Breathwork Interventions for Adults with Clinically Diagnosed Anxiety Disorders: A Scoping Review
Abstract
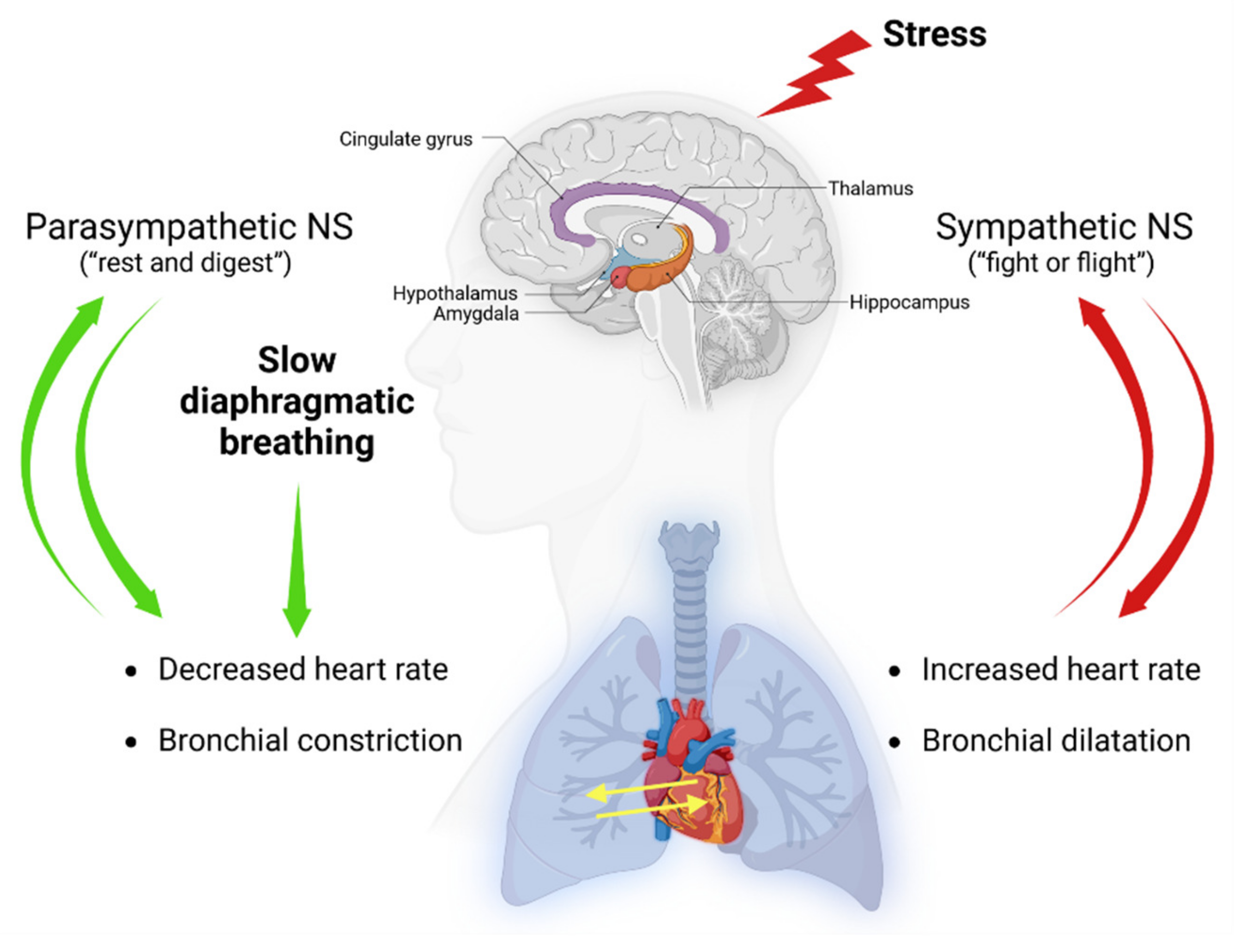
1. Introduction
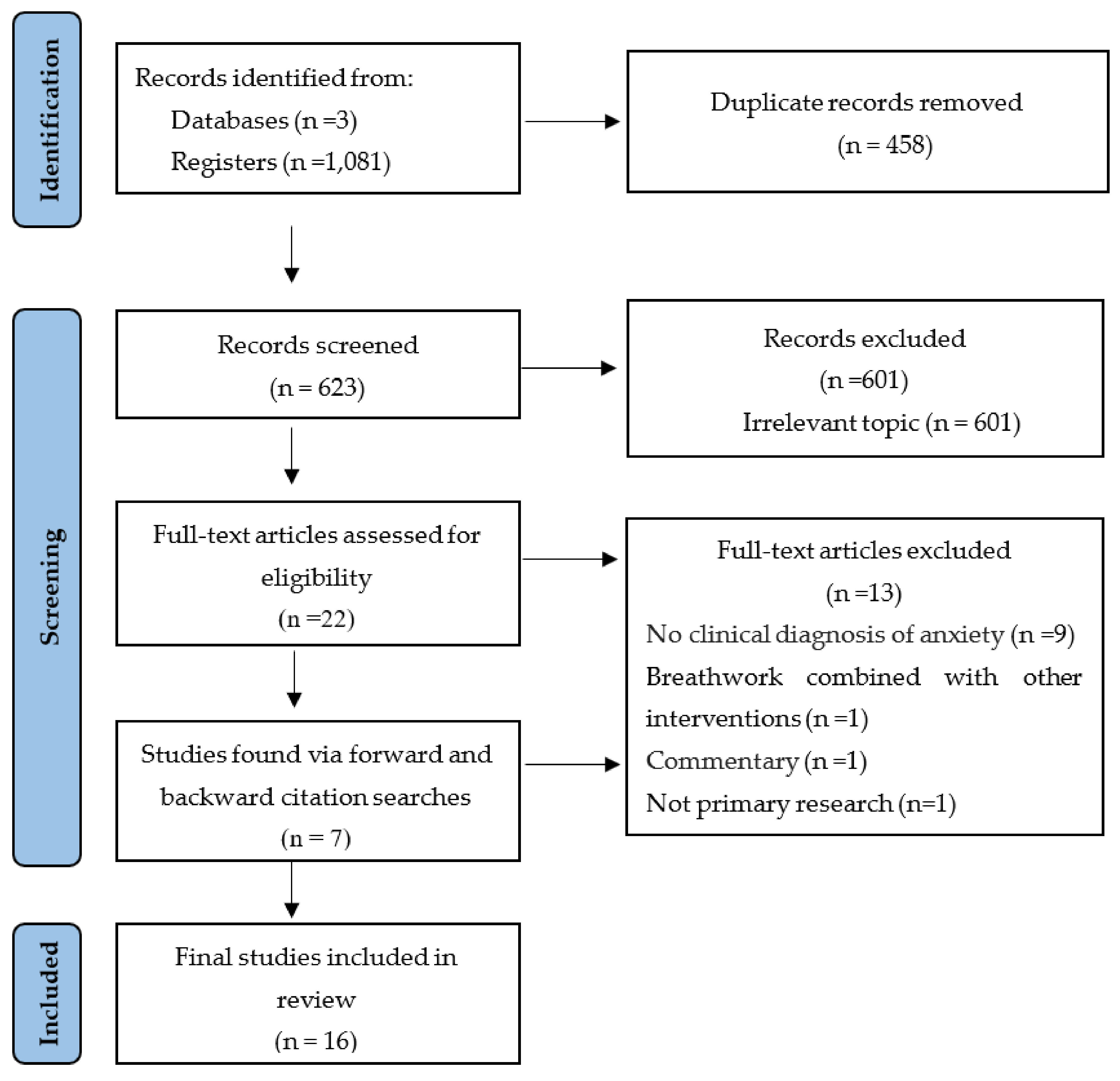
2. Materials and Methods
3. Results
3.1. Publication Analysis
3.2. Participants
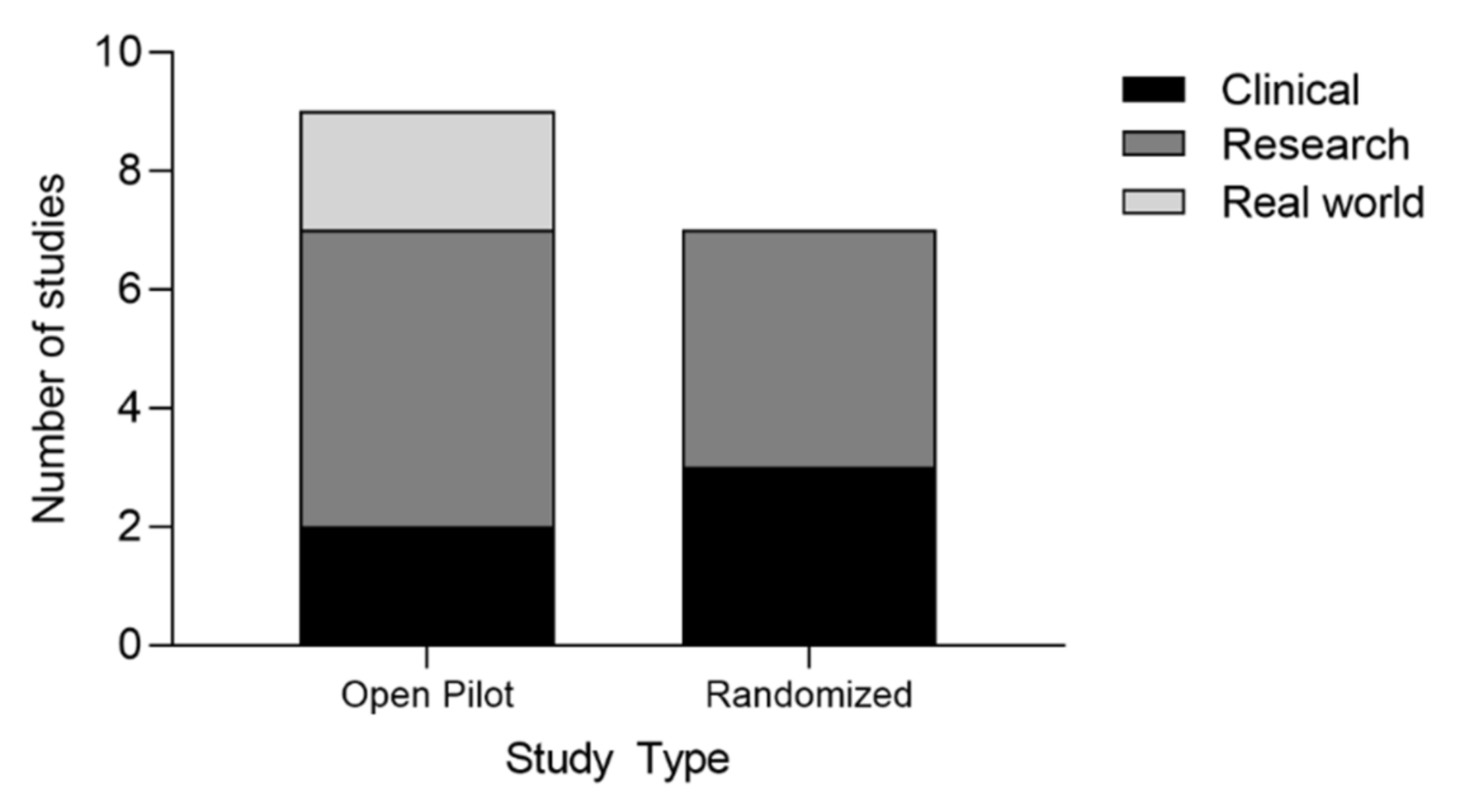
3.3. Study Designs
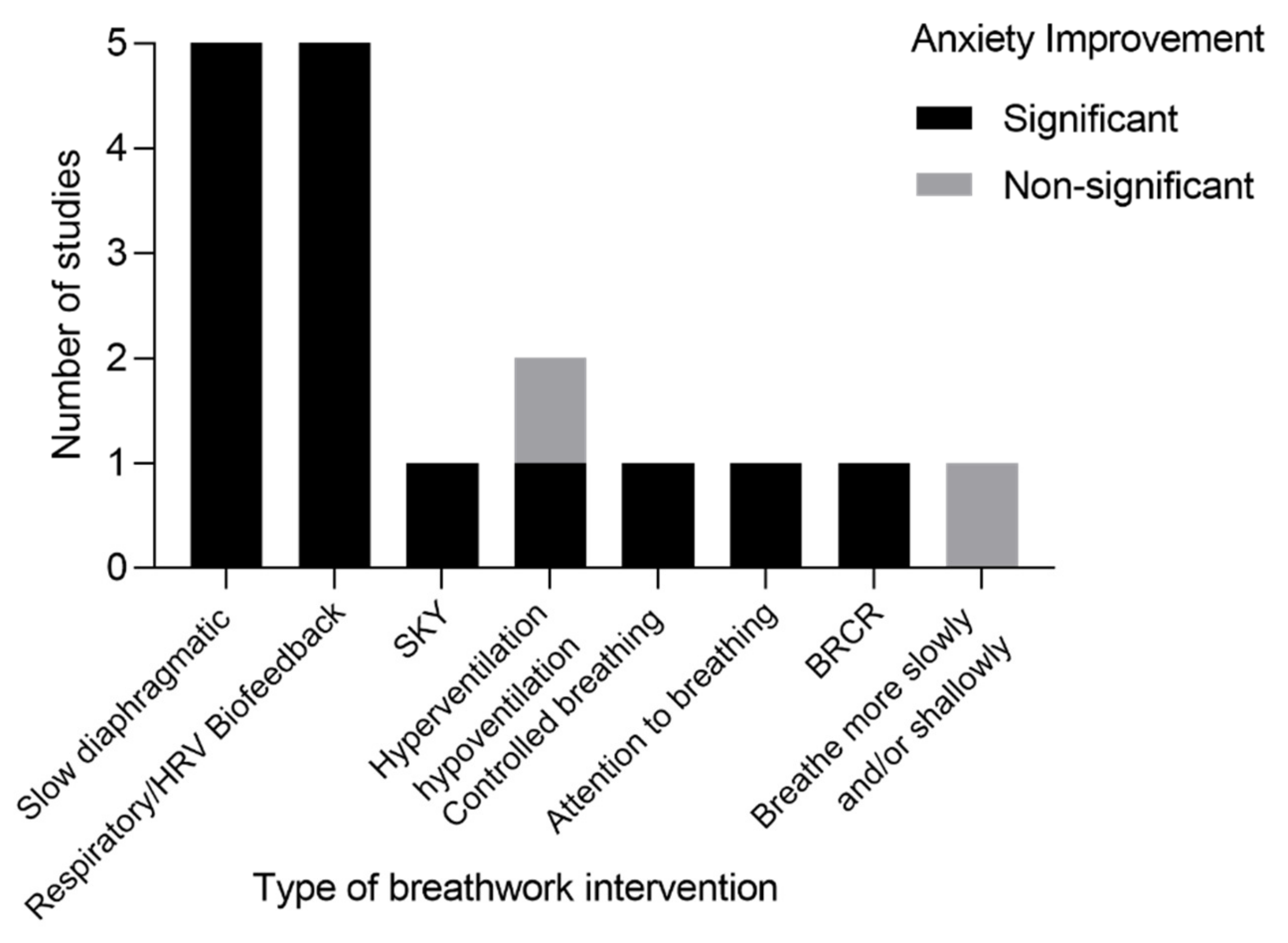
3.4. Breathwork Styles
3.5. Breathwork Regimens
3.6. Breathwork Outcomes
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Vos, T.; Lim, S.S.; Abbafati, C.; Abbas, K.M.; Abbasi, M.; Abbasifard, M.; Bhutta, Z.A.; Abbastabar, H.; Aboyan, V.; Abrams, E.M.; et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef] [PubMed]
- Vos, T.; Abajobir, A.A.; Abate, K.H.; Abbafati, C.; Abbas, K.M.; Abd-Allah, F.; Abdulkader, R.S.; Abdulle, A.M.; Abebo, T.A.; Abera, S.F.; et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1211–1259. [Google Scholar] [CrossRef] [PubMed]
- Penninx, B.W.J.H.; Pine, D.S.; Holmes, E.A.; Reif, A. Anxiety disorders. Lancet 2021, 397, 914–927. [Google Scholar] [CrossRef] [PubMed]
- Stein, D.J.; Scott, K.M.; de Jonge, P.; Kessler, R.C. Epidemiology of anxiety disorders: From surveys to nosology and back. Dialog. Clin. Neurosci. 2017, 19, 127–136. [Google Scholar] [CrossRef] [PubMed]
- Okon-Singer, H. The role of attention bias to threat in anxiety: Mechanisms, modulators and open questions. Curr. Opin. Behav. Sci. 2018, 19, 26–30. [Google Scholar] [CrossRef]
- Dymond, S.; Dunsmoor, J.E.; Vervliet, B.; Roche, B.; Hermans, D. Fear Generalization in Humans: Systematic Review and Implications for Anxiety Disorder Research. Behav. Ther. 2015, 46, 561–582. [Google Scholar] [CrossRef]
- Rudaz, M.; Ledermann, T.; Margraf, J.; Becker, E.S.; Craske, M.G. The moderating role of avoidance behavior on anxiety over time: Is there a difference between social anxiety disorder and specific phobia? PLoS ONE 2017, 12, e0180298. [Google Scholar] [CrossRef]
- Zorowitz, S.; Momennejad, I.; Daw, N.D. Anxiety, avoidance, and sequential evaluation. Comput. Psychiatr. 2020, 4, 10. [Google Scholar] [CrossRef]
- Sharpe, L.; Todd, J.; Scott, A.; Gatzounis, R.; Menzies, R.E.; Meulders, A. Safety behaviours or safety precautions? The role of subtle avoidance in anxiety disorders in the context of chronic physical illness. Clin. Psychol. Rev. 2022, 92, 102126. [Google Scholar] [CrossRef]
- Weinstein, R.S. Panic disorder. Am. Fam. Physic. 1995, 52, 2055–2063, 2067–2068. [Google Scholar]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.; Monahan, P.O.; Löwe, B. Anxiety disorders in primary care: Prevalence, impairment, comorbidity, and detection. Ann. Intern. Med. 2007, 146, 317–325. [Google Scholar] [CrossRef]
- Katzman, M.A.; Bleau, P.; Blier, P.; Chokka, P.; Kjernisted, K.; Van Ameringen, M.; the Canadian Anxiety Guidelines Initiative Group on behalf of the Anxiety Disorders Association of Canada/Association Canadienne des troubles anxieux and McGill University. Canadian clinical practice guidelines for the management of anxiety, posttraumatic stress and obsessive-compulsive disorders. BMC Psychiatr. 2014, 14, S1. [Google Scholar] [CrossRef]
- Vermani, M.; Marcus, M.; Katzman, M.A. Rates of detection of mood and anxiety disorders in primary care: A descriptive, cross-sectional study. Prim. Care Compan. CNS Disord. 2011, 13, 27211. [Google Scholar] [CrossRef]
- Stein, M.B.; Sherbourne, C.D.; Craske, M.G.; Means-Christensen, A.; Bystritsky, A.; Katon, W.; Sullivan, G.; Roy-Byrne, P.P. Quality of care for primary care patients with anxiety disorders. Am. J. Psychiatr. 2004, 161, 2230–2237. [Google Scholar] [CrossRef]
- Kroenke, K.; Jackson, J.L.; Chamberlin, J. Depressive and anxiety disorders in patients presenting with physical complaints: Clinical predictors and outcome. Am. J. Med. 1997, 103, 339–347. [Google Scholar] [CrossRef]
- Young, A.S.; Klap, R.; Sherbourne, C.D.; Wells, K.B. The quality of care for depressive and anxiety disorders in the United States. Arch. Gen. Psychiatr. 2001, 58, 55–61. [Google Scholar] [CrossRef]
- Morgan, A.J.; Jorm, A.F. Outcomes of self-help efforts in anxiety disorders. Expert Rev. Pharm. Outcomes Res. 2009, 9, 445–459. [Google Scholar] [CrossRef]
- Chisholm, D.; Sweeny, K.; Sheehan, P.; Rasmussen, B.; Smit, F.; Cuijpers, P.; Saxena, S. Scaling-up treatment of depression and anxiety: A global return on investment analysis. Lancet Psychiatr. 2016, 3, 415–424. [Google Scholar] [CrossRef]
- Slee, A.; Nazareth, I.; Bondaronek, P.; Liu, Y.; Cheng, Z.; Freemantle, N. Pharmacological treatments for generalised anxiety disorder: A systematic review and network meta-analysis. Lancet 2019, 393, 768–777. [Google Scholar] [CrossRef]
- Leyro, T.M.; Versella, M.V.; Yang, M.-J.; Brinkman, H.R.; Hoyt, D.L.; Lehrer, P. Respiratory therapy for the treatment of anxiety: Meta-analytic review and regression. Clin. Psychol. Rev. 2021, 84, 101980. [Google Scholar] [CrossRef]
- Paulus, M.P. The Breathing Conundrum—Interoceptive Sensitivity and Anxiety. Depress. Anxiet. 2013, 30, 315–320. [Google Scholar] [CrossRef] [PubMed]
- Kerr, W.J.; Gliebe, P.A.; Dalton, J.W. Physical Phenomena Associated with Anxiety States: The Hyperventilation Syndrome. Cal. West Med. 1938, 48, 12–16. [Google Scholar] [PubMed]
- Du Pasquier, D.; Fellrath, J.M.; Sauty, A. Hyperventilation syndrome and dysfunctional breathing: Update. Rev. Med. Suisse. 2020, 16, 1243–1249. [Google Scholar] [PubMed]
- Roth, W.T.; Wilhelm, F.H.; Pettit, D. Are current theories of panic falsifiable? Psychol. Bull. 2005, 131, 171–192. [Google Scholar] [CrossRef] [PubMed]
- Lewis, B.I. Hyperventilation syndrome: A clinical and physiological evaluation. Calif. Med. 1959, 91, 121–126. [Google Scholar]
- Thompson, W.P. The electrocardiogram in the hyperventilation syndrome. Am. Heart J. 1943, 25, 372–390. [Google Scholar] [CrossRef]
- Feinstein, J.S.; Gould, D.; Khalsa, S.S. Amygdala-driven apnea and the chemoreceptive origin of anxiety. Biol. Psychol. 2022, 170, 108305. [Google Scholar] [CrossRef]
- Van Diest, I.; Stegen, K.; Van de Woestijne, K.P.; Schippers, N.; Van den Bergh, O. Hyperventilation and attention: Effects of hypocapnia on performance in a stroop task. Biol. Psychol. 2000, 53, 233–252. [Google Scholar] [CrossRef]
- Fatouleh, R.; Macefield, V.G. Cardiorespiratory coupling of sympathetic outflow in humans: A comparison of respiratory and cardiac modulation of sympathetic nerve activity to skin and muscle. Exp. Physiol. 2013, 98, 1327–1336. [Google Scholar] [CrossRef]
- Van den Bergh, O.; Zaman, J.; Bresseleers, J.; Verhamme, P.; Van Diest, I. Anxiety, pCO2 and cerebral blood flow. Int. J. Psychophysiol. 2013, 89, 72–77. [Google Scholar] [CrossRef]
- Spicuzza, L.; Porta, C.; Bramanti, A.; Maffeis, M.; Casucci, G.; Casiraghi, N.; Bernardi, L. Interaction between central-peripheral chemoreflexes and cerebro-cardiovascular control. Clin. Auton. Res. 2005, 15, 373–381. [Google Scholar] [CrossRef]
- Thayer, J.F.; Lane, R.D. Claude Bernard and the heart-brain connection: Further elaboration of a model of neurovisceral integration. Neurosci. Biobehav. Rev. 2009, 33, 81–88. [Google Scholar] [CrossRef]
- Ernst, G. Heart-Rate Variability-More than Heart Beats? Front. Public Health 2017, 5, 240. [Google Scholar] [CrossRef]
- Brown, R.P.; Gerbarg, P.L.; Muench, F. Breathing practices for treatment of psychiatric and stress-related medical conditions. Psychiatr. Clin. N. Am. 2013, 36, 121–140. [Google Scholar] [CrossRef]
- Brown, R.P.; Gerbarg, P.L. Sudarshan Kriya Yogic breathing in the treatment of stress, anxiety, and depression. Part II--clinical applications and guidelines. J. Altern. Complement. Med. 2005, 11, 711–717. [Google Scholar] [CrossRef]
- Dhawan, A.; Chopra, A.; Jain, R.; Yadav, D.; Vedamurthachar. Effectiveness of yogic breathing intervention on quality of life of opioid dependent users. Int. J. Yoga 2015, 8, 144–147. [Google Scholar] [CrossRef]
- Gerbarg, P.; Brown, R.; Streeter, C.; Katzman, M.; Vermani, M. Breath Practices for Survivor and Caregiver Stress, Depression, and Post-traumatic Stress Disorder: Connection, Co-regulation, Compassion. OBM Integr. Complement. Med. 2019, 4, 1903045. [Google Scholar] [CrossRef]
- Hopper, S.I.; Murray, S.L.; Ferrara, L.R.; Singleton, J.K. Effectiveness of diaphragmatic breathing for reducing physiological and psychological stress in adults: A quantitative systematic review. JBI Database Syst. Rev. Implement. Rep. 2019, 17, 1855–1876. [Google Scholar] [CrossRef]
- Chen, Y.F.; Huang, X.Y.; Chien, C.H.; Cheng, J.F. The Effectiveness of Diaphragmatic Breathing Relaxation Training for Reducing Anxiety. Perspect. Psychiatr. Care 2017, 53, 329–336. [Google Scholar] [CrossRef]
- Chandla, S.S.; Sood, S.; Dogra, R.; Das, S.; Shukla, S.K.; Gupta, S. Effect of short-term practice of pranayamic breathing exercises on cognition, anxiety, general well being and heart rate variability. J. Indian Med. Assoc. 2013, 111, 662–665. [Google Scholar]
- Valenza, M.C.; Valenza-Peña, G.; Torres-Sánchez, I.; González-Jiménez, E.; Conde-Valero, A.; Valenza-Demet, G. Effectiveness of controlled breathing techniques on anxiety and depression in hospitalized patients with COPD: A randomized clinical Trial. Respir. Care 2014, 59, 209–215. [Google Scholar] [CrossRef] [PubMed]
- Russo, M.A.; Santarelli, D.M.; O’Rourke, D. The physiological effects of slow breathing in the healthy human. Breathe 2017, 13, 298–309. [Google Scholar] [CrossRef] [PubMed]
- Gerritsen, R.J.S.; Band, G.P.H. Breath of Life: The Respiratory Vagal Stimulation Model of Contemplative Activity. Front. Hum. Neurosci. 2018, 12, 397. [Google Scholar] [CrossRef] [PubMed]
- Zaccaro, A.; Piarulli, A.; Laurino, M.; Garbella, E.; Menicucci, D.; Neri, B.; Gemignani, A. How Breath-Control Can Change Your Life: A Systematic Review on Psycho-Physiological Correlates of Slow Breathing. Front. Hum. Neurosci. 2018, 12, 353. [Google Scholar] [CrossRef] [PubMed]
- Dick, T.E.; Hsieh, Y.H.; Dhingra, R.R.; Baekey, D.M.; Galán, R.F.; Wehrwein, E.; Morris, K.F. Cardiorespiratory coupling: Common rhythms in cardiac, sympathetic, and respiratory activities. Prog. Brain Res. 2014, 209, 191–205. [Google Scholar] [CrossRef]
- Tharion, E.; Samuel, P.; Rajalakshmi, R.; Gnanasenthil, G.; Subramanian, R.K. Influence of deep breathing exercise on spontaneous respiratory rate and heart rate variability: A randomised controlled trial in healthy subjects. Indian J. Physiol. Pharm. 2012, 56, 80–87. [Google Scholar]
- Rhinewine, J.P.; Williams, O.J. Holotropic Breathwork: The potential role of a prolonged, voluntary hyperventilation procedure as an adjunct to psychotherapy. J. Altern. Complement. Med. 2007, 13, 771–776. [Google Scholar] [CrossRef]
- Smith, P.J.; Merwin, R.M. The Role of Exercise in Management of Mental Health Disorders: An Integrative Review. Annu. Rev. Med. 2021, 72, 45–62. [Google Scholar] [CrossRef]
- Shevchuk, N.A. Adapted cold shower as a potential treatment for depression. Med. Hypotheses 2008, 70, 995–1001. [Google Scholar] [CrossRef]
- Kox, M.; van Eijk, L.T.; Zwaag, J.; van den Wildenberg, J.; Sweep, F.C.; van der Hoeven, J.G.; Pickkers, P. Voluntary activation of the sympathetic nervous system and attenuation of the innate immune response in humans. Proc. Natl. Acad. Sci. USA 2014, 111, 7379–7384. [Google Scholar] [CrossRef]
- Mariotti, A. The effects of chronic stress on health: New insights into the molecular mechanisms of brain-body communication. Future Sci. OA 2015, 1, fso23. [Google Scholar] [CrossRef]
- Marin, M.F.; Lord, C.; Andrews, J.; Juster, R.P.; Sindi, S.; Arsenault-Lapierre, G.; Fiocco, A.J.; Lupien, S.J. Chronic stress, cognitive functioning and mental health. Neurobiol. Learn. Mem. 2011, 96, 583–595. [Google Scholar] [CrossRef]
- Conrad, A.; Müller, A.; Doberenz, S.; Kim, S.; Meuret, A.E.; Wollburg, E.; Roth, W.T. Psychophysiological effects of breathing instructions for stress management. Appl. Psychophysiol. Biofeedback 2007, 32, 89–98. [Google Scholar] [CrossRef]
- Gorman, J.M.; Papp, L.A.; Coplan, J.D.; Martinez, J.M.; Lennon, S.; Goetz, R.R.; Ross, D.; Klein, D.F. Anxiogenic effects of CO2 and hyperventilation in patients with panic disorder. Am. J. Psychiatr. 1994, 151, 547–553. [Google Scholar] [CrossRef]
- Kim, S.; Wollburg, E.; Roth, W.T. Opposing breathing therapies for panic disorder: A randomized controlled trial of lowering vs raising end-tidal PCO2. J. Clin. Psychiatr. 2012, 73, 931–939. [Google Scholar] [CrossRef]
- Meuret, A.E.; Rosenfield, D.; Seidel, A.; Bhaskara, L.; Hofmann, S.G. Respiratory and cognitive mediators of treatment change in panic disorder: Evidence for intervention specificity. J. Consult. Clin. Psychol. 2010, 78, 691–704. [Google Scholar] [CrossRef]
- Meuret, A.E.; Wilhelm, F.H.; Ritz, T.; Roth, W.T. Feedback of end-tidal pCO2 as a therapeutic approach for panic disorder. J. Psychiatr. Res. 2008, 42, 560–568. [Google Scholar] [CrossRef]
- Wollburg, E.; Roth, W.T.; Kim, S. Effects of breathing training on voluntary hypo- and hyperventilation in patients with panic disorder and episodic anxiety. Appl. Psychophysiol. Biofeedback 2011, 36, 81–91. [Google Scholar] [CrossRef]
- Meuret, A.E.; Wilhelm, F.H.; Roth, W.T. Respiratory biofeedback-assisted therapy in panic disorder. Behav. Modif. 2001, 25, 584–605. [Google Scholar] [CrossRef]
- Tolin, D.F.; McGrath, P.B.; Hale, L.R.; Weiner, D.N.; Gueorguieva, R. A Multisite Benchmarking Trial of Capnometry Guided Respiratory Intervention for Panic Disorder in Naturalistic Treatment Settings. Appl. Psychophysiol. Biofeedback 2017, 42, 51–58. [Google Scholar] [CrossRef]
- Bonn, J.A.; Readhead, C.P.; Timmons, B.H. Enhanced adaptive behavioural response in agoraphobic patients pretreated with breathing retraining. Lancet 1984, 2, 665–669. [Google Scholar] [CrossRef] [PubMed]
- Hibbert, G.A.; Chan, M. Respiratory control: Its contribution to the treatment of panic attacks. A controlled study. Br. J. Psychiatr. 1989, 154, 232–236. [Google Scholar] [CrossRef]
- Ito, L.M.; Noshirvani, H.; Başoğlu, M.; Marks, I.M. Does exposure to internal cues enhance exposure to external cues in agoraphobia with panic? Psychother. Psychosom. 1996, 65, 24–28. [Google Scholar] [CrossRef] [PubMed]
- de Ruiter, C.; Ryken, H.; Garssen, B.; Kraaimaat, F. Breathing retraining, exposure and a combination of both, in the treatment of panic disorder with agoraphobia. Behav. Res. 1989, 27, 647–655. [Google Scholar] [CrossRef] [PubMed]
- Doria, S.; De Vuono, A.; Sanlorenzo, R.; Irtelli, F.; Mencacci, C. Anti-anxiety efficacy of Sudarshan Kriya Yoga in general anxiety disorder: A multicomponent, yoga based, breath intervention program for patients suffering from generalized anxiety disorder with or without comorbidities. J. Affect. Disord. 2015, 184, 310–317. [Google Scholar] [CrossRef]
- Han, J.N.; Stegen, K.; De Valck, C.; Clément, J.; Van de Woestijne, K.P. Influence of breathing therapy on complaints, anxiety and breathing pattern in patients with hyperventilation syndrome and anxiety disorders. J. Psychosom. Res. 1996, 41, 481–493. [Google Scholar] [CrossRef]
- Herhaus, B.; Siepmann, M.; Kahaly, G.J.; Conrad, R.; Petrowski, K. Effect of a Biofeedback Intervention on Heart Rate Variability in Individuals with Panic Disorder: A Randomized Controlled Trial. Psychosom. Med. 2022, 84, 199–209. [Google Scholar] [CrossRef]
- Yamada, T.; Inoue, A.; Mafune, K.; Hiro, H.; Nagata, S. Recovery of Percent Vital Capacity by Breathing Training in Patients With Panic Disorder and Impaired Diaphragmatic Breathing. Behav. Modif. 2017, 41, 665–682. [Google Scholar] [CrossRef]
- Leander, M.; Lampa, E.; Rask-Andersen, A.; Franklin, K.; Gislason, T.; Oudin, A.; Svanes, C.; Torén, K.; Janson, C. Impact of anxiety and depression on respiratory symptoms. Respir. Med. 2014, 108, 1594–1600. [Google Scholar] [CrossRef]
- Grassi, M.; Caldirola, D.; Vanni, G.; Guerriero, G.; Piccinni, M.; Valchera, A.; Perna, G. Baseline respiratory parameters in panic disorder: A meta-analysis. J. Affect. Disord. 2013, 146, 158–173. [Google Scholar] [CrossRef]
- Perna, G.; Gabriele, A.; Caldirola, D.; Bellodi, L. Hypersensitivity to inhalation of carbon dioxide and panic attacks. Psychiatr. Res. 1995, 57, 267–273. [Google Scholar] [CrossRef]
- Papp, L.A.; Klein, D.F.; Gorman, J.M. Carbon dioxide hypersensitivity, hyperventilation, and panic disorder. Am. J. Psychiatr. 1993, 150, 1149–1157. [Google Scholar] [CrossRef]
- Vieira, A.A.; Santoro, I.L.; Dracoulakis, S.; Caetano, L.B.; Fernandes, A.L. Anxiety and depression in asthma patients: Impact on asthma control. J. Bras. Pneumol. 2011, 37, 13–18. [Google Scholar] [CrossRef]
- Kunik, M.E.; Roundy, K.; Veazey, C.; Souchek, J.; Richardson, P.; Wray, N.P.; Stanley, M.A. Surprisingly high prevalence of anxiety and depression in chronic breathing disorders. Chest 2005, 127, 1205–1211. [Google Scholar] [CrossRef]
- Wang, G.; Zhou, T.; Wang, L.; Wang, L.; Fu, J.J.; Zhang, H.P.; Ji, Y.L. Relationship between current psychological symptoms and future risk of asthma outcomes: A 12-month prospective cohort study. J. Asthma. 2011, 48, 1041–1050. [Google Scholar] [CrossRef]
- Thomas, M.; Bruton, A.; Moffat, M.; Cleland, J. Asthma and psychological dysfunction. Prim. Care. Respir. J. 2011, 20, 250–256. [Google Scholar] [CrossRef]
- Oraka, E.; King, M.E.; Callahan, D.B. Asthma and serious psychological distress: Prevalence and risk factors among US adults, 2001–2007. Chest 2010, 137, 609–616. [Google Scholar] [CrossRef]
- Moss, D.P. Principles and Practice of Stress Management, 4th ed.; Lehrer, P.M., Woolfolk, R.L., Eds.; Guilford Press: New York, NY, USA, 2022; Volume 47, pp. 143–144. [Google Scholar] [CrossRef]
- Magnon, V.; Dutheil, F.; Vallet, G.T. Benefits from one session of deep and slow breathing on vagal tone and anxiety in young and older adults. Sci. Rep. 2021, 11, 19267. [Google Scholar] [CrossRef]
- Wells, R.; Outhred, T.; Heathers, J.A.; Quintana, D.S.; Kemp, A.H. Matter over mind: A randomised-controlled trial of single-session biofeedback training on performance anxiety and heart rate variability in musicians. PLoS ONE 2012, 7, e46597. [Google Scholar] [CrossRef]
- Beng, T.S.; Ahmad, F.; Loong, L.C.; Chin, L.E.; Zainal, N.Z.; Guan, N.C.; Ann, Y.H.; Li, L.M.; Meng, C.B.C. Distress Reduction for Palliative Care Patients and Families With 5-Minute Mindful Breathing: A Pilot Study. Am. J. Hosp. Palliat. Med. 2016, 33, 555–560. [Google Scholar] [CrossRef]
- Balban, M.Y.; Neri, E.; Kogon, M.M.; Weed, L.; Nouriani, B.; Jo, B.; Holl, G.; Zeitzer, J.M.; Spiegel, D.; Huberman, A.D. Brief structured respiration practices enhance mood and reduce physiological arousal. Cell Rep. Med. 2023, 4, 100895. [Google Scholar] [CrossRef] [PubMed]
- Reyes del Paso, G.A.; Godoy, J.; Vila, J. Respiratory sinus arrhythmia as an index of parasympathetic cardiac control during the cardiac defense response. Biol. Psychol. 1993, 35, 17–35. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, S.G.; Moscovitch, D.A.; Litz, B.T.; Kim, H.J.; Davis, L.L.; Pizzagalli, D.A. The worried mind: Autonomic and prefrontal activation during worrying. Emotion 2005, 5, 464–475. [Google Scholar] [CrossRef] [PubMed]
- Kemp, A.H.; Quintana, D.S.; Felmingham, K.L.; Matthews, S.; Jelinek, H.F. Depression, comorbid anxiety disorders, and heart rate variability in physically healthy, unmedicated patients: Implications for cardiovascular risk. PLoS ONE 2012, 7, e30777. [Google Scholar] [CrossRef] [PubMed]
- Gorman, J.M.; Sloan, R.P. Heart rate variability in depressive and anxiety disorders. Am. Heart J. 2000, 140, 77–83. [Google Scholar] [CrossRef]
- Thayer, J.F.; Yamamoto, S.S.; Brosschot, J.F. The relationship of autonomic imbalance, heart rate variability and cardiovascular disease risk factors. Int. J. Cardiol. 2010, 141, 122–131. [Google Scholar] [CrossRef]
- Lehrer, P.M.; Gevirtz, R. Heart rate variability biofeedback: How and why does it work? Front. Psychol. 2014, 5, 756. [Google Scholar] [CrossRef]
- Hsieh, C.W.; Mao, C.W.; Young, M.S.; Yeh, T.L.; Yeh, S.J. Respiratory effect on the pulse spectrum. J. Med. Eng. Technol. 2003, 27, 77–84. [Google Scholar] [CrossRef]
- Tonhajzerova, I.; Mestanik, M.; Mestanikova, A.; Jurko, A. Respiratory sinus arrhythmia as a non-invasive index of ‘brain-heart’ interaction in stress. Indian J. Med. Res. 2016, 144, 815–822. [Google Scholar] [CrossRef]
- Fincham, G.W.; Strauss, C.; Montero-Marin, J.; Cavanagh, K. Effect of breathwork on stress and mental health: A meta-analysis of randomised-controlled trials. Sci. Rep. 2023, 13, 432. [Google Scholar] [CrossRef]
- Ley, R. Blood, breath, and fears: A hyperventilation theory of panic attacks and agoraphobia. Clin. Psychol. Rev. 1985, 5, 271–285. [Google Scholar] [CrossRef]
- Klein, D.F. False suffocation alarms, spontaneous panics, and related conditions. An integrative hypothesis. Arch. Gen. Psychiatr. 1993, 50, 306–317. [Google Scholar] [CrossRef]
- Maddock, R.J.; Carter, C.S. Hyperventilation-induced panic attacks in panic disorder with agoraphobia. Biol. Psychiatr. 1991, 29, 843–854. [Google Scholar] [CrossRef]
- Ley, R. The efficacy of breathing retraining and the centrality of hyperventilation in panic disorder: A reinterpretation of experimental findings. Behav. Res. Ther. 1991, 29, 301–304. [Google Scholar] [CrossRef]
- Cuyler, R.N. Commentary on Kim et al., Effects of therapeutic relationship, expectancy, and credibility in breathing therapies for anxiety. Bull. Menn. Clin. 2015, 79, 356–361. [Google Scholar] [CrossRef]
- Grof, S. Beyond the Brain: Birth, Death, and Transcendence in Psychotherapy; Suny Press: Albany, NY, USA, 1985. [Google Scholar]
- Miller, T.; Nielsen, L. Measure of Significance of Holotropic Breathwork in the Development of Self-Awareness. J. Altern. Complement. Med. 2015, 21, 796–803. [Google Scholar] [CrossRef]

| Breathwork search terms | *Breathwork, *breathing exercise, *breathing technique, *breathing practice, *breath regulation, *pranayama, *mindful breathing, *paced breathing, *controlled breathing, *slow breathing, *fast breathing, *hyperventilation, *deep breathing, *metronome breathing, *nasal breathing, *mouth breathing, *diaphragmatic breathing |
| Anxiety search terms (DSM-5 classification system) | *Anxiety, *anxiety disorders, *stress disorders, *stress, *anxiety, *phobia, *phobic, *panic, *stress disorder, *agoraphobia |
| PICOS Criteria | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| P (population) |
|
|
| I (intervention) |
|
|
| O (outcome) |
|
|
| S (study design) |
|
|
| Population Characteristics | Breathwork Intervention Characteristics | |||||||
|---|---|---|---|---|---|---|---|---|
| Study reference/ year/ country | Study design a. Study type b. Design c. Setting | Diagnosis | Experimental group a. No. of participants (N) and sex b. Mean age | Control group a. No. of participants (N) and sex b. Mean age | Type of breathwork intervention | Breathwork protocol (treatment) | Details of breathwork intervention a. Duration of session b. No. of sessions c. Treatment duration d. Follow-up | Breathwork protocol (control) |
| Bonn et al. [61] 1984 England | a. Open pilot b. Between subject c. Clinical | Agoraphobia | a. N = 7 (4 females, 3 males) b. 35.5 | a. N = 5 (3 females, 2 males) b. 39 | Slow diaphragmatic breathing | Breathing retraining via guided diaphragmatic respiration, 8–10 BPM | a. 120 min b. 9 sessions c. 10 weeks d. 1, 6 months | Real-life exposure (9 × 120 min/9 weeks) |
| Conrad et al. [53] 2007 United States | a. Open pilot b. Between subject c. Research | Panic disorder | a. N = 13 (11 females, 2 males) b. 39.2 | a. N = 15 (10 females, 5 males) b. 40.7 | Direct attention to breathing, instructions to breathe more slowly and/or shallowly | Paying attention to breathing or breathing at a slower pace than usual or breathing shallower than usual or breathing shallower and slower than usual | a. 180 min b. 1 session c. NA d. NA | Same as treatment |
| de Ruiter et al. [64] 1989 The Netherlands | a. Randomized trial b. Between subject c. Clinical | Panic disorder with agoraphobia | a. N = 13 (7 females, 6 males) b. 34.0 | a. N = 27 (17 females, 10 males) b. 34.0 | Breathing retraining cognitive restructuring (BRCR) | Voluntary hyperventilation, hyperventilation and catastrophic thinking explanation, muscle relaxation training, slow diaphragmatic breathing training | a. 60 min b. 8 sessions c. NA d. NA | Graded self-exposure in vivo (8 × 60 min); breathing retraining or cognitive restructuring (4 × 60 min) plus graded self-exposure in vivo (4 × 60 min) |
| Gorman et al. [54] 1994 United States | a. Open pilot b. Between subject c. Research | Panic disorder/ agoraphobia | a. N = 24 (15 females, 9 males) b. 36.3 | a. N = 18 (12 females, 6 males) b. 32.5 | CO2 inhalation and room-air hyperventilation | (a) Air breathing (20 min). (b) 5% CO2 (20 min) or hyperventilation (15 min), metronome-guided breathing (30 BPM). (c) Air breathing (15 min). (d) 5% CO2 (20 min) or hyperventilation (15 min). (e) Air breathing (15 min). (f) 7% CO2 (20 min). | a. 35 min b. 1 session c. NA d. NA | Same as treatment |
| Herhaus et al. [67] 2022 Germany | a. Randomized trial b. Between subject c. Clinical | Panic disorder/ agoraphobia | a. N = 26 (19 females, 7 males) b. 35.7 | a. N = 26 (17 females, 9 males) b. 35.7 | Heart rate variability-biofeedback (HRV-BF) training | Heart rate variability-biofeedback at 0.1 Hz breathing (10 × 20 min), and at-home breathing training with 0.1 Hz breathing via audio track (2 × 20 min/day) | a. 20 min b. 10 sessions c. 4 weeks d. NA | Sham HRV-B biofeedback without paced breathing (10 × 20 min/4 weeks) |
| Hibbert and Chan [62] 1989 England | a. Randomized trial b. Between subject c. Research | Panic disorder with agoraphobia | a. N = 21 (13 females, 8 males) b. 35.0 | a. N = 19 (13 females, 6 males) b. 35 | Controlled breathing training | First treatment session: provocation test (rebreathing using a paper bag, 2 min of forced ventilation, rebreathing with the bag); second treatment session: paced breathing, overbreathing | a. Not reported b. 2 sessions c. 3 weeks d. NA | Psychoeducation (1 ×/1 week) plus diary homework (1 × 30 min/day) followed by anxiety management strategies |
| Ito et al. [63] 1996 England | a. Randomized trial b. Between subject c. Clinical | Panic disorder with agoraphobia | a. N = 10 b. 37.0 | a. N = 9 b. 38 | Slow deep breathing | Slowed breathing (2 × 5 min/day) plus self-exposure (30–45 min) × 7 sessions/10 weeks, plus therapist-accompanied internal exposure (2 × 30 min/2 weeks). Daily exposure homework: 60 min external plus 30 min internal exposure. Exposure protocol: hyperventilation (1 min), shaking head side to side (30 s), running on spot (1 min), head between legs (30 s) and then quickly lifting head up. Slow breathing after each exercise to return to baseline anxiety level. | a. Not reported b. 7 sessions c. 10 weeks d. 4, 10, 14, 24 weeks | Slowed breathing (2× 5 min/day) plus self-exposure (30–45 min) × 7 sessions/10 weeks, plus therapist-accompanied external exposure (1 × 60 min/1 week). Daily between-session exposure homework: 90 min of external exposure. Exposure protocol same as treatment. |
| Kim et al. [55] 2012 United States | a. Randomized trial b. Between subject c. Research | Panic disorder/ agoraphobia | a. N = 74 (51 females, 23 males) b. 41.9 | a. N = 30 (21 females, 9 males) b. 43 | Hypoventilation, hyperventilation | Biofeedback-assisted hypercapnic or hypocapnic breathing therapy (5 ×/5 weeks) plus at-home breathing exercises (2 × day/5 weeks). Breathing exercises: baseline breathing (2 min), breathing more deeply or shallowly to reach PCO2 = 30 mm Hg (lower-CO2 group) or 40 mm Hg (raise-CO2 group) by breathing via audio tape (10 min) followed by breathing without audio tape (5 min). RR maintained at 9 BPM. | a. 17 min b. 5 sessions c. 5 weeks d. 1, 6 months | Delayed treatment |
| Meuret et al. [56] 2010 United States | a. Open pilot b. Between subject c. Research | Panic disorder with agoraphobia | a. N = 21 (17 females, 4 males) b. 31.4 | a. N = 20 (17 females, 3 males) b. 35 | Capnometry-assisted respiratory training (CART) | Education and teaching to control end-tidal PCO2 and RR. Between-session exercises (2 × 17 min/day): (a) 2 min physiological baseline recording. (b) 10 min synchronized breathing with recorded tones (weekly BPM targets: 13, 11, 9, 6) and PCO2 of 40 ± 3 mm Hg. (c) 5 min transfer with visual feedback. | a. 60 min b. 5 sessions c. 4 weeks d. None | Cognitive skill training (5 × 60 min/week) plus cognitive homework (2 × 17 min/day) |
| Meuret et al. [57] 2008 United States | a. Randomized trial b. Between subject c. Research | Panic disorder/ agoraphobia | a. N = 20 b. 41.0 | a. N = 17 b. 41 | Capnometry-assisted breathing therapy (BRT) | Education, direct attention to respiratory patterns, breathing maneuvers, teaching control of pCO2 and RR. Daily breathing exercises (2 × 17 min/day): (a) 2 min physiological baseline recording. (b) 10 min synchronized breathing with recorded tones (weekly BPM targets: 13, 11, 9, 6) in a normocapnic range (pCO2 > 35 mmHg. (c) 5 min transfer, breathing without pacing tones. | a. 60 min b. 5 sessions c. 4 weeks d. 2, 12 months | Delayed treatment |
| Wollburg et al. [58] 2011 United States | a. Randomized trial b. Between subject c. Research | Panic disorder | a. N = 45 (30 females, 15 males) b. 41.8 | a. N = 20 (11 females, 9 males) b. 45.7 | Hypoventilation, hyperventilation | (a) Education. (b) Biofeedback-assisted hypercapnic or hypocapnic breathing therapy (5 ×/5 weeks). (c) At-home breathing exercises (2 × day/5 weeks): training by breathing more deeply or shallowly to obtain the target pCO2 (lower: 30 mmHg, raise: 40 mmHg) at 9 BPM. | a. Not reported b. 5 sessions c. NA d. 1 month | Delayed treatment |
| Yamada et al. [68] 2017 Japan | a. Open pilot b. Between subject c. Clinical | Panic disorder | a. N = 28 (20 females, 8 males) b. 31.1 | a. N = 28 (20 females, 8 males) b. 31.1 | Slow diaphragmatic breathing | CBT (weekly). Diaphragmatic breathing retraining (daily): (a) relaxed breathing–supine breathing training w/500 g weight and hand pressure. (b) Seated breathing training w/lumbar spine flexed w/expiration and dorsiflexed w/inspiration. Stretching exercises for breathing muscles. | a. Not reported b. CBT weekly, BT daily. c. 6–13 weeks d. None | Same as treatment |
| Doria et al. [65] 2015 Italy | a. Open pilot b. Within subject c. Real world | Generalized anxiety disorder | a. N = 69 (41 females, 28 males) b. Not specified | NA | Surdashan Kriya Yoga (SKY) | Ujjayi, slow breathing 3–4 cycles per minute; Nadi Shodhana, alternate nostril breathing, Kapalabhati, fast diaphragmatic breathing; Bhastrika, rapid exhalation at 20–30 cycles/min; and Sudarshan Kriya, rhythmic, cyclical breathing in slow, medium, and fast cycles | a. 120 min b. 10 sessions c. 2 weeks d. 2 weeks, 3 and 6 months | NA |
| Han et al. [66] 1996 Belgium | a. Open pilot b. Within subject c. Research | Hyperventilation syndrome | a. N = 92 (60 females, 32 males) b. 37.0 | NA | Abdominal slow breathing | Hyperventilation (3 min), reattribution of symptoms to hyperventilation, abdominal breathing with slowed expiration, breathing retraining | a. 45 min b. 17 sessions c. 2.5 months d. NA | NA |
| Meuret et al. [59] 2001 United States | a. Open pilot b. Within subject c. Research | Panic disorder/ agoraphobia | a. N = 4 (2 females, 2 males) b. 42.0 | NA | Respiratory biofeedback-assisted therapy | Education, teaching techniques to control respirations, direct attention to respiratory patterns. Home breathing exercises (2 × 17 min/day): (a) 2 min baseline recording. (b) 10 min paced breathing with recorded tones (weekly BPM targets: 13, 11, 9, 6). (c) 5 min transfer, breathing without pacing tones. | a. 80 min b. 5 sessions c. 4 weeks d. 2 months | NA |
| Tolin et al. [60] 2017 United States | a. Open pilot b. Within subject c. Real world | Panic disorder | a. N = 69 (41 females, 28 males) b. 36.6 | NA | Capnometry guided respiratory intervention (CGRI) | Breathing sessions (2 × 17 min/day): (a) baseline breathing (2 min), (b) 10 min paced breathing via audio tape (weekly BPM targets: 13, 11, 9, 6), target PETCO2 level (37–40 mmHg). (c) 5 min transfer, breathing without pacing tones. | a. 17 min b. 56 sessions c. 4 weeks d. 2, 6, 12 months | NA |
| Study Measures | ||||
|---|---|---|---|---|
| Study Reference | Objective Measures | Subjective Measures | Custom Measures | Primary Findings |
| Bonn et al. [61] | Panic attack frequency, resting breathing rate | NA | Phobia and agoraphobia scores, somatic symptoms | Significant improvement in all measures compared with control, maintained at 6-month follow-up |
| Conrad et al. [53] | Skin conductance, pCO2, tidal volume, HR | ASI, BAI, BDI, PSS, PSWQ | Mood questionnaire | No change in respiratory or autonomic measures in direction of relaxation, except for attention to breathing |
| de Ruiter et al. [64] | pCO2, RR | FBSQ, FSS-III, SCL-90 | Phobic anxiety and avoidance scales, panic attack diary | Significant improvement in all measures, except panic frequency, with reduction in RR; no significant differences between groups |
| Gorman et al. [54] | pCO2 | API, RPE, SADS-LA | Anxiety and apprehension scales | Significant sensitivity to anxiogenic effects of CO2 compared with controls; 7% CO2 discriminated best. CO2 is a more potent anxiogenic stimulus than room-air hyperventilation. |
| Herhaus et al. [67] | HR, BMP, EEG signals | ACQ, ASI, BDI, BSQ, MI, PAS | NA | Improved HRV and panic symptoms compared with controls |
| Hibbert and Chan [62] | NA | BDI, FQ, HARS | Panic attack and exposure diary | Significant improvement in anxiety measures compared with controls; no significant differences in hyperventilators compared with non-hyperventilators |
| Ito et al. [63] | NA | ACQ, BDI, BSQ, FQ, HARS, PT, disability (measure not defined) | Panic attack diary | Significant improvement in all measures at post-treatment and follow-up; no significant differences between groups, but a slightly greater number of patients in the treatment group showed improvement in phobic avoidance and fear |
| Kim et al. [55] | pCO2, RR | ACQ, ACQ, ASI, BAI, BDI, MIA, PDSS | NA | Significant improvement in panic severity by using both breathing training methods, maintained at 6-month follow-up; patients learned to alter pCO2 and RR via therapy |
| Meuret et al. [56] | pCO2, RR | BSQ, ASI, BSQ/ASI, ACQ, PDSS, CEQ | NA | Significant improvement in panic symptoms, panic-related cognitions, and perceived control in both treatment groups; corrections from hypocapnic to normocapnic levels only in capnometry-assisted respiratory training group |
| Meuret et al. [57] | pCO2, RR | PDSS, clinician-rated PD severity, CGI, ASI, SDS, MI-AAL, BDI | NA | Significant improvement in all measures in treated but not untreated patients; psychological outcomes maintained at 2- and 12-month follow-up |
| Wollburg et al. [58] | Expired CO2, end-tidal pCO2, RR, respiratory rate instability, TV, TV instability, HR, skin conductance | ASI, MI, BDI, ASQ | PDSS, ASI, mobility inventory for agoraphobia, BDI, anxiety symptom checklist, pCO2, expired CO2, RR, RR instability, tidal volume, TV instability, HR, respiratory sinus arrhythmia, skin conductance | Before treatment: higher respiration rates, tidal volume instability and sighing at rest of panic patients compared with non-anxious controls. After lowering pCO2 therapy: lower pCO2 during testing of panic patients but no significant differences in reactivity, recovery, or treatment effect between groups; baseline abnormalities somewhat specific to PD |
| Yamada et al. [68] | VC, %VC | Diaphragmatic breathing assessment | NA | %VC was significantly reduced in patients with impaired diaphragmatic breathing, which was equally recoverable compared with controls, with breathing retraining |
| Doria et al. [65] | NA | HRSA, HRSD, SCL-90, ZSAS, ZSDS | NA | Significant improvement in anxiety and depression |
| Han et al. [66] | pCO2, inspiratory time, inspiratory volume, expiratory time, expiratory volume | NQ, STAI, ZBV-DY1, ZBV-DY2 | NA | Significantly improved daily life complaints and state anxiety; markedly changed breathing pattern |
| Meuret et al. [59] | pCO2, RR | PDSS, ASI, STAIT-T, BDI | Rate average anxiety, depression, anticipation, and worry daily; panic attack diary | Significant improvement in PD symptoms and pCO2 that continued through follow-up; equal reductions in fear, anxiety and depression |
| Tolin et al. [60] | pCO2, RR | PDSS, NINI, CGI-S, SDS, MI-AAL, ASI, BDI, panic frequency | Patient satisfaction | Significant improvement in PD severity, with high treatment response and remission maintained at 12-month follow-up. Decrease in functional impairment and global illness severity. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Banushi, B.; Brendle, M.; Ragnhildstveit, A.; Murphy, T.; Moore, C.; Egberts, J.; Robison, R. Breathwork Interventions for Adults with Clinically Diagnosed Anxiety Disorders: A Scoping Review. Brain Sci. 2023, 13, 256. https://doi.org/10.3390/brainsci13020256
Banushi B, Brendle M, Ragnhildstveit A, Murphy T, Moore C, Egberts J, Robison R. Breathwork Interventions for Adults with Clinically Diagnosed Anxiety Disorders: A Scoping Review. Brain Sciences. 2023; 13(2):256. https://doi.org/10.3390/brainsci13020256
Chicago/Turabian StyleBanushi, Blerida, Madeline Brendle, Anya Ragnhildstveit, Tara Murphy, Claire Moore, Johannes Egberts, and Reid Robison. 2023. "Breathwork Interventions for Adults with Clinically Diagnosed Anxiety Disorders: A Scoping Review" Brain Sciences 13, no. 2: 256. https://doi.org/10.3390/brainsci13020256
APA StyleBanushi, B., Brendle, M., Ragnhildstveit, A., Murphy, T., Moore, C., Egberts, J., & Robison, R. (2023). Breathwork Interventions for Adults with Clinically Diagnosed Anxiety Disorders: A Scoping Review. Brain Sciences, 13(2), 256. https://doi.org/10.3390/brainsci13020256







