“Corp-Osa-Mente”, a Combined Psychosocial–Neuropsychological Intervention for Adolescents and Young Adults with Fragile X Syndrome: An Explorative Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Implementation of “Corposamente”
2.3. Treatment Aims Procedures and Settings
- Increase participants’ knowledge about FXS, its symptomatology and its management.
- Provide information about adolescence, transition to adulthood and sexuality issues.
- Help participants to manage their negative emotions, especially anxiety.
- Promote the development of new autonomies, mostly in the community.
- Improve the socio-pragmatic skills and the ability to relate with the group of peers.
- Improve cognitive abilities, with a particular focus on EF.
- Positive reinforcement, consisting in a reward/praise that was provided in order to encourage positive behaviors.
- Antecedent-based Interventions, focused on the modification of the environment to reduce the likelihood that something in the environment could trigger an interfering behavior.
- Extinction, consisting mostly in ignoring dysfunctional behaviors. When one participant exhibited a dysfunctional behavior, the entire group was coached not to pay attention to it.
- Modelling and Shaping, in order to reward the desired behavior.
- Mindfulness Techniques and physical exercise, in order to help participants to calm down and to manage their negative emotions.
- Neuropsychological intervention that aimed to train visual attention, different components of EF, perspective memory, receptive, written and expressive language. Material was adapted to each participant’s cognitive level, with the difficulty of the tasks growing session to session. At the end of every session, the psychologist assigned cognitive homework to be completed before the next meeting. Tasks were extracted and adapted by the book “Una palestra per la mente” [22]. Other exercises were directly designed by the psychologist based on her neuropsychological experience.
- Occupational intervention, aimed to engage participants in meaningful activities of daily life. Activities included tasks of counting money and change, grocery stores and bars simulations, role playing activities to learn to start and maintain conversations with peers, etc. Occupational intervention focused mostly on Socialization and Community living.
3. Results
3.1. Sample Description in March 2020, at Time of Recruitment
3.2. Sample Description in September 2022, at the End of the Intervention
3.3. The Survey
3.4. Descriptive Analysis of the Survey
3.4.1. Treatment Satisfaction
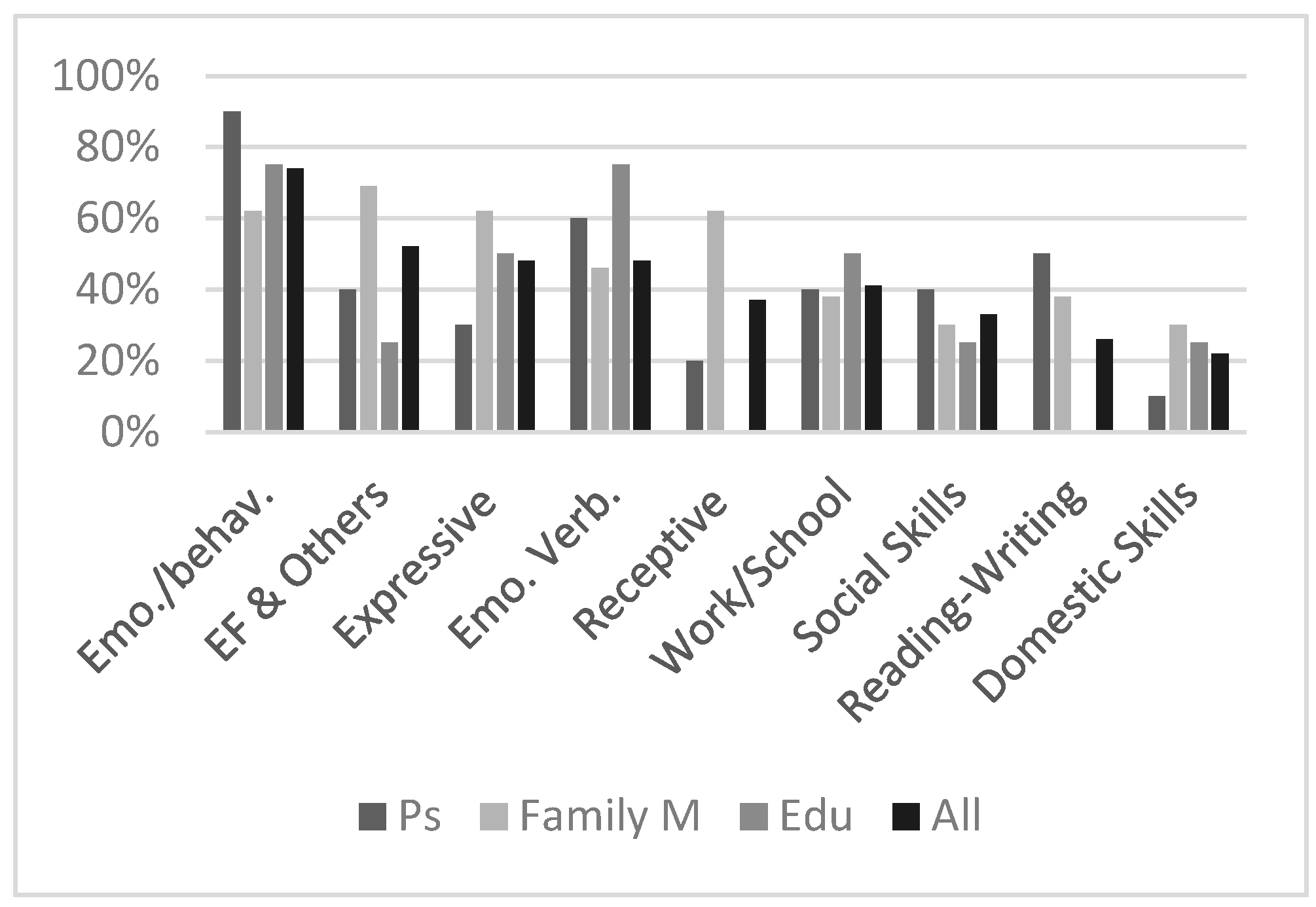
3.4.2. Areas of Improvement
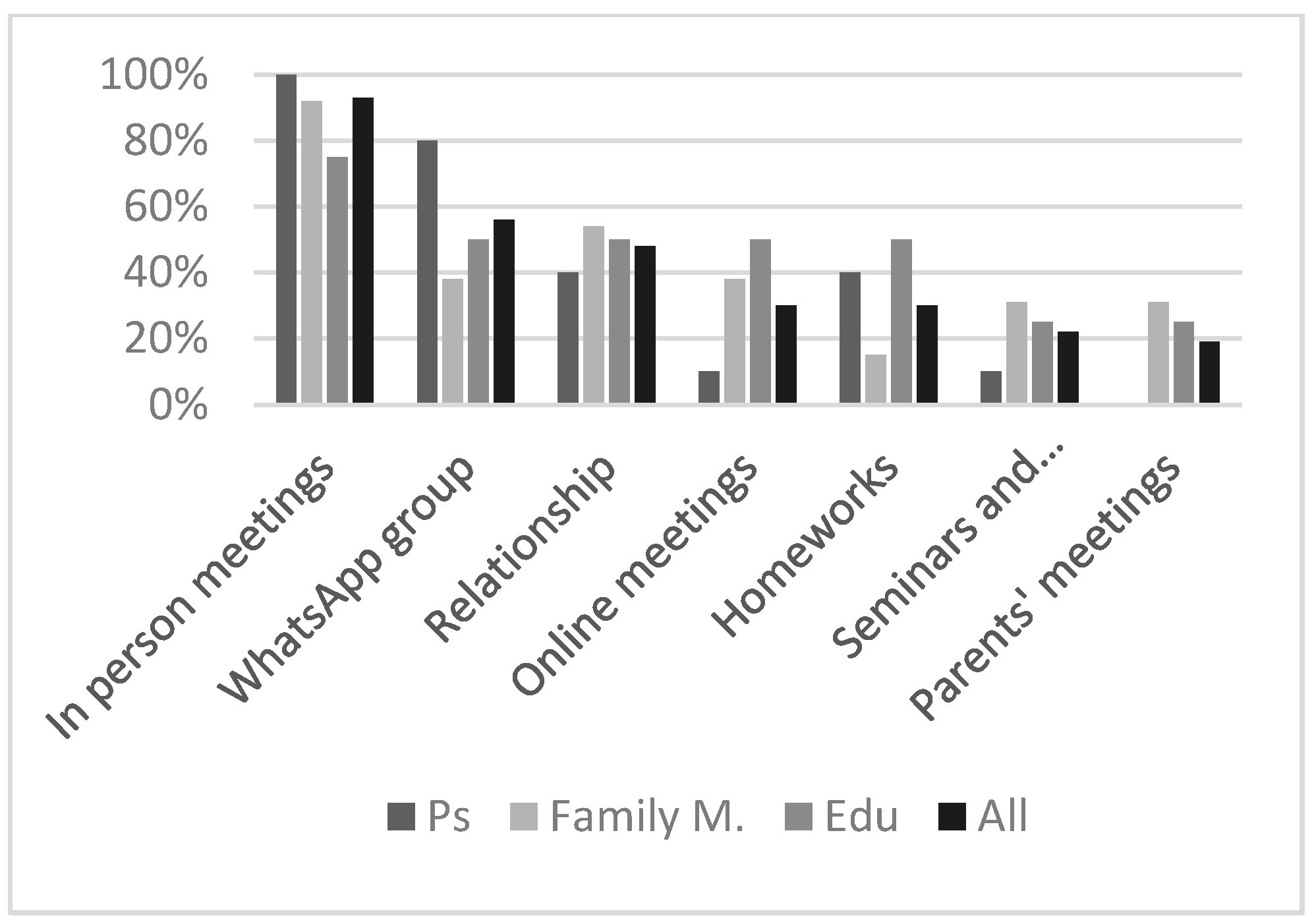
3.4.3. The Most Preferred Aspects of the Intervention
3.4.4. The Techniques Considered the Most Effective
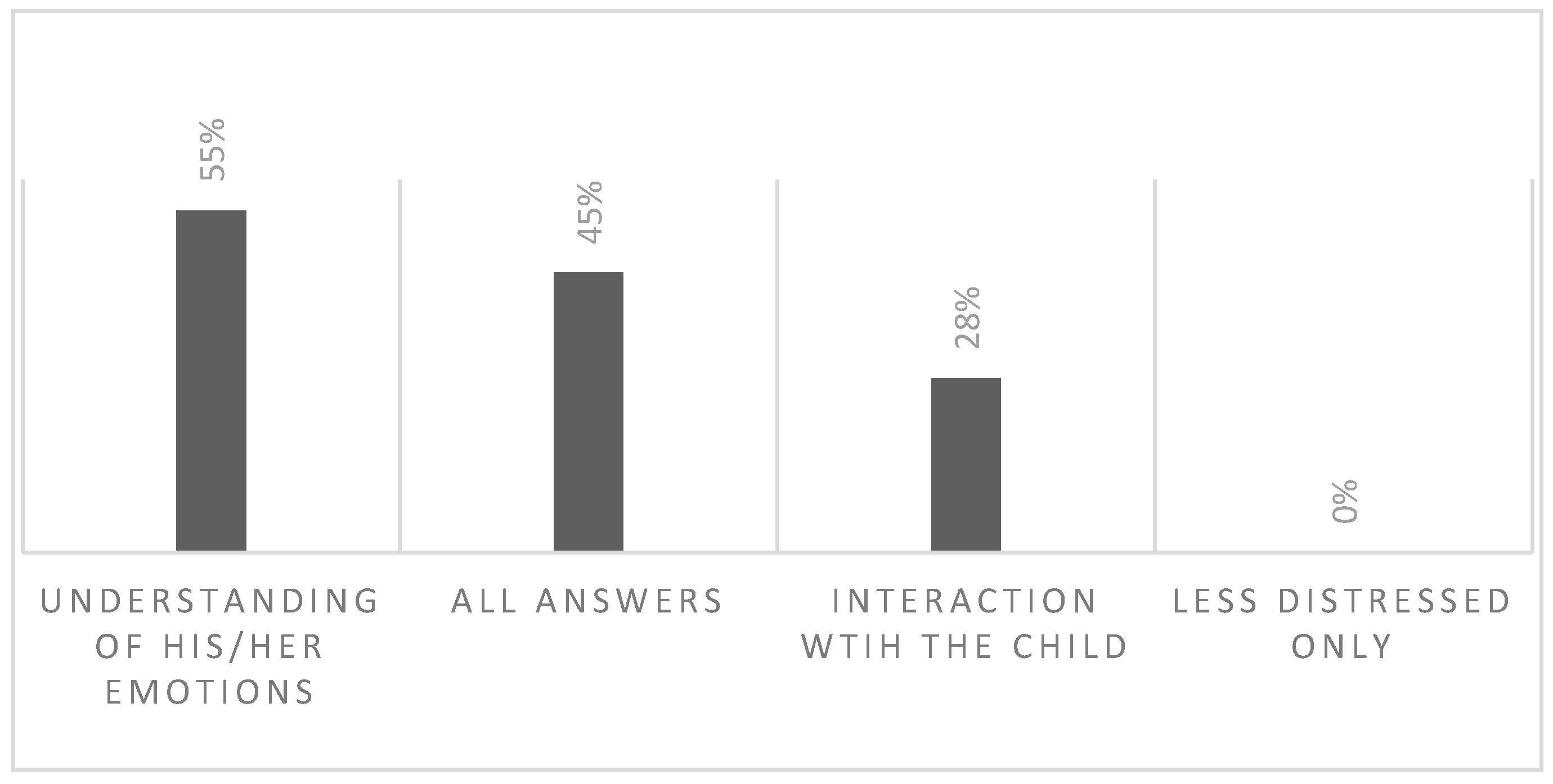
3.4.5. Family Members Only
3.4.6. Educators Only
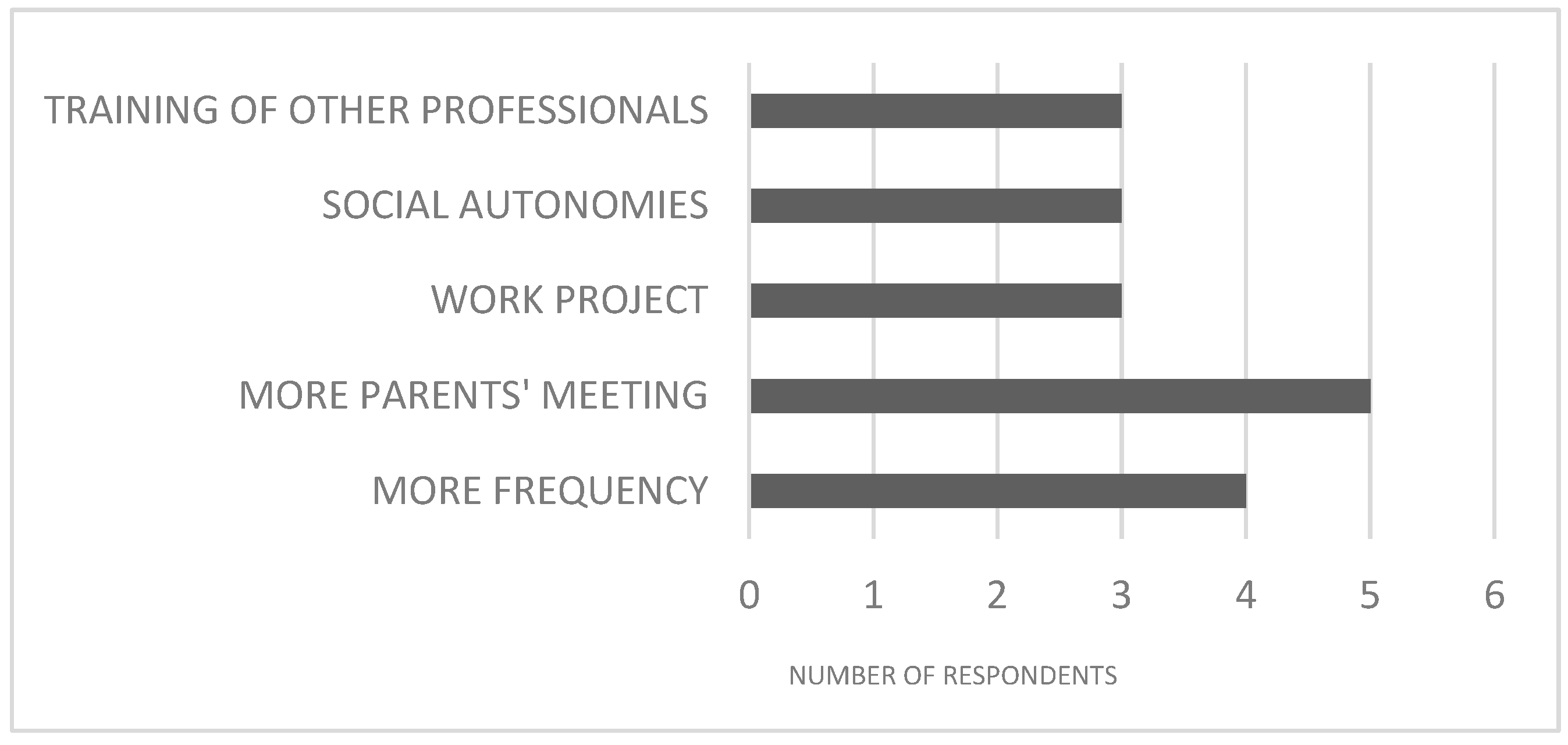
3.4.7. Some Suggestions
4. Discussion
5. Limitations, Future Directions and Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Smith, L.E.; Barker, E.T.; Seltzer, M.M.; Abbeduto, L.; Greenberg, J.S. Behavioral phenotype of fragile X syndrome in adolescence and adulthood. Am. J. Intellect. Dev. Disabil. 2012, 117, 1–17. [Google Scholar] [CrossRef]
- Saldarriaga, W.; Tassone, F.; González-Teshima, L.Y.; Forero-Forero, J.V.; Ayala-Zapata, S.; Hagerman, R. Fragile X syndrome. Colomb. Med. 2014, 45, 190–198. [Google Scholar]
- Salcedo-Arellano, M.J.; Hagerman, R.J.; Martínez-Cerdeño, V. Fragile X syndrome: Clinical presentation, pathology and treatment. Síndrome X frágil: Presentación clínica, patología y tratamiento. Gac. Med. Mex. 2020, 156, 60–66. [Google Scholar] [CrossRef]
- Willemsen, R.; Levenga, J.; Oostra, B.A. CGG repeat in the FMR1 gene: Size matters. Clin. Genet. 2011, 80, 214–225. [Google Scholar] [CrossRef]
- Hagerman, P.J.; Hagerman, R. Fragile X syndrome. Curr. Biol. CB 2021, 31, R273–R275. [Google Scholar] [CrossRef]
- Protic, D.; Salcedo-Arellano, M.J.; Dy, J.B.; Potter, L.A.; Hagerman, R.J. New Targeted Treatments for Fragile X Syndrome. Curr. Pediatr. Rev. 2019, 15, 251–258. [Google Scholar] [CrossRef]
- Roberts, J.E.; Mankowski, J.B.; Sideris, J.; Goldman, B.D.; Hatton, D.D.; Mirrett, P.L.; Baranek, G.T.; Reznick, J.S.; Long, A.C.; Bailey, D.B., Jr. Trajectories and predictors of the development of very young boys with fragile X syndrome. J. Pediatr. Psychol. 2009, 34, 827–836. [Google Scholar] [CrossRef]
- Schmitt, L.M.; Shaffer, R.C.; Hessl, D.; Erickson, C. Executive Function in Fragile X Syndrome: A Systematic Review. Brain Sci. 2019, 9, 15. [Google Scholar] [CrossRef]
- Garber, K.B.; Visootsak, J.; Warren, S.T. Fragile X syndrome. Eur. J. Hum. Genet. EJHG 2008, 16, 666–672. [Google Scholar] [CrossRef]
- Hagerman, R.J.; Berry-Kravis, E.; Kaufmann, W.E.; Ono, M.Y.; Tartaglia, N.; Lachiewicz, A.; Kronk, R.; Delahunty, C.; Hessl, D.; Visootsak, J.; et al. Advances in the treatment of fragile X syndrome. Pediatrics 2009, 123, 378–390. [Google Scholar] [CrossRef]
- Klaiman, C.; Quintin, E.M.; Jo, B.; Lightbody, A.A.; Hazlett, H.C.; Piven, J.; Hall, S.S.; Chromik, L.C.; Reiss, A.L. Longitudinal profiles of adaptive behavior in fragile X syndrome. Pediatrics 2014, 134, 315–324. [Google Scholar] [CrossRef] [PubMed]
- Wiegers, A.M.; Curfs, L.M.; Vermeer, E.L.; Fryns, J.P. Adaptive behavior in the fragile X syndrome: Profile and development. Am. J. Med. Genet. 1993, 47, 216–220. [Google Scholar] [CrossRef] [PubMed]
- Hahn, L.J.; Brady, N.C.; Warren, S.F.; Fleming, K.K. Do Children with Fragile X Syndrome Show Declines or Plateaus in Adaptive Behavior? Am. J. Intellect. Dev. Disabil. 2015, 120, 412–432. [Google Scholar] [CrossRef]
- Weber, J.D.; Smith, E.; Berry-Kravis, E.; Cadavid, D.; Hessl, D.; Erickson, C. Voice of People with Fragile X Syndrome and Their Families: Reports from a Survey on Treatment Priorities. Brain Sci. 2019, 9, 18. [Google Scholar] [CrossRef] [PubMed]
- Hessl, D.; Dyer-Friedman, J.; Glaser, B.; Wisbeck, J.; Barajas, R.G.; Taylor, A.; Reiss, A.L. The influence of environmental and genetic factors on behavior problems and autistic symptoms in boys and girls with fragile X syndrome. Pediatrics 2001, 108, e88. [Google Scholar] [CrossRef]
- Moskowitz, L.J.; Jones, E.A. Uncovering the evidence for behavioral interventions with individuals with fragile X syndrome: A systematic review. Res. Dev. Disabil. 2015, 38, 223–241. [Google Scholar] [CrossRef] [PubMed]
- Vismara, L.A.; McCormick, C.E.; Shields, R.; Hessl, D. Extending the parent-delivered Early Start Denver Model to young children with fragile X syndrome. J. Autism Dev. Disord. 2019, 49, 1250–1266. [Google Scholar] [CrossRef]
- Kaufmann, W.E.; Kidd, S.A.; Andrews, H.F.; Budimirovic, D.B.; Esler, A.; Haas-Givler, B.; Stackhouse, T.; Riley, C.; Peacock, G.; Sherman, S.L.; et al. Autism spectrum disorder in fragile X syndrome: Cooccurring conditions and current treatment. Pediatrics 2017, 139 (Suppl. S3), S194–S206. [Google Scholar] [CrossRef]
- Ellis, A.; Gaines, C. Rational-Emotive Therapy; Big Sur Recordings: Milano, Italy, 1973; pp. 32–44. [Google Scholar]
- Di Pietro, M. L’ABC Delle mie Emozioni-8-13 Anni: Programma di Alfabetizzazione Socio-Affettiva Secondo il Metodo REBT; Edizioni Centro Studi Erickson: Trento, Italy, 2020. [Google Scholar]
- Ricci, C.; Magaudda, C.; Carradori, G.; Bellifemine, D.; Romeo, A. Il Manuale ABA-VB-Applied Behavior Analysis and Verbal Behavior: Fondamenti, Tecniche e Programmi di Intervento; Edizioni Centro Studi Erickson: Trento, Italy, 2014. [Google Scholar]
- Gollin, D.; Ferrari, A.; Peruzzi, A. Book: Una Palestra per la Mente; Erickson: Trento, Italy, 2011. [Google Scholar]
- Marmarosh, C.; Holtz, A.; Schottenbauer, M. Group cohesiveness, group-derived collective self-esteem, group-derived hope, and the well-being of group therapy members. Group Dyn. Theory Res. Pract. 2005, 9, 32. [Google Scholar] [CrossRef]
- Sukhodolsky, D.G.; Butter, E.M. Social skills training for children with intellectual disabilities. In Handbook of Intellectual and Developmental Disabilities; Springer: Boston, MA, USA, 2007; pp. 601–618. [Google Scholar]
- Adibsereshki, N.; Abkenar, S.J.; Ashoori, M.; Mirzamani, M. The effectiveness of using reinforcements in the classroom on the academic achievement of students with intellectual disabilities. J. Intellect. Disabil. 2015, 19, 83–93. [Google Scholar] [CrossRef]
- Suveg, C.; Sood, E.; Comer, J.S.; Kendall, P.C. Changes in emotion regulation following cognitive-behavioral therapy for anxious youth. J. Clin. Child Adolesc. Psychol. 2009, 38, 390–401. [Google Scholar] [CrossRef]
- Cooney, P.; Jackman, C.; Coyle, D.; O’Reilly, G. Computerised cognitive–behavioural therapy for adults with intellectual disability: Randomised controlled trial. Br. J. Psychiatry 2017, 211, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Blakeley-Smith, A.; Meyer, A.T.; Boles, R.E.; Reaven, J. Group Cognitive Behavioural Treatment for Anxiety in Autistic Adolescents with Intellectual Disability: A Pilot and Feasibility Study. J. Appl. Res. Intellect. Disabil. JARID 2021, 34, 777–788. [Google Scholar] [CrossRef] [PubMed]
- Hessl, D.; Schweitzer, J.B.; Nguyen, D.V.; McLennan, Y.A.; Johnston, C.; Shickman, R.; Chen, Y. Cognitive training for children and adolescents with fragile X syndrome: A randomized controlled trial of Cogmed. J. Neurodev. Disord. 2019, 11, 4. [Google Scholar] [CrossRef] [PubMed]
- Monlux, K.D.; Pollard, J.S.; Bujanda Rodriguez, A.Y.; Hall, S.S. Telehealth Delivery of Function-Based Behavioral Treatment for Problem Behaviors Exhibited by Boys with Fragile X Syndrome. J. Autism Dev. Disord. 2019, 49, 2461–2475. [Google Scholar] [CrossRef]
- Hällgren, M.; Kottorp, A. Effects of occupational therapy intervention on activities of daily living and awareness of disability in persons with intellectual disabilities. Aust. Occup. Ther. J. 2005, 52, 350–359. [Google Scholar] [CrossRef]
- Braden, M. The effect of fragile X syndrome on learning. In Educating Children with Fragile X: A Multi-Professional Handbook; Dew-Hughes, D., Ed.; Routledge: Oxford, UK, 2003; pp. 43–47. [Google Scholar]
- McLennan, Y.; Polussa, J.; Tassone, F.; Hagerman, R. Fragile x syndrome. Curr. Genom. 2011, 12, 216–224. [Google Scholar] [CrossRef]
- Douds, F.; McKechanie, A.; Simpson, Y.; Murphy, L. “Staying Well”: A psychoeducational group for people with an intellectual disability, co-morbid mental illness and offending behaviour. J. Intellect. Disabil. Offending Behav. 2014, 5, 54–59. [Google Scholar] [CrossRef]
- Leaf, J.B.; Cihon, J.H.; Leaf, R.; McEachin, J.; Liu, N.; Russell, N.; Unumb, L.; Shapiro, S.; Khosrowshahi, D. Concerns About ABA-Based Intervention: An Evaluation and Recommendations. J. Autism Dev. Disord. 2022, 52, 2838–2853. [Google Scholar] [CrossRef]
- Kim, J.M.; Mahoney, G. The effects of relationship focused intervention on Korean parents and their young children with disabilities. Res. Dev. Disabil. 2005, 26, 117–130. [Google Scholar] [CrossRef]
- Alfieri, P.; Scibelli, F.; Casula, L.; Piga, S.; Napoli, E.; Valeri, G.; Vicari, S. Cooperative Parent-Mediated Therapy in Children with Fragile X Syndrome and Williams Beuren Syndrome: A Pilot RCT Study of a Transdiagnostic Intervention-Preliminary Data. Brain Sci. 2021, 12, 8. [Google Scholar] [CrossRef]
- Luu, S.; Province, H.; Berry-Kravis, E.; Hagerman, R.; Hessl, D.; Vaidya, D.; Lozano, R.; Rosselot, H.; Erickson, C.; Kaufmann, W.E.; et al. Response to Placebo in Fragile X Syndrome Clinical Trials: An Initial Analysis. Brain Sci. 2020, 10, 629. [Google Scholar] [CrossRef] [PubMed]



| Participant’s Number Code | Gender | Age at Recruitment (Years, Months) |
|---|---|---|
| 1 | Female | 26.9 |
| 2 | Female | 20.9 |
| 3 | Female | 24.9 |
| 4 | Male | 30.1 |
| 5 | Male | 17.9 |
| 6 | Male | 16.3 |
| 7 | Male | 21.5 |
| 8 | Male | 27.7 |
| 9 | Male | 20.4 |
| 10 | Male | 28.1 |
| Total | M 24.3 SD 4.2 MED 24.9 RANGE 16.3–30.1 |
| Participant’s Number Code | Gender | ID Level | Personal Assistant/ Educator | School/Work | Descriptive Information of Adaptive Behavior |
|---|---|---|---|---|---|
| 1 | Female | Moderate ID | Yes | No occupation | Communication: Can understand complex instructions (receptive skills). Can talk about everyday experiences and clarify to other people what she is thinking or doing (expressive skills). Can pay attention to a 30-min informational talk. Can understand alphabetical order. Can write one-page papers, but with different grammatical errors. Daily living Skills: Very dependent from her family. Can assist in food preparation. Can take care of herself, but she cannot remain alone at home. Socialization: Strong social difficulties and social inhibition. Behavior: Social anxiety traits. She can be very fearful of common situations. |
| 2 | Female | Mild ID | Yes | Work in her father’s company | Communication: Can understand complex instructions (receptive skills). Can talk about everyday experiences and clarify to other people what she is thinking or doing (expressive skills). Can pay attention to a 30-min informational talk. Can understand basic sarcasm. Can understand alphabetical order. Can write one-page papers, but with different grammatical errors. Daily living Skills: Can take means of transports alone. Can cook and do the laundry. Can take care of herself and of her brother. Socialization: Severe social difficulties, manipulating behavior with peers and family. Behavior: Can have crises for no clear reason. Can feel helpless. Can destroy her own objects when nervous. This happens at least twice/week and represents a problem for family and peers. On parents’ perspective, these crises represent the main issue. |
| 3 | Female | Mild ID | Yes | University student (Individualized Education Program—IEP) | Communication: Can understand complex instructions (receptive skills). Can talk about everyday experiences and clarify to other people what she is thinking or doing (expressive skills). Can pay attention to a 30-min informational talk. Can understand basic sarcasm. Can understand alphabetical order. Can write papers that are three pages or more, but with some grammatical errors. Can read at a sixth-grade level. Daily living skills: Can take means of transports alone. Can assist in food preparation and prepare simple food (i.e., a sandwich) without support. Socialization: Important social difficulties, manipulating behavior with peers. Behavior: Can sometimes worry for no clear reason. Can have crises if she is not the focus of attention (around once/week). This behavior represents a problem for peers, but not for her family. |
| 4 | Male | Severe ID | Yes | No occupation | Communication: Receptive and expressive skills strongly impaired, but receptive language is more preserved. Can pay attention to a story for less than 15 min. Can write his name and some basic words. Daily living skills: Can prepare very simple food under supervision. In other activities, total support is required. Socialization: Social drive is present, but with difficulties in understanding social rules. Behavior: Can get fixated on topics. Cannot distinguish between negative emotions. |
| 5 | Male | Moderate ID | No | High school student (Individualized Education Program—IEP) | Communication: Can understand complex instructions (receptive skills). Can talk about everyday experiences and clarify to other people what he is thinking or doing (expressive skills). Can pay attention to a 15-min informational talk. Can write one-page papers, but with different grammatical errors. Daily living skills: Can take means of transports alone. Can go out with friends and arrange meetings. Can assist in food preparation. Socialization: Strong social drive. Some difficulties in respecting social rules. Behavior: ADHD traits. Can be irritable and impulsive. Can verbally bully other people or is verbally abusive (at least twice a week). This represents a problem for his parents as this symptom creates obstacles for school and social functioning. |
| 6 | Male | Severe ID | Yes | High school student (Individualized Education Program—IEP) | Communication: Receptive skills are more preserved than expressive and written. Can produce basic sentences. Can write his name and other few words. Can pay attention for less than 15 min. Daily living skills: Can prepare very simple food under supervision. Socialization: Social drive is present, but with difficulties in understanding social rules. Behavior: Can get fixated on topics. Cannot distinguish between negative emotions. |
| 7 | Male | Severe ID | Yes | No occupation | Communication: Very basic expressive, receptive and written skills. Can produce basic sentences and understand very simple instructions. Can pay attention for around 15 min. Daily living skills: Basic personal and domestic functioning (i.e., can take a shower alone). Can assist in food preparation but needs some support. Can go to the supermarket, buying just one piece at time. Socialization: Strong social drive but shows difficulties in peers’ relationships. Behavior: Can sometimes be verbally abusive with friends and parents (less than once a week), however this symptom does not represent a problem both for parents and friends. |
| 8 | Male | Severe ID | Yes | Work in his aunt’s company | Communication: Receptive skills more preserved than expressive and written. Can understand basic instructions and produce basic sentences. Can pay attention for around 15 min. Daily living skills: Can assist in food preparation but needs some support. Can take means of transports alone. Socialization: Strong social drive, but difficulties in peers’ relationships. Behavior: Can sometimes be verbally abusive with friends and parents (less than once/week and only when very distressed). This does not represent a problem for his family and friends. |
| 9 | Male | Mild ID | No | No occupation | Communication Can understand complex instructions (receptive skills). Can talk about everyday experiences and clarify to other people what he is thinking or doing (expressive skills), can understand sarcasm and reads at a sixth-grade level. Can produce papers that are three or more pages long. Can pay attention to a 30-min informational talk. Daily living skills: Can cook, can go to the supermarket and can take means of transports alone. Socialization: Important social problems. Social avoidance can be present. Behavior: Can sometimes be sad for no clear reason and feel hopeless (around once/week). This doesn’t seem to represent a problem for his family. |
| 10 | Male | Mild ID | No | Work with regular contract in a restaurant | Communication: Can understand complex instructions (receptive skills). Can talk about everyday experiences and clarify to other people what he is thinking or doing (expressive skills), can understand sarcasm and reads at a sixth-grade level. Can produce papers that are three or more pages long. Can pay attention to a 30-min informational talk. Daily living skills: Can cook and take care of himself. Can take means of transport alone. Socialization: Strong social problems. He doesn’t have friends. Behavior: Can sometimes get fixated on topics and situations (less than once/week). |
| Participant’s Number Code | Gender | School/Work | Descriptive Information of Adaptive Behavior |
|---|---|---|---|
| 1 | Female | University student (Individualized Education Program—IEP) | Communication: Can understand complex instructions (receptive skills). Can tell about everyday experiences and clarify to other people what she is thinking or doing (expressive skills). Can understand basic irony and write papers that are at least three pages long, even though she can still make some grammar mistakes. Daily living skills: Can go out alone. Can go to the supermarket and cook her own food. Can go to university (in another city) with the support of an educator. Can use money and credit card. Less dependent from her family. Socialization: Still no close friends but can sometimes go to a community center. Behavior: Social anxiety traits are still present, but she is less fearful. Can control her anxiety and approach to novel situations. |
| 2 | Female | Work in her father’s company. | Communication: Can understand complex instructions (receptive skills). Can tell about everyday experiences and clarify to other people what she is thinking or doing (expressive skills). Can pay attention to a 30-min informational talk. Can understand basic sarcasm. Can write two-page papers, but with different grammatical errors. Can speak basic English after having attended a course. Daily living skills: Can take means of transports alone. Can manage own money without assistance. Can perform routine household care. Socialization: Still severe social difficulties and dramatic behavior. Behavior: Frequency of crises did not decrease, but now she can recognize triggers to anxiety and behavioral problems. With the help of the psychologist or the educator, can modify irrational thinking and avoid some dysfunctional behaviors. Parents tell to be less distressed as now they know how to manage this behavior. |
| 3 | Female | Bachelor’s degree. Masters’ university student. (Individualized Education Program—IEP) | Communication: Can understand complex instructions (receptive skills). Can tell about everyday experiences and clarify to other people what she is thinking or doing (expressive skills). Can makes plans and communicate them to other people. Can pay attention to a 30-min informational talk. Can understand basic sarcasm and be ironic. Can write papers that are three pages or more, but still with some grammatical errors. Can read at a sixth-grade level or more. Daily living skills: Can cook food without assistance. Can take means of transports alone and manage her time independently. Can perform routine household care, with some practical support. She needs help in managing money. Socialization: Some social difficulties mostly in peers’ relationships and theatrical behavior. In a romantic relationship. Behavior: Can still worry for no reason but can accept not to be the focus of attention. Crises are now present once every two weeks, making social inclusion easier. |
| 4 | Male | No occupation | Communication: Can now send WhatsApp vocal notes. Daily living skills: Can cook food with minimal support. Can make the bed. Can remember some daily life activities. Socialization: Social drive is present, but he doesn’t have close friends. Behavior: Can now distinguish between some basic emotions (i.e., sadness from anger). Can still get fixated on topics but can now recognize this behavior and cope with it with the help of the educator or the psychologist. |
| 5 | Male | Graduated at High school | Communication: Can understand complex instructions (receptive skills). Can tell about everyday experiences and clarify to other people what she is thinking or doing (expressive skills). Can pay attention to a 15-min informational talk. Can write one-page papers, but with different grammatical errors. Daily living skills: Can take means of transports alone. Has a group of friends that meets regularly. Enrolled in a course for driving license. Went on Erasmus with the support of the National Fragile X Syndrome Association. Socialization: Strong social drive, but still difficulties in respecting social rules. Can support his friends and show empathy. Behavior: less pronounced ADHD traits. Less impulsive. Is still sometimes verbally abusive, but frequency is dramatically reduced (less than once/week and only when very distressed). Parents report to be less distressed as the frequency of this behavior is lower and as now, he knows how to cope with it (i.e., by using the mindfulness practices that he learnt during the intervention) |
| 6 | Male | High school student. From June to August 2022 got a summer job in a bar. | Communication: Can send WhatsApp vocal notes. Can orally expound basic school material. Can write basic sentences. Daily living skills: Can take the bus alone. Can make his bed, can get a shower alone. Can cook food with some assistance. Socialization: Social drive is present. Can go out with his educator. Behavior: Can become verbally abusive when tired (around once/week) but can now recognize it and cooperate to modify this behavior. This symptom, absent before, appeared during the intervention, and was immediately treated with behavioral techniques. Still not able to distinguish between negative emotions. |
| 7 | Male | From June to August 2022 got a summer job in a bar. From September 2022 works in the civil service. | Communication: Still very basic expressive, receptive and written skills. Daily living skills: Can take means of transport with an educator. Can go to the supermarket where buys food with the help of a shopping list. Can plan his daily life with the help of the educator. Socialization: Can go out with and educator who became a friend when his work ended. Behavior: Can now recognize when he is getting nervous and ask for help to avoid verbal offenses. |
| 8 | Male | Work in his aunt’s company. | Communication: Expressive and written skills really improved. Receptive skills still more preserved. Friends report that he writes texts and can sustain longer conversations. Daily living skills: Can take means of transports alone. Can make his bed and prepare basilar food without support. He is learning graphic techniques with the support of a video-maker. Socialization: Strong social drive, but still difficulties in peers’ relationships. Behavior: Can recognize when he is getting nervous and ask for help to avoid verbal offenses. |
| 9 | Male | No occupation | Communication: Can understand complex instructions (receptive skills). Can tell about everyday experiences and clarify to other people what he is thinking or doing (expressive skills), can understand sarcasm and reads at a sixth-grade level. Can produce papers that are three or more pages long. Can pay attention to a 30-min informational talk. Can write poetries. Daily living skills. Still no occupation, but he is participating in various job competitions. He is attending an English course. Can take means of transports alone. He is getting a drive license. Socialization: Still strong social impairment. Can contact other CoM’s participants and go out with them. Behavior: Can now recognize depressive symptomatology and ask to other members’ group or to the psychologist to help him. |
| 10 | Male | Work with regular contract in a restaurant. | Communication: Can understand complex instructions (receptive skills). Can tell about everyday experiences and clarify to other people what he is thinking or doing (expressive skills), can understand sarcasm and reads at a sixth-grade level. Can produce papers that are three or more pages long. Can pay attention to a 30-min informational talk. Daily living skills: Can take means of transports alone. Can prepare food without assistance. Can do the laundry. Socialization: Still strong social problems. Can go to other members’ group hometowns to see them. Decided to go to the swimming pool to meet new people. Behavior: Can now recognize repetitive thought and speech and use cognitive strategies to stop them. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Montanaro, F.A.M.; Alfieri, P.; Vicari, S. “Corp-Osa-Mente”, a Combined Psychosocial–Neuropsychological Intervention for Adolescents and Young Adults with Fragile X Syndrome: An Explorative Study. Brain Sci. 2023, 13, 277. https://doi.org/10.3390/brainsci13020277
Montanaro FAM, Alfieri P, Vicari S. “Corp-Osa-Mente”, a Combined Psychosocial–Neuropsychological Intervention for Adolescents and Young Adults with Fragile X Syndrome: An Explorative Study. Brain Sciences. 2023; 13(2):277. https://doi.org/10.3390/brainsci13020277
Chicago/Turabian StyleMontanaro, Federica Alice Maria, Paolo Alfieri, and Stefano Vicari. 2023. "“Corp-Osa-Mente”, a Combined Psychosocial–Neuropsychological Intervention for Adolescents and Young Adults with Fragile X Syndrome: An Explorative Study" Brain Sciences 13, no. 2: 277. https://doi.org/10.3390/brainsci13020277
APA StyleMontanaro, F. A. M., Alfieri, P., & Vicari, S. (2023). “Corp-Osa-Mente”, a Combined Psychosocial–Neuropsychological Intervention for Adolescents and Young Adults with Fragile X Syndrome: An Explorative Study. Brain Sciences, 13(2), 277. https://doi.org/10.3390/brainsci13020277








