteine residues in the peroxiredoxin-type tryparedoxin peroxidase of Crithidia fasciculata. Eur. J. Biochem. 1999, 264, 516–524. [Google Scholar] [CrossRef]
- Chen, J.W.; Dodia, C.; Feinstein, S.I.; Jain, M.K.; Fisher, A.B. 1-Cys peroxiredoxin, a bifunctional enzyme with glutathione peroxidase and phospholipase a2 activities. J. Biol. Chem. 2000, 275, 28421–28427. [Google Scholar] [CrossRef] [PubMed]
- Flohé, L.; Budde, H.; Bruns, K.; Castro, H.; Clos, J.; Hofmann, B.; Kansal-Kalavar, S.; Krumme, D.; Menge, U.; Plank-Schumacher, K.; et al. Tryparedoxin peroxidase of Leishmania donovani: Molecular cloning, heterologous expression, specificity, and catalytic mechanism. Arch. Biochem. Biophys. 2002, 397, 324–335. [Google Scholar] [CrossRef] [PubMed]
- König, J.; Lotte, K.; Plessow, R.; Brockhinke, A.; Baier, M.; Dietz, K.J. Reaction mechanism of plant 2-Cys peroxiredoxin. Role of the C-terminus and the quaternary structure. J. Biol. Chem. 2003, 278, 24409–24420. [Google Scholar] [CrossRef] [PubMed]
- Deponte, M.; Becker, K. Biochemical characterization of Toxoplasma gondii 1-cys peroxiredoxin 2 with mechanistic similarities to typical 2-Cys Prx. Mol. Biochem. Parasitol. 2005, 140, 87–96. [Google Scholar] [CrossRef] [PubMed]
- Poole, L.B. The catalytic mechanism of peroxiredoxins. Sub Cell. Biochem. 2007, 44, 61–81. [Google Scholar]
- Dalla Tiezza, M.; Bickelhaupt, F.M.; Flohé, L.; Maiorino, M.; Ursini, F.; Orian, L. A dual attack on the peroxide bond. The common principle of peroxidatic cysteine or selenocysteine residues. Redox Biol. 2020, 34, 101540. [Google Scholar] [CrossRef]
- Hofmann, B.; Hecht, H.J.; Flohé, L. Peroxiredoxins. Biol. Chem. 2002, 383, 347–364. [Google Scholar] [CrossRef]
- Peshenko, I.V.; Novoselov, V.I.; Evdokimov, V.A.; Nikolaev Yu, V.; Shuvaeva, T.M.; Lipkin, V.M.; Fesenko, E.E. Novel 28-kda secretory protein from rat olfactory epithelium. FEBS Lett. 1996, 381, 12–14. [Google Scholar] [CrossRef]
- Singh, A.K.; Shichi, H. A novel glutathione peroxidase in bovine eye. Sequence analysis, mRNA level, and translation. J. Biol. Chem. 1998, 273, 26171–26178. [Google Scholar] [CrossRef]
- Manevich, Y. Peroxiredoxin 6 as glutathione peroxidase. In Glutathione; Flohé, L., Ed.; CRC Press: Boca Raton, FL, USA, 2019; pp. 143–159. [Google Scholar]
- Greetham, D.; Grant, C.M. Antioxidant activity of the yeast mitochondrial one-Cys peroxiredoxin is dependent on thioredoxin reductase and glutathione in vivo. Mol. Cell. Biol. 2009, 29, 3229–3240. [Google Scholar] [CrossRef]
- Monteiro, G.; Horta, B.B.; Pimenta, D.C.; Augusto, O.; Netto, L.E. Reduction of 1-Cys peroxiredoxins by ascorbate changes the thiol-specific antioxidant paradigm, revealing another function of vitamin c. Proc. Natl. Acad. Sci. USA 2007, 104, 4886–4891. [Google Scholar] [CrossRef] [PubMed]
- Anschau, V.; Ferrer-Sueta, G.; Aleixo-Silva, R.L.; Bannitz Fernandes, R.; Tairum, C.A.; Tonoli, C.C.C.; Murakami, M.T.; de Oliveira, M.A.; Netto, L.E.S. Reduction of sulfenic acids by ascorbate in proteins, connecting thiol-dependent to alternative redox pathways. Free Radic. Biol. Med. 2020, 156, 207–216. [Google Scholar] [CrossRef] [PubMed]
- Budde, H.; Flohé, L.; Hofmann, B.; Nimtz, M. Verification of the interaction of a tryparedoxin peroxidase with tryparedoxin by esi-ms/ms. Biol. Chem. 2003, 384, 1305–1309. [Google Scholar] [CrossRef] [PubMed]
- Budde, H.; Flohé, L.; Hecht, H.J.; Hofmann, B.; Stehr, M.; Wissing, J.; Lünsdorf, H. Kinetics and redox-sensitive oligomerisation reveal negative subunit cooperativity in tryparedoxin peroxidase of trypanosoma brucei brucei. Biol. Chem. 2003, 384, 619–633. [Google Scholar] [CrossRef]
- Peralta, D.; Bronowska, A.K.; Morgan, B.; Doka, E.; Van Laer, K.; Nagy, P.; Grater, F.; Dick, T.P. A proton relay enhances H2O2 sensitivity of GAPDH to facilitate metabolic adaptation. Nat. Chem. Biol. 2015, 11, 156–163. [Google Scholar] [CrossRef]
- Little, C.; O’Brien, P.J. Mechanism of peroxide-inactivation of the sulphydryl enzyme glyceraldehyde-3-phosphate dehydrogenase. Eur. J. Biochem. 1969, 10, 533–538. [Google Scholar] [CrossRef]
- Hildebrandt, T.; Knuesting, J.; Berndt, C.; Morgan, B.; Scheibe, R. Cytosolic thiol switches regulating basic cellular functions: GAPDH as an information hub? Biol. Chem. 2015, 396, 523–537. [Google Scholar] [CrossRef]
- Christman, M.F.; Morgan, R.W.; Jacobson, F.S.; Ames, B.N. Positive control of a regulon for defenses against oxidative stress and some heat-shock proteins in salmonella typhimurium. Cell 1985, 41, 753–762. [Google Scholar] [CrossRef]
- Pedre, B.; Young, D.; Charlier, D.; Mourenza, A.; Rosado, L.A.; Marcos-Pascual, L.; Wahni, K.; Martens, E.; Rubia, A.G.D.L.; Belousov, V.V.; et al. Structural snapshots of OxyR reveal the peroxidatic mechanism of H2O2 sensing. Proc. Natl. Acad. Sci. USA 2018, 115, E11623–E11632. [Google Scholar] [CrossRef]
- Brigelius-Flohé, R.; Flohé, L. Basic principles and emerging concepts in the redox control of transcription factors. Antioxid. Redox Signal. 2011, 15, 2335–2381. [Google Scholar] [CrossRef]
- Ferrer-Sueta, G.; Manta, B.; Botti, H.; Radi, R.; Trujillo, M.; Denicola, A. Factors affecting protein thiol reactivity and specificity in peroxide reduction. Chem. Res. Toxicol. 2011, 24, 434–450. [Google Scholar] [CrossRef] [PubMed]
- Winterbourn, C.C.; Hampton, M.B. Thiol chemistry and specificity in redox signaling. Free Radic. Biol. Med. 2008, 45, 549–561. [Google Scholar] [CrossRef] [PubMed]
- Forman, H.J.; Maiorino, M.; Ursini, F. Signaling functions of reactive oxygen species. Biochemistry 2010, 49, 835–842. [Google Scholar] [CrossRef] [PubMed]
- Delaunay, A.; Pflieger, D.; Barrault, M.B.; Vinh, J.; Toledano, M.B. A thiol peroxidase is an H2O2 receptor and redox-transducer in gene activation. Cell 2002, 111, 471–481. [Google Scholar] [CrossRef]
- Ross, S.J.; Findlay, V.J.; Malakasi, P.; Morgan, B.A. Thioredoxin peroxidase is required for the transcriptional response to oxidative stress in budding yeast. Mol. Biol. Cell 2000, 11, 2631–2642. [Google Scholar] [CrossRef]
- Okazaki, S.; Naganuma, A.; Kuge, S. Peroxiredoxin-mediated redox regulation of the nuclear localization of yap1, a transcription factor in budding yeast. Antioxid. Redox Signal. 2005, 7, 327–334. [Google Scholar] [CrossRef]
- Maiorino, M.; Bosello-Travain, V.; Cozza, G.; Miotto, G.; Roveri, A.; Toppo, S.; Zaccarin, M.; Ursini, F. Understanding mammalian glutathione peroxidase 7 in the light of its homologs. Free Radic. Biol. Med. 2015, 83, 352–360. [Google Scholar] [CrossRef]
- Nguyen, V.D.; Saaranen, M.J.; Karala, A.R.; Lappi, A.K.; Wang, L.; Raykhel, I.B.; Alanen, H.I.; Salo, K.E.; Wang, C.C.; Ruddock, L.W. Two endoplasmic reticulum pdi peroxidases increase the efficiency of the use of peroxide during disulfide bond formation. J. Mol. Biol. 2011, 406, 503–515. [Google Scholar] [CrossRef]
- Ramming, T.; Appenzeller-Herzog, C. Destroy and exploit: Catalyzed removal of hydroperoxides from the endoplasmic reticulum. Int. J. Cell Biol. 2013, 2013, 1–13. [Google Scholar] [CrossRef]
- Wei, P.C.; Hsieh, Y.H.; Su, M.I.; Jiang, X.; Hsu, P.H.; Lo, W.T.; Weng, J.Y.; Jeng, Y.M.; Wang, J.M.; Chen, P.L.; et al. Loss of the oxidative stress sensor NPGPX compromises GRP78 chaperone activity and induces systemic disease. Mol. Cell 2012, 48, 747–759. [Google Scholar] [CrossRef]
- Stöcker, S.; Maurer, M.; Ruppert, T.; Dick, T.P. A role for 2-cys peroxiredoxins in facilitating cytosolic protein thiol oxidation. Nat. Chem. Biol. 2018, 14, 148–155. [Google Scholar] [CrossRef] [PubMed]
- Flohé, L. The impact of thiol peroxidases on redox regulation. Free Radic. Res. 2016, 50, 126–142. [Google Scholar] [CrossRef] [PubMed]
- Lavoisier, A. Traité Élémentaire de Chimie, Presenté dans un Ordre Nouveau et d’après Découvertes Modernes; Cuchet, Libraire: Paris, France, 1789. [Google Scholar]
- Gomberg, M. An instance of trivalent carbon: Triphenylmethyl. J. Am. Chem. Soc. 1900, 22, 757–771. [Google Scholar] [CrossRef]
- Reichard, P. The biosynthesis of deoxyribonucleic acid by the chick embryo. IV. Formation of deoxycytidine and deoxyguanosine phosphates with soluble enzymes. J. Biol. Chem. 1961, 236, 2511–2513. [Google Scholar] [PubMed]
- Reichard, P.; Rutberg, L. Formation of deoxycytidine 5’-phosphate from cytidine 5’-phosphate with enzymes from Escherichia coli. Biochim. Biophys. Acta 1960, 37, 554–555. [Google Scholar] [CrossRef]
- Ehrenberg, A.; Reichard, P. Electron spin resonance of the iron-containing protein b2 from ribonucleotide reductase. J. Biol. Chem. 1972, 247, 3485–3488. [Google Scholar]
- Sjöberg, B.M.; Reichard, P.; Graslund, A.; Ehrenberg, A. The tyrosine free radical in ribonucleotide reductase from Escherichia coli. J. Biol. Chem. 1978, 253, 6863–6865. [Google Scholar]
- Laurent, T.C.; Moore, E.C.; Reichard, P. Enzymatic synthesis of deoxyribonucleotides. Iv. Isolation and characterization of thioredoxin, the hydrogen donor from Escherichia coli b. J. Biol. Chem. 1964, 239, 3436–3444. [Google Scholar]
- Holmgren, A.; Reichard, P.; Thelander, L. Enzymatic synthesis of deoxyribonucleotides, 8. The effects of ATP and dATP in the CDP reductase system from E. coli. Proc. Natl. Acad. Sci. USA 1965, 54, 830–836. [Google Scholar] [CrossRef]
- Holmgren, A. Hydrogen donor system for Escherichia coli ribonucleoside-diphosphate reductase dependent upon glutathione. Proc. Natl. Acad. Sci. USA 1976, 73, 2275–2279. [Google Scholar] [CrossRef]
- Dormeyer, M.; Reckenfelderbäumer, N.; Lüdemann, H.; Krauth-Siegel, R.L. Trypanothione-dependent synthesis of deoxyribonucleotides by Trypanosoma brucei ribonucleotide reductase. J. Biol. Chem. 2001, 276, 10602–10606. [Google Scholar] [CrossRef] [PubMed]
- Jordan, A.; Reichard, P. Ribonucleotide reductases. Annu. Rev. Biochem. 1998, 67, 71–98. [Google Scholar] [CrossRef] [PubMed]
- Holmgren, A. Thioredoxin. Annu. Rev. Biochem. 1985, 54, 237–271. [Google Scholar] [CrossRef] [PubMed]
- Kang, G.; Taguchi, A.T.; Stubbe, J.; Drennan, C.L. Structure of a trapped radical transfer pathway within a ribonucleotide reductase holocomplex. Science 2020, 368, 424–427. [Google Scholar] [CrossRef] [PubMed]
- Michaelis, L. The formation ofsemiquinones as intermediary reduction productsfrom pyocyamineand other dyestuffs. J. Biol. Chem. 1931, 92, 211–232. [Google Scholar]
- Haber, F.; Weiss, J. The catalytic decomposition of hydrogen peroxide by iron salts. Proc. R. Soc. Lond. Series A Math. Phys. Sci. 1934, 147, 332–351. [Google Scholar]
- McCord, J.; Fridovich, I. Superoxide dismutases: A history. In Superoxide and Superoxide Dismutases; Michelson, A.M., McCord, M.J., Fridovich, I., Eds.; Acad Press: London, UK; New York, NY, USA; San Francisxco, CA, USA, 1977; pp. 1–10. [Google Scholar]
- McCord, J.M.; Fridovich, I. The reduction of cytochrome c by milk xanthine oxidase. J. Biol. Chem. 1968, 243, 5753–5760. [Google Scholar]
- McCord, J.M.; Fridovich, I. Superoxide dismutase. An enzymic function for erythrocuprein (hemocuprein). J. Biol. Chem. 1969, 244, 6049–6055. [Google Scholar]
- Mann, T.; Keilin, D. Haemocuprei and hepatocuprein, copper-proteins of blood and liver of mammals. Proc. R. Soc. B. Biol. Sci. 1938, 128, 303–315. [Google Scholar]
- Markowitz, H.; Cartwright, G.E.; Wintrobe, M.M. Studies on copper metabolism. XXVII. The isolation and properties of an erythrocyte cuproprotein (erythrocuprein). J. Biol. Chem. 1959, 234, 40–45. [Google Scholar]
- Porter, H.; Folch, J. Cerebrocuprein i. A copper-containing protein isolated from brain. J. Neurochem. 1957, 1, 260–271. [Google Scholar] [CrossRef] [PubMed]
- Klug, D.; Rabani, J.; Fridovich, I. A direct demonstration of the catalytic action of superoxide dismutase through the use of pulse radiolysis. J. Biol. Chem. 1972, 247, 4839–4842. [Google Scholar] [PubMed]
- Fridovich, I. Superoxide dismutases. Annu. Rev. Biochem. 1975, 44, 147–159. [Google Scholar] [CrossRef] [PubMed]
- Koppenol, W.H. The physiological role of the charge ditribution on superoxide dismutase. In Oxygen and Oxyradicals in Chemistry and Biology; Rodgers, M.A.J., Powers, E.L., Eds.; Academic Press: New York, NY, USA, 1981; pp. 671–674. [Google Scholar]
- Tainer, J.A.; Getzoff, E.D.; Richardson, J.S.; Richardson, D.C. Structure and mechanism of copper, zinc superoxide dismutase. Nature 1983, 306, 284–287. [Google Scholar] [CrossRef]
- Getzoff, E.D.; Tainer, J.A.; Weiner, P.K.; Kollman, P.A.; Richardson, J.S.; Richardson, D.C. Electrostatic recognition between superoxide and copper, zinc superoxide dismutase. Nature 1983, 306, 287–290. [Google Scholar] [CrossRef]
- Keele, B.B.; McCord, J.M.; Fridovich, I. Superoxide dismutase from Escherichia coli b. A new manganese-containing enzyme. J. Biol. Chem. 1970, 245, 6176–6181. [Google Scholar]
- Weisiger, R.A.; Fridovich, I. Mitochondrial superoxide simutase. Site of synthesis and intramitochondrial localization. J. Biol. Chem. 1973, 248, 4793–4796. [Google Scholar]
- Yost, F.J.; Fridovich, I. An iron-containing superoxide dismutase from Escherichia coli. J. Biol. Chem. 1973, 248, 4905–4908. [Google Scholar]
- Bruchhaus, I.; Brattig, N.W.; Tannich, E. Recombinant expression, purification and biochemical characterization of a superoxide dismutase from Entamoeba histolytica. Arch. Med. Res. 1992, 23, 27–29. [Google Scholar]
- Marklund, S.L. Extracellular superoxide dismutase in human tissues and human cell lines. J. Clin. Investig. 1984, 74, 1398–1403. [Google Scholar] [CrossRef]
- Puget, K.; Lavelle, F.; Michelson, A.M. Superoxide dismutases from procaryote and eucaryote bioluminescent organisms. In Superoxide and Superoxide Dismutases; Michelson, A.M., McCord, J.M., Fridovich, I., Eds.; Academic Press: London, UK; New York, NY, USA; San Francisco, CA, USA, 1977; pp. 139–150. [Google Scholar]
- Steffens, G.J.; Bannister, J.V.; Bannister, W.H.; Flohé, L.; Günzler, W.A.; Kim, S.M.; Ötting, F. The primary structure of cu-zn superoxide dismutase from Photobacterium leiognathi: Evidence for a separate evolution of Cu-Zn superoxide dismutase in bacteria. Hoppe Seylers Z. Physiol. Chem. 1983, 364, 675–690. [Google Scholar] [CrossRef] [PubMed]
- Steinman, H.M. Copper-zinc superoxide dismutase from Caulobacter crescentus cb15. A novel bacteriocuprein form of the enzyme. J. Biol. Chem. 1982, 257, 10283–10293. [Google Scholar] [PubMed]
- Fee, J.A.; Teitelbaum, H.D. Evidence that superoxide dismutase plays a role in protecting red blood cells against peroxidative hemolysis. Biochem. Biophys. Res. Commun. 1972, 49, 150–158. [Google Scholar] [CrossRef]
- Flohé, L.; Zimmermann, R. The role of GSH peroxidase in protecting the membrane of rat liver mitochondria. Biochim. Biophys. Acta 1970, 223, 210–213. [Google Scholar] [CrossRef]
- Flohé, L.; Zimmermann, R. GSH-induced high-ampltude swelling of mitochondria. In Glutathione; Flohé, L., Benöhr, H.C., Sies, H., Waller, H.D., Wendel, A., Eds.; Thieme: Stuttgart, Germany, 1974; pp. 245–260. [Google Scholar]
- Zimmermann, R.; Flohé, L.; Weser, U.; Hartmann, H.-J. Inhibition of lipid peroxidation in isolated inner membrane of rat liver mitochondria by superoxide dismutase. FEBS Lett. 1973, 29, 117–120. [Google Scholar] [CrossRef]
- Neubert, D.; Wojtczak, A.B.; Lehninger, A.L. Purification and enzymatic identity of mitochondrial contraction-factors I and II. Proc. Natl. Acad. Sci. USA 1962, 48, 1651–1658. [Google Scholar] [CrossRef]
- Hunter, F.E.; Scott, A.; Hoffsten, P.E.; Gebicki, J.M.; Weinstein, J.; Schneider, A. Studies on the mechanism of swelling, lysis, and distintegration of isolated liver mitochondria exposed to mixtures of oxidized and reduced glutathione. J. Biol. Chem. 1964, 239, 614–621. [Google Scholar]
- Lehninger, A.L.; Schneider, M. Mitochondrial swelling induced by glutathione. J. Biophys. Biochem. Cytol. 1959, 5, 109–116. [Google Scholar] [CrossRef]
- Misra, H.P. Generation of superoxide free radical during the autoxidation of thiols. J. Biol. Chem. 1974, 249, 2151–2155. [Google Scholar]
- Dorfman, L.M.; Adams, G.E. Reactivity of Hydroxyl Radical in Aqueous Solution; National Bureau of Standards: Washington, DC, USA, 1973; Volume 46, p. 72. [Google Scholar]
- Fenton, H.J.H. Oxidation of tartaric acid in presence of iron. J. Chem. Soc. Trans. 1894, 65, 899–910. [Google Scholar] [CrossRef]
- Carrier, A.J.; Hamid, S.; Oakley, D.; Oakes, K.; Zhang, X. Singlet oxygen generation in classical fenton chemistry. In ChemRxiv; ChemRxiv: Washington, DC, USA, 2019. [Google Scholar] [CrossRef]
- Scalano, J.G. Kinetic studies of alkoxy radicals. In Oxygen Radicals in Biology and Medicine; Simic, M.G., Taylor, K.A., Ward, J.F., Von Sonntag, C., Eds.; Plenum Press: New York, NY, USA; London, UK, 1988; Volume 49, pp. 59–66. [Google Scholar]
- Sagadevan, A.; Hwang, K.C.; Su, M.D. Singlet oxygen-mediated selective C-H bond hydroperoxidation of ethereal hydrocarbons. Nat. Commun. 2017, 8, 1812. [Google Scholar] [CrossRef] [PubMed]
- Tatsuzawa, H.; Maruyama, T.; Hori, K.; Sano, Y.; Nakano, M. Singlet oxygen ((1)delta(g)O(2)) as the principal oxidant in myeloperoxidase-mediated bacterial killing in neutrophil phagosome. Biochem. Biophys. Res. Commun. 1999, 262, 647–650. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.U. Myeloperoxidase singlet molecular oxygen generation detected by direct infrared electronic emission. Biochem. Biophys. Res. Commun. 1984, 122, 668–675. [Google Scholar] [CrossRef]
- Khan, A.U.; Gebauer, P.; Hager, L.P. Chloroperoxidase generation of singlet delta molecular oxygen observed directly by spectroscopy in the 1- to 1.6-mum region. Proc. Natl. Acad. Sci. USA 1983, 80, 5195–5197. [Google Scholar] [CrossRef] [PubMed]
- Brash, A.R. Lipoxygenases: Occurrence, functions, catalysis, and acquisition of substrate. J. Biol. Chem. 1999, 274, 23679–23682. [Google Scholar] [CrossRef]
- Mashima, R.; Okuyama, T. The role of lipoxygenases in pathophysiology; new insights and future perspectives. Redox Biol. 2015, 6, 297–310. [Google Scholar] [CrossRef] [PubMed]
- Morgenstern, R.; Haeggström, J.Z.; Jakobsson, P.-J.; Flohé, L. The role of glutathione in biosynthetic pathways of the eicosanoid metabolism. In Glutathione; Flohé, L., Ed.; CRC Press: Boca Raton, FL, USA, 2019; pp. 215–226. [Google Scholar]
- Haurand, M.; Flohé, L. Kinetic studies on arachidonate 5-lipoxygenase from rat basophilic leukemia cells. Biol. Chem. Hoppe Seyler 1988, 369, 133–142. [Google Scholar] [CrossRef]
- Hill, T.D.; White, J.G.; Rao, G.H. Role of glutathione and glutathione peroxidase in human platelet arachidonic acid metabolism. Prostaglandins 1989, 38, 21–32. [Google Scholar] [CrossRef]
- Azzi, A.; Loschen, G.; Flohé, L. Structural and functional aspects of H2O2 formation in the mitochondrial membrane. In Glutathione; Flohé, L., Benöhr, H.C., Sies, H., Waller, H.D., Wendel, A., Eds.; Thieme: Stuttgart, Germany, 1974; pp. 237–244. [Google Scholar]
- Weisiger, R.A.; Fridovich, I. Superoxide dismutase. Organelle specificity. J. Biol. Chem. 1973, 248, 3582–3592. [Google Scholar]
- Weser, U.; Bunnenberg, E.; Cammack, R.; Djerassi, C.; Flohé, L.; Thomas, G.; Voelter, W. A study on purified bovine erythrocuprein. Biochim. Biophys. Acta 1971, 243, 203–213. [Google Scholar] [CrossRef]
- Loschen, G.; Azzi, A.; Richter, C.; Flohé, L. Superoxide radicals as precursors of mitochondrial hydrogen peroxide. FEBS Lett. 1974, 42, 68–72. [Google Scholar] [CrossRef]
- Azzi, A. How I became a biochemist. IUBMB Life 2003, 55, 555–558. [Google Scholar] [CrossRef] [PubMed]
- Boveris, A.; Cadenas, E. Mitochondrial production of superoxide anions and its relationship to the antimycin insensitive respiration. FEBS Lett. 1975, 54, 311–314. [Google Scholar] [CrossRef]
- Forman, H.J.; Kennedy, J.A. Role of superoxide radical in mitochondrial dehydrogenase reactions. Biochem. Biophys. Res. Commun. 1974, 60, 1044–1050. [Google Scholar] [CrossRef]
- Richter, C.; Azzi, A.; Weser, U.; Wendel, A. Hepatic microsomal dealkylations. Inhibition by a tyrosine-copper (II) complex provided with superoxide dismutase activity. J. Biol. Chem. 1977, 252, 5061–5066. [Google Scholar] [PubMed]
- Boveris, A.; Cadenas, E.; Stoppani, A.O. Role of ubiquinone in the mitochondrial generation of hydrogen peroxide. Biochem. J. 1976, 156, 435–444. [Google Scholar] [CrossRef]
- Boveris, A.; Cadenas, E. Mitochondrial production of hydrogen peroxide regulation by nitric oxide and the role of ubisemiquinone. IUBMB Life 2000, 50, 245–250. [Google Scholar] [CrossRef]
- Gerth, K.; Irschik, H.; Reichenbach, H.; Trowitzsch, W. Myxothiazol, an antibiotic from Myxococcus fulvus (myxobacterales). I. Cultivation, isolation, physico-chemical and biological properties. J. Antibiot. 1980, 33, 1474–1479. [Google Scholar] [CrossRef]
- Thierbach, G.; Reichenbach, H. Myxothiazol, a new inhibitor of the cytochrome b-c1 segment of the respiratory chain. Biochim. Biophys. Acta 1981, 638, 282–289. [Google Scholar] [CrossRef]
- Nohl, H.; Jordan, W. The mitochondrial site of superoxide formation. Biochem. Biophys. Res. Commun. 1986, 138, 533–539. [Google Scholar] [CrossRef]
- Brand, M.D. Mitochondrial generation of superoxide and hydrogen peroxide as the source of mitochondrial redox signaling. Free Radic. Biol. Med. 2016, 100, 14–31. [Google Scholar] [CrossRef] [PubMed]
- Murphy, M.P. How mitochondria produce reactive oxygen species. Biochem. J. 2009, 417, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Babior, B.M.; Kipnes, R.S.; Curnutte, J.T. Biological defense mechanisms. The production by leukocytes of superoxide, a potential bactericidal agent. J. Clin. Investig. 1973, 52, 741–744. [Google Scholar] [CrossRef] [PubMed]
- Baehner, R.L.; Murrmann, S.K.; Davis, J.; Johnston, R.B. The role of superoxide anion and hydrogen peroxide in phagocytosis-associated oxidative metabolic reactions. J. Clin. Investig. 1975, 56, 571–576. [Google Scholar] [CrossRef] [PubMed]
- Johnston, R.B.; Keele, B.B.; Misra, H.P.; Lehmeyer, J.E.; Webb, L.S.; Baehner, R.L.; RaJagopalan, K.V. The role of superoxide anion generation in phagocytic bactericidal activity. Studies with normal and chronic granulomatous disease leukocytes. J. Clin. Investig. 1975, 55, 1357–1372. [Google Scholar] [CrossRef] [PubMed]
- Johnston, R.B.; Lehmeyer, J.E.; Guthrie, L.A. Generation of superoxide anion and chemiluminescence by human monocytes during phagocytosis and on contact with surface-bound immunoglobulin g. J. Exp. Med. 1976, 143, 1551–1556. [Google Scholar] [CrossRef]
- Lowrie, D.B.; Aber, V.R. Superoxide production by rabbit pulmonary alveolar macrophages. Life Sci. 1977, 21, 1575–1584. [Google Scholar] [CrossRef]
- Baldridge, C.W.; Gerard, R.W. The extra respiration of phagocytosis. Am. J. Physiol. 1933, 103, 235–236. [Google Scholar] [CrossRef]
- Metchnikoff, E. Untersuchungen über die mesodermalen Phagocyten einiger Wirbeltiere. Biol. Zent. 1883, 3, 560–565. [Google Scholar]
- Klebanoff, S.J. Iodination of bacteria: A bactericidal mechanism. J. Exp. Med. 1967, 126, 1063–1078. [Google Scholar] [CrossRef]
- Klebanoff, S.J. Myeloperoxidase-halide-hydrogen peroxide antibacterial system. J. Bacteriol. 1968, 95, 2131–2138. [Google Scholar] [CrossRef] [PubMed]
- Flohé, L.; Beckmann, R.; Giertz, H.; Loschen, G. Oxygen-centered radcals as mediators of inflammation. In Oxidative Stress, 1st ed.; Sies, H., Ed.; Academic Press: Orlando, FL, USA, 1985; pp. 403–435. [Google Scholar]
- Esnouf, M.P.; Green, M.R.; Hill, H.A.O.; Irvine, G.B.; Walter, S.J. Ciba Foundation Oxygen Free Radicals and Tissue Damage; Ciba Foundation Symposium 65 (new series); Excerpta Medica: Amsterdam, The Netherlands, 1979; pp. 187–197. [Google Scholar] [CrossRef]
- Roos, D.; Weening, R.S. Defects in oxidative killing of microorganismsby phagocytic leukocytes. In Oxygen Rree Radicals and Tissue Damage; Ciba Foundation Symposium 65 (new series); Excerpta Medica: Amsterdam, the Netherlands; Oxford, UK; New York, NY, USA, 1979; pp. 225–262. [Google Scholar] [CrossRef]
- Huber, W.; Saifer, M.G.P. Orgotein, the drug version of bovine Cu-Zn superoxide dismutase: 1. A summary account of safety and pharmacology in laboratory animals. In Superoxide and Superoxide Dismutases; Michelson, A.M., McCord, J.M., Fridovich, I., Eds.; Academic Press: London, UK; New York, NY, USA; San Francisco, CA, USA, 1977; pp. 517–536. [Google Scholar]
- Flohé, L.; Kim, S.-M.A.; Ötting, F.; Saunders, D.; Schwertner, E.; Steffens, G.J.; Blacher, R.; Masiarz, F.; Scandella, C.; Hallewell, R. Comparison of human Cu/Zn superoxide dismutase derived from erythrocytes, recombinant E. coli and recombinant yeast. In Superoxide and Superoxide Dismutase in Chemistry, Biology and Medicine; Rotilio, G., Ed.; Elsevier: Amsterdam, The Netherlands; New York, NY, USA; Oxford, UK, 1986; pp. 266–269. [Google Scholar]
- Hallewell, R.A.; Masiarz, F.R.; Najarian, R.C.; Puma, J.P.; Quiroga, M.R.; Randolph, A.; Sanchez-Pescador, R.; Scandella, C.J.; Smith, B.; Steimer, K.S. Human Cu/Zn superoxide dismutase cDNA: Isolation of clones synthesising high levels of active or inactive enzyme from an expression library. Nucleic Acids Res. 1985, 13, 2017–2034. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Schneider, J.; Friderichs, E.; Heintze, K.; Flohé, L. Effects of recombinant human superoxide dismutase on increased lung vascular permeability and respiratory disorder in endotoxemic rats. Circ. Shock. 1990, 30, 97–106. [Google Scholar] [PubMed]
- Fincke, U.; Schneider, J.; Friderichs, E.; Giertz, H.; Flohé, L. Enhanced myocardial salvage by combined treatment with recombinant single-chain urokinase-type plasminogen activator and recombinant human superoxide dismutase in a canine coronary thrombosis model. Arzneim. Forsch. 1988, 38, 138–142. [Google Scholar]
- Flohé, L. Superoxide dismutase for therapeutic use: Clinical experience, dead ends and hopes. Mol. Cell. Biochem. 1988, 84, 123–131. [Google Scholar] [CrossRef]
- Sbarra, A.J.; Karnowski, M.L. The biochemical basis of phagocytosis. I. Metabolic changes during the ingestion of particles by polymorphonuclear leukocytes. J. Biol. Chem. 1959, 234, 1355–1362. [Google Scholar]
- Touyz, R.M.; Briones, A.M.; Sedeek, M.; Burger, D.; Montezano, A.C. NOX isoforms and reactive oxygen species in vascular health. Mol. Interv. 2011, 11, 27–35. [Google Scholar] [CrossRef]
- Panday, A.; Sahoo, M.K.; Osorio, D.; Batra, S. NADPH oxidases: An overview from structure to innate immunity-associated pathologies. Cell. Mol. Immunol. 2015, 12, 5–23. [Google Scholar] [CrossRef]
- Baehner, R.L.; Nathan, D.G.; Karnovsky, M.L. Correction of metabolic deficiencies in the leukocytes of patients with chronic granulomatous disease. J. Clin. Investig. 1970, 49, 865–870. [Google Scholar] [CrossRef][Green Version]
- Schröder, K. NADPH oxidases: Current aspects and tools. Redox Biol. 2020, 34, 101512. [Google Scholar] [CrossRef]
- Segal, A.W.; Jones, O.T. Novel cytochrome b system in phagocytic vacuoles of human granulocytes. Nature 1978, 276, 515–517. [Google Scholar] [CrossRef] [PubMed]
- Janeway, C.A.; Craig, J.; Davidson, M.; Downey, W.; Gitlin, D.; Sullivan, J.C. Hypergammaglobulinemia associated with severe, recurrent and non-specific infection. Am. J. Dis. Child. 1954, 88, 388–392. [Google Scholar]
- Roos, D. Chronic granulomatous disease. Methods Mol. Biol. 2019, 1982, 531–542. [Google Scholar] [PubMed]
- Moncada, S.; Palmer, R.M.; Higgs, E.A. The discovery of nitric oxide as the endogenous nitrovasodilator. Hypertension 1988, 12, 365–372. [Google Scholar] [CrossRef] [PubMed]
- Murad, F. Die Entdeckung einiger biologischer Wirkungen von Stickstoffmonoxid und seiner Rolle für die Zellkommunikation. Angew. Chem. 1999, 111, 1976–1989. [Google Scholar] [CrossRef]
- Ignarro, L.J. Stichsatoffmonoxid: Ein einziartiges Signalmolekül in der Gefäßbiologie. Angew. Chem. 1999, 111, 2002–2013. [Google Scholar] [CrossRef]
- Furchgott, R.F. An historical survey and prospects of research on EDRF. Nihon Heikatsukin Gakkai Zasshi 1987, 23, 435–440. [Google Scholar] [CrossRef]
- Furchgott, R.F. Der relaxierende Faktor aus Endothelzellen: Entdeckung, frühe Untersuchungen und Identifizierung als Stickstoffmonoxid (Nobel-Vortrag). Angew. Chem. 1999, 111, 1991–2000. [Google Scholar] [CrossRef]
- Koppenol, W.H. 100 years of peroxynitrite chemistry and 11 years of peroxynitrite biochemistry. Redox Rep. Commun. Free Radic. Res. 2001, 6, 339–341. [Google Scholar] [CrossRef]
- Furchgott, R.F.; Zawadzki, J.V. The obligatory role of endothelial cells in the relaxation of arterial smooth muscle by acetylcholine. Nature 1980, 288, 373–376. [Google Scholar] [CrossRef]
- Murad, F.; Mittal, C.K.; Arnold, W.P.; Katsuki, S.; Kimura, H. Guanylate cyclase: Activation by azide, nitro compounds, nitric oxide, and hydroxyl radical and inhibition by hemoglobin and myoglobin. Adv. Cycle Nucleotide Res. 1978, 9, 145–158. [Google Scholar]
- Ignarro, L.J.; Buga, G.M.; Wood, K.S.; Byrns, R.E.; Chaudhuri, G. Endothelium-derived relaxing factor produced and released from artery and vein is nitric oxide. Proc. Natl. Acad. Sci. USA 1987, 84, 9265–9269. [Google Scholar] [CrossRef] [PubMed]
- Palmer, R.M.; Ferrige, A.G.; Moncada, S. Nitric oxide release accounts for the biological activity of endothelium-derived relaxing factor. Nature 1987, 327, 524–526. [Google Scholar] [CrossRef] [PubMed]
- NobelPrize.org. The nobel prize in physiology or medicine 1998. In The Nobel Prizes; The Nobel Founation: Stockholm, Sweden, 1998. [Google Scholar]
- Ignarro, L.J. Nitric Oxide. Biology and Pathobiology; Academic Press: San Diego, CA, USA; New York, NY, USA; Boston, UK; Sydney, Australia; Tokyo, Japan, 2000; p. 1003. [Google Scholar]
- Kapil, V.; Khambata, R.S.; Jones, D.A.; Rathod, K.; Primus, C.; Massimo, G.; Fukuto, J.M.; Ahluwalia, A. The noncanonical pathway for in vivo nitric oxide generation: The nitrate-nitrite-nitric oxide pathway. Pharmacol. Rev. 2020, 72, 692–766. [Google Scholar] [CrossRef]
- Fukuto, J.M.; Cho, J.Y.; Switzer, C.H. The chemical properties of nitric oxide and related nitrogen oxides. In Nitric Oxide. Biology and Pathobiology, 1st ed.; Ignarro, L.J., Ed.; Academic Press: San Diego, CA, USA; New York, NY, USA; Boston, UK; Sydney, Australia; Tokyo, Japan, 2000; pp. 21–40. [Google Scholar]
- Iglesias, D.E.; Bombicino, S.S.; Valdez, L.B.; Boveris, A. Nitric oxide interacts with mitochondrial complex III producing antimycin-like effects. Free Radic. Biol. Med. 2015, 89, 602–613. [Google Scholar] [CrossRef]
- Koppenol, W.H. The basic chemistry of nitrogen monoxide and peroxynitrite. Free Radic. Biol. Med. 1998, 25, 385–391. [Google Scholar] [CrossRef]
- Radi, R. Nitric oxide, oxidants, and protein tyrosine nitration. Proc. Natl. Acad. Sci. USA 2004, 101, 4003–4008. [Google Scholar] [CrossRef]
- Radi, R.; Denicola, A.; Alvarez, B.; Ferrer-Sueta, G.; Rubbo, H. The biological chemistry of peroxynitrite. In Nitric Oxide: Biology an Pathobiolgy; Ignarro, L.J., Ed.; Academic Press: San Francisco, CA, USA; New York, NY, USA; Boston, UK; Sydney, Australia; Tokyo, Japan, 2000; pp. 57–82. [Google Scholar]
- Rubbo, H.; Radi, R. Antioxidant properties of nitric oxide. In Handbook of Antioxidants; Cadenas, E., Packer, L., Eds.; Marcel Decker Inc: New York, NY, USA; Basel, Switzerland, 2001; pp. 689–706. [Google Scholar]
- Kissner, R.; Nauser, T.; Bugnon, P.; Lye, P.G.; Koppenol, W.H. Formation and properties of peroxynitrite as studied by laser flash photolysis, high-pressure stopped-flow technique, and pulse radiolysis. Chem. Res. Toxicol. 1998, 10, 1285–1292. [Google Scholar] [CrossRef]
- Beckman, J.S.; Koppenol, W.H. Nitric oxide, superoxide, and peroxynitrite: The good, the bad, and ugly. Am. J. Physiol. 1996, 271, C1424–C1437. [Google Scholar] [CrossRef]
- Khan, A.U.; Kovacic, D.; Kolbanovskiy, A.; Desai, M.; Frenkel, K.; Geacintov, N.E. The decomposition of peroxynitrite to nitroxyl anion (NO-) and singlet oxygen in aqueous solution. Proc. Natl. Acad. Sci. USA 2000, 97, 2984–2989. [Google Scholar] [CrossRef]
- Merenyi, G.; Lind, J.; Czapski, G.; Goldstein, S. The decomposition of peroxynitrite does not yield nitroxyl anion and singlet oxygen. Proc. Natl. Acad. Sci. USA 2000, 97, 8216–8218. [Google Scholar] [CrossRef] [PubMed]
- Martinez, G.R.; Di Mascio, P.; Bonini, M.G.; Augusto, O.; Briviba, K.; Sies, H.; Maurer, P.; Rothlisberger, U.; Herold, S.; Koppenol, W.H. Peroxynitrite does not decompose to singlet oxygen ((1)delta(g)O(2)) and nitroxyl (NO(-)). Proc. Natl. Acad. Sci. USA 2000, 97, 10307–10312. [Google Scholar] [CrossRef] [PubMed]
- Moncada, S.; Radomski, M.W.; Palmer, R.M. Endothelium-derived relaxing factor. Identification as nitric oxide and role in the control of vascular tone and platelet function. Biochem. Pharmacol. 1988, 37, 2495–2501. [Google Scholar] [CrossRef]
- Gryglewski, R.J.; Palmer, R.M.; Moncada, S. Superoxide anion is involved in the breakdown of endothelium-derived vascular relaxing factor. Nature 1986, 320, 454–456. [Google Scholar] [CrossRef] [PubMed]
- Alvarez, B.; Demicheli, V.; Duran, R.; Trujillo, M.; Cervenansky, C.; Freeman, B.A.; Radi, R. Inactivation of human Cu, Zn superoxide dismutase by peroxynitrite and formation of histidinyl radical. Free Radic. Biol. Med. 2004, 37, 813–822. [Google Scholar] [CrossRef]
- Carballal, S.; Radi, R.; Kirk, M.C.; Barnes, S.; Freeman, B.A.; Alvarez, B. Sulfenic acid formation in human serum albumin by hydrogen peroxide and peroxynitrite. Biochemistry 2003, 42, 9906–9914. [Google Scholar] [CrossRef]
- Quijano, C.; Hernandez-Saavedra, D.; Castro, L.; McCord, J.M.; Freeman, B.A.; Radi, R. Reaction of peroxynitrite with Mn-superoxide dismutase. Role of the metal center in decomposition kinetics and nitration. J. Biol. Chem. 2001, 276, 11631–11638. [Google Scholar] [CrossRef]
- Buxton, I.L.O.; Barnett, S.D. Nitric oxide and S-nitrosoglutathione. In Glutathione; Flohé, L., Ed.; CRC Press: Boca Raton, FL, USA, 2019; pp. 227–248. [Google Scholar]
- Kourosh-Arami, M.; Hosseini, N.; Mohsenzadegan, M.; Komaki, A.; Joghataei, M.T. Neurophysiologic implications of neuronal nitric oxide synthase. Rev. Neurosci. 2020, 31, 617–636. [Google Scholar] [CrossRef]
- Rajendran, S.; Shen, X.; Glawe, J.; Kolluru, G.K.; Kevil, C.G. Nitric oxide and hydrogen sulfide regulation of ischemic vascular growth and remodeling. Compr. Physiol. 2019, 9, 1213–1247. [Google Scholar]
- Harman, D. Aging: A theory based on free radical and radiation chemistry. J. Gerontol. 1956, 11, 298–300. [Google Scholar] [CrossRef]
- Gershman, R.; Gilbert, D.L.; Nye, S.W.; Dwyer, P.; Fenn, W.O. Oxgen poisoning and x-irradiation: A mechanism in common. Science 1954, 118, 623–626. [Google Scholar] [CrossRef] [PubMed]
- Cohen, A.A.; Kennedy, B.K.; Anglas, U.; Bronikowski, A.M.; Deelen, J.; Dufour, F.; Ferbeyre, G.; Ferrucci, L.; Franceschi, C.; Frasca, D.; et al. Lack of consensus on an aging biology paradigm? A global survey reveals an agreement to disagree, and the need for an interdisciplinary framework. Mech. Ageing Dev. 2020, 111316. [Google Scholar] [CrossRef] [PubMed]
- Michelson, A.M.; McCord, J.M.; Fridovich, I. Superoxide and Superoxide Dismutases; Academic Press: London, UK; New York, NY, USA; San Francisco, CA, USA, 1997; p. 568. [Google Scholar]
- Sies, H. Oxidative Stress, 1st ed.; Academic Press: Orlando, FL, USA, 1985; p. 507. [Google Scholar]
- Bors, W.; Saran, M.; Tait, D. Oxygen Radicals in Biology and Medicine; Walter de Gruyter: Berlin, Germany; New York, NY, USA, 1984; p. 1029. [Google Scholar]
- Yagi, K. Active Oxygen Species, Lipid Peroxides and Antioxidants; CRC Press: Boca Raton, FL, USA, 1993; p. 372. [Google Scholar]
- Hayaishi, O.; Niki, E.; Kondo, M.; Yosahikawa, T. Medical, Biochemical and Chemical Aspects of Free Radicals Volumes 1 and 2; Elsevier: Amsterdam, The Netherlands; New York, NY, USA; Oxford, UK; Tokyo, Japan, 1989; p. 1557. [Google Scholar]
- Simic, M.G.; Taylor, K.A.; Ward, J.F.; von Sonntag, C. Oxygen Radicals in Biology and Medicine; Plenum Press: New York, NY, USA; London, UK, 1988; Volume 49, p. 1095. [Google Scholar]
- Maiorino, M.; Conrad, M.; Ursini, F. GPx4, lipid peroxidation, and cell death: Discoveries, rediscoveries, and open issues. Antioxid. Redox Signal. 2018, 29, 61–74. [Google Scholar] [CrossRef] [PubMed]
- Ursini, F.; Maiorino, M. Lipid peroxidation and ferroptosis: The role of GSH and GPx4. Free Radic. Biol. Med. 2020, 152, 175–185. [Google Scholar] [CrossRef]
- Jacob, H.S.; Jandl, J.H. Effects of sulfhydryl inhibition on red blood cells. 3. Glutathione in the regulation of the hexose monophosphate pathway. J. Biol. Chem. 1966, 241, 4243–4250. [Google Scholar]
- Pontremoli, S.; Traniello, S.; Enser, M.; Shapiro, S.; Horecker, B.L. Regulation of fructose diphosphatase activity by disulfide exchange. Proc. Natl. Acad. Sci. USA 1967, 58, 286–293. [Google Scholar] [CrossRef]
- Czech, M.P. Current status of the thiol redox model for the regulation of hexose transport by insulin. J. Cell. Physiol. 1976, 89, 661–668. [Google Scholar] [CrossRef]
- Czech, M.P.; Lawrence, J.C.; Lynn, W.S. Evidence for the involvement of sulfhydryl oxidation in the regulation of fat cell hexose transport by insulin. Proc. Natl. Acad. Sci. USA 1974, 71, 4173–4177. [Google Scholar] [CrossRef]
- May, J.M.; de Haen, C. The insulin-like effect of hydrogen peroxide on pathways of lipid synthesis in rat adipocytes. J. Biol. Chem. 1979, 254, 9017–9021. [Google Scholar]
- McClung, J.P.; Roneker, C.A.; Mu, W.; Lisk, D.J.; Langlais, P.; Liu, F.; Lei, X.G. Development of insulin resistance and obesity in mice overexpressing cellular glutathione peroxidase. Proc. Natl. Acad. Sci. USA 2004, 101, 8852–8857. [Google Scholar] [CrossRef]
- Steinbrenner, H.; Klotz, L.-O. Glutathione peroxidase 1 as a modulator of insulin production and signaling. In Glutathione; Flohé, L., Ed.; CRC Press: Boca Raton, FL, USA, 2019; pp. 81–93. [Google Scholar]
- Eggleston, L.V.; Krebs, H.A. Regulation of the pentose phosphate cycle. Biochem. J. 1974, 138, 425–435. [Google Scholar] [CrossRef] [PubMed]
- Brigelius, R. Mixed disulfides: Biological functions and increase in oxidative stress. In Oxidative Stress, 1st ed.; Sies, H., Ed.; Academic Stress: London, UK; Orlando, FL, USA; San Diego, CA, USA; New York, NY, USA; Tornto, ON, Canada; Montreal, OC, Canada; Sydney, Australia; Tokyo, Japan, 1986; pp. 243–272. [Google Scholar]
- Fischer, E.H. Cellular regulation by protein phosphorylation: A historical overview. BioFactors 1997, 6, 367–374. [Google Scholar] [CrossRef] [PubMed]
- Shimazu, T.; Tokutake, S.; Usami, M. Inactivation of phosphorylase phosphatase by a factor from rabbit liver and its chemical characterization as glutathione disulfide. J. Biol. Chem. 1978, 253, 7376–7382. [Google Scholar] [PubMed]
- Flohé, L. Changing paradigms in thiology from antioxidant defense toward redox regulation. Methods Enzymol. 2010, 473, 1–39. [Google Scholar] [PubMed]
- Thannickal, V.J.; Fanburg, B.L. Reactive oxygen species in cell signaling. Am. J. Physiol. Lung Cell. Mol. Physiol. 2000, 279, L1005–L1028. [Google Scholar] [CrossRef] [PubMed]
- Finkel, T. Signal transduction by reactive oxygen species in non-phagocytic cells. J. Leukoc. Biol. 1999, 65, 337–340. [Google Scholar] [CrossRef] [PubMed]
- Finkel, T. Oxidant signals and oxidative stress. Curr. Opin. Cell Biol. 2003, 15, 247–254. [Google Scholar] [CrossRef]
- Baeuerle, P.A.; Baltimore, D. Nf-kappa B: Ten years after. Cell 1996, 87, 13–20. [Google Scholar] [CrossRef]
- Kretz-Remy, C.; Mehlen, P.; Mirault, M.E.; Arrigo, A.P. Inhibition of I kappa B-alpha phosphorylation and degradation and subsequent Nf-kappa B activation by glutathione peroxidase overexpression. J. Cell Biol. 1996, 133, 1083–1093. [Google Scholar] [CrossRef]
- Flohé, L.; Brigelius-Flohé, R.; Saliou, C.; Traber, M.G.; Packer, L. Redox regulation of Nf-kappa B activation. Free Radic. Biol. Med. 1997, 22, 1115–1126. [Google Scholar] [CrossRef]
- Sulciner, D.J.; Irani, K.; Yu, Z.X.; Ferrans, V.J.; Goldschmidt-Clermont, P.; Finkel, T. Rac1 regulates a cytokine-stimulated, redox-dependent pathway necessary for Nf-kappa B activation. Mol. Cell. Biol. 1996, 16, 7115–7121. [Google Scholar] [CrossRef] [PubMed]
- Thannickal, V.J.; Fanburg, B.L. Activation of an H2O2-generating NADH oxidase in human lung fibroblasts by transforming growth factor beta 1. J. Biol. Chem. 1995, 270, 30334–30338. [Google Scholar] [CrossRef] [PubMed]
- Sundaresan, M.; Yu, Z.X.; Ferrans, V.J.; Sulciner, D.J.; Gutkind, J.S.; Irani, K.; Goldschmidt-Clermont, P.J.; Finkel, T. Regulation of reactive-oxygen-species generation in fibroblasts by Rac1. Biochem. J. 1996, 318, 379–382. [Google Scholar] [CrossRef] [PubMed]
- Sundaresan, M.; Yu, Z.X.; Ferrans, V.J.; Irani, K.; Finkel, T. Requirement for generation of H2O2 for platelet-derived growth factor signal transduction. Science 1995, 270, 296–299. [Google Scholar] [CrossRef] [PubMed]
- Bae, Y.S.; Kang, S.W.; Seo, M.S.; Baines, I.C.; Tekle, E.; Chock, P.B.; Rhee, S.G. Epidermal growth factor (EGF)-induced generation of hydrogen peroxide. Role in EGF receptor-mediated tyrosine phosphorylation. J. Biol. Chem. 1997, 272, 217–221. [Google Scholar] [CrossRef] [PubMed]
- Di Meo, S.; Venditti, P. Evolution of the knowledge on free radicals and other oxidants. In Oxidative Medicine and Cellular Longevity; Hindawi: London, UK, 2020; p. 32. [Google Scholar]
- Greenberg, J.T.; Monach, P.; Chou, J.H.; Josephy, P.D.; Demple, B. Positive control of a global antioxidant defense regulon activated by superoxide-generating agents in Escherichia coli. Proc. Natl. Acad. Sci. USA 1990, 87, 6181–6185. [Google Scholar] [CrossRef] [PubMed]
- Tsaneva, I.R.; Weiss, B. SoxR, a locus governing a superoxide response regulon in Escherichia coli k-12. J. Bacteriol. 1990, 172, 4197–4205. [Google Scholar] [CrossRef]
- Dubbs, J.M.; Mongkolsuk, S. Peroxiredoxins in bacterial antioxidant defense. Sub Cell. Biochem. 2007, 44, 143–193. [Google Scholar]
- Brigelius-Flohé, R.; Friedrichs, B.; Maurer, S.; Schultz, M.; Streicher, R. Interleukin-1-induced nuclear factor kappa B activation is inhibited by overexpression of phospholipid hydroperoxide glutathione peroxidase in a human endothelial cell line. Biochem. J. 1997, 328, 199–203. [Google Scholar] [CrossRef]
- Nakashima, I.; Takeda, K.; Kawamoto, Y.; Okuno, Y.; Kato, M.; Suzuki, H. Redox control of catalytic activities of membrane-associated protein tyrosine kinases. Arch. Biochem. Biophys. 2005, 434, 3–10. [Google Scholar] [CrossRef]
- Itoh, K.; Chiba, T.; Takahashi, S.; Ishii, T.; Igarashi, K.; Katoh, Y.; Oyake, T.; Hayashi, N.; Satoh, K.; Hatayama, I.; et al. An Nrf2/small Maf heterodimer mediates the induction of phase II detoxifying enzyme genes through antioxidant response elements. Biochem. Biophys. Res. Commun. 1997, 236, 313–322. [Google Scholar] [CrossRef] [PubMed]
- Itoh, K.; Mimura, J.; Yamamoto, M. Discovery of the negative regulator of Nrf2, Keap1: A historical overview. Antioxid. Redox Signal. 2010, 13, 1665–1678. [Google Scholar] [CrossRef] [PubMed]
- Wasserman, W.W.; Fahl, W.E. Functional antioxidant responsive elements. Proc. Natl. Acad. Sci. USA 1997, 94, 5361–5366. [Google Scholar] [CrossRef] [PubMed]
- Rushmore, T.H.; Pickett, C.B. Transcriptional regulation of the rat glutathione S-transferase Ya subunit gene. Characterization of a xenobiotic-responsive element controlling inducible expression by phenolic antioxidants. J. Biol. Chem. 1990, 265, 14648–14653. [Google Scholar] [PubMed]
- Forman, H.J.; Davies, K.J.; Ursini, F. How do nutritional antioxidants really work: Nucleophilic tone and para-hormesis versus free radical scavenging in vivo. Free Radic. Biol. Med. 2014, 66, 24–35. [Google Scholar] [CrossRef] [PubMed]
- Stefanson, A.L.; Bakovic, M. Dietary regulation of Keap1/Nrf2/ARE pathway: Focus on plant-derived compounds and trace minerals. Nutrients 2014, 6, 3777–3801. [Google Scholar] [CrossRef]
- Saitoh, M.; Nishitoh, H.; Fujii, M.; Takeda, K.; Tobiume, K.; Sawada, Y.; Kawabata, M.; Miyazono, K.; Ichijo, H. Mammalian thioredoxin is a direct inhibitor of apoptosis signal-regulating kinase (ASK) 1. EMBO J. 1998, 17, 2596–2606. [Google Scholar] [CrossRef]
- Hayashi, T.; Funato, Y.; Terabayashi, T.; Morinaka, A.; Sakamoto, R.; Ichise, H.; Fukuda, H.; Yoshida, N.; Miki, H. Nucleoredoxin negatively regulates toll-like receptor 4 signaling via recruitment of flightless-i to myeloid differentiation primary response gene (88). J. Biol. Chem. 2010, 285, 18586–18593. [Google Scholar] [CrossRef]
- Funato, Y.; Miki, H. Nucleoredoxin, a novel thioredoxin family member involved in cell growth and differentiation. Antioxid. Redox Signal. 2007, 9, 1035–1057. [Google Scholar] [CrossRef]
- Toledano, M.B.; Delaunay, A.; Monceau, L.; Tacnet, F. Microbial H2O2 sensors as archetypical redox signaling modules. Trends Biochem. Sci. 2004, 29, 351–357. [Google Scholar] [CrossRef]
- Jeong, W.; Bae, S.H.; Toledano, M.B.; Rhee, S.G. Role of sulfiredoxin as a regulator of peroxiredoxin function and regulation of its expression. Free Radic. Biol. Med. 2012, 53, 447–456. [Google Scholar] [CrossRef] [PubMed]
- Toledano, M.B.; Huang, B. Microbial 2-Cys peroxiredoxins: Insights into their complex physiological roles. Mol. Cells 2016, 39, 31–39. [Google Scholar] [PubMed]
- Sjölander, J.J.; Tarczykowska, A.; Picazo, C.; Cossio, I.; Redwan, I.N.; Gao, C.; Solano, C.; Toledano, M.B.; Grotli, M.; Molin, M.; et al. A redox-sensitive thiol in Wis1 modulates the fission yeast mitogen-activated protein kinase response to H2O2 and is the target of a small molecule. Mol. Cell. Biol. 2020, 40. [Google Scholar] [CrossRef]
- Lee, B.C.; Peterfi, Z.; Hofmann, F.W.; Moore, R.E.; Kaya, A.; Avanesov, A.; Tarrago, L.; Zhou, Y.; Weerapana, E.; Formenko, D.E.; et al. Mrsb1 and micals regulate actin assembly and macrophage function via reversible stereospecfic methionine oxidation. Mol. Cell 2013, 51, 397–404. [Google Scholar] [CrossRef]
- Quijano, C.; Trujillo, M.; Castro, L.; Trostchansky, A. Interplay between oxidant species and energy metabolism. Redox Biol. 2016, 8, 28–42. [Google Scholar] [CrossRef]
- Egea, J.; Fabregat, I.; Frapart, Y.M.; Ghezzi, P.; Gorlach, A.; Kietzmann, T.; Kubaichuk, K.; Knaus, U.G.; Lopez, M.G.; Olaso-Gonzalez, G.; et al. European contribution to the study of ROS: A summary of the findings and prospects for the future from the COST Action BM1203 (EU-Ros). Redox Biol. 2017, 13, 94–162. [Google Scholar] [CrossRef]
- Planche, L.A. Note sur la sophistication de la résine de jalap et sur les moyens de la reconaitre. Bull. Pharm. 1810, 578–580. [Google Scholar]
- von Humboldt, F.W.H.A. Versuche über die Zerlegung des Luftkreises und über einige Gegenstände der Naturlehre; Vieweg: Braunschweig, Germany, 1799. [Google Scholar]
- Forman, H.J.; Augusto, O.; Brigelius-Flohé, R.; Dennery, P.A.; Kalyanaraman, B.; Ischiropoulos, H.; Mann, G.E.; Radi, R.; Roberts, L.J., II; Vina, J.; et al. Even free radicals should follow some rules: A guide to free radical research terminology and methodology. Free Radic. Biol. Med. 2015, 78, 233–235. [Google Scholar] [CrossRef]
- Sies, H.; Jones, D.A. Oxidative stress. In Encyclopedia of Stress, 2nd ed.; Fink, G., Ed.; Elsevier: Amsterdam, The Netherlands, 2007; Volume 3, pp. 45–48. [Google Scholar]
- Sies, H. Role of metabolic H2O2 generation: Redox signaling and oxidative stress. J. Biol. Chem. 2014, 289, 8735–8741. [Google Scholar] [CrossRef]
- Lushchak, V.I. Free radicals, reactive oxygen species, oxidative stresses and their classifications. Ukr. Biochem. J. 2015, 87, 11–18. [Google Scholar] [CrossRef]
- Halliwell, B.; Gutteridge, J.M.C. Free Radicals in Biology & Medicine, 5th ed.; Oxford University Press: Oxford, UK, 2015; p. 905. [Google Scholar]
- Sies, H.; Berndt, C.; Jones, D.P. Oxidative stress. Annu. Rev. Biochem. 2017, 86, 715–748. [Google Scholar] [CrossRef] [PubMed]
- Sies, H. Oxidative stress: Concept and some practical aspects. Antioxidants 2020, 9, 852. [Google Scholar] [CrossRef] [PubMed]
- Toppo, S.; Flohé, L.; Ursini, F.; Vanin, S.; Maiorino, M. Catalytic mechanisms and specificities of glutathione peroxidases: Variations of a basic scheme. Biochim. Biophys. Acta 2009, 1790, 1486–1500. [Google Scholar] [CrossRef] [PubMed]
- Trujillo, M.; Ferrer-Sueta, G.; Thomson, L.; Flohé, L.; Radi, R. Kinetics of peroxiredoxins and their role in the decomposition of peroxynitrite. Sub Cell. Biochem. 2007, 44, 83–113. [Google Scholar]
- Bielski, B.H.J.; Shiue, G.G. Reaction rates of superoxideradicals with essential amino acids. In Oxygen Free Radicals and Tissue Damage; Ciba FoundationSymposium 65 (new series); Birkhäuser: Amsterdam, The Netherlands; Oxford, UK; New York, NY, USA, 1979; Volume 65, pp. 43–56. [Google Scholar]
- Brigelius, R.; Hartmann, H.J.; Bors, W.; Saran, M.; Lengfelder, E.; Weser, U. Superoxide dismutase activity of Cu(tyr)2 and Cu, Co-erythrocuprein. Hoppe Seylers Z Physiol. Chem. 1975, 356, 739–745. [Google Scholar] [CrossRef]
- Beyer, H. Lehrbuch der Organischen Chemie, 11/12 ed.; S. Hirzel Verlag: Leipzig, Germany, 1968; p. 815. [Google Scholar]
- Klages, F. Lehrbuch der Organischen Chemie; Walter de Gruyter & Co: Berlin, Germany, 1958; Volume 1, p. 559. [Google Scholar]
- Moureau, C.; Dufraisse, C. Catalysis and auto-oxidation. Anti-oxygenig and pro-oxygenic activity. Chem. Rev. 1926, 3, 113–162. [Google Scholar] [CrossRef]
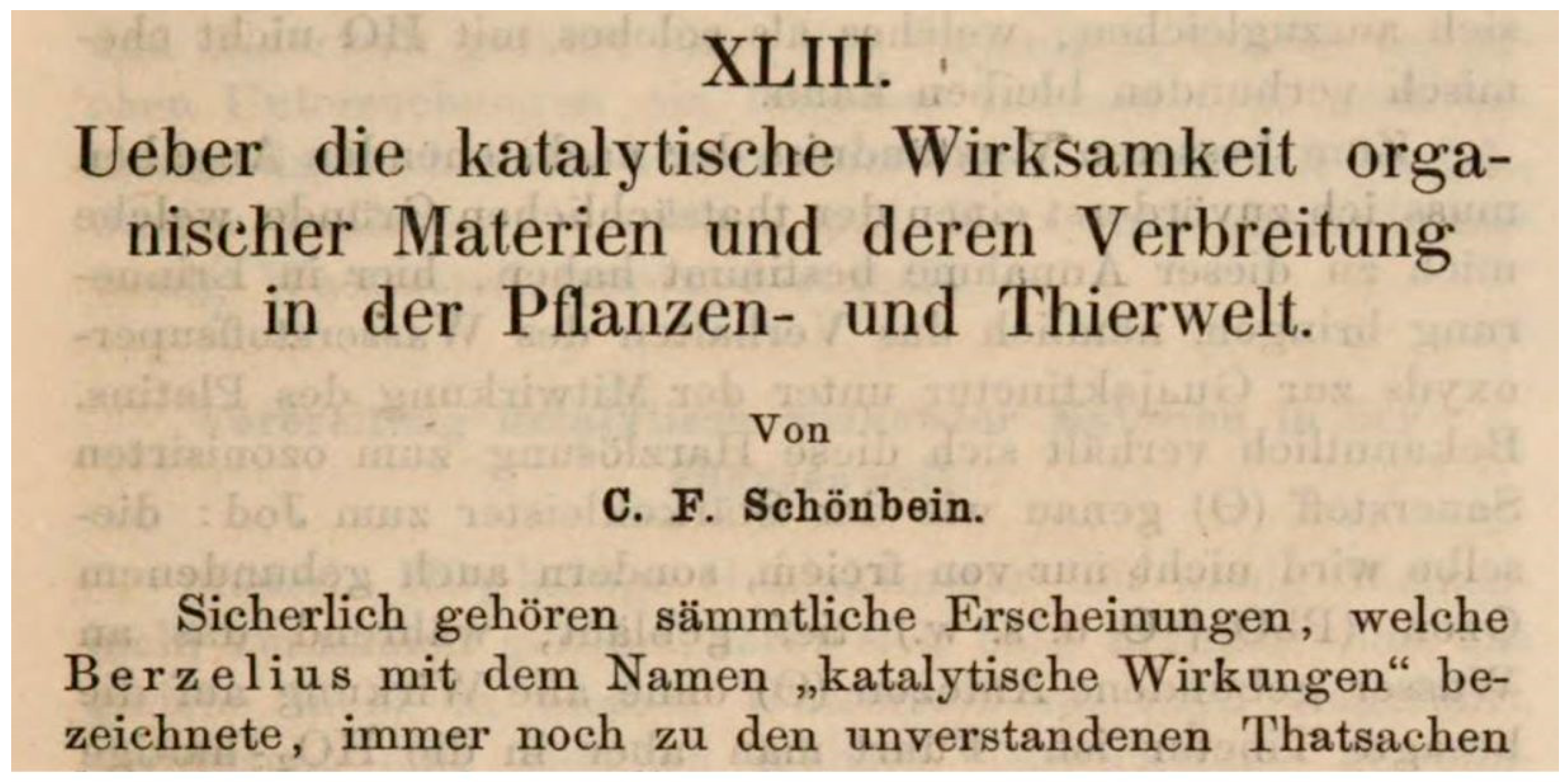
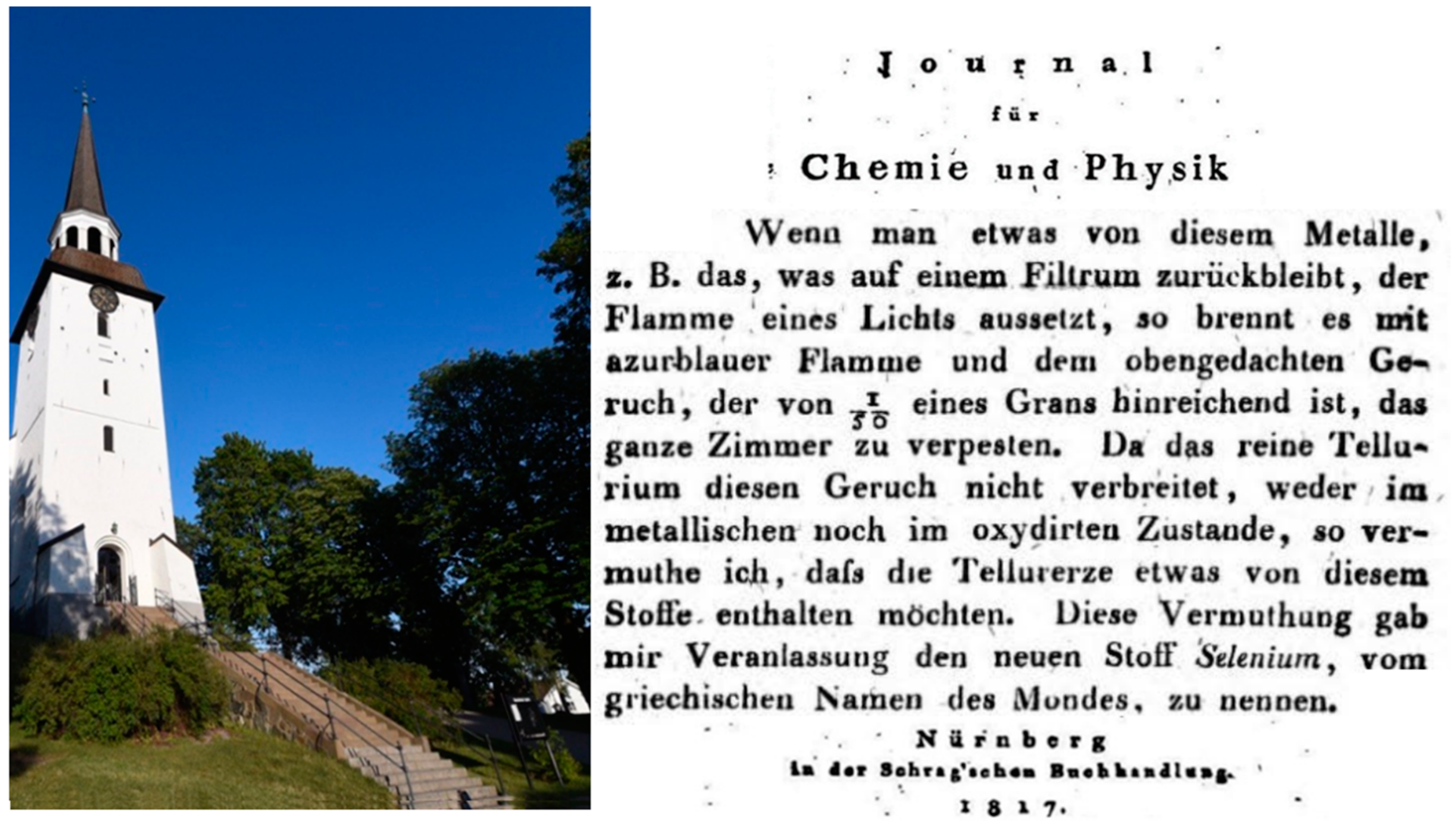
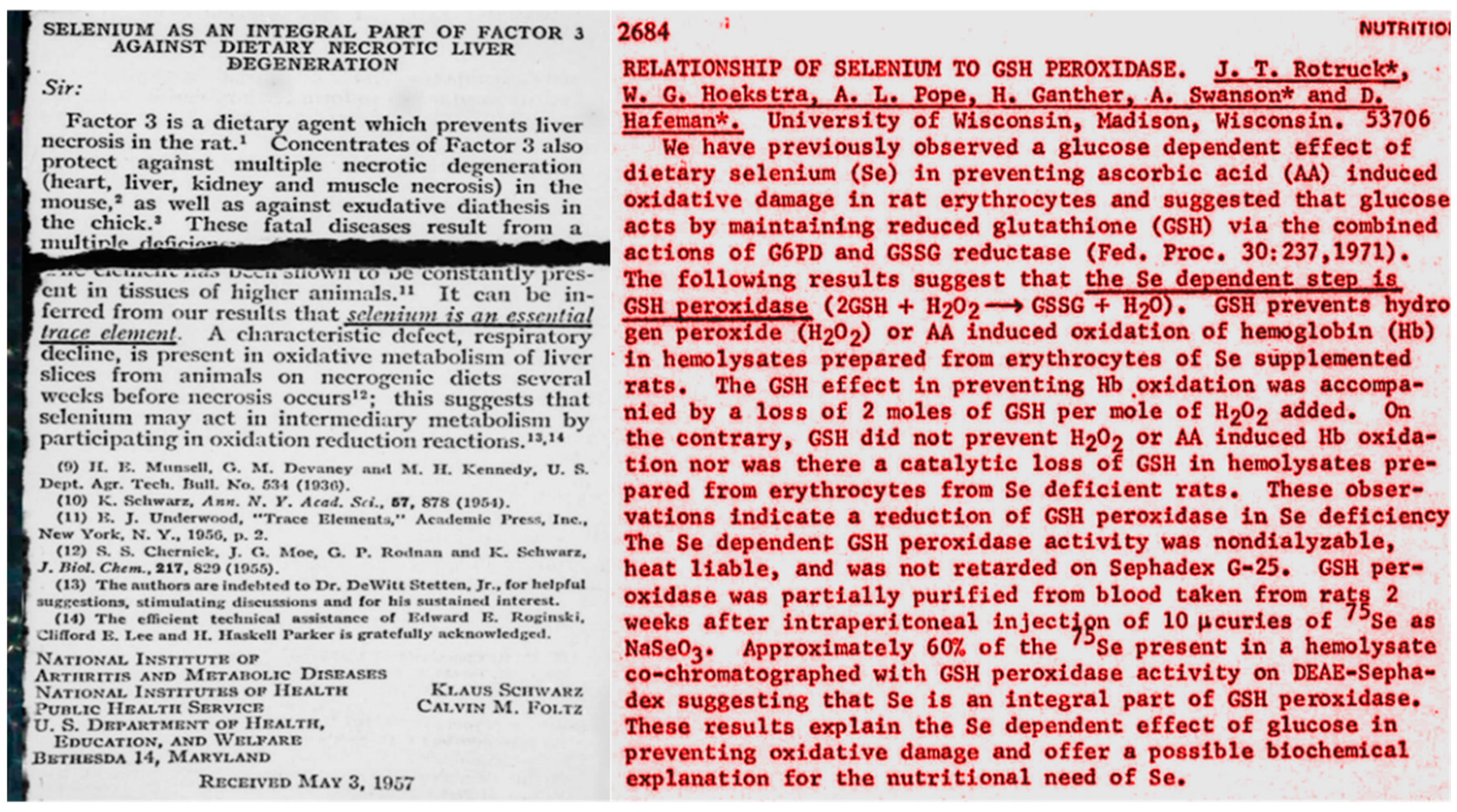
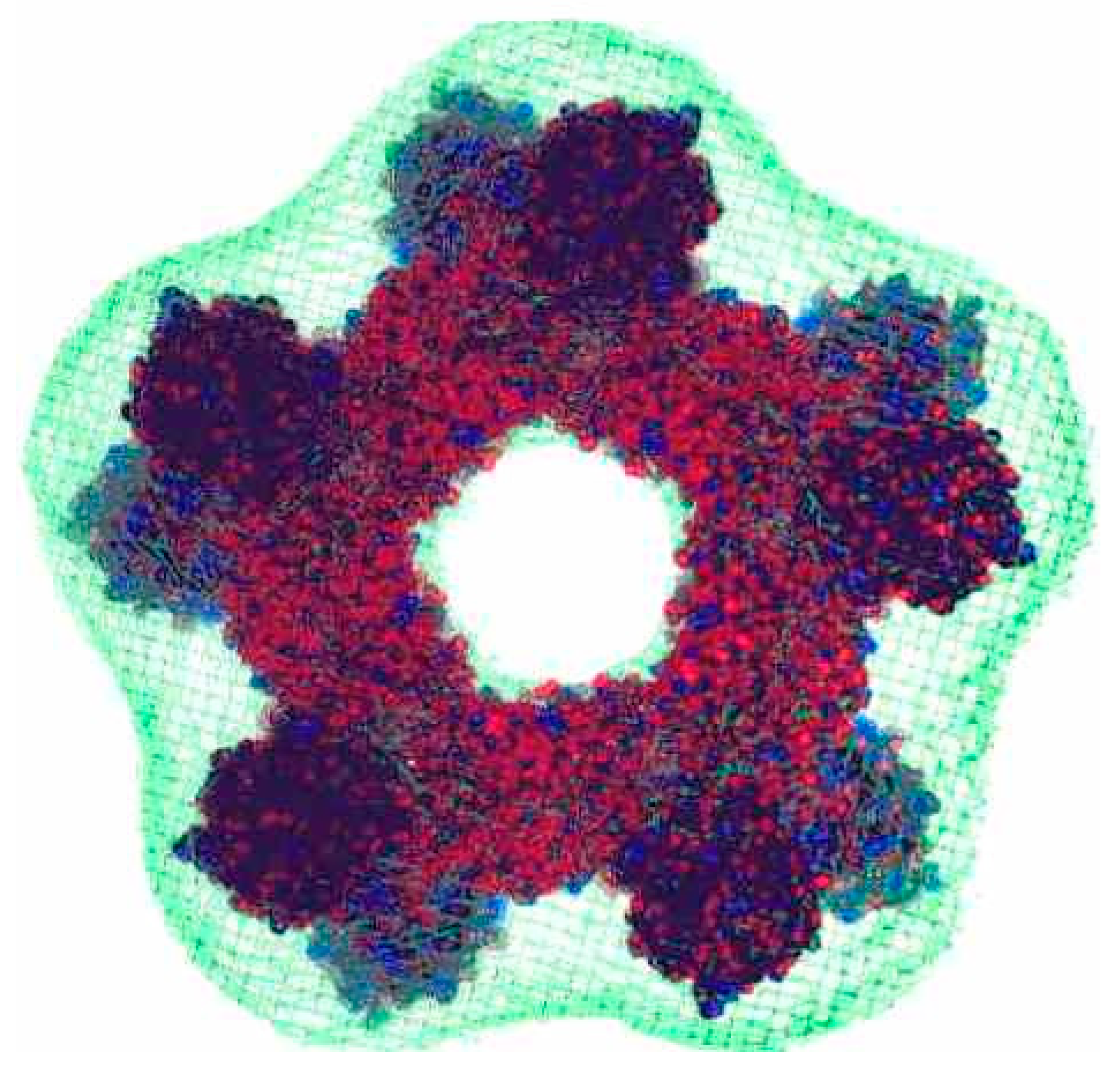
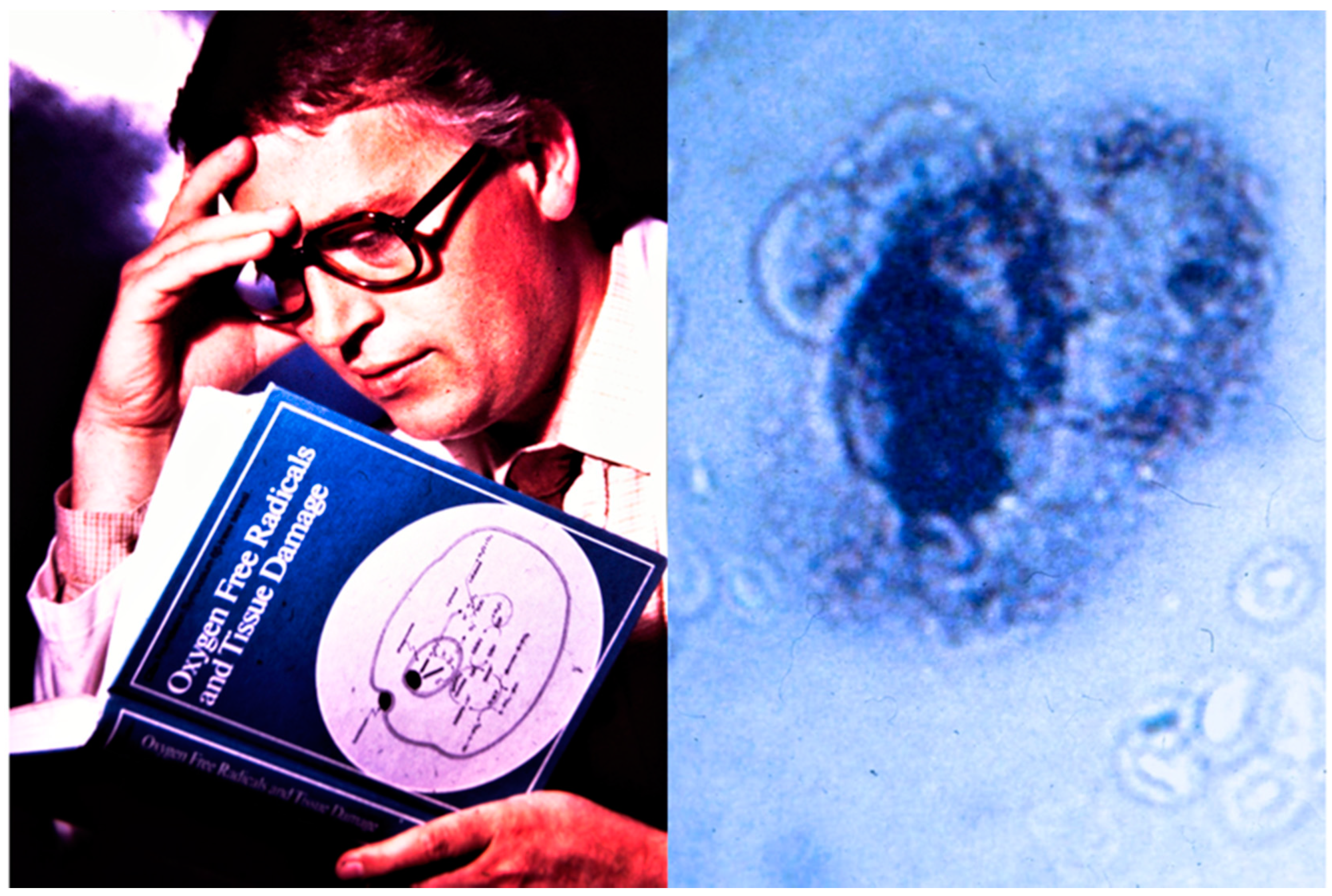
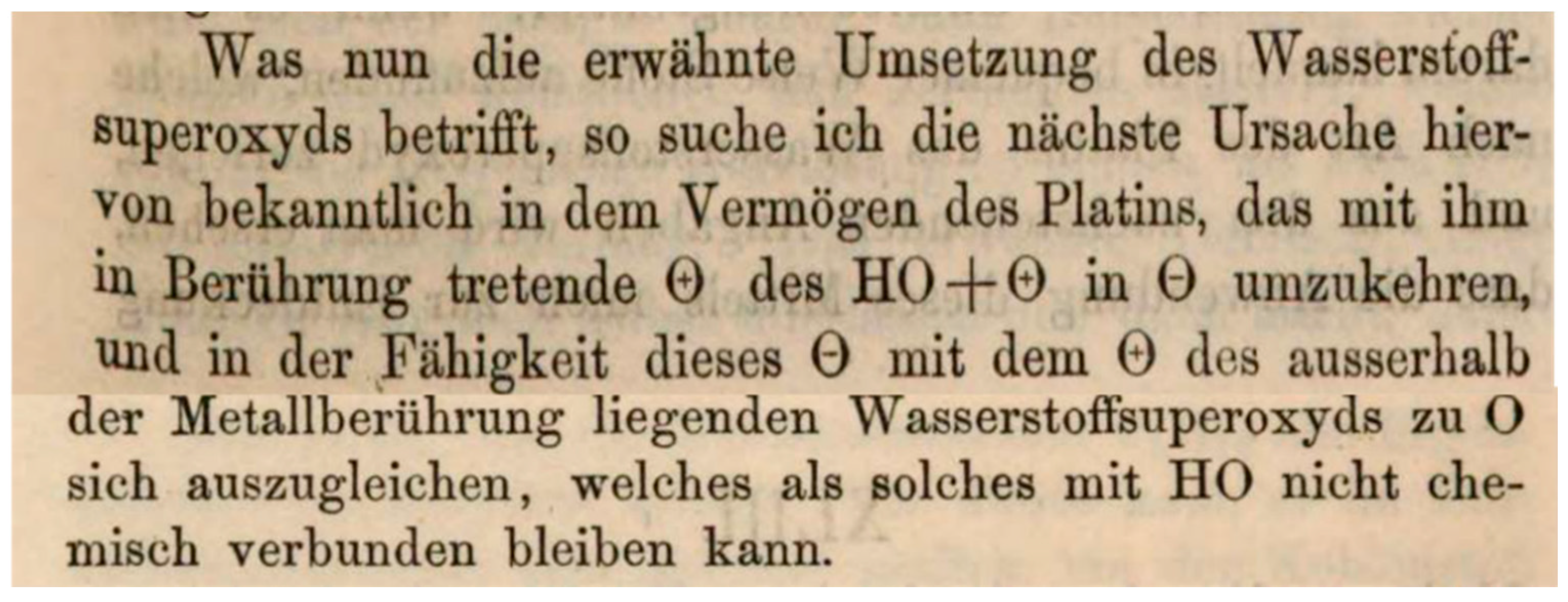
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Flohé, L. Looking Back at the Early Stages of Redox Biology. Antioxidants 2020, 9, 1254. https://doi.org/10.3390/antiox9121254
Flohé L. Looking Back at the Early Stages of Redox Biology. Antioxidants. 2020; 9(12):1254. https://doi.org/10.3390/antiox9121254
Chicago/Turabian StyleFlohé, Leopold. 2020. "Looking Back at the Early Stages of Redox Biology" Antioxidants 9, no. 12: 1254. https://doi.org/10.3390/antiox9121254
APA StyleFlohé, L. (2020). Looking Back at the Early Stages of Redox Biology. Antioxidants, 9(12), 1254. https://doi.org/10.3390/antiox9121254