Pharmacotherapy against Oxidative Stress in Chronic Kidney Disease: Promising Small Molecule Natural Products Targeting Nrf2-HO-1 Signaling
Abstract
1. Introduction
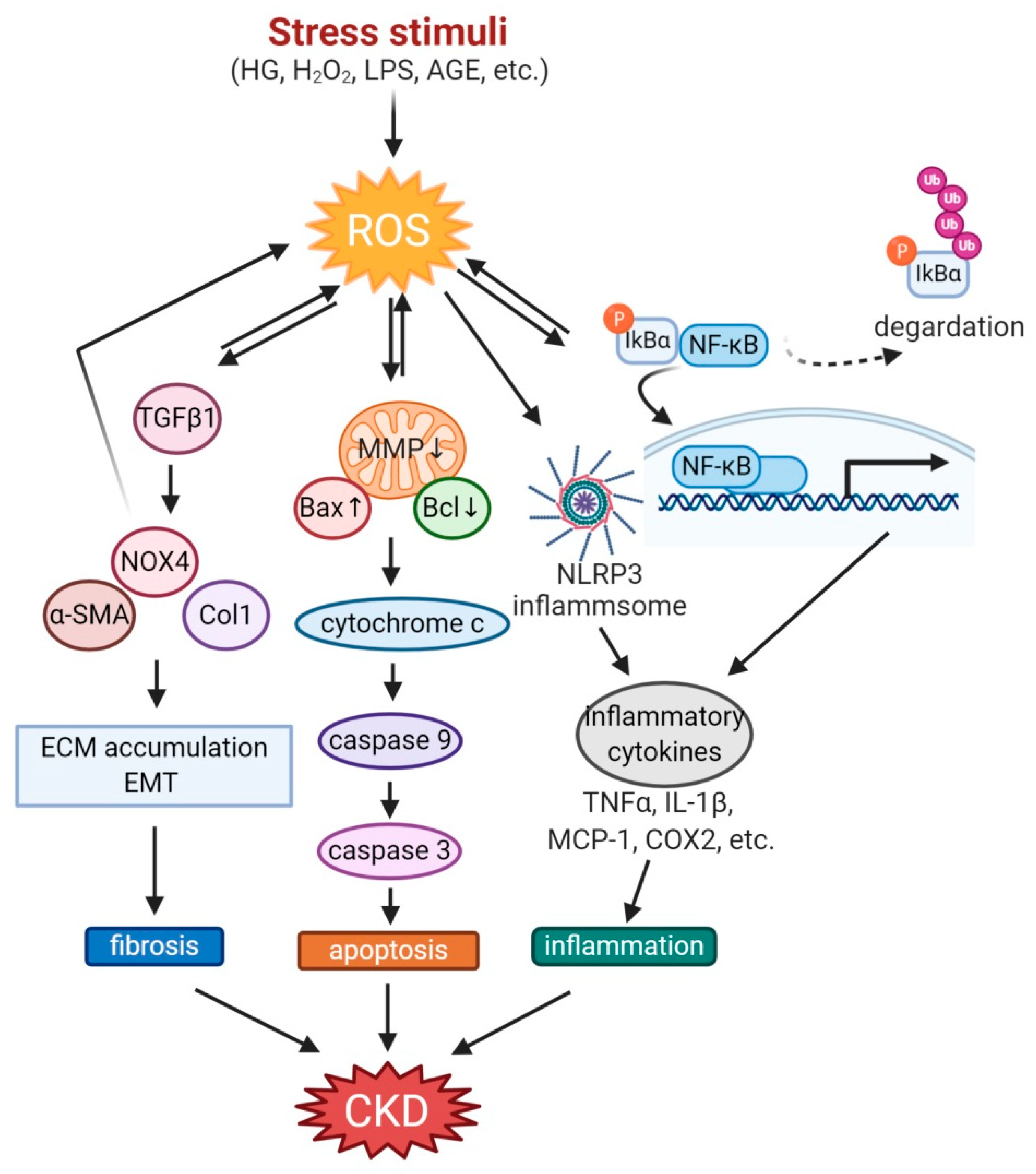
2. Oxidative Stress in Chronic Kidney Disease
2.1. Diabetic Kidney Disease (DKD)
2.2. Glomerulosclerosis and Glomerulonephritis
2.3. Lupus Nephritis (LN) and Systemic Lupus Erythematosus (SLE)
2.4. Tubulointerstitial Fibrosis
2.5. Chronic Renal Allograft Dysfunction (CRAD)
2.6. The Role of Oxidative Stress in Kidney Cells
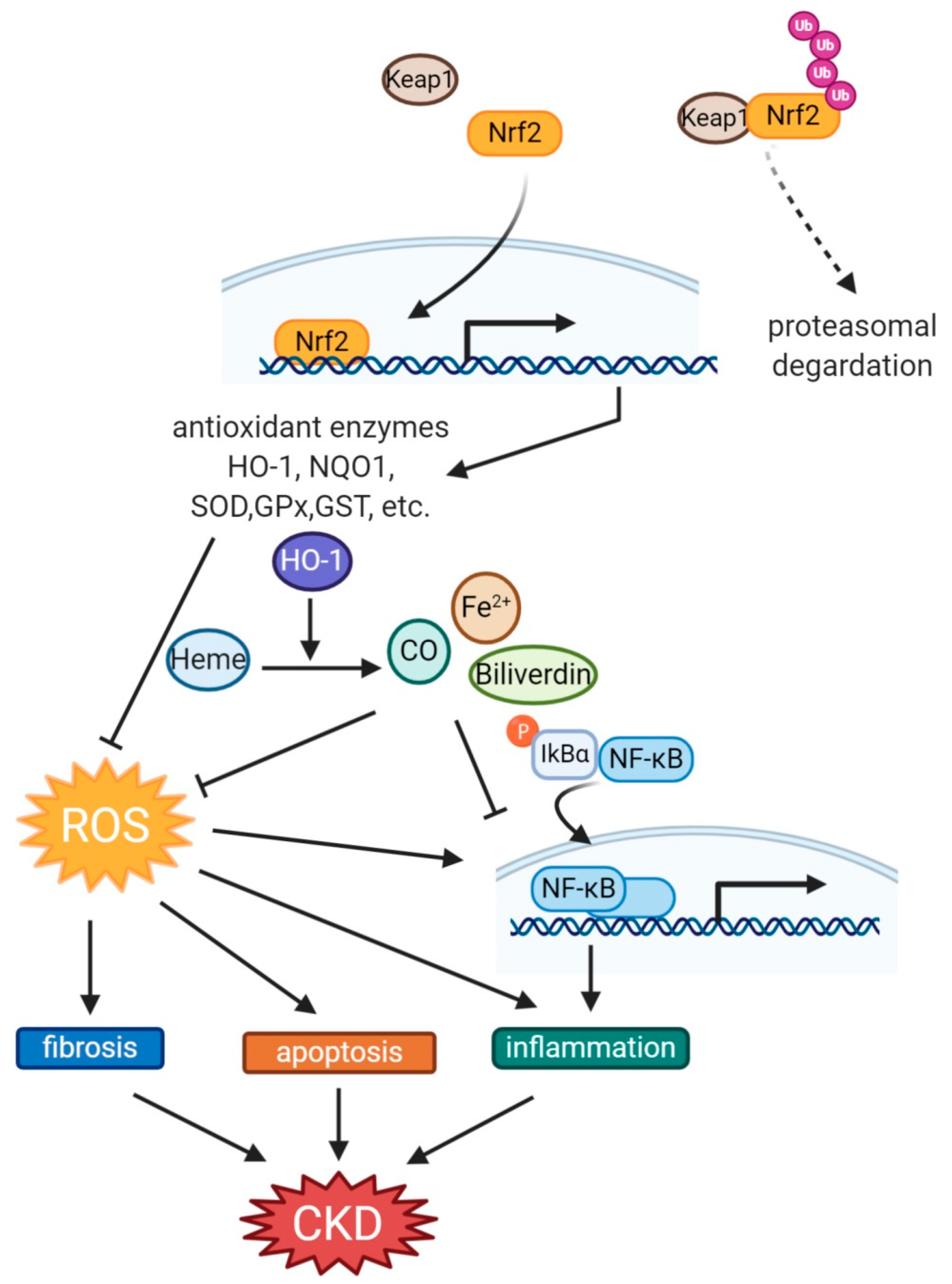
3. Role of Nrf2 and HO-1 against Oxidative Stress
4. Functional Link between Nrf2 and HO-1
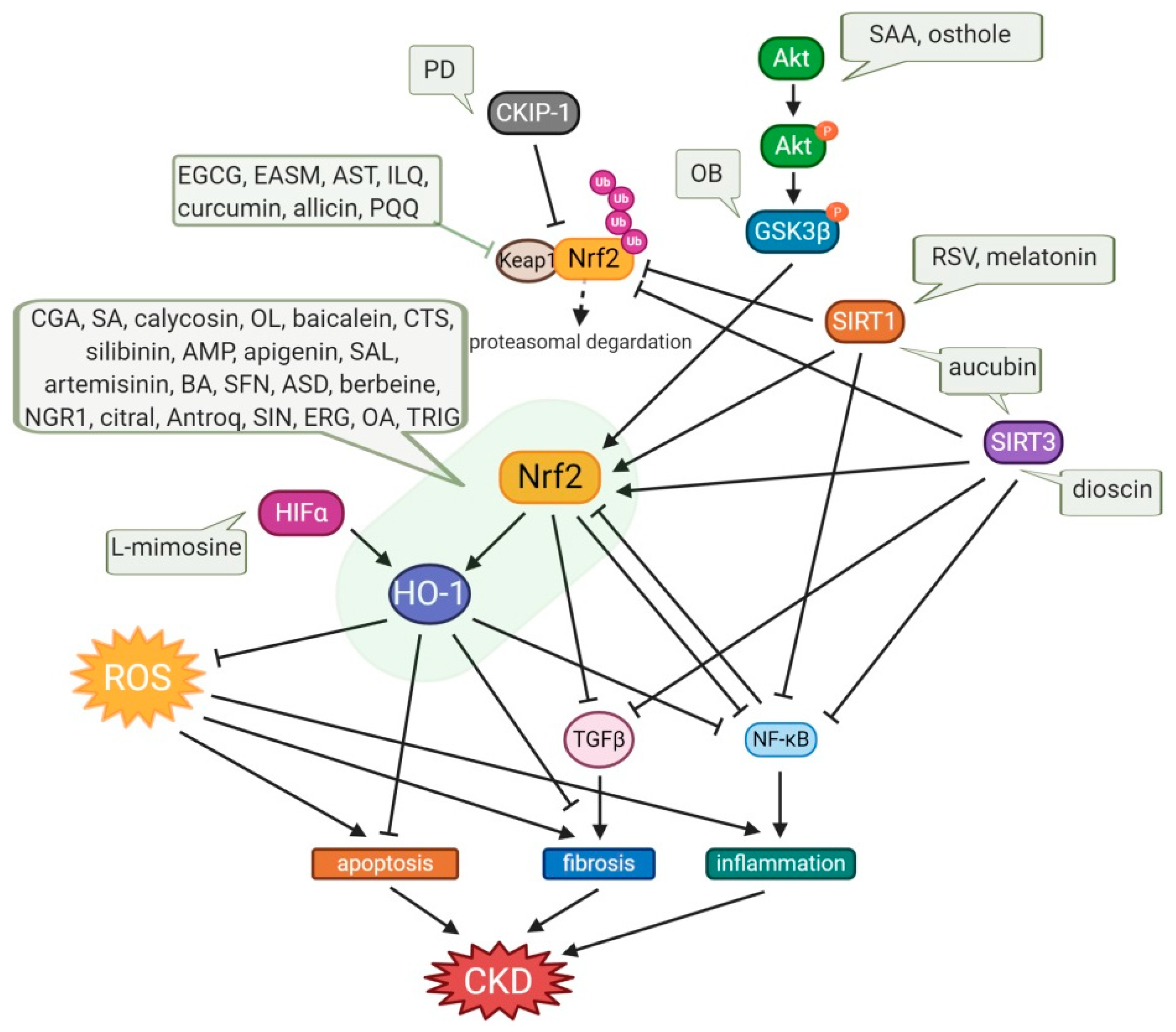
5. Small Molecule Natural Products Activating Nrf2-HO-1 Signaling
5.1. Phenolic Compounds
5.2. Non-Phenolic Compounds
6. Conclusions and Future Perspectives
Author Contributions
Funding
Conflicts of Interest
References
- Carrero, J.J.; Hecking, M.; Chesnaye, N.C.; Jager, K.J. Sex and gender disparities in the epidemiology and outcomes of chronic kidney disease. Nat. Rev. Nephrol. 2018, 14, 151–164. [Google Scholar] [CrossRef] [PubMed]
- Carney, E.F. The impact of chronic kidney disease on global health. Nat. Rev. Nephrol. 2020. [Google Scholar] [CrossRef]
- Liu, M.; Li, X.C.; Lu, L.; Cao, Y.; Sun, R.R.; Chen, S.; Zhang, P.Y. Cardiovascular disease and its relationship with chronic kidney disease. Eur. Rev. Med. Pharmacol. Sci. 2014, 18, 2918–2926. [Google Scholar]
- Clausen, P.; Jensen, J.S.; Jensen, G.; Borch-Johnsen, K.; Feldt-Rasmussen, B. Elevated urinary albumin excretion is associated with impaired arterial dilatory capacity in clinically healthy subjects. Circulation 2001, 103, 1869–1874. [Google Scholar] [CrossRef]
- Chan, D.T.; Irish, A.B.; Dogra, G.K.; Watts, G.F. Dyslipidaemia and cardiorenal disease: Mechanisms, therapeutic opportunities and clinical trials. Atherosclerosis 2008, 196, 823–834. [Google Scholar] [CrossRef] [PubMed]
- Holtkamp, F.A.; De Zeeuw, D.; Thomas, M.C.; Cooper, M.E.; De Graeff, P.A.; Hillege, H.J.L.; Parving, H.H.; Brenner, B.M.; Shahinfar, S.; Heerspink, H.J.L. An acute fall in estimated glomerular filtration rate during treatment with losartan predicts a slower decrease in long-term renal function. Kidney Int. 2011, 80, 282–287. [Google Scholar] [CrossRef]
- Wanner, C.; Inzucchi, S.E.; Lachin, J.M.; Fitchett, D.; Von Eynatten, M.; Mattheus, M.; Johansen, O.E.; Woerle, H.J.; Broedl, U.C.; Zinman, B.; et al. Empagliflozin and progression of kidney disease in type 2 diabetes. N. Engl. J. Med. 2016, 375, 323–334. [Google Scholar] [CrossRef]
- Gregg, L.P.; Hedayati, S.S. Management of traditional cardiovascular risk factors in CKD: What are the data? Am. J. Kidney Dis. 2018, 72, 728–744. [Google Scholar] [CrossRef]
- Cruz, M.C.; Andrade, C.; Urrutia, M.; Draibe, S.; Nogueira-Martins, L.A.; Sesso, R.C.C. Quality of life in patients with chronic kidney disease. Clinics 2011, 66, 991–995. [Google Scholar] [CrossRef]
- Lee, H.B.; Yu, M.R.; Yang, Y.; Jiang, Z.; Ha, H. Reactive oxygen species-regulated signaling pathways in diabetic nephropathy. J. Am. Soc. Nephrol. 2003, 14, S241–S245. [Google Scholar] [CrossRef]
- Podkowińska, A.; Formanowicz, D. Chronic kidney disease as oxidative stress-and inflammatory-mediated cardiovascular disease. Antioxidants 2020, 9, 752. [Google Scholar] [CrossRef]
- Noh, H.; Ha, H. Reactive oxygen species and oxidative stress. In Contributions to Nephrology; Karger: Basel, Switzerland, 2011; Volume 170, pp. 102–112. [Google Scholar]
- Ha, H.; Hwang, I.A.; Park, J.H.; Lee, H.B. Role of reactive oxygen species in the pathogenesis of diabetic nephropathy. Diabetes Res. Clin. Pract. 2008, 82, S42–S45. [Google Scholar] [CrossRef]
- Harman, D. The aging process. Proc. Natl. Acad. Sci. USA 1981, 78, 7124. [Google Scholar] [CrossRef]
- Kim, J.; Kil, I.S.; Seok, Y.M.; Yang, E.S.; Kim, D.K.; Lim, D.G.; Park, J.W.; Bonventre, J.V.; Park, K.M. Orchiectomy attenuates post-ischemic oxidative stress and ischemia/reperfusion injury in mice. A role for manganese superoxide dismutase. J. Biol. Chem. 2006, 281, 20349–20356. [Google Scholar] [CrossRef] [PubMed]
- Stępniewska, J.; Gołembiewska, E.; Dołęgowska, B.; Domański, M.; Ciechanowski, K. Oxidative stress and antioxidative enzyme activities in chronic kidney disease and different types of renal replacement therapy. Curr. Protein Pept. Sci. 2015, 16, 243–248. [Google Scholar] [CrossRef]
- Surh, Y.J.; Kundu, J.K.; Na, H.K. Nrf2 as a master redox switch in turning on the cellular signaling involved in the induction of cytoprotective genes by some chemopreventive phytochemicals. Planta Med. 2008, 74, 1526–1539. [Google Scholar] [CrossRef]
- Lv, W.; Booz, G.W.; Fan, F.; Wang, Y.; Roman, R.J. Oxidative stress and renal fibrosis: Recent insights for the development of novel therapeutic strategies. Front. Physiol. 2018, 9, 105. [Google Scholar] [CrossRef]
- Chen, D.Q.; Hu, H.H.; Wang, Y.N.; Feng, Y.L.; Cao, G.; Zhao, Y.Y. Natural products for the prevention and treatment of kidney disease. Phytomedicine 2018, 50, 50–60. [Google Scholar] [CrossRef]
- Rapa, S.F.; Di Iorio, B.R.; Campiglia, P.; Heidland, A.; Marzocco, S. Inflammation and oxidative stress in chronic kidney disease-potential therapeutic role of minerals, vitamins and plant-derived metabolites. Int. J. Mol. Sci. 2019, 21, 263. [Google Scholar] [CrossRef]
- Nezu, M.; Suzuki, N.; Yamamoto, M. Targeting the KEAP1-NRF2 system to prevent kidney disease progression. Am. J. Nephrol. 2017, 45, 473–483. [Google Scholar] [CrossRef] [PubMed]
- Lu, M.; Wang, P.; Qiao, Y.; Jiang, C.; Ge, Y.; Flickinger, B.; Malhotra, D.K.; Dworkin, L.D.; Liu, Z.; Gong, R. GSK3β-mediated Keap1-independent regulation of Nrf2 antioxidant response: A molecular rheostat of acute kidney injury to chronic kidney disease transition. Redox Biol. 2019, 26, 101275. [Google Scholar] [CrossRef]
- Yamawaki, K.; Kanda, H.; Shimazaki, R. Nrf2 activator for the treatment of kidney diseases. Toxicol. Appl. Pharmacol. 2018, 360, 30–37. [Google Scholar] [CrossRef]
- Choi, B.H.; Kang, K.S.; Kwak, M.K. Effect of redox modulating NRF2 activators on chronic kidney disease. Molecules 2014, 19, 12727–12759. [Google Scholar] [CrossRef]
- Kanda, H.; Yamawaki, K. Bardoxolone methyl: Drug development for diabetic kidney disease. Clin. Exp. Nephrol. 2020, 24, 857–864. [Google Scholar] [CrossRef]
- Abraham, N.G.; Kappas, A. Heme oxygenase and the cardiovascular–renal system. Free Radic. Biol. Med. 2005, 39, 1–25. [Google Scholar] [CrossRef]
- Li, S.; Qiu, B.; Lu, H.; Lai, Y.; Liu, J.; Luo, J.; Zhu, F.; Hu, Z.; Zhou, M.; Tian, J.; et al. Hyperhomocysteinemia accelerates acute kidney injury to chronic kidney disease progression by downregulating Heme Oxygenase-1 expression. Antioxid. Redox Signal. 2019, 30, 1635–1650. [Google Scholar] [CrossRef]
- Demirogullari, B.; Ekingen, G.; Guz, G.; Bukan, N.; Erdem, O.; Ozen, I.O.; Memis, L.; Sert, S. A comparative study of the effects of hemin and bilirubin on bilateral renal ischemia reperfusion injury. Nephron Exp. Nephrol. 2006, 103, e1–e5. [Google Scholar] [CrossRef] [PubMed]
- Chang, T.T.; Chen, Y.A.; Li, S.Y.; Chen, J.W. Nrf-2 mediated heme oxygenase-1 activation contributes to the anti-inflammatory and renal protective effects of Ginkgo biloba extract in diabetic nephropathy. J. Ethnopharmacol. 2020, 266, 113474. [Google Scholar] [CrossRef]
- Di Noia, M.A.; Van Driesche, S.; Palmieri, F.; Yang, L.M.; Quan, S.; Goodman, A.I.; Abraham, N.G. Heme oxygenase-1 enhances renal mitochondrial transport carriers and cytochrome C oxidase activity in experimental diabetes. J. Biol. Chem. 2006, 281, 15687–15693. [Google Scholar] [CrossRef]
- Bolisetty, S.; Traylor, A.; Zarjou, A.; Johnson, M.S.; Benavides, G.A.; Ricart, K.; Boddu, R.; Moore, R.D.; Landar, A.; Barnes, S.; et al. Mitochondria-targeted heme oxygenase-1 decreases oxidative stress in renal epithelial cells. Am. J. Physiol. Ren. Physiol. 2013, 305, F255–F264. [Google Scholar] [CrossRef] [PubMed]
- Kwak, J.Y.; Takeshige, K.; Cheung, B.S.; Minakami, S. Bilirubin inhibits the activation of superoxide-producing NADPH oxidase in a neutrophil cell-free system. Biochim. Biophys. Acta 1991, 1076, 369–373. [Google Scholar] [CrossRef]
- Nath, K.A. Heme oxygenase-1: A provenance for cytoprotective pathways in the kidney and other tissues. Kidney Int. 2006, 70, 432–443. [Google Scholar] [CrossRef] [PubMed]
- Lever, J.M.; Boddu, R.; George, J.F.; Agarwal, A. Heme oxygenase-1 in kidney health and disease. Antioxid. Redox Signal. 2016, 25, 165–183. [Google Scholar] [CrossRef]
- Funes, S.C.; Rios, M.; Fernández-Fierro, A.; Covián, C.; Bueno, S.M.; Riedel, C.A.; Mackern-Oberti, J.P.; Kalergis, A.M. Naturally derived Heme-Oxygenase 1 inducers and their therapeutic application to immune-mediated diseases. Front. Immunol. 2020, 11, 1467. [Google Scholar] [CrossRef] [PubMed]
- Daenen, K.; Andries, A.; Mekahli, D.; Van Schepdael, A.; Jouret, F.; Bammens, B. Oxidative stress in chronic kidney disease. Pediatr. Nephrol. 2019, 34, 975–991. [Google Scholar] [CrossRef] [PubMed]
- Manning, R.D., Jr.; Tian, N.; Meng, S. Oxidative stress and antioxidant treatment in hypertension and the associated renal damage. Am. J. Nephrol. 2005, 25, 311–317. [Google Scholar] [CrossRef] [PubMed]
- Coughlan, M.T.; Sharma, K. Challenging the dogma of mitochondrial reactive oxygen species overproduction in diabetic kidney disease. Kidney Int. 2016, 90, 272–279. [Google Scholar] [CrossRef]
- Hallan, S.; Sharma, K. The role of mitochondria in diabetic kidney disease. Curr. Diabetes Rep. 2016, 16, 61. [Google Scholar] [CrossRef]
- Kwon, G.; Uddin, M.J.; Lee, G.; Jiang, S.; Cho, A.; Lee, J.H.; Lee, S.R.; Bae, Y.S.; Moon, S.H.; Lee, S.J.; et al. A novel pan-Nox inhibitor, APX-115, protects kidney injury in streptozotocin-induced diabetic mice: Possible role of peroxisomal and mitochondrial biogenesis. Oncotarget 2017, 8, 74217–74232. [Google Scholar] [CrossRef]
- Jiang, T.; Huang, Z.; Lin, Y.; Zhang, Z.; Fang, D.; Zhang, D.D. The protective role of Nrf2 in streptozotocin-induced diabetic nephropathy. Diabetes 2010, 59, 850–860. [Google Scholar] [CrossRef]
- Shopit, A.; Niu, M.; Wang, H.; Tang, Z.; Li, X.; Tesfaldet, T.; Ai, J.; Ahmad, N.; Al-Azab, M.; Tang, Z. Protection of diabetes-induced kidney injury by phosphocreatine via the regulation of ERK/Nrf2/HO-1 signaling pathway. Life Sci. 2020, 242, 117248. [Google Scholar] [CrossRef]
- Shevalye, H.; Lupachyk, S.; Watcho, P.; Stavniichuk, R.; Khazim, K.; Abboud, H.E.; Obrosova, I.G. Prediabetic nephropathy as an early consequence of the high-calorie/high- fat diet: Relation to oxidative stress. Endocrinology 2012, 153, 1152–1161. [Google Scholar] [CrossRef]
- Ruggiero, C.; Ehrenshaft, M.; Cleland, E.; Stadler, K. High-fat diet induces an initial adaptation of mitochondrial bioenergetics in the kidney despite evident oxidative stress and mitochondrial ROS production. Am. J. Physiol. Endocrinol. Metab. 2011, 300, E1047–E1058. [Google Scholar] [CrossRef] [PubMed]
- Raza, H.; John, A.; Howarth, F.C. Increased metabolic stress in Zucker diabetic fatty rat kidney and pancreas. Cell. Physiol. Biochem. 2013, 32, 1610–1620. [Google Scholar] [CrossRef]
- Tesch, G.H.; Lim, A.K.H. Recent insights into diabetic renal injury from the db/db mouse model of type 2 diabetic nephropathy. Am. J. Physiol. Ren. Physiol. 2011, 300, F301–F310. [Google Scholar] [CrossRef]
- Hodgkinson, A.D.; Bartlett, T.; Oates, P.J.; Millward, B.A.; Demaine, A.G. The response of antioxidant genes to hyperglycemia is abnormal in patients with type 1 diabetes and diabetic nephropathy. Diabetes 2003, 52, 846–851. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Vaziri, N.D. Contribution of impaired Nrf2-Keap1 pathway to oxidative stress and inflammation in chronic renal failure. Am. J. Physiol. Ren. Physiol. 2010, 298, F662–F671. [Google Scholar] [CrossRef] [PubMed]
- Ceriello, A.; Quagliaro, L.; Catone, B.; Pascon, R.; Piazzola, M.; Bais, B.; Marra, G.; Tonutti, L.; Taboga, C.; Motz, E. Role of hyperglycemia in nitrotyrosine postprandial generation. Diabetes Care 2002, 25, 1439–1443. [Google Scholar] [CrossRef]
- Ceriello, A.; Bortolotti, N.; Motz, E.; Crescentini, A.; Lizzio, T.S.; Russo, A.; Tonutti, L.; Taboga, C. Meal-generated oxidative stress in type 2 diabetic patients. Diabetes Care 1998, 21, 1529–1533. [Google Scholar] [CrossRef] [PubMed]
- Szalay, C.I.; Erdélyi, K.; Kökény, G.; Lajtár, E.; Godó, M.; Révész, C.; Kaucsár, T.; Kiss, N.; Sárközy, M.; Csont, T.; et al. Oxidative/nitrative stress and inflammation drive progression of doxorubicin-induced renal fibrosis in rats as revealed by comparing a normal and a fibrosis-resistant rat strain. PLoS ONE 2015, 10, e0127090. [Google Scholar] [CrossRef] [PubMed]
- Bülbül, M.; Öner, A.; Demircin, G.; Erdoğan, Ö. Oxidative stress in children with acute glomerulonephritis. Ren. Fail. 2008, 30, 209–214. [Google Scholar] [CrossRef]
- Wójcicka, G.; Marciniak, A.; Bełtowski, J.; Górny, D.; Chibowski, D.; Korolczuk, A.; Czabak-Garbacz, R. Oxidative stress in experimental acute glomerulonephritis. Prz. Lek. 2004, 61, 135–140. [Google Scholar]
- Liu, Y.; Xu, X.; Xu, R.; Zhang, S. Renoprotective effects of isoliquiritin against cationic bovine serum albumin-induced membranous glomerulonephritis in experimental rat model through its anti-oxidative and anti- inflammatory properties. Drug Des. Dev. Ther. 2019, 13, 3735–3751. [Google Scholar] [CrossRef] [PubMed]
- Bona, N.; Pezzarini, E.; Balbi, B.; Daniele, S.M.; Rossi, M.F.; Monje, A.L.; Basiglio, C.L.; Pelusa, H.F.; Arriaga, S.M.M. Oxidative stress, inflammation and disease activity biomarkers in lupus nephropathy. Lupus 2020, 29, 311–323. [Google Scholar] [CrossRef] [PubMed]
- Tsai, P.Y.; Ka, S.M.; Chang, J.M.; Chen, H.C.; Shui, H.A.; Li, C.Y.; Hua, K.F.; Chang, W.L.; Huang, J.J.; Yang, S.S.; et al. Epigallocatechin-3-gallate prevents lupus nephritis development in mice via enhancing the Nrf2 antioxidant pathway and inhibiting NLRP3 inflammasome activation. Free Radic. Biol. Med. 2011, 51, 744–754. [Google Scholar] [CrossRef] [PubMed]
- Jiang, T.; Tian, F.; Zheng, H.; Whitman, S.A.; Lin, Y.; Zhang, Z.; Zhang, N.; Zhang, D.D. Nrf2 suppresses lupus nephritis through inhibition of oxidative injury and the NF-κB-mediated inflammatory response. Kidney Int. 2014, 85, 333–343. [Google Scholar] [CrossRef]
- Tsai, C.-Y.; Hsieh, S.-C.; Lu, C.-S.; Wu, T.-H.; Liao, H.-T.; Wu, C.-H.; Li, K.-J.; Kuo, Y.-M.; Lee, H.-T.; Shen, C.-Y.; et al. Cross-talk between mitochondrial dysfunction-provoked oxidative stress and aberrant noncoding RNA expression in the pathogenesis and pathophysiology of SLE. Int. J. Mol. Sci. 2019, 20, 5183. [Google Scholar] [CrossRef]
- Dendooven, A.; Ishola, D.A., Jr.; Nguyen, T.Q.; Van der Giezen, D.M.; Kok, R.J.; Goldschmeding, R.; Joles, J.A. Oxidative stress in obstructive nephropathy. Int. J. Exp. Pathol. 2011, 92, 202–210. [Google Scholar] [CrossRef] [PubMed]
- Aminzadeh, M.A.; Nicholas, S.B.; Norris, K.C.; Vaziri, N.D. Role of impaired Nrf2 activation in the pathogenesis of oxidative stress and inflammation in chronic tubulo-interstitial nephropathy. Nephrol. Dial. Transplant. 2013, 28, 2038–2045. [Google Scholar] [CrossRef]
- Al Za’abi, M.; Al Busaidi, M.; Yasin, J.; Schupp, N.; Nemmar, A.; Ali, B.H. Development of a new model for the induction of chronic kidney disease via intraperitoneal adenine administration, and the effect of treatment with gum acacia thereon. Am. J. Transl. Res. 2015, 7, 28–38. [Google Scholar] [PubMed]
- Zhou, Q.; Lv, D.; Xia, Y.; Zhao, Z.; Zou, H. Decreased expression of sirtuin 3 protein correlates with early stage chronic renal allograft dysfunction in a rat kidney model. Exp. Ther. Med. 2018, 15, 3725–3732. [Google Scholar] [CrossRef] [PubMed]
- Hannken, T.; Schroeder, R.; Stahl, R.A.K.; Wolf, G. Angiotensin II-mediated expression of p27(Kip1) and induction of cellular hypertrophy in renal tubular cells depend on the generation of oxygen radicals. Kidney Int. 1998, 54, 1923–1933. [Google Scholar] [CrossRef]
- Quoilin, C.; Mouithys-Mickalad, A.; Lécart, S.; Fontaine-Aupart, M.P.; Hoebeke, M. Evidence of oxidative stress and mitochondrial respiratory chain dysfunction in an in vitro model of sepsis-induced kidney injury. Biochim. Biophys. Acta Bioenerg. 2014, 1837, 1790–1800. [Google Scholar] [CrossRef] [PubMed]
- Shin, J.H.; Kim, K.M.; Jeong, J.U.; Shin, J.M.; Kang, J.H.; Bang, K.; Kim, J.H. Nrf2-Heme Oxygenase-1 attenuates high-glucose-induced epithelial-to-mesenchymal transition of renal tubule cells by inhibiting ROS-mediated PI3K/Akt/GSK-3β signaling. J. Diabetes Res. 2019, 2019, 2510105. [Google Scholar] [CrossRef] [PubMed]
- Bae, E.H.; Cho, S.; Joo, S.Y.; Ma, S.K.; Kim, S.H.; Lee, J.; Kim, S.W. 4-Hydroxy-2-hexenal-induced apoptosis in human renal proximal tubular epithelial cells. Nephrol. Dial. Transplant. 2011, 26, 3866–3873. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.I.; Kim, H.J.; Park, J.S.; Kim, I.J.; Bae, E.H.; Ma, S.K.; Kim, S.W. PGC-1α attenuates hydrogen peroxide-induced apoptotic cell death by upregulating Nrf-2 via GSK3β inactivation mediated by activated p38 in HK-2 Cells. Sci. Rep. 2017, 7. [Google Scholar] [CrossRef]
- Ryoo, I.G.; Ha, H.; Kwak, M.K. Inhibitory role of the KEAP1-NRF2 pathway in TGFbβ1-stimulated renal epithelial transition to fibroblastic cells: A modulatory effect on SMAD signaling. PLoS ONE 2014, 9, e93265. [Google Scholar] [CrossRef] [PubMed]
- Cao, L.C.; Honeyman, T.W.; Cooney, R.; Kennington, L.; Scheid, C.R.; Jonassen, J.A. Mitochondrial dysfunction is a primary event in renal cell oxalate toxicity. Kidney Int. 2004, 66, 1890–1900. [Google Scholar] [CrossRef]
- Lal, M.A.; Brismar, H.; Eklöf, A.C.; Aperia, A. Role of oxidative stress in advanced glycation end product-induced mesangial cell activation. Kidney Int. 2002, 61, 2006–2014. [Google Scholar] [CrossRef]
- Li, M.; Zhang, T.; Wu, X.; Chen, Y.; Sun, L. High glucose provokes microvesicles generation from glomerular podocytes via NOX4/ROS pathway. Biosci. Rep. 2019, 39. [Google Scholar] [CrossRef]
- Yuan, Y.; Xu, X.; Zhao, C.; Zhao, M.; Wang, H.; Zhang, B.; Wang, N.; Mao, H.; Zhang, A.; Xing, C. The roles of oxidative stress, endoplasmic reticulum stress, and autophagy in aldosterone/mineralocorticoid receptor-induced podocyte injury. Lab. Investig. 2015, 95, 1374–1386. [Google Scholar] [CrossRef]
- Itoh, K.; Wakabayashi, N.; Katoh, Y.; Ishii, T.; Igarashi, K.; Engel, J.D.; Yamamoto, M. Keap1 represses nuclear activation of antioxidant responsive elements by Nrf2 through binding to the amino-terminal Neh2 domain. Genes Dev. 1999, 13, 76–86. [Google Scholar] [CrossRef]
- McMahon, M.; Itoh, K.; Yamamoto, M.; Hayes, J.D. Keap1-dependent proteasomal degradation of transcription factor Nrf2 contributes to the negative regulation of antioxidant response element-driven gene expression. J. Biol. Chem. 2003, 278, 21592–21600. [Google Scholar] [CrossRef]
- Ruiz, S.; Pergola, P.E.; Zager, R.A.; Vaziri, N.D. Targeting the transcription factor Nrf2 to ameliorate oxidative stress and inflammation in chronic kidney disease. Kidney Int. 2013, 83, 1029–1041. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, M.; Kensler, T.W.; Motohashi, H. The KEAP1-NRF2 system: A thiol-based sensor-effector apparatus for maintaining redox homeostasis. Physiol. Rev. 2018, 98, 1169–1203. [Google Scholar] [CrossRef]
- Maines, M.D. The heme oxygenase system: A regulator of second messenger gases. Annu. Rev. Pharmacol. Toxicol. 1997, 37, 517–554. [Google Scholar] [CrossRef]
- Uddin, M.J.; Li, C.-S.; Joe, Y.; Chen, Y.; Zhang, Q.; Ryter, S.W.; Chung, H.T. Carbon monoxide inhibits tenascin-C mediated inflammation via IL-10 expression in a septic mouse model. Mediat. Inflamm. 2015, 2015. [Google Scholar] [CrossRef] [PubMed]
- Uddin, M.J.; Jeong, S.-O.; Zheng, M.; Chen, Y.; Cho, G.J.; Chung, H.T.; Joe, Y. Carbon monoxide attenuates dextran sulfate sodium-induced colitis via inhibition of GSK-3beta Signaling. Oxidative Med. Cell. Longev. 2013. [Google Scholar] [CrossRef] [PubMed]
- Uddin, M.; Pak, E.; Ha, H. Carbon monoxide releasing molecule-2 protects mice against acute kidney injury through inhibition of ER stress. Korean J. Physiol. Pharmacol. 2018. [Google Scholar] [CrossRef]
- Ryter, S.W.; Alam, J.; Choi, A.M. Heme oxygenase-1/carbon monoxide: From basic science to therapeutic applications. Physiol. Rev. 2006, 86, 583–650. [Google Scholar] [CrossRef] [PubMed]
- Hu, Z.; Pei, G.; Wang, P.; Yang, J.; Zhu, F.; Guo, Y.; Wang, M.; Yao, Y.; Zeng, R.; Liao, W.; et al. Biliverdin Reductase A (BVRA) mediates macrophage expression of Interleukin-10 in injured kidney. Int. J. Mol. Sci. 2015, 16, 22621–22635. [Google Scholar] [CrossRef]
- Llesuy, S.F.; Tomaro, M.L. Heme oxygenase and oxidative stress. Evidence of involvement of bilirubin as physiological protector against oxidative damage. BBA Mol. Cell Res. 1994, 1223, 9–14. [Google Scholar] [CrossRef]
- Balla, G.; Jacob, H.S.; Balla, J.; Rosenberg, M.; Nath, K.; Apple, F.; Eaton, J.W.; Vercellotti, G.M. Ferritin: A cytoprotective antioxidant strategem of endothelium. J. Biol. Chem. 1992, 267, 18148–18153. [Google Scholar] [CrossRef]
- Kim, H.J.; Zheng, M.; Kim, S.K.; Cho, J.J.; Shin, C.H.; Joe, Y.; Chung, H.T. CO/HO-1 Induces NQO-1 Expression via Nrf2 Activation. Immune Netw. 2011, 11, 376–382. [Google Scholar] [CrossRef]
- Turkseven, S.; Kruger, A.; Mingone, C.J.; Kaminski, P.; Inaba, M.; Rodella, L.F.; Ikehara, S.; Wolin, M.S.; Abraham, N.G. Antioxidant mechanism of heme oxygenase-1 involves an increase in superoxide dismutase and catalase in experimental diabetes. Am. J. Physiol. Heart Circ. Physiol. 2005, 289, H701–H707. [Google Scholar] [CrossRef]
- Jarmi, T.; Agarwal, A. Heme oxygenase and renal disease. Curr. Hypertens. Rep. 2009, 11, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Hill-Kapturczak, N.; Chang, S.H.; Agarwal, A. Heme oxygenase and the kidney. DNA Cell Biol. 2002, 21, 307–321. [Google Scholar] [CrossRef] [PubMed]
- Miranda-Díaz, A.G.; Pazarín-Villaseñor, L.; Yanowsky-Escatell, F.G.; Andrade-Sierra, J. Oxidative stress in diabetic nephropathy with early chronic kidney disease. J. Diabetes Res. 2016, 2016, 7047238. [Google Scholar] [CrossRef]
- Chang, S.H.; Barbosa-Tessmann, I.; Chen, C.; Kilberg, M.S.; Agarwal, A. Glucose deprivation induces heme oxygenase-1 gene expression by a pathway independent of the unfolded protein response. J. Biol. Chem. 2002, 277, 1933–1940. [Google Scholar] [CrossRef] [PubMed]
- Di Filippo, C.; Marfella, R.; Cuzzocrea, S.; Piegari, E.; Petronella, P.; Giugliano, D.; Rossi, F.; D’Amico, M. Hyperglycemia in streptozotocin-induced diabetic rat increases infarct size associated with low levels of myocardial HO-1 during ischemia/reperfusion. Diabetes 2005, 54, 803–810. [Google Scholar] [CrossRef] [PubMed]
- Kruger, A.L.; Peterson, S.; Turkseven, S.; Kaminski, P.M.; Zhang, F.F.; Quan, S.; Wolin, M.S.; Abraham, N.G. D-4F induces heme oxygenase-1 and extracellular superoxide dismutase, decreases endothelial cell sloughing, and improves vascular reactivity in rat model of diabetes. Circulation 2005, 111, 3126–3134. [Google Scholar] [CrossRef] [PubMed]
- Abraham, N.G.; Kappas, A. Pharmacological and clinical aspects of heme oxygenase. Pharmacol. Rev. 2008, 60, 79–127. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, T.; Yamamoto, M. Molecular basis of the Keap1-Nrf2 system. Free Radic. Biol. Med. 2015, 88, 93–100. [Google Scholar] [CrossRef] [PubMed]
- Alam, J.; Stewart, D.; Touchard, C.; Boinapally, S.; Choi, A.M.; Cook, J.L. Nrf2, a Cap’n’Collar transcription factor, regulates induction of the heme oxygenase-1 gene. J. Biol. Chem. 1999, 274, 26071–26078. [Google Scholar] [CrossRef]
- Loboda, A.; Damulewicz, M.; Pyza, E.; Jozkowicz, A.; Dulak, J. Role of Nrf2/HO-1 system in development, oxidative stress response and diseases: An evolutionarily conserved mechanism. Cell. Mol. Life Sci. 2016, 73, 3221–3247. [Google Scholar] [CrossRef]
- Ahmed, S.M.; Luo, L.; Namani, A.; Wang, X.J.; Tang, X. Nrf2 signaling pathway: Pivotal roles in inflammation. Biochim. Biophys. Acta Mol. Basis Dis. 2017, 1863, 585–597. [Google Scholar] [CrossRef]
- Chen, X.; Han, K.; Zhang, T.; Qi, G.; Jiang, Z.; Hu, C. Grass carp (Ctenopharyngodon idella) NRF2 alleviates the oxidative stress and enhances cell viability through upregulating the expression of HO-1. Fish Physiol. Biochem. 2020, 46, 417–428. [Google Scholar] [CrossRef]
- Tanaka, Y.; Maher, J.M.; Chen, C.; Klaassen, C.D. Hepatic ischemia-reperfusion induces renal heme oxygenase-1 via NF-E2-related factor 2 in rats and mice. Mol. Pharmacol. 2007, 71, 817–825. [Google Scholar] [CrossRef]
- Yoh, K.; Itoh, K.; Enomoto, A.; Hirayama, A.; Yamaguchi, N.; Kobayashi, M.; Morito, N.; Koyama, A.; Yamamoto, M.; Takahashi, S. Nrf2-deficient female mice develop lupus-like autoimmune nephritis. Kidney Int. 2001, 60, 1343–1353. [Google Scholar] [CrossRef]
- Thimmulappa, R.K.; Scollick, C.; Traore, K.; Yates, M.; Trush, M.A.; Liby, K.T.; Sporn, M.B.; Yamamoto, M.; Kensler, T.W.; Biswal, S. Nrf2-dependent protection from LPS induced inflammatory response and mortality by CDDO-Imidazolide. Biochem. Biophys. Res. Commun. 2006, 351, 883–889. [Google Scholar] [CrossRef]
- Wei, Y.; Gong, J.; Yoshida, T.; Eberhart, C.G.; Xu, Z.; Kombairaju, P.; Sporn, M.B.; Handa, J.T.; Duh, E.J. Nrf2 has a protective role against neuronal and capillary degeneration in retinal ischemia-reperfusion injury. Free Radic. Biol. Med. 2011, 51, 216–224. [Google Scholar] [CrossRef] [PubMed]
- Harrison, E.M.; McNally, S.J.; Devey, L.; Garden, O.J.; Ross, J.A.; Wigmore, S.J. Insulin induces heme oxygenase-1 through the phosphatidylinositol 3-kinase/Akt pathway and the Nrf2 transcription factor in renal cells. FEBS J. 2006, 273, 2345–2356. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Wang, F.; Zhang, L.; Cao, Y.; Liu, W.; Hao, J.; Liu, Q.; Duan, H. Modulation of Nrf2 expression alters high glucose-induced oxidative stress and antioxidant gene expression in mouse mesangial cells. Cell. Signal. 2011, 23, 1625–1632. [Google Scholar] [CrossRef] [PubMed]
- Pae, H.O.; Oh, G.S.; Lee, B.S.; Rim, J.S.; Kim, Y.M.; Chung, H.T. 3-Hydroxyanthranilic acid, one of l-tryptophan metabolites, inhibits monocyte chemoattractant protein-1 secretion and vascular cell adhesion molecule-1 expression via heme oxygenase-1 induction in human umbilical vein endothelial cells. Atherosclerosis 2006, 187, 274–284. [Google Scholar] [CrossRef] [PubMed]
- Mylroie, H.; Dumont, O.; Bauer, A.; Thornton, C.C.; Mackey, J.; Calay, D.; Hamdulay, S.S.; Choo, J.R.; Boyle, J.J.; Samarel, A.M.; et al. PKCε-CREB-Nrf2 signalling induces HO-1 in the vascular endothelium and enhances resistance to inflammation and apoptosis. Cardiovasc. Res. 2015, 106, 509–519. [Google Scholar] [CrossRef] [PubMed]
- Martin, D.; Rojo, A.I.; Salinas, M.; Diaz, R.; Gallardo, G.; Alam, J.; De Galarreta, C.M.; Cuadrado, A. Regulation of heme oxygenase-1 expression through the phosphatidylinositol 3-kinase/Akt pathway and the Nrf2 transcription factor in response to the antioxidant phytochemical carnosol. J. Biol. Chem. 2004, 279, 8919–8929. [Google Scholar] [CrossRef]
- Sun, J.; Hoshino, H.; Takaku, K.; Nakajima, O.; Muto, A.; Suzuki, H.; Tashiro, S.; Takahashi, S.; Shibahara, S.; Alam, J.; et al. Hemoprotein Bach1 regulates enhancer availability of heme oxygenase-1 gene. EMBO J. 2002, 21, 5216–5224. [Google Scholar] [CrossRef]
- Dong, C.; Wu, G.; Li, H.; Qiao, Y.; Gao, S. Ampelopsin inhibits high glucose-induced extracellular matrix accumulation and oxidative stress in mesangial cells through activating the Nrf2/HO-1 pathway. Phytother. Res. 2020, 34, 2044–2052. [Google Scholar] [CrossRef]
- Zhang, J.; Zhao, X.; Zhu, H.; Wang, J.; Ma, J.; Gu, M. Apigenin protects against renal tubular epithelial cell injury and oxidative stress by high glucose via regulation of NF-E2-related factor 2 (Nrf2) pathway. Med. Sci. Monit. 2019, 25, 5280–5288. [Google Scholar] [CrossRef]
- Xie, X.; Chen, Q.; Tao, J. Astaxanthin promotes Nrf2/ARE signaling to inhibit hg-induced renal fibrosis in GMCs. Mar. Drugs 2018, 16, 117. [Google Scholar] [CrossRef]
- He, L.; Liu, G.; Shi, Y.; Peng, X.; Liu, H.; Peng, Y. Astaxanthin attenuates adriamycin-induced focal segmental glomerulosclerosis. Pharmacology 2015, 95, 193–200. [Google Scholar] [CrossRef]
- Li, D.; Shi, G.; Wang, J.; Zhang, D.; Pan, Y.; Dou, H.; Hou, Y. Baicalein ameliorates pristane-induced lupus nephritis via activating Nrf2/HO-1 in myeloid-derived suppressor cells. Arthritis Res. Ther. 2019, 21. [Google Scholar] [CrossRef]
- Elsherbiny, N.M.; Said, E.; Atef, H.; Zaitone, S.A. Renoprotective effect of calycosin in high fat diet-fed/STZ injected rats: Effect on IL-33/ST2 signaling, oxidative stress and fibrosis suppression. Chem. Biol. Interact. 2020, 315. [Google Scholar] [CrossRef] [PubMed]
- Bao, L.; Li, J.; Zha, D.; Zhang, L.; Gao, P.; Yao, T.; Wu, X. Chlorogenic acid prevents diabetic nephropathy by inhibiting oxidative stress and inflammation through modulation of the Nrf2/HO-1 and NF-ĸB pathways. Int. Immunopharmacol. 2018, 54, 245–253. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Wang, X.; Zhang, X.S.; Liang, C.Z. Cryptotanshinone attenuates oxidative stress and inflammation through the regulation of Nrf-2 and NF-κB in mice with unilateral ureteral obstruction. Basic Clin. Pharmacol. Toxicol. 2018, 123, 714–720. [Google Scholar] [CrossRef]
- Tapia, E.; García-Arroyo, F.; Silverio, O.; Rodríguez-Alcocer, A.N.; Jiménez-Flores, A.B.; Cristobal, M.; Arellano, A.S.; Soto, V.; Osorio-Alonso, H.; Molina-Jijón, E.; et al. Mycophenolate mofetil and curcumin provide comparable therapeutic benefit in experimental chronic kidney disease: Role of Nrf2-Keap1 and renal dopamine pathways. Free Radic. Res. 2016, 50, 781–792. [Google Scholar] [CrossRef]
- Ali, B.H.; Al-Salam, S.; Al Suleimani, Y.; Al Kalbani, J.; Al Bahlani, S.; Ashique, M.; Manoj, P.; Al Dhahli, B.; Al Abri, N.; Naser, H.T.; et al. Curcumin ameliorates kidney function and oxidative stress in experimental chronic kidney disease. Basic Clin. Pharmacol. Toxicol. 2018, 122, 65–73. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Liang, D.; Guo, L.; Liang, W.; Jiang, Y.; Li, H.; Zhao, Y.; Lu, S.; Chi, Z.H. Curcumin protects renal tubular epithelial cells from high glucose-induced epithelial-to-mesenchymal transition through Nrf2-mediated upregulation of heme oxygenase-1. Mol. Med. Rep. 2015, 12, 1347–1355. [Google Scholar] [CrossRef]
- Sun, W.; Liu, X.; Zhang, H.; Song, Y.; Li, T.; Liu, X.; Liu, Y.; Guo, L.; Wang, F.; Yang, T.; et al. Epigallocatechin gallate upregulates NRF2 to prevent diabetic nephropathy via disabling KEAP1. Free Radic. Biol. Med. 2017, 108, 840–857. [Google Scholar] [CrossRef]
- Wang, Y.; Wang, B.; Du, F.; Su, X.; Sun, G.; Zhou, G.; Bian, X.; Liu, N. Epigallocatechin-3-Gallate attenuates oxidative stress and inflammation in obstructive nephropathy via NF-κB and Nrf2/HO-1 signalling pathway regulation. Basic Clin. Pharmacol. Toxicol. 2015, 117, 164–172. [Google Scholar] [CrossRef]
- An, L.; Zhou, M.; Marikar, F.M.M.T.; Hu, X.W.; Miao, Q.Y.; Li, P.; Chen, J. Salvia miltiorrhiza lipophilic fraction attenuates oxidative stress in diabetic nephropathy through activation of nuclear factor erythroid 2-related factor 2. Am. J. Chin. Med. 2017, 45, 1441–1457. [Google Scholar] [CrossRef]
- Castejon, M.L.; Sánchez-Hidalgo, M.; Aparicio-Soto, M.; Montoya, T.; Martín-LaCave, I.; Fernández-Bolaños, J.G.; Alarcón-de-la-Lastra, C. Dietary oleuropein and its new acyl-derivate attenuate murine lupus nephritis through HO-1/Nrf2 activation and suppressing JAK/STAT, NF-κB, MAPK and NLRP3 inflammasome signaling pathways. J. Nutr. Biochem. 2019, 74. [Google Scholar] [CrossRef] [PubMed]
- Huang, T.; Dong, Z. Osthole protects against inflammation in a rat model of chronic kidney failure via suppression of nuclear factor-κB, transforming growth factor-β1 and activation of phosphoinositide 3-kinase/protein kinase B/nuclear factor (erythroid-derived 2)-like 2 signaling. Mol. Med. Rep. 2017, 16, 4915–4921. [Google Scholar] [CrossRef] [PubMed]
- Koca, H.B.; Pektas, M.B.; Koca, S.; Pektas, G.; Sadi, G. Diabetes-induced renal failure is associated with tissue inflammation and neutrophil gelatinase-associated lipocalin: Effects of resveratrol. Arch. Biol. Sci. 2016, 68, 747–752. [Google Scholar] [CrossRef]
- Bae, E.H.; Joo, S.Y.; Ma, S.K.; Lee, J.U.; Kim, S.W. Resveratrol attenuates 4-hydroxy-2-hexenal-induced oxidative stress in mouse cortical collecting duct cells. Korean J. Physiol. Pharmacol. 2016, 20, 229–236. [Google Scholar] [CrossRef]
- Sun, Y.; Zhang, Y.; Zhao, D.; Ding, G.; Huang, S.; Zhang, A.; Jia, Z. Rotenone remarkably attenuates oxidative stress, inflammation, and fibrosis in chronic obstructive uropathy. Mediat. Inflamm. 2014, 2014. [Google Scholar] [CrossRef]
- Lu, H.; Li, Y.; Zhang, T.; Liu, M.; Chi, Y.; Liu, S.; Shi, Y. Salidroside reduces high-glucose-induced podocyte apoptosis and oxidative stress via upregulating heme oxygenase-1 (HO-1) expression. Med. Sci. Monit. 2017, 23, 4067–4076. [Google Scholar] [CrossRef]
- Wu, P.; Yan, Y.; Ma, L.L.; Hou, B.Y.; He, Y.Y.; Zhang, L.; Niu, Z.R.; Song, J.K.; Pang, X.C.; Yang, X.Y.; et al. Effects of the Nrf2 protein modulator salvianolic acid a alone or combined with metformin on diabetes-associated macrovascular and renal injury. J. Biol. Chem. 2016, 291, 22288–22301. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.H.; Zhang, H.F.; Wang, J.H.; Wang, Y.L.; Gao, C.; Gu, Y.T.; Huang, J.; Zhang, Z. Salvianolic acid A protects the kidney against oxidative stress by activating the Akt/GSK-3 β /Nrf2 signaling pathway and inhibiting the NF- B signaling pathway in 5/6 nephrectomized rats. Oxidative Med. Cell. Longev. 2019, 2019. [Google Scholar] [CrossRef]
- Prabu, S.M.; Muthumani, M. Silibinin ameliorates arsenic induced nephrotoxicity by abrogation of oxidative stress, inflammation and apoptosis in rats. Mol. Biol. Rep. 2012, 39, 11201–11216. [Google Scholar] [CrossRef]
- Alaofi, A.L. Sinapic acid ameliorates the progression of streptozotocin (STZ)-induced diabetic nephropathy in rats via NRF2/HO-1 mediated pathways. Front. Pharmacol. 2020, 11. [Google Scholar] [CrossRef]
- Lu, C.; Fan, G.; Wang, D. Akebia Saponin D ameliorated kidney injury and exerted anti-inflammatory and anti-apoptotic effects in diabetic nephropathy by activation of NRF2/HO-1 and inhibition of NF-KB pathway. Int. Immunopharmacol. 2020, 84. [Google Scholar] [CrossRef] [PubMed]
- García Trejo, E.M.Á.; Buendía, A.S.A.; Reyes, O.S.; Arroyo, F.E.G.; García, R.A.; Mendoza, M.L.L.; Tapia, E.; Lozada, L.G.S.; Alonso, H.O. The beneficial effects of Allicin in chronic kidney disease are comparable to Losartan. Int. J. Mol. Sci. 2017, 18, 1980. [Google Scholar] [CrossRef]
- Tsai, P.Y.; Ka, S.M.; Chao, T.K.; Chang, J.M.; Lin, S.H.; Li, C.Y.; Kuo, M.T.; Chen, P.; Chen, A. Antroquinonol reduces oxidative stress by enhancing the Nrf2 signaling pathway and inhibits inflammation and sclerosis in focal segmental glomerulosclerosis mice. Free Radic. Biol. Med. 2011, 50, 1503–1516. [Google Scholar] [CrossRef]
- Zhang, H.; Qi, S.; Song, Y.; Ling, C. Artemisinin attenuates early renal damage on diabetic nephropathy rats through suppressing TGF-β1 regulator and activating the Nrf2 signaling pathway. Life Sci. 2020, 256. [Google Scholar] [CrossRef] [PubMed]
- Ma, B.; Zhu, Z.; Zhang, J.; Ren, C.; Zhang, Q. Aucubin alleviates diabetic nephropathy by inhibiting NF-κB activation and inducing SIRT1/SIRT3-FOXO3a signaling pathway in high-fat diet/streptozotocin-induced diabetic mice. J. Funct. Foods 2020, 64. [Google Scholar] [CrossRef]
- Zhang, X.; He, H.; Liang, D.; Jiang, Y.; Liang, W.; Chi, Z.H.; Ma, J. Protective effects of berberine on renal injury in streptozotocin (STZ)-Induced diabetic mice. Int. J. Mol. Sci. 2016, 17, 1327. [Google Scholar] [CrossRef] [PubMed]
- Xie, R.; Zhang, H.; Wang, X.Z.; Yang, X.Z.; Wu, S.N.; Wang, H.G.; Shen, P.; Ma, T.H. The protective effect of betulinic acid (BA) diabetic nephropathy on streptozotocin (STZ)-induced diabetic rats. Food Funct. 2017, 8, 299–306. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.M.; Hua, K.F.; Lin, Y.C.; Chen, A.; Chang, J.M.; Kuoping Chao, L.; Ho, C.L.; Ka, S.M. Citral is renoprotective for focal segmental glomerulosclerosis by inhibiting oxidative stress and apoptosis and activating Nrf2 pathway in mice. PLoS ONE 2013, 8, e74871. [Google Scholar] [CrossRef]
- Qiao, Y.; Xu, L.; Tao, X.; Yin, L.; Qi, Y.; Xu, Y.; Han, X.; Tang, Z.; Ma, X.; Liu, K.; et al. Protective effects of dioscin against fructose-induced renal damage via adjusting Sirt3-mediated oxidative stress, fibrosis, lipid metabolism and inflammation. Toxicol. Lett. 2018, 284, 37–45. [Google Scholar] [CrossRef]
- Chen, L.; Chen, D.Q.; Wang, M.; Liu, D.; Chen, H.; Dou, F.; Vaziri, N.D.; Zhao, Y.Y. Role of RAS/Wnt/β-catenin axis activation in the pathogenesis of podocyte injury and tubulo-interstitial nephropathy. Chem. Biol. Interact. 2017, 273, 56–72. [Google Scholar] [CrossRef]
- Yu, X.; Fang, Y.; Ding, X.; Liu, H.; Zhu, J.; Zou, J.; Xu, X.; Zhong, Y. Transient hypoxia-inducible factor activation in rat renal ablation and reduced fibrosis with L-mimosine. Nephrology 2012, 17, 58–67. [Google Scholar] [CrossRef] [PubMed]
- Bonomini, F.; Dos Santos, M.; Veronese, F.V.; Rezzani, R. NLRP3 inflammasome modulation by melatonin supplementation in chronic pristane-induced lupus nephritis. Int. J. Mol. Sci. 2019, 20, 3466. [Google Scholar] [CrossRef]
- Zhang, B.; Zhang, X.; Zhang, C.; Shen, Q.; Sun, G.; Sun, X. Notoginsenoside R1 protects db/db mice against diabetic nephropathy via upregulation of Nrf2-mediated HO-1 expression. Molecules 2019, 24, 247. [Google Scholar] [CrossRef]
- Zhou, J.; Wang, T.; Wang, H.; Jiang, Y.; Peng, S. Obacunone attenuates high glucose-induced oxidative damage in NRK-52E cells by inhibiting the activity of GSK-3β. Biochem. Biophys. Res. Commun. 2019, 513, 226–233. [Google Scholar] [CrossRef]
- Hong, Y.A.; Lim, J.H.; Kim, M.Y.; Kim, E.N.; Koh, E.S.; Shin, S.J.; Choi, B.S.; Park, C.W.; Chang, Y.S.; Chung, S. Delayed treatment with oleanolic acid attenuates tubulointerstitial fibrosis in chronic cyclosporine nephropathy through Nrf2/HO-1 signaling. J. Transl. Med. 2014, 12. [Google Scholar] [CrossRef]
- Wang, Z.; Han, N.; Zhao, K.; Li, Y.; Chi, Y.; Wang, B. Protective effects of pyrroloquinoline quinine against oxidative stress-induced cellular senescence and inflammation in human renal tubular epithelial cells via Keap1/Nrf2 signaling pathway. Int. Immunopharmacol. 2019, 72, 445–453. [Google Scholar] [CrossRef]
- Qin, T.; Yin, S.; Yang, J.; Zhang, Q.; Liu, Y.; Huang, F.; Cao, W. Sinomenine attenuates renal fibrosis through Nrf2-mediated inhibition of oxidative stress and TGFβ signaling. Toxicol. Appl. Pharmacol. 2016, 304, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Khaleel, S.A.; Raslan, N.A.; Alzokaky, A.A.; Ewees, M.G.; Ashour, A.A.; Abdel-Hamied, H.E.; Abd-Allah, A.R. Contrast media (meglumine diatrizoate) aggravates renal inflammation, oxidative DNA damage and apoptosis in diabetic rats which is restored by sulforaphane through Nrf2/HO-1 reactivation. Chem. Biol. Interact. 2019, 309. [Google Scholar] [CrossRef] [PubMed]
- Lv, D.; Zhou, Q.; Xia, Y.; You, X.; Zhao, Z.; Li, Y.; Zou, H. The association between oxidative stress alleviation via sulforaphane-induced Nrf2-HO-1/NQO-1 signaling pathway activation and chronic renal allograft dysfunction improvement. Kidney Blood Press. Res. 2018, 43, 191–205. [Google Scholar] [CrossRef]
- Peerapen, P.; Thongboonkerd, V. Protective roles of trigonelline against oxalate-induced epithelial-to-mesenchymal transition in renal tubular epithelial cells: An in vitro study. Food Chem. Toxicol. 2020, 135. [Google Scholar] [CrossRef] [PubMed]
- Gong, W.; Li, J.; Chen, Z.; Huang, J.; Chen, Q.; Cai, W.; Liu, P.; Huang, H. Polydatin promotes Nrf2-ARE anti-oxidative pathway through activating CKIP-1 to resist HG-induced up-regulation of FN and ICAM-1 in GMCs and diabetic mice kidneys. Free Radic. Biol. Med. 2017, 106, 393–405. [Google Scholar] [CrossRef] [PubMed]
- Jiménez-Osorio, A.S.; García-Niño, W.R.; González-Reyes, S.; Álvarez-Mejía, A.E.; Guerra-León, S.; Salazar-Segovia, J.; Falcón, I.; Montes de Oca-Solano, H.; Madero, M.; Pedraza-Chaverri, J. The effect of dietary supplementation with curcumin on redox status and Nrf2 activation in patients with nondiabetic or diabetic proteinuric chronic kidney disease: A pilot study. J. Ren. Nutr. 2016, 26, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Alvarenga, L.; Salarolli, R.; Cardozo, L.F.M.F.; Santos, R.S.; de Brito, J.S.; Kemp, J.A.; Reis, D.; de Paiva, B.R.; Stenvinkel, P.; Lindholm, B.; et al. Impact of curcumin supplementation on expression of inflammatory transcription factors in hemodialysis patients: A pilot randomized, double-blind, controlled study. Clin. Nutr. 2020. [Google Scholar] [CrossRef] [PubMed]
| No. | Modulator | Chemical Class and Natural Sources | Experimental Model | Disease Model | Pathobiology Involved | Major Research Outcomes | Molecular Markers | Ref. |
|---|---|---|---|---|---|---|---|---|
| Phenolic compounds | ||||||||
| 1 | Ampelopsin | Flavonoid; Ampelopsis grossedentata | HG-stimulated hGMCs | OS | OS, ECM accumulation | Amelioration of OS and ECM accumulation | ↓ROS, ↓MDA, ↑SOD, ↓Nox2, ↓Nox4, ↓NADPH, ↓FN, ↓Col IV, ↑n-Nrf2, ↑HO-1, | [109] |
| 2 | Apigenin | Flavonoid; common fruits and vegetables | HG-treated HK-2 cells | Oxidative damage | Oxidative damage | Decrease in apoptosis, inhibition of OS, and inflammatory response | ↓LDH, ↓MDA, ↑SOD, ↑CAT, ↓TNFα, ↓IL-1β, ↓IL-6, ↑Nrf2, ↑HO-1 | [110] |
| 3 | Astaxanthin | Xanthophyll carotenoid; algae, shrimp, lobster, crab, salmon, and other organisms | STZ-injected rat | DKD | ECM accumulation | Amelioration of kidney injury | ↓FN, ↓TGFβ1, ↓ICAM-1 | [111] |
| HG-treated GMCs | Kidney fibrosis | OS | Increase in antioxidative capacity | ↓FN, ↓TGFβ1, ↓ICAM-1, ↑SOD, ↓MDA, ↓ROS, ↓DHE, ↑n-Nrf2, ↓keap1, ↓SOD-1, ↓Nqo1, ↓HO-1 | ||||
| Adriamycin-treated BALB/c mice | FSGS | OS, inflammation | Anti-inflammation, antioxidation | ↓TGFβ1, ↓collagen1, ↓α-SMA, ↓MDA, ↑GSH, ↑SOD, ↑CAT, (serum: ↓IL-1 β, IL-18), ↑Nrf2, ↓NLRP3 | [112] | |||
| 4 | Baicalein | Flavonoid; roots of Scutellaria baicalensis Georgi | Pristine -injected BALB/c mice | LN | OS, inflammation | Attenuation of kidney dysfunction, antioxidation, anti-inflammation, inhibition of MDSC expansion | ↓IL-1b, ↓IL-18, ↓O2¯˙, ↑ GPx, ↑Nrf2, ↑HO-1, ↓ NLRP3, ↓Casp-1, ↓mIL-1 β, ↓p-NF-kB | [113] |
| LPS-primed spleen-derived MDSCs | OS, inflammation | ↓ROS, ↓IL-1β, ↓IL-18, ↑Nrf2, ↑HO-1, ↓NLRP3, ↓mIL-1β/pro-IL-1β, ↓Casp-1-p20/pro-casp-1-p45, ↓p-NF-kB/NF-kB, ↓Ang-1, ↓p47phox, ↓GP91phox, ↓iNOS | ||||||
| 5 | Calycosin | Isoflavone; root of Astragalus membranaceus | HFD-fed/ STZ-injected SD rat | DKD | Inflammation, OS, fibrosis | Inhibition of inflammatory, oxidative, and fibrotic events | ↓IL-33, ↓ST2, ↓NF-kB p65, ↓TNFα, ↓IL-1 β, ↓IL-6, ↑Nrf2, ↓MDA, ↓TGFβ | [114] |
| 6 | Chlorogenic acid | Cinnamate ester; coffee, fruits, and vegetables | STZ-injected and HFD-fed SD rat | DKD | OS, inflammation | Relieve kidney injury, mitigation of OS, inflammation | ↓MDA, ↑SOD, ↑GSH-Px, ↑n-Nrf2, ↑HO-1, ↓IL-6, ↓TNFα, ↓IL-1 β, ↑c-NF-kB, ↓n-NF-kB, ↑IkBα, ↓p-IkBα, | [115] |
| HG-treated rat mesangial cell line (HBZY-1) | Mitigation of OS, inflammation, increase in cell proliferation | ↑n-Nrf2, ↑HO-1, ↑c-NF-kB, ↓n-NF-kB, ↑IkBα, ↓p-IkBα, ↓IL-6, ↓TNFα, ↓IL-1 β | ||||||
| 7 | Cryptotanshinone | Quinoid diterpene; Salvia miotiorrhiza bunge | UUO-operated mice | Kidney fibrosis | OS, inflammation | Attenuation of OS and inflammation | ↓collagen-1, ↓FN, ↓CD68, ↓CD3, ↑IkBα, ↓NF-kB p65, ↑SOD2, ↑CAT, ↑GSH, ↓MDA, ↑Nuclear Nrf2, ↓cytosolic Nrf2, ↑HO-1 | [116] |
| 8 | Curcumin | Curcuminoid; turmeric (Curcuma longa) | 5/6 nephrectomy Wistar rat | CKD | OS, inflammation | Protection of kidney function, antioxidant, anti-inflammation | ↓Nox4, ↑eNOS, ↓nitrotyrosine, ↓MCP-1, ↓Keap-1, ↑Nrf2, ↑GPx-1, ↑CAT, ↑SOD-1, ↓phospho serine D1R | [117] |
| 0.25% Adenine -diet rat | CKD | OS, inflammation | Amelioration of kidney function and OS | ↓IL-1 β, ↓IL-6, ↓TNFα, ↑cycstatin C, ↓adiponecitn, ↑sclerostin, ↑SOD, ↑Nrf2, ↑GSH reductase. ↓ caspase3 | [118] | |||
| HG-treated NRK-52E cells | OS | OS | Increase in cell viability, inhibition of EMT | ↑E-cadherin, ↓α-SMA, ↑Nrf2, ↑HO-1 | [119] | |||
| 9 | Epigallocatechin-3 -Gallate | Polyphenol; Dried leaves of tea plant (Camellia sinensis) | STZ-injected mice | DKD | Oxidative damage, inflammation, | Anti-OS | ↓TGFβ1, ↓PAI-1, ↓ICAM-1, ↓VCAM-1, ↓MDA, ↓iNOS, ↓3-NT, ↑Nqo1, ↑HO-1, ↑t-Nrf2, ↑c-Nrf2, ↑n-Nrf2, ↑n-Nrf2/t-Nrf2 | [120] |
| HG-cultured MMC | ↑t-Nrf2, ↑c-Nrf2, ↑n-Nrf2, ↑Nqo1, ↑HO-1, ↓MDA, ↓iNOS, ↓VCAM-1, ↓ICAM-1, ↓COL4, ↓FN | |||||||
| NZB/W F1 lupus-prone mice | LN | OS | Antioxidant and anti-inflammation | ↑Nrf2, ↓p47phox, ↑Nqo1, ↑HO-1, ↑GPx, ↓CD3, ↓F4/80, ↓NF-kB, ↓NLRP3, ↓IL-1 β, ↓IL-18, ↓casp1-p20, | [56] | |||
| UUO mice | CKD | OS, inflammation | Kidney function improvement, prevention of OS and inflammation | ↑SOD, ↑CAT, ↑GSH-Px, ↓MPO, ↓TNFα, ↓IL-6, ↓IL-1 β, ↑IkBα, ↓p-IkBα, ↓NF-kB, ↑n-Nrf2, ↑HO-1, ↑t-bilirubin | [121] | |||
| 10 | Ethyl acetate extract of Saliva miltiorrhiza | Diterpenoids, phenolic compounds, flavonoids, triterpenoids; dried root of Salvia miltiorrhiza Bunge | STZ-injected mice | DKD | Oxidative stress | Antioxidation, attenuation of kidney dysfunction | ↑Nrf2, ↑HO-1, ↑Nqo1, ↓Keap1 | [122] |
| HG-treated SV40-MES-13 MMCs | hyperglycemia | Antioxidation | ↓ROS, ↑Nrf2, ↑HO-1, ↑Nqo1, ↓Keap1 | |||||
| 11 | Isoliquiritin | Flavonoid glycoside; Chinese licorice (Glycyrrhiza uralensis) | Cationic BSA-injected SD rat | MGN | Inflammation and OS | Antioxidative, anti-inflammatory activities | ↓Keap1, ↑Nrf2, ↓n-Nrf2, ↑c-Nrf2, ↑HO-1, ↑Nqo1, ↓MDA, ↓NO, ↑SOD, ↑CAT, ↑GPx, ↑GSH, ↓NF-kB p65, ↓nuclear NF-kB p65, ↑cyclic NF-kB, ↓IKKb, ↓p-IKKb, ↓TNFα, ↓IL-1 β, ↓COX2, ↓iNOS, ↓p38 MAPK, ↓p-p38 MAPK | [54] |
| 12 | Oleuropein, peracetylatedoleuropein | Secoiridoid; olive leaves, roots, and unprocessed olive drupes | Pristine -injected BALB/c mice | LN | Inflammation and OS | Amelioration of kidney abnormalities, inhibition of proinflammation, antioxidation | ↓MMP-3, ↓iNOS, ↓mPGEs-1, ↓PGE2, ↑Nrf2, ↑HO-1, ↓pSTAT3, ↓NF-kB-p65, ↑IkBα, ↓pp38, ↓pJNK, ↓pERK1/2 ↓NLRP3, ↓ASC, ↓IL-18, ↓ IL-1β, ↓cleaved caspase-1, ↓cleaved caspase 11 | [123] |
| 13 | Osthole | Coumarin; Fructus Cnidii | 2% adenine suspension -received rat | CKD | Inflammation | Protection of kidney function, antiinflammation | ↓TNFα, ↓IL-6, ↓IL-8, ↓NF-kB/p65, ↓TGFβ1, ↓MCP-1, ↑p-Akt/Akt, ↑Nrf2 | [124] |
| 14 | Polydatin | Stilbenoid glucoside; Polygonum cuspidatum Sieb.et Zucc | STZ-injected diabetic mice | DKD | OS | Improvement of antioxidative effect and kidney dysfunction | ↑CKIP-1, ↑Nrf2, ↑HO-1, ↑SOD1, ↓FN, ↓ICAM-1, ↓MDA, ↑t-SOD | |
| HG-treated rat GMCs | ↑Nrf2, ↓Keap1, ↑n-Nrf2, ↓n-CKIP-1, ↑ARE binding activity, ↑HO-1, ↑SOD1, ↓DHE, ↓H2O2, ↓FN, ↓ICAM-1 | |||||||
| 15 | Resveratrol | Phytoalexin; red grapes (Vitis vinifera L.), peanuts (Arachis spp.), berries (Vaccinium spp.) | STZ-induced Wistar rat | DKD | OS | Anti-inflammation, Anti-OS | ↓iNOS, ↓NF-kB, ↓Nrf2, ↓NGAL, ↓IL-1β, ↓IL-6, ↓IL-8, ↓TNFα | [125] |
| 4-hydroxy-2-hexenal-treated mouse cortical collecting duct cells (M1) | OS | ↓nuclear p65, ↑cytosol IkB, ↑SIRT1, ↓Nox4, ↓COX2, ↑AQP2, ↓pERK/ERK, ↓pJNK/JNK, ↓pP38/P38, ↓Nrf2, ↑Keap1 | [126] | |||||
| 16 | Rotenone | Isoflavonone; seeds and stems of jicama vine plant, the roots of Fabaceae, etc. | UUO-operated mice | Kidney fibrosis | Mitochondrial abnormality | Anti-OS, anti-inflammation, anti-fibrosis | ↓TBARS, ↓HO-1, ↓TNFα, ↓IL-1β, ↓ICAM1, ↓collagen I, ↓FN, ↓α-SMA, ↓PAI-1, ↓collagen III, ↓TGFβ, ↑mtDNA, ↑mtNd1 | [127] |
| 17 | Salidroside | phenylpropanoid glycoside; plant Rhodiola rosea | HG-treated mouse podocytes | Apoptosis | Apoptosis | Improvement of cell viability | ↓Caspase-9, ↓caspase-3, ↑HO-1, ↑p-ILK/ILK, ↑p-Akt/Akt, ↑p-ERK/ERK, ↑p-JNK/JNK, ↓p-p38/p38, ↑Nrf2 | [128] |
| 18 | Salvianolic acid A | Polyphenol derivative; root of Salvia miltiorrhiza | STZ-injected mice | DKD | OS | Anti-OS | ↓VCAM-1, ↑HO-1, ↓α-SMA, ↓NT, ↓DHE, ↑GPx-1 | [129] |
| HG-treated HK-2 cells | ↑HO-1, ↓α-SMA, ↓p65, ↓ROS | |||||||
| 5/6 nephrectomized SD rats | CKD | OS | OS attenuation, | ↑t-SOD, ↑GPx, ↑CAT, ↓MDA, ↓ROS, ↓Nox4, ↑p-Akt/Akt, ↑p-GSK3β/GSK3β, ↑p-Nrf2/Nrf2, ↑HO-1 | [130] | |||
| H2O2-treated/LPS-treated HK-2 cells | Cell viability improvement, decrease in OS | ↑t-SOD, ↑GPx, ↑CAT, ↓MDA, ↓ROS, ↓Nox4, ↑p-Akt/Akt, ↑p-GSK3β/GSK3β, ↑n-Nrf2, ↑HO-1, ↓p-NF-kB p65/NF-kB p65, ↓ICAM-1, ↓p-NF-kB p65, ↓ICAM-1, ↑n-Nrf2, ↑HO-1 | ||||||
| 19 | Silibinin | Flavonoliganas: milk thistle seeds | Arsenic -induced rat | CKD | Inflammation | Attenuation of OS, inflammation, and apoptosis | ↓TNFα, ↓iNOS, ↓NO, ↓NF-kB, ↓Caspase-3, ↓NADPH oxidase, ↑Nrf2 | [131] |
| 20 | Sinapnic acid | Hydroxycinnamic acid; wine, vinegar | STZ-injected rat | DKD | OS, inflammation | Amelioration of OS and inflammation | ↑CAT, ↑GPx, ↑SOD, ↓TNFα, ↓IL-6, ↓NO2, ↓MDA, ↓TFGβ, ↑HO-1, ↑Nrf2, ↓NF-kB, ↑IkBα, ↑Bcl2, ↓Caspase3, ↓Bax | [132] |
| No. | Modulator | Chemical Class and Natural Sources | Experimental Model | Disease Model | Pathobiology Involved | Major Research Outcomes | Molecular Markers | Ref. |
|---|---|---|---|---|---|---|---|---|
| Non-phenolic compounds | ||||||||
| 1 | Akebia Saponin D | triterpenoid saponin; Dipsaci Radix | STZ-injected mice | DKD | OS, inflammation | Amelioration of kidney damage, inflammation, OS, and apoptosis | ↓TNFα, ↓IL-1β, ↓IL-6, ↓MCP-1, ↓ROS, ↓MDA, ↓LDH, ↑SOD, ↑Bcl2, ↓Bax, ↓cleaved caspase3/caspase3, ↓cleaved caspase9/caspase9, ↑n-Nrf2, ↓p-NF-kB/t-NF-kB, ↑HO-1, ↑Nqo1, ↓p-IkBα/t-IkBα | [133] |
| HG-treated HK-2 cells | ↓TNFα, ↓IL-1β, ↓IL-6, ↓MCP-1, ↓ROS, ↓MDA, ↓LDH, ↑SOD, ↑Bcl2, ↓Bax, ↓cleaved caspase3/caspase3, ↓cleaved caspase9/caspase9, ↑Nrf2, ↓p-NF-kB/t-NF-kB, ↑HO-1, ↑Nqo1, ↓p-IkBα/t-IkBα | |||||||
| 2 | Allicin | Diallyl thiosulfinate; garlic (Allium sativum L.) | 5/6 nephrectomy Wistar rat | CKD | Fibrosis, OS | Antihypertensive and antioxidant effects | ↑AT1R, ↑AT2R, ↑Nrf2, ↓Keap1, ↑CAT, ↑SOD, ↓HO-1, ↑eNOS | [134] |
| 3 | Antroquinonol | Enone; mushroom (Antrodia camphorate) | Adriamycin -injected BALB/c mice | FSGS | OS | Decrease in kidney dysfunction, anti-OS, anti-inflammation | ↓desmin, ↓O2●−, (serum, urine ↓ O2●−, ↓NO), ↓DHE, ↓p47phox, ↑Nrf2, ↑GPx, ↓NF-kB p65, ↓MCP-1, ↓IL-6, ↓CD3, ↓F4/80, ↓Col I, ↓Col III, ↓Col IV, ↓TGFβ1 | [135] |
| 4 | Artemisinin | sesquiterpene lactones; Asteraceae Artemisia annua | STZ-injected rat | DKD | OS | Amelioration of kidney dysfunction and OS | ↓MDA, ↑t-SOD, ↑GPx, ↓TGFβ1, ↑t-Nrf2, ↑n-Nrf2, ↑HO-1, ↑Nqo1 | [136] |
| 5 | Aucubin | iridoid glycoside; leaf of Eucommia ulmoides | HFD-fed and STZ-injected mice | DKD | OS, inflammation | Amelioration of kidney dysfunction, anti-inflammation, anti-OS | ↓FN, ↓collagen IV, ↓MDA, ↑SOD, ↑CAT, ↑GSH/T-GSH, ↓TNFα, ↓IL-6, ↓IL-1β, ↓p65, ↓IkBα, ↑Nrf2, ↑HO-1, ↑Nqo1, ↑FOXO3α, ↓p-FOXO3α/FOXO3α, ↑SIRT1, ↑SIRT3, ↓Ac-FOXO3α/FOXO3α | [137] |
| 6 | Berberine | isoquinoline alkaloid; Coptidis Rhizoma and Cortex Phellodendri | STZ-injected mice | DKD | OS | Anti-fibrosis | ↓α-SMA, ↓collagen-1, ↑Nrf2, ↑NQO1, ↑HO-1 | [138] |
| HG-treated NRK 52E cells | EMT | ↓E-cadherin, ↓α-SMA, ↑n-Nrf2, ↑Nqo1, ↑HO-1, ↓p-Smad2, ↓p-Smad3 | ||||||
| 7 | Betulinic acid | pentacyclic triterpenoid; from the outer bark of white birch trees (Betula alba) | STZ-injected SD rat | DKD | OS | Anti-OS | ↓IL-1 β, ↓IL-6, ↓MDA, ↑SOD, ↑CAT, ↑p-AMPK/AMPK, ↓p-IkBα/IkBα, ↓p-NF-kB/NF-kB, ↑Nrf2, ↑HO-1 | [139] |
| 8 | Citral | Terpeonids; Litsea cubeba | Adriamycin -injected BALB/c mice | FSGS | OS | Amelioration of kidney dysfunction, anti-OS, anti-inflammation, anti-apoptosis | ↓O2¯˙, (serum, urine ↓O2¯˙, ↓NO), ↓DHE, ↓p47phox, ↑Nrf2, ↑Nqo1, ↑HO-1, ↓desmin, ↓TUNEL, ↓Casp-3p17, ↓Casp-9p37, ↓Bax/Bcl2, ↓pNF-kB p65, ↓MCP-1, ↓ CD3, ↓F4/80 | [140] |
| LPS-treated RAW 264.7 macrophages | OS | ↓NO, ↓NF-kB, ↓IL-6, ↓TNFα, ↓IL-1β, ↓p-ERK1/2(10min), ↓p-JNK1/2(15,30min) | ||||||
| 9 | Dioscin | Steroid saponin; Dioscoreae rhizoma | 10% fructose -fed mice | CKD | Oxidative damage, lipid metabolism, fibrosis | Inhibition of inflammation, lipid metabolism, OS, kidney fibrosis | ↓MDA, ↑SOD, ↑GSH-Px, ↓α-SMA, ↑SIRT3, ↑SOD2, ↓IL-1β, ↓IL6, ↓TNFα, ↓NF-kB, ↓HMGB1, ↓COX2, ↓c-Jun, ↓c-Fos, ↓SREBP-1c, ↓SCD-1, ↓FASn, ↓p-Akt, ↓p-FoxO1A, ↓ACC, ↑CPT1, ↑Nrf2, ↓Keap1, ↑GST, ↓TGFβ1, ↓p-Smad3, ↑Smad7 | [141] |
| 10 | Ergone (alisol B 23-acetate, pachymic acid B) | steroid; Polyporus umbellatus, surface layer of Poria cocos, Alisma orientale | AngII- treated HK-2 and conditionally immortalized MPC5 cells | CKD | OS, inflammation, impaired Nrf 2 activation | inhibition of the RAS/Wnt/b-catenin signaling cascade | (HK-2) ↓Snail1, ↓MMP-7, ↓Twist, ↓FSP-1, ↓Col I, ↓Col III, ↓α-SMA, ↓vimentin, ↑E-cadherin, ↓NF-kB, ↓MCP-1, ↓COX2, ↑Nrf2, ↑HO-1 (podocyte) ↓Snail1, ↓MMP-7, ↓Twist, ↓FSP-1, ↑podocin, ↑nephrin, ↑podocalyxin, ↑synaptopodin, ↓desmin, ↑WT1, ↓Akt2, ↓NF-kB, ↓MCP-1, ↓COX2, ↑Nrf2, ↑HO-1 | [142] |
| 11 | L-mimosine | Amino acid; Mimosa pudica | Rats with remnant kidneys after subtotal nephrectomy (5/6 nephrectomy) | CKD | Fibrosis | Improvement of kidney function, inhibition of fibrosis | ↑HIF-1α, ↑HIF-2α, ↑VEGF, ↑HO-1, ↑GLUT-1, ↓α-SMA, ↓collagen III | [143] |
| 12 | Melatonin | Endogenous indoleamine, coffee, walnut, etc. | Pristine -injected BALB/c mice | LN | OS, inflammation | Attenuation of OS, inflammation | ↑SIRT1, ↑Nrf2, ↓TNFα, ↓NF-kB, ↓iNOS, ↓NLRP3, ↑CD31 | [144] |
| 13 | Notoginsenoside R1 | Saponin; Panax notoginseng | db/db mice | DKD | OS | Anti-OS, decrease in apoptosis | ↓Collagen I, ↓TGFβ1, ↑Nrf2, ↑HO-1, ↓Bax/Bcl2, ↓Caspase-3, ↓Caspase-9 | [145] |
| AGEs-treated HK-2 cells | Mitochondria injury | ↓LDH, ↓ROS, ↑n-Nrf2, ↑HO-1, ↓Bax/Bcl2, ↓Cspase-3, ↓Caspase-9, ↓TGFβ1, ↓collagen I | ||||||
| 14 | Obacunone | Triterpenoid limonoid; citrus and other plants of the Rutaceae family | HG-treated NRK-52E cells | OS | OS | Inhibition of OS, mitochondrial injury, and apoptosis | ↑SOD, ↑GSH, ↑CAT, ↓ROS, ↓JC-1 monomer/aggregate, ↑p-GSK3β/GSK3β, ↓n-Fyn, ↑n-Nrf2, ↑Nqo1, ↑HO-1, ↑SOD, ↑GSH, ↑CAT, ↓c-CytC/m-CytC, ↓cleaved caspase3 | [146] |
| 15 | Oleanolic acid | Triterpenoid; olive oil, Phytolacca Americana, Syzygium spp, garlic, etc. | Cyclosporine -treated ICR mice | Chronic nephropathy | Inflammation, fibrosis | Antioxidation, anti-inflammation | ↓α-SMA, ↑HO-1, ↑nuclear/total Nrf2, ↑SOD1, ↓MDA, ↓urinary 8-iso-PGF2α, ↓urine 8-oxo-dG, ↓Bax/Bcl2, ↓active caspase-3 | [147] |
| 16 | Pyrroloquinoline quinone | In soil and foods such as kiwifruit and human breast milk | HG-treated HK-2 cells | OS | OS | Decrease in OS, inflammation and cellular senescence | ↓IL-1β, ↓TNFα, ↓NF-kB, ↓p16, ↓p21, ↓ROS, ↑SOD2, ↑CAT, ↓keap1, ↑Nrf2, ↑HO-1, ↑Nqo1, ↑GST, ↑GPx3, | [148] |
| 17 | Sinomenine | Alkaloid; Sinomenium acutum | UUO-operated ICR mice | CKD | Fibrosis, OS | Anti-fibrosis, antioxidation | ↑E-cadherin, ↓α-SMA, ↓FN, ↑HO-1, ↑Nqo1, ↑Nrf2, ↑SOD, ↑GPx, ↑CAT, ↑SOD2, ↓p-Smad3, ↓β-catenin | [149] |
| TGFβ-treated/H2O2-treated HEK293 cells, TGFβ-treated RAW264.7 cells | ↑E-cadherin, ↓α-SMA, ↓FN, ↑HO-1, ↑Nqo1, ↑Nrf2, ↑SOD, ↑GPx, ↑CAT, ↑SOD2, ↓p-Smad3, ↓β-catenin | |||||||
| 18 | Sulforaphane | Isothiocyanate (organosulfur compound); Cruciferous vegetables such as broccoli, brussels sprouts, and cabbages | STZ-injected and meglumine diatrizoate-injected Wistar rats | DKD, CIN | OS | Renoprotective | ↓MDA, ↓8-oxo-dG, ↑Nrf2, ↑HO-1, ↓IL6, ↑Caspase3 | [150,151] |
| Meglumine diatrizoate-treated NRK-52E cells | Cell viability | ↑Nrf2, ↑HO-1, ↓IL6 | ||||||
| F344 rat kidneys transplanted Lewis rat | CRAD | OS | OS alleviation, kidney functional and morphological improvements | ↓MDA, ↓8-isoprostane, ↓ox-LDL, ↓8-oxo-dG, ↑SOD, ↑CAT, ↑GPx, ↑GR, ↑ γ-GCS, ↑Nrf2, ↑HO-1, ↑Nqo-1 | [151] | |||
| 19 | Trigonelline | Alkaloid; traditional herbs (especially fenugreek), coffee bean, soybean, and other edible food plants | Oxalate-induced MDCK cells | EMT | Fibrosis | Attenuation of EMT, prevention of cell migration and ROS overproduction, | ↓FN, ↓vimentin, ↓α-SMA, ↑ E-cadherin, ↑ZO-1, ↓MMP9, ↓ROS, ↑Nrf2 | [152] |
| Compound | Conditions or Disease | Phase of Clinical Trials | Outcome Measures | Clinical trials.gov Identifier or Ref. | |
|---|---|---|---|---|---|
| Curcumin | Curcumin (320 mg/day, for 8 weeks) | CKD | Phase III (2013.2-2014. 4, 101 participants) | Oxidative stress markers (MDA, GSH, GSSG), antioxidants (GPx, SOD, CAT, Nrf2 activity. | NCT01831193 [154] |
| Curcumin supplementation (500 mg of curcumin and 5 mg of piperine/day, for 12 weeks) | CKD | Not applicable (2018.2–2021.12, 31 participants) | Antioxidants (Nrf2, GPx, HO-1) and inflammatory biomarkers (NF-kB, IL-6, TNFα) in blood samples | NCT03475017 [155] | |
| Curcumin supplementation (500 mg of curcumin and 5 mg of piperine/day, for 12 weeks) | CKD, Peritoneal dialysis, hemodialysis | Not applicable (2020.10–2021.10, 30 participants) | Antioxidants (Nrf2, GPx, HO-1) and inflammatory biomarkers (NF-kB, IL-6, TNFα, CRP, IL-18, TBARS, inflammasome) in blood samples | NCT04413266 | |
| Curcumin, NFE2L2 A > G (400 mg/2 times/day, for up to 24 weeks) | CKD, Type 2 diabetes mellitus, Polymorphism | Phase II/III (2018.8–2019.4, 176 participants) | Antioxidants (Nrf2, SOD, HO-1, GPx) | NCT03262363 | |
| Resveratrol | Resveratrol (500 mg/day, for 4 weeks) | CKD | Phase III (2013.01–2014.12, 20 participants) | Antioxidants (Nrf2, GPx, HO-1) and inflammatory biomarkers (NF-kB, IL-6, TNFα) in blood samples | NCT02433925 |
| Resveratrol 200 mg/2 times/day, for 6 weeks) | CKD, Endothelial dysfunction | Not applicable (2019.1–2021. 8, 25 participants) | Oxidative stress | NCT03597568 | |
| Sulforaphane | Sulforaphane (4 g L-sulforaphane/day, for 2 months + 4 g corn starch colored with chlorophyll /day, for 2 months) | CKD | Not applicable (2021.1–2022.12, 122 participants) | Antioxidants (Nrf2, GPx, HO-1) and inflammatory biomarkers (NF-kB, IL-6, TNFα) in blood samples | NCT04608903 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Uddin, M.J.; Kim, E.H.; Hannan, M.A.; Ha, H. Pharmacotherapy against Oxidative Stress in Chronic Kidney Disease: Promising Small Molecule Natural Products Targeting Nrf2-HO-1 Signaling. Antioxidants 2021, 10, 258. https://doi.org/10.3390/antiox10020258
Uddin MJ, Kim EH, Hannan MA, Ha H. Pharmacotherapy against Oxidative Stress in Chronic Kidney Disease: Promising Small Molecule Natural Products Targeting Nrf2-HO-1 Signaling. Antioxidants. 2021; 10(2):258. https://doi.org/10.3390/antiox10020258
Chicago/Turabian StyleUddin, Md Jamal, Ee Hyun Kim, Md. Abdul Hannan, and Hunjoo Ha. 2021. "Pharmacotherapy against Oxidative Stress in Chronic Kidney Disease: Promising Small Molecule Natural Products Targeting Nrf2-HO-1 Signaling" Antioxidants 10, no. 2: 258. https://doi.org/10.3390/antiox10020258
APA StyleUddin, M. J., Kim, E. H., Hannan, M. A., & Ha, H. (2021). Pharmacotherapy against Oxidative Stress in Chronic Kidney Disease: Promising Small Molecule Natural Products Targeting Nrf2-HO-1 Signaling. Antioxidants, 10(2), 258. https://doi.org/10.3390/antiox10020258









