Does Music Therapy Improve Gait after Traumatic Brain Injury and Spinal Cord Injury? A Mini Systematic Review and Meta-Analysis
Abstract
:1. Introduction
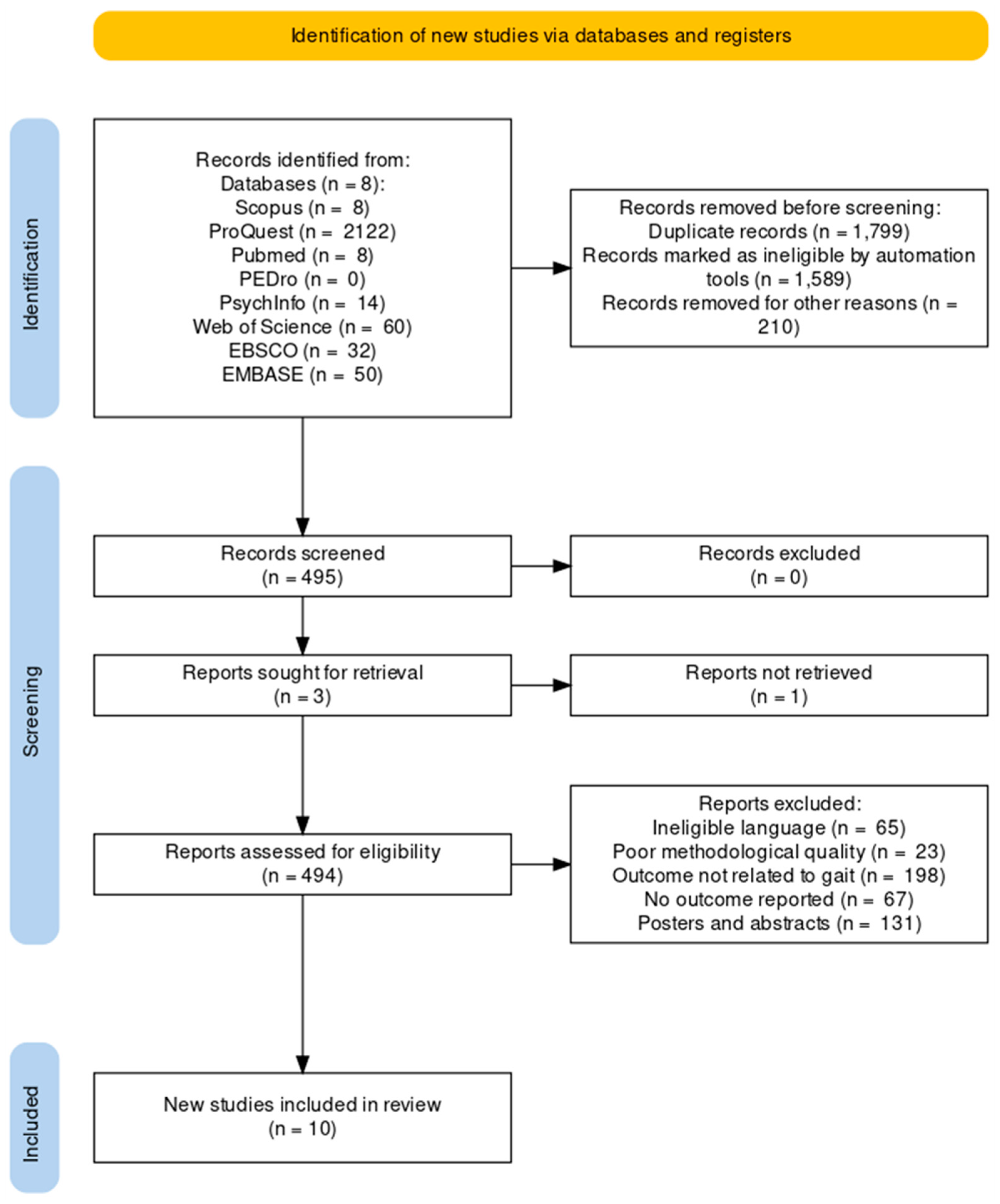
2. Materials and Methods
2.1. Data Sources and Search Strategy
2.2. Evaluation of the Methodological Quality
2.3. Data Analysis
3. Results
3.1. Study Design
3.2. Country of Research
3.3. Risk of Bias
3.4. Publication Bias
3.5. Systematic Review Report
3.5.1. Participants
3.5.2. Years since Injury
3.5.3. Outcome
3.5.4. Characteristics of Music Therapy
3.6. Meta-Analysis Report
Sensitivity Analysis
4. Discussion
4.1. Limitations
4.2. Future Directions
5. Conclusions
Supplementary Materials
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Badhiwala, J.H.; Wilson, J.R.; Fehlings, M.G. Global burden of traumatic brain and spinal cord injury. Lancet Neurol. 2019, 18, 24–25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Williams, G.; Morris, M.E.; Schache, A.; McCrory, P.R. Incidence of gait abnormalities after traumatic brain injury. Arch. Phys. Med. Rehabil. 2009, 90, 587–593. [Google Scholar] [CrossRef]
- Williams, G.; Galna, B.; Morris, M.E.; Olver, J. Spatiotemporal deficits and kinematic classification of gait following a traumatic brain injury: A systematic review. J. Head Trauma Rehabil. 2010, 25, 366–374. [Google Scholar] [CrossRef] [PubMed]
- Waters, R.L.; Yakura, J.S.; Adkins, R.H. Gait performance after spinal cord injury. Clin. Orthop. Relat. Res. 1993, 288, 87–96. [Google Scholar] [CrossRef]
- Mirelman, A.; Shema, S.; Maidan, I.; Hausdorff, J.M. Chapter 7—Gait. In Handbook of Clinical Neurology; Day, B.L., Lord, S.R., Eds.; Elsevier: Amsterdam, The Netherlands, 2018; Volume 159, pp. 119–134. [Google Scholar]
- Williams, G.; Willmott, C. Higher levels of mobility are associated with greater societal participation and better quality-of-life. Brain Inj. 2012, 26, 1065–1071. [Google Scholar] [CrossRef]
- Riggins, M.S.; Kankipati, P.; Oyster, M.L.; Cooper, R.A.; Boninger, M.L. The relationship between quality of life and change in mobility 1 year postinjury in individuals with spinal cord injury. Arch. Phys. Med. Rehabil. 2011, 92, 1027–1033. [Google Scholar] [CrossRef]
- Bland, D.C.; Zampieri, C.; Damiano, D.L. Effectiveness of physical therapy for improving gait and balance in individuals with traumatic brain injury: A systematic review. Brain Inj. 2011, 25, 664–679. [Google Scholar] [CrossRef] [Green Version]
- Fehlings, M.G.; Pedro, K.; Hejrati, N. Management of Acute Spinal Cord Injury: Where Have We Been? Where Are We Now? Where Are We Going? J. Neurotrauma 2022, 39, 1591–1602. [Google Scholar] [CrossRef]
- Brancatisano, O.; Baird, A.; Thompson, W.F. Why is music therapeutic for neurological disorders? The Therapeutic Music Capacities Model. Neurosci. Biobehav. Rev. 2020, 112, 600–615. [Google Scholar] [CrossRef]
- Hegde, S. Music-based cognitive remediation therapy for patients with traumatic brain injury. Front. Neurol. 2014, 5, 34. [Google Scholar] [CrossRef] [Green Version]
- Mishra, R.; Florez-Perdomo, W.A.; Shrivatava, A.; Chouksey, P.; Raj, S.; Moscote-Salazar, L.R.; Rahman, M.M.; Sutar, R.; Agrawal, A. Role of music therapy in traumatic brain injury: A systematic review and meta-analysis. World Neurosurg. 2021, 146, 197–204. [Google Scholar] [CrossRef]
- Mercier, L.J.; Grant, C.; Langelier, D.M.; Plamondon, S. Scoping review of music therapy and music interventions in spinal cord injury. Disabil. Rehabil. 2022, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Braun Janzen, T.; Koshimori, Y.; Richard, N.M.; Thaut, M.H. Rhythm and Music-Based Interventions in Motor Rehabilitation: Current Evidence and Future Perspectives. Front. Hum. Neurosci. 2022, 15, 789467. [Google Scholar] [CrossRef] [PubMed]
- Hunt, N.; McGrath, D.; Stergiou, N. The influence of auditory-motor coupling on fractal dynamics in human gait. Sci. Rep. 2014, 4, 5879. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hurt, C.P.; Rice, R.R.; McIntosh, G.C.; Thaut, M.H. Rhythmic auditory stimulation in gait training for patients with traumatic brain injury. J. Music Ther. 1998, 35, 228–241. [Google Scholar] [CrossRef] [PubMed]
- Verga, L.; Schwartze, M.; Stapert, S.; Winkens, I.; Kotz, S.A. Dysfunctional Timing in Traumatic Brain Injury Patients: Co-occurrence of Cognitive, Motor, and Perceptual Deficits. Front. Psychol. 2021, 12, 731898. [Google Scholar] [CrossRef]
- Mioni, G.; Grondin, S.; Stablum, F. Temporal dysfunction in traumatic brain injury patients: Primary or secondary impairment? Front. Hum. Neurosci. 2014, 8, 269. [Google Scholar] [CrossRef] [Green Version]
- Rosin, R.; Topka, H.; Dichgans, J. Gait initiation in Parkinson’s disease. Mov. Disord. Off. J. Mov. Disord. Soc. 1997, 12, 682–690. [Google Scholar] [CrossRef]
- Phadke, C.P.; Thompson, F.J.; Kukulka, C.G.; Nair, P.M.; Bowden, M.G.; Madhavan, S.; Trimble, M.H.; Behrman, A.L. Soleus H-reflex modulation after motor incomplete spinal cord injury: Effects of body position and walking speed. J. Spinal Cord Med. 2010, 33, 371–378. [Google Scholar] [CrossRef]
- Naka, T.; Hayashi, T.; Sugyo, A.; Watanabe, R.; Towatari, F.; Maeda, T. The effects of lower extremity deep sensory impairments on walking capability in patients with incomplete cervical spinal cord injury. J. Spinal Cord Med. 2022, 45, 287–292. [Google Scholar] [CrossRef]
- Zwijgers, E.; van Asseldonk, E.H.F.; Vos-van der Hulst, M.; Geurts, A.C.H.; Keijsers, N.L.W. Impaired foot placement strategy during walking in people with incomplete spinal cord injury. J. NeuroEng. Rehabil. 2022, 19, 134. [Google Scholar] [CrossRef] [PubMed]
- Giangregorio, L.; McCartney, N. Bone loss and muscle atrophy in spinal cord injury: Epidemiology, fracture prediction, and rehabilitation strategies. J. Spinal Cord Med. 2006, 29, 489–500. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Molinari, M.; Leggio, M.G.; De Martin, M.; Cerasa, A.; Thaut, M. Neurobiology of Rhythmic Motor Entrainment. Ann. N. Y. Acad. Sci. 2003, 999, 313–321. [Google Scholar] [CrossRef]
- Nombela, C.; Hughes, L.E.; Owen, A.M.; Grahn, J.A. Into the groove: Can rhythm influence Parkinson’s disease? Neurosci. Biobehav. Rev. 2013, 37, 2564–2570. [Google Scholar] [CrossRef] [Green Version]
- Ghai, S.; Ghai, I.; Schmitz, G.; Effenberg, A.O. Effect of rhythmic auditory cueing on parkinsonian gait: A systematic review and meta-analysis. Sci. Rep. 2018, 8, 506. [Google Scholar] [CrossRef] [Green Version]
- Silvestrini, N.; Piguet, V.; Cedraschi, C.; Zentner, M.R. Music and auditory distraction reduce pain: Emotional or attentional effects? Music Med. 2011, 3, 264–270. [Google Scholar] [CrossRef]
- Garza-Villarreal, E.; Wilson, A.; Vase, L.; Brattico, E.; Barrios, F.; Jensen, T.; Romero-Romo, J.; Vuust, P. Music reduces pain and increases functional mobility in fibromyalgia. Front. Psychol. 2014, 5, 90. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wood, C.; Cutshall, S.M.; Lawson, D.K.; Ochtrup, H.M.; Henning, N.B.; Larsen, B.E.; Bauer, B.A.; Mahapatra, S.; Wahner-Roedler, D.L. Music Therapy for Anxiety and Pain After Spinal Cord Injury: A Pilot Study. Glob. Adv. Health Med. 2021, 10, 21649561211058697. [Google Scholar] [CrossRef]
- Koelsch, S. A neuroscientific perspective on music therapy. Ann. N. Y. Acad. Sci. 2009, 1169, 374–384. [Google Scholar] [CrossRef]
- Thaut, M.H.; McIntosh, G.C.; Hoemberg, V. Neurobiological foundations of neurologic music therapy: Rhythmic entrainment and the motor system. Front. Psychol. 2015, 5, 1185. [Google Scholar] [CrossRef] [Green Version]
- Nishida, D.; Mizuno, K.; Yamada, E.; Hanakawa, T.; Liu, M.; Tsuji, T. The neural correlates of gait improvement by rhythmic sound stimulation in adults with Parkinson’s disease–A functional magnetic resonance imaging study. Park. Relat. Disord. 2021, 84, 91–97. [Google Scholar] [CrossRef] [PubMed]
- Vik, B.M.D.; Skeie, G.O.; Vikane, E.; Specht, K. Effects of music production on cortical plasticity within cognitive rehabilitation of patients with mild traumatic brain injury. Brain Inj. 2018, 32, 634–643. [Google Scholar] [CrossRef] [PubMed]
- Altenmüller, E.; Schlaug, G. Neurologic music therapy: The beneficial effects of music making on neurorehabilitation. Acoust. Sci. Technol. 2013, 34, 5–12. [Google Scholar] [CrossRef] [Green Version]
- Sihvonen, A.J.; Siponkoski, S.-T.; Martínez-Molina, N.; Laitinen, S.; Holma, M.; Ahlfors, M.; Kuusela, L.; Pekkola, J.; Koskinen, S.; Särkämö, T. Neurological Music Therapy Rebuilds Structural Connectome after Traumatic Brain Injury: Secondary Analysis from a Randomized Controlled Trial. J. Clin. Med. 2022, 11, 2184. [Google Scholar] [CrossRef] [PubMed]
- Siponkoski, S.-T.; Martínez-Molina, N.; Kuusela, L.; Laitinen, S.; Holma, M.; Ahlfors, M.; Jordan-Kilkki, P.; Ala-Kauhaluoma, K.; Melkas, S.; Pekkola, J.; et al. Music Therapy Enhances Executive Functions and Prefrontal Structural Neuroplasticity after Traumatic Brain Injury: Evidence from a Randomized Controlled Trial. J. Neurotrauma 2019, 37, 618–634. [Google Scholar] [CrossRef] [PubMed]
- Särkämö, T. Cognitive, emotional, and neural benefits of musical leisure activities in aging and neurological rehabilitation: A critical review. Ann. Phys. Rehabil. Med. 2018, 61, 414–418. [Google Scholar] [CrossRef]
- Ghai, S.; Maso, F.D.; Ogourtsova, T.; Porxas, A.-X.; Villeneuve, M.; Penhune, V.; Boudrias, M.-H.; Baillet, S.; Lamontagne, A. Neurophysiological Changes Induced by Music-Supported Therapy for Recovering Upper Extremity Function after Stroke: A Case Series. Brain Sci. 2021, 11, 666. [Google Scholar] [CrossRef]
- Bangert, M.; Altenmüller, E.O. Mapping perception to action in piano practice: A longitudinal DC-EEG study. BMC Neurosci. 2003, 4, 26. [Google Scholar] [CrossRef] [Green Version]
- Ghai, S.; Ghai, I.; Effenberg, A.O. Effects of dual tasks and dual-task training on postural stability: A systematic review and meta-analysis. Clin. Interv. Aging 2017, 12, 557. [Google Scholar] [CrossRef] [Green Version]
- Ronsse, R.; Puttemans, V.; Coxon, J.P.; Goble, D.J.; Wagemans, J.; Wenderoth, N.; Swinnen, S.P. Motor learning with augmented feedback: Modality-dependent behavioral and neural consequences. Cereb. Cortex 2011, 21, 1283–1294. [Google Scholar] [CrossRef] [Green Version]
- Ghai, S.; Ghai, I.; Effenberg, A.O. Effect of rhythmic auditory cueing on aging gait: A systematic review and meta-analysis. Aging Dis. 2018, 9, 901. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ghai, S.; Schmitz, G.; Hwang, T.-H.; Effenberg, A.O. Auditory proprioceptive integration: Effects of real-time kinematic auditory feedback on knee proprioception. Front. Neurosci. 2018, 12, 142. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ghai, S.; Schmitz, G.; Hwang, T.H.; Effenberg, A.O. Training proprioception with sound: Effects of real-time auditory feedback on intermodal learning. Ann. N. Y. Acad. Sci. 2019, 1438, 50–61. [Google Scholar] [CrossRef]
- Danna, J.; Velay, J.-L. On the auditory-proprioception substitution hypothesis: Movement sonification in two deafferented subjects learning to write new characters. Front. Neurosci. 2017, 11, 137. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tian, R.; Zhang, B.; Zhu, Y. Rhythmic Auditory Stimulation as an Adjuvant Therapy Improved Post-stroke Motor Functions of the Upper Extremity: A Randomized Controlled Pilot Study. Front. Neurosci. 2020, 14, 649. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.J.; Yoo, G.E.; Shin, Y.K.; Cho, S.R. Gait training for adults with cerebral palsy following harmonic modification in rhythmic auditory stimulation. Ann. N. Y. Acad. Sci. 2020, 1473, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Thaut, M.H.; Abiru, M. Rhythmic auditory stimulation in rehabilitation of movement disorders: A review of current research. Music Percept. 2010, 27, 263–269. [Google Scholar] [CrossRef] [Green Version]
- Schaefer, R.S. Auditory rhythmic cueing in movement rehabilitation: Findings and possible mechanisms. Philos. Trans. R. Soc. B Biol. Sci. 2014, 369, 20130402. [Google Scholar] [CrossRef]
- Fritz, T.H.; Halfpaap, J.; Grahl, S.; Kirkland, A.; Villringer, A. Musical feedback during exercise machine workout enhances mood. Front. Psychol. 2013, 4, 921. [Google Scholar] [CrossRef] [Green Version]
- Bella, S.D.; Dotov, D.; Bardy, B.; de Cock, V.C. Individualization of music-based rhythmic auditory cueing in Parkinson’s disease. Ann. N. Y. Acad. Sci. 2018, 1423, 308–317. [Google Scholar] [CrossRef]
- Effenberg, A.O.; Fehse, U.; Schmitz, G.; Krueger, B.; Mechling, H. Movement sonification: Effects on motor learning beyond rhythmic adjustments. Front. Neurosci. 2016, 10, 219. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baram, Y.; Miller, A. Auditory feedback control for improvement of gait in patients with Multiple Sclerosis. J. Neurol. Sci. 2007, 254, 90–94. [Google Scholar] [CrossRef] [PubMed]
- Yovanoff, M.A.; Chen, H.-E.; Pepley, D.F.; Mirkin, K.A.; Han, D.C.; Moore, J.Z.; Miller, S.R. Investigating the Effect of Simulator Functional Fidelity and Personalized Feedback on Central Venous Catheterization Training. J. Surg. Educ. 2018, 75, 1410–1421. [Google Scholar] [CrossRef] [PubMed]
- Françoise, J.; Bevilacqua, F. Motion-sound mapping through interaction: An approach to user-centered design of auditory feedback using machine learning. ACM Trans. Interact. Intell. Syst. 2018, 8, 1–30. [Google Scholar] [CrossRef]
- Iber, M.; Dumphart, B.; Oliveira, V.-A.d.J.; Ferstl, S.; Reis, J.M.; Slijepčević, D.; Heller, M.; Raberger, A.-M.; Horsak, B. Mind the Steps: Towards Auditory Feedback in Tele-Rehabilitation Based on Automated Gait Classification. In Proceedings of the Audio Mostly 2021, Virtual/Trento, Italy, 1–3 September 2021; Association for Computing Machinery: New York, NY, USA, 2021; pp. 139–146. [Google Scholar]
- Lee, S.Y.; Amatya, B.; Judson, R.; Truesdale, M.; Reinhardt, J.D.; Uddin, T.; Xiong, X.-H.; Khan, F. Clinical practice guidelines for rehabilitation in traumatic brain injury: A critical appraisal. Brain Inj. 2019, 33, 1263–1271. [Google Scholar] [CrossRef]
- Jones, M.; Harness, E.; Denison, P.; Tefertiller, C.; Evans, N.; Larson, C. Activity-based Therapies in Spinal Cord Injury: Clinical Focus and Empirical Evidence in Three Independent Programs. Top. Spinal Cord Inj. Rehabil. 2012, 18, 34–42. [Google Scholar] [CrossRef] [Green Version]
- Zbogar, D.; Eng, J.J.; Miller, W.C.; Krassioukov, A.V.; Verrier, M.C. Movement repetitions in physical and occupational therapy during spinal cord injury rehabilitation. Spinal Cord 2017, 55, 172–179. [Google Scholar] [CrossRef] [Green Version]
- Amatachaya, S.; Keawsutthi, M.; Amatachaya, P.; Manimmanakorn, N. Effects of external cues on gait performance in independent ambulatory incomplete spinal cord injury patients. Spinal Cord 2009, 47, 668–673. [Google Scholar] [CrossRef] [Green Version]
- Singhal, K.; Kataria, C. Short Term Effects of Rhythmic Auditory Stimulation with Body Weight Supported Treadmill Training on Gait and Balance in Individuals with Incomplete Spinal Cord Injury. Int. J. Sci. Healthc. Res. 2021, 6, 191–197. [Google Scholar] [CrossRef]
- Wilfong, J.L. The Effects of Rhythmic Auditory Stimulation (RAS) on Gait Training for Persons with Traumatic Brain Injury. Master’s Thesis, Michigan State University, East Lansing, MI, USA, 2009. [Google Scholar]
- Thompson, S.; Hays, K.; Weintraub, A.; Ketchum, J.M.; Kowalski, R.G. Rhythmic auditory stimulation and gait training in traumatic brain injury: A pilot study. J. Music Ther. 2021, 58, 70–94. [Google Scholar] [CrossRef]
- Tamburella, F.; Lorusso, M.; Tagliamonte, N.L.; Bentivoglio, F.; Bigioni, A.; Pisotta, I.; Lancini, M.; Pasinetti, S.; Ghidelli, M.; Masciullo, M. Load auditory feedback boosts crutch usage in subjects with central nervous system lesions: A pilot study. Front. Neurol. 2021, 12, 1115. [Google Scholar] [CrossRef]
- Sheridan, C.; Thaut, C.; Brooks, D.; Patterson, K.K. Feasibility of a rhythmic auditory stimulation gait training program in community-dwelling adults after TBI: A case report. NeuroRehabilitation 2021, 48, 221–230. [Google Scholar] [CrossRef] [PubMed]
- de l’Etoile, S.K. The effect of rhythmic auditory stimulation on the gait parameters of patients with incomplete spinal cord injury: An exploratory pilot study. Int. J. Rehabil. Res. 2008, 31, 155–157. [Google Scholar] [CrossRef] [PubMed]
- Nayak, S.; Wheeler, B.L.; Shiflett, S.C.; Agostinelli, S. Effect of music therapy on mood and social interaction among individuals with acute traumatic brain injury and stroke. Rehabil. Psychol. 2000, 45, 274. [Google Scholar] [CrossRef]
- Moseley, A.M.; Rahman, P.; Wells, G.A.; Zadro, J.R.; Sherrington, C.; Toupin-April, K.; Brosseau, L. Agreement between the Cochrane risk of bias tool and Physiotherapy Evidence Database (PEDro) scale: A meta-epidemiological study of randomized controlled trials of physical therapy interventions. PLoS ONE 2019, 14, e0222770. [Google Scholar] [CrossRef] [Green Version]
- Cashin, A.G.; McAuley, J.H. Clinimetrics: Physiotherapy Evidence Database (PEDro) Scale. J. Physiother. 2020, 66, 59. [Google Scholar] [CrossRef] [PubMed]
- Borenstein, M. Comprehensive Meta-Analysis Software. In Systematic Reviews in Health Research; John Wiley & Sons: Hoboken, NJ, USA, 2022; pp. 535–548. [Google Scholar] [CrossRef]
- Brydges, C.R. Effect Size Guidelines, Sample Size Calculations, and Statistical Power in Gerontology. Innov. Aging 2019, 3, igz036. [Google Scholar] [CrossRef] [PubMed]
- West, S.L.; Gartlehner, G.; Mansfield, A.J.; Poole, C.; Tant, E.; Lenfestey, N.; Lux, L.J.; Amoozegar, J.; Morton, S.C.; Carey, T.C. Comparative Effectiveness Review Methods: Clinical Heterogeneity [Internet]; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2010.
- Willis, B.H.; Riley, R.D. Measuring the statistical validity of summary meta-analysis and meta-regression results for use in clinical practice. Stat. Med. 2017, 36, 3283–3301. [Google Scholar] [CrossRef] [Green Version]
- Duval, S.; Tweedie, R. Trim and fill: A simple funnel-plot–based method of testing and adjusting for publication bias in meta-analysis. Biometrics 2000, 56, 455–463. [Google Scholar] [CrossRef]
- Haddaway, N.R.; Page, M.J.; Pritchard, C.C.; McGuinness, L.A. PRISMA2020: An R package and Shiny app for producing PRISMA 2020—Compliant flow diagrams, with interactivity for optimised digital transparency and Open Synthesis. Campbell Syst. Rev. 2022, 18, e1230. [Google Scholar] [CrossRef]
- Goldshtrom, Y.; Knorr, G.; Goldshtrom, I. Rhythmic exercises in rehabilitation of TBI patients: A case report. J. Bodyw. Mov. Ther. 2010, 14, 336–345. [Google Scholar] [PubMed]
- Park, H.J. Exploring the use of melody during RAS gait training for adolescents with traumatic brain injury: A case study. J. Music Hum. Behav. 2015, 12, 19–36. [Google Scholar]
- Espy, D.D.; Yang, F.; Bhatt, T.; Pai, Y.C. Independent influence of gait speed and step length on stability and fall risk. Gait Posture 2010, 32, 378–382. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nascimento, L.R.; de Oliveira, C.Q.; Ada, L.; Michaelsen, S.M.; Teixeira-Salmela, L.F. Walking training with cueing of cadence improves walking speed and stride length after stroke more than walking training alone: A systematic review. J. Physiother. 2015, 61, 10–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Molinares, D.M.; Gater, D.R.; Daniel, S.; Pontee, N.L. Nontraumatic Spinal Cord Injury: Epidemiology, Etiology and Management. J. Pers. Med. 2022, 12, 1872. [Google Scholar] [CrossRef] [PubMed]
- Crasta, J.E.; Thaut, M.H.; Anderson, C.W.; Davies, P.L.; Gavin, W.J. Auditory priming improves neural synchronization in auditory-motor entrainment. Neuropsychologia 2018, 117, 102–112. [Google Scholar] [CrossRef] [PubMed]
- Alwis, D.S.; Yan, E.B.; Morganti-Kossmann, M.-C.; Rajan, R. Sensory Cortex Underpinnings of Traumatic Brain Injury Deficits. PLoS ONE 2012, 7, e52169. [Google Scholar] [CrossRef] [Green Version]
- Qaiser, T.; Eginyan, G.; Chan, F.; Lam, T. The sensorimotor effects of a lower limb proprioception training intervention in individuals with a spinal cord injury. J. Neurophysiol. 2019, 122, 2364–2371. [Google Scholar] [CrossRef]
- Beninato, M.; Fernandes, A.; Plummer, L.S. Minimal clinically important difference of the functional gait assessment in older adults. Phys. Ther. 2014, 94, 1594–1603. [Google Scholar] [CrossRef]
- Beek, P.J.; van Wieringen, P.C.W. Perspectives on the relation between information and dynamics: An epilogue. Hum. Mov. Sci. 1994, 13, 519–533. [Google Scholar] [CrossRef]
- Nutt, J.G.; Bloem, B.R.; Giladi, N.; Hallett, M.; Horak, F.B.; Nieuwboer, A. Freezing of gait: Moving forward on a mysterious clinical phenomenon. Lancet Neurol. 2011, 10, 734–744. [Google Scholar] [CrossRef] [PubMed]
- Neumann, M.; Wang, Y.; Kim, S.; Hong, S.M.; Jeng, L.; Bilgen, M.; Liu, J. Assessing gait impairment following experimental traumatic brain injury in mice. J. Neurosci. Methods 2009, 176, 34–44. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nadeau, S.; Duclos, C.; Bouyer, L.; Richards, C.L. Guiding task-oriented gait training after stroke or spinal cord injury by means of a biomechanical gait analysis. Prog. Brain Res. 2011, 192, 161–180. [Google Scholar]
- Laroche, D.P.; Cook, S.B.; Mackala, K. Strength asymmetry increases gait asymmetry and variability in older women. Med. Sci. Sport. Exerc. 2012, 44, 2172–2181. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Siponkoski, S.-T.; Koskinen, S.; Laitinen, S.; Holma, M.; Ahlfors, M.; Jordan-Kilkki, P.; Ala-Kauhaluoma, K.; Martínez-Molina, N.; Melkas, S.; Laine, M.; et al. Effects of neurological music therapy on behavioural and emotional recovery after traumatic brain injury: A randomized controlled cross-over trial. Neuropsychol. Rehabil. 2022, 32, 1356–1388. [Google Scholar] [CrossRef] [PubMed]
- Baker, F.A.; Tamplin, J.; Rickard, N.; Ponsford, J.; New, P.W.; Lee, Y.-E.C. A therapeutic songwriting intervention to promote reconstruction of self-concept and enhance well-being following brain or spinal cord injury: Pilot randomized controlled trial. Clin. Rehabil. 2019, 33, 1045–1055. [Google Scholar] [CrossRef] [PubMed]
- Siponkoski, S.-T. Music Therapy in the Cognitive and Neural Rehabilitation of Traumatic Brain Injury. Ph.D. Thesis, University of Helsinki, Helsinki, Finland, 2022. [Google Scholar]
- Zhou, Z.; Zhou, R.; Wei, W.; Luan, R.; Li, K. Effects of music-based movement therapy on motor function, balance, gait, mental health, and quality of life for patients with Parkinson’s disease: A systematic review and meta-analysis. Clin. Rehabil. 2021, 35, 937–951. [Google Scholar] [CrossRef]
- Ghai, S.; Ghai, I. Effects of (music-based) rhythmic auditory cueing training on gait and posture post-stroke: A systematic review & dose-response meta-analysis. Sci. Rep. 2019, 9, 2183. [Google Scholar] [CrossRef] [Green Version]
- Wang, L.; Peng, J.-l.; Xiang, W.; Huang, Y.-j.; Chen, A.-l. Effects of rhythmic auditory stimulation on motor function and balance ability in stroke: A systematic review and meta-analysis of clinical randomized controlled studies. Front. Neurosci. 2022, 16, 1043575. [Google Scholar] [CrossRef]
- Ghai, S.; Ghai, I.; Narciss, S. Auditory Stimulation Improves Gait and Posture in Cerebral Palsy: A Systematic Review with Between- and Within-Group Meta-Analysis. Children 2022, 9, 1752. [Google Scholar] [CrossRef]
- Schmitz, G.; Mohammadi, B.; Hammer, A.; Heldmann, M.; Samii, A.; Münte, T.F.; Effenberg, A.O. Observation of sonified movements engages a basal ganglia frontocortical network. BMC Neurosci. 2013, 14, 32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Effenberg, A.O.; Schmitz, G. Acceleration and deceleration at constant speed: Systematic modulation of motion perception by kinematic sonification. Ann. N. Y. Acad. Sci. 2018, 1425, 52–69. [Google Scholar] [CrossRef] [PubMed]


| Authors Country of Research | Sample Size (N) Gender Distribution (F, M) (Age in Years as Mean ± SD/Range) | Glasgow Coma Scale Years Since Injury | Outcomes | Training Schedule | Music Therapy (MT) Characteristics | Results |
|---|---|---|---|---|---|---|
| Thompson, Hays [63] USA | N = 10 2F, 8M (37.9 ± 15.2) | 4.1 ± 1.6 1.3 to 16.9 | Gait speed Cadence Step length Functional gait assessment 10-m walk test (meter/sec) 10-m walk test (sec) | Session length: 30 min Times per week: - Weeks: 2 Total sessions: 10 | Rhythmic click as per preferred cadence added to preferred music | Gait speed: ↑ with MT. Cadence: ↑ with MT. Step length: ↑ with MT. Functional gait assessment: ↑ with MT. 10-m walk test (meter/sec): ↑ with MT. 10-m walk test (sec): ↓ with MT. |
| Sheridan, Thaut [65] USA | N = 1 1M 42 | - - | Preferred pace, maximum pace Gait speed Cadence Step length Step time variability Step length variability Step width variability Clinical gait and balance measures 6-min walk test | Session length: 30 min Times per week: 3 Weeks: 3 | Rhythmic auditory stimulation with music recordings at a predetermined frequency | Gait speed: ↑ with MT. Cadence: No difference. Step length: ↑ with MT. Step time variability: ↓ with MT. Step length variability: ↓ with MT. Step width variability: No difference. |
| N = 1 1M 54 | Gait speed: ↓ with MT. Cadence: ↓ with MT. Step length: ↓ with MT. Step time variability: ↑ with MT. Step length variability: ↑ with MT. Step width variability: ↑ with MT. | |||||
| Park [77] South Korea | N = 1 1M (10) | - 0.6 | Gait speed Cadence Step length Stride length Step time Stride time Gait symmetry | Session length: 30 min Times per week: - Weeks: 3 Total sessions: 8 | Rhythmic harmonic stimulation at preferred cadence with music | Gait speed: ↑ with MT. Cadence: ↑ with MT. Step length: ↑ with MT on the left side, ↓ with MT. On the right side. Stride length: ↑ with MT. Step time: ↓ with MT on the left side, ↑ with MT. On the right side. Stride time: ↑ with MT. Gait symmetry (kinematic parameters of hip and knee): ↑ with MT. |
| N = 1 1F (14) | - 0.6 | Gait speed: ↑ with MT. Cadence: ↑ with MT. Step length: ↑ with MT. Stride length: ↑ with MT. Step time: ↑ with MT. Stride time: ↑ with MT. Gait symmetry (kinematic parameters of hip and knee): ↑ with MT. | ||||
| N = 1 1M (16) | - 1.1 | Gait speed: ↑ with MT. Cadence: ↑ with MT. Step length: ↑ with MT. Stride length: ↑ with MT. Step time: ↑ with MT. Stride time: ↑ with MT. Gait symmetry (kinematic parameters of hip and knee): ↑ with MT. | ||||
| Goldshtrom, Knorr [76] USA | N = 1 1F 24 | - 9 | Gait speed Cadence | Session length: - Times per week: - Weeks: - | Rhythmic exercise program with auditory cues | Gait speed: ↑ with MT. Cadence: ↑ with MT. |
| Wilfong [62] USA | N = 7 3F, 4M (34.7 ± 13.6) | - - | Gait speed Cadence Stride length | Session length: 15 min Times per week: 3 Weeks: 3 | Rhythmic auditory stimulation with a timed metronome | Gait speed: ↑ with MT. Cadence: ↑ with MT. Stride length: ↑ with MT. |
| Hurt, Rice [16] USA | N = 8 3F, 5M (30 ± 5) | - 0.3 to 2 | Normal gait, fast gait Gait speed Cadence Stride length Gait symmetry | Session length: - Times per week: - Weeks: - | Rhythmic auditory stimulation at the preferred cadence | Normal gait Gait speed: ↑ with MT. Cadence: ↑ with MT. Stride length: ↑ with MT. Gait symmetry: ↑ with MT. Fast gait Gait speed: ↓ with MT. Cadence: ↓ with MT. Stride length: ↓ with MT. Gait symmetry: ↑ with MT. |
| Session length: - Times per week: 7 Weeks: 5 | Normal gait Gait speed: ↑ with MT. Cadence: ↑ with MT. Stride length: ↑ with MT. Gait symmetry: ↑ with MT. Fast gait Gait speed: ↑ with MT. Cadence: ↑ with MT. Stride length: ↑ with MT. Gait symmetry: ↑ with MT. |
| Authors Country of Research | Sample Size (N) Gender Distribution (F, M) (Age in Years as Mean ± SD/Range) | ASIA Score Years Since Injury | Outcomes | Training Schedule | Music Therapy (MT) Characteristics | Results |
|---|---|---|---|---|---|---|
| Singhal and Kataria [61] India | MT: N = 4 4M (32.2 ± 16.8) | ASIA C: 2 ASIA D: 2 - | Gait speed Cadence Step length Walking index for spinal cord injury II | Session length: 30 min Times per week: - Weeks: 2 Total sessions: 10 | Rhythmic auditory stimulation at preferred cadence with a metronome with bodyweight supported treadmill | Gait speed: ↑ with MT. Cadence: ↑ with MT. Step length: ↑ with MT. Walking index for spinal cord injury II: ↑ with MT. |
| Ct: N = 4 4M (32 ± 4) | ASIA C: 2 ASIA D: 2 - | Bodyweight supported treadmill | Gait speed: ↑ with MT. Cadence: No difference. Step length: ↑ with MT. Walking index for spinal cord injury II: ↑ with MT. | |||
| Tamburella, Lorusso [64] Italy | N = 4 4M (35.2 ± 15.5) | ASIA D: 3 One patient not specified 0.30 to 1 | Gait speed | Session length: - Times per week: - Weeks: - Total sessions: 1 | Load-related auditory feedback (low and high pitch tones) with a crutch | Gait speed: No difference. |
| Amatachaya, Keawsutthi [60] Thailand | N = 29 7F, 22M (44 ± 15.2) | ASIA C: 4 ASIA D: 25 16 to 27 | Gait speed Stride length Cadence Step symmetry | Session length: - Times per week: - Weeks: - | Rhythmic auditory stimulation with metronome 25% faster than preferred cadence | Gait speed: ↑ with MT. Stride length: No difference. Cadence: ↑ with MT. Step symmetry: ↑ with MT. |
| de l’Etoile [66] USA | N = 17 4F, 13M (41) | - 5.8 ± 4.8 | Gait speed Cadence Stride length | Session length: - Times per week: - Weeks: - | Rhythmic auditory stimulation at the preferred cadence | Gait speed: ↓ with MT. Cadence: ↓ with MT. Stride length: ↑ with MT. |
| Rhythmic auditory stimulation at 5% faster than normal cadence | Gait speed: ↓ with MT. Cadence: ↓ with MT. Stride length: ↓ with MT. |
| Overall Score | Point Estimates and Variability | Random Allocation | Between-Group Comparison | Intention to Treat | Blinded Subjects | Adequate Follow-Up | Blinded Assessors | Blinded Therapists | Baseline Comparability | Concealed Allocation | Eligibility Criteria | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Singhal and Kataria [61] | 6 | + | + | + | + | - | - | - | - | + | - | + |
| Tamburella, Lorusso [64] | 5 | + | - | + | + | - | - | - | - | + | - | + |
| Thompson, Hays [63] | 5 | + | - | + | + | - | - | - | - | + | - | + |
| Sheridan, Thaut [65] | 4 | + | - | + | + | - | - | - | - | - | - | + |
| Park [77] | 4 | + | - | + | + | - | - | - | - | - | - | + |
| Goldshtrom, Knorr [76] | 4 | + | - | + | + | - | - | - | - | - | - | + |
| Amatachaya, Keawsutthi [60] | 5 | + | + | + | + | - | - | - | - | - | - | + |
| Wilfong [62] | 5 | + | + | + | + | - | - | - | - | - | - | + |
| de l’Etoile [66] | 6 | + | + | + | + | - | - | + | - | - | - | + |
| Hurt, Rice [16] | 5 | + | + | + | + | - | - | - | - | - | - | + |
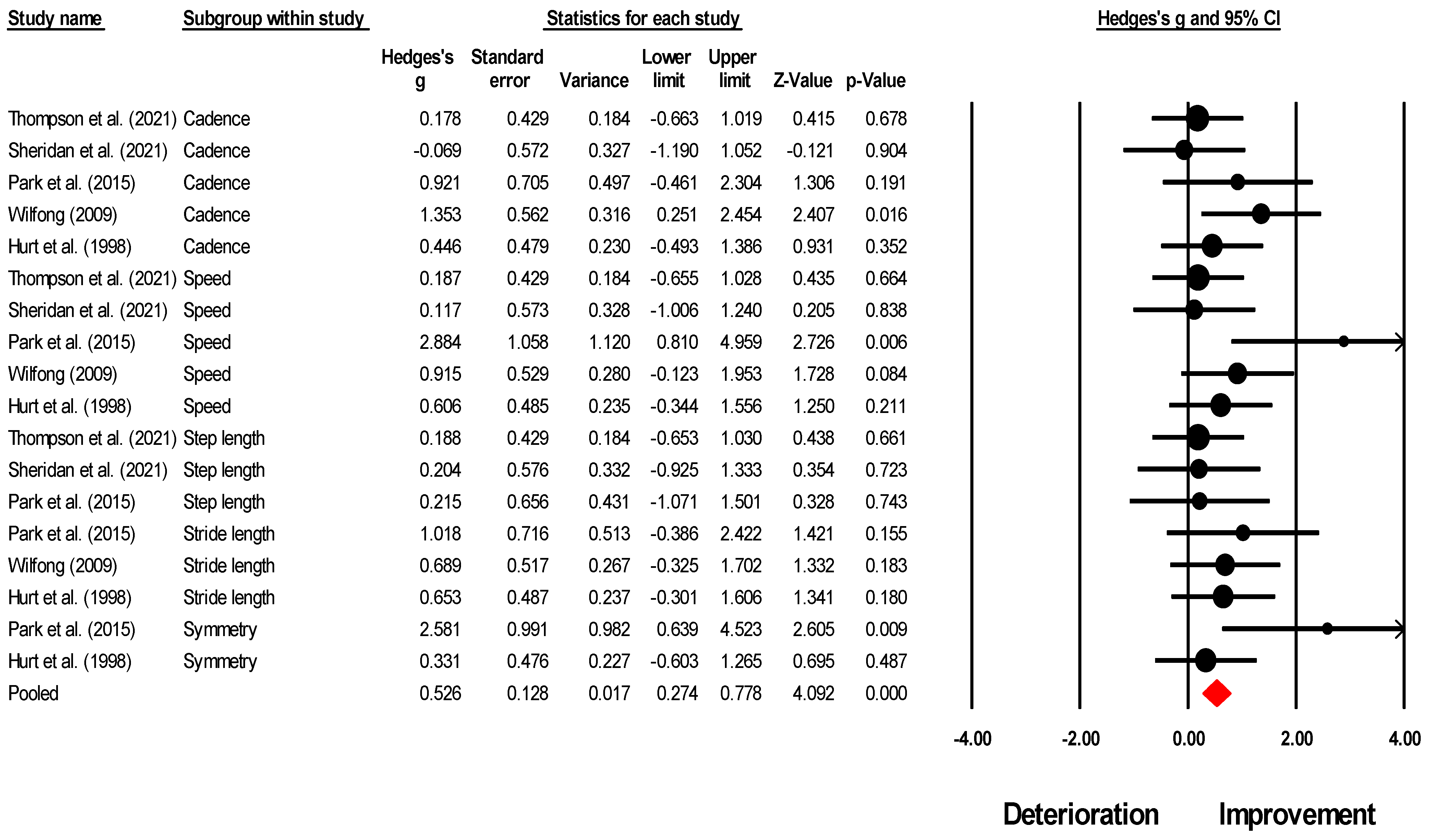
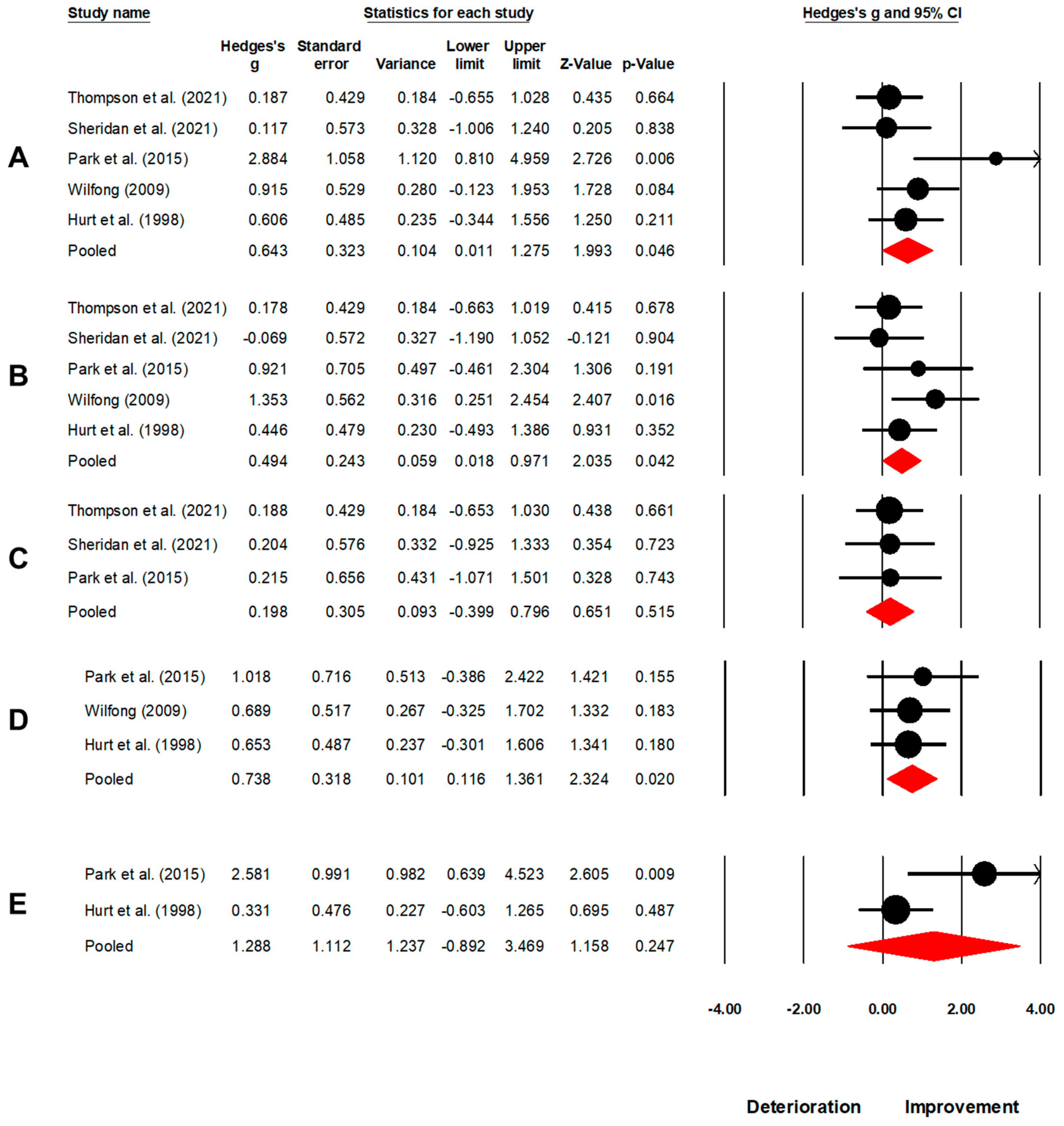
| Number | Outcome | Number of Studies Included in the Analysis; (References) | Meta-Analysis Result Hedge’s g, 95% C.I., p-Value | Heterogeneity I2 Stastistics | Figure Number |
|---|---|---|---|---|---|
| 1. | Overall spatiotemporal outcomes | N = 5; [16,62,63,65,77] | 0.52, 0.27 to 0.77, p < 0.001 | 1% | Figure 4 |
| 2. | Gait speed | N = 5; [16,62,63,65,77] | 0.64, 0.01 to 1.27, p = 0.046 | 40% | Figure 5A |
| 3. | Cadence | N = 5; [16,62,63,65,77] | 0.49, 0.01 to 0.97, p = 0.042 | 5% | Figure 5B |
| 4. | Step length | N = 3; [63,65,77] | 0.19, −0.40 to 0.79, p = 0.515 | 0% | Figure 5C |
| 5. | Stride length | N = 3; [16,62,77] | 0.73, 0.11 to 1.36, p = 0.020 | 0% | Figure 5D |
| 6. | Gait symmetry | N = 2; [16,77] | 1.28, −0.89 to 3.46, p = 0.247 | 0% | Figure 5E |
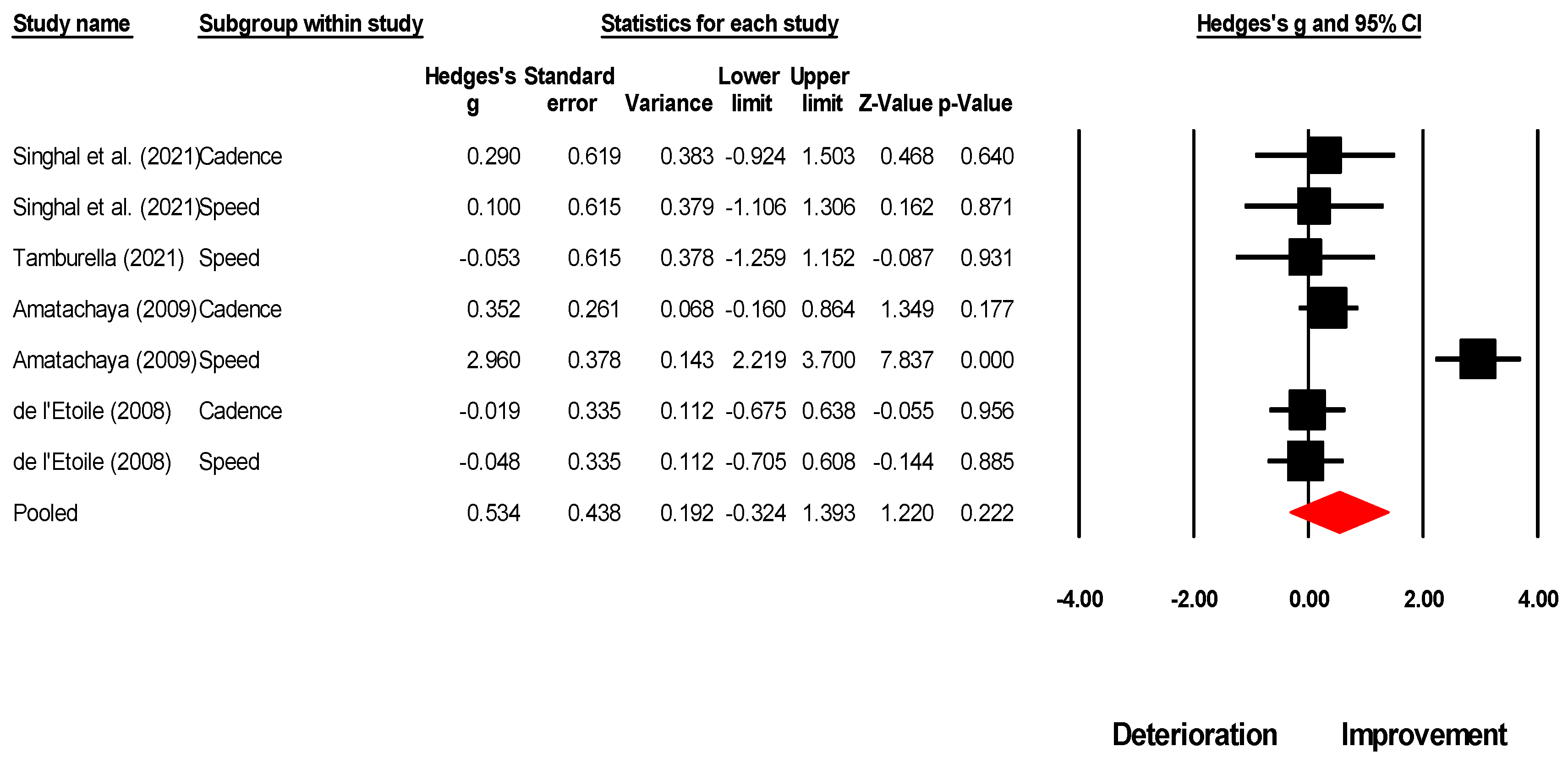
| Number | Outcome | Number of Studies Included in the Analysis; (References) | Meta-Analysis Result Hedge’s g, 95% C.I., p-Value | Heterogeneity I2 Stastistics | Figure Number |
|---|---|---|---|---|---|
| 1. | Overall spatiotemporal outcomes | N = 4; [60,61,64,66] | 0.534, −0.32 to 1.39, p = 0.222 | 88% | Figure 6 |
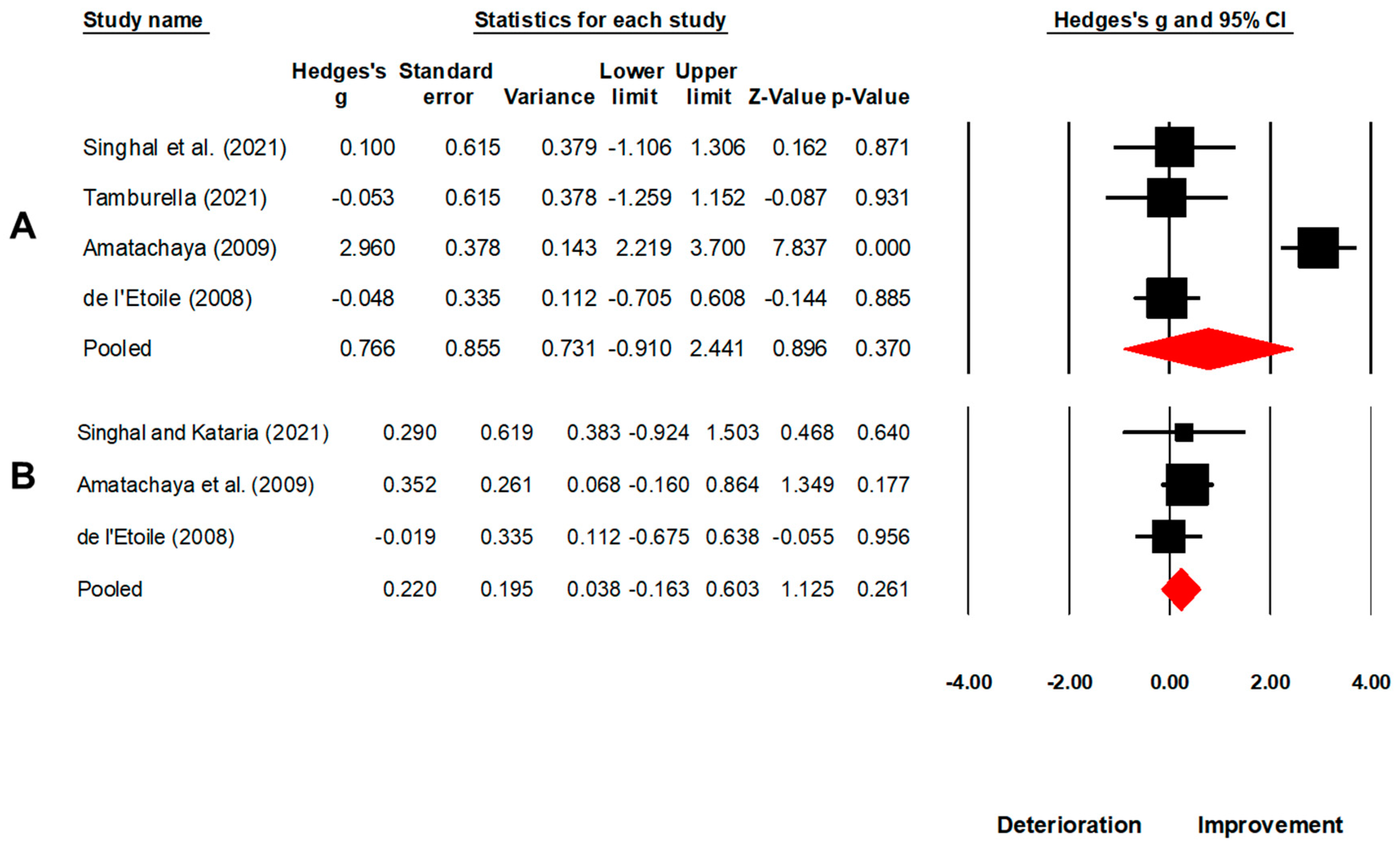
| 2. | Gait speed | N = 4; [60,61,64,66] | 0.76, −0.91 to 2.44, p = 0.370 | 93% | Figure 7A |
| 3. | Cadence | N = 3; [60,61,66] | 0.22, −0.16 to 0.60, p = 0.260 | 0% | Figure 7B |
| 4. | Step length | N = 1; [61] | - | - | - |
| 5. | Stride length | - | - | - | - |
| 6. | Gait symmetry | - | - | - | - |
| Number | Analysis | Meta-Analysis p-Value | I2 | Studies Impacting p-Value upon Removal | p-Value upon Removal | Figure |
|---|---|---|---|---|---|---|
| Traumatic brain injury | ||||||
| 1. | Overall spatiotemporal outcomes | <0.001 | 1% | No effect | - | Figure S1 |
| 2. | Gait speed | 0.046 | 40% | Park [77] Wilfong [62] Hurt, Rice [16] | 0.074 0.139 0.104 | Figure S2 |
| 3. | Cadence | 0.042 | 5% | Park [77] Wilfong [62] Hurt, Rice [16] | 0.116 0.238 0.103 | Figure S3 |
| 4. | Step length | 0.515 | 0% | - | - | - |
| 5. | Stride length | 0.020 | 0% | - | - | - |
| 6. | Gait symmetry | 0.247 | 0% | - | - | - |
| Spinal cord injury | ||||||
| 7. | Overall spatiotemporal outcomes | 0.222 | 88% | No effect | - | Figure S4 |
| 8. | Gait speed | 0.370 | 93% | No effect * | - | Figure S5 |
| 9. | Cadence | 0.220 | 0% | - | - | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ghai, S. Does Music Therapy Improve Gait after Traumatic Brain Injury and Spinal Cord Injury? A Mini Systematic Review and Meta-Analysis. Brain Sci. 2023, 13, 522. https://doi.org/10.3390/brainsci13030522
Ghai S. Does Music Therapy Improve Gait after Traumatic Brain Injury and Spinal Cord Injury? A Mini Systematic Review and Meta-Analysis. Brain Sciences. 2023; 13(3):522. https://doi.org/10.3390/brainsci13030522
Chicago/Turabian StyleGhai, Shashank. 2023. "Does Music Therapy Improve Gait after Traumatic Brain Injury and Spinal Cord Injury? A Mini Systematic Review and Meta-Analysis" Brain Sciences 13, no. 3: 522. https://doi.org/10.3390/brainsci13030522
APA StyleGhai, S. (2023). Does Music Therapy Improve Gait after Traumatic Brain Injury and Spinal Cord Injury? A Mini Systematic Review and Meta-Analysis. Brain Sciences, 13(3), 522. https://doi.org/10.3390/brainsci13030522






