Phytochemistry, Pharmacology, and Toxicology of Datura Species—A Review
Abstract
:1. Introduction
2. Ethnobotanical Description of Datura
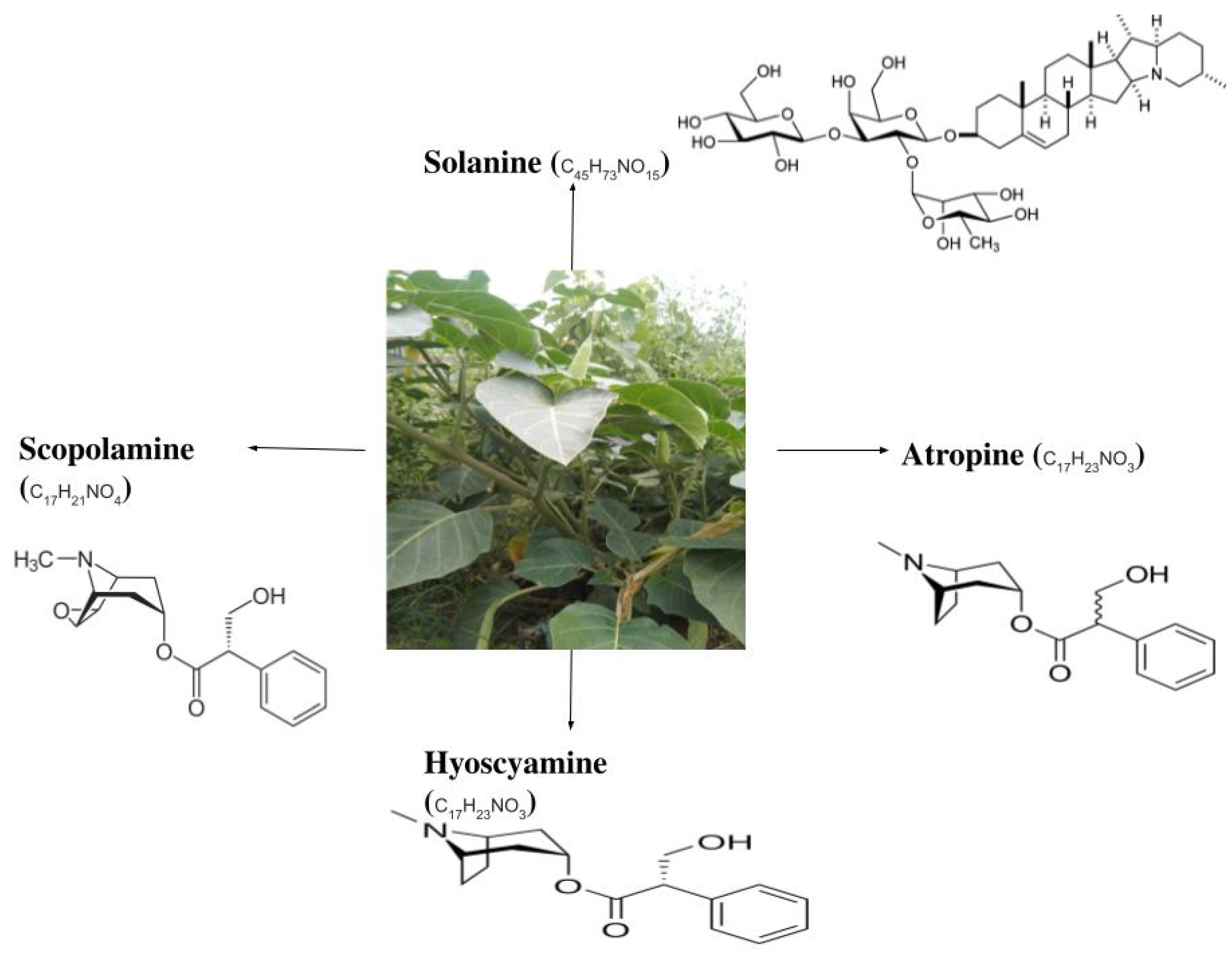
3. Biochemical Composition of Datura
4. Pharmacological Activity of Datura
4.1. Anti-Inflammatory and Analgesic Activities
4.2. Antioxidation Activities
4.3. Antimicrobial Potential of Datura
4.4. Anti-Asthmatic and Bronchodilating Effects
4.5. Anticancer Potentail of Datura
4.6. Activity against Harmful Insects
4.7. Cellular Protective and Wound-Healing Effects
5. Toxicology of Datura
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Sayyed, A.; Shah, M. Phytochemistry, Pharmacological and Traditional Uses of Datura stramonium L. Rev. J. Pharm. Phytochem. 2014, 2, 123–125. [Google Scholar]
- Alabri, T.H.A.; Al Musalami, A.H.S.; Hossain, M.A.; Weli, A.M.; Al-Riyami, Q. Comparative Study of Phytochemical Screening, Antioxidant and Antimicrobial Capacities of Fresh and Dry Leaves Crude Plant Extracts of Datura metel L. J. King Saud Univ. Sci. 2014, 26, 237–243. [Google Scholar] [CrossRef]
- Gaire, B.P.; Subedi, L. A Review on the Pharmacological and Toxicological Aspects of Datura stramonium L. J. Integr. Med. 2013, 11, 73–79. [Google Scholar] [CrossRef]
- Monira, K.M.; Munan, S.M. Review on Datura Metel: A Potential Medicinal Plant. Glob. J. Res. Med. Plants Indig. Med. 2012, 1, 123. [Google Scholar]
- Nasir, B.; Baig, M.W.; Majid, M.; Ali, S.M.; Khan, M.Z.I.; Kazmi, S.T.B.; Haq, I. Preclinical Anticancer Studies on the Ethyl Acetate Leaf Extracts of Datura Stramonium and Datura Inoxia. BMC Complement. Med. Ther. 2020, 20, 188. [Google Scholar] [CrossRef] [PubMed]
- Shah, V.V.; Shah, N.D.; Patrekar, P.V. Medicinal Plants from Solanaceae Family. Res. J. Pharm. Technol. 2013, 6, 143–151. [Google Scholar]
- Alam, W.; Khan, H.; Khan, S.A.; Nazir, S.; Akkol, E.K. Datura Metel: A Review on Chemical Constituents, Traditional Uses and Pharmacological Activities. Curr. Pharm. Des. 2020, 27, 2545–2557. [Google Scholar] [CrossRef] [PubMed]
- Al-Snafi, A.E. Medical Importance of Datura fastuosa (Syn: Datura metel) and Datura stramonium—A Review. IOSR J. Pharm. 2017, 7, 43–58. [Google Scholar] [CrossRef]
- Devi, M.R.; Bawari, M.; Paul, S.B.; Sharma, G.D. Neurotoxic and Medicinal Properties of Datura stramonium L.–Review. Assam Univ. J. Sci. Technol. 2011, 7, 139–144. [Google Scholar]
- Meselhy, K.M. Cytotoxic and Insect-Repellent Activities of Surface Flavonoids from Datura stramonium L. Grown in Egypt. Life Sci. J. 2012, 9, 3154–3158. [Google Scholar]
- Jakabová, S.; Vincze, L.; Farkas, Á.; Kilár, F.; Boros, B.; Felinger, A. Determination of Tropane Alkaloids Atropine and Scopolamine by Liquid Chromatography–Mass Spectrometry in Plant Organs of Datura Species. J. Chromatogr. A 2012, 1232, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Setshogo, M.P. A Review of Some Medicinal and or Hallucinogenic Solanaceous Plants of Botswana: The Genus Datura L. Int. J. Appl. Res. Nat. Prod. 2015, 1, 15–23. [Google Scholar]
- Soni, P.; Siddiqui, A.A.; Dwivedi, J.; Soni, V. Pharmacological Properties of Datura stramonium L. as a Potential Medicinal Tree: An Overview. Asian Pac. J. Trop. Biomed. 2012, 2, 1002–1008. [Google Scholar] [CrossRef]
- Kadam, S.D.; Chavhan, S.A.; Shinde, S.A.; Sapkal, P.N. Pharmacognostic Review on Datura. Int. J. Pharm. Chin. Med. 2018, 2, 1–9. [Google Scholar] [CrossRef]
- Naik, V.; Babu, K.S.; Latha, J.; Kolluru, B. A Review on Phytochemical and Pharmacological Activity of Datura stramonium. (Medicinal Plant). Res. J. Pharmacogn. Phytochem. 2018, 10, 77–80. [Google Scholar] [CrossRef]
- Mukhtar, Y.; Tukur, S.; Bashir, R.A. An Overview on Datura stramonium L. (Jimson Weed): A Notable Psychoactive Drug Plant. Am. J. Nat. Sci. 2019, 2, 1–9. [Google Scholar]
- Das, S.; Kumar, P.; Basu, S.P. Phytoconstituents and Therapeutic Potentials of Datura stramonium Linn. J. Drug Deliv. Ther. 2012, 2, 4–7. [Google Scholar] [CrossRef]
- Boumba, V.; Mitselou, A.; Vujuk, T. Fatal Poisoning from Ingestion of Datura stramonium Seeds. Vet. Hum. Toxicol. 2004, 46, 81–82. [Google Scholar]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015: Elaboration and Explanation. BMJ 2015, 349, g7647. [Google Scholar] [CrossRef]
- Ibrahim, M.; Siddique, S.; Rehman, K.; Husnain, M.; Hussain, A.; Akash, M.S.H.; Azam, F. Comprehensive Analysis of Phytochemical Constituents and Ethnopharmacological Investigation of Genus Datura. Crit. Rev. Eukaryot. Gene Expr. 2018, 28, 223–283. [Google Scholar] [CrossRef]
- Bagewadi, Z.K.; Muddapur, U.M.; Madiwal, S.S.; Mulla, S.I.; Khan, A. Biochemical and Enzyme Inhibitory Attributes of Methanolic Leaf Extract of Datura inoxia Mill. Environ. Sustain. 2019, 2, 75–87. [Google Scholar] [CrossRef]
- Fatima, H.; Khan, K.; Zia, M.; Ur-Rehman, T.; Mirza, B.; Haq, I. Extraction Optimization of Medicinally Important Metabolites from Datura innoxia Mill.: An in Vitro Biological and Phytochemical Investigation. BMC Complement. Altern. Med. 2015, 15, 376. [Google Scholar] [CrossRef]
- Nayyar, M.S.; Hanif, M.A.; Mjaeed, M.I.; Ayub, M.A.; Rehman, R. Datura. In Medicinal Plants of South Asia; Elsevier: Amsterdam, The Netherlands, 2020; pp. 207–216. [Google Scholar]
- Lim, K.M.C.; Dagalea, F.M.S.; Vicencio, M.C.G. Antibacterial Activity of Datura metel Linn. (TALONG-PUNAY) Fruit Extract. J. Pharm. Res. Int. 2020, 32, 96–101. [Google Scholar] [CrossRef]
- Nandakumar, A.; Vaganan, M.M.; Sundararaju, P.; Udayakumar, R. Phytochemical Analysis and Nematicidal Activity of Ethanolic Leaf Extracts of Datura metel, Datura inoxia and Brugmansia suaveolens against Meloidogyne incognita. Asian J. Biol. 2017, 2, 1–11. [Google Scholar] [CrossRef]
- Al-Snafi, A.E. Medicinal Plants Alkaloids, as Promising Therapeutics-A Review (Part 1). IOSR J. Pharm. 2021, 11, 51–67. [Google Scholar]
- Alinejad, S.; Sarabi, V.; Bakhtvari, A.R.S.; Hashempour, H. Variation in Physiological Traits, Yield and Secondary Metabolites of Jimsonweed (Datura stramonium L.) under Different Irrigation Regimes and Nutrition Systems. Ind. Crop. Prod. 2020, 143, 111916. [Google Scholar] [CrossRef]
- Oseni, O.A.; Olarinoye, C.O.; Amoo, I.A. Studies on Chemical Compositions and Functional Properties of Thorn Apple (Datura stramonium L.) Solanaceae. Afr. J. Food Sci. 2010, 5, 40–44. [Google Scholar]
- Ayuba, V.O.; Ojobe, T.O.; Ayuba, S.A. Phytochemical and Proximate Composition of Datura innoxia Leaf, Seed, Stem, Pod and Root. J. Med. Plants Res. 2011, 5, 2952–2955. [Google Scholar]
- Butnariu, M. An Analysis of Sorghum Halepense’s Behavior in Presence of Tropane Alkaloids from Datura stramonium Extracts. Chem. Cent. J. 2012, 6, 75. [Google Scholar] [CrossRef]
- Maheshwari, N.O.; Khan, A.; Chopade, B.A. Rediscovering the Medicinal Properties of Datura Sp.: A Review. J. Med. Plants Res. 2013, 7, 2885–2897. [Google Scholar]
- Roy, S.; Samant, L.; Ganjhu, R.; Mukherjee, S.; Chowdhary, A. Assessment of in Vivo Antiviral Potential of Datura metel Linn. Extracts against Rabies Virus. Pharmacogn. Res. 2018, 10, 109. [Google Scholar]
- Roy, S.; Mukherjee, S.; Pawar, S.; Chowdhary, A. Evaluation of In Vitro Antiviral Activity of Datura metel Linn. against Rabies Virus. Pharmacogn. Res. 2016, 8, 265. [Google Scholar] [CrossRef]
- Hameed Baloch, I.A.; Hanif-ur-Rehman, I.A.B. Review Article on Poisonous Plants of Balochistan. Balochistaniyat 2017, 6, 36–56. [Google Scholar]
- Agarwal, R.; Gupta, R.; Yadav, R.; Asati, V.; Rathi, J.C. Anti-Inflammatory Activity of Seeds Extract of Datura stramonium against Carrageenan Induced Paw Edema on Albino Wistar Rats. J. Pharm. Biol. Sci. 2019, 7, 41–46. [Google Scholar]
- Chandan, G.; Kumar, C.; Chibber, P.; Kumar, A.; Singh, G.; Satti, N.K.; Gulilat, H.; Saini, A.K.; Bishayee, A.; Saini, R.V. Evaluation of Analgesic and Anti-Inflammatory Activities and Molecular Docking Analysis of Steroidal Lactones from Datura stramonium L. Phytomedicine 2021, 89, 153621. [Google Scholar] [CrossRef]
- Muthusamy, P.; Nivedhitha, M.; Jayshree, N. Analgesic and Anti-Inflammatory Activities of Datura metel Linn. Root in Experimental Animal Models. Res. J. Pharm. Technol. 2010, 3, 897–899. [Google Scholar]
- Nivedhitha, S.; Gobinath, M.; Muthusamy, P.; Rao, K.M. Studies on Anti-Inflammatory Activity of Root Extracts of Datura fastuosa (Linn). J. Pharm. Res. 2010, 3, 2686–2688. [Google Scholar]
- Jaafar, F.R.; Ajeena, S.J.; Mehdy, S.S. Anti-Inflammatory Impacts and Analgesiac Activity of Aqueous Extract Datura innoxia Leaves against Induced Pain and Inflammation in Mice. J. Entomol. Zool. Stud. 2018, 6, 1894–1899. [Google Scholar]
- Belayneh, Y.M.; Birhanu, Z.; Birru, E.M.; Getenet, G. Evaluation of In Vivo Antidiabetic, Antidyslipidemic, and in Vitro Antioxidant Activities of Hydromethanolic Root Extract of Datura stramonium, L. (Solanaceae). J. Exp. Pharmacol. 2019, 11, 29. [Google Scholar] [CrossRef]
- Iqbal, S.; Sivaraj, C.; Gunasekaran, K. Antioxidant and Anticancer Activities of Methanol Extract of Seeds of Datura stramonium L. Free Radic. Antioxid. 2017, 7, 184–189. [Google Scholar] [CrossRef]
- Al-Snafi, A.E. Medicinal Plants Possessed Antioxidant and Free Radical Scavenging Effects (Part 3)—A Review. IOSR J. Pharm. 2017, 7, 48–62. [Google Scholar] [CrossRef]
- Khan, W.; Subhan, S.; Shams, D.F.; Afridi, S.G.; Ullah, R.; Shahat, A.A.; Alqahtani, A.S. Antioxidant Potential, Phytochemicals Composition, and Metal Contents of Datura Alba. BioMed Res. Int. 2019, 2019, 2403718. [Google Scholar] [CrossRef] [PubMed]
- Gachande, B.D.; Khillare, E.M. In-Vitro Evaluation of Datura Species for Potential Antimicrobial Activity. Biosci. Discov. 2013, 4, 78–81. [Google Scholar]
- Shagal, M.H.; Modibbo, U.U.; Liman, A.B. Pharmacological Justification for the Ethnomedical Use of Datura stramonium Stem-Bark Extract in Treatment of Diseases Caused by Some Pathogenic Bacteria. Int. Res. Pharm. Pharmacol. 2012, 2, 16–19. [Google Scholar]
- Girmay, S. Preliminary Phytochemical Screening and In Vitro Antimicrobial Activity of Datura stramonium Leaves Extracts Collected from Eastern Ethiopia. Res. J. Chem. Sci. 2015, 22, 606X. [Google Scholar]
- Kalim, M.; Hussain, F.; Ali, H.; Ahmad, I.; Iqbal, M.N. Antifungal Activities of Methanolic Extracts of Datura inoxia. PSM Biol. Res. 2016, 1, 70–73. [Google Scholar]
- Bachheti, R.K.; Rai, I.; Mishra, V.K.; Joshi, A. Antioxidant and Antimicrobial Properties of Seed Oil of Datura metel. J. Environ. Biol. 2018, 39, 182–188. [Google Scholar] [CrossRef]
- Choudhary, M.; Sharma, I.; Agrawal, D.C.; Dhar, M.K.; Kaul, S. Neurotoxic Potential of Alkaloids from Thorn Apple (Datura stramonium L.): A Commonly Used Indian Folk Medicinal Herb. In Medicinal Herbs and Fungi; Springer: Berlin/Heidelberg, Germany, 2021; pp. 391–420. [Google Scholar]
- Kuraki, T. Bronchodilators for COPD: At What Stage Should Therapeutic Intervention Be Initiated? In Chronic Obstructive Pulmonary Disease; Springer: Berlin/Heidelberg, Germany, 2017; pp. 211–243. [Google Scholar]
- Yamada, M.; Ichinose, M. The Cholinergic Pathways in Inflammation: A Potential Pharmacotherapeutic Target for COPD. Front. Pharmacol. 2018, 9, 1426. [Google Scholar] [CrossRef]
- Papi, A.; Fabbri, L.M.; Kerstjens, H.A.; Rogliani, P.; Watz, H.; Singh, D. Inhaled Long-Acting Muscarinic Antagonists in Asthma—A Narrative Review. Eur. J. Intern. Med. 2021, 85, 14–22. [Google Scholar] [CrossRef]
- Miraj, S. Datura Stramonium: An Updated Review. Pharm. Chem. 2016, 8, 253–257. [Google Scholar]
- Roy, S.; Pawar, S.; Chowdhary, A. Evaluation of in Vitro Cytotoxic and Antioxidant Activity of Datura metel Linn. and Cynodon dactylon Linn. Extracts. Pharmacogn. Res. 2016, 8, 123. [Google Scholar] [CrossRef]
- Alper, M. Investigation of potential anti-cancer and anti-inflammatory effects of Datura stramonium ethanolic extracts against selected human cancer cell lines. Fresenius Environ. Bull. 2019, 28, 8993–9003. [Google Scholar]
- Mir, M.A.; Hamdani, S.S.; Sheikh, B.A.; Mehraj, U. Recent Advances in Metabolites from Medicinal Plants in Cancer Prevention and Treatment. Curr. Immunol. Rev. 2019, 15, 185–201. [Google Scholar] [CrossRef]
- Al-Zharani, M.; Nasr, F.A.; Alqahtani, A.S.; Cordero, M.A.W.; Alotaibi, A.A.; Bepari, A.; Alarifi, S.; Daoud, A.; Barnawi, I.O.; Daradka, H.M. In Vitro Cytotoxic Evaluation and Apoptotic Effects of Datura innoxia Grown in Saudi Arabia and Phytochemical Analysis. Appl. Sci. 2021, 11, 2864. [Google Scholar] [CrossRef]
- Swathi, S. Larvicidal and Repellent Activities of Ethanolic Extract of Datura stramonium Leaves against Mosquitoes. Int. J. Pharmacogn. Phytochem. Res. 2012, 4, 25–27. [Google Scholar]
- Jawalkar, N.; Zambare, S.; Zanke, S. Insecticidal Property of Datura Stramonium L. Seed Extracts against Sitophilus oryzae L. (Coleoptera: Curculionidae) in Stored Wheat Grains. J. Entomol. Zool. Stud. 2016, 4, 92–96. [Google Scholar]
- Karimzadeh, J.; Rabiei, A. Larvicidal and Oviposition Deterrent Effects of the Jimsonweed (Datura stramonium) Extracts on the Diamondback Moth, Plutella Xylostella. J. Agric. Sci. Technol. 2020, 22, 1279–1293. [Google Scholar]
- Ali, K.; Sagheer, M.; Rashid, A. Impact of Extracts of Azadirachta Indica and Datura inoxia on the Esterases and Phosphatases of Three Stored Grains Insect Pests of Economic Importance. Pak. J. Agric. Sci. 2017, 54, 71–81. [Google Scholar]
- Manpreet, K.; Anita, S.; Piyush, G. Phytochemical and pharmacological study of dhatura: A review. Int. J. Res. AYUSH Pharm. Sci. 2017, 1, 113–118. [Google Scholar]
- Bania, T.C.; Chu, J.; Bailes, D.; O’Neill, M. Jimson Weed Extract as a Protective Agent in Severe Organophosphate Toxicity. Acad. Emerg. Med. 2004, 11, 335–338. [Google Scholar] [CrossRef]
- Al-Snafi, A.E. Arabian Medicinal Plants with Dermatological Effects-Plant Based Review (Part 1). IOSR J. Pharm. 2018, 8, 44–73. [Google Scholar]
- Bouzidi, A.; Mahdeb, N.; Kara, N. Toxicity Studies of Alkaloids of Seeds of Datura stramonium and Synthesis Alkaloids in Male Rats. J. Med. Plants Res. 2011, 5, 3421–3431. [Google Scholar]
- Ogunmoyole, T.; Adeyeye, R.I.; Olatilu, B.O.; Akande, O.A.; Agunbiade, O.J. Multiple Organ Toxicity of Datura stramonium Seed Extracts. Toxicol. Rep. 2019, 6, 983–989. [Google Scholar] [CrossRef] [PubMed]
- Krenzelok, E.P. Aspects of Datura Poisoning and Treatment. Clin. Toxicol. 2010, 48, 104–110. [Google Scholar] [CrossRef]
- Al-Snafi, A.E.; Talab, T.A.; Majid, W.J. Medicinal Plants with Central Nervous Activity-An Overview (Part 1). IOSR J. Pharm. 2019, 9, 52–102. [Google Scholar]
| Chemical Constituents | D. metel (%) [8] | D. stramonium (%) [28] | D. innoxia (%) [29] |
|---|---|---|---|
| Fat/lipid | 14.72 | 16.60 | 15.52 |
| Carbohydrate | 51.22 | 26.20 | - |
| Protein | 20.73 | 16.20 | 13.90 |
| Moisture | 4.63 | 8.50 | 10.00 |
| Ash content | 5.14 | 8.70 | 8.26 |
| Crude fibre | 17.35 | 23.70 | 6.55 |
| Plant Parts | Alkaloid | Young Plant | Adult Plant |
|---|---|---|---|
| Stems | Atropine | 0.915 ± 0.015 | 0.001 ± 0.001 |
| Scopolamine | 0.129 ± 0.014 | ||
| Seeds | Atropine | 0.670 ± 0.003 | 0.387 ± 0.015 |
| Scopolamine | 0.012 ± 0.001 | 0.089 ± 0.010 | |
| Flowers | Atropine | 0.299 ± 0.021 | 0.270 ± 0.026 |
| Scopolamine | 0.106 ± 0.031 | 0.066 ± 0.004 | |
| Roots | Atropine | 0.121 ± 0.015 | - |
| Scopolamine | 0.014 ± 0.004 | - | |
| Medium leaves | Atropine | 0.831 ± 0.014 | 0.150 ± 0.002 |
| Scopolamine | 0.041 ± 0.005 | 0.022 ± 0.005 |
| Root Extract Concentration (μg/mL) | DPPH Scavenging Activity (%) |
|---|---|
| 12.5 | 16.31 |
| 25 | 30.65 |
| 50 | 44.31 |
| 100 | 67.79 |
| 200 | 81.23 |
| 400 | 90.32 |
| Insect | Extract of Plant Part | Species | References |
|---|---|---|---|
| Helicoverpa armigera | Methanolic seed extracts | D. metel | [4,8] |
| Aedes aegypti | Ethanolic leaf extracts | D. stramonium | [58] |
| Anopheles stephensi | ethanolic leaf extracts | D. stramonium | [58] |
| Culex quinquefasciatus | ethanolic leaf extracts | D. stramonium | [58] |
| Sitophilus oryzae | Methanolic seed extracts | D. stramonium | [59] |
| Plutella xylostella | extract from the different plant parts | D. stramonium | [60] |
| Tribolium castaneum | Acetone extracts | D. innoxia | [61] |
| Trogoderma granarium | Acetone extracts | D. innoxia | [61] |
| Sitophilus granarius | Acetone extracts | D. innoxia | [61] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sharma, M.; Dhaliwal, I.; Rana, K.; Delta, A.K.; Kaushik, P. Phytochemistry, Pharmacology, and Toxicology of Datura Species—A Review. Antioxidants 2021, 10, 1291. https://doi.org/10.3390/antiox10081291
Sharma M, Dhaliwal I, Rana K, Delta AK, Kaushik P. Phytochemistry, Pharmacology, and Toxicology of Datura Species—A Review. Antioxidants. 2021; 10(8):1291. https://doi.org/10.3390/antiox10081291
Chicago/Turabian StyleSharma, Meenakshi, Inderpreet Dhaliwal, Kusum Rana, Anil Kumar Delta, and Prashant Kaushik. 2021. "Phytochemistry, Pharmacology, and Toxicology of Datura Species—A Review" Antioxidants 10, no. 8: 1291. https://doi.org/10.3390/antiox10081291
APA StyleSharma, M., Dhaliwal, I., Rana, K., Delta, A. K., & Kaushik, P. (2021). Phytochemistry, Pharmacology, and Toxicology of Datura Species—A Review. Antioxidants, 10(8), 1291. https://doi.org/10.3390/antiox10081291








