Cerebral Cortex Activation and Gait Performance between Healthy and Prefrail Older Adults during Cognitive and Walking Tasks
Abstract
1. Introduction
2. Material and Methods
2.1. Participants
2.2. Clinical Measurements
2.3. The 2-Back Task
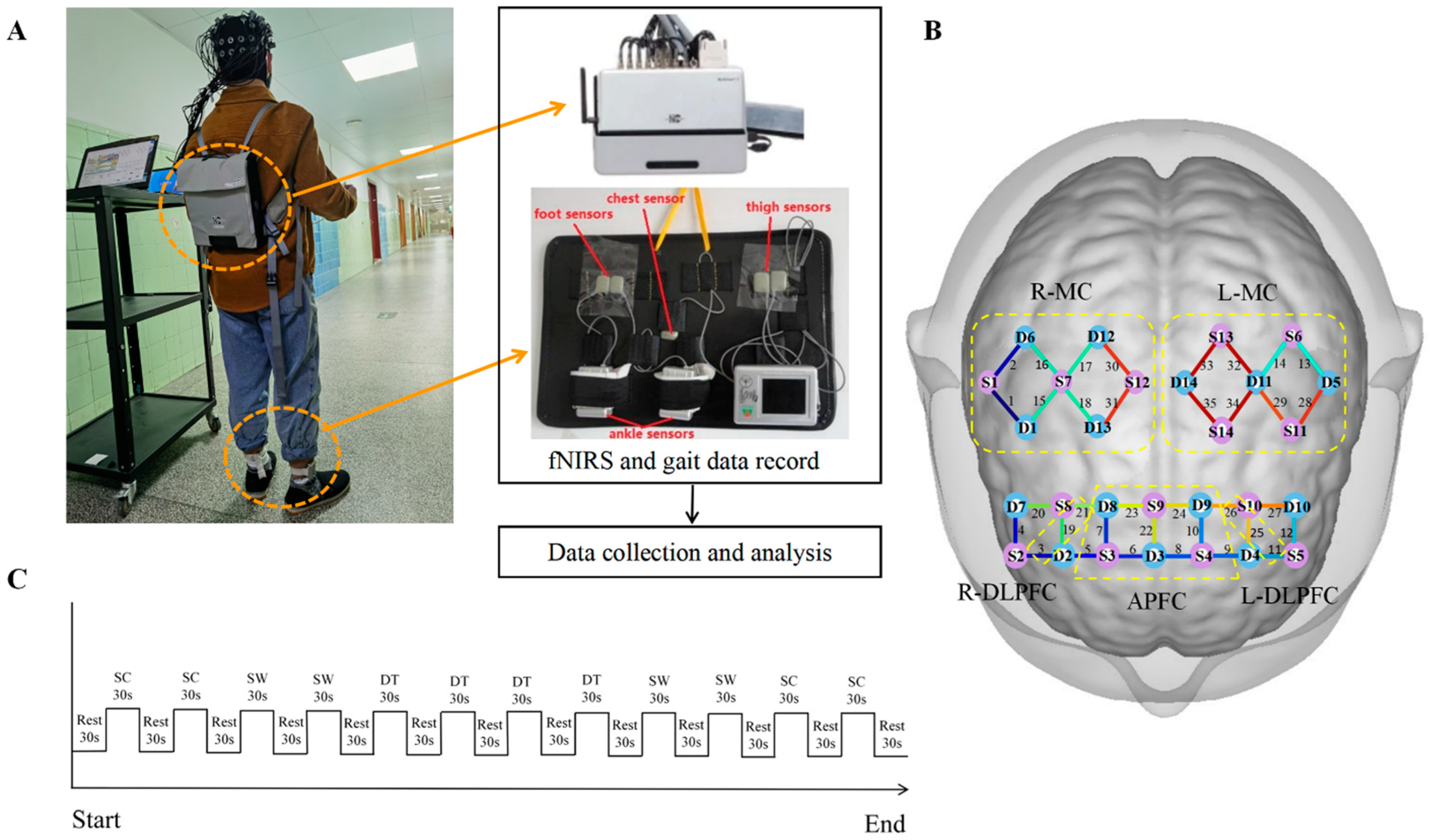
2.4. fNIRS Measurements and Data Processing
2.5. Gait Measurements
2.6. Procedures
2.7. Statistical Analysis
3. Results
3.1. Participants’ Characteristics
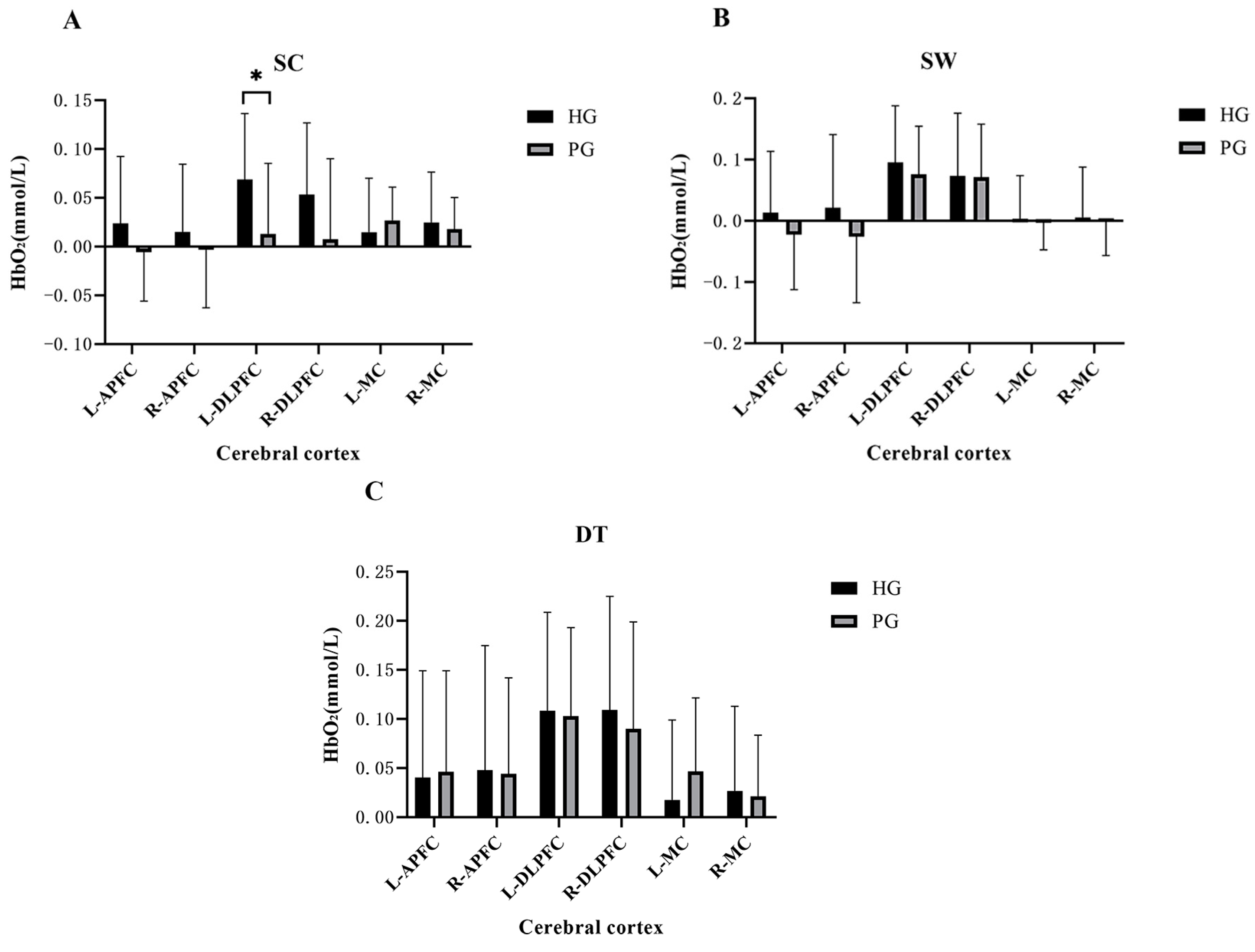
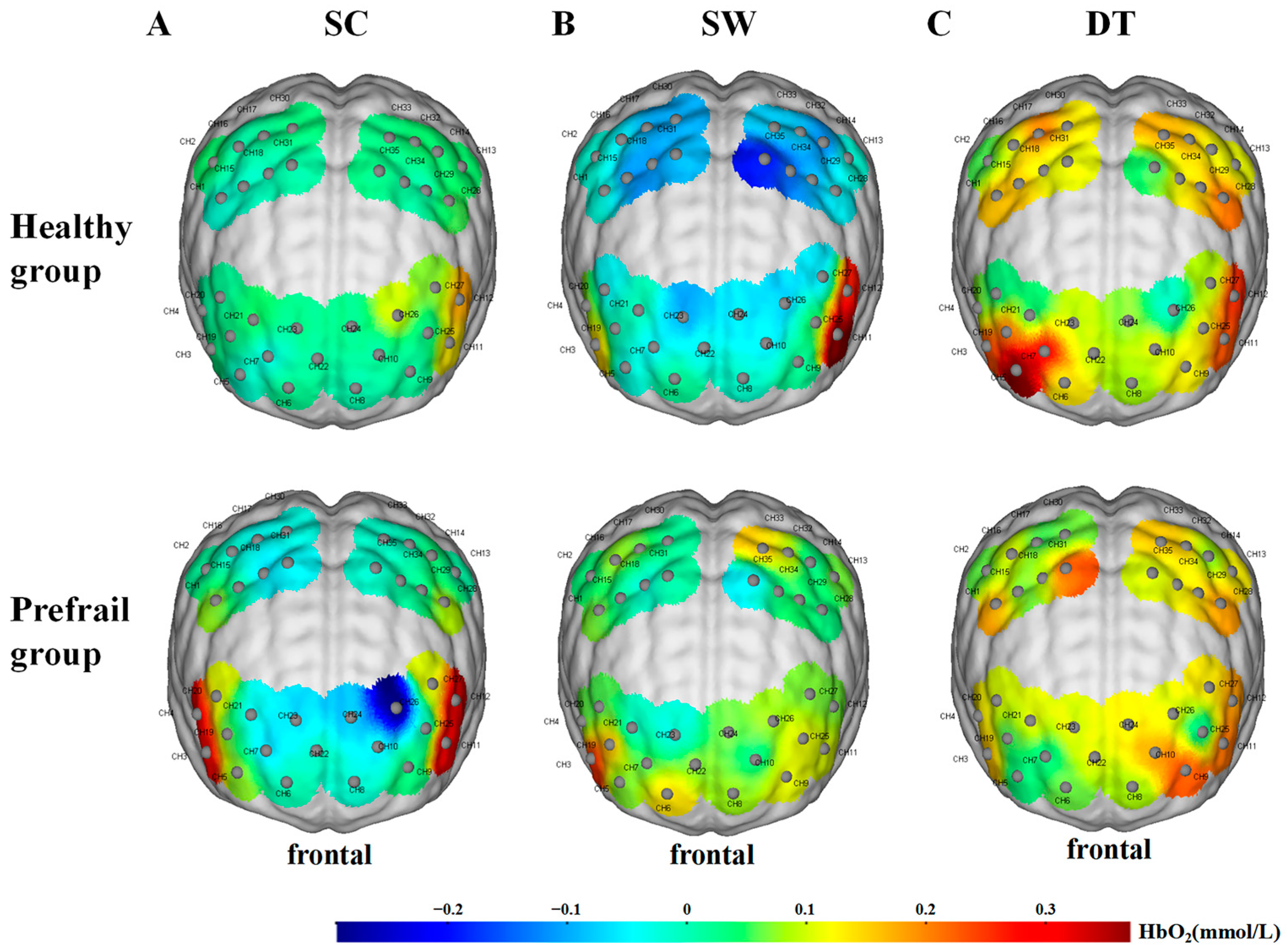
3.2. Cerebral Cortex Activation
3.3. The 2-Back Task Performance
3.4. Gait Performance
3.5. Association between Measured Cerebral Cortex Oxygenation and Gait Parameters
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Xue, Q.L. The frailty syndrome: Definition and natural history. Clin. Geriatr. Med. 2011, 27, 1–15. [Google Scholar] [CrossRef] [PubMed]
- He, B.; Ma, Y.; Wang, C.; Jiang, M.; Geng, C.; Chang, X.; Ma, B.; Han, L. Prevalence and Risk Factors for Frailty among Community-Dwelling Older People in China: A Systematic Review and Meta-Analysis. J. Nutr. Health Aging 2019, 23, 442–450. [Google Scholar] [CrossRef] [PubMed]
- Walston, J.; Hadley, E.C.; Ferrucci, L.; Guralnik, J.M.; Newman, A.B.; Studenski, S.A.; Ershler, W.B.; Harris, T.; Fried, L.P. Research agenda for frailty in older adults: Toward a better understanding of physiology and etiology: Summary from the American Geriatrics Society/National Institute on Aging Research Conference on Frailty in Older Adults. J. Am. Geriatr. Soc. 2006, 54, 991–1001. [Google Scholar] [CrossRef] [PubMed]
- O’Caoimh, R.; Sezgin, D.; O’Donovan, M.R.; Molloy, D.W.; Clegg, A.; Rockwood, K.; Liew, A. Prevalence of frailty in 62 countries across the world: A systematic review and meta-analysis of population-level studies. Age Ageing 2021, 50, 96–104. [Google Scholar] [CrossRef] [PubMed]
- Sezgin, D.; Liew, A.; O’Donovan, M.R.; O’Caoimh, R. Pre-frailty as a multi-dimensional construct: A systematic review of definitions in the scientific literature. Geriatr. Nurs. 2020, 41, 139–146. [Google Scholar] [CrossRef]
- Puts, M.T.E.; Toubasi, S.; Andrew, M.K.; Ashe, M.C.; Ploeg, J.; Atkinson, E.; Ayala, A.P.; Roy, A.; Rodriguez Monforte, M.; Bergman, H.; et al. Interventions to prevent or reduce the level of frailty in community-dwelling older adults: A scoping review of the literature and international policies. Age Ageing 2017, 46, 383–392. [Google Scholar] [CrossRef]
- Dent, E.; Morley, J.E.; Cruz-Jentoft, A.J.; Woodhouse, L.; Rodriguez-Manas, L.; Fried, L.P.; Woo, J.; Aprahamian, I.; Sanford, A.; Lundy, J.; et al. Physical Frailty: ICFSR International Clinical Practice Guidelines for Identification and Management. J. Nutr. Health Aging 2019, 23, 771–787. [Google Scholar] [CrossRef]
- Hanlon, P.; Nicholl, B.I.; Jani, B.D.; Lee, D.; McQueenie, R.; Mair, F.S. Frailty and pre-frailty in middle-aged and older adults and its association with multimorbidity and mortality: A prospective analysis of 493 737 UK Biobank participants. Lancet Public Health 2018, 3, e323–e332. [Google Scholar] [CrossRef]
- Nikolin, S.; Tan, Y.Y.; Schwaab, A.; Moffa, A.; Loo, C.K.; Martin, D. An investigation of working memory deficits in depression using the n-back task: A systematic review and meta-analysis. J. Affect. Disord. 2021, 284, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.H.; Liu, L.K.; Chen, W.T.; Lee, W.J.; Peng, L.N.; Wang, P.N.; Chen, L.K. Cognitive Function in Individuals With Physical Frailty but Without Dementia or Cognitive Complaints: Results From the I-Lan Longitudinal Aging Study. J. Am. Med. Dir. Assoc. 2015, 16, 899.e9–899.e16. [Google Scholar] [CrossRef]
- Bortone, I.; Sardone, R.; Lampignano, L.; Castellana, F.; Zupo, R.; Lozupone, M.; Moretti, B.; Giannelli, G.; Panza, F. How gait influences frailty models and health-related outcomes in clinical-based and population-based studies: A systematic review. J. Cachexia Sarcopenia Muscle 2021, 12, 274–297. [Google Scholar] [CrossRef] [PubMed]
- Wollesen, B.; Wanstrath, M.; van Schooten, K.S.; Delbaere, K. A taxonomy of cognitive tasks to evaluate cognitive-motor interference on spatiotemoporal gait parameters in older people: A systematic review and meta-analysis. Eur. Rev. Aging Phys. Act. 2019, 16, 12. [Google Scholar] [CrossRef] [PubMed]
- Cheng, S.J.; Hsu, W.C.; Yang, Y.R.; Liu, Y.C.; Kuo, H.T.; Wang, R.Y. Gait Performance and Brain Activities during Cognitive and Motor Dual Task in Prefrail Elderly. Int. J. Gerontol. 2021, 15, 53–57. [Google Scholar] [CrossRef]
- Noguchi-Shinohara, M.; Ono, K.; Yuki-Nozaki, S.; Iwasa, K.; Yokogawa, M.; Komai, K.; Thyreau, B.; Tatewaki, Y.; Taki, Y.; Shibata, M.; et al. Association of the prefrailty with global brain atrophy and white matter lesions among cognitively unimpaired older adults: The Nakajima study. Sci. Rep. 2022, 12, 12129. [Google Scholar] [CrossRef]
- Del Brutto, O.H.; Mera, R.M.; Cagino, K.; Fanning, K.D.; Milla-Martinez, M.F.; Nieves, J.L.; Zambrano, M.; Sedler, M.J. Neuroimaging signatures of frailty: A population-based study in community-dwelling older adults (the Atahualpa Project). Geriatr. Gerontol. Int. 2017, 17, 270–276. [Google Scholar] [CrossRef]
- Lu, W.H.; de Souto Barreto, P.; Rolland, Y.; Rodriguez-Manas, L.; Bouyahia, A.; Fischer, C.; Mangin, J.F.; Giudici, K.V.; Vellas, B.; Group, M.D. Cross-sectional and prospective associations between cerebral cortical thickness and frailty in older adults. Exp. Gerontol. 2020, 139, 111018. [Google Scholar] [CrossRef]
- Ferrari, M.; Quaresima, V. A brief review on the history of human functional near-infrared spectroscopy (fNIRS) development and fields of application. Neuroimage 2012, 63, 921–935. [Google Scholar] [CrossRef] [PubMed]
- Soekadar, S.R.; Kohl, S.H.; Mihara, M.; von Luhmann, A. Optical brain imaging and its application to neurofeedback. Neuroimage Clin. 2021, 30, 102577. [Google Scholar] [CrossRef]
- Yeung, M.K.; Chan, A.S. A Systematic Review of the Application of Functional Near-Infrared Spectroscopy to the Study of Cerebral Hemodynamics in Healthy Aging. Neuropsychol. Rev. 2021, 31, 139–166. [Google Scholar] [CrossRef]
- Udina, C.; Avtzi, S.; Durduran, T.; Holtzer, R.; Rosso, A.L.; Castellano-Tejedor, C.; Perez, L.M.; Soto-Bagaria, L.; Inzitari, M. Functional Near-Infrared Spectroscopy to Study Cerebral Hemodynamics in Older Adults During Cognitive and Motor Tasks: A Review. Front. Aging Neurosci. 2019, 11, 367. [Google Scholar] [CrossRef]
- Holtzer, R.; Epstein, N.; Mahoney, J.R.; Izzetoglu, M.; Blumen, H.M. Neuroimaging of mobility in aging: A targeted review. J. Gerontol. A Biol. Sci. Med. Sci. 2014, 69, 1375–1388. [Google Scholar] [CrossRef]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef] [PubMed]
- Nasreddine, Z.S.; Phillips, N.A.; Bedirian, V.; Charbonneau, S.; Whitehead, V.; Collin, I.; Cummings, J.L.; Chertkow, H. The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. J. Am. Geriatr. Soc. 2005, 53, 695–699. [Google Scholar] [CrossRef]
- Boey, K.W. Cross-validation of a short form of the CES-D in Chinese elderly. Int. J. Geriatr. Psychiatry 1999, 14, 608–617. [Google Scholar] [CrossRef]
- Podsiadlo, D.; Richardson, S. The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [CrossRef] [PubMed]
- Macfarlane, D.J.; Lee, C.C.; Ho, E.Y.; Chan, K.L.; Chan, D.T. Reliability and validity of the Chinese version of IPAQ (short, last 7 days). J. Sci. Med. Sport 2007, 10, 45–51. [Google Scholar] [CrossRef]
- Huang, L.; Liu, Y.; Lin, T.; Hou, L.; Song, Q.; Ge, N.; Yue, J. Reliability and validity of two hand dynamometers when used by community-dwelling adults aged over 50 years. BMC Geriatr. 2022, 22, 580. [Google Scholar] [CrossRef]
- Maruya, K.; Arai, T.; Fujita, H. Brain Activity in the Prefrontal Cortex during Cognitive Tasks and Dual Tasks in Community-Dwelling Elderly People with Pre-Frailty: A Pilot Study for Early Detection of Cognitive Decline. Healthcare 2021, 9, 1250. [Google Scholar] [CrossRef]
- Rossi, C.; Roemmich, R.T.; Schweighofer, N.; Bastian, A.J.; Leech, K.A. Younger and Late Middle-Aged Adults Exhibit Different Patterns of Cognitive-Motor Interference During Locomotor Adaptation, With No Disruption of Savings. Front. Aging Neurosci. 2021, 13, 729284. [Google Scholar] [CrossRef]
- Shigeta, T.T.; Leahy, A.A.; Smith, J.J.; Eather, N.; Lubans, D.R.; Hillman, C.H. Cardiorespiratory and muscular fitness associations with older adolescent cognitive control. J. Sport Health Sci. 2021, 10, 82–90. [Google Scholar] [CrossRef]
- Bopp, K.L.; Verhaeghen, P. Aging and n-Back Performance: A Meta-Analysis. J. Gerontol. B Psychol. Sci. Soc. Sci. 2020, 75, 229–240. [Google Scholar] [CrossRef]
- Zhou, C.; Cheng, X.; Liu, C.; Li, P. Interpersonal coordination enhances brain-to-brain synchronization and influences responsibility attribution and reward allocation in social cooperation. Neuroimage 2022, 252, 119028. [Google Scholar] [CrossRef]
- Lin, C.C.; Bair, W.N.; Willson, J. Age differences in brain activity in dorsolateral prefrontal cortex and supplementary motor areas during three different walking speed tasks. Hum. Mov. Sci. 2022, 85, 102982. [Google Scholar] [CrossRef]
- Miyai, I.; Tanabe, H.C.; Sase, I.; Eda, H.; Oda, I.; Konishi, I.; Tsunazawa, Y.; Suzuki, T.; Yanagida, T.; Kubota, K. Cortical mapping of gait in humans: A near-infrared spectroscopic topography study. Neuroimage 2001, 14, 1186–1192. [Google Scholar] [CrossRef]
- Suzuki, M.; Miyai, I.; Ono, T.; Kubota, K. Activities in the frontal cortex and gait performance are modulated by preparation. An fNIRS study. Neuroimage 2008, 39, 600–607. [Google Scholar] [CrossRef]
- Scholkmann, F.; Spichtig, S.; Muehlemann, T.; Wolf, M. How to detect and reduce movement artifacts in near-infrared imaging using moving standard deviation and spline interpolation. Physiol. Meas. 2010, 31, 649–662. [Google Scholar] [CrossRef]
- Herold, F.; Wiegel, P.; Scholkmann, F.; Muller, N.G. Applications of Functional Near-Infrared Spectroscopy (fNIRS) Neuroimaging in Exercise–Cognition Science: A Systematic, Methodology-Focused Review. J. Clin. Med. 2018, 7, 466. [Google Scholar] [CrossRef]
- Maffiuletti, N.A.; Gorelick, M.; Kramers-de Quervain, I.; Bizzini, M.; Munzinger, J.P.; Tomasetti, S.; Stacoff, A. Concurrent validity and intrasession reliability of the IDEEA accelerometry system for the quantification of spatiotemporal gait parameters. Gait Posture 2008, 27, 160–163. [Google Scholar] [CrossRef]
- Marsh, A.P.; Vance, R.M.; Frederick, T.L.; Hesselmann, S.A.; Rejeski, W.J. Objective assessment of activity in older adults at risk for mobility disability. Med. Sci. Sport. Exerc. 2007, 39, 1020–1026. [Google Scholar] [CrossRef]
- Montero-Odasso, M.; Muir, S.W.; Hall, M.; Doherty, T.J.; Kloseck, M.; Beauchet, O.; Speechley, M. Gait variability is associated with frailty in community-dwelling older adults. J. Gerontol. A Biol. Sci. Med. Sci. 2011, 66, 568–576. [Google Scholar] [CrossRef]
- Holtzer, R.; Ross, D.; Izzetoglu, M. Intraindividual variability in neural activity in the prefrontal cortex during active walking in older adults. Psychol. Aging 2020, 35, 1201–1214. [Google Scholar] [CrossRef]
- Talamonti, D.; Vincent, T.; Fraser, S.; Nigam, A.; Lesage, F.; Bherer, L. The Benefits of Physical Activity in Individuals with Cardiovascular Risk Factors: A Longitudinal Investigation Using fNIRS and Dual-Task Walking. J. Clin. Med. 2021, 10, 579. [Google Scholar] [CrossRef]
- Doumas, M.; Rapp, M.A.; Krampe, R.T. Working memory and postural control: Adult age differences in potential for improvement, task priority, and dual tasking. J. Gerontol. B Psychol. Sci. Soc. Sci. 2009, 64, 193–201. [Google Scholar] [CrossRef]
- Kant, I.M.J.; de Bresser, J.; van Montfort, S.J.T.; Aarts, E.; Verlaan, J.J.; Zacharias, N.; Winterer, G.; Spies, C.; Slooter, A.J.C.; Hendrikse, J.; et al. The association between brain volume, cortical brain infarcts, and physical frailty. Neurobiol. Aging 2018, 70, 247–253. [Google Scholar] [CrossRef]
- Sui, S.X.; Hendy, A.M.; Teo, W.P.; Moran, J.T.; Nuzum, N.D.; Pasco, J.A. A Review of the Measurement of the Neurology of Gait in Cognitive Dysfunction or Dementia, Focusing on the Application of fNIRS during Dual-Task Gait Assessment. Brain Sci. 2022, 12, 968. [Google Scholar] [CrossRef]
- Cabeza, R. Hemispheric asymmetry reduction in older adults: The HAROLD model. Psychol. Aging 2002, 17, 85–100. [Google Scholar] [CrossRef]
- Yeung, M.K.; Lee, T.L.; Chan, A.S. Depressive and anxiety symptoms are related to decreased lateral prefrontal cortex functioning during cognitive control in older people. Biol. Psychol. 2021, 166, 108224. [Google Scholar] [CrossRef]
- Lu, C.F.; Liu, Y.C.; Yang, Y.R.; Wu, Y.T.; Wang, R.Y. Maintaining Gait Performance by Cortical Activation during Dual-Task Interference: A Functional Near-Infrared Spectroscopy Study. PLoS ONE 2015, 10, e0129390. [Google Scholar] [CrossRef]
- Koch, S.B.J.; Mars, R.B.; Toni, I.; Roelofs, K. Emotional control, reappraised. Neurosci. Biobehav. Rev. 2018, 95, 528–534. [Google Scholar] [CrossRef]
- Takayanagi, N.; Sudo, M.; Yamashiro, Y.; Chiba, I.; Lee, S.; Niki, Y.; Shimada, H. Screening prefrailty in Japanese community-dwelling older adults with daily gait speed and number of steps via tri-axial accelerometers. Sci. Rep. 2021, 11, 18673. [Google Scholar] [CrossRef]
- Schwenk, M.; Mohler, J.; Wendel, C.; D’Huyvetter, K.; Fain, M.; Taylor-Piliae, R.; Najafi, B. Wearable sensor-based in-home assessment of gait, balance, and physical activity for discrimination of frailty status: Baseline results of the Arizona frailty cohort study. Gerontology 2015, 61, 258–267. [Google Scholar] [CrossRef]
- Matsushita, E.; Okada, K.; Ito, Y.; Satake, S.; Shiraishi, N.; Hirose, T.; Kuzuya, M. Characteristics of physical prefrailty among Japanese healthy older adults. Geriatr. Gerontol. Int. 2017, 17, 1568–1574. [Google Scholar] [CrossRef]
- Savva, G.M.; Donoghue, O.A.; Horgan, F.; O’Regan, C.; Cronin, H.; Kenny, R.A. Using timed up-and-go to identify frail members of the older population. J. Gerontol. A Biol. Sci. Med. Sci. 2013, 68, 441–446. [Google Scholar] [CrossRef]
- Verghese, J.; Holtzer, R.; Lipton, R.B.; Wang, C. Quantitative gait markers and incident fall risk in older adults. J. Gerontol. A Biol. Sci. Med. Sci. 2009, 64, 896–901. [Google Scholar] [CrossRef]
- Schwenk, M.; Howe, C.; Saleh, A.; Mohler, J.; Grewal, G.; Armstrong, D.; Najafi, B. Frailty and technology: A systematic review of gait analysis in those with frailty. Gerontology 2014, 60, 79–89. [Google Scholar] [CrossRef]
- Robertson, D.A.; Savva, G.M.; Coen, R.F.; Kenny, R.A. Cognitive function in the prefrailty and frailty syndrome. J. Am. Geriatr. Soc. 2014, 62, 2118–2124. [Google Scholar] [CrossRef]
- Tian, Q.; Chastan, N.; Bair, W.N.; Resnick, S.M.; Ferrucci, L.; Studenski, S.A. The brain map of gait variability in aging, cognitive impairment and dementia-A systematic review. Neurosci. Biobehav. Rev. 2017, 74, 149–162. [Google Scholar] [CrossRef]

| Characteristics of Frailty | Specific Embodiment |
|---|---|
| 1. Unintentional weight loss | At least 5% or more than 10 pounds of the previous year’s body weight |
| 2. Exhaustion | Self-report in Epidemiological Studies Depression Scale |
| 3. Low grip strength | Males: |
| BMI ≤ 24 kg/m2, ≤29 kg; BMI 24.1–26 kg/m2, ≤30 kg; | |
| BMI 26.1–28 kg/m2, ≤30 kg; BMI > 28 kg/m2, ≤32 kg. | |
| Females: | |
| BMI ≤ 23 kg/m2, ≤17 kg; BMI 23.1–26 kg/m2, ≤17.3 kg; | |
| BMI 26.1–29 kg/m2, ≤18 kg; BMI > 29 kg/m2, ≤21 kg. | |
| 4. Slow pace | Males: height ≤ 173 cm, ≥7 s; height > 173 cm, ≥6 s |
| Females: height ≤ 159 cm, ≥7 s; height > 159 cm, ≥6 s | |
| 5. Low physical activity | Males: <383 Kcals per week |
| Females: <270 Kcals per week |
| Variable | HG (N = 21) | PG (N = 15) | p-Value |
|---|---|---|---|
| Gender (female/all) | 12/21 | 8/15 | 1.000 |
| Age (years) | 65.95 ± 3.81 | 67.93 ± 3.96 | 0.139 |
| Body weight (kg) | 62.67 ± 9.28 | 62.20 ± 6.12 | 0.866 |
| Body height (cm) | 160.95 ± 8.00 | 161.53 ± 6.88 | 0.822 |
| BMI (kg/m2) | 24.14 ± 2.67 | 23.89 ± 2.48 | 0.778 |
| Years of education (years) | 12.57 ± 2.56 | 11.60 ± 2.97 | 0.266 |
| HGS (kg) | 28.04 ± 6.14 | 25.15 ± 5.26 | 0.116 |
| MoCA (maximum = 30) | 27.14 ± 2.20 | 26.73 ± 1.39 | 0.529 |
| CESD-10 (maximum = 30) | 2.86 ± 2.65 | 3.27 ± 2.74 | 0.525 |
| TUG (s) | 9.25 ± 1.00 | 10.20 ± 1.03 | 0.010 |
| IPAQ-SF (MET-min/week) | 1242.90 ± 713.37 | 1026.93 ± 842.73 | 0.216 |
| Frailty characteristics (number of participants) | |||
| Unintentional body weight loss | / | 2 | / |
| Exhaustion | / | 0 | / |
| Low physical activity | / | 6 | / |
| Slow pace | / | 6 | / |
| Reduced grip strength | / | 3 | / |
| Variable | SC | F | p | DT | F | p | ||
|---|---|---|---|---|---|---|---|---|
| HG (N = 21) | PG (N = 15) | HG (N = 21) | PG (N = 15) | |||||
| Accuracy (%) | 64.88 ± 20.14 | 59.16 ± 16.18 | 0.826 | 0.261 | 57.27 ± 12.87 | 54.44 ± 15.61 | 0.354 | 0.556 |
| Reaction time (ms) | 1050.47 ± 144.48 | 1082.36 ± 133.69 | 0.453 | 0.505 | 1067.02 ± 124.45 | 1044.08 ± 159.72 | 0.235 | 0.987 |
| Variable | SW | F | p | DT | F | p | ||
|---|---|---|---|---|---|---|---|---|
| HG (N = 21) | PG (N = 15) | HG (N = 21) | PG (N = 15) | |||||
| Step speed (m/s) | 1.20 ± 0.14 | 1.08 ± 0.13 | 6.607 | 0.015 | 1.13 ± 0.18 | 1.00 ± 0.20 | 4.033 | 0.053 |
| Step frequency (steps/min) | 113.38 ± 9.05 | 109.25 ± 8.38 | 1.929 | 0.174 | 110.96 ± 10.17 | 106.37 ± 12.93 | 1.422 | 0.241 |
| Step length (m) | 0.62 ± 0.07 | 0.59 ± 0.05 | 2.691 | 0.110 | 0.60 ± 0.07 | 0.56 ± 0.06 | 3.887 | 0.057 |
| Step speed CV | 4.64 ± 4.11 | 4.00 ± 2.56 | 0.284 | 0.642 | 4.34 ± 3.95 | 5.02 ± 5.49 | 0.188 | 0.665 |
| Step frequency CV | 3.11 ± 4.53 | 2.41 ± 1.67 | 0.329 | 0.936 | 2.70 ± 3.91 | 3.21 ± 5.54 | 0.106 | 0.785 |
| Step length CV | 2.27 ± 1.14 | 2.32 ± 1.34 | 0.018 | 0.860 | 1.92 ± 0.79 | 3.83 ± 5.24 | 2.748 | 0.026 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fan, W.; Xiao, C.; He, L.; Chen, L.; Qu, H.; Yao, Q.; Li, G.; Hu, J.; Zou, J.; Zeng, Q.; et al. Cerebral Cortex Activation and Gait Performance between Healthy and Prefrail Older Adults during Cognitive and Walking Tasks. Brain Sci. 2023, 13, 1018. https://doi.org/10.3390/brainsci13071018
Fan W, Xiao C, He L, Chen L, Qu H, Yao Q, Li G, Hu J, Zou J, Zeng Q, et al. Cerebral Cortex Activation and Gait Performance between Healthy and Prefrail Older Adults during Cognitive and Walking Tasks. Brain Sciences. 2023; 13(7):1018. https://doi.org/10.3390/brainsci13071018
Chicago/Turabian StyleFan, Weichao, Chongwu Xiao, Longlong He, Ling Chen, Hang Qu, Qiuru Yao, Gege Li, Jinjing Hu, Jihua Zou, Qing Zeng, and et al. 2023. "Cerebral Cortex Activation and Gait Performance between Healthy and Prefrail Older Adults during Cognitive and Walking Tasks" Brain Sciences 13, no. 7: 1018. https://doi.org/10.3390/brainsci13071018
APA StyleFan, W., Xiao, C., He, L., Chen, L., Qu, H., Yao, Q., Li, G., Hu, J., Zou, J., Zeng, Q., & Huang, G. (2023). Cerebral Cortex Activation and Gait Performance between Healthy and Prefrail Older Adults during Cognitive and Walking Tasks. Brain Sciences, 13(7), 1018. https://doi.org/10.3390/brainsci13071018





