Abstract
Mitochondria are the cellular powerhouses that generate adenosine triphosphate (ATP) to substantiate various biochemical activities. Instead of being a static intracellular structure, they are dynamic organelles that perform constant structural and functional remodeling in response to different metabolic stresses. In situations that require a high ATP supply, new mitochondria are assembled (mitochondrial biogenesis) or formed by fusing the existing mitochondria (mitochondrial fusion) to maximize the oxidative capacity. On the other hand, nutrient overload may produce detrimental metabolites such as reactive oxidative species (ROS) that wreck the organelle, leading to the split of damaged mitochondria (mitofission) for clearance (mitophagy). These vital processes are tightly regulated by a sophisticated quality control system involving energy sensing, intracellular membrane interaction, autophagy, and proteasomal degradation to optimize the number of healthy mitochondria. The effective mitochondrial surveillance is particularly important to skeletal muscle fitness because of its large tissue mass as well as its high metabolic activities for supporting the intensive myofiber contractility. Indeed, the failure of the mitochondrial quality control system in skeletal muscle is associated with diseases such as insulin resistance, aging, and muscle wasting. While the mitochondrial dynamics in cells are believed to be intrinsically controlled by the energy content and nutrient availability, other upstream regulators such as hormonal signals from distal organs or factors generated by the muscle itself may also play a critical role. It is now clear that skeletal muscle actively participates in systemic energy homeostasis via producing hundreds of myokines. Acting either as autocrine/paracrine or circulating hormones to crosstalk with other organs, these secretory myokines regulate a large number of physiological activities including insulin sensitivity, fuel utilization, cell differentiation, and appetite behavior. In this article, we will review the mechanism of myokines in mitochondrial quality control and ROS balance, and discuss their translational potential.
1. Introduction
Skeletal muscle is the largest organ in the human body in terms of tissue mass. In addition to supporting locomotion, it is a metabolic reservoir of amino acids and postprandial glucose [1,2]. A finding in the 60s proposed that skeletal muscle might actively participate in systemic metabolic regulation possibly by releasing humoral hypoglycemic factors [3]. This idea of “myokine” was finally established in 2003 after interleukin 6 (IL-6) secretion from skeletal muscle during exercise was confirmed [4]. By definition, myokines are cytokines or peptides that are produced, expressed, and released by muscle fibers to induce functional changes in tissues via cross-talking with other organs or acting locally on skeletal muscle. The functions of myokines are multitudinous that include metabolic regulation in liver and pancreas, remodeling of adipose tissues, improvement of cognitive function and neurogenesis in the central nervous system (CNS), bone mass maintenance, angiogenesis regulation, and immunomodulation [5,6]. Using mass spectrometry-based proteomics and in silico genomic analysis, it is estimated that ~650–1000 proteins/factors can be found in the skeletal muscle [7]. The number of potential myokines can be as much as 1000 if the presence of secretory signal peptide is set as a selection criterion. Nevertheless, less than 10% of the identified myokines have been functionally and mechanistically characterized, which leaves a huge knowledge gap in the area of endocrinology and metabolism research.
Mitochondria are the central organelles of skeletal muscle metabolism. A large amount of evidence has shown that maintaining the normal function of mitochondria is essential for the general health of an organism, and dysfunction of mitochondrial activity is tightly associated with diseases such as muscle wasting and metabolic syndromes [8,9]. Due to the improvement in gene manipulation, biochemical detection, metabolomics, proteomics, and genomic analyses, our understanding of the mitochondria activity in various physiological and disease conditions has been greatly advanced. It is now clear that the activity of mitochondria could be regulated by numerous intracellular and external factors such as nutrient availability and exercise status. However, the relationship between myokines and mitochondrial activity is still being established.
In addition to adenosine triphosphate (ATP) generation, mitochondria also produce reactive oxygen species (ROS) as a side product. ROS is a group of oxygen-derived molecules and free radicals that may bring about oxidative damage to muscle fibers via apoptosis, autophagy, inflammation, and atrophy. Nevertheless, the presence of ROS is essential in maintaining muscle functions such as myocyte repair, mitochondria biogenesis, muscle survival, and muscle maturation [10]. A highly regulated antioxidation system is thus indispensable to balance the ROS content in muscles. Although numerous modulatory factors on oxidative stress regulation have been identified, less is known about the relationship between myokine and ROS/antioxidation in muscle. In this review, we will discuss the functional and mechanistic actions of myokines in mitochondrial recycling and reactive oxidative species homeostasis.
2. Myokines and Mitochondrial Dynamics
Due to the high activity of oxidative phosphorylation, mitochondria are faced with oxidative damages regularly. This oxidative menace is increased when the tissues are required to handle a large amount of nutrient input during obesity or stressed by the demand for extra ATP during physical exercise. Consequently, the mitochondrial pool has to undergo regular recycling to replace the damaged organelle with new and functional mitochondria, which is a critical event to maintain the functionality of cells.
The life cycle of mitochondria includes mitochondrial biogenesis, mitofusion, mitofission, and mitophagy. The majority of new mitochondria are synthesized through the nucleus-initiated “mitochondrial biogenesis” or “retrograde signaling” from mitochondria [11]. In situations where a prolonged supply of additional ATP is required (e.g., exercise and cold adaptation), the transcriptional co-activator peroxisome proliferator-activated receptor-γ coactivator 1α (PGC-1α) plays the master role of nucleus-initiated mitochondrial biogenesis [12]. Activated by the energy-sensing kinase AMP-activated protein kinase (AMPK) [13,14] and cooperating with another transcription factor nuclear respiratory factor 1 (NRF1), PGC-1α induces the expression of genes such as mitochondrial transcription factor A (mtTFA) for promoting the synthesis of new mitochondrial proteins [15]. The activity of PGC-1α is also regulated by another energy sensor sirtuin 1 (SIRT1) in response to low glucose availability. This NAD+-dependent deacetylase activates PGC-1α by deacetylation, leading to elevated expression of mitochondrial proteins and β-oxidation-related genes [16]. Apart from the cellular energy status, mitochondria biosynthesis can also be initiated by the damaged mitochondria [17]. The disrupted membrane potential of deformed mitochondria, which is associated with Ryr-1-dependent increase of cytosolic [Ca2+], activates calcineurin-dependent nuclear factor of activated T-cells (NFATc), myocyte enhancer factor 2 (MEF2), and c-Jun N-terminal kinase (JNK)-dependent activating transcription factor 2 (ATF2) pathways to trigger new mitochondria synthesis [18].
Mitochondrial fusion improves the capacity of oxidative phosphorylation and allows redistribution of mitochondrial DNA (mtDNA) between the healthy and damaged mitochondria [19]. It is also an important process to protect the elongated mitochondria from non-selective degradation by autophagy during energy scarcity [20]. The regulatory mechanism driving mitofusion is highly conserved among species. In mammals, the dynamin-like GTPases mitofusins (MFN1 and MFN2) and optic atrophy protein 1 (OPA1) are the major mediators of mitochondrial fusion. Loss-of-function studies showed that trans-interaction of MFNs brings together mitochondrial outer members to trigger the fusion of two individual mitochondria [21]. Similarly, OPA1 forms oligomers in the inner mitochondrial membrane to promote membrane curvature and lipid mixing during membrane fusion [22]. Because mitochondrial fusion reduces the mobility of mitochondria, permanent fusions are rare events and less than 10% of mitochondria undergo complete fusion. Instead, mitochondria often adopt transient fusions so that two mitochondria are temporarily merged to exchange intra-matrix materials, which are then separated to their original form [23].
Despite that mitochondria fusion is remedial to stressed cells, there is a limit to the stress level [24]. If the threshold is reached, the mitochondria will undergo “mitofission” in which the organelle split asymmetrically into a “healthy” mother mitochondria and a “damaged” daughter mitochondria with disrupted membrane potential [25,26]. Mitofission is mainly mediated by dynamin-related protein 1 (DRP1), a GTPase of the dynamin family that normally resides in the cytoplasm [27]. When recruited by mitochondrial membrane receptors such as mitochondrial fission protein 1 (Fis1) or mitochondrial fission factor (Mff), DRP1 forms spiral oligomers that constrict the mitochondrial membrane upon GTP hydrolysis [28,29]. The mitofission-stimulatory role of DRP1 also depends on its phosphorylation status. During starvation, protein kinase A (PKA) phosphorylates DRP1 at Ser 637 to suppresses its GTPase activity, which keeps the mitochondria in the fused state [30]. When mitofission is prohibited permanently in muscle-specific Drp1 knockout (Drp1−/−) mice, muscle atrophy and mitochondrial dysfunction were observed [31,32]. Despite an increase in volume, the mitochondria isolated from Drp1−/− mice showed reduced respiration activity and lower expression levels of complex I and III of the electron transport chain (ETC). The calcium homeostasis of their mitochondria was also disrupted, leading to the upregulation of ubiquitin ligases (e.g., atrogin-1 and MuRF1) that promote muscle atrophy [33]. Hence, a balance of mitofission and mitofusion is essential to optimize the muscle functions.
Degradation of the split mitochondria can be processed in PTEN-induced kinase 1 (PINK1)-dependent or PINK1-independent manner. PINK1 is a mitochondrial membrane protein that undergoes autophosphorylation when the mitochondrial membrane potential is disrupted. Activated PINK1 phosphorylates the E3 ubiquitin ligase Parkin at Ser 65 [34], which subsequently ubiquitinates a number of proteins such as MFNs [35], Tom20 [36], and VDAC [37] on the damaged mitochondria. The ubiquitinated proteins are then recognized by the adaptor protein p62/STQM, which tethers the mitochondria to the microtubule-associated protein 1A/1B-light chain 3 (LC3) on the autophagosome [38,39]. Mitochondrial uptake by autophagosome can also be initiated without the involvement of PINK1. Mitophagy receptors such as BCL2/adenovirus E1B 19 kDa protein-interacting protein 3-like (BNIP3L) or FUN4 domain containing protein 1 (FUNDC1) could be recruited to the depolarized mitochondrial membrane, which forms a linkage directly with lipidated LC3 (LC3-II) on the autophagosomes [38]. Due to the independence of PINK1/Parkin- and mitophagy receptor-mediated mechanisms, they may serve as complementary pathways to maintain mitochondrial quality [40].
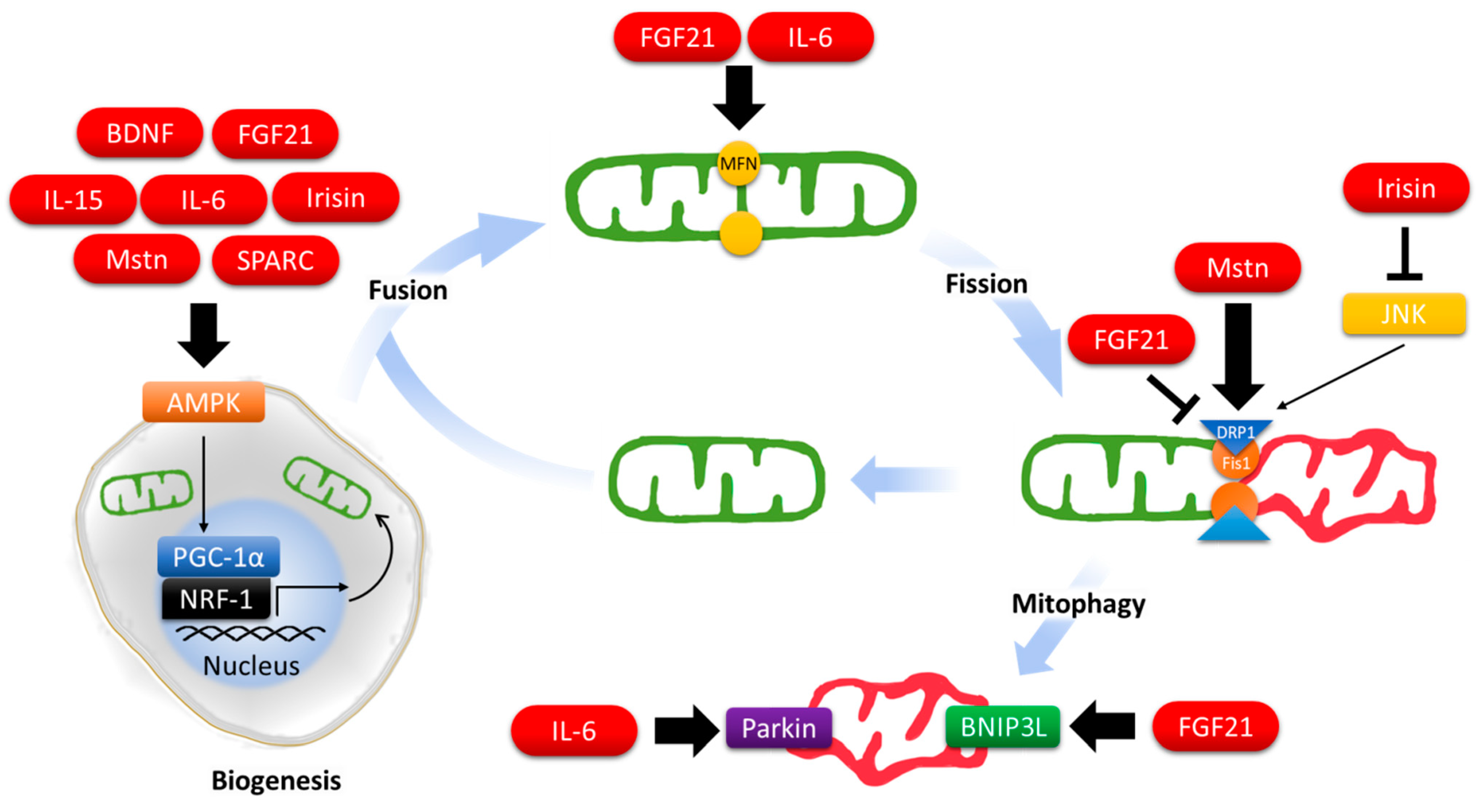
Given the importance of mitochondria in supporting bioenergetics homeostasis, the mitochondrial life cycle is tightly coupled to the cellular concentration of nutrients and ATP via the energy sensors AMPK [41] and mammalian target of rapamycin (mTOR) [42,43]. For instance, AMPK induces mitochondrial synthesis through PGC-1α [44], triggers the formation of autophagosomes by enhancing Unc-51-like kinase 1 (ULK1) activity [45], initiates mitophagy by promoting mitochondrial recruitment of PINK1 [46], and catalyzes mitofission by increasing MFF-DRP1 interaction [47]. Numerous efforts have been put in identifying the signaling cascades and intracellular regulation of the mitochondrial life cycle in the last decades but little is known about how the cells provoke mitochondrial adaptation in response to the extracellular clues. In the following section, we will present examples of myokines that are involved in mitochondrial recycling control (Figure 1).
Figure 1.
Regulation of mitochondrial dynamics by myokines.
2.1. Brain-Derived Neurotrophic Factor (BDNF)
BDNF is a critical growth factor in neuronal development, neuron survival, and synaptic plasticity [48,49] and is associated with many neurodegenerative diseases including Alzheimer’s disease, Parkinson’s disease, Rett syndrome, etc. [50,51]. BDNF level in circulation and Bdnf expression in skeletal muscle were enhanced after physical exercise or food deprivation [52,53,54]. It has been suggested that the skeletal muscle-generated BDNF acted solely as an autocrine because overexpression of BDNF in the muscle did not alter its concentration in blood [53]. Using the muscle-specific BDNF knockout (MBKO) mice, however, we and Fulgenzi et al. have found recently that BDNF can be secreted into circulation [54,55]. We and Matthews et al. have also shown that BDNF is a positive regulator of mitochondrial activity in the cultured muscle cells [53,54]. Hence, BDNF might serve as a myokine that regulates the mitochondrial activity in muscle and other tissues when the animals are metabolically stressed. In support of this notion, we have demonstrated that muscle-generated BDNF is essential to preserve the mitochondrial content in skeletal muscle during fasting [54]. Moreover, chronic activation of BDNF receptor, TrkB, by the non-peptidyl agonist 7,8-dihydroxyflavone (7,8-DHF), increased mitochondrial content in mouse skeletal muscles through activating the AMPK-PGC-1α cascade and alleviated the detrimental effects of diet-induced obesity [56]. BDNF is also able to promote mitochondrial biogenesis in hippocampal neurons [57] and controls mitochondrial dynamics and clearance in adipocytes [58], myocardium [59], motor neurons [60], and retinal cells [61]. Although all these findings suggest that BDNF is a regulator of mitochondrial behavior in a great variety of tissues, it is interesting to note that none of these studies were exercise-related. Hence, the functional significance of BDNF spur during exercise still remains unsolved.
2.2. Fibroblast Growth Factor 21 (FGF21)
In Fgf21-ablated skeletal muscle, BNIP3L-mediated mitophagy was diminished, suggesting that FGF21 drives mitophagy. This notion was further demonstrated by the augmented mitochondrial breakdown in Fgf21-overexpressed cells [62]. Nevertheless, it was found that FGF21 temporarily promotes mitochondrial fusion and inhibits mitofission to prevent apoptosis or senescence when the mesenchymal stem cells (MSCs) are short of energy supply [63]. The role of FGF21 in mitochondrial biogenesis has not been fully explored but there was evidence showing that FGF21 induced mitochondrial replication through PGC-1α and SIRT1 activations [64]. FGF21 also activates the PGC-1α-NRF1-mtTFA pathway to induce mtDNA replication in goat adipocytes [65]. Nonetheless, there is no direct evidence showing that FGF21 increases the mitochondrial number or mitochondrial protein expression in laboratory rodents.
2.3. Interleukin 6 (IL-6)
IL-6 poses prominent effects on mitochondrial dynamics in a number of tissues. For instance, it promoted mitochondrial biogenesis in cortical astrocytes [66] and colorectal cancer cells [67]. In myocardium without IL-6 production, compromised mitochondrial dynamics was detected as the cells showed augmented mitochondria size with reduced Mfn2 expression [68]. Imbalanced mitochondrial production and degradation was found in the skeletal muscle of cancer cachexia, in which IL-6 overexpression in this tissue diminished mitochondrial content but simultaneously elevated the expressions of PGC-1α and Mfns [69]. Fix et al. reported that knocking out the IL-6 receptor reduced mitophagic flux despite augmented mitofission [70], which concurs with the compromised muscle endurance and reduced oxygen consumption in the IL-6 knockout (IL-6−/−) mice [71]. Because exercise intervention was not able to increase the amount of mitochondrial proteins such as citrate synthase and COX in IL-6−/− mice [71,72], this myokine might play a role in promoting mitochondrial biogenesis. Indeed, IL-6 stimulated 3T3-L1 adipocytes showed upregulated mitochondria biogenesis as a compensation for the ROS-induced mitochondria loss, suggesting the mitochondrial dynamic regulatory actions of IL-6 is valid in multiple tissues.
2.4. Interleukin 15 (IL-15)
Circulating IL-15 level is inversely associated with the overall adiposity in both human [73] and laboratory rodents [74,75]. When the animals received a supraphysiological dose of IL-15 or having IL-15 overexpressed in their skeletal muscle, a lower respiratory exchange ratio and higher whole-body fatty acid oxidation (FAO) were observed [76,77]. Since FAO increased in rat muscle after a short IL-15 incubation, it was suspected that IL-15 mediated the fat-burning function via enhancing the activity of mitochondrial enzymes. Nevertheless, the possibility that mitochondrial biogenesis also contributed to the augmented FAO should not be excluded as IL-15 has a stimulatory effect on the expression of mitochondrial biogenesis-related genes including peroxisome proliferator-activated receptor α (PPARα), PPARδ, PGC-1α, PGC-1β, uncoupling protein 2 (UCP2), and NRF1 in muscle cells [78,79]. The observation of increased mtDNA content after chronic IL-15 stimulation further supported this idea [80]. Interestingly, the high circulating level of IL-15 was still able to increase the mitochondrial content in the muscle of IL-15 receptor knockout mice indicating that IL-15 may mediate its effect via an unknown mechanism other than IL-15 receptor activation [81,82,83].
2.5. Irisin
Irisin is an exercise-induced myokine formed by proteolytic cleavage of fibronectin type III domain-containing protein 5 (FNDC5) [84]. It promotes mitochondrial biogenesis in muscle via the AMPK-PGC-1α activation [85], resulting in increased cellular mitochondrial content and oxygen consumption [86]. When Fndc5 expression was suppressed, on the other hand, the consequential PGC-1α defects lowered the abundance and size of mitochondria [87]. Irisin was also able to retain mitochondrial biogenesis, dynamics, and autophagic program in chondrocytes to repress inflammation-mediated oxidative stress and extracellular matrix underproduction [88]. Interestingly, irisin inhibits mitochondrial fission via the JNK-LATS2 pathway in cardiomyocytes [89] and hepatocytes [90] when excessive fission occurred during inflammation. Presumably, irisin may function as a beneficial effector of exercise to protect against excessive damage induced by inflammation.
2.6. Myostatin (Mstn)
Mstn is a known inhibitory myokine to suppress myogenesis [91]. In Mstn knockout (Mstn−/−) mice, muscle hypertrophy was observed with a higher ratio of glycolytic-to-oxidative myofibers [92,93], suggesting Mstn is also crucial to myofiber type determination. Moreover, the muscle of Mstn−/− mice contained less mtDNA and displayed smaller mitochondrial volume [94,95]. The underlying mechanism causing these mitochondrial defects has not been identified but there is evidence that Mstn promotes mitochondrial biogenesis through Smad signaling [96]. Interestingly, Mstn also stimulates both mitochondrial breakdown and mitofission via modulating the expression of mediators such as Drp1 and Fis1 [97,98], suggesting the mitochondrial recycling mechanism is boosted. However, the physiological implication of this stimulatory function is unknown at the current stage.
2.7. Osteonectin/Secreted Protein Acidic and Rich in Cysteine (SPARC)
Similar to IL-15 and irisin, the expression of osteonectin (also known as SPARC) can be induced by exercise [99]. Current studies have only uncovered the activities of osteonectin in undifferentiated myoblasts, where it upregulated mitochondrial proteins such as ubiquinol-cytochrome c reductase core protein II (UQCRC2) and succinate dehydrogenase subunit (SDHB) probably through AMPK activation [100,101]. This osteonectin-dependent elevation of mitochondrial protein is important to myogenesis [100]. Because no study on the role of osteonectin in post-exercise skeletal muscle has been performed, the action mechanism of this myokine in mitochondrial adaptation remains unknown.
3. Myokines and Oxidative Stress
ROS are a group of oxygen-derived molecules and free radicals that are constantly generated and scavenged intracellularly. Common ROS include superoxide anion, peroxide, hydroxyl radical, hydroxyl ion, and nitric oxide [102]. Among the organelles, respiring mitochondria are the major ROS production sites. During the conversion of ADP into ATP by the ETC complexes located on the inner mitochondrial membrane, superoxide (O2•−) is formed at complex I and complex III due to intrinsic electron leakage [103]. The free electrons generated by oxidative phosphorylation may also attack oxygen molecules and thus produce intracellular O2•− [104]. These superoxides in the mitochondrial matrix or intermembrane space would be converted into hydrogen peroxide (H2O2) and ultimately into water molecule (H2O) [105]. Both O2•− and H2O2 are considered as mitochondrial ROS (mtROS). ROS can also be formed by cytosolic NADPH oxidase (NOX). Located on the cell membrane, NOX plays a major role in oxidizing NADPH to NADP+ in response to signaling stimulation or extracellular stresses. Formation of cellular ROS and mtROS could be a spontaneous response to environmental factors such as ionizing radiation [106,107]. Excessive accumulation of ROS is detrimental to almost all biological macromolecules. The toxic effect of ROS could be demonstrated by their actions in DNA damage, peroxidation of fatty acids and amino acids, and inactivation of enzymes or receptors. For instance, peroxidation of the mitochondrial lipid cardiolipin on the inner mitochondrial membrane causes the release of cytochrome c and reduced ATP production [108]. In addition to organelle proteins, both mtDNA and nuclear DNA are also targets of ROS. Damage of mtDNA is especially devastating as it might lead to mitochondrial protein dysfunction that produces more mtROS, resulting in a vicious cycle of mtROS amplification [109]. Moreover, ROS are prominent inducers of apoptosis via the c-Jun N-terminal kinases (JNK)/p53 pathway [110,111] and necrosis through the formation of receptor-interacting serine/threonine protein kinase (RIP) 1 and 3 complexes [112]. Hence, detoxification of excessive ROS is critical to relieve intracellular oxidative stress and maintain cell survival. Several antioxidant mechanisms are present to scavenge cellular ROS. Superoxide dismutase (SOD) is a multigene family consisting of three isoforms. They convert O2•− into H2O2, which will be further decomposed into water molecules and oxygen by another antioxidant enzyme catalase [113]. Small molecules such as glutathione, a tripeptide composes of cysteine, glycine, and glutamate, also play a crucial role in ROS clearance. Glutathione at reduced state (GSH) turns into the oxidized state (GSSG) when they are attacked by ROS, which could be restored into the reduced state by glutathione reductase (GR) [114]. Hence, the level of GSH represents the ‘antioxidation capacity’ of a cell to protect important cellular structures or molecules from ROS attack.
It is noteworthy that the formation of ROS in trace amounts (i.e., mitohormesis) is necessary as they are essential messenger molecules to convey intra-and inter-cellular signaling. For instance, nitric oxide (•NO) is a common extracellular ROS messenger for blood vessel dilation and blood pressure control [115]. Similarly, mtROS is an important second messenger of neurokinin, a neurologically active peptide, in damage-sensing neurons [116]. Intracellular H2O2 molecules also provide the capacity of converting cysteine residues from thiolate anion (Cys-S−) into sulfenic group (Cys-SOH) or even higher oxidative forms, which are important to alter protein conformation and functions [117,118].
Mitochondrial structure and cellular ROS content are bi-directionally linked. On one hand, the stress response signaling pathways induced by ROS activate the mitochondrial fission machinery in a number of tissues including skeletal muscles [119]. On the other hand, the aberrant mechanism in mitochondrial dynamics as observed in the depletion of Mfn1 or Mfn2 results in the formation of mtROS [120]. The molecular details that govern or modulate these activities have not been well-established but the post-translational modification of key enzymes (e.g., S-nitrosylation of Drp1) in mitochondrial dynamics might play an indispensable role [121]. Given the interconnection between ROS generation and mitochondrial remodeling, myokines that control mitochondrial dynamics might also serve as the regulators of ROS production in cells. While the regulatory activities of myokines in ROS generation or oxidative stress-defense system have been reported in a number of cell types, surprisingly, their effect on skeletal muscle remains poorly studied. We will discuss the role of myokines that are potential regulators of muscle ROS homeostasis in the following section (Table 1).

Table 1.
Oxidative stress regulation by myokines in different cells/tissues.
3.1. BDNF
Numerous studies have demonstrated that BDNF is a protective factor against ROS-induced damage in neurons. Cortical cultures challenged with 3-nitropropionic acid (an irreversible inhibitor of mitochondrial complex II) have high cellular ROS, which could be alleviated by the BDNF-stimulated sestrin2-nitric oxide (NO)-protein kinase G (PKG)-NFκB pathway [122]. Similarly, recombinant BDNF incubation averted the H2O2-induced cell death in cortical neurons and astrocytes [123], which was believed as an important mechanism to delay neuronal aging [124]. The ROS removal effect of BDNF could also be observed in H2O2-stressed adult neural stem/progenitor cells (NSPCs) via enhancing the activities of GR and SOD [125]. On the other hand, attenuating the long non-coding RNA (lncRNA)-suppressed BDNF expression lowered the ROS intensity and malondialdehyde content in PC12 cells [126], suggesting BDNF may work as an autocrine to protect the cells from oxidative damage. It has also been reported that hyperglycemia-induced ROS generation in brain microvascular endothelial cells could be inhibited by exogenous BDNF stimulation, which extricated the cells from apoptotic programming [127]. Because ROS elimination prevents neuronal cell apoptosis [125] and boosts survival rate in neural transplantation surgery [128], augmenting BDNF production may represent a compelling method to alleviate the pathological outcomes caused by excessive oxidative stress in the CNS. Recently, BDNF was also found effective in suppressing the oxidized low-density lipoprotein (oxLDL)-induced ROS surge in human umbilical vein endothelial cells (HUVECs) [129]. Hence, it would be tempting to postulate that this function might also be conserved in non-CNS tissues, such as skeletal muscle.
3.2. FGF21
FGF21 is a repressor of ROS generation in multiple tissues. HUVECs pre-incubated with recombinant FGF21 were rescued from glucose-induced ROS production and cell death [130]. Another study also reported that FGF21 inhibited the oxLDL-provoked mtROS production in vascular endothelial cells [131], which provides an explanation of how these cells escape from pyroptotic cell death [131,132]. FGF21 treatment in cultured cardiomyocytes enhanced the expression of genes in antioxidative pathways [133]. It has also been reported that FGF21 compromised the hypoxia-mediated ROS synthesis in cerebral microvascular endothelial cells and restored their antioxidants activities [134]. FGF21 is particularly effective in protecting the cells from mitochondria-dependent stress. In MSCs, mtROS accumulation was observed after FGF21 depletion, which resulted in cell senescence at early passage [63]. In addition, FGF21 relieves the oxidative stress of pathological conditions such as alcoholic fatty liver disease that FGF21 pre-incubation or FGF21 injection restored the antioxidant activities of SOD and glutathione peroxidase in ethanol-induced HepG2 cells and alcohol-gavaged mice, respectively [135]. Whether FGF21 also imposes a protective role against oxidative stress in skeletal muscle remains to be determined.
3.3. IL-6
In skeletal muscle, IL-6 stimulation increased mtROS production via opening the transition pore in isolated mitochondria and cultured C2C12 myotubes [136]. In IL-6-overexpressed mice, their diaphragm muscles showed increased NOX2 expression, higher ROS accumulation, and diminished NRF2-related antioxidant responses [137]. IL-6 also acts as an oxidative stress inducer in various cell types, particularly in cancer cells. It promotes cell proliferation by activating the mitochondrial single strand DNA binding protein (mtSSB) in colorectal cancer cells, resulting in accelerated mitochondrial biogenesis and mtROS over-production [67]. In hepatocellular carcinoma cells, IL-6 treatment generated intracellular ROS via the pathways of JNK, disintegrin and metalloproteinase domain-containing protein 9, and NOX1, which is important to epithelial-mesenchymal transition [138,139]. Moreover, several reports have suggested that IL-6 increased ROS levels in 3T3-L1 adipocytes [140], TIG3 fibroblasts [141], and human brain microvascular endothelial cells [142]. These findings demonstrate that IL-6 is a pivotal ROS up-regulator in numerous conditions and cells. However, there is also evidence showing that IL-6 lowered the cellular ROS by promoting removing the antioxidant repressor KEAP1 in pancreatic β-cells [143], suggesting that IL-6 might have opposite functions according to the cell type.
3.4. IL-15
IL-15 is a ROS scavenger that protects immune cells from immunological response-derived oxidative stress. In human T cells, ROS-induced apoptosis is prevented by the upregulation of GR, thioredoxin (TXN) reductase 1, peroxiredoxin, and SOD after IL-15 stimulation [144]. A recent study also reported that IL15-primed natural killer (NK) cells are shielded from oxidative stress, in which IL-15 boosts the TXN expression and reducing mitochondrial localization of TXN-interacting protein via mTOR activation. These IL-15-primed NK cells also present denser cell surface thiol groups for counteracting the ROS cytotoxicity [145]. In cultured muscle cells, H2O2-induced oxidative stress could be relieved by IL-15 pre-incubation [146]. Because no other study regarding the role of IL-15 in muscular oxidative stress regulation is available, it remains unknown if IL-15 modulates the ROS level of mouse muscle in vivo.
3.5. Irisin
Although adenovirus-mediated overexpression of irisin in mouse cardiomyocytes increased cellular level of superoxide [147], it alleviated the oxidative stress in the heart and protected the tissue from ischemia/reperfusion injury. This protective effect relies on SOD activity promotion, and restoration of SOD into the mitochondrial compartment [148]. It has also been reported that irisin lowered the cellular ROS content by upregulating mitochondrial uncoupling protein 2 (UCP2) in both ischemia/reperfusion-injured alveolar cells [149] and hepatocytes [90]. The oxLDL-promoted ROS generation in vascular endothelial cells could be reversed by irisin through Akt/mTOR/NRF2 pathway activation [150]. Surprisingly, irisin increased the ROS generation activating AMPK-induced glucose uptake in L6 muscle cells [151]. It remains unknown if this ROS generation is a part of mitohormesis in muscle and more studies are needed to reveal the role of this important myokine in skeletal muscle metabolism.
3.6. Mstn
There are a number of studies showing that Mstn is a ROS-inducing myokine in skeletal muscles. Mstn treatment resulted in a drastic increase of intracellular ROS content of C2C12 myotubes [152]. This ROS generation is initiated via the MAPKs (p38 and ERK) signaling pathway, which ultimately triggered oxidative stress-dependent muscle wasting [153]. Activities of the antioxidants catalases were significantly reduced in both gastrocnemius and soleus of Mstn−/− mice but enhanced GSH amount, higher glutathione peroxidase activity, and decreased glutaredoxin activity were observed only in their gastrocnemius, suggesting Mstn suppresses muscular antioxidant systems in a myofiber-specific manner [94]. Mstn also regulates intracellular oxidative stress in non-muscle tissues. For instance, ablation of MSTN in HeLa cells promoted fatty acid oxidation-related mtROS generation and caused mitochondria-dependent apoptosis [154]. Alternatively, recombinant Mstn treatment induced a ROS level surge alongside the upregulated NOX expression in proximal tubular epithelial cell [155]. These findings indicate that Mstn is an inducer of intracellular oxidative stress in various tissue types.
4. Therapeutic Potential of Myokines in Mitochondria/Ros ROS Dysregulation
Defective mitochondrial dynamics and ROS imbalance are observed in pathological conditions including metabolic disorders, immunological disease, neurodegenerative disease, cancer development, and aging [156,157,158,159,160,161,162]. Thus, the use of chemical agents that promote new mitochondrial synthesis or removing the damaged mitochondria should be beneficial to the health of these patients. Proof-of-principle evidence is available that accelerating the mitochondrial dynamics by chemical agents such as AMPK agonist 5-aminoimidazole-4-carboxamide ribonucleotide (AICAR) effectively alleviated the pathological symptoms of disease with mitochondrial dysfunction [163]. Similarly, strengthening the defense system that opposes excess ROS production during disease progression is a hit target of research. For instance, the administration of an antioxidant peptide SS31 promoted mtROS elimination during cardiac IR injury [164,165]. Because of their regulatory roles in mitochondrial activity regulation, the application of myokines should have a great potential to treat mitochondrial-related diseases, in particular since most myokines have promising effects in multiple tissues. Because numerous excellent reviews have already discussed the muscle-tissues crosstalk via myokine in health maintenance [166,167,168,169,170], we will here present evidence to show the potential use of myokines as an “exercise pill” and an anti-aging drug.
4.1. Can Myokines Be Used as an Exercise Mimetic?
Exercise has been recognized by the World Health Organization (WHO) as an effective intervention to prevent or alleviate various chronic diseases [171]. Endurance exercise training also provides cytoprotection to skeletal muscle fibers against damaging insults such as chemical-induced injury and inactivity-induced atrophy [172]. Although the mechanism of exercise-provoked benefits has not been fully elucidated, it is hypothesized that mitochondrial remodeling plays a central role because exercise promotes mitochondrial turnover in skeletal muscles [173]. Extensive studies have shown that exercise training, regardless of the intensity and duration, increases the mitochondrial mass [174], mtDNA content [175], FAO [176,177], and mitochondrial volume density in skeletal muscle [178]. Post-exercise upregulation of mitophagy is also required to ensure sufficient clearance of the damaged mitochondria, which depends on the AMPK-ULK1 signaling [179]. Because myokine expression in skeletal muscle is increased after exercise [180,181], and that myokines participate in multiple regulatory points of mitochondrial homeostasis, they are thus naturally linked to the metabolic and functional benefits of exercise. A canonical example stated that SPARC is the essential effector of exercise to suppress colon tumorigenesis [99]. The finding that irisin injection was able to prevent bone loss and muscle atrophy in hind-limb suspended mice further encourages the use of myokines as an exercise mimetic to provide health benefits to those subjects with locomotion impairments [182,183]. However, it should be noted that hundreds of myokines are induced during exercise and it is hard to be convinced that increasing a single myokine in vivo would significantly mimic all beneficial effects of exercise. Infusion of exosomes, the nano-vesicles that contain a mixture of multiple myokines, miRNA, and nucleic acids derived from young exercised muscle [184], may represent an alternative to single myokine administration, which in principle has a higher translational value. Nevertheless, the variation of exercise intensity and duration might produce a highly heterogeneous set of exosomes with unmanageable effects, and that their action mechanisms in various tissues have not been well characterized. More research on exosome biology is thus needed before it becomes a choice of therapeutic interventions.
It is also interesting to foresee that myokines can be used to boost exercise performance because genetic ablation studies have demonstrated the essential role of some myokines in muscle endurance [54]. Increased mitochondrial biogenesis is believed to play a major role in enhancing the energetic capacity of skeletal muscle [185,186]. As such, it is not surprising to find that the overexpression of signaling molecules such as PGC-1α or myokines like musclin improves the exercise performance of mice [187]. Those myokines such as IL-6 and IL-15 that are able to enhance FAO in skeletal muscle might also have performance enhancing functions such as shifting the energy source from carbohydrates to fatty acid during exercise, which is essential to extend the muscular endurance capacity [188,189].
Because of their antioxidant activity, some myokines could also be applied to protect against muscle fatigue. It is well-known that muscle contraction promotes the synthesis of ROS and free radicals [190,191], which are associated with muscle fatigue [192]. The application of anti-oxidants that protect against mtROS accumulation in muscle is able to delay muscle exhaustion, indicating that ROS scavengers are useful in relieving tissue tiredness [193]. Nevertheless, the regular generation of ROS at a moderate level is essential to redox homeostasis for enhancing the capacity of the antioxidant defense system in the exercised muscle [194]. A recent study also proposed that myocellular ROS production contributed to GLUT4 translocation [195], which is a key modulator of exercised-stimulated glucose uptake in muscle [196]. As such, myokine administration should not be used as a daily supplement but as a recovery measure after strenuous exercise or over-training when the detrimental effects of ROS are exaggerated [197].
4.2. Can Myokines Be Used as Rejuvenation Agents?
Mega-analysis suggests that as much as 83% of the elderly are physically inactive [198]. Such immobility can be explained by the deterioration of muscles including muscle mass decreases, reduced muscle strength, and loss of functional capacity [199,200]. If the muscle is not stimulated by sufficient levels of physical activity, the synthesis and release of myokines will be limited, which may contribute to the malfunction of several organs. Indeed, physical idleness is associated with reduced myokine secretion. For instance, the contents of bone morphogenetic factor 7 (BMP7) and irisin are decreased in aged skeletal muscle, which could be restored by physical exercise [201,202]. Because BMP7 is important to counteract the aging-dependent dysfunction of neuromuscular junctions [203], its deficiency may contribute to the sarcopenic phenotypes of the elderly. It is also found that progenitor/satellite cells isolated from aged rat skeletal muscles underwent increased internalization of SPARC, resulting in less muscle-generated SPARC. Such a decline in SPARC level caused muscle adipogenesis and fat accumulation [204]. Other myokines including IL-15, β-aminoisobutyric acid (BAIBA), and IGF-1 were also decreased in aged subjects [205]. Because myokines such as irisin, FGF21, and decorin are important in maintaining muscle mass [206], the lack of sufficient myokines in the elderly may form a looping back model to magnify muscle atrophy and dynapenia.
In a gerontological study that compared the vastus lateralis biopsies collected from young (average age = 22 years) and old (average age = 72 years) males, it was found that oxidative damage was more severe in the aged group [207]. A similar rise of H2O2 and O2•− were also detected in old rat muscles [208], suggesting the increases of muscular oxidative stress during aging is a universal event among different species. Moreover, mitochondrial activity is lower in the skeletal muscle of aged mice [209]. Their muscles are thus less potent in eliminating the impaired ROS-generating mitochondria, which leads to more ROS generation [210,211]. The cause of this elevated ROS production has not been clearly elucidated because discrepant observations were reported. While a drop of catalase protein level has been proposed as the major contributor of the elevated oxidative stress in the gastrocnemius of middle-aged to old mice [212], there are also studies reporting that muscle catalase activity was increased in an age-dependent manner [207,213,214]. Similarly, SOD content upon aging is inconsistent with reports that the muscles from healthy aged human subjects displayed higher SOD activity [207,215]. A decrease of SOD2 activity in sedentary old adults [216] and in 12- or 24-months old mice [212] has also been reported.
Although myokine levels have a close-relationship with aging, its anti-aging effect has not been systemically evaluated. Fragmented but yet encouraging results were reported that intramuscular injection of decorin significantly induced muscle hypertrophy in pre-clinical models of muscle dystrophy [217]. Reza et al. have also shown that irisin was able to promote myogenesis and muscle regeneration [218], which are both severely impaired in the elderly [219,220]. Moreover, administration of myostatin-neutralizing antibody increased muscle mass and muscle strength in aged mice [221]. Because myokines such as myostatin and IGF-I were independently associated with muscle wasting [222], the use of myokine as a biomarker of frailty, a reversible state of increased vulnerability to health-related negative outcomes, including disability and mortality, was proposed [223]. Indeed, the close association of irisin or BDNF levels with the sarcopenia index suggested that these myokines can be used as a reliable biomarker of sarcopenia and frailty [224,225].
5. Conclusions and Future Perspectives
The identification of myokines has provided a new conceptual basis and paradigm on the regulation of metabolism but our knowledge on this new hormone class is still incomplete. Because deficiency of some myokines is highly associated with diseases such as Alzheimer’s disease [226,227] or metabolic syndromes [228], the large number of potential myokines in muscle provides a valuable resource for disease prognosis and treatment. They can also be used as biomarkers for assessing the type and amount of exercise that are required for the prescription of exercise for people with chronic diseases [229]. Nevertheless, most myokines are still uncharacterized, which limits their translational potential. An immediate challenge in the field is to accelerate the functional studies of these factors systematically. The use of reverse genetic methods is essential, which has greatly advanced our understanding of myokines’ functions in the last decades. However, the knockout models of rarely-studied or novel myokines are not always available. Collaboration with the International Mouse Phenotyping Consortium (IMPC), a central platform that aims to knockout each of the roughly 20,000 genes of the mouse genome, might provide great support to facilitate the myokine characterizations [230].
The use of exogenous hormone/peptide supplementation is another well-accepted method to delineate the function of myokines. Most studies performed in laboratory animals require injections of myokines in high dose, which is a less desirable method for therapeutic purposes in human because of the peptidyl limitations such as proteolytic instability, low solubility, short half-life in plasma, and toxicity in a high dose of myokines. Ideally, non-peptidyl bioavailable mimetics should be used but there is only a limited number of myokine mimetics have been developed. To our best knowledge, only the non-peptidyl mimetics for FGF21 and BDNF have been proved as beneficial agents to metabolic syndromes and neurological disorders [56,231]. More resources should be invested to develop reliable and potent mimetics for those myokines with translational potential in the future.
Although a lot of peptides are classified as myokines, most of them are commonly expressed in various tissues rather than generated solely by skeletal muscle. For instance, IL-6 expression could be detected in macrophages [232], cancer cells [232], osteoblasts [233], smooth muscle cells [234], and adipocytes [235]. This leads to the concern on the source of myokines secreted in response to stress because the tissue-specific function of myokines might jeopardize their potential application in health improvement. IL-6 is one of the classic examples that the IL-6 produced in muscle enhances glucose disposal [236], lipolysis, and fat oxidation [188] but the adipocyte-derived IL-6 promoted insulin resistance [235]. Presumably, simply elevating the circulating myokine levels may not be beneficial if it possesses contradictory functions in different tissues. A full revelation of the functional spectrum of myokines that are also expressed in other tissues is a must before they can be considered for clinical usage.
Author Contributions
Writing—original draft preparation, B.P.S.P., W.S.C., C.B.C.; writing—review and editing, B.P.S.P., W.S.C., C.B.C.; visualization, B.P.S.P., W.S.C.; supervision, C.B.C.; funding acquisition, C.B.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research is funded by the Hong Kong Government Research Grant Council (grant numbers GRF17113817 and GRF17108618) and Hong Kong Medical Research Fund (grant numbers HMRF06171836).
Conflicts of Interest
The authors declare no conflict of interest.
References
- Ferrer, J.C.; Favre, C.; Gomis, R.R.; Fernández-Novell, J.M.; García-Rocha, M.; de La Iglesia, N.; Cid, E.; Guinovart, J.J. Control of glycogen deposition. FEBS Lett. 2003, 546, 127–132. [Google Scholar] [CrossRef]
- Wagenmakers, A.J. Muscle amino acid metabolism at rest and during exercise: Role in human physiology and metabolism. Exerc. Sport Sci. Rev. 1998, 26, 287–314. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, M.S. Humoral Nature of the Hypoglycemic Factor of Muscular Work. Diabetes 1961, 10, 232–234. [Google Scholar] [CrossRef] [PubMed]
- Ostrowski, K.; Rohde, T.; Zacho, M.; Asp, S.; Pedersen, B.K. Evidence that interleukin-6 is produced in human skeletal muscle during prolonged running. J. Physiol. 1998, 508, 949–953. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, B.K. Myokines and Metabolism. In Metabolic Syndrome; Ahima, R.S., Ed.; Springer International Publishing: Cham, Switzerland, 2016; pp. 541–554. [Google Scholar]
- Delezie, J.; Handschin, C. Endocrine Crosstalk between Skeletal Muscle and the Brain. Front. Neurol. 2018, 9, 698. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.U.; Ghafoor, S. Myokines: Discovery Challenges and Therapeutic Impediments. J. Pak. Med. Assoc. 2019, 69, 1014–1017. [Google Scholar]
- Calvani, R.; Joseph, A.-M.; Adhihetty, P.J.; Miccheli, A.; Bossola, M.; Leeuwenburgh, C.; Bernabei, R.; Marzetti, E. Mitochondrial pathways in sarcopenia of aging and disuse muscle atrophy. Biol. Chem. 2013, 394, 393–414. [Google Scholar] [CrossRef]
- Bhatti, J.S.; Bhatti, G.K.; Reddy, P.H. Mitochondrial dysfunction and oxidative stress in metabolic disorders—A step towards mitochondria based therapeutic strategies. Biochim. Biophys. Acta (BBA)-Mol. Basis Dis. 2017, 1863, 1066–1077. [Google Scholar] [CrossRef]
- Barbieri, E.; Sestili, P. Reactive Oxygen Species in Skeletal Muscle Signaling. J. Signal Transduct. 2012, 2012, 1–17. [Google Scholar] [CrossRef]
- Dominy, J.E.; Puigserver, P. Mitochondrial Biogenesis through Activation of Nuclear Signaling Proteins. Cold Spring Harb. Perspect. Biol. 2013, 5, a015008. [Google Scholar] [CrossRef]
- Puigserver, P.; Wu, Z.; Park, C.W.; Graves, R.; Wright, M.; Spiegelman, B.M. A Cold-Inducible Coactivator of Nuclear Receptors Linked to Adaptive Thermogenesis. Cell 1998, 92, 829–839. [Google Scholar] [CrossRef]
- Hardie, D.G. AMP-activated protein kinase–An energy sensor that regulates all aspects of cell function. Genes Dev. 2011, 25, 1895–1908. [Google Scholar] [CrossRef] [PubMed]
- Hardie, D.G.; Hawley, S.A. AMP-activated protein kinase: The energy charge hypothesis revisited. BioEssays 2001, 23, 1112–1119. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.; Puigserver, P.; Andersson, U.; Zhang, C.; Adelmant, G.; Mootha, V.; Troy, A.; Cinti, S.; Lowell, B.; Scarpulla, R.C.; et al. Mechanisms Controlling Mitochondrial Biogenesis and Respiration through the Thermogenic Coactivator PGC-1. Cell 1999, 98, 115–124. [Google Scholar] [CrossRef]
- Gerhart-Hines, Z.; Rodgers, J.T.; Bare, O.; Lerin, C.; Kim, S.-H.; Mostoslavsky, R.; Alt, F.W.; Wu, Z.; Puigserver, P. Metabolic control of muscle mitochondrial function and fatty acid oxidation through SIRT1/PGC-1α. EMBO J. 2007, 26, 1913–1923. [Google Scholar] [CrossRef]
- Bohovych, I.; Khalimonchuk, O. Sending Out an SOS: Mitochondria as a Signaling Hub. Front. Cell Dev. Biol. 2016, 4, 109. [Google Scholar] [CrossRef]
- Biswas, G.; Adebanjo, O.A.; Freedman, B.D.; Anandatheerthavarada, H.K.; Vijayasarathy, C.; Zaidi, M.; Kotlikoff, M.; Avadhani, N.G. Retrograde Ca2+ signaling in c2c12 skeletal myocytes in response to mitochondrial genetic and metabolic stress: A novel mode of inter-organelle crosstalk. EMBO J. 1999, 18, 522–533. [Google Scholar] [CrossRef]
- Gao, S.; Hu, J. Mitochondrial Fusion: The Machineries In and Out. Trends Cell Biol. 2021, 31, 62–74. [Google Scholar] [CrossRef]
- Mejlvang, J.; Olsvik, H.; Svenning, S.; Bruun, J.; Abudu, Y.P.; Larsen, K.B.; Brech, A.; Hansen, T.E.; Brenne, H.; Hansen, T.; et al. Starvation induces rapid degradation of selective autophagy receptors by endosomal microautophagy. J. Cell Biol. 2018, 217, 3640–3655. [Google Scholar] [CrossRef]
- Eura, Y.; Ishihara, N.; Yokota, S.; Mihara, K. Two Mitofusin Proteins, Mammalian Homologues of FZO, with Distinct Functions Are Both Required for Mitochondrial Fusion. J. Biochem. 2003, 134, 333–344. [Google Scholar] [CrossRef]
- Chen, H.; Detmer, S.A.; Ewald, A.J.; Griffin, E.E.; Fraser, S.E.; Chan, D.C. Mitofusins Mfn1 and Mfn2 coordinately regulate mitochondrial fusion and are essential for embryonic development. J. Cell Biol. 2003, 160, 189–200. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Weaver, D.; Shirihai, O.; Hajnóczky, G. Mitochondrial ‘kiss-and-run’: Interplay between mitochondrial motility and fusion–fission dynamics. EMBO J. 2009, 28, 3074–3089. [Google Scholar] [CrossRef] [PubMed]
- Youle, R.J.; van der Bliek, A.M. Mitochondrial Fission, Fusion, and Stress. Science 2012, 337, 1062–1065. [Google Scholar] [CrossRef] [PubMed]
- Twig, G.; Elorza, A.; Molina, A.A.J.; Mohamed, H.; Wikstrom, J.D.; Walzer, G.; Stiles, L.; Haigh, S.E.; Katz, S.; Las, G.; et al. Fission and selective fusion govern mitochondrial segregation and elimination by autophagy. EMBO J. 2008, 27, 433–446. [Google Scholar] [CrossRef]
- Van Der Bliek, A.M.; Shen, Q.; Kawajiri, S. Mechanisms of Mitochondrial Fission and Fusion. Cold Spring Harb. Perspect. Biol. 2013, 5, a011072. [Google Scholar] [CrossRef]
- Smirnova, E.; Griparic, L.; Shurland, D.-L.; van der Bliek, A.M. Dynamin-related Protein Drp1 Is Required for Mitochondrial Division in Mammalian Cells. Mol. Biol. Cell 2001, 12, 2245–2256. [Google Scholar] [CrossRef]
- Losón, O.C.; Song, Z.; Chen, H.; Chan, D.C. Fis1, Mff, MiD49, and MiD51 mediate Drp1 recruitment in mitochondrial fission. Mol. Biol. Cell 2013, 24, 659–667. [Google Scholar] [CrossRef]
- Mears, J.A.; Lackner, L.L.; Fang, S.; Ingerman, E.; Nunnari, J.; Hinshaw, J.E. Conformational changes in Dnm1 support a contractile mechanism for mitochondrial fission. Nat. Struct. Mol. Biol. 2010, 18, 20–26. [Google Scholar] [CrossRef]
- Gomes, L.C.; Di Benedetto, G.; Scorrano, L. During autophagy mitochondria elongate, are spared from degradation and sustain cell viability. Nat. Cell Biol. 2011, 13, 589–598. [Google Scholar] [CrossRef]
- Dulac, M.; Leduc-Gaudet, J.; Reynaud, O.; Ayoub, M.; Guérin, A.; Finkelchtein, M.; Na Hussain, S.; Gouspillou, G. Drp1 knockdown induces severe muscle atrophy and remodelling, mitochondrial dysfunction, autophagy impairment and denervation. J. Physiol. 2020, 598, 3691–3710. [Google Scholar] [CrossRef]
- Favaro, G.; Romanello, V.; Varanita, T.; Desbats, M.A.; Morbidoni, V.; Tezze, C.; Albiero, M.; Canato, M.; Gherardi, G.; De Stefani, D.; et al. DRP1-mediated mitochondrial shape controls calcium homeostasis and muscle mass. Nat. Commun. 2019, 10, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Romanello, V.; Guadagnin, E.; Gomes, L.; Roder, I.; Sandri, C.; Petersen, Y.; Milan, G.; Masiero, E.; del Piccolo, P.; Foretz, M.; et al. Mitochondrial fission and remodelling contributes to muscle atrophy. EMBO J. 2010, 29, 1774–1785. [Google Scholar] [CrossRef]
- Kondapalli, C.; Kazlauskaite, A.; Zhang, N.; Woodroof, H.I.; Campbell, D.G.; Gourlay, R.; Burchell, L.; Walden, H.; Macartney, T.J.; Deak, M.; et al. PINK1 is activated by mitochondrial membrane potential depolarization and stimulates Parkin E3 ligase activity by phosphorylating Serine 65. Open Biol. 2012, 2, 120080. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, A.; Cleland, M.M.; Xu, S.; Narendra, D.P.; Suen, D.-F.; Karbowski, M.; Youle, R.J. Proteasome and p97 mediate mitophagy and degradation of mitofusins induced by Parkin. J. Cell Biol. 2010, 191, 1367–1380. [Google Scholar] [CrossRef] [PubMed]
- Bingol, B.; Tea, J.S.; Phu, L.; Reichelt, M.; Bakalarski, C.E.; Song, Q.; Foreman, O.; Kirkpatrick, D.S.; Sheng, M. The mitochondrial deubiquitinase USP30 opposes parkin-mediated mitophagy. Nat. Cell Biol. 2014, 510, 370–375. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Vashisht, A.A.; Tchieu, J.; Wohlschlegel, J.A.; Dreier, L. Voltage-dependent Anion Channels (VDACs) Recruit Parkin to Defective Mitochondria to Promote Mitochondrial Autophagy. J. Biol. Chem. 2012, 287, 40652–40660. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.-K.; Lee, J.-A. Role of the mammalian ATG8/LC3 family in autophagy: Differential and compensatory roles in the spatiotemporal regulation of autophagy. BMB Rep. 2016, 49, 424–430. [Google Scholar] [CrossRef]
- Nakatogawa, H.; Ichimura, Y.; Ohsumi, Y. Atg8, a Ubiquitin-like Protein Required for Autophagosome Formation, Mediates Membrane Tethering and Hemifusion. Cell 2007, 130, 165–178. [Google Scholar] [CrossRef]
- Park, J.-S.; Koentjoro, B.; Sue, C.M. Commentary: Nix restores mitophagy and mitochondrial function to protect against PINK1/Parkin-related Parkinson’s disease. Front. Mol. Neurosci. 2017, 10, 297. [Google Scholar] [CrossRef]
- Hardie, D.G.; Ross, F.A.; Hawley, S.A. AMPK: A nutrient and energy sensor that maintains energy homeostasis. Nat. Rev. Mol. Cell Biol. 2012, 13, 251–262. [Google Scholar] [CrossRef]
- Goberdhan, D.C.; Wilson, C.; Harris, A.L. Amino Acid Sensing by mTORC1: Intracellular Transporters Mark the Spot. Cell Metab. 2016, 23, 580–589. [Google Scholar] [CrossRef] [PubMed]
- Shimobayashi, M.; Hall, M.N. Multiple amino acid sensing inputs to mTORC1. Cell Res. 2016, 26, 7–20. [Google Scholar] [CrossRef] [PubMed]
- Marin, T.L.; Gongol, B.; Zhang, F.; Martin, M.; Johnson, D.A.; Xiao, H.; Wang, Y.; Subramaniam, S.; Chien, S.; Shyy, J.Y.-J. AMPK promotes mitochondrial biogenesis and function by phosphorylating the epigenetic factors DNMT1, RBBP7, and HAT1. Sci. Signal. 2017, 10, eaaf7478. [Google Scholar] [CrossRef] [PubMed]
- Egan, D.F.; Shackelford, D.B.; Mihaylova, M.M.; Gelino, S.R.; Kohnz, R.A.; Mair, W.; Vasquez, D.S.; Joshi, A.; Gwinn, D.M.; Taylor, R.; et al. Phosphorylation of ULK1 (hATG1) by AMP-Activated Protein Kinase Connects Energy Sensing to Mitophagy. Science 2010, 331, 456–461. [Google Scholar] [CrossRef]
- Wang, B.; Nie, J.; Wu, L.; Hu, Y.; Wen, Z.; Dong, L.; Zou, M.H.; Chen, C.; Wang, D.W. Ampkalpha2 protects against the development of heart failure by enhancing mitophagy via pink1 phosphorylation. Circ. Res. 2018, 122, 712–729. [Google Scholar] [CrossRef]
- Toyama, E.Q.; Herzig, S.; Courchet, J.; Lewis, T.L.; Losón, O.C.; Hellberg, K.; Young, N.P.; Chen, H.; Polleux, F.; Chan, D.C.; et al. AMP-activated protein kinase mediates mitochondrial fission in response to energy stress. Science 2016, 351, 275–281. [Google Scholar] [CrossRef]
- Cohen-Cory, S.; Kidane, A.H.; Shirkey, N.J.; Marshak, S. Brain-derived neurotrophic factor and the development of structural neuronal connectivity. Dev. Neurobiol. 2010, 70, 271–288. [Google Scholar] [CrossRef]
- Kowiański, P.; Lietzau, G.; Czuba, E.; Waśkow, M.; Steliga, A.; Moryś, J. BDNF: A Key Factor with Multipotent Impact on Brain Signaling and Synaptic Plasticity. Cell. Mol. Neurobiol. 2018, 38, 579–593. [Google Scholar] [CrossRef]
- Zuccato, C.; Cattaneo, E. Brain-derived neurotrophic factor in neurodegenerative diseases. Nat. Rev. Neurol. 2009, 5, 311–322. [Google Scholar] [CrossRef]
- Diniz, B.S.; Teixeira, A.L. Brain-Derived Neurotrophic Factor and Alzheimer’s Disease: Physiopathology and Beyond. NeuroMolecular Med. 2011, 13, 217–222. [Google Scholar] [CrossRef]
- Cuppini, R.; Sartini, S.; Agostini, D.; Guescini, M.; Ambrogini, P.; Betti, M.; Bertini, L.; Vallasciani, M.; Stocchi, V. Bdnf expression in rat skeletal muscle after acute or repeated exercise. Arch. Ital. Biol. 2007, 145, 99–110. [Google Scholar] [PubMed]
- Matthews, V.B.; Åström, M.-B.; Chan, M.H.S.; Bruce, C.R.; Krabbe, K.S.; Prelovsek, O.; Åkerström, T.; Yfanti, C.; Broholm, C.; Mortensen, O.H.; et al. Brain-derived neurotrophic factor is produced by skeletal muscle cells in response to contraction and enhances fat oxidation via activation of AMP-activated protein kinase. Diabetologia 2009, 52, 1409–1418. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Brobst, D.; Chan, W.S.; Tse, M.C.L.; Herlea-Pana, O.; Ahuja, P.; Bi, X.; Zaw, A.M.; Kwong, Z.S.W.; Jia, W.-H.; et al. Muscle-generated BDNF is a sexually dimorphic myokine that controls metabolic flexibility. Sci. Signal. 2019, 12, eaau1468. [Google Scholar] [CrossRef] [PubMed]
- Fulgenzi, G.; Hong, Z.; Tomassoni-Ardori, F.; Barella, L.F.; Becker, J.; Barrick, C.; Swing, D.; Yanpallewar, S.; Croix, B.S.; Wess, J.; et al. Novel metabolic role for bdnf in pancreatic beta-cell insulin secretion. Nat. Commun. 2020, 11, 1950. [Google Scholar] [CrossRef]
- Wood, J.; Tse, M.C.L.; Yang, X.; Brobst, D.; Liu, Z.; Pang, B.P.S.; Chan, W.S.; Zaw, A.M.; Chow, B.K.; Ye, K.; et al. BDNF mimetic alleviates body weight gain in obese mice by enhancing mitochondrial biogenesis in skeletal muscle. Metabolism 2018, 87, 113–122. [Google Scholar] [CrossRef] [PubMed]
- Cheng, A.; Wan, R.; Yang, J.-L.; Kamimura, N.; Son, T.G.; Ouyang, X.; Luo, Y.; Okun, E.; Mattson, M.P. Involvement of PGC-1α in the formation and maintenance of neuronal dendritic spines. Nat. Commun. 2012, 3, 1–12. [Google Scholar] [CrossRef]
- Colitti, M.; Montanari, T. Brain-derived neurotrophic factor modulates mitochondrial dynamics and thermogenic phenotype on 3T3-L1 adipocytes. Tissue Cell 2020, 66, 101388. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Wang, S.-P.; Shao, Q.; Li, P.-F.; Sun, Y.; Luo, L.-Z.; Yan, X.-Q.; Fan, Z.-Y.; Hu, J.; Du, Z.-M.; et al. Brain-derived neurotrophic factor mimetic, 7,8-dihydroxyflavone, protects against myocardial ischemia by rebalancing optic atrophy 1 processing. Free. Radic. Biol. Med. 2019, 145, 187–197. [Google Scholar] [CrossRef]
- Cawley, M. The Role of Skeletal Muscle-Synthesized Brain Derived Neurotrophic Factor in the Maintenance of Motor Neuron Mitochondrial Populations. Master’s Thesis, Northern Michigan University, Marquette, MI, USA, June 2020. [Google Scholar]
- Shim, M.S.; Kim, K.-Y.; Noh, M.; Ko, J.Y.; Ahn, S.; An, M.A.; Iwata, T.; Perkins, G.A.; Weinreb, R.N.; Ju, W.-K. Optineurin E50K triggers BDNF deficiency-mediated mitochondrial dysfunction in retinal photoreceptor cell line. Biochem. Biophys. Res. Commun. 2018, 503, 2690–2697. [Google Scholar] [CrossRef]
- Oost, L.J.; Kustermann, M.; Armani, A.; Blaauw, B.; Romanello, V. Fibroblast growth factor 21 controls mitophagy and muscle mass. J. Cachexia Sarcopenia Muscle 2019, 10, 630–642. [Google Scholar] [CrossRef]
- Li, X.; Hong, Y.; He, H.; Jiang, G.; You, W.; Liang, X.; Fu, Q.; Han, S.; Lian, Q.; Zhang, Y. FGF21 Mediates Mesenchymal Stem Cell Senescence via Regulation of Mitochondrial Dynamics. Oxidative Med. Cell. Longev. 2019, 2019, 4915149-13. [Google Scholar] [CrossRef] [PubMed]
- Forsström, S.; Jackson, C.B.; Carroll, C.J.; Kuronen, M.; Pirinen, E.; Pradhan, S.; Marmyleva, A.; Auranen, M.; Kleine, I.-M.; Khan, N.A.; et al. Fibroblast Growth Factor 21 Drives Dynamics of Local and Systemic Stress Responses in Mitochondrial Myopathy with mtDNA Deletions. Cell Metab. 2019, 30, 1040–1054.e7. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Li, L.; Wang, Q.; Zhan, S.; Wang, L.; Zhong, T.; Guo, J.; Zhang, H. Fibroblast growth factor 21 induces lipolysis more efficiently than it suppresses lipogenesis in goat adipocytes. Cytotechnology 2018, 70, 1423–1433. [Google Scholar] [CrossRef]
- Chen, X.-L.; Wang, Y.; Peng, W.-W.; Zheng, Y.-J.; Zhang, T.-N.; Wang, P.-J.; Huang, J.-D.; Zeng, Q. Effects of interleukin-6 and IL-6/AMPK signaling pathway on mitochondrial biogenesis and astrocytes viability under experimental septic condition. Int. Immunopharmacol. 2018, 59, 287–294. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.; Wang, Q.; Huang, Q.; Chen, Y.; Sun, X.; He, L.; Zhan, L.; Guo, X.; Yin, C.; Fang, Y.; et al. Upregulation of mtSSB by interleukin-6 promotes cell growth through mitochondrial biogenesis-mediated telomerase activation in colorectal cancer. Int. J. Cancer 2019, 144, 2516–2528. [Google Scholar] [CrossRef]
- Tomasz, A.B.; Magdalena, D.; Magdalena, S.; Beata, S.; Ewa, W.; Maria, M.W.; Karol, A.K. Interleukin-6 affects aging-related changes of the ppar[alpha]-pgc-1[alpha] axis in the myocardium. J. Interferon Cytokine Res. 2017, 37, 513. [Google Scholar]
- White, J.P.; Puppa, M.J.; Sato, S.; Gao, S.; Price, R.L.; Baynes, J.W.; Kostek, M.C.; E Matesic, L.; Carson, J.A. IL-6 regulation on skeletal muscle mitochondrial remodeling during cancer cachexia in the ApcMin/+ mouse. Skelet. Muscle 2012, 2, 14. [Google Scholar] [CrossRef]
- Fix, D.K.; Hardee, J.P.; Gao, S.; Vanderveen, B.N.; Velázquez, K.T.; Carson, J.A. Role of gp130 in basal and exercise-trained skeletal muscle mitochondrial quality control. J. Appl. Physiol. 2018, 124, 1456–1470. [Google Scholar] [CrossRef]
- Fäldt, J.; Wernstedt, I.; Fitzgerald, S.M.; Wallenius, K.; Bergström, G.R.; Jansson, J.-O. Reduced exercise endurance in interleukin-6-deficient mice. Endocrinology 2004, 145, 2680–2686. [Google Scholar] [CrossRef]
- Wojewoda, M.; Kmiecik, K.; Majerczak, J.; Ventura-Clapier, R.; Fortin, D.; Onopiuk, M.; Róg, J.; Kamiński, K.A.; Chlopicki, S.; Zoladz, J. Skeletal Muscle Response to Endurance Training in IL-6−/− Mice. Int. J. Sports Med. 2015, 36, 1163–1169. [Google Scholar] [CrossRef]
- Hingorjo, M.R.; Zehra, S.; Saleem, S.; Qureshi, M.A. Serum Interleukin-15 and its relationship with adiposity Indices before and after short-term endurance exercise. Pak. J. Med. Sci. 2018, 34, 1125–1131. [Google Scholar] [CrossRef] [PubMed]
- Alvarez, B.; Carbó, N.; López-Soriano, J.; Drivdahl, R.H.; Busquets, S.; López-Soriano, F.J.; Argilés, J.M.; Quinn, L.S. Effects of interleukin-15 (IL-15) on adipose tissue mass in rodent obesity models: Evidence for direct IL-15 action on adipose tissue. Biochim. Biophys. Acta (BBA)-Gen. Subj. 2002, 1570, 33–37. [Google Scholar] [CrossRef]
- Quinn, L.S.; Anderson, B.G.; Strait-Bodey, L.; Stroud, A.M.; Argilés, J.M. Oversecretion of interleukin-15 from skeletal muscle reduces adiposity. Am. J. Physiol. Metab. 2009, 296, E191–E202. [Google Scholar] [CrossRef] [PubMed]
- Nadeau, L.; Aguer, C. Interleukin-15 as a myokine: Mechanistic insight into its effect on skeletal muscle metabolism. Appl. Physiol. Nutr. Metab. 2019, 44, 229–238. [Google Scholar] [CrossRef]
- Almendro, V.; Busquets, S.; Ametller, E.; Carbo, N.; Figueras, M.; Fuster, G.; Argiles, J.M.; Lopez-Soriano, F.J. Effects of interleukin-15 on lipid oxidation: Disposal of an oral [(14)c]-triolein load. Biochim. Biophys. Acta 2006, 1761, 37–42. [Google Scholar] [CrossRef]
- Thornton, S.M.; Krolopp, J.E.; Abbott, M.J. IL-15 Mediates Mitochondrial Activity through a PPARδ-Dependent-PPARα-Independent Mechanism in Skeletal Muscle Cells. PPAR Res. 2016, 2016, 1–12. [Google Scholar] [CrossRef]
- Almendro, V.; Fuster, G.; Busquets, S.; Ametller, E.; Figueras, M.; Argilés, J.M.; López-Soriano, F.J. Effects of il-15 on rat brown adipose tissue: Uncoupling proteins and ppars. Obesity 2008, 16, 285–289. [Google Scholar] [CrossRef]
- O’Connell, G.C.; Pistilli, E.E. Interleukin-15 directly stimulates pro-oxidative gene expression in skeletal muscle in-vitro via a mechanism that requires interleukin-15 receptor alpha. Biochem. Biophys. Res. Commun. 2015, 458, 614–619. [Google Scholar] [CrossRef]
- Loro, E.; Bisetto, S.; Khurana, T.S. Mitochondrial ultrastructural adaptations in fast muscles of mice lacking IL15RA. J. Cell Sci. 2018, 131, jcs218313. [Google Scholar] [CrossRef]
- O’Connell, G.C.; Nichols, C.; Guo, G.; Croston, T.L.; Thapa, D.; Hollander, J.M.; Pistilli, E.E. IL-15Rα deficiency in skeletal muscle alters respiratory function and the proteome of mitochondrial subpopulations independent of changes to the mitochondrial genome. Mitochondrion 2015, 25, 87–97. [Google Scholar] [CrossRef]
- Pistilli, E.E.; Bogdanovich, S.; Garton, F.; Yang, N.; Gulbin, J.P.; Conner, J.D.; Anderson, B.G.; Quinn, L.S.; North, K.; Ahima, R.S.; et al. Loss of IL-15 receptor α alters the endurance, fatigability, and metabolic characteristics of mouse fast skeletal muscles. J. Clin. Investig. 2011, 121, 3120–3132. [Google Scholar] [CrossRef] [PubMed]
- Arhire, L.I.; Mihalache, L.; Covasa, M. Irisin: A Hope in Understanding and Managing Obesity and Metabolic Syndrome. Front. Endocrinol. 2019, 10, 524. [Google Scholar] [CrossRef] [PubMed]
- Huh, J.Y.; Mougios, V.; Kabasakalis, A.; Fatouros, I.; Siopi, A.; Douroudos, I.I.; Filippaios, A.; Panagiotou, G.; Park, K.H.; Mantzoros, C.S. Exercise-Induced Irisin Secretion Is Independent of Age or Fitness Level and Increased Irisin May Directly Modulate Muscle Metabolism Through AMPK Activation. J. Clin. Endocrinol. Metab. 2014, 99, E2154–E2161. [Google Scholar] [CrossRef] [PubMed]
- Vaughan, R.A.; Gannon, N.P.; Mermier, C.M.; Conn, C.A. Irisin, a unique non-inflammatory myokine in stimulating skeletal muscle metabolism. J. Physiol. Biochem. 2015, 71, 679–689. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Li, R.; Liu, X.; Wang, L.; Hui, P.; Chan, L.; Saha, P.K.; Hu, Z. ROCK1 reduces mitochondrial content and irisin production in muscle suppressing adipocyte browning and impairing insulin sensitivity. Sci. Rep. 2016, 6, 29669. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.-S.; Kuo, C.-W.; Ko, J.-Y.; Chen, Y.-S.; Wang, S.-Y.; Ke, H.-J.; Kuo, P.-C.; Lee, C.-H.; Wu, J.-C.; Lu, W.-B.; et al. Irisin Mitigates Oxidative Stress, Chondrocyte Dysfunction and Osteoarthritis Development through Regulating Mitochondrial Integrity and Autophagy. Antioxidants 2020, 9, 810. [Google Scholar] [CrossRef]
- Tan, Y.; Ouyang, H.; Xiao, X.; Zhong, J.; Dong, M. Irisin ameliorates septic cardiomyopathy via inhibiting DRP1-related mitochondrial fission and normalizing the JNK-LATS2 signaling pathway. Cell Stress Chaperones 2019, 24, 595–608. [Google Scholar] [CrossRef]
- Bi, J.; Zhang, J.; Ren, Y.; Du, Z.; Li, Q.; Wang, Y.; Wei, S.; Yang, L.; Zhang, J.; Liu, C.; et al. Irisin alleviates liver ischemia-reperfusion injury by inhibiting excessive mitochondrial fission, promoting mitochondrial biogenesis and decreasing oxidative stress. Redox Biol. 2019, 20, 296–306. [Google Scholar] [CrossRef]
- McPherron, A.C.; Lawler, A.M.; Lee, S.J. Regulation of skeletal muscle mass in mice by a new tgf-beta superfamily member. Nature 1997, 387, 83–90. [Google Scholar] [CrossRef]
- Girgenrath, S.; Song, K.; Whittemore, L.A. Loss of myostatin expression alters fiber-type distribution and expression of myosin heavy chain isoforms in slow-and fast-type skeletal muscle. Muscle Nerve Off. J. Am. Assoc. Electrodiagn. Med. 2005, 31, 34–40. [Google Scholar] [CrossRef]
- Hennebry, A.; Berry, C.; Siriett, V.; O’Callaghan, P.; Chau, L.; Watson, T.; Sharma, M.; Kambadur, R. Myostatin regulates fiber-type composition of skeletal muscle by regulating MEF2 and MyoD gene expression. Am. J. Physiol. Physiol. 2009, 296, C525–C534. [Google Scholar] [CrossRef] [PubMed]
- Ploquin, C.; Chabi, B.; Fouret, G.; Vernus, B.; Feillet-Coudray, C.; Coudray, C.; Bonnieu, A.; Ramonatxo, C. Lack of myostatin alters intermyofibrillar mitochondria activity, unbalances redox status, and impairs tolerance to chronic repetitive contractions in muscle. Am. J. Physiol. Metab. 2012, 302, E1000–E1008. [Google Scholar] [CrossRef] [PubMed]
- Helge, A.; Raymond, M.; Roberto, N.; Markus, S.; Susan, C.B.; Anthony, O.; Thomas, V.; Francesco, M.; Gerta, V.; Terence, P.; et al. Lack of myostatin results in excessive muscle growth but impaired force generation. Proc. Natl. Acad. Sci. USA 2007, 104, 1835–1840. [Google Scholar]
- Ge, X.; Vajjala, A.; McFarlane, C.; Wahli, W.; Sharma, M.; Kambadur, R. Lack of Smad3 signaling leads to impaired skeletal muscle regeneration. Am. J. Physiol. Metab. 2012, 303, E90–E102. [Google Scholar] [CrossRef]
- Manfredi, L.H.; Ang, J.; Peker, N.; Dagda, R.K.; McFarlane, C. G protein-coupled receptor kinase 2 regulates mitochondrial bioenergetics and impairs myostatin-mediated autophagy in muscle cells. Am. J. Physiol. Physiol. 2019, 317, C674–C686. [Google Scholar] [CrossRef]
- Lokireddy, S.; Wijesoma, I.W.; Sze, S.K.; McFarlane, C.; Kambadur, R.; Sharma, M. Identification of atrogin-1-targeted proteins during the myostatin-induced skeletal muscle wasting. Am. J. Physiol. Physiol. 2012, 303, C512–C529. [Google Scholar] [CrossRef]
- Aoi, W.; Naito, Y.; Takagi, T.; Tanimura, Y.; Takanami, Y.; Kawai, Y.; Sakuma, K.; Hang, L.P.; Mizushima, K.; Hirai, Y.; et al. A novel myokine, secreted protein acidic and rich in cysteine (SPARC), suppresses colon tumorigenesis via regular exercise. Gut 2012, 62, 882–889. [Google Scholar] [CrossRef]
- Melouane, A.; Carbonell, A.; Yoshioka, M.; Puymirat, J.; St-Amand, J. Implication of SPARC in the modulation of the extracellular matrix and mitochondrial function in muscle cells. PLoS ONE 2018, 13, e0192714. [Google Scholar] [CrossRef]
- Melouane, A.; Yoshioka, M.; Kanzaki, M.; St-Amand, J. Sparc, an EPS-induced gene, modulates the extracellular matrix and mitochondrial function via ILK/AMPK pathways in C2C12 cells. Life Sci. 2019, 229, 277–287. [Google Scholar] [CrossRef]
- Hayyan, M.; Hashim, M.A.; Alnashef, I.M. Superoxide Ion: Generation and Chemical Implications. Chem. Rev. 2016, 116, 3029–3085. [Google Scholar] [CrossRef]
- Madamanchi, N.R.; Runge, M.S. Mitochondrial Dysfunction in Atherosclerosis. Circ. Res. 2007, 100, 460–473. [Google Scholar] [CrossRef] [PubMed]
- Paravicini, T.M.; Touyz, R.M. NADPH Oxidases, Reactive Oxygen Species, and Hypertension: Clinical implications and therapeutic possibilities. Diabetes Care 2008, 31, S170–S180. [Google Scholar] [CrossRef] [PubMed]
- Aon, M.A.; Stanley, B.A.; Sivakumaran, V.; Kembro, J.M.; O’Rourke, B.; Paolocci, N.; Cortassa, S. Glutathione/thioredoxin systems modulate mitochondrial H2O2 emission: An experimental-computational study. J. Gen. Physiol. 2012, 139, 479–491. [Google Scholar] [CrossRef] [PubMed]
- Zou, Z.; Chang, H.; Li, H.; Wang, S. Induction of reactive oxygen species: An emerging approach for cancer therapy. Apoptosis 2017, 22, 1321–1335. [Google Scholar] [CrossRef] [PubMed]
- Tulard, A.; Hoffschir, F.; de Boisferon, F.H.; Luccioni, C.; Bravard, A. Persistent oxidative stress after ionizing radiation is involved in inherited radiosensitivity. Free. Radic. Biol. Med. 2003, 35, 68–77. [Google Scholar] [CrossRef]
- Galley, H.F. Oxidative stress and mitochondrial dysfunction in sepsis. Br. J. Anaesth. 2011, 107, 57–64. [Google Scholar] [CrossRef]
- Shokolenko, I.N.; Wilson, G.L.; Alexeyev, M.F. Aging: A mitochondrial DNA perspective, critical analysis and an update. World J. Exp. Med. 2014, 4, 46–57. [Google Scholar] [CrossRef]
- Mao, X.; Yu, C.R.; Li, W.H. Induction of apoptosis by shikonin through a ROS/JNK-mediated process in Bcr/Abl-positive chronic myelogenous leukemia (CML) cells. Cell Res. 2008, 18, 879–888. [Google Scholar] [CrossRef]
- Shi, Y.; Nikulenkov, F.; Zawacka-Pankau, J.; Li, H.; Gabdoulline, R.R.; Xu, J.; Eriksson, S.; Hedström, E.; Issaeva, N.; Kel, A.; et al. ROS-dependent activation of JNK converts p53 into an efficient inhibitor of oncogenes leading to robust apoptosis. Cell Death Differ. 2014, 21, 612–623. [Google Scholar] [CrossRef]
- He, L.; He, T.; Farrar, S.; Ji, L.; Liu, T.; Ma, X. Antioxidants Maintain Cellular Redox Homeostasis by Elimination of Reactive Oxygen Species. Cell. Physiol. Biochem. 2017, 44, 532–553. [Google Scholar] [CrossRef]
- Gaetani, G.; Ferraris, A.; Rolfo, M.; Mangerini, R.; Arena, S.; Kirkman, H. Predominant role of catalase in the disposal of hydrogen peroxide within human erythrocytes. Blood 1996, 87, 1595–1599. [Google Scholar] [CrossRef] [PubMed]
- Couto, N.; Malys, N.; Gaskell, S.J.; Barber, J. Partition and Turnover of Glutathione Reductase from Saccharomyces cerevisiae: A Proteomic Approach. J. Proteome Res. 2013, 12, 2885–2894. [Google Scholar] [CrossRef] [PubMed]
- Hou, Y.C.; Janczuk, A.; Wang, P.G. Current trends in the development of nitric oxide donors. Curr. Pharm. Des. 1999, 5, 417–441. [Google Scholar] [PubMed]
- Linley, J.E.; Ooi, L.; Pettinger, L.; Kirton, H.; Boyle, J.P.; Peers, C.; Gamper, N. Reactive oxygen species are second messengers of neurokinin signaling in peripheral sensory neurons. Proc. Natl. Acad. Sci. USA 2012, 109, E1578–E1586. [Google Scholar] [CrossRef] [PubMed]
- Rhee, S.G. Cell signaling: H2O2, a Necessary Evil for Cell Signaling. Science 2006, 312, 1882–1883. [Google Scholar] [CrossRef] [PubMed]
- Winterbourn, C.C.; Hampton, M.B. Thiol chemistry and specificity in redox signaling. Free. Radic. Biol. Med. 2008, 45, 549–561. [Google Scholar] [CrossRef]
- Fan, X.; Hussien, R.; Brooks, G.A. H2O2-induced mitochondrial fragmentation in C2C12 myocytes. Free. Radic. Biol. Med. 2010, 49, 1646–1654. [Google Scholar] [CrossRef]
- Muñoz, J.P.; Ivanova, S.; Sánchez-Wandelmer, J.; Martínez-Cristóbal, P.; Noguera, E.; Sancho, A.; Díaz-Ramos, A.; Hernández-Alvarez, M.I.; Sebastián, D.; Mauvezin, C.; et al. Mfn2 modulates the UPR and mitochondrial function via repression of PERK. EMBO J. 2013, 32, 2348–2361. [Google Scholar] [CrossRef]
- Barsoum, M.J.; Yuan, H.; Gerencser, A.A.; Liot, G.; Kushnareva, Y.; Gräber, S.; Kovacs, I.; Lee, W.D.; Waggoner, J.; Cui, J.; et al. Nitric oxide-induced mitochondrial fission is regulated by dynamin-related GTPases in neurons. EMBO J. 2006, 25, 3900–3911. [Google Scholar] [CrossRef]
- Wu, C.L.; Chen, S.D.; Yin, J.H.; Hwang, C.S.; Yang, D.I. Nuclear factor-kappab-dependent sestrin2 induction mediates the antioxidant effects of bdnf against mitochondrial inhibition in rat cortical neurons. Mol. Neurobiol. 2016, 53, 4126–4142. [Google Scholar] [CrossRef]
- Molinari, C.; Morsanuto, V.; Ruga, S.; Notte, F.; Farghali, M.; Galla, R.; Uberti, F. The Role of BDNF on Aging-Modulation Markers. Brain Sci. 2020, 10, 285. [Google Scholar] [CrossRef] [PubMed]
- Petzold, A.; Psotta, L.; Brigadski, T.; Endres, T.; Lessmann, V. Chronic BDNF deficiency leads to an age-dependent impairment in spatial learning. Neurobiol. Learn. Mem. 2015, 120, 52–60. [Google Scholar] [CrossRef] [PubMed]
- Hachem, L.D.; Mothe, A.J.; Tator, C.H. Effect of BDNF and Other Potential Survival Factors in Models of In Vitro Oxidative Stress on Adult Spinal Cord–Derived Neural Stem/Progenitor Cells. BioResearch Open Access 2015, 4, 146–159. [Google Scholar] [CrossRef] [PubMed]
- Guo, C.C.; Jiao, C.H.; Gao, Z.M. Silencing of lncrna bdnf-as attenuates abeta25-35-induced neurotoxicity in pc12 cells by suppressing cell apoptosis and oxidative stress. Neurol Res. 2018, 40, 795–804. [Google Scholar] [CrossRef]
- Jin, H.; Zhu, Y.; Li, Y.; Ding, X.; Ma, W.; Han, X.; Wang, B. BDNF-mediated mitophagy alleviates high-glucose-induced brain microvascular endothelial cell injury. Apoptosis 2019, 24, 511–528. [Google Scholar] [CrossRef]
- Rosenblum, S.; Smith, T.N.; Wang, N.; Chua, J.Y.; Westbroek, E.; Wang, K.; Guzman, R. BDNF Pretreatment of Human Embryonic-Derived Neural Stem Cells Improves Cell Survival and Functional Recovery after Transplantation in Hypoxic–Ischemic Stroke. Cell Transplant. 2015, 24, 2449–2461. [Google Scholar] [CrossRef]
- Jin, H.; Zhu, Y.; Wang, X.-D.; Luo, E.-F.; Li, Y.-P.; Wang, B.-L.; Chen, Y.-F. BDNF corrects NLRP3 inflammasome-induced pyroptosis and glucose metabolism reprogramming through KLF2/HK1 pathway in vascular endothelial cells. Cell. Signal. 2021, 78, 109843. [Google Scholar] [CrossRef]
- Guo, D.; Xiao, L.; Hu, H.; Liu, M.; Yang, L.; Lin, X. FGF21 protects human umbilical vein endothelial cells against high glucose-induced apoptosis via PI3K/Akt/Fox3a signaling pathway. J. Diabetes Complicat. 2018, 32, 729–736. [Google Scholar] [CrossRef]
- Zeng, Z.; Zheng, Q.; Chen, J.; Tan, X.; Li, Q.; Ding, L.; Zhang, R.; Xiaolong, L. FGF21 mitigates atherosclerosis via inhibition of NLRP3 inflammasome-mediated vascular endothelial cells pyroptosis. Exp. Cell Res. 2020, 393, 112108. [Google Scholar] [CrossRef]
- Xu, M.; Wang, L.; Wang, M.; Wang, H.; Zhang, H.; Chen, Y.; Wang, X.; Gong, J.; Zhang, J.; Adcock, I.M.; et al. Mitochondrial ROS and NLRP3 inflammasome in acute ozone-induced murine model of airway inflammation and bronchial hyperresponsiveness. Free. Radic. Res. 2019, 53, 780–790. [Google Scholar] [CrossRef]
- Planavila, A.; Redondo-Angulo, I.; Ribas, F.; Garrabou, G.; Casademont, J.; Giralt, M.; Villarroya, F. Fibroblast growth factor 21 protects the heart from oxidative stress. Cardiovasc. Res. 2014, 106, 19–31. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.-W.; Jiang, X.; Zhang, Y.; Wang, J.; Xie, J.; Wang, Y.-Q.; Li, Y.-H. FGF21 Protects Against Hypoxia Injury Through Inducing HSP72 in Cerebral Microvascular Endothelial Cells. Front. Pharmacol. 2019, 10, 101. [Google Scholar] [CrossRef] [PubMed]
- Zhu, S.; Ma, L.; Wu, Y.; Ye, X.; Zhang, T.; Zhang, Q.; Rasoul, L.M.; Liu, Y.; Guo, M.; Zhou, B.; et al. FGF21 treatment ameliorates alcoholic fatty liver through activation of AMPK-SIRT1 pathway. Acta Biochim. Biophys. Sin. 2014, 46, 1041–1048. [Google Scholar] [CrossRef] [PubMed]
- Abid, H.; Hart, C.; Lanza, I. Effects of local interleukin-6 on skeletal muscle mitochondrial physiology. FASEB J. 2018, 32, 603–607. [Google Scholar]
- Forcina, L.; Miano, C.; Scicchitano, B.M.; Rizzuto, E.; Berardinelli, M.G.; De Benedetti, F.; Pelosi, L.; Musarò, A. Increased Circulating Levels of Interleukin-6 Affect the Redox Balance in Skeletal Muscle. Oxidative Med. Cell. Longev. 2019, 2019, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Dong, Y.; Wu, Z.; He, M.; Chen, Y.; Chen, Y.; Shen, X.; Zhao, X.; Zhang, L.; Yuan, B.; Zeng, Z.-C. ADAM9 mediates the interleukin-6-induced Epithelial–Mesenchymal transition and metastasis through ROS production in hepatoma cells. Cancer Lett. 2018, 421, 1–14. [Google Scholar] [CrossRef]
- Ding, W.; You, H.; Dang, H.; Leblanc, F.; Galicia, V.; Lu, S.C.; Stiles, B.; Rountree, C.B. Epithelial-to-mesenchymal transition of murine liver tumor cells promotes invasion. Hepatology 2010, 52, 945–953. [Google Scholar] [CrossRef]
- Ji, C.; Chen, X.; Gao, C.; Jiao, L.; Wang, J.; Xu, G.; Fu, H.; Guo, X.; Zhao, Y. IL-6 induces lipolysis and mitochondrial dysfunction, but does not affect insulin-mediated glucose transport in 3T3-L1 adipocytes. J. Bioenerg. Biomembr. 2011, 43, 367–375. [Google Scholar] [CrossRef]
- Kojima, H.; Kunimoto, H.; Inoue, T.; Nakajima, K. The STAT3-IGFBP5 axis is critical for IL-6/gp130-induced premature senescence in human fibroblasts. Cell Cycle 2012, 11, 730–739. [Google Scholar] [CrossRef]
- Rochfort, K.D.; Collins, L.E.; Murphy, R.P.; Cummins, P.M. Downregulation of Blood-Brain Barrier Phenotype by Proinflammatory Cytokines Involves NADPH Oxidase-Dependent ROS Generation: Consequences for Interendothelial Adherens and Tight Junctions. PLoS ONE 2014, 9, e101815. [Google Scholar] [CrossRef]
- Marasco, M.R.; Conteh, A.M.; Reissaus, C.A.; Cupit, J.E.T.; Appleman, E.M.; Mirmira, R.G.; Linnemann, A.K. Interleukin-6 reduces beta-cell oxidative stress by linking autophagy with the antioxidant response. Diabetes 2018, 67, 1576–1588. [Google Scholar] [CrossRef] [PubMed]
- Kaur, N.; Naga, O.S.; Norell, H.; Al-Khami, A.A.; Scheffel, M.J.; Chakraborty, N.G.; Voelkel-Johnson, C.; Mukherji, B.; Mehrotra, S. T cells expanded in presence of IL-15 exhibit increased antioxidant capacity and innate effector molecules. Cytokine 2011, 55, 307–317. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Neo, S.Y.; Chen, Z.; Cui, W.; Chen, Y.; Guo, M.; Wang, Y.; Xu, H.; Kurzay, A.; Alici, E.; et al. Thioredoxin activity confers resistance against oxidative stress in tumor-infiltrating NK cells. J. Clin. Investig. 2020, 130, 5508–5522. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Li, Y.; Tang, Y.; Lin, B.; Kong, X.; Oladele, O.A.; Yin, Y. Protective effect of myokine IL-15 against H2O2-mediated oxidative stress in skeletal muscle cells. Mol. Biol. Rep. 2014, 41, 7715–7722. [Google Scholar] [CrossRef]
- Ho, M.-Y.; Wen, M.-S.; Yeh, J.-K.; Hsieh, I.-C.; Chen, C.-C.; Hsieh, M.-J.; Tsai, M.-L.; Yang, C.-H.; Wu, V.C.-C.; Hung, K.-C.; et al. Excessive irisin increases oxidative stress and apoptosis in murine heart. Biochem. Biophys. Res. Commun. 2018, 503, 2493–2498. [Google Scholar] [CrossRef]
- Wang, Z.; Chen, K.; Han, Y.; Zhu, H.; Zhou, X.; Tan, T.; Zeng, J.; Zhang, J.; Liu, Y.; Li, Y.; et al. Irisin Protects Heart Against Ischemia-Reperfusion Injury Through a SOD2-Dependent Mitochondria Mechanism. J. Cardiovasc. Pharmacol. 2018, 72, 259–269. [Google Scholar] [CrossRef]
- Chen, K.; Xu, Z.; Liu, Y.; Wang, Z.; Li, Y.; Xu, X.; Chen, C.; Xia, T.; Liao, Q.; Yao, Y.; et al. Irisin protects mitochondria function during pulmonary ischemia/reperfusion injury. Sci. Transl. Med. 2017, 9, eaao6298. [Google Scholar] [CrossRef]
- Zhang, M.; Xu, Y.; Jiang, L. Irisin attenuates oxidized low-density lipoprotein impaired angiogenesis through AKT/mTOR/S6K1/Nrf2 pathway. J. Cell. Physiol. 2019, 234, 18951–18962. [Google Scholar] [CrossRef]
- Lee, H.J.; Lee, J.O.; Kim, N.; Kim, J.K.; Kim, H.I.; Lee, Y.W.; Kim, S.J.; Choi, J.-I.; Oh, Y.; Kim, J.H.; et al. Irisin, a Novel Myokine, Regulates Glucose Uptake in Skeletal Muscle Cells via AMPK. Mol. Endocrinol. 2015, 29, 873–881. [Google Scholar] [CrossRef]
- Aravena, J.; Abrigo, J.; Gonzalez, F.; Aguirre, F.; Gonzalez, A.; Simon, F.; Cabello-Verrugio, C. Angiotensin (1–7) decreases myostatin-induced nf-kappab signaling and skeletal muscle atrophy. Int. J. Mol. Sci. 2020, 21, 1167. [Google Scholar] [CrossRef]
- Sriram, S.; Subramanian, S.; Juvvuna, P.K.; Ge, X.; Lokireddy, S.; McFarlane, C.D.; Wahli, W.; Kambadur, R.; Sharma, M. Myostatin augments muscle-specific ring finger protein-1 expression through an nf-kb independent mechanism in smad3 null muscle. Mol. Endocrinol. 2014, 28, 317–330. [Google Scholar] [CrossRef] [PubMed]
- Han, Y.-Q.; Ming, S.-L.; Wu, H.-T.; Zeng, L.; Ba, G.; Li, J.; Lu, W.-F.; Han, J.; Du, Q.-J.; Sun, M.-M.; et al. Myostatin knockout induces apoptosis in human cervical cancer cells via elevated reactive oxygen species generation. Redox Biol. 2018, 19, 412–428. [Google Scholar] [CrossRef] [PubMed]
- Verzola, D.; Milanesi, S.; Viazzi, F.; Ansaldo, F.; Saio, M.; Garibaldi, S.; Carta, A.; Costigliolo, F.; Salvidio, G.; Barisione, C.; et al. Enhanced myostatin expression and signalling promote tubulointerstitial inflammation in diabetic nephropathy. Sci. Rep. 2020, 10, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Forrester, S.J.; Kikuchi, D.S.; Hernandes, M.S.; Xu, Q.; Griendling, K.K. Reactive Oxygen Species in Metabolic and Inflammatory Signaling. Circ. Res. 2018, 122, 877–902. [Google Scholar] [CrossRef]
- Angelova, P.R.; Abramov, A.Y. Role of mitochondrial ROS in the brain: From physiology to neurodegeneration. FEBS Lett. 2018, 592, 692–702. [Google Scholar] [CrossRef] [PubMed]
- Liou, G.Y.; Storz, P. Reactive oxygen species in cancer. Free Radic. Res. 2010, 44, 479–496. [Google Scholar] [CrossRef]
- Liguori, I.; Russo, G.; Curcio, F.; Bulli, G.; Aran, L.; Della-Morte, D.; Gargiulo, G.; Testa, G.; Cacciatore, F.; Bonaduce, D.; et al. Oxidative stress, aging, and diseases. Clin. Interv. Aging 2018, 13, 757–772. [Google Scholar] [CrossRef]
- Chan, D.C. Mitochondrial Dynamics and Its Involvement in Disease. Annu. Rev. Pathol. Mech. Dis. 2020, 15, 235–259. [Google Scholar] [CrossRef]
- Sharma, A.; Smith, H.J.; Yao, P.; Mair, W.B. Causal roles of mitochondrial dynamics in longevity and healthy aging. EMBO Rep. 2019, 20, e48395. [Google Scholar] [CrossRef]
- Geto, Z.D.; Molla, M.D.; Challa, F.; Belay, Y.; Getahun, T. Mitochondrial Dynamic Dysfunction as a Main Triggering Factor for Inflammation Associated Chronic Non-Communicable Diseases. J. Inflamm. Res. 2020, 13, 97–107. [Google Scholar] [CrossRef]
- Zhang, H.; Liu, B.; Li, T.; Zhu, Y.; Luo, G.; Jiang, Y.; Tang, F.; Jian, Z.; Xiao, Y. AMPK activation serves a critical role in mitochondria quality control via modulating mitophagy in the heart under chronic hypoxia. Int. J. Mol. Med. 2017, 41, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Kornfeld, O.S.; Hwang, S.; Disatnik, M.H.; Chen, C.H.; Qvit, N.; Mochly-Rosen, D. Mitochondrial reactive oxygen species at the heart of the matter: New therapeutic approaches for cardiovascular diseases. Circ. Res. 2015, 116, 1783–1799. [Google Scholar] [CrossRef] [PubMed]
- Szeto, H.H. Mitochondria-targeted peptide antioxidants: Novel neuroprotective agents. AAPS J. 2006, 8, E521–E531. [Google Scholar] [CrossRef] [PubMed]
- Eckel, J. Myokines in metabolic homeostasis and diabetes. Diabetologia 2019, 62, 1523–1528. [Google Scholar] [CrossRef]
- Bostroem, P.; Wu, J.; Jedrychowski, M.P.; Korde, A.; Ye, L.; Lo, J.C.; Rasbach, K.A.; Bostroem, E.A.; Choi, J.H.; Long, J.Z.; et al. A PGC1-α-dependent myokine that drives brown-fat-like development of white fat and thermogenesis. Nat. Cell Biol. 2012, 481, 463–468. [Google Scholar] [CrossRef]
- Görgens, S.W.; Eckardt, K.; Jensen, J.D.; Drevon, C.A.; Eckel, J. Exercise and Regulation of Adipokine and Myokine Production. Progress Mol. Biol. Transl. Sci. 2015, 135, 313–336. [Google Scholar] [CrossRef]
- Pedersen, B.K. Physical activity and muscle–brain crosstalk. Nat. Rev. Endocrinol. 2019, 15, 383–392. [Google Scholar] [CrossRef]
- Giudice, J.; Taylor, J.M. Muscle as a paracrine and endocrine organ. Curr. Opin. Pharmacol. 2017, 34, 49–55. [Google Scholar] [CrossRef]
- WHO. Global Recommendations on Physical Activity for Health; WHO: Geneva, Switzerland, 2010. [Google Scholar]
- Powers, S.K.; Bomkamp, M.; Ozdemir, M.; Hyatt, H. Mechanisms of exercise-induced preconditioning in skeletal muscles. Redox Biol. 2020, 35, 101462. [Google Scholar] [CrossRef]
- Drake, J.C.; Wilson, R.J.; Yan, Z. Molecular mechanisms for mitochondrial adaptation to exercise training in skeletal muscle. FASEB J. 2016, 30, 13–22. [Google Scholar] [CrossRef]
- Leek, B.T.; Mudaliar, S.R.D.; Henry, R.; Mathieu-Costello, O.; Richardson, R.S. Effect of acute exercise on citrate synthase activity in untrained and trained human skeletal muscle. Am. J. Physiol. Integr. Comp. Physiol. 2001, 280, R441–R447. [Google Scholar] [CrossRef] [PubMed]
- Menshikova, E.V.; Ritov, V.B.; Fairfull, L.; Ferrell, R.E.; Kelley, D.E.; Goodpaster, B.H. Effects of Exercise on Mitochondrial Content and Function in Aging Human Skeletal Muscle. J. Gerontol. Ser. A Boil. Sci. Med Sci. 2006, 61, 534–540. [Google Scholar] [CrossRef] [PubMed]
- Talanian, J.L.; Galloway, S.D.R.; Heigenhauser, G.J.F.; Bonen, A.; Spriet, L.L. Two weeks of high-intensity aerobic interval training increases the capacity for fat oxidation during exercise in women. J. Appl. Physiol. 2007, 102, 1439–1447. [Google Scholar] [CrossRef] [PubMed]
- MacInnis, M.J.; Zacharewicz, E.; Martin, B.J.; Haikalis, M.E.; Skelly, L.E.; Tarnopolsky, M.A.; Murphy, R.M.; Gibala, M.J. Superior mitochondrial adaptations in human skeletal muscle after interval compared to continuous single-leg cycling matched for total work. J. Physiol. 2017, 595, 2955–2968. [Google Scholar] [CrossRef] [PubMed]
- Arribat, Y.; Broskey, N.T.; Greggio, C.; Boutant, M.; Alonso, S.C.; Kulkarni, S.S.; Lagarrigue, S.; Carnero, E.A.; Besson, C.; Canto, C.; et al. Distinct patterns of skeletal muscle mitochondria fusion, fission and mitophagy upon duration of exercise training. Acta Physiol. 2018, 225, e13179. [Google Scholar] [CrossRef]
- Brandt, N.; Gunnarsson, T.P.; Bangsbo, J.; Pilegaard, H. Exercise and exercise training-induced increase in autophagy markers in human skeletal muscle. Physiol. Rep. 2018, 6, e13651. [Google Scholar] [CrossRef]
- Leal, L.G.; Lopes, M.A.; Batista, J.M.L. Physical Exercise-Induced Myokines and Muscle-Adipose Tissue Crosstalk: A Review of Current Knowledge and the Implications for Health and Metabolic Diseases. Front. Physiol. 2018, 9, 1307. [Google Scholar] [CrossRef]
- Mäkelä, J.; Tselykh, T.V.; Maiorana, F.; Eriksson, O.; Do, H.T.; Mudò, G.; Korhonen, L.T.; Belluardo, N.; Lindholm, D. Fibroblast growth factor-21 enhances mitochondrial functions and increases the activity of PGC-1α in human dopaminergic neurons via Sirtuin-1. SpringerPlus 2014, 3, 1–12. [Google Scholar] [CrossRef]
- Fan, W.; Evans, R.M. Exercise Mimetics: Impact on Health and Performance. Cell Metab. 2017, 25, 242–247. [Google Scholar] [CrossRef]
- Colaianni, G.; Mongelli, T.; Cuscito, C.; Pignataro, P.; Lippo, L.; Spiro, G.; Notarnicola, A.; Severi, I.; Passeri, G.; Mori, G.; et al. Irisin prevents and restores bone loss and muscle atrophy in hind-limb suspended mice. Sci. Rep. 2017, 7, 1–16. [Google Scholar] [CrossRef]
- Trovato, E.; Di Felice, V.; Barone, R. Extracellular Vesicles: Delivery Vehicles of Myokines. Front. Physiol. 2019, 10, 522. [Google Scholar] [CrossRef] [PubMed]
- Huertas, J.R.; Casuso, R.A.; Agustín, P.H.; Cogliati, S. Stay Fit, Stay Young: Mitochondria in Movement: The Role of Exercise in the New Mitochondrial Paradigm. Oxidative Med. Cell. Longev. 2019, 2019, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Jubrias, S.A.; Esselman, P.C.; Price, L.B.; Cress, M.E.; Conley, K.E. Large energetic adaptations of elderly muscle to resistance and endurance training. J. Appl. Physiol. 2001, 90, 1663–1670. [Google Scholar] [CrossRef]
- Ekaterina, S.; Ana, S.; Zhiyong, Z.; Zhan, G.; Siva Rama Krishna, K.; Santiago, R.; Elizabeth, S.; Susan, A.W.; Michael, R.A.; Carmen, M.P.-T.; et al. Musclin is an activity-stimulated myokine that enhances physical endurance. Proc. Natl. Acad. Sci. USA 2015, 112, 16042–16047. [Google Scholar]
- Wolsk, E.; Mygind, H.; Grøndahl, T.S.; Pedersen, B.K.; van Hall, G. IL-6 selectively stimulates fat metabolism in human skeletal muscle. Am. J. Physiol. Metab. 2010, 299, E832–E840. [Google Scholar] [CrossRef] [PubMed]
- Quinn, L.S.; Anderson, B.G.; Conner, J.D.; Wolden-Hanson, T. IL-15 Overexpression Promotes Endurance, Oxidative Energy Metabolism, and Muscle PPARδ, SIRT1, PGC-1α, and PGC-1β Expression in Male Mice. Endocrinology 2013, 154, 232–245. [Google Scholar] [CrossRef] [PubMed]
- Dillard, C.J.; Litov, R.E.; Savin, W.M.; Dumelin, E.E.; Tappel, A.L. Effects of exercise, vitamin E, and ozone on pulmonary function and lipid peroxidation. J. Appl. Physiol. 1978, 45, 927–932. [Google Scholar] [CrossRef]
- Davies, K.J.; Quintanilha, A.T.; Brooks, G.A.; Packer, L. Free radicals and tissue damage produced by exercise. Biochem. Biophys. Res. Commun. 1982, 107, 1198–1205. [Google Scholar] [CrossRef]
- Venditti, P.; di Meo, S. Effect of Training on Antioxidant Capacity, Tissue Damage, and Endurance of Adult Male Rats. Int. J. Sports Med. 1997, 18, 497–502. [Google Scholar] [CrossRef]
- Saborido, A.; Naudí, A.; Portero-Otin, M.; Pamplona, R.; Megías, A. Stanozolol treatment decreases the mitochondrial ROS generation and oxidative stress induced by acute exercise in rat skeletal muscle. J. Appl. Physiol. 2011, 110, 661–669. [Google Scholar] [CrossRef]
- Dröge, W. Free Radicals in the Physiological Control of Cell Function. Physiol. Rev. 2002, 82, 47–95. [Google Scholar] [CrossRef] [PubMed]
- Henriquez-Olguín, C.; Knudsen, J.R.; Raun, S.H.; Li, Z.; Dalbram, E.; Treebak, J.T.; Sylow, L.; Holmdahl, R.; Richter, E.A.; Jaimovich, E.; et al. Cytosolic ROS production by NADPH oxidase 2 regulates muscle glucose uptake during exercise. Nat. Commun. 2019, 10, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Jensen, T.E.; Schjerling, P.; Viollet, B.; Wojtaszewski, J.F.P.; Richter, E.A. AMPK α1 Activation Is Required for Stimulation of Glucose Uptake by Twitch Contraction, but Not by H2O2, in Mouse Skeletal Muscle. PLoS ONE 2008, 3, e2102. [Google Scholar] [CrossRef] [PubMed]
- Santos-Silva, A.; Rebelo, M.I.; Castro, E.M.B.; Belo, L.; Guerra, A.; Rego, C.; Quintanilha, A. Leukocyte activation, erythrocyte damage, lipid profile and oxidative stress imposed by high competition physical exercise in adolescents. Clin. Chim. Acta 2001, 306, 119–126. [Google Scholar] [CrossRef]
- Sun, F.; Norman, I.J.; While, A.E. Physical activity in older people: A systematic review. BMC Public Health 2013, 13, 449. [Google Scholar] [CrossRef]
- Goodpaster, B.H.; Park, S.W.; Harris, T.B.; Kritchevsky, S.B.; Nevitt, M.; Schwartz, A.V.; Simonsick, E.M.; Tylavsky, F.A.; Visser, M.; Newman, A.B.; et al. The Loss of Skeletal Muscle Strength, Mass, and Quality in Older Adults: The Health, Aging and Body Composition Study. J. Gerontol. Ser. A Boil. Sci. Med Sci. 2006, 61, 1059–1064. [Google Scholar] [CrossRef]
- Baumann, C.W.; Kwak, D.; Liu, H.M.; Thompson, L.V. Age-induced oxidative stress: How does it influence skeletal muscle quantity and quality? J. Appl. Physiol. 2016, 121, 1047–1052. [Google Scholar] [CrossRef]
- Kim, J.-S.; Lee, Y.-H.; Yi, H.-K. Gradual downhill running improves age-related skeletal muscle and bone weakness: Implication of autophagy and bone morphogenetic proteins. Exp. Physiol. 2016, 101, 1528–1540. [Google Scholar] [CrossRef]
- Kim, H.-J.; So, B.; Choi, M.; Kang, D.; Song, W. Resistance exercise training increases the expression of irisin concomitant with improvement of muscle function in aging mice and humans. Exp. Gerontol. 2015, 70, 11–17. [Google Scholar] [CrossRef]
- Piccirillo, R. Exercise-Induced Myokines With Therapeutic Potential for Muscle Wasting. Front. Physiol. 2019, 10, 287. [Google Scholar] [CrossRef]
- Nakamura, K.; Yamanouchi, K.; Nishihara, M. Secreted protein acidic and rich in cysteine internalization and its age-related alterations in skeletal muscle progenitor cells. Aging Cell 2013, 13, 175–184. [Google Scholar] [CrossRef] [PubMed]
- Kwon, J.H.; Moon, K.M.; Min, K.-W. Exercise-Induced Myokines can Explain the Importance of Physical Activity in the Elderly: An Overview. Healthcare 2020, 8, 378. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Jun, H.-S. Role of Myokines in Regulating Skeletal Muscle Mass and Function. Front. Physiol. 2019, 10, 42. [Google Scholar] [CrossRef] [PubMed]
- Gianni, P.; Jan, K.J.; Douglas, M.J.; Stuart, P.M.; Tarnopolsky, M.A. Oxidative stress and the mitochondrial theory of aging in human skeletal muscle. Exp. Gerontol. 2004, 39, 1391–1400. [Google Scholar] [CrossRef] [PubMed]
- Sullivan-Gunn, M.J.; Lewandowski, P.A. Elevated hydrogen peroxide and decreased catalase and glutathione peroxidase protection are associated with aging sarcopenia. BMC Geriatr. 2013, 13, 104. [Google Scholar] [CrossRef]
- Liverini, G.; Bianco, F.; Mazzoli, A.; Giacco, A.; Liverini, G.; Iossa, S. Alterations in proton leak, oxidative status and uncoupling protein 3 content in skeletal muscle subsarcolemmal and intermyofibrillar mitochondria in old rats. BMC Geriatr. 2014, 14, 79. [Google Scholar] [CrossRef]
- Joseph, A.-M.; Adhihetty, P.J.; Leeuwenburgh, C. Beneficial effects of exercise on age-related mitochondrial dysfunction and oxidative stress in skeletal muscle. J. Physiol. 2016, 594, 5105–5123. [Google Scholar] [CrossRef]
- Carter, H.N.; Chen, C.C.W.; Hood, D.A. Mitochondria, Muscle Health, and Exercise with Advancing Age. Physiology 2015, 30, 208–223. [Google Scholar] [CrossRef]
- Yeo, D.; Kang, C.; Ji, L.L. Aging alters acetylation status in skeletal and cardiac muscles. GeroScience 2020, 42, 963–976. [Google Scholar] [CrossRef]
- Pansarasa, O.; Castagna, L.; Colombi, B.; Vecchiet, J.; Felzani, G.; Marzatico, F. Age and sex differences in human skeletal muscle: Role of reactive oxygen species. Free. Radic. Res. 2000, 33, 287–293. [Google Scholar] [CrossRef]
- Siu, P.M.; Pistilli, E.E.; Alway, S.E. Age-dependent increase in oxidative stress in gastrocnemius muscle with unloading. J. Appl. Physiol. 2008, 105, 1695–1705. [Google Scholar] [CrossRef] [PubMed]
- Pansarasa, O.; Bertorelli, L.; Vecchiet, J.; Felzani, G.; Marzatico, F. Age-dependent changes of antioxidant activities and markers of free radical damage in human skeletal muscle. Free. Radic. Biol. Med. 1999, 27, 617–622. [Google Scholar] [CrossRef]
- Safdar, A.; Hamadeh, M.J.; Kaczor, J.J.; Raha, S.; Debeer, J.; Tarnopolsky, M.A. Aberrant Mitochondrial Homeostasis in the Skeletal Muscle of Sedentary Older Adults. PLoS ONE 2010, 5, e10778. [Google Scholar] [CrossRef] [PubMed]
- Guiraud, S.; van Wittenberghe, L.; Georger, C.; Scherman, D.; Kichler, A. Identification of decorin derived peptides with a zinc dependent anti-myostatin activity. Neuromuscul. Disord. 2012, 22, 1057–1068. [Google Scholar]
- Reza, M.M.; Subramaniyam, N.; Sim, C.M.; Ge, X.; Sathiakumar, D.; McFarlane, C.; Sharma, M.; Kambadur, R. Irisin is a pro-myogenic factor that induces skeletal muscle hypertrophy and rescues denervation-induced atrophy. Nat. Commun. 2017, 8, 1–17. [Google Scholar] [CrossRef]
- Jang, Y.C.; Sinha, M.; Cerletti, M.; Dall’Osso, C.; Wagers, A.J. Skeletal Muscle Stem Cells: Effects of Aging and Metabolism on Muscle Regenerative Function. Cold Spring Harb. Symp. Quant. Biol. 2011, 76, 101–111. [Google Scholar] [CrossRef]
- Belli, R.; Bonato, A.; De Angelis, L.; Mirabilii, S.; Ricciardi, M.R.; Tafuri, A.; Molfino, A.; Leigheb, M.; Costelli, P.; Caruso, M.; et al. Metabolic Reprogramming Promotes Myogenesis During Aging. Front. Physiol. 2019, 10, 897. [Google Scholar] [CrossRef]
- Camporez, J.-P.G.; Petersen, M.C.; Abudukadier, A.; Moreira, G.V.; Jurczak, M.J.; Friedman, G.; Haqq, C.M.; Petersen, K.F.; Shulman, G.I. Anti-myostatin antibody increases muscle mass and strength and improves insulin sensitivity in old mice. Proc. Natl. Acad. Sci. USA 2016, 113, 2212–2217. [Google Scholar] [CrossRef]
- Delanaye, P.; Bataille, S.; Quinonez, K.; Buckinx, F.; Warling, X.; Krzesinski, J.-M.; Pottel, H.; Burtey, S.; Bruyère, O.; Cavalier, E. Myostatin and Insulin-Like Growth Factor 1 Are Biomarkers of Muscle Strength, Muscle Mass, and Mortality in Patients on Hemodialysis. J. Ren. Nutr. 2019, 29, 511–520. [Google Scholar] [CrossRef]
- Coelho-Junior, H.; Picca, A.; Calvani, R.; Uchida, M.C.; Marzetti, E. If my muscle could talk: Myokines as a biomarker of frailty. Exp. Gerontol. 2019, 127, 110715. [Google Scholar] [CrossRef]
- Park, H.-S.; Kim, H.C.; Zhang, D.; Yeom, H.; Kil Lim, S. The novel myokine irisin: Clinical implications and potential role as a biomarker for sarcopenia in postmenopausal women. Endocrine 2019, 64, 341–348. [Google Scholar] [CrossRef] [PubMed]
- Miyazaki, S.; Iino, N.; Koda, R.; Narita, I.; Kaneko, Y. Brain-derived neurotrophic factor is associated with sarcopenia and frailty in Japanese hemodialysis patients. Geriatr. Gerontol. Int. 2021, 21, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Ng, T.K.S.; Ho, C.; Tam, W.; Kua, E.H.; Ho, R. Decreased Serum Brain-Derived Neurotrophic Factor (BDNF) Levels in Patients with Alzheimer’s Disease (AD): A Systematic Review and Meta-Analysis. Int. J. Mol. Sci. 2019, 20, 257. [Google Scholar] [CrossRef] [PubMed]
- Miranda, M.; Morici, J.F.; Zanoni, M.B.; Bekinschtein, P. Brain-Derived Neurotrophic Factor: A Key Molecule for Memory in the Healthy and the Pathological Brain. Front. Cell. Neurosci. 2019, 13, 363. [Google Scholar] [CrossRef]
- Khan, I.U. Irisin: As a Therapeutic Target for Metabolic Disorders. J. Endocrinol. Metab. 2018, 8, 87–93. [Google Scholar] [CrossRef]
- Suomalainen, A.; Elo, J.M.; Pietiläinen, K.H.; Hakonen, A.H.; Sevastianova, K.; Korpela, M.; Isohanni, P.; Marjavaara, S.K.; Tyni, T.; Kiuru-Enari, S.; et al. FGF-21 as a biomarker for muscle-manifesting mitochondrial respiratory chain deficiencies: A diagnostic study. Lancet Neurol. 2011, 10, 806–818. [Google Scholar] [CrossRef]
- Muñoz-Fuentes, V.; Cacheiro, P.; Meehan, T.F.; Aguilar-Pimentel, J.A.; Brown, S.D.M.; Flenniken, A.M.; Flicek, P.; Galli, A.; Mashhadi, H.H.; Hrabě de Angelis, M.; et al. The International Mouse Phenotyping Consortium (IMPC): A functional catalogue of the mammalian genome that informs conservation. Conserv. Genet. 2018, 19, 995–1005. [Google Scholar] [CrossRef]
- Talukdar, S.; Zhou, Y.; Li, D.; Rossulek, M.; Dong, J.; Somayaji, V.; Weng, Y.; Clark, R.; Lanba, A.; Owen, B.M.; et al. A Long-Acting FGF21 Molecule, PF-05231023, Decreases Body Weight and Improves Lipid Profile in Non-human Primates and Type 2 Diabetic Subjects. Cell Metab. 2016, 23, 427–440. [Google Scholar] [CrossRef]
- Li, Y.-Y.; Hsieh, L.-L.; Tang, R.-P.; Liao, S.-K.; Yeh, K.-Y. Interleukin-6 (IL-6) released by macrophages induces IL-6 secretion in the human colon cancer HT-29 cell line. Hum. Immunol. 2009, 70, 151–158. [Google Scholar] [CrossRef]
- Fukuno, N.; Matsui, H.; Kanda, Y.; Suzuki, O.; Matsumoto, K.; Sasaki, K.; Kobayashi, T.; Tamura, S. Tgf-beta-activated kinase 1 mediates mechanical stress-induced il-6 expression in osteoblasts. Biochem. Biophys. Res. Commun. 2011, 408, 202–207. [Google Scholar] [CrossRef]
- Zampetaki, A.; Zhang, Z.; Hu, Y.; Xu, Q. Biomechanical stress induces il-6 expression in smooth muscle cells via ras/rac1-p38 mapk-nf-kappab signaling pathways. Am. J. Physiol. Heart Circ. Physiol. 2005, 288, H2946–H2954. [Google Scholar] [CrossRef] [PubMed]
- Han, M.S.; White, A.; Perry, R.J.; Camporez, J.-P.; Hidalgo, J.; Shulman, G.I.; Davis, R.J. Regulation of adipose tissue inflammation by interleukin 6. Proc. Natl. Acad. Sci. USA 2020, 117, 2751–2760. [Google Scholar] [CrossRef] [PubMed]
- Glund, S.; Deshmukh, A.; Long, Y.C.; Moller, T.; Koistinen, H.A.; Caidahl, K.; Zierath, J.R.; Krook, A. Interleukin-6 Directly Increases Glucose Metabolism in Resting Human Skeletal Muscle. Diabetes 2007, 56, 1630–1637. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).