The Impact of Punica granatum Linn and Its Derivatives on Oxidative Stress, Inflammation, and Endothelial Function in Diabetes Mellitus: Evidence from Preclinical and Clinical Studies
Abstract
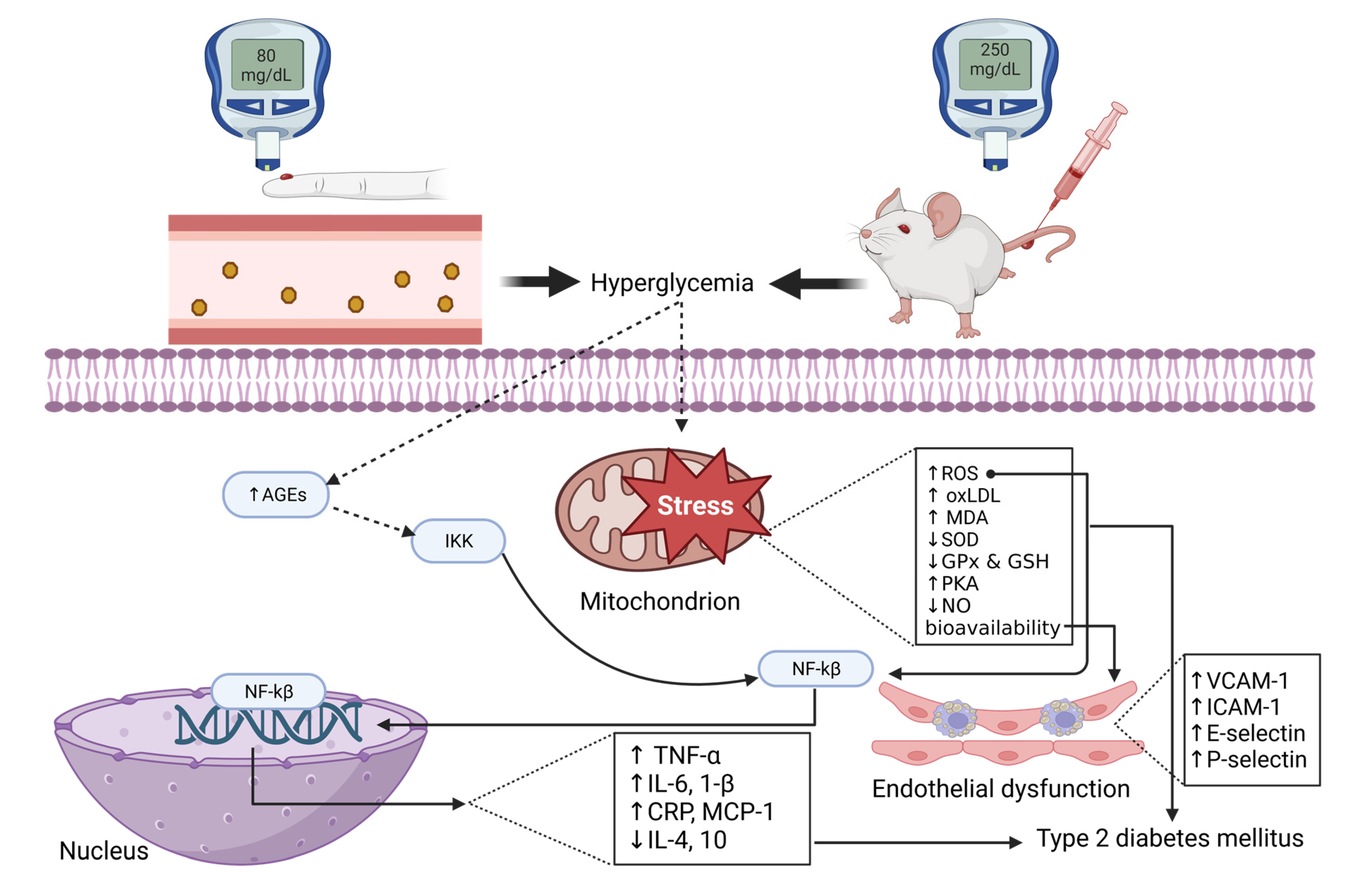
1. Introduction
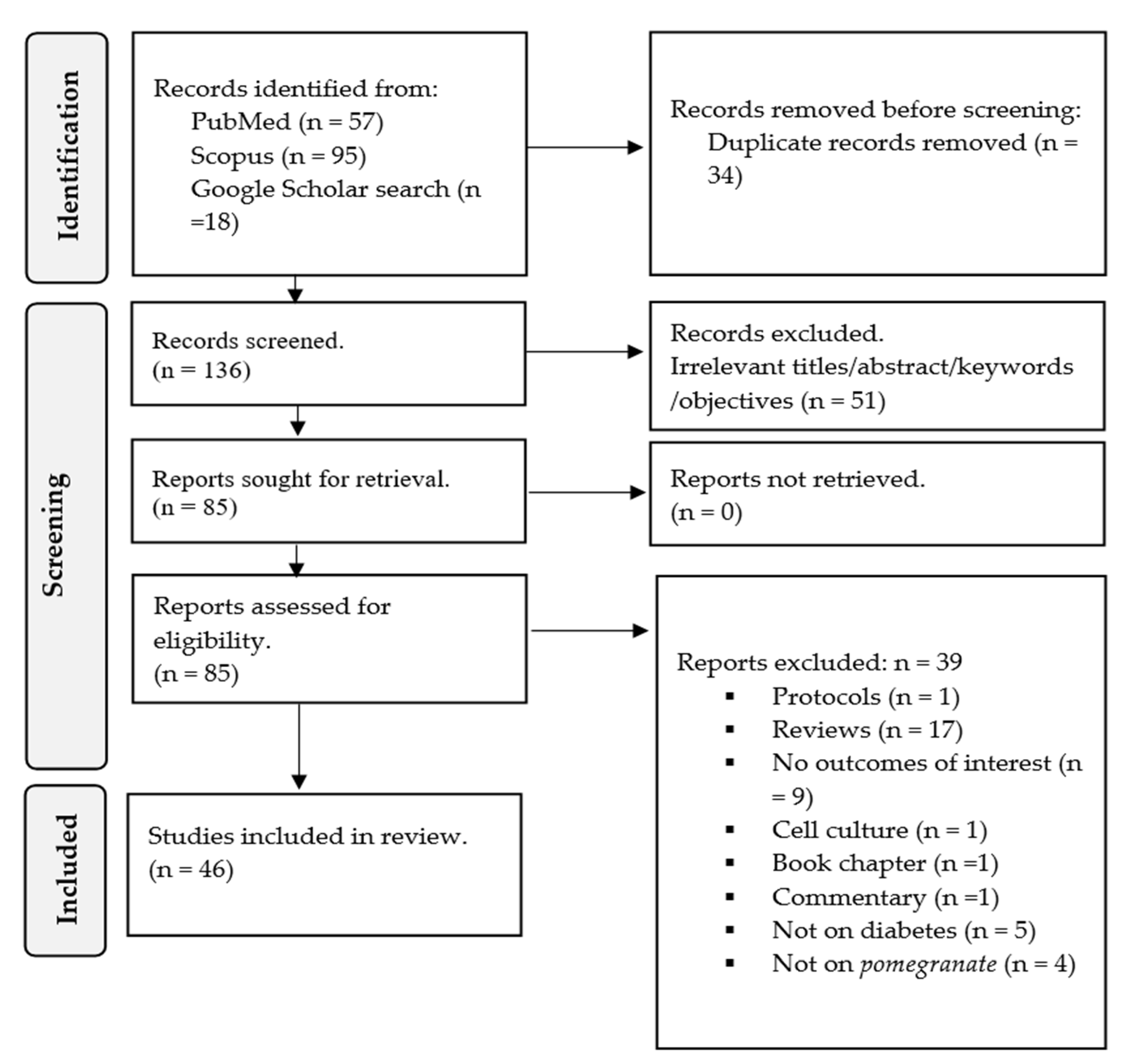
2. Methodology
2.1. Search Strategy
2.2. Study Selection
2.3. Data Extraction
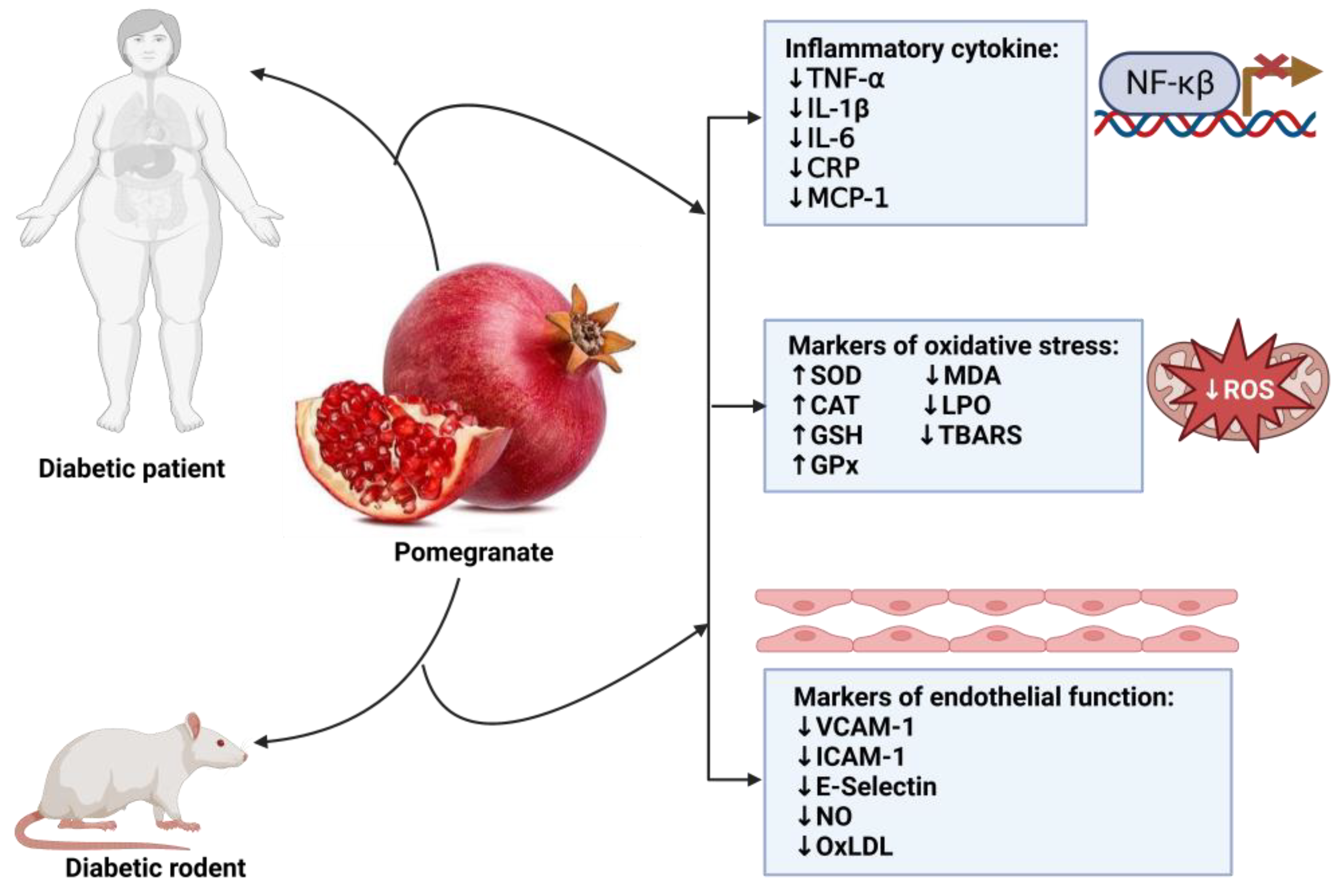
3. Results
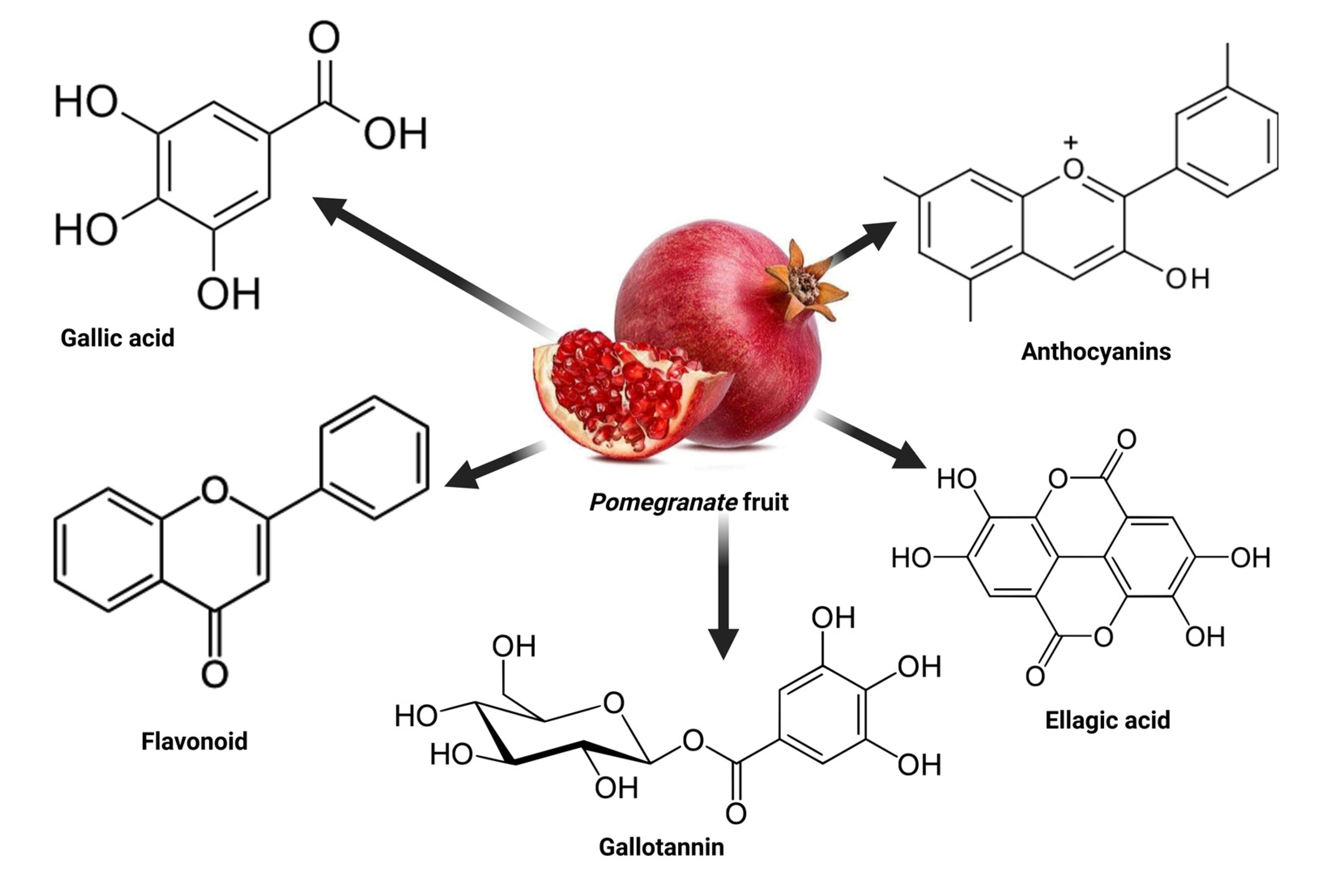
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- World Health Organisation. Diabetes. Available online: https://www.who.int/news-room/fact-sheets/detail/diabetes (accessed on 29 April 2023).
- Sun, H.; Saeedi, P.; Karuranga, S.; Pinkepank, M.; Ogurtsova, K.; Duncan, B.B.; Stein, C.; Basit, A.; Chan, J.C.N.; Mbanya, J.C.; et al. IDF Diabetes Atlas: Global, Regional and Country-Level Diabetes Prevalence Estimates for 2021 and Projections for 2045. Diabetes Res. Clin. Pract. 2022, 183, 109119. [Google Scholar] [CrossRef] [PubMed]
- Oguntibeju, O.O. Type 2 Diabetes Mellitus, Oxidative Stress and Inflammation: Examining the Links. Int. J. Physiol. Pathophysiol. Pharmacol. 2019, 11, 45–63. [Google Scholar] [PubMed]
- Baig, S.; Shabeer, M.; Parvaresh Rizi, E.; Agarwal, M.; Lee, M.H.; Ooi, D.S.Q.; Chia, C.; Aung, N.; Ng, G.; Teo, Y.; et al. Heredity of Type 2 Diabetes Confers Increased Susceptibility to Oxidative Stress and Inflammation. BMJ Open Diabetes Res. Care 2020, 8, e000945. [Google Scholar] [CrossRef] [PubMed]
- Pizzino, G.; Irrera, N.; Cucinotta, M.; Pallio, G.; Mannino, F.; Arcoraci, V.; Squadrito, F.; Altavilla, D.; Bitto, A. Oxidative Stress: Harms and Benefits for Human Health. Oxid. Med. Cell. Longev. 2017, 2017, 8416763. [Google Scholar] [CrossRef]
- Chaudhury, A.; Duvoor, C.; Reddy Dendi, V.S.; Kraleti, S.; Chada, A.; Ravilla, R.; Marco, A.; Shekhawat, N.S.; Montales, M.T.; Kuriakose, K.; et al. Clinical Review of Antidiabetic Drugs: Implications for Type 2 Diabetes Mellitus Management. Front. Endocrinol. 2017, 8, 6. [Google Scholar] [CrossRef]
- Padhi, S.; Nayak, A.K.; Behera, A. Type II Diabetes Mellitus: A Review on Recent Drug Based Therapeutics. Biomed. Pharmacother. 2020, 131, 110708. [Google Scholar] [CrossRef]
- Stumvoll, M.; Häring, H.U. Glitazones: Clinical Effects and Molecular Mechanisms. Ann. Med. 2002, 34, 217–224. [Google Scholar] [CrossRef] [PubMed]
- Lebovitz, H.E. Thiazolidinediones: The Forgotten Diabetes Medications. Curr. Diabetes Rep. 2019, 19, 151. [Google Scholar] [CrossRef]
- WHO. Supports Scientifically-Proven Traditional Medicine. Available online: https://www.afro.who.int/news/who-supports-scientifically-proven-traditional-medicine (accessed on 3 April 2023).
- Cock, I.E.; Ndlovu, N.; Van Vuuren, S.F. The Use of South African Botanical Species for the Control of Blood Sugar. J. Ethnopharmacol. 2021, 264, 113234. [Google Scholar] [CrossRef] [PubMed]
- Mokgalaboni, K.; Phoswa, W.N. Corchorus Olitorius Extract Exhibit Anti-Hyperglycemic and Anti-Inflammatory Properties in Rodent Models of Obesity and Diabetes Mellitus. Front. Nutr. 2023, 10, 1099880. [Google Scholar] [CrossRef]
- Fahmy, H.; Hegazi, N.; El-Shamy, S.; Farag, M.A. Pomegranate Juice as a Functional Food: A Comprehensive Review of Its Polyphenols, Therapeutic Merits, and Recent Patents. Food Funct. 2020, 11, 5768–5781. [Google Scholar] [CrossRef] [PubMed]
- Das, S.; Barman, S. Antidiabetic and Antihyperlipidemic Effects of Ethanolic Extract of Leaves of Punica granatum in Alloxan-Induced Non-Insulin-Dependent Diabetes Mellitus Albino Rats. Indian J. Pharmacol. 2012, 42, 219–224. [Google Scholar] [CrossRef]
- Venkitasamy, C.; Zhao, L.; Zhang, R.; Pan, Z. Pomegranate. In Integrated Processing Technologies for Food and Agricultural By-Products; Elsevier: Amsterdam, The Netherlands, 2019; pp. 181–216. ISBN 9780128141397. [Google Scholar]
- Aboonabi, A.; Rahmat, A.; Othman, F. Antioxidant Effect of Pomegranate against Streptozotocin-Nicotinamide Generated Oxidative Stress Induced Diabetic Rats. Toxicol. Rep. 2014, 1, 915–922. [Google Scholar] [CrossRef] [PubMed]
- Amri, Z.; Ben Khedher, M.R.; Zaibi, M.S.; Kharroubi, W.; Turki, M.; Ayadi, F.; Hammami, M. Anti-Diabetic Effects of Pomegranate Extracts in Long-Term High Fructose-Fat Fed Rats. Clin. Phytoscience 2020, 6, 55. [Google Scholar] [CrossRef]
- Sun, W.; Yan, C.; Frost, B.; Wang, X.; Hou, C.; Zeng, M.; Gao, H.; Kang, Y.; Liu, J. Pomegranate Extract Decreases Oxidative Stress and Alleviates Mitochondrial Impairment by Activating AMPK-Nrf2 in Hypothalamic Paraventricular Nucleus of Spontaneously Hypertensive Rats. Sci. Rep. 2016, 6, srep34246. [Google Scholar] [CrossRef]
- Onal, E.; Yilmaz, D.; Kaya, E.; Bastaskin, T.; Bayatli, N.; Gur, S. Pomegranate Juice Causes a Partial Improvement through Lowering Oxidative Stress for Erectile Dysfunction in Streptozotocin-Diabetic Rat. Int. J. Impot. Res. 2016, 28, 234–240. [Google Scholar] [CrossRef]
- Bagheri, S.; Khorramabadi, R.M.; Assadollahi, V.; Khosravi, P.; Cheraghi Venol, A.; Veiskerami, S.; Ahmadvand, H. The Effects of Pomegranate Peel Extract on the Gene Expressions of Antioxidant Enzymes in a Rat Model of Alloxan-Induced Diabetes. Arch. Physiol. Biochem. 2021, 129, 870–878. [Google Scholar] [CrossRef]
- Tugcu, B.; Nacaroglu, S.A.; Gedikbasi, A.; Uhri, M.; Acar, N.; Ozdemir, H. Protective Effect of Pomegranate Juice on Retinal Oxidative Stress in Streptozotocin-Induced Diabetic Rats. Int. J. Ophthalmol. 2017, 10, 1662–1668. [Google Scholar] [CrossRef]
- Wang, J.Y.; Zhu, C.; Qian, T.W.; Guo, H.; Wang, D.D.; Zhang, F.; Yin, X. Extracts of Black Bean Peel and Pomegranate Peel Ameliorate Oxidative Stress-Induced Hyperglycemia in Mice. Exp. Ther. Med. 2015, 9, 43–48. [Google Scholar] [CrossRef]
- Mollazadeh, H.; Sadeghnia, H.R.; Hoseini, A.; Farzadnia, M.; Boroushaki, M.T. Effects of Pomegranate Seed Oil on Oxidative Stress Markers, Serum Biochemical Parameters and Pathological Findings in Kidney and Heart of Streptozotocin-Induced Diabetic Rats. Ren. Fail. 2016, 38, 1256–1266. [Google Scholar] [CrossRef]
- Mohan, M.; Waghulde, H.; Kasture, S. Effect of Pomegranate Juice on Angiotensin II-Induced Hypertension in Diabetic Wistar Rats. Phytother. Res. 2010, 24, S196–S203. [Google Scholar] [CrossRef]
- Sohrab, G.; Ebrahimof, S.; Sotoudeh, G.; Neyestani, T.R.; Angoorani, P.; Hedayati, M.; Siasi, F. Effects of Pomegranate Juice Consumption on Oxidative Stress in Patients with Type 2 Diabetes: A Single-Blind, Randomized Clinical Trial. Int. J. Food Sci. Nutr. 2017, 68, 249–255. [Google Scholar] [CrossRef] [PubMed]
- Sohrab, G.; Angoorani, P.; Tohidi, M.; Tabibi, H.; Kimiagar, M.; Nasrollahzadeh, J. Pomegranate (Punicagranatum) Juice Decreases Lipid Peroxidation, but Has No Effect on Plasma Advanced Glycated End-Products in Adults with Type 2 Diabetes: A Randomized Double-Blind Clinical Trial. Food Nutr. Res. 2015, 59, 28551. [Google Scholar] [CrossRef] [PubMed]
- Jandari, S.; Hatami, E.; Ziaei, R.; Ghavami, A.; Yamchi, A.M. The Effect of Pomegranate (Punica granatum) Supplementation on Metabolic Status in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis. Complement. Ther. Med. 2020, 52, 102478. [Google Scholar] [CrossRef]
- Fuhrman, B.; Volkova, N.; Aviram, M. Pomegranate Juice Polyphenols Increase Recombinant Paraoxonase-1 Binding to High-Density Lipoprotein: Studies in Vitro and in Diabetic Patients. Nutrition 2010, 26, 359–366. [Google Scholar] [CrossRef]
- Rosenblat, M.; Hayek, T.; Aviram, M. Anti-Oxidative Effects of Pomegranate Juice (PJ) Consumption by Diabetic Patients on Serum and on Macrophages. Atherosclerosis 2006, 187, 363–371. [Google Scholar] [CrossRef]
- Parsaeyan, N.; Mozaffari-Khosravi, H.; Mozayan, M.R. Effect of Pomegranate Juice on Paraoxonase Enzyme Activity in Patients with Type 2 Diabetes. J. Diabetes Metab. Disord. 2012, 11, 11. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Zhang, Q.; Hou, H.; Liu, Z.; Wang, L.; Rasekhmagham, R.; Kord-Varkaneh, H.; Santos, H.O.; Yao, G. The Effects of Pomegranate Supplementation on Biomarkers of Inflammation and Endothelial Dysfunction: A Meta-Analysis and Systematic Review. Complement. Ther. Med. 2020, 49, 102358. [Google Scholar] [CrossRef]
- Morvaridzadeh, M.; Sepidarkish, M.; Daneshzad, E.; Akbari, A.; Mobini, G.R.; Heshmati, J. The Effect of Pomegranate on Oxidative Stress Parameters: A Systematic Review and Meta-Analysis. Complement. Ther. Med. 2020, 48, 102252. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Zhang, Y.; Tan, X.; Cao, Y.; An, X.; Chen, J.; Yang, L. Punicalagin Protects against Diabetic Liver Injury by Upregulating Mitophagy and Antioxidant Enzyme Activities. Nutrients 2022, 14, 2782. [Google Scholar] [CrossRef] [PubMed]
- Jin, D.; Zhang, B.; Li, Q.; Tu, J.; Zhou, B. Effect of Punicalagin on Multiple Targets in Streptozotocin/High-Fat Diet-Induced Diabetic Mice. Food Funct. 2020, 11, 10617–10634. [Google Scholar] [CrossRef]
- El-Beih, N.M.; Ramadan, G.; El-Husseiny, E.A.; Hussein, A.M. Effects of Pomegranate Aril Juice and Its Punicalagin on Some Key Regulators of Insulin Resistance and Oxidative Liver Injury in Streptozotocin-Nicotinamide Type 2 Diabetic Rats. Mol. Biol. Rep. 2019, 46, 3701–3711. [Google Scholar] [CrossRef] [PubMed]
- Mabrouk Gabr, N. Effects of Pomegranate (Punica granatum L.) Fresh Juice and Peel Extract on Diabetic Male Albino Rats. Al-Azhar Med. J. 2017, 46, 965–980. [Google Scholar] [CrossRef]
- Mosaoa, R.M.; Yaghmoor, S.S.; Moselhy, S.S. Oxygen Scavenging, Anti-Inflammatory, and Antiglycation Activity of Pomegranate Flavonoids (Punica granum) against Streptozotocin Toxicity Induced Diabetic Nephropathy in Rats. Environ. Sci. Pollut. Res. 2023, 30, 16687–16693. [Google Scholar] [CrossRef] [PubMed]
- Saad, E.A.; Hassanien, M.; Elhagrasy, M.; Saad, E.A.; Hassanien, M.M.; El-Hagrasy, M.A.; Radwan, K.H. Antidiabetic, Hypolipidemic and Antioxidant Activities and Protective Effects of Punica granatum Peels Powder against Pancreatic and Hepatic Tissues Injuries in Streptozotocin Induced IDDM in Rats. Int. J. Pharm. Pharm. Sci. 2015, 7, 397–402. [Google Scholar]
- Osman, H.F.; Eshak, M.G.; El-Sherbiny, M.; Bayoumi, M.M.; Hala; Osman, F. Biochemical and Genetical Evaluation of Pomegranate Impact on Diabetes Mellitus Induced by Alloxan in Female Rats Genetical Evaluation of Pomegranate Impact on Diabetes Mellitus Induced by Alloxan in Female Rats. Life Sci. J. 2012, 9, 1543–1553. [Google Scholar]
- El Deeb, K.S.; Eid, H.H.; Ali, Z.Y.; Shams, M.M.; Elfiky, A.M. Bioassay-Guided Fractionation and Identification of Antidiabetic Compounds from the Rind of Punica granatum Var. Nana. Nat. Prod. Res. 2021, 35, 2103–2106. [Google Scholar] [CrossRef]
- El-Missiry, M.A.; Amer, M.A.; Hemieda, F.A.E.; Othman, A.I.; Sakr, D.A.; Abdulhadi, H.L. Cardioameliorative Effect of Punicalagin against Streptozotocin-Induced Apoptosis, Redox Imbalance, Metabolic Changes and Inflammation. Egypt. J. Basic Appl. Sci. 2015, 2, 247–260. [Google Scholar] [CrossRef]
- Abo-Saif, M.A.; Ragab, A.E.; Ibrahim, A.O.; Abdelzaher, O.F.; Mehanyd, A.B.M.; Saber-Ayad, M.; El-Feky, O.A. Pomegranate Peel Extract Protects against the Development of Diabetic Cardiomyopathy in Rats by Inhibiting Pyroptosis and Downregulating LncRNA-MALAT1. Front. Pharmacol. 2023, 14, 1166653. [Google Scholar] [CrossRef]
- Shaker, O.G.; Sourour, D.A. Protective Effects of Pomegranate Seed Extract on Streptozotocin-Induced β-Cell Damage in Rats: Inhibition of Pancreatic Nuclear Factor Kappa Beta, Transforming Growth Factor Beta and Matrix Metalloproteinase-2 Genes Expression. Int. J. Adv. Res. 2013, 1, 88–102. [Google Scholar]
- Patel, A.N.; Bandawane, D.D.; Mhetre, N.K. Pomegranate (Punica granatum Linn.) Leaves Attenuate Disturbed Glucose Homeostasis and Hyperglycemia Mediated Hyperlipidemia and Oxidative Stress in Streptozotocin Induced Diabetic Rats. Eur. J. Integr. Med. 2014, 6, 307–321. [Google Scholar] [CrossRef]
- Ankita, P.; Deepti, B.; Nilam, M. Flavonoid Rich Fraction of Punica granatum Improves Early Diabetic Nephropathy by Ameliorating Proteinuria and Disturbed Glucose Homeostasis in Experimental Animals. Pharm. Biol. 2015, 53, 61–71. [Google Scholar] [CrossRef] [PubMed]
- Bagri, P.; Ali, M.; Aeri, V.; Bhowmik, M.; Sultana, S. Antidiabetic Effect of Punica granatum Flowers: Effect on Hyperlipidemia, Pancreatic Cells Lipid Peroxidation and Antioxidant Enzymes in Experimental Diabetes. Food Chem. Toxicol. 2009, 47, 50–54. [Google Scholar] [CrossRef] [PubMed]
- Salwe, K.J.; Sachdev, D.O.; Bahurupi, Y.; Kumarappan, M. Evaluation of Antidiabetic, Hypolipedimic and Antioxidant Activity of Hydroalcoholic Extract of Leaves and Fruit Peel of Punica granatum in Male Wistar Albino Rats. J. Nat. Sci. Biol. Med. 2015, 6, 56–62. [Google Scholar] [CrossRef]
- Mollazadeh, H.; Boroushaki, M.T.; Soukhtanloo, M.; Afshari, A.R.; Vahedi, M.M. Effects of Pomegranate Seed Oil on Oxidant/Antioxidant Balance in Heart and Kidney Homogenates and Mitochondria of Diabetic Rats and High Glucose-Treated H9c2 Cell Line. AJP 2017, 7, 317–333. [Google Scholar]
- Gharib, E.; Kouhsari, S.M.; Izad, M. Punica granatum L. Fruit Aqueous Extract Suppresses Reactive Oxygen Species-Mediated P53/P65/MiR-145 Expressions Followed by Elevated Levels of Irs-1 in Alloxan-Diabetic Rats. Cell J. 2018, 19, 520–527. [Google Scholar] [CrossRef]
- Prasetyastuti; Anthony, M.W.P.; Rahman, N.A.; Ngadikun; Sunarti. Hypoglycemic and Antioxidative Effects of Pomegranate (Punica granatum L.) Juice in Streptozotocin Induced Diabetic Rats. Pak. J. Nutr. 2014, 13, 567–572. [Google Scholar] [CrossRef]
- Rozenberg, O.; Howell, A.; Aviram, M. Pomegranate Juice Sugar Fraction Reduces Macrophage Oxidative State, Whereas White Grape Juice Sugar Fraction Increases It. Atherosclerosis 2006, 188, 68–76. [Google Scholar] [CrossRef]
- Abdulhadi, H.L.; Dabdoub, B.R.; Ali, L.H.; Othman, A.I.; Amer, M.E.; El-Missiry, M.A. Punicalagin Protects against the Development of Pancreatic Injury and Insulitis in Rats with Induced T1DM by Reducing Inflammation and Oxidative Stress. Mol. Cell Biochem. 2022, 477, 2817–2828. [Google Scholar] [CrossRef]
- Rouhi, S.Z.T.; Sarker, M.M.R.; Rahmat, A.; Alkahtani, S.A.; Othman, F. The Effect of Pomegranate Fresh Juice versus Pomegranate Seed Powder on Metabolic Indices, Lipid Profile, Inflammatory Biomarkers, and the Histopathology of Pancreatic Islets of Langerhans in Streptozotocin-Nicotinamide Induced Type 2 Diabetic Sprague-Dawley Rats. BMC Complement. Altern. Med. 2017, 17, 156. [Google Scholar] [CrossRef]
- Betanzos-Cabrera, G.; Guerrero-Solano, J.A.; Martínez-Pérez, M.M.; Calderón-Ramos, Z.G.; Belefant-Miller, H.; Cancino-Diaz, J.C. Pomegranate Juice Increases Levels of Paraoxonase1 (PON1) Expression and Enzymatic Activity in Streptozotocin-Induced Diabetic Mice Fed with a High-Fat Diet. Food Res. Int. 2011, 44, 1381–1385. [Google Scholar] [CrossRef]
- El-Mansi, A.A.; Al-Kahtani, M.A. Calcitriol and Punica granatum Extract Concomitantly Attenuate Cardiomyopathy of Diabetic Mother Rats and Their Neonates via Activation of Raf/MEK/ERK Signalling and Mitigation of Apoptotic Pathways. Folia Biol. 2019, 65, 70–87. [Google Scholar]
- Cambay, Z.; Baydas, G.; Tuzcu, M.; Bal, R. Pomegranate (Punica granatum L.) Flower Improves Learning and Memory Performances Impaired by Diabetes Mellitus in Rats. Acta Physiol. Hung. 2011, 98, 409–420. [Google Scholar] [CrossRef]
- Çukurova, Z.; Hergünsel, O.; Eren, G.; Gedikbaşi, A.; Uhri, M.; Demir, G.; Tekdöş, Y. The Effect of Pomegranate Juice on Diabetes-Related Oxidative Stress in Rat Lung. Turk. Klin. J. Med. Sci. 2012, 32, 444–452. [Google Scholar] [CrossRef]
- McFarlin, B.K.; Strohacker, K.A.; Kueht, M.L. Pomegranate Seed Oil Consumption during a Period of High-Fat Feeding Reduces Weight Gain and Reduces Type 2 Diabetes Risk in CD-1 Mice. Br. J. Nutr. 2009, 102, 54–59. [Google Scholar] [CrossRef]
- Rock, W.; Rosenblat, M.; Miller-Lotan, R.; Levy, A.P.; Elias, M.; Aviram, M. Consumption of Wonderful Variety Pomegranate Juice and Extract by Diabetic Patients Increases Paraoxonase 1 Association with High-Density Lipoprotein and Stimulates Its Catalytic Activities. J. Agric. Food Chem. 2008, 56, 8704–8713. [Google Scholar] [CrossRef]
- Shishehbor, F.; Shahi, M.M.; Zarei, M.; Saki, A.; Zakerkish, M.; Shirani, F.; Zare, M. Effects of Concentrated Pomegranate Juice on Subclinical Inflammation and Cardiometabolic Risk Factors for Type 2 Diabetes: A Quasi-Experimental Study. Int. J. Endocrinol. Metab. 2016, 14, e33835. [Google Scholar] [CrossRef]
- Sohrab, G.; Nasrollahzadeh, J.; Zand, H.; Amiri, Z.; Tohidi, M.; Kimiagar, M. Effects of Pomegranate Juice Consumption on Inflammatory Markers in Patients with Type 2 Diabetes: A Randomized, Placebo-Controlled Trial. J. Res. Med. Sci. 2014, 19, 215–220. [Google Scholar]
- Khajebishak, Y.; Payahoo, L.; Hamishehkar, H.; Alivand, M.; Alipour, M.; Solhi, M.; Alipour, B. Effect of Pomegranate Seed Oil on the Expression of PPAR-γ and pro-Inflammatory Biomarkers in Obese Type 2 Diabetic Patients. Nutr. Food Sci. 2019, 49, 854–865. [Google Scholar] [CrossRef]
- Yarmohammadi, M.; Mahjoub, S. Effects of Aerobic Exercise and Pomegranate Extract on Antioxidant Markers in Women Postmenopausal with Type 2 Diabetes. Hormozgan Med. J. 2017, 21, 129–137. [Google Scholar] [CrossRef]
- Sohrab, G.; Nasrollahzadeh, J.; Tohidi, M.; Zand, H.; Nikpayam, O. Pomegranate Juice Increases Sirtuin1 Protein in Peripheral Blood Mononuclear Cell from Patients with Type 2 Diabetes: A Randomized Placebo Controlled Clinical Trial. Metab. Syndr. Relat. Disord. 2018, 16, 446–451. [Google Scholar] [CrossRef] [PubMed]
- Kutan Fenercioglu, A.; Saler, T.; Genc, E.; Sabuncu, H.; Altuntas, Y. The Effects of Polyphenol-Containing Antioxidants on Oxidative Stress and Lipid Peroxidation in Type 2 Diabetes Mellitus without Complications. J. Endocrinol. Investig. 2010, 33, 118–124. [Google Scholar] [CrossRef] [PubMed]
- Grabež, M.; Škrbić, R.; Stojiljković, M.P.; Vučić, V.; Grujić, V.R.; Jakovljević, V.; Djuric, D.M.; Suručić, R.; Šavikin, K.; Bigović, D.; et al. A Prospective, Randomized, Double-Blind, Placebo-Controlled Trial of Polyphenols on the Outcomes of Inflammatory Factors and Oxidative Stress in Patients with Type 2 Diabetes Mellitus. Rev. Cardiovasc. Med. 2022, 23, 57. [Google Scholar] [CrossRef] [PubMed]
- Morton, J.F.; Dowling, C.F. Pomegranate. Available online: https://www.worldcat.org/title/Fruits-of-warm-climates/oclc/16947184 (accessed on 28 May 2023).
- Mphahlele, R.R.; Fawole, O.A.; Mokwena, L.M.; Opara, U.L. Effect of Extraction Method on Chemical, Volatile Composition and Antioxidant Properties of Pomegranate Juice. South Afr. J. Bot. 2016, 103, 135–144. [Google Scholar] [CrossRef]
- Maphetu, N.; Unuofin, J.O.; Masuku, N.P.; Olisah, C.; Lebelo, S.L. Medicinal Uses, Pharmacological Activities, Phytochemistry, and the Molecular Mechanisms of Punica granatum L. (Pomegranate) Plant Extracts: A Review. Biomed. Pharmacother. 2022, 153, 113256. [Google Scholar] [CrossRef]
- Bhosle, V.K.; Altit, G.; Autmizguine, J.; Chemtob, S. Drugs That Cause Significant Displacement of Bilirubin from Albumin in Vitro. In Fetal and Neonatal Physiology, 2-Volume Set; Elsevier: Amsterdam, The Netherlands, 2017; pp. 187–201.e3. ISBN 9780323352147. [Google Scholar]
- Lipińska, L.; Klewicka, E.; Sójka, M. Structure, Occurrence and Biological Activity of Ellagitannins: A General Review. Acta Sci. Pol. Technol. Aliment. 2014, 13, 289–299. [Google Scholar] [CrossRef]
- Rippin; Beniwal, V.; Sharma, A.; Singh, B.J.; Ramniwas, S.; Sak, K.; Kumar, S.; Sharma, A.K. Ginnalin A and Hamamelitannin: The Unique Gallotannins with Promising Anti-Carcinogenic Potential. Explor. Target. Antitumor Ther. 2023, 4, 208–216. [Google Scholar] [CrossRef]
- Falcão, L.; Araújo, M.E.M. Tannins Characterisation in New and Historic Vegetable Tanned Leathers Fibres by Spot Tests. J. Cult. Herit. 2011, 12, 149–156. [Google Scholar] [CrossRef]
- He, H.F. Recognition of Gallotannins and the Physiological Activities: From Chemical View. Front. Nutr. 2022, 9, 888892. [Google Scholar] [CrossRef]
- Rozadi, N.; Oktavia, S.; Fauziah, F. Pharmacological Activities of Punicalagin: A Review. J. Drug Deliv. Ther. 2022, 12, 148–155. [Google Scholar] [CrossRef]
- Esposto, S.; Veneziani, G.; Taticchi, A.; Urbani, S.; Selvaggini, R.; Sordini, B.; Daidone, L.; Gironi, G.; Servili, M. Chemical Composition, Antioxidant Activity, and Sensory Characterization of Commercial Pomegranate Juices. Antioxidants 2021, 10, 1381. [Google Scholar] [CrossRef] [PubMed]
- Benchagra, L.; Berrougui, H.; Islam, M.O.; Ramchoun, M.; Boulbaroud, S.; Hajjaji, A.; Fulop, T.; Ferretti, G.; Khalil, A. Antioxidant Effect of Moroccan Pomegranate (Punica granatum L. Sefri Variety) Extracts Rich in Punicalagin against the Oxidative Stress Process. Foods 2021, 10, 2219. [Google Scholar] [CrossRef] [PubMed]
- Akhavan, H.; Barzegar, M.; Weidlich, H.; Zimmermann, B.F. Phenolic Compounds and Antioxidant Activity of Juices from Ten Iranian Pomegranate Cultivars Depend on Extraction. J. Chem. 2015, 2015, 907101. [Google Scholar] [CrossRef]
- Peng, Y. Comparative Analysis of the Biological Components of Pomegranate Seed from Different Cultivars. Int. J. Food Prop. 2019, 22, 784–794. [Google Scholar] [CrossRef]
- Elfalleh, W. Total Phenolic Contents and Antioxidant Activities of Pomegranate Peel, Seed, Leaf and Flower. J. Med. Plants Res. 2012, 6, 4724–4730. [Google Scholar] [CrossRef]
- Takeda, Y.; Matoba, K.; Sekiguchi, K.; Nagai, Y.; Yokota, T.; Utsunomiya, K.; Nishimura, R. Endothelial Dysfunction in Diabetes. Biomedicines 2020, 8, 182. [Google Scholar] [CrossRef]
- Du Plooy, C.S.; Martha Cornelia Mels, C.; Huisman, H.W.; Kruger, R. The Association of Endothelin-1 with Markers of Oxidative Stress in a Biethnic South African Cohort: The SABPA Study. Hypertens. Res. 2017, 40, 189–195. [Google Scholar] [CrossRef]
- Gopal, N.; Maithilikarpagaselvi, N.; Rajendiran, A.; Srinivasan, A.R.; Gowda, P.; Subramanyam, V. Association of Endothelin-1 with Oxidative Stress and Inflammatory Response in Pre-Hypertensives. Cor Vasa 2019, 6, 562–566. [Google Scholar] [CrossRef]
- Wang, X.; Bao, W.; Liu, J.; Ouyang, Y.Y.; Wang, D.; Rong, S.; Xiao, X.; Shan, Z.L.; Zhang, Y.; Yao, P.; et al. Inflammatory Markers and Risk of Type 2 Diabetes: A Systematic Review and Meta-Analysis. Diabetes Care 2013, 36, 166–175. [Google Scholar] [CrossRef]
- Pradhan, A.D.; Manson, J.E.; Rifai, N.; Buring, J.E.; Ridker, P.M. C-Reactive Protein, Interleukin 6, and Risk of Developing Type 2 Diabetes Mellitus. JAMA 2002, 286, 327–334. [Google Scholar] [CrossRef]
- Moya, C.; Máñez, S. Paraoxonases: Metabolic Role and Pharmacological Projection. Naunyn Schmiedebergs Arch. Pharmacol. 2018, 391, 349–359. [Google Scholar] [CrossRef] [PubMed]
- Turk, H.M.; Sevinc, A.; Camci, C.; Cigli, A.; Buyukberber, S.; Savli, H.; Bayraktar, N. Plasma Lipid Peroxidation Products and Antioxidant Enzyme Activities in patients with Type 2 Diabetes Mellitus. Acta Diabetol. 2002, 39, 117–122. [Google Scholar] [CrossRef] [PubMed]
- Saparbekova, A.A.; Kantureyeva, G.O.; Kudasova, D.E.; Konarbayeva, Z.K.; Latif, A.S. Potential of Phenolic Compounds from Pomegranate (Punica granatum L.) by-Product with Significant Antioxidant and Therapeutic Effects: A Narrative Review. Saudi J. Biol. Sci. 2023, 30, 103553. [Google Scholar] [CrossRef]
- Melgarejo-Sánchez, P.; Núñez-Gómez, D.; Martínez-Nicolás, J.J.; Hernández, F.; Legua, P.; Melgarejo, P. Pomegranate Variety and Pomegranate Plant Part, Relevance from Bioactive Point of View: A Review. Bioresour. Bioprocess. 2021, 8, 2. [Google Scholar] [CrossRef]
- Gumienna, M.; Szwengiel, A.; Górna, B. Bioactive Components of Pomegranate Fruit and Their Transformation by Fermentation Processes. Eur. Food Res. Technol. 2016, 242, 631–640. [Google Scholar] [CrossRef]
- Harakeh, S.; Qari, M.; Rajeh, N.; Ali, S.; El-Shitany, N.; Hassan, S.; Abd-Allah, E.A.; Tashkandi, H.; Malik, M.F.A.; Aljabri, F.K.; et al. Ellagic Acid Nanoparticles Attenuate Oxidative Stress and Testicular Damage in High Fat Diet/Streptozotocin-Induced Diabetic Rats. J. King Saud Univ. Sci. 2022, 34, 101720. [Google Scholar] [CrossRef]
- Rao, F.; Tian, H.; Li, W.; Hung, H.; Sun, F. Potential Role of Punicalagin against Oxidative Stress Induced Testicular Damage. Asian J. Androl. 2016, 18, 627–632. [Google Scholar] [CrossRef]
- Xu, J.; Cao, K.; Liu, X.; Zhao, L.; Feng, Z.; Liu, J. Punicalagin Regulates Signaling Pathways in Inflammation-Associated Chronic Diseases. Antioxidants 2022, 11, 29. [Google Scholar] [CrossRef]
- Wang, Y.; Huang, M.; Yang, X.; Yang, Z.; Li, L.; Mei, J. Supplementing Punicalagin Reduces Oxidative Stress Markers and Restores Angiogenic Balance in a Rat Model of Pregnancy-Induced Hypertension. Korean J. Physiol. Pharmacol. 2018, 22, 409–417. [Google Scholar] [CrossRef]
- Martins, I.C.V.S.; Maciel, M.G.; do Nascimento, J.L.M.; Mafra, D.; Santos, A.F.; Padilha, C.S. Anthocyanins-Rich Interventions on Oxidative Stress, Inflammation and Lipid Profile in Patients Undergoing Hemodialysis: Meta-Analysis and Meta-Regression. Eur. J. Clin. Nutr. 2023, 77, 316–324. [Google Scholar] [CrossRef] [PubMed]
- Speer, H.; D’Cunha, N.M.; Alexopoulos, N.I.; McKune, A.J.; Naumovski, N. Anthocyanins and Human Health—A Focus on Oxidative Stress, Inflammation and Disease. Antioxidants 2020, 9, 366. [Google Scholar] [CrossRef]
- Kostka, T.; Ostberg-Potthoff, J.J.; Briviba, K.; Matsugo, S.; Winterhalter, P.; Esatbeyoglu, T. Pomegranate (Punica granatum L.) Extract and Its Anthocyanin and Copigment Fractions—Free Radical Scavenging Activity and Influence on Cellular Oxidative Stress. Foods 2020, 9, 1617. [Google Scholar] [CrossRef] [PubMed]
- Hou, D.X.; Yanagita, T.; Uto, T.; Masuzaki, S.; Fujii, M. Anthocyanidins Inhibit Cyclooxygenase-2 Expression in LPS-Evoked Macrophages: Structure-Activity Relationship and Molecular Mechanisms Involved. Biochem. Pharmacol. 2005, 70, 417–425. [Google Scholar] [CrossRef] [PubMed]
- Poznyak, A.V.; Nikiforov, N.G.; Markin, A.M.; Kashirskikh, D.A.; Myasoedova, V.A.; Gerasimova, E.V.; Orekhov, A.N. Overview of OxLDL and Its Impact on Cardiovascular Health: Focus on Atherosclerosis. Front. Pharmacol. 2021, 11, 613780. [Google Scholar] [CrossRef] [PubMed]
| Author, Country | Experimental Model | Intervention and Duration | Main Findings |
|---|---|---|---|
| Rozenberg et al. [52] Israel | Streptozotocin (STZ)-induced diabetes in male Balb/C mice. | Diabetic rats were treated with pomegranate juice (PJ) as drinking water as a sugar fraction for ten days. | PJ sugars treatment significantly decreased macrophage peroxides and increased macrophagic glutathione (GSH). |
| McFarlin et al. [59] USA | Wild-type CD-1 male mice fed a high-fat diet (HFD). | HFD mice were treated with 61.79 mg of pomegranate for 14 weeks. | Treatment with pomegranate oil resulted in no significant difference in C-reactive protein (CRP). |
| Bagri et al. [47] India | STZ-induced diabetes in male albino Wistar rats. | 500 g of powdered pomegranate (250 mg/kg and 500 mg/kg) were administered orally in an aqueous solution (3% v/v, 80 in water) for 21 days. | The treatment of diabetic rats with aqueous pomegranate (250 and 500 mg/kg) markedly decreased pancreatic thiobarbituric acid reactive substances (TBARS) and malondialdehyde (MDA) and increased glutathione peroxide (GPx), GSH, catalases (CAT), and superoxide dismutase (SOD) activity. |
| Mohan et al. [24] India | STZ-induced diabetes in male albino Wistar rats. | 1 kilogram of pomegranates: the seeds were grounded to obtain juice. The concentration of the extracts was dissolved in distilled water. Diabetic rats were treated with PJ at (100 or 300 mg/kg) for four weeks. | Treatments significantly increased GSH, CAT, and SOD and decreased TBARS. |
| Betanzos-Cabrera et al. [55] Mexico | STZ-induced diabetes in mice fed with a high-fat diet (HFD). | Fresh PJ was prepared by diluting 12.5 mL/L in 1 L of water to make 0.35 mmol. The diluted PJ was given to the mice orally in their drinking water for four months. | Treatments significantly increased paraoxonase-1 (PON1) gene expression and its activity. |
| Cambay et al. [57] Turkey | STZ-induced diabetes in albino Wistar rats. | Ground powder of pomegranate flowers (PGFs) and powdered rat feed were mixed to make rat pellet feed. Diabetic rats were fed the mixed pellet as PGFs at 300, 400, and 500 mg/kg for eight weeks. | PGF treatment significantly decreased lipid peroxidation (LPO) and increased GSH levels. |
| Çukurova et al. [58] Turkey | STZ-induced diabetes in Sprague Dawley rats. | Pomegranates were washed, crushed, and squeezed to make PJ. Concentrated PJ was diluted in water (20 mL of concentrated juice in 500 mL of distilled water) to make 2.5 mL diluted PJ. Diabetic rats were treated with PJ for ten weeks. | PJ treatment significantly decreased endothelial nitric oxide synthase (eNOS) expression and increased SOD without significant changes in GSH. |
| Osman et al. [40] Egypt | Alloxan-induced diabetes in female albino rats. | Pomegranate peel dried and ground to powder (250 mg/kg). Seeds were used to make fresh juice (5 mL/kg). Diabetic rats were treated orally fed 250 PP mg/kg PP mixed with diet and oral PJ at 5 mL/kg) daily for four weeks. | Treatment with both regimens significantly increased total antioxidant capacity (TAC). |
| Shaker et al. [44] Egypt | STZ-induced diabetes in male Wistar rats. | Pomegranate seed extract (PSE), grounded to powder and dissolved in distilled water to form PSE (300 mg/kg/day), was given orally by gavage for four weeks. | PSE significantly decreased the pancreatic expression of nuclear factor kappa-beta (NF-κβ) and increased pancreatic GSH content. |
| Aboonabi et al. [16] Malaysia | STZ-nicotinamide (NAD)-induced diabetes in male Sprague Dawley rats. | The red pomegranate fruit was washed and peeled, and the arils were crushed and squeezed to make juice (1 mL of juice). The pomegranate seeds (PSs) were freeze-dried and ground into powder. The powder was dissolved into distilled water (100 mg of PSs + 1 mL DW). Pomegranate juice–seed (1 mL of PJ + 100 mg of PS) Diabetic rats were treated orally with pomegranate seeds and juice for 21 days. | Treatment with pomegranate significantly increased the enzymatic antioxidants, including CAT, SOD, and TAC, and decreased MDA in the plasma. |
| Patel et al. [45] India | STZ-induced diabetes in Wistar rat. | The leaf powder (100 g) was dissolved into methanol: water (70:30) for 72 h to obtain the hydroalcoholic extract. Diabetic rats were treated via oral route using an oral feeding needle once with 50, 100, and 200 mg/kg of ethyl acetate fraction of Punica granatum Linn. Leaves (EAPG) for 28 days. | EAPG significantly decreased MDA, pronounced at 200 mg/kg, while GSH, CAT, and SOD increased. |
| Praseytastuti et al. [51] Indonesia | STZ-induced diabetes in Sprague Dawley rats | Diabetic rats were treated orally with 1, 2, and 4 mL/200 g of PJ for four weeks. | Treatment with 2 mL/200 g of PJ significantly decreased MDA. |
| Ankita et al. [46] India | STZ-induced diabetes Wistar rats. | Leaf powder (100 g) was dissolved in methanol: water (70:30) for 72 h to obtain a hydroalcoholic extract. Diabetic rats were treated with a flavonoid-rich fraction of pomegranate leaves (PGFF) at 50, 100, and 200 mg/kg for 28 days. | PGFF significantly decreased MDA, pronounced at 200 mg/kg, while GSH, CAT, and increased SOD. |
| El-Missiry et al. [42] Egypt | STZ-induced diabetes in male Wistar rats. | Punicalagin (PU) powder dissolved in 0.2 mL saline solution and was intraperitoneally administered at 1 mg/kg daily for 15 days. | PU treatment significantly decreased tumor necrosis factor-alpha (TNF-α), interleukin-6 (IL-6), and MDA while increasing interleukin-1-beta (IL-1β), GSH, CAT, and SOD. |
| Salwe et al. [48] India | STZ-induced diabetes in male Wistar rats. | 40 g of dried powder dissolved in 95% ethanol to make a hydroalcoholic extract. Leaf extract 100 and 200 mg/kg of pomegranate, fruit peel extract 100 mg/kg, and peel extract 200 mg/kg of pomegranate. | Treatment significantly increased SOD and CAT while decreasing TBARS. |
| Saad et al. [39] Egypt | STZ-induced insulin-dependent diabetes mellitus (IDDM) in male Swiss Albino rats. | Dried pomegranate peels were grounded into a fine powder, dissolved in distilled water (100 mg/1 mL), and given orally through the stomach tube to rats at a 200 mg/kg dose for 20 days. | Pomegranate peel powder significantly increased SOD and TAC, while MDA and nitric oxide (NO) decreased. |
| Wang et al. [22] China | STZ-induced diabetes in male Kunming mice. | Diabetic rats were treated with 400 mg/kg of PPE via oral gavage for four weeks. | Treatment significantly increased anti-oxidative activity, GSH, and TAC. |
| Mollazadeh et al. [23] Iran | STZ-induced diabetes in male Wistar rats. | Diabetic rats were orally treated daily with pomegranate seed oil (PSO) at 0.4 and 0.8 mg/kg for 28 days. | PSO at both concentrations significantly increased total thiol content and decreased MDA levels in the heart and kidneys. |
| Onal et al. [19] Turkey | STZ-induced diabetes in male Sprague Dawley rats. | Diabetic rats were treated with PJ at 100 mg kg for ten weeks. | Treatment with PJ significantly decreased MDA levels without significant changes in inducible nitric oxide synthase (iNOS) and endothelial nitric oxide synthase (eNOS) protein. |
| Mollazadeh et al. [49] Iran | STZ-induced diabetes in male Wistar rats. | PSO dissolved in dimethyl sulfoxide, and the rats were treated orally with PSO at 0.4 and 0.8 mL/kg for three weeks. | PSO treatment significantly increased CAT, SOD, and GPx activity and decreased oxidative stress index values in tissue and mitochondrial fractions. |
| Rouhi et al. [54] Malaysia | STZ-NAD-induced diabetes in male Sprague Dawley rats. | The rats were orally treated with 1 mL of PJ or 100 mg of pomegranate seed powder (PS) in 1 mL distilled water for 21 days. | Treatment significantly ameliorated inflammation by decreasing inflammatory markers such as TNF-α, NF-κβ, and IL-6. |
| Gabr et al. [37] Egypt | Alloxan-induced diabetes in male albino rats. | PJ or peel extract at 500 mg/kg orally for four weeks. | Treatment with either juice or seed extract increased CAT and decreased MDA levels. |
| Tugcu et al. [21] Turkey | STZ-induced diabetes in Sprague Dawley rats. | PJ of 20 mL concentrated juice in 500 mL of distilled water to make 100 μL. PJ treatment was administered at 100 μL through gastric gavage for ten weeks. | Treatment significantly increased GSH and GPx and decreased MDA without changes in SOD. |
| Gharib et al. [50] Iran | Alloxan monohydrate induced diabetes in Wistar rats. | Pomegranate fruit aqueous extract (PGE) orally with PGE for 21 days. Treated with 100, 200, and 350 mg/kg of PGE. | Treatment significantly reduced ROS generation. |
| El-Beih et al. [36] Egypt | STZ-NAD-induced diabetes in male Wistar albino rats. | Diabetic rats received pomegranate aril juice (PAJ) daily at 100 or 300 mg of PAJ/kg orally for six weeks. | PAJ at both concentrations significantly decreased MDA and NADPH oxidase (NOx) levels and increased GPx, GSH, SOD, and CAT. |
| El-Mans et al. [56] Saudi Arabia | STZ-induced diabetes in female Sprague Dawley rats. | 50 g of pomegranate powder dissolved in 500 mL of methanol. Diabetic rats received 150 mg/kg/daily by gavage for 18 days. | IL-1β, IL-6, and endothelin-1 (ET-1) significantly decreased compared to the untreated diabetic group. Pomegranate in diabetic mothers and embryos significantly decreased the actvity of MDA and GPx and increased that of CAT and SOD. |
| Jin et al. [35] China | HFD-STZ-induced diabetes in C57BL/6J mice. | Punicalagin at 100, 150, and 200 mg/kg doses were administered daily through oral gavage for four weeks. | Treatment significantly decreased IL-6, TNF-α, and MCP-1 mRNA expression. |
| El-Deeb et al. [41] Egypt | STZ-NAD-induced diabetes in male albino Sprague Dawley rats. | 850 g of pomegranate powder dissolved in 95% ethanol (10 × 1 L). Diabetic rats were treated orally with 200 mg/ kg of ethanolic extract for four weeks. | TNF-α, IL-6, and MDA decreased; NO, TAC, and GSH increased. |
| Abdulhadi et al. [53] Iraq | STZ-induced diabetes in male Wistar rats. | Diabetic rats received an intraperitoneal injection of PU at 1 mg/kg for 15 days. | PU significantly decreased the level of intercellular adhesion molecules-1 (ICAM-1), vascular adhesion molecule-1 (VCAM-1), E-selectin, CRP, monocyte chemoattractant protein-1 (MCP-1), protein, LPO and MDA while increasing the activities of GPx, SOD, GSH, and PON1 in serum. |
| Bagheri et al. [20] Iran | Alloxan-induced diabetes in male Wistar rats. | Hydroalcoholic pomegranate peel extract (PoPE), dissolving (PoPE powder 50% distilled water and 50% ethanol). | Treatment significantly increased GSH, GPx, and SOD and decreased CAT and MDA. |
| Zhang et al. [34] China | STZ-induced diabetes in HFD-fed male C57BL/6 mice. | Diabetic rats were orally gavaged with PU daily at (20 mg/kg body weight) for eight weeks. | PU treatment significantly decreased MDA and free fatty acid (FFA) levels in the serum and liver and increased the liver’s total-superoxide dismutase (T-SOD) activity without significant changes in serum T-SOD activity. |
| Abo-Saif et al. [43] Egypt | STZ-induced diabetes in male Wistar rats. | 1 mL of the PoPE at a dose of 150 mg/kg orally for eight weeks, | Treatment significantly decreased lipid peroxidation, IL-1β, and MDA in the heart tissue. |
| Mosaoa et al. [38] Egypt | STZ-induced diabetes in female Wister rats. | Seeds (100 g) were ground in a mixer. Then, the juice was added to 1000 mL of 80% n-hexane.Diabetic rats were treated orally with three pomegranate hexane extracts (PHE) (25, 50, 75 mg/kg) for eight weeks. | PHE at these concentrations significantly decreased TAC and MDA and increased GSH, CAT, and SOD. |
| Author, Country | Study Design | Population | Age (Years) | BMI (kg/m2) | Male, n (%) | Intervention and Duration | General Findings |
|---|---|---|---|---|---|---|---|
| Rosenblat et al. [29] Israel | Case study | Ten non-insulin-dependent diabetes mellitus and ten healthy participants | 50 ± 10 | N/A | 10 (50) | Concentrated pomegranate juice (PJ) was diluted (1:5) with water to make 50 mL and administered for three months. | PJ treatment significantly decreased serum oxidative stress, thiobarbituric acid reactive substance (TBARS) serum level, and oxidized lipoprotein (ox-LDL) uptake and increased glutathione (GSH) activity. |
| Rock et al. [60] Israel | Randomized controlled trial (RCT) | Thirty patients with type 2 diabetes (T2D) | Pomegranate polyphenol extract (PPE): 54 ± 3; PJ: 59 ± 2 | PPE: 33 ± 2 PJ: 30 ± 3 | 20 (67) | PJ (50 mL) was administered daily for four weeks. PPE (5 mL) was administered daily for six weeks. | PJ consumption significantly decreased TBARS and increased thiol levels, representing the serum’s antioxidant capacity (AOC). |
| Sohrab et al. [65] Iran | RCT | 44 T2D patients | 55 ± 6.7 | 29.3 ± 3.9 | 11 (50) | 250 mL of PJ daily for 12 weeks. | PJ significantly reduced soluble intercellular adhesion molecule-1 (sICAM-1) and E-selectin without any effect on soluble vascular cell adhesion molecule-1 (sVCAM-1) and nuclear factor kappa-beta (NF-κβ). |
| Fenercioglu et al. [66] Turkey | RCT | 56 T2D and 58 healthy controls | 53.51 ± 6.82 | 31.37 ± 4.98 | 22 (39) | One capsule (500 mg) containing pomegranate extract was administered for three months. | Treatment significantly decreased malondialdehyde (MDA) and increased antioxidant defense, total plasma glutathione (GSH), and AOC. |
| Fuhrman et al. [28] Israel | Quasi-experimental study | 6 T2D patients | 59 ± 2 | 30 ± 3 | 6 (100) | 50 mL of concentrated PJ was administered daily for four weeks. | Treatment with PJ and its derivatives increased PON1 arylesterase activity. |
| Parsaeyan et al. [30] Iran | Quasi-experimental study | 50 T2D patients | 48 ± 8 | 30 ± 3 | Not reported | 200 mL of PJ was administered daily for six weeks. | PON1 and arylesterase activity significantly increased, while decreasing MDA levels. |
| Sohrab et al. [62] Iran | RCT | 44 T2D patients | 55 ± 6.7 | 29.4 ± 3.9 | 11 (50) | 250 mL of PJ administered daily for 12 weeks | C-reactive protein (CRP), tumor necrosis factor-alpha (TNF-α), and interleukin-6 (IL-6) significantly decreased from baseline compared to post exposure. |
| Sohrab et al. [26] Iran | RCT | 22 T2D, 22 healthy controls | 59 ± 6.7 | 29.49 ± 3.9 | 11 (50) | 250 mL of PJ was administered daily for 12 weeks. | PJ significantly increased total antioxidant capacity (TAC) and decreased MDA. |
| Shishehbor et al. [61] Iran | Quasi-experimental | 31 T2D patients | 46 ± 8.3 | 29.53 ± 0.69 | 15 (48) | 50 g of concentrated pomegranate juice administered daily for four weeks | PJ significantly increased TAC and decreased IL-6, while TNF-α and CRP were not different between baseline and post treatment. |
| Sohrab et al. [25] Iran | RCT | 30 T2D and 30 healthy controls | 54.6 ± 8.4 | 27.2 ± 3.4 | 15 (50) | 200 mL of PJ was administered daily for six weeks. | PJ treatment significantly decreased ox-LDL and anti-ox-LDL antibodies and TAC, while the PON-1 activity increased significantly. |
| Yarmohamadi et al. [64] Iran | Semi-experimental study | 33 T2D patients | 56.50 ± 3.85 | 26.42 ± 4.79 | 0 (0) | 150 mL of pomegranate extract was administered daily for six weeks. | Pomegranate extract treatment significantly increased glutathione peroxidase (GPx), SOD, plasma GSH, and TAC levels. |
| Khajebishak et al. [63] Iran | RCT | 52 obese T2D patients | 44.6 ± 5.1 | 33.96 ± 4.9 | 9 (34.6) | 3 g pomegranate seed oil (PSO) was administered daily for eight weeks. | PSO treatment significantly decreased IL-6 and TNF-α with no significant changes in high-sensitivity C-reactive protein (hs-CRP). |
| Grabez et al. [67] Bosnia & Herzegovina | RCT | 60 T2D patients | 57.87 ± 6.08 | 30.95 ± 4.37 | 15 (50) | Pomegranate peel extract (PoPEx) containing a capsule (250 mg) was administered twice daily for eight weeks. | Treatment significantly decreased TBARS, nitrites (NO2−), superoxide anion radical (O2−), CRP, IL-6, and TNF-α while increasing TAC. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mokgalaboni, K.; Dlamini, S.; Phoswa, W.N.; Modjadji, P.; Lebelo, S.L. The Impact of Punica granatum Linn and Its Derivatives on Oxidative Stress, Inflammation, and Endothelial Function in Diabetes Mellitus: Evidence from Preclinical and Clinical Studies. Antioxidants 2023, 12, 1566. https://doi.org/10.3390/antiox12081566
Mokgalaboni K, Dlamini S, Phoswa WN, Modjadji P, Lebelo SL. The Impact of Punica granatum Linn and Its Derivatives on Oxidative Stress, Inflammation, and Endothelial Function in Diabetes Mellitus: Evidence from Preclinical and Clinical Studies. Antioxidants. 2023; 12(8):1566. https://doi.org/10.3390/antiox12081566
Chicago/Turabian StyleMokgalaboni, Kabelo, Sanele Dlamini, Wendy N. Phoswa, Perpetua Modjadji, and Sogolo L. Lebelo. 2023. "The Impact of Punica granatum Linn and Its Derivatives on Oxidative Stress, Inflammation, and Endothelial Function in Diabetes Mellitus: Evidence from Preclinical and Clinical Studies" Antioxidants 12, no. 8: 1566. https://doi.org/10.3390/antiox12081566
APA StyleMokgalaboni, K., Dlamini, S., Phoswa, W. N., Modjadji, P., & Lebelo, S. L. (2023). The Impact of Punica granatum Linn and Its Derivatives on Oxidative Stress, Inflammation, and Endothelial Function in Diabetes Mellitus: Evidence from Preclinical and Clinical Studies. Antioxidants, 12(8), 1566. https://doi.org/10.3390/antiox12081566








