Is Social Training Delivered with a Head-Mounted Display Suitable for Patients with Hereditary Ataxia?
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Hardware Solution
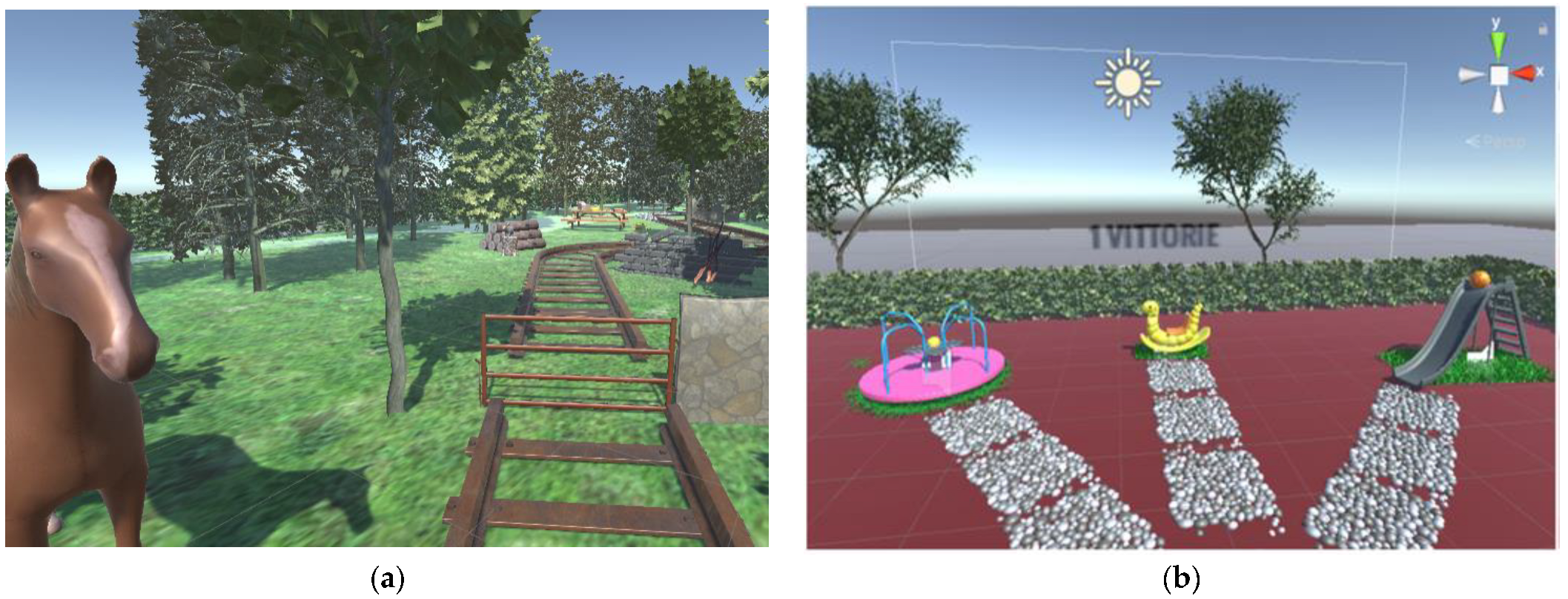
2.3. Unity 3D Environmental Setup
2.4. Software
2.5. Experimental Procedure
2.5.1. Patient Baseline Assessment
2.5.2. Familiarization with the Virtual Environment
2.5.3. VR-SPIRIT Session
2.5.4. Questionnaire Administration
- SUS—System Usability Scale [27]. The primary outcome of the study, which evaluates the usability of the system. The SUS is a simple, ten-item five-point Likert scale giving a global view of subjective assessments of usability.
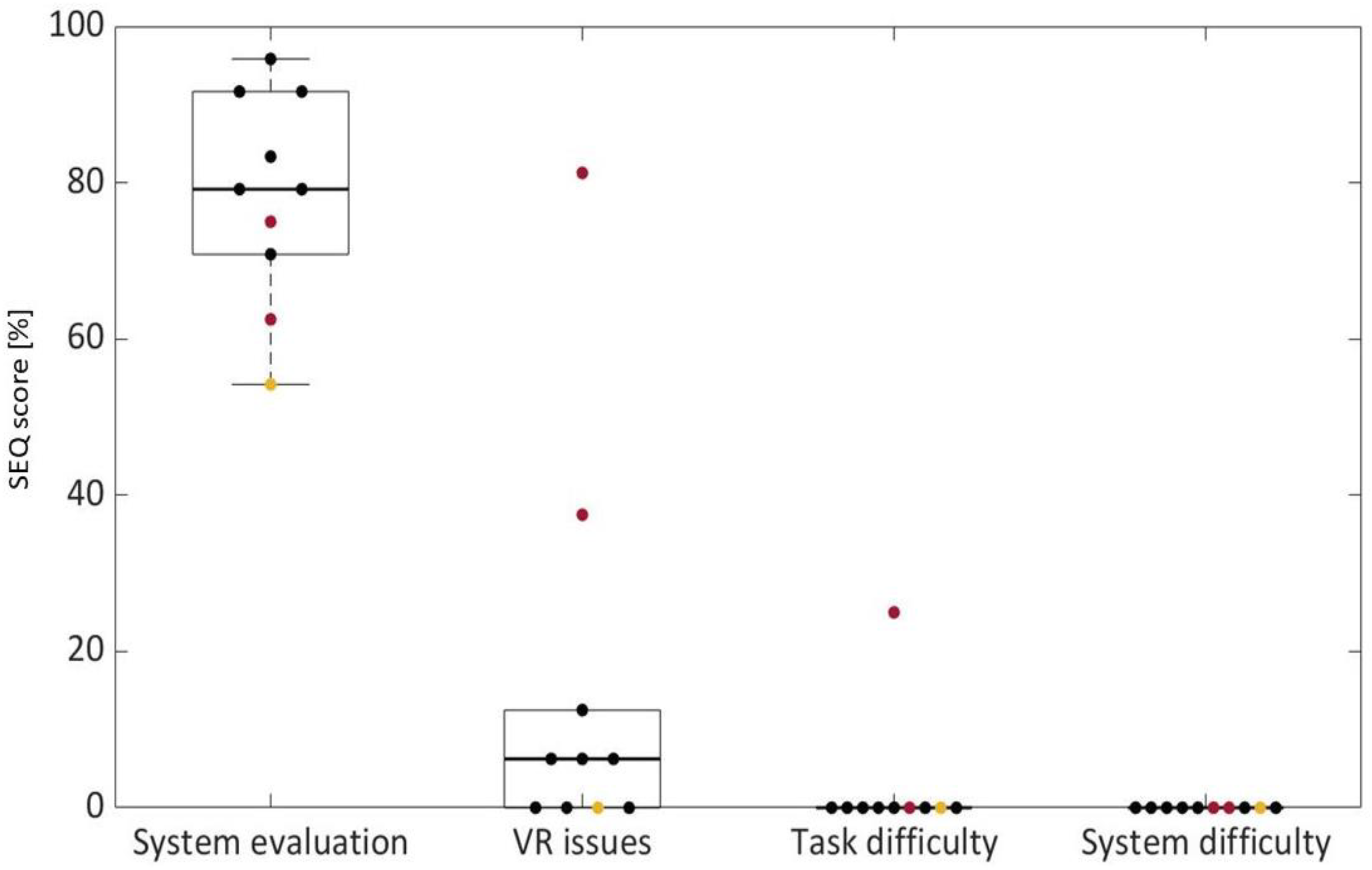
- SEQ—Suitability Evaluation Questionnaire [28]. The questionnaire is especially designed to test VR systems, and it evaluates both sense of presence and tolerability to detect problems frequently associated with virtual rehabilitation systems. The SEQ includes 14 questions, 13 of them with a response graded on a 5-point Likert Scale, and a last open question asking if the subject felt uncomfortable alongside the reasons for this. Questions one to seven can be clustered to assess “system evaluation”: they measure enjoyment, sense of being in the system, feeling of success and control, realism, easy-to-understand instructions, and general discomfort, as explained in [28]. Questions eight to ten are related to cyber sickness issues. Finally, the last two questions are focused on the difficulty, respectively, of the task and of the physical interface used in the system.
- SSQ—Simulator Sickness Questionnaire [29]. The questionnaire evaluates the effects of cyber sickness. Participants have to score 16 symptoms on a four-point scale (0–3). The symptoms can be placed into three general categories: oculomotor, disorientation, and nausea. Weights are assigned to each of the categories and summed together to obtain a single score.
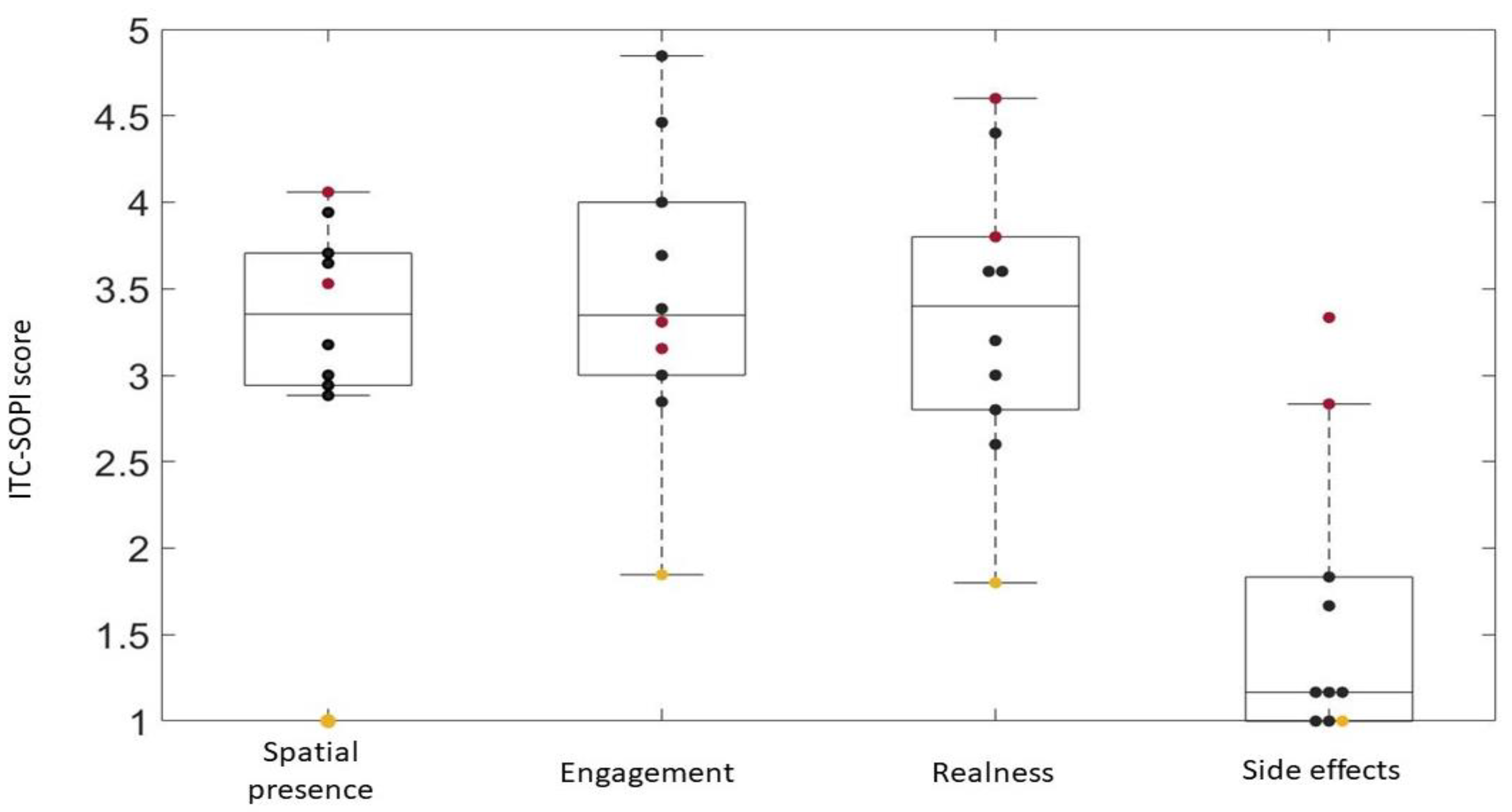
- ITC-SOPI-Independent Television Commission-Sense of Presence Inventory [30]. It is a 5-point Likert scale, composed of 44 items. This questionnaire evaluates the user experience to understand if the person enjoyed the game, the setting, and the overall experience. In particular, the questionnaire addresses four factors: spatial presence, engagement, realness of the environment, and side effects (cyber sickness).
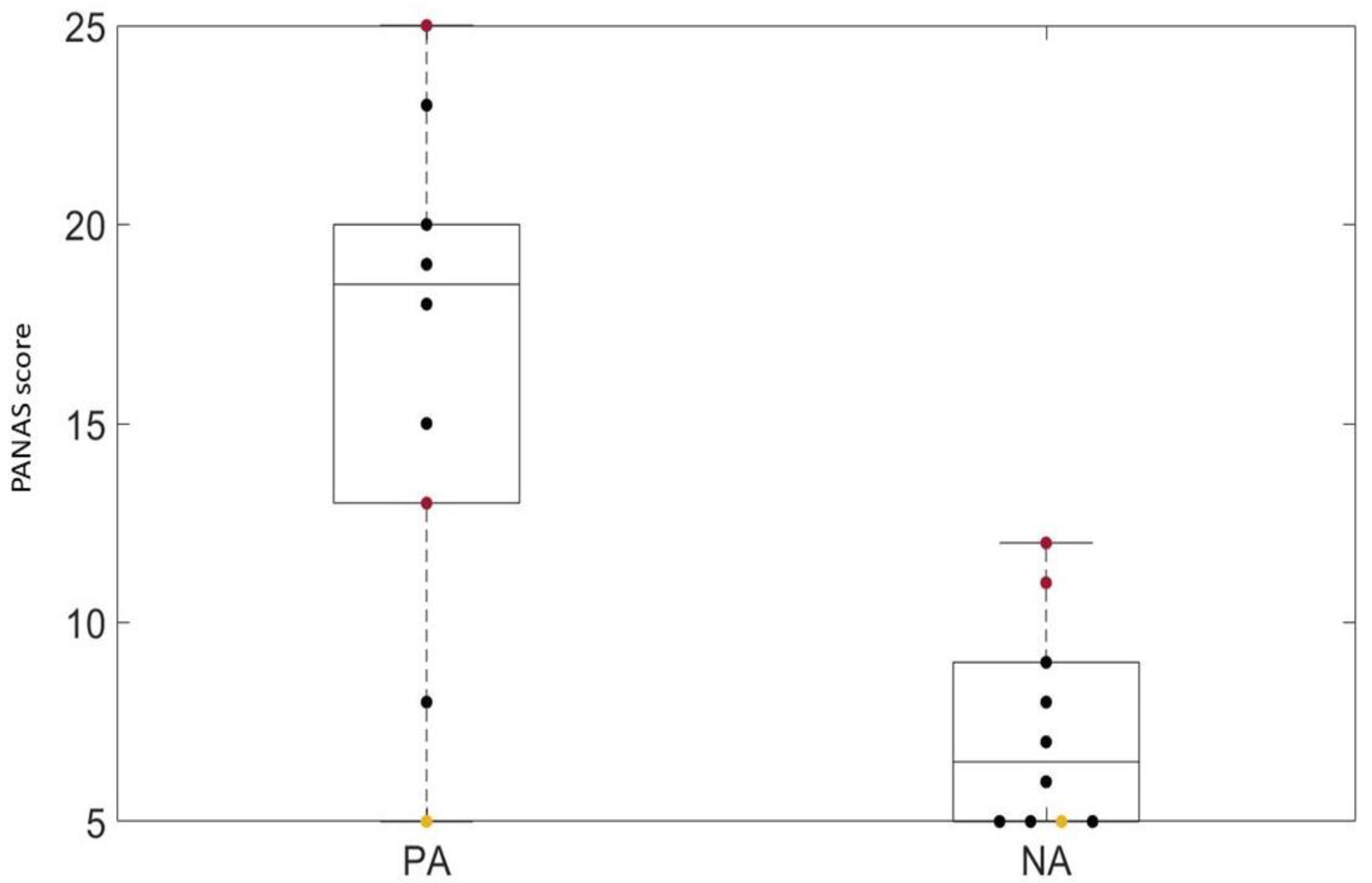
- Short-form of PANASs—Positive Affect and Negative Affect Scales [31]. In the questionnaire, the participant must evaluate how much s/he feels in the way described by the adjective when filling out the questionnaire, responding on a 5-point Likert scale. The PANAS provides measures of Positive Affects (PAs) and Negative Affects (NAs). The PA and NA scores are the sums of the ratings of the PA items and the NA items, respectively. PA indicates the level of pleasurable engagement with the product, while NA is a general factor of subjective distress.
2.6. Statistical Analysis
- Data collected during the baseline assessment and the questionnaires investigating system usability and tolerability, sense of presence, and emotional wellbeing.
- Baseline assessment and indices about a patient’s performance automatically collected during the trial.
- Questionnaires and indices of a patient’s performance.
- All of the questionnaires.
3. Results
3.1. VR-SPIRIT Application Testing
3.2. Subjects’ Performance
3.3. Usability and Tolerability
3.4. Correlations Assessment
3.4.1. Correlation among Baseline Assessments and Questionnaires
3.4.2. Correlation among Baseline Assessments and Indices of Patients’ Performance
3.4.3. Correlation among Questionnaires and Indices of Performance
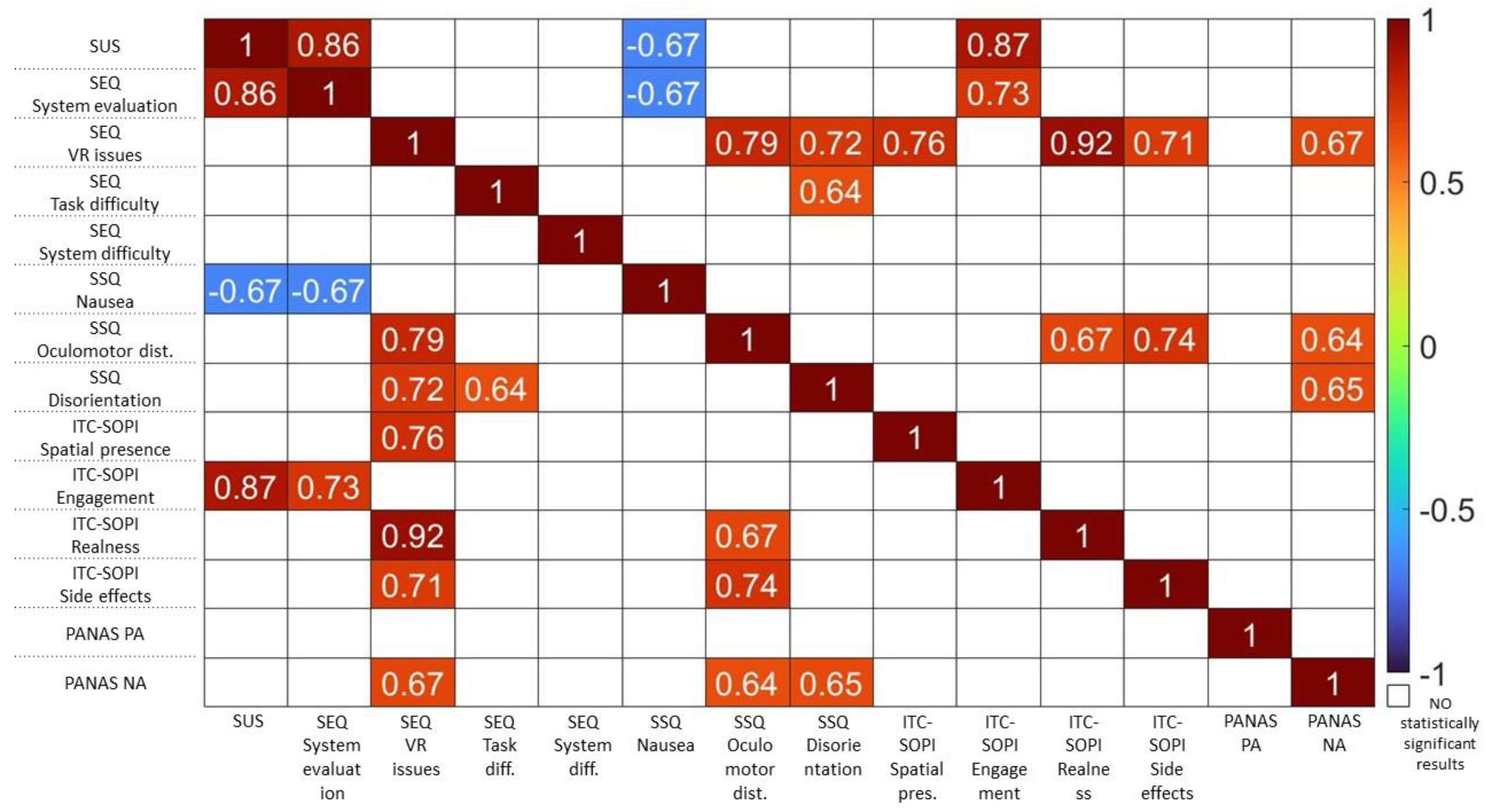
3.4.4. Correlation among Questionnaires
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Helliwell, J.F.; Putnam, R.D. The social context of well–being. Philos. Trans. R. Soc. London. Ser. B Biol. Sci. 2004, 359, 1435–1446. [Google Scholar] [CrossRef] [PubMed]
- Sherman, E.M.; Griffiths, S.Y.; Akdag, S.; Connolly, M.B.; Slick, D.J.; Wiebe, S. Sociodemographic correlates of health-related quality of life in pediatric epilepsy. Epilepsy Behav. 2008, 12, 96–101. [Google Scholar] [CrossRef] [PubMed]
- Abdelgabar, A.R.; Suttrup, J.; Broersen, R.; Bhandari, R.; Picard, S.; Keysers, C.; De Zeeuw, C.I.; Gazzola, V. Action perception recruits the cerebellum and is impaired in patients with spinocerebellar ataxia. Brain 2019, 142, 3791–3805. [Google Scholar] [CrossRef] [PubMed]
- Cattaneo, L.; Fasanelli, M.; Andreatta, O.; Bonifati, D.M.; Barchiesi, G.; Caruana, F. Your Actions in My Cerebellum: Subclinical Deficits in Action Observation in Patients with Unilateral Chronic Cerebellar Stroke. Cerebellum 2012, 11, 264–271. [Google Scholar] [CrossRef] [PubMed]
- Adamaszek, M.; D’agata, F.; Ferrucci, R.; Habas, C.; Keulen, S.; Kirkby, K.C.; Leggio, M.; Mariën, P.; Molinari, M.; Moulton, E.; et al. Consensus Paper: Cerebellum and Emotion. Cerebellum 2017, 16, 552–576. [Google Scholar] [CrossRef]
- Hoche, F.; Guell, X.; Sherman, J.C.; Vangel, M.G.; Schmahmann, J.D. Cerebellar Contribution to Social Cognition. Cerebellum 2015, 15, 732–743. [Google Scholar] [CrossRef]
- Clausi, S.; Olivito, G.; Lupo, M.; Siciliano, L.; Bozzali, M.; Leggio, M. The Cerebellar Predictions for Social Interactions: Theory of Mind Abilities in Patients With Degenerative Cerebellar Atrophy. Front. Cell. Neurosci. 2019, 12, 510. [Google Scholar] [CrossRef]
- Sokolovsky, N.; Cook, A.; Hunt, H.; Giunti, P.; Cipolotti, L. A preliminary characterisation of cognition and social cognition in spinocerebellar ataxia types 2, 1, and 7. Behav. Neurol. 2010, 23, 17–29. [Google Scholar] [CrossRef]
- Seriès, P.; Seitz, A.R. Learning what to expect (in visual perception). Front. Hum. Neurosci. 2013, 7, 668. [Google Scholar] [CrossRef]
- Siman-Tov, T.; Granot, R.Y.; Shany, O.; Singer, N.; Hendler, T.; Gordon, C.R. Is there a prediction network? Meta-analytic evidence for a cortical-subcortical network likely subserving prediction. Neurosci. Biobehav. Rev. 2019, 105, 262–275. [Google Scholar] [CrossRef]
- Ishikawa, T.; Tomatsu, S.; Izawa, J.; Kakei, S. The cerebro-cerebellum: Could it be loci of forward models? Neurosci. Res. 2016, 104, 72–79. [Google Scholar] [CrossRef]
- Sokolov, A.A.; Miall, R.C.; Ivry, R.B. The Cerebellum: Adaptive Prediction for Movement and Cognition. Trends Cogn. Sci. 2017, 21, 313–332. [Google Scholar] [CrossRef] [PubMed]
- Oldrati, V.; Ferrari, E.; Butti, N.; Cattaneo, Z.; Borgatti, R.; Urgesi, C.; Finisguerra, A. How social is the cerebellum? Exploring the effects of cerebellar transcranial direct current stimulation on the prediction of social and physical events. Anat. Embryol. 2021, 226, 671–684. [Google Scholar] [CrossRef] [PubMed]
- Ma, Q.; Pu, M.; Heleven, E.; Haihambo, N.P.; Baetens, K.; Baeken, C.; Deroost, N.; Van Overwalle, F. The posterior cerebellum supports implicit learning of social belief sequences. Cogn. Affect. Behav. Neurosci. 2021, 21, 970–992. [Google Scholar] [CrossRef] [PubMed]
- Van Overwalle, F.; De Coninck, S.; Heleven, E.; Perrotta, G.; Ben Taib, N.O.; Manto, M.; Mariën, P. The role of the cerebellum in reconstructing social action sequences: A pilot study. Soc. Cogn. Affect. Neurosci. 2019, 14, 549–558. [Google Scholar] [CrossRef]
- Urgesi, C.; Butti, N.; Finisguerra, A.; Biffi, E.; Valente, E.M.; Romaniello, R.; Borgatti, R. Social prediction in pediatric patients with congenital, non-progressive malformations of the cerebellum: From deficits in predicting movements to rehabilitation in virtual reality. Cortex 2021, 144, 82–98. [Google Scholar] [CrossRef]
- Butti, N.; Corti, C.; Finisguerra, A.; Bardoni, A.; Borgatti, R.; Poggi, G.; Urgesi, C. Cerebellar Damage Affects Contextual Priors for Action Prediction in Patients with Childhood Brain Tumor. Cerebellum 2020, 19, 799–811. [Google Scholar] [CrossRef]
- Butti, N.; Biffi, E.; Genova, C.; Romaniello, R.; Redaelli, D.F.; Reni, G.; Borgatti, R.; Urgesi, C. Virtual Reality Social Prediction Improvement and Rehabilitation Intensive Training (VR-SPIRIT) for paediatric patients with congenital cerebellar diseases: Study protocol of a randomised controlled trial. Trials 2020, 21, 82. [Google Scholar] [CrossRef]
- Jayadev, S.; Bird, T.D. Hereditary ataxias: Overview. Anesth. Analg. 2013, 15, 673–683. [Google Scholar] [CrossRef]
- Manto, M.; Mariën, P. Schmahmann’s syndrome—Identification of the third cornerstone of clinical ataxiology. Cerebellum Ataxias 2015, 2, 2. [Google Scholar] [CrossRef]
- Schmahmann, J.D.; Sherman, J.C. The cerebellar cognitive affective syndrome. Brain J. Neurol. 1998, 121, 561–579. [Google Scholar] [CrossRef]
- Van Overwalle, F.; Manto, M.; Cattaneo, Z.; Clausi, S.; Ferrari, C.; Gabrieli, J.D.E.; Guell, X.; Heleven, E.; Lupo, M.; Ma, Q.; et al. Consensus Paper: Cerebellum and Social Cognition. Cerebellum 2020, 19, 833–868. [Google Scholar] [CrossRef] [PubMed]
- Leggio, M.; Molinari, M. Cerebellar Sequencing: A Trick for Predicting the Future. Cerebellum 2015, 14, 35–38. [Google Scholar] [CrossRef] [PubMed]
- Davis, S.; Nesbitt, K.; Nalivaiko, E. A systematic review of cybersickness. In Proceedings of the 2014 Conference on Interactive Entertainment, Newcastle, Australia, 2–3 December 2014; pp. 1–9. [Google Scholar]
- Unity 3D Official Webpage. Available online: https:/unity3d.com (accessed on 21 September 2021).
- Subramony, S.H. SARA—A new clinical scale for the assessment and rating of ataxia. Nat. Clin. Pract. Neurol. 2007, 3, 136–137. [Google Scholar] [CrossRef]
- Brooke, J. SUS: A ’Quick and Dirty’ Usability Scale. Usability Eval. Ind. 1996, 189, 4–7. [Google Scholar]
- Gil-Gómez, J.-A.; Gil-Gómez, H.; Lozano-Quilis, J.-A.; Manzano-Hernández, P.; Albiol-Pérez, S.; Aula-Valero, C. SEQ: Suitability evaluation questionnaire for virtual rehabilitation systems. Application in a virtual rehabilitation system for balance rehabilitation. In Proceedings of the 2013 7th International Conference on Pervasive Computing Technologies for Healthcare and Workshops, Venice, Italy, 5–8 May 2013; pp. 335–338. [Google Scholar]
- Kennedy, R.S.; Lane, N.E.; Berbaum, K.S.; Lilienthal, M.G. Simulator Sickness Questionnaire: An Enhanced Method for Quantifying Simulator Sickness. Int. J. Aviat. Psychol. 1993, 3, 203–220. [Google Scholar] [CrossRef]
- Lessiter, J.; Freeman, J.; Keogh, E.; Davidoff, J. A Cross-Media Presence Questionnaire: The ITC-Sense of Presence Inventory. PRESENCE Virtual Augment. Real. 2001, 10, 282–297. [Google Scholar] [CrossRef]
- Watson, D.; Clark, L.A.; Tellegen, A. Development and validation of brief measures of positive and negative affect: The PANAS scales. J. Pers. Soc. Psychol. 1988, 54, 1063. [Google Scholar] [CrossRef] [PubMed]
- Bangor, A.; Kortum, P.; Miller, J. Determining what individual SUS scores mean: Adding an adjective rating scale. J. Usability Stud. 2009, 4, 114–123. [Google Scholar]
- LaViola, J.J. A discussion of cybersickness in virtual environments. ACM SIGCHI Bull. 2000, 32, 47–56. [Google Scholar] [CrossRef]
- Morizio, C.; Compagnat, M.; Boujut, A.; Labbani-Igbida, O.; Billot, M.; Perrochon, A. Immersive Virtual Reality during Robot-Assisted Gait Training: Validation of a New Device in Stroke Rehabilitation. Medicina 2022, 58, 1805. [Google Scholar] [CrossRef]
- Winter, C.; Kern, F.; Gall, D.; Latoschik, M.E.; Pauli, P.; Käthner, I. Immersive virtual reality during gait rehabilitation increases walking speed and motivation: A usability evaluation with healthy participants and patients with multiple sclerosis and stroke. J. Neuroeng. Rehabil. 2021, 18, 68. [Google Scholar] [CrossRef] [PubMed]
- Weber, L.M.; Nilsen, D.M.; Gillen, G.; Yoon, J.; Stein, J. Immersive virtual reality mirror therapy for upper limb recovery following stroke: A pilot study. Am. J. Phys. Med. Rehabil. 2019, 98, 783. [Google Scholar] [CrossRef] [PubMed]
- Mondellini, M.; Arlati, S.; Pizzagalli, S.; Greci, L.; Sacco, M.; Ferrigno, G. Assessment of the usability of an immersive virtual supermarket for the cognitive rehabilitation of elderly patients: A pilot study on young adults. In Proceedings of the 2018 IEEE 6th International Conference on Serious Games and Applications for Health (SeGAH), Vienna, Austria, 16–18 May 2018; pp. 1–8. [Google Scholar] [CrossRef]
- Corrêa, A.G.D.; Kintschner, N.R.; Campos, V.Z.; Blascovi-Assis, S.M. Gear VR and leap motion sensor applied in virtual rehabilitation for manual function training: An opportunity for home rehabilitation. In Proceedings of the 5th Workshop on ICTs for improving Patients Rehabilitation Research Techniques, Popayan, Columbia, 11–13 September 2019; pp. 148–151. [Google Scholar]
- Shum, L.C.; Valdes, B.A.; Hodges, N.J.; Van der Loos, H.F.M. Error Augmentation in Immersive Virtual Reality for Bimanual Upper-Limb Rehabilitation in Individuals With and Without Hemiplegic Cerebral Palsy. IEEE Trans. Neural Syst. Rehabil. Eng. 2019, 28, 541–549. [Google Scholar] [CrossRef] [PubMed]
- Mathiak, K.A.; Klasen, M.; Zvyagintsev, M.; Weber, R.; Mathiak, K. Neural networks underlying affective states in a multimodal virtual environment: Contributions to boredom. Front. Hum. Neurosci. 2013, 7, 820. [Google Scholar] [CrossRef] [PubMed]
- Grassini, S.; Laumann, K.; Luzi, A.K. Association of Individual Factors with Simulator Sickness and Sense of Presence in Virtual Reality Mediated by Head-Mounted Displays (HMDs). Multimodal Technol. Interact. 2021, 5, 7. [Google Scholar] [CrossRef]
- Kim, H.; Kim, D.J.; Chung, W.H.; Park, K.-A.; Kim, J.D.K.; Kim, D.; Kim, K.; Jeon, H.J. Clinical predictors of cybersickness in virtual reality (VR) among highly stressed people. Sci. Rep. 2021, 11, 12139. [Google Scholar] [CrossRef]



| Patient | Age (Years) | Gender | SARA Score | Disease | Disease Onset (Years Old) |
|---|---|---|---|---|---|
| S1 | 21.0 | F | 17.5 | Friedreich’s ataxia | 9 |
| S2 | 18.8 | M | 13.5 | Friedreich’s ataxia | 11 |
| S3 | 28.7 | M | 23.5 | Ataxia of Charlevoix–Saguenay | 3 |
| S4 | 49.9 | M | 22 | Spinocerebellar ataxia | 23 |
| S5 | 51.6 | M | 18 | Spinocerebellar ataxia | 21 |
| S6 | 31.4 | M | 19 | Friedreich’s ataxia | 16 |
| S7 | 46.9 | M | 19.5 | Spinocerebellar ataxia | 40 |
| S8 | 58.7 | F | 27 | Friedreich’s ataxia | 39 |
| S9 | 51.9 | M | 20 | Spinocerebellar ataxia | 44 |
| S10 | 18.3 | F | 15.5 | Spinocerebellar ataxia | 1 |
| Patient | Duration (s) | Prediction Score (%) |
|---|---|---|
| S1 | 16.7 (0.8) | 41.3 (18.5) |
| S2 | 15.6 (0.7) | 95.0 (8.7) |
| S3 | 17.2 (1.1) | 61.7 (7.6) |
| S4 | 17.0 (1.0) | 66.7 (30.1) |
| S5 | 11.1 (2.1) | 61.7 (29.3) |
| S8 | 11.8 (2.4) | 55.0 (13.2) |
| S10 | 11.9 (2.1) | 71.7 (2.9) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Malerba, G.; Bellazzecca, S.; Urgesi, C.; Butti, N.; D’Angelo, M.G.; Diella, E.; Biffi, E. Is Social Training Delivered with a Head-Mounted Display Suitable for Patients with Hereditary Ataxia? Brain Sci. 2023, 13, 1017. https://doi.org/10.3390/brainsci13071017
Malerba G, Bellazzecca S, Urgesi C, Butti N, D’Angelo MG, Diella E, Biffi E. Is Social Training Delivered with a Head-Mounted Display Suitable for Patients with Hereditary Ataxia? Brain Sciences. 2023; 13(7):1017. https://doi.org/10.3390/brainsci13071017
Chicago/Turabian StyleMalerba, Giorgia, Silvia Bellazzecca, Cosimo Urgesi, Niccolò Butti, Maria Grazia D’Angelo, Eleonora Diella, and Emilia Biffi. 2023. "Is Social Training Delivered with a Head-Mounted Display Suitable for Patients with Hereditary Ataxia?" Brain Sciences 13, no. 7: 1017. https://doi.org/10.3390/brainsci13071017
APA StyleMalerba, G., Bellazzecca, S., Urgesi, C., Butti, N., D’Angelo, M. G., Diella, E., & Biffi, E. (2023). Is Social Training Delivered with a Head-Mounted Display Suitable for Patients with Hereditary Ataxia? Brain Sciences, 13(7), 1017. https://doi.org/10.3390/brainsci13071017







