Cognitive Rehabilitation Improves Functional Vision Skills in Children with Cerebral Visual Impairment
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Tools
2.2.1. Sociodemographic and Background Form
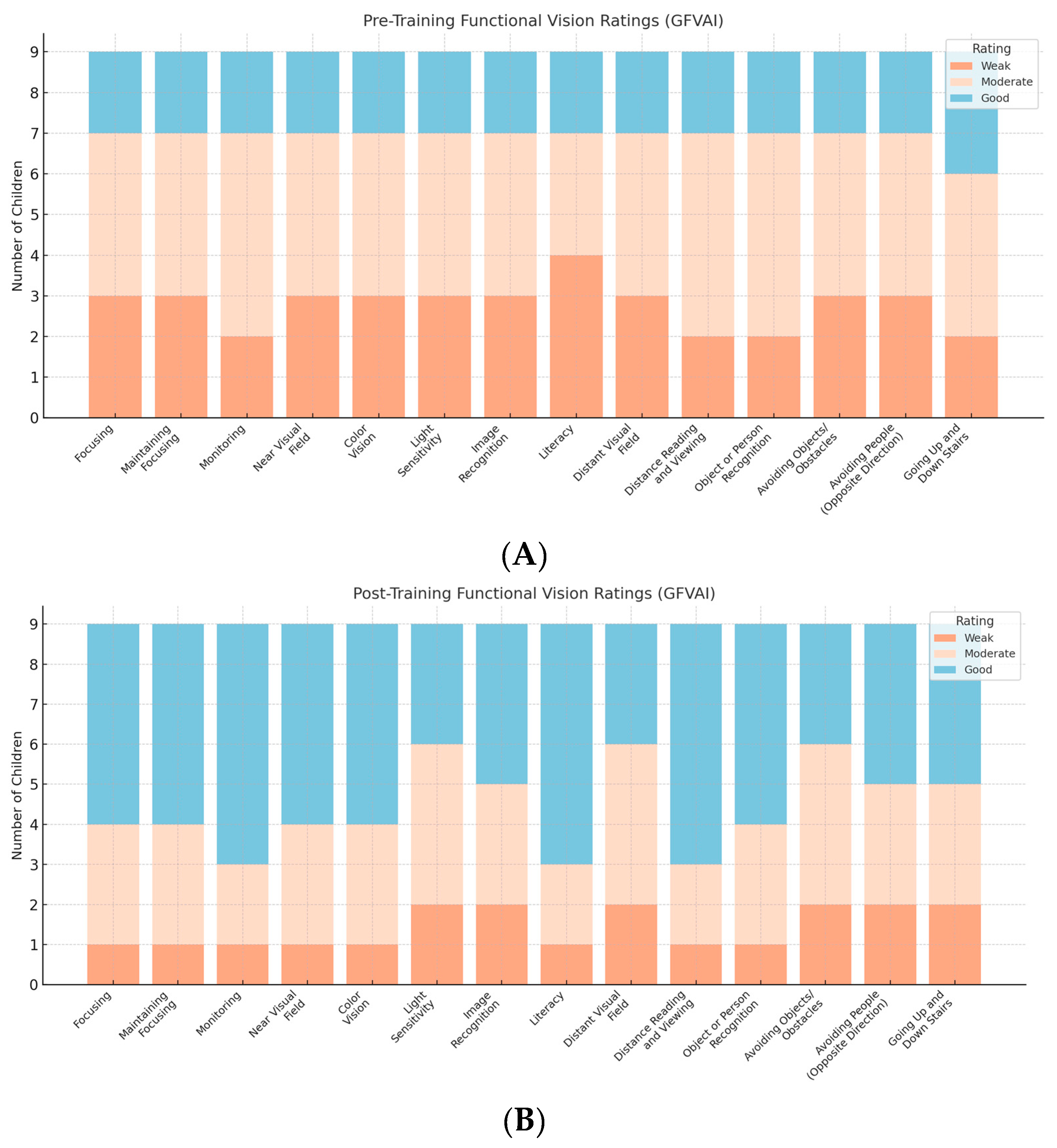
2.2.2. Gazi Functional Vision Assessment Instrument (GFVAI)
- Near Vision Skills (8 subdimensions): Focusing, Maintaining Focus (on single and two objects), Monitoring/Scanning, Color Vision, Light Sensitivity, Image Recognition, Near Visual Field, and Use of Writing Tools.
- Distance Vision Skills (6 subdimensions): Distance Visual Field (central, left, right), Distance Reading and Viewing, Object/Person Recognition, Avoiding Obstacles, Avoiding People, and Navigating Stairs.
2.2.3. Dynamic Occupational Therapy Cognitive Assessment for Children (DOTCA-Ch)
2.2.4. Motor-Free Visual Perception Test-Fourth Edition (MVPT-4)
2.3. Training Protocol
2.4. Analysis
3. Results
3.1. Quantitative Results
3.2. Qualitative Results
3.3. Effect Size and Power Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CRT | Cognitive Rehabilitation Therapy |
| CVI | Cerebral visual impairment |
| GFVAI | Gazi Functional Vision Assessment Instrument |
| DOTCA-Ch | Dynamic Occupational Therapy Cognitive Assessment for Children |
| MVPT-4 | Motor-Free Visual Perception Test-Fourth Edition (MVPT-4) |
Appendix A
Appendix A.1. Cognitive Rehabilitation Protocol for Children with Cerebral Visual Impairment

- (A)
- Training Program Structured According to the CRT Process
- Training on Cognitive Strengths and WeaknessesFollowing the individual evaluation of each child, the planned training program and its expected outcomes (such as improved attention, increased duration and amount of information remembered, better perception of visual stimuli, improved comprehension of verbal input, and enhanced reasoning when required to act) were explained to both the child and the family.
- Developing Underlying Cognitive Skills Through Practice or RetrainingActivities selected from the activity pool were matched to the child’s skill level and interests and designed to stimulate relevant cognitive domains. These activities helped strengthen fundamental skills and promote progress toward more advanced skills.
- Teaching External and Internal Compensatory StrategiesActivities selected from the pool were presented as games such as completing puzzles, remembering spoken information, or reconstructing structures. Initially, each game was explained, and the child was first asked to play alone, then with the therapist. By observing the therapist, the child could integrate new strategies with their own. After each game, discussions were held about why one side won and what the other could have done differently, emphasizing strategy development.
- Adapting Acquired Skills to Daily Life and Using Functional Activities to Improve Cognitive SkillsSessions were conducted in the child’s natural environments, such as home or school, with participation from peers and family. These sessions took place during the final one or few sessions of the program using functional activities from the activity pool. For example, for the “What should I do now?” activity, the session was held at the child’s school. The child, their teacher, and family were consulted. Real-life tasks the child struggled with were practiced, including focusing during class, copying from the board, visiting the canteen during breaks, making purchases, finding classrooms, and organizing belongings at the end of class. The therapist referred to previous activities: "We did this in the game—what should we do here now?" and guided the child to find the answer, providing prompts as needed.
- (B)
- According to MVF Parameters:
- Based on Stored and Usable Individual Characteristics:
- Based on Environmental Cues:
- Based on Visual Skills:
Appendix A.2. Activity Examples
- Random Words Activity to Improve Attention:
- Conducted in silent or distracting environments;
- Word frequency can vary (e.g., every 3–5 words for lower skill levels or every 8–10 for higher levels);
- A visual cue (e.g., a picture of a tree) may initially be provided and later removed;
- Played as a competitive game with the therapist to build strategies (e.g., “Who hears the most ‘tree’ words?”);
- Actions can range from simple (tapping) to complex (threading beads);
- Distractors can include unrelated categories (e.g., colors/shapes for lower levels, plant names for higher);
- Timing can be rhythmic (for lower attention) or arrhythmic (for higher levels);
- Complexity of the target word can be adjusted (e.g., “tree” for beginners, abstract or broader categories for advanced);
- Duration can range from 5 to 20 min based on attention span.
- Color Puzzle Activity for Visual Processing:
- Begin with two distinct color groups (e.g., red and blue for easier contrast, yellow and orange for harder);
- Progress to selecting one color among several;
- Advance to placing pieces in the correct locations;
- Puzzle pieces can be distributed across the child’s preferred, then wider, and finally full visual fields;
- The child may collect multiple pieces at once to promote wide visual scanning;
- Initially, time limits may not apply; later, completion within a set time is expected;
- Pieces can first be placed on plain backgrounds and later on striped ones to build visual discrimination.
- Memory Skill Training Using Color Puzzle:
- Practiced in quiet or noisy settings to study attention’s impact on memory;
- The number of images increases gradually;
- Images can be named immediately or recalled after all have been shown;
- Time intervals between viewing and recalling can be extended over time;
- A distractor task may follow image presentation (e.g., an obstacle course);
- Familiarity of images can be varied from everyday to abstract;
- The number and similarity of choices can increase with skill level;
- Memory tasks can progress to recalling not just objects but their color, size, context, and use.
- Direction-Following Activity for Information Processing:
- Varying grid size and complexity;
- Drawing a compass to aid lower-level processing;
- Reducing intervals between commands over time;
- Commands can be relative to the start point or previous box;
- Initially, directions are demonstrated; later, given verbally only;
- Distractions may be added in advanced stages.
- Word Grouping Activity for Executive Function:
- Terms may be familiar (low level) or unfamiliar (advanced);
- Categories may be hierarchical (e.g., “vehicles” split into “land/air”) or intersecting (e.g., “spinach” under both “green” and “edible”);
- The child is asked to suggest other items or categories;
- At higher levels, the child may create their own categorization system.
| Cognitive Domain | Example Activity | CRT Step | MVF Component Targeted | Adaptation Example |
|---|---|---|---|---|
| Attention | Random Word Task—The child listens to a sequence of spoken words and taps the table whenever a specific target word (e.g., “tree”) is heard. | Step 2 and 3 | Individual characteristics, visual skills | Modify word frequency, add background noise, or remove visual prompts. |
| Visual Processing | Color Puzzle—The child matches puzzle pieces by color, using a set of contrasting color options. | Step 2 and 3 | Environmental cues, visual skills | Start with high-contrast colors in a simple visual field, then progress to low-contrast and complex backgrounds. |
| Memory | Puzzle Recall—The child views colored shapes, then recalls and reconstructs them after a delay or distraction. | Step 2 | Individual characteristics | Increase the number of stimuli, delay intervals, or introduce interference tasks. |
| Information Processing | Directional Tracking Task—The child follows multi-step verbal commands on a grid (e.g., “Move two squares right”). | Step 2 and 3 | Individual characteristics, environmental cues | Adjust command complexity, timing, and visual supports (e.g., compass reference). |
| Executive Function | Word Grouping—The child categorizes object names (e.g., food, animals) and discusses alternative groupings. | Step 3 and 4 | All three MVF components | Add multi-layered or overlapping group rules, and ask the child to generate their own categories. |
References
- Ospina, L.H. Cortical Visual Impairment. Pediatr. Rev. 2009, 30, e81. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Causes of Blindness and Vision Impairment in 2020 and Trends over 30 Years, and Prevalence of Avoidable Blindness in Relation to VISION 2020. Lancet Glob. Health 2021, 9, e144–e160. [Google Scholar] [CrossRef] [PubMed]
- Dutton, G.; Bax, M. Visual Impairment in Children Due to Damage to the Brain: Clinics in Developmental Medicine; John Wiley & Sons: Hoboken, NJ, USA, 2010; Available online: https://www.wiley.com/en-us/Visual+Impairment+in+Children+due+to+Damage+to+the+Brain-p-9781898683865 (accessed on 9 April 2025).
- Roman-Lantzy, C. Cortical Visual Impairment: An Approach to Assessment and Intervention; American Foundation for the Blind, 2018. Available online: https://catalog.library.vanderbilt.edu/discovery/fulldisplay/alma991043720402203276/01VAN_INST:vanui (accessed on 9 April 2025).
- Aldrich, M.S.; Alessi, A.G.; Beck, R.W.; Gilman, S. Cortical Blindness: Etiology, Diagnosis, and Prognosis. Ann. Neurol. 1987, 21, 149–158. [Google Scholar] [CrossRef] [PubMed]
- Williams, J. CVI Is Permanent but Not Unchanging: Early Neuroplasticity and Cognitive Rehabilitation. Neurodev. Disabil. Rev. 2024, 18, 20–29. [Google Scholar] [CrossRef]
- Resnikoff, S.; Pascolini, D.; Etya’Ale, D.; Kocur, I.; Pararajasegaram, R.; Pokharel, G.P.; Mariotti, S.P. Global Data on Visual Impairment in the Year 2002. Bull. World Health Organ. 2004, 82, 844–851. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2623053/pdf/15640920.pdf (accessed on 9 April 2025).
- Corn, A.L.; Erin, J.N. Foundations of Low Vision: Clinical and Functional Perspectives; American Foundation for the Blind: New York, NY, USA, 2010; Available online: https://www.worldcat.org/title/foundations-of-low-vision-clinical-and-functional-perspectives/oclc/458583903 (accessed on 9 April 2025).
- Markowitz, S.N. Principles of Modern Low Vision Rehabilitation. Can. J. Ophthalmol. 2006, 41, 289–312. [Google Scholar] [CrossRef]
- Corn, A.L. Visual Function: A Theoretical Model for Individuals with Low Vision. J. Vis. Impair. Blind. 1983, 77, 373–377. [Google Scholar] [CrossRef]
- Fonteyn-Vinke, A.; Fakir, H.; Steendam, M.; Vervloed, M.P.J. Effects of a Guideline for Children with Cerebral Visual Impairment on the Daily Practices of Vision Habilitation and Rehabilitation Workers. Br. J. Vis. Impair. 2024, 43, 328–341. [Google Scholar] [CrossRef]
- Ostrovsky, Y.; Andalman, A.; Sinha, P. Vision Following Extended Congenital Blindness. Psychol. Sci. 2006, 17, 1009–1014. [Google Scholar] [CrossRef]
- Malkowicz, D.E.; Myers, G.; Leisman, G. Rehabilitation of Cortical Visual Impairment in Children. Int. J. Neurosci. 2006, 116, 1015–1033. [Google Scholar] [CrossRef]
- Reid, D.K.; Johnson, R.A.; Morreale, L. Cognitive Rehabilitation for Pediatric Brain Injury: A Review of the Literature. Pediatr. Rehabil. 2015, 18, 301–312. [Google Scholar] [CrossRef]
- Boivin, M.J.; Busman, R.A.; Parikh, S.M.; Bangirana, P.; Page, C.F.; Opoka, R.O.; Giordani, B. A pilot study of the neuropsychological benefits of computerized cognitive rehabilitation in Ugandan children with HIV. Neuropsychology 2010, 24, 667–673. [Google Scholar] [CrossRef] [PubMed]
- Galetto, V.; Sacco, K. Neuroplastic Changes Induced by Cognitive Rehabilitation in Traumatic Brain Injury: A Review. Neurorehabilit. Neural Repair 2017, 31, 800–813. [Google Scholar] [CrossRef]
- Malia, K.; Brannagan, A. How to Do Cognitive Rehabilitation Therapy: A Guide for All of Us; Brain Tree Training, 2005. Available online: https://www.worldcat.org/title/how-to-do-cognitive-rehabilitation-therapy-a-guide-for-all-of-us-part-two/oclc/1036222296 (accessed on 9 April 2025).
- Bergquist, T.F.; Malec, J.F. Psychology: Current Practice and Training Issues in Treatment of Cognitive Dysfunction. NeuroRehabilitation 1997, 8, 49–56. [Google Scholar] [CrossRef]
- Weden, K.M.; Barstow, E.A.; Oster, R.A.; DeCarlo, D.K. A Quantitative Assessment of Visual Function for Young and Medically Complex Children with Cerebral Visual Impairment: Development and Inter-Rater Reliability. medRxiv 2024, preprint. [Google Scholar] [CrossRef]
- Bennett, R.; Tibaudo, M.E.; Mazel, E.C.; Nai, Y. Implications of Cerebral/Cortical Visual Impairment on Life and Learning: Insights and Strategies from Lived Experiences. Front. Hum. Neurosci. 2025, 18, 1496153. [Google Scholar] [CrossRef]
- Waddington, J.; Hodgson, T. Review of Rehabilitation and Habilitation Strategies for Children and Young People with Homonymous Visual Field Loss Caused by Cerebral Vision Impairment. Br. J. Vis. Impair. 2017, 35, 197–210. [Google Scholar] [CrossRef]
- Çalık, B.B.; Kitiş, A.; Cavlak, U.; Oğuzhanoğlu, A. The Impact of Attention Training on Children with Low Vision: A Randomized Trial. Turk. J. Med. Sci. 2012, 42 (Suppl. 1), 1186–1193. [Google Scholar] [CrossRef]
- Morawietz, C.; Dumalski, N.; Wissmann, A.M.; Wecking, J.; Muehlbauer, T. Consistency of Spatial Ability Performance in Children, Adolescents, and Young Adults. Front. Psychol. 2024, 15, 1365941. [Google Scholar] [CrossRef]
- Şafak, P.; Çakmak, S.; Kaan, A.; O’dwyer, P.A. Gazi İşlevsel Görme Değerlendirme Aracı ile Az Gören Öğrencilerin Görme Becerilerinin Değerlendirilmesi; TUBITAK, Contract No.: 111K549. Available online: https://app.trdizin.gov.tr/proje/TVRRMk9ERXg/gazi-islevsel-gorme-degerlendirme-araci-ile-az-goren-ogrencilerin-gorme-becerilerinin-degerlendirilmesi (accessed on 9 April 2025).
- Safak, P.; Cakmak, S.; Karakoc, T.; O’Dwyer, P.A. Development of Gazi Functional Vision Assessment Instrument. Eur. J. Educ. Res. 2021, 10, 1973–1987. [Google Scholar] [CrossRef]
- Katz, N.; Golstand, S.; Bar-Ilan, R.T.; Parush, S. The Dynamic Occupational Therapy Cognitive Assessment for Children (DOTCA-Ch): A New Instrument for Assessing Learning Potential. Am. J. Occup. Ther. 2007, 61, 41–52. [Google Scholar] [CrossRef] [PubMed]
- Colarusso, R.; Hammill, D.D. MVPT-4: Motor-Free Visual Perception Test, 4th ed.; Academic Therapy Publications: Novato, CA, USA, 2015; Available online: https://www.academictherapy.com/detailATP.tpl?eqskudatarq=8962-9 (accessed on 9 April 2025).
- IBM Corp. IBM SPSS Statistics for Windows, Version 23.0; IBM Corp.: Armonk, NY, USA, 2015. [Google Scholar]
- Kang, H. Sample Size Determination and Power Analysis Using the G*Power Software. J. Educ. Eval. Health Prof. 2021, 18, 17. [Google Scholar] [CrossRef] [PubMed]
- OpenAI. ChatGPT (Version 4) [Large Language Model]. 2024. Available online: https://chat.openai.com (accessed on 21 May 2025).
- Waddington, J.; Ellis, R. Retrospective Investigation of Improvements in Functional Vision for Adolescent Students with Cerebral Vision Impairments. Br. J. Vis. Impair. 2024. [CrossRef]
- Ganesh, S.; Sethi, S.; Srivastav, S.; Chaudhary, A.; Arora, P. Impact of Low Vision Rehabilitation on Functional Vision Performance of Children with Visual Impairment. Oman J. Ophthalmol. 2013, 6, 170–174. [Google Scholar] [CrossRef]
- Graham, H.K.; Rosenbaum, P.; Paneth, N.; Dan, B.; Lin, J.P.; Damiano, D.L.; Becher, J.G.; Gaebler-Spira, D.; Colver, A.; Reddihough, D.S.; et al. Cerebral Palsy. Nat. Rev. Dis. Primers 2016, 2, 15082. [Google Scholar] [CrossRef]
- Novak, I.; Morgan, C.; Fahey, M.; Finch-Edmondson, M.; Galea, C.; Hines, A.; Langdon, K.; Badawi, N. State of the Evidence Traffic Lights 2019: Systematic Review of Interventions for Preventing and Treating Children with Cerebral Palsy. Curr. Neurol. Neurosci. Rep. 2019, 19, 92. [Google Scholar] [CrossRef]
- Korsunskaya, L.L.; Ageeva, E.S.; Larina, N.V. The Role of Neurotrophic Factors during Rehabilitation Therapy in Patients with Cerebral Palsy. Ross. Nevrol. Zh. 2025, 29, 23–30. [Google Scholar] [CrossRef]
- Collart, L.; Ortibus, E.; Ben Itzhak, N. Health-Related Quality of Life and Its Relation with Functional Vision in Children with Cerebral Visual Impairment. Res. Dev. Disabil. 2024, 154, 104861. [Google Scholar] [CrossRef]
- Çakmak, S.; Karakoç, T.; Şafak, P. Comparing Functional Vision Skills of Students with Low Vision in Schools for the Visually Impaired and Inclusive Classrooms. Educ. Sci. 2016, 41, 165–179. [Google Scholar] [CrossRef]
- Grbović, A.; Stanimirov, K. Learning Mediums for Children with Visual Impairment. Teme 2013, 37, 769–783. Available online: https://scindeks.ceon.rs/article.aspx?artid=0353-79191302769G (accessed on 9 April 2025).
- Aki, E.; Atasavun, S.; Turan, A.; Kayihan, H. Training Motor Skills of Children with Low Vision. Percept. Mot. Ski. 2007, 104 (Suppl. 3), 1328–1336. [Google Scholar] [CrossRef] [PubMed]
- Janssen, M.J.; Hulsbosch, M. Visual Assessment Scale for CVI in Children with Profound Intellectual and Multiple Disabilities (CVI-PIMD); Royal Dutch Visio: Amsterdam, The Netherlands, 2017; Available online: https://www.visio.org/media/gojky4v2/tg_uk_handleiding-vas-cvi-zevmb_digitaal_def.pdf (accessed on 21 May 2025).
| ID | Age | Gender | Diagnosis | Optical Aid | Medical History | Family History | Medication | Educational Placement | School Grade |
|---|---|---|---|---|---|---|---|---|---|
| P1 | 7 | Male | CVI, Color Blindness, Photophobia | Glasses | No | No | No | Inclusive Mainstream Classroom | 2nd |
| P2 | 10 | Male | CVI | Glasses | No | No | No | Inclusive Mainstream Classroom | 3rd |
| P3 | 9 | Male | CP CVI | Glasses | Spasticity operation | Yes | Yes | Inclusive Mainstream Classroom | 4th |
| P4 | 11 | Male | CVI | None | No | No | No | Inclusive Mainstream Classroom | 5th |
| P5 | 7 | Female | CVI | Glasses | No | No | Yes | Special Ed in Mainstream School | 5th |
| P6 | 11 | Female | CVI | None | No | No | Yes | Special Ed in Mainstream School | 5th |
| P7 | 11 | Male | CP, CVI, Epilepsy Nystagmus | None | No | No | Yes | School for the Visually Impaired | 6th |
| P8 | 11 | Female | CVI, Epilepsy Nystagmus | None | No | No | Yes | School for the Visually Impaired | 6th |
| P9 | 10 | Female | CVI | Telescopic Glasses | No | No | Yes | School for the Visually Impaired | 6th |
| Skill | Pre-Training X ± SD | Post-Training X ± SD | z | p |
|---|---|---|---|---|
| GRVAI-Near Vision Skills | ||||
| Focusing | 25.1 ± 8.1 | 36.0 ± 6.0 | −2.410 | 0.016 * |
| Maintaining Focusing | 19.3 ± 8.1 | 28.7 ± 4.0 | −2.371 | 0.018 * |
| Monitoring | 36.9 ± 19.2 | 54.7 ± 11.1 | −2.201 | 0.028 * |
| Near Visual Field | 12.0 ± 3.3 | 16.1 ± 0.8 | −2.555 | 0.011 * |
| Color Vision * | 42.0 ± 14.0 | 54.2 ± 10.2 | −2.366 | 0.018 * |
| Light Sensitivity * | 1.0 ± 0.0 | 3.0 ± 0.0 | −3.000 | 0.003 ** |
| Image recognition | 1.8 ± 0.4 | 2.8 ± 0.4 | −2.714 | 0.007 ** |
| Literacy | 2.1 ± 0.8 | 2.3 ± 0.7 | −1.414 | 0.157 |
| GRVAI-Distant Vision Skills | ||||
| Distant Visual Field | 19.7 ± 6.00 | 36.4 ± 5.5 | −2.670 | 0.008 ** |
| Distance Reading and Viewing | 1.4 ± 0.7 | 2.1 ± 0.6 | −2.449 | 0.014 |
| Object or Person Recognition | 1.8 ± 0.7 | 2.2 ± 0.7 | −1.633 | 0.102 |
| Avoiding Objects/Obstacles | 1.7 ± 0.5 | 2.4 ± 0.5 | −2.333 | 0.020 * |
| Avoiding people from the opposite direction | 1.6 ± 0.5 | 2.3 ± 0.5 | −2.333 | 0.020 * |
| Going Up and Down Stairs | 1.8 ± 0.4 | 2.7 ± 0.7 | −2.530 | 0.011 * |
| DOTC-Ch | ||||
| Orientation | 5.5 ± 5.2 | 8.1 ± 4.6 | −2.388 | 0.017 * |
| Spatial Perception | 6.9 ± 2.2 | 10.7 ± 2.0 | −2.539 | 0.011 * |
| Praxis | 12.9 ± 8.3 | 25.6 ± 12.3 | −2.666 | 0.008 ** |
| Visual Motor Organization | 9.8 ± 2.9 | 21.3 ± 6.4 | −2.668 | 0.008 ** |
| Thinking Processes | 12.6 ± 5.7 | 24.7 ± 6.7 | −2.684 | 0.007 ** |
| MVPT-4 | ||||
| Visual perception | 14.9 ± 5.7 | 23.0 ± 6.1 | −2.675 | 0.007 ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Celik Turan, Z.; Aki, E. Cognitive Rehabilitation Improves Functional Vision Skills in Children with Cerebral Visual Impairment. Brain Sci. 2025, 15, 590. https://doi.org/10.3390/brainsci15060590
Celik Turan Z, Aki E. Cognitive Rehabilitation Improves Functional Vision Skills in Children with Cerebral Visual Impairment. Brain Sciences. 2025; 15(6):590. https://doi.org/10.3390/brainsci15060590
Chicago/Turabian StyleCelik Turan, Zeynep, and Esra Aki. 2025. "Cognitive Rehabilitation Improves Functional Vision Skills in Children with Cerebral Visual Impairment" Brain Sciences 15, no. 6: 590. https://doi.org/10.3390/brainsci15060590
APA StyleCelik Turan, Z., & Aki, E. (2025). Cognitive Rehabilitation Improves Functional Vision Skills in Children with Cerebral Visual Impairment. Brain Sciences, 15(6), 590. https://doi.org/10.3390/brainsci15060590






