Pilot Findings Indicate a Cognitive Behavioral Healthy Lifestyle Intervention for PTSD Improves Sleep and Physical Activity
Abstract
:1. Introduction
2. Methods
2.1. Participants
2.2. Measures
2.2.1. Pittsburgh Sleep Quality Index (PSQI)
2.2.2. The 7-Day Physical Activity Recall
2.2.3. Weekly Stress Inventory Short Form (WSI)
2.2.4. The Post-Traumatic Stress Checklist 5th Edition (PCL-5)
3. Procedures
Healthy Lifestyle Intervention
4. Results
4.1. Descriptive Data
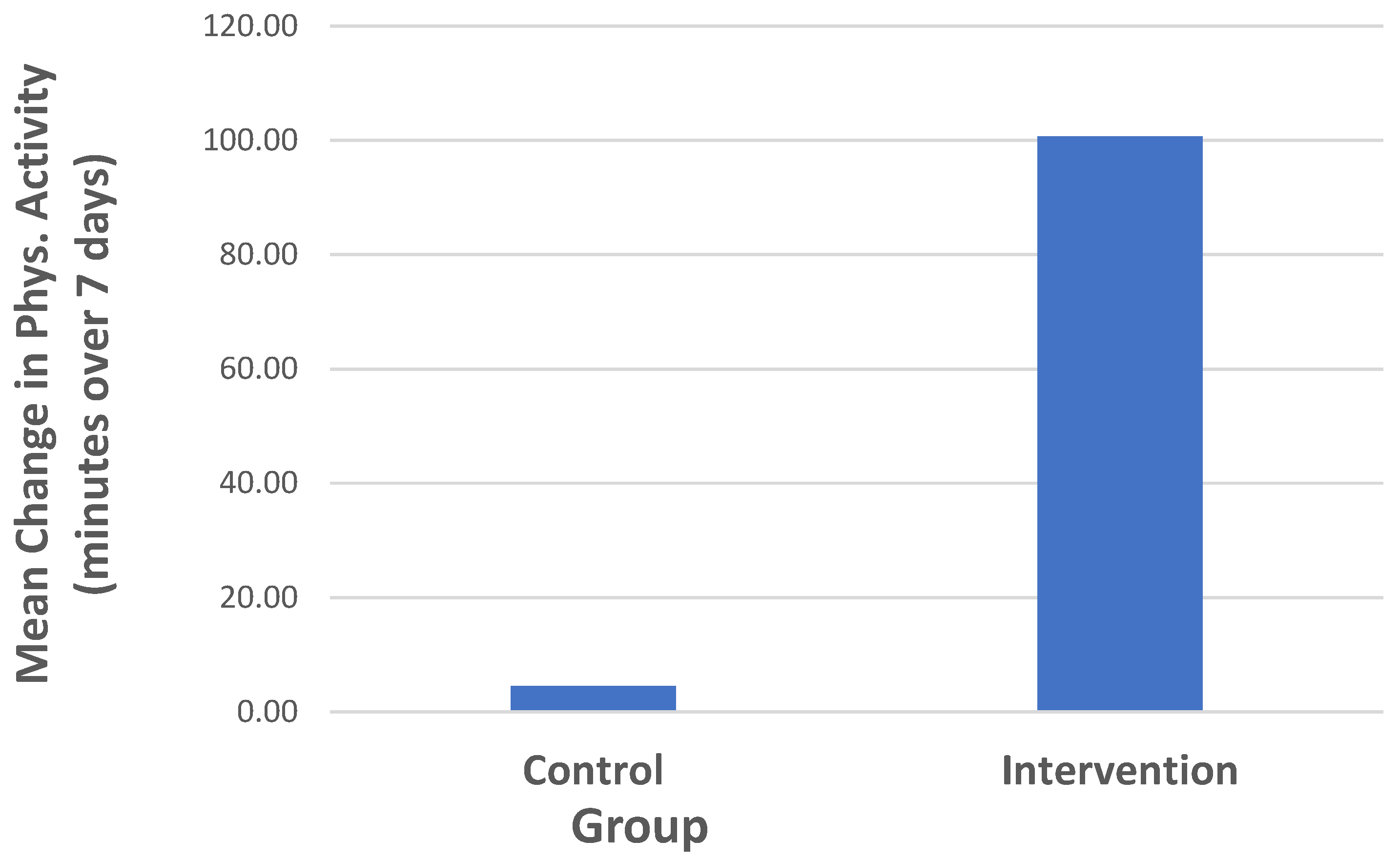
4.2. Group Differences in Primary Outcome Measures
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Browne, J.; Morey, M.C.; Beckham, J.C.; Bosworth, H.B.; Porter Starr, K.N.; Bales, C.W.; McDermott, J.; Sloane, R.; Gregg, J.J.; Hall, K.S. Diet quality and exercise in older veterans with PTSD: A pilot study. Transl. Behav. Med. 2021, 11, 2116–2122. [Google Scholar] [CrossRef]
- Kibler, J.L.; Ma, M.; Tursich, M.; Malcolm, L.; Llabre, M.M.; Greenbarg, R.; Gold, S.N.; Beckham, J.C. Cardiovascular risks in relation to posttraumatic stress severity among young trauma-exposed women. J. Affect. Disord. 2018, 241, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Scherrer, J.F.; Salas, J.; Schneider, F.D.; Friedman, M.J.; van den Berk-Clark, C.; Chard, K.M.; Norman, S.B.; Schnurr, P.P.; Tuerk, P.; Cohen, B.E.; et al. PTSD improvement and incident cardiovascular disease in more than 1000 Veterans. J. Psychosom. Res. 2020, 134, 110–128. [Google Scholar] [CrossRef] [PubMed]
- Smith, T.W.; Baron, C.E.; Caska-Wallace, C.M.; Knobloch-Fedders, L.M.; Renshaw, K.D.; Uchino, B.N. PTSD in veterans, couple behavior, and cardiovascular response during marital conflict. Emotion, 2020; ahead-of-print. [Google Scholar] [CrossRef] [PubMed]
- Jordan, H.T.; Miller-Archie, S.; Cone, J.E.; Morabia, A.; Stellman, S.D. Heart disease among adults exposed to the September 11, 2001 World Trade Center disaster: Results from the World Trade Center Health Registry. Prev. Med. 2011, 53, 370–376. [Google Scholar] [CrossRef] [PubMed]
- Reis, D.J.; Kaizer, A.M.; Kinney, A.R.; Bahraini, N.H.; Forster, J.E.; Brenner, L.A. The unique association of posttraumatic stress disorder with hypertension among veterans: A replication of Kibler et al. (2009) using Bayesian estimation and data from the United States-Veteran Microbiome Project. Psychol. Trauma Theory Res. Pract. Policy 2023, 15, 131–139. [Google Scholar] [CrossRef] [PubMed]
- Sumner, J.; Kubzansky, L.; Roberts, A.; Chen, Q.; Rimm, E.; Koenen, K. Not all posttraumatic stress disorder symptoms are equal: Fear, dysphoria, and risk of developing hypertension in trauma-exposed women. Psychol. Med. 2020, 50, 38–47. [Google Scholar] [CrossRef] [PubMed]
- Sumner, J.A.; Kubzansky, L.D.; Roberts, A.L.; Gilsanz, P.; Chen, Q.; Winning, A.; Rimm, E.; Forman, J.P.; Koenen, K.C. Posttraumatic stress disorder symptoms and risk of hypertension over 22 years in a large cohort of younger and middle-aged women. Psychol. Med. 2016, 46, 3105–3116. [Google Scholar] [CrossRef] [PubMed]
- Bourassa, K.J.; Hendrickson, R.C.; Reger, G.M.; Norr, A.M. Posttraumatic stress disorder treatment effects on cardiovascular physiology: A systematic review and agenda for future research. J. Trauma. Stress 2021, 34, 384–393. [Google Scholar] [CrossRef]
- Farr, O.M.; Sloan, D.M.; Keane, T.M.; Mantzoros, C.S. Stress- and PTSD-associated obesity and metabolic dysfunction: A growing problem requiring further research and novel treatments. Metab. Clin. Exp. 2014, 63, 1463–1468. [Google Scholar] [CrossRef]
- National Heart Lung and Blood Institute. NHLBI Working Group: The Cardiovascular Consequences of Post-Traumatic Stress Disorder. 2018. Available online: https://www.nhlbi.nih.gov/events/2018/nhlbi-working-group-cardiovascular-consequences-post-traumatic-stress-disorder (accessed on 9 September 2023).
- Hall, K.S.; Hoerster, K.D.; Yancy, W.S. Posttraumatic stress disorder, physical activity, and eating behaviors. Epidemiol. Rev. 2015, 37, 103–115. [Google Scholar] [CrossRef] [PubMed]
- Harte, C.B.; Vujanovic, A.A.; Potter, C.M. Association between exercise and posttraumatic stress symptoms among trauma-exposed adults. Eval. Health Prof. 2015, 38, 42–52. [Google Scholar] [CrossRef] [PubMed]
- Asmundson, G.J.; Stapleton, J.A. Associations between dimensions of anxiety sensitivity and PTSD symptom clusters in active-duty police officers. Cogn. Behav. Ther. 2008, 37, 66–75. [Google Scholar] [CrossRef] [PubMed]
- Stanley, I.H.; Hom, M.A.; Spencer-Thomas, S.; Joiner, T.E. Examining anxiety sensitivity as a mediator of the association between PTSD symptoms and suicide risk among women firefighters. J. Anxiety Disord. 2017, 50, 94–102. [Google Scholar] [CrossRef] [PubMed]
- Broman-Fulks, J.J.; Berman, M.E.; Rabian, B.A.; Webster, M.J. Effects of aerobic exercise on anxiety sensitivity. Behav. Res. Ther. 2004, 42, 125–136. [Google Scholar] [CrossRef] [PubMed]
- Sabourin, B.C.; Hilchey, C.A.; Lefaivre, M.J.; Watt, M.C.; Stewart, S.H. Why do they exercise less? Barriers to exercise in high-anxiety-sensitive women. Cogn. Behav. Ther. 2011, 40, 206–215. [Google Scholar] [CrossRef] [PubMed]
- Hall, K.S.; Morey, M.C.; Beckham, J.C.; Bosworth, H.B.; Sloane, R.; Pieper, C.F.; Pebole, M.M. Warrior Wellness: A randomized controlled pilot trial of the effects of exercise on physical function and clinical health risk factors in older military Veterans with PTSD. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2020, 75, 2130–2138. [Google Scholar] [CrossRef] [PubMed]
- Lamarche, L.; De Koninck, J.D. Sleep disturbance in adults with posttraumatic stress disorder: A review. J. Clin. Psychiatry 2007, 68, 1257–1270. [Google Scholar] [CrossRef]
- Mellman, T.A.; Hipolito, M.M.S. Sleep disturbances in the aftermath of trauma and posttraumatic stress disorder. CNS Spectr. 2006, 11, 611–615. [Google Scholar] [CrossRef]
- St-Onge, M.P.; Campbell, A.; Zuraikat, F.; Cheng, B.; Shah, R.; Berger, J.S.; Sampogna, R.V.; Jelic, S. Impact of change in bedtime variability on body composition and inflammation: Secondary findings from the Go Red for Women Strategically Focused Research Network. Int. J. Obes. 2020, 44, 1803–1806. [Google Scholar] [CrossRef]
- Javaheri, S.; Reid, M.; Drerup, M.; Mehra, R.; Redline, S. Reducing coronary heart disease risk through treatment of insomnia using web-based cognitive behavioral therapy for insomnia: A methodological approach. Behav. Sleep Med. 2020, 18, 334–344. [Google Scholar] [CrossRef]
- Makarem, N.; St-Onge, M.P.; Liao, M.; Lloyd-Jones, D.M.; Aggarwal, B. Association of sleep characteristics with cardiovascular health among women and differences by race/ethnicity and menopausal status: Findings from the American Heart Association Go Red for Women Strategically Focused Research Network. Sleep Health 2019, 5, 501–508. [Google Scholar] [CrossRef] [PubMed]
- Galovski, T.E.; Monson, C.; Bruce, S.E.; Resick, P.A. Does cognitive-behavioral therapy improve perceived health and sleep impairment? J. Trauma. Stress 2009, 22, 197–204. [Google Scholar] [CrossRef] [PubMed]
- Pruiksma, K.E.; Taylor, D.J.; Wachen, J.S.; Mintz, J.; Young-McCaughan, S.; Peterson, A.L.; Yarvis, J.S.; Litz, B.T.; Hembree, E.A.; Resick, P.A.; et al. Residual sleep disturbances following PTSD treatment in active duty military personnel. Psychol. Trauma Theory Res. Pract. Policy 2016, 8, 697–701. [Google Scholar] [CrossRef] [PubMed]
- Krakow, B.; Hollifield, M.; Johnston, L.; Koss, M.; Schrader, R.; Warner, T.D.; Prince, H. Imagery rehearsal therapy for chronic nightmares in sexual assault survivors with posttraumatic stress disorder: A randomized controlled trial. JAMA J. Am. Med. Assoc. 2001, 286, 537–545. [Google Scholar] [CrossRef] [PubMed]
- Moore, B.A.; Krakow, B. Imagery rehearsal therapy for acute posttraumatic nightmares among combat soldiers in Iraq. Am. J. Psychiatry 2007, 164, 683–684. [Google Scholar] [CrossRef] [PubMed]
- Eid, S.W.; Brown, R.F.; Birmingham, C.L.; Maloney, S.K. A comparison of physical activity levels, sleep disrupting behavior, and stress/affective distress as predictors of sleep as indexed by actigraphy. J. Phys. Act. Health 2021, 18, 937–948. [Google Scholar] [CrossRef] [PubMed]
- Zhu, X.; Haegele, J.A.; Liu, H.; Yu, F. Academic stress, physical activity, sleep, and mental health among Chinese adolescents. Int. J. Environ. Res. Public Health 2021, 18, 7257. [Google Scholar] [CrossRef]
- Smith, T.W.; Deits-Lebehn, C.; Caska-Wallace, C.M.; Renshaw, K.D.; Uchino, B.N. Resting high frequency heart rate variability and PTSD symptomatology in Veterans: Effects of respiration, role in elevated heart rate, and extension to spouses. Biol. Psychol. 2020, 154, 107928. [Google Scholar] [CrossRef]
- Kibler, J.L. An extension of the perseverative cognition hypothesis to PTSD symptomatology: Cardiovascular recovery in relation to PTSD severity and cognitive appraisals. J. Trauma. Stress 2018, 31, 25–34. [Google Scholar] [CrossRef]
- Steptoe, A.; Donald, A.E.; O’Donnell, K.; Marmot, M.; Deanfield, J.E. Delayed blood pressure recovery after psychological stress is associated with carotid intima-media thickness: Whitehall psychobiology study. Arteriosclerosis. Thromb. Vasc. Biol. 2006, 26, 2547–2551. [Google Scholar] [CrossRef] [PubMed]
- Steptoe, A.; Marmot, M. Impaired cardiovascular recovery following stress predicts 3-year increases in blood pressure. J. Hypertens. 2005, 23, 529–536. [Google Scholar] [CrossRef] [PubMed]
- Iverson, K.; King, M.; Cunningham, K.C.; Resick, P. Rape survivors’ trauma-related beliefs before and after Cognitive Processing Therapy: Associations with PTSD and depression symptoms. Behav. Res. Ther. 2015, 66, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Folkman, S.; Lazarus, R.S.; Gruen, J.; DeLongis, A. Appraisal, coping, health status, and psychological symptoms. J. Personal. Soc. Psychol. 1986, 50, 571–579. [Google Scholar] [CrossRef]
- Backhaus, J.; Junghanns, K.; Broocks, A.; Riemann, D.; Hohagen, F. Test-retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. J. Psychosom. Res. 2002, 53, 737–740. [Google Scholar] [CrossRef] [PubMed]
- Cole, J.C.; Motivala, S.J.; Buysse, D.J.; Oxman, M.N.; Levin, M.J.; Irwin, M.R. Validation of a 3-factor scoring model for the Pittsburgh Sleep Quality Index in older adults. Sleep 2006, 29, 112–116. [Google Scholar] [CrossRef]
- Brantley, P.J.; Bodenlos, J.S.; Cowles, M.; Whitehead, D.; Ancona, M.; Jones, G.M. Development and validation of the Weekly Stress Inventory-Short Form. J. Psychopathol. Behav. Assess. 2007, 29, 54–59. [Google Scholar] [CrossRef]
- Wortmann, J.H.; Jordan, A.H.; Weathers, F.W.; Resick, P.A.; Dondanville, K.A.; Hall-Clark, B.; Foa, E.B.; Mintz, J.; Peterson, A.L.; Litz, B.T.; et al. Psychometric analysis of the PTSD Checklist-5 (PCL-5) among treatment-seeking military service members. Psychol. Assess. 2016, 28, 1392–1403. [Google Scholar] [CrossRef]
- Beck, J.S. Cognitive Behavior Therapy: Basics and Beyond, 3rd ed.; The Guilford Press: New York, NY, USA, 2021. [Google Scholar]
- DeViva, J.C.; Zayfert, C.; Pigeon, W.R.; Mellman, T.A. Treatment of residual insomnia after CBT for PTSD: Case studies. J. Trauma. Stress 2005, 18, 155–159. [Google Scholar] [CrossRef]
- Krakow, B.J.; Melendrez, D.C.; Johnston, L.G.; Clark, J.O.; Santana, E.M.; Warner, T.D.; Lee, S.A. Sleep Dynamic Therapy for Cerro Grande Fire evacuees with posttraumatic stress symptoms: A preliminary report. J. Clin. Psychiatry 2002, 63, 673–684. [Google Scholar] [CrossRef]
- Nagaya, T.; Yoshida, H.; Takahashi, H.; Kawai, M. Cigarette smoking weakens exercise habits in healthy men. Nicotine Tob. Res. Off. J. Soc. Res. Nicotine Tob. 2007, 9, 1027–1032. [Google Scholar] [CrossRef] [PubMed]
- Prochaska, J.J.; Spring, B.; Nigg, C.R. Multiple health behavior change research: An introduction and overview. Prev. Med. 2008, 46, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Björkman, F.; Ekblom, Ö. Physical exercise as treatment for PTSD: A systematic review and meta-analysis. Mil. Med. 2021, 187, e1103–e1113. [Google Scholar] [CrossRef] [PubMed]
- Pebole, M.M.; Hall, K.S. Physical activity promotion in women with PTSD: What we need for progress. Psychol. Sport Exerc. 2019, 41, 127–129. [Google Scholar] [CrossRef] [PubMed]
- Felitti, V.J. The relation between adverse childhood experiences and adult health: Turning gold into lead. Perm. J. 2002, 6, 44–47. [Google Scholar] [PubMed]
- Kubzansky, L.D.; Koenen, K.C.; Jones, C.; Eaton, W.W. A prospective study of posttraumatic stress disorder symptoms and coronary heart disease in women. Health Psychol. Off. J. Div. Health Psychol. Am. Psychol. Assoc. 2009, 28, 125–130. [Google Scholar] [CrossRef]
- Sumner, J.A.; Kubzansky, L.D.; Elkind, M.S.; Roberts, A.L.; Agnew-Blais, J.; Chen, Q.; Cerdá, M.; Rexrode, K.M.; Rich-Edwards, J.W.; Spiegelman, D.; et al. Trauma Exposure and Posttraumatic Stress Disorder Symptoms Predict Onset of Cardiovascular Events in Women. Circulation 2015, 132, 251–259. [Google Scholar] [CrossRef]
- Hegberg, N.J.; Hayes, J.P.; Hayes, S.M. Exercise intervention in PTSD: A narrative review and rationale for implementation. Front. Psychiatry 2019, 10, 133. [Google Scholar] [CrossRef]
- Shivakumar, G.; Anderson, E.H.; Suris, A.M.; North, C.S. Exercise for PTSD in women veterans: A proof-of-concept study. Mil. Med. 2017, 182, e1809–e1814. [Google Scholar] [CrossRef]
| Participant Group | Test of Significance | ||
|---|---|---|---|
| Variable | Health Behavior Intervention | Control Group | p Value |
| Mean Age (SD) | 32.8 (13.6) | 31.8 (15.1) | 0.87 |
| Race/ethnicity (# per group): | 0.46 | ||
| Hispanic White | 1 | 1 | |
| Non-Hispanic White | 5 | 5 | |
| Carribean Black (not Hispanic) | 0 | 2 | |
| African American | 1 | 2 | |
| Asian | 2 | 0 | |
| Haitian | 2 | 1 | |
| Education (# per group): | 0.32 | ||
| High school or equivalent | 3 | 3 | |
| Associate’s Degree | 1 | 0 | |
| Bachelor’s Degree | 4 | 2 | |
| Master’s Degree | 3 | 3 | |
| Other | 0 | 3 | |
| Marital Status (# per group) | 0.38 | ||
| Single | 6 | 8 | |
| Married | 1 | 1 | |
| Divorced, separated, or widowed | 4 | 2 | |
| Income (# per group) | 0.74 | ||
| <USD 5000 | 1 | 3 | |
| USD 5000–USD 10,000 | 1 | 1 | |
| USD 10,001–USD 15,000 | 1 | 0 | |
| USD 15,001–USD 20,000 | 1 | 1 | |
| USD 20,001–USD 30,000 | 0 | 0 | |
| USD 30,001–USD 40,000 | 3 | 1 | |
| USD 40,001–USD 50,000 | 0 | 1 | |
| USD 50,001–USD 75,000 | 1 | 1 | |
| USD 75,001–USD 100,000 | 1 | 2 | |
| USD 100,000+ | 0 | 1 | |
| Analysis of Variance | |||||
|---|---|---|---|---|---|
| Source | Sum of Squares | df | Mean Square | F | Sig. |
| Between groups | 7.860 | 1 | 7.860 | 5.118 | 0.036 |
| Within groups | 29.181 | 20 | 1.536 | ||
| Total | 37.042 | 21 |
| Analysis of Variance | |||||
|---|---|---|---|---|---|
| Source | Sum of Squares | df | Mean Square | F | Sig. |
| Between groups | 64,776.648 | 1 | 64,776.648 | 2.048 | 0.169 |
| Within groups | 600,898.352 | 20 | 31,626.229 | ||
| Total | 665,675.000 | 21 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kibler, J.; Ma, M.; Hrzich, J.; Choe, J. Pilot Findings Indicate a Cognitive Behavioral Healthy Lifestyle Intervention for PTSD Improves Sleep and Physical Activity. Brain Sci. 2023, 13, 1565. https://doi.org/10.3390/brainsci13111565
Kibler J, Ma M, Hrzich J, Choe J. Pilot Findings Indicate a Cognitive Behavioral Healthy Lifestyle Intervention for PTSD Improves Sleep and Physical Activity. Brain Sciences. 2023; 13(11):1565. https://doi.org/10.3390/brainsci13111565
Chicago/Turabian StyleKibler, Jeffrey, Mindy Ma, Jacquelyn Hrzich, and Jessica Choe. 2023. "Pilot Findings Indicate a Cognitive Behavioral Healthy Lifestyle Intervention for PTSD Improves Sleep and Physical Activity" Brain Sciences 13, no. 11: 1565. https://doi.org/10.3390/brainsci13111565
APA StyleKibler, J., Ma, M., Hrzich, J., & Choe, J. (2023). Pilot Findings Indicate a Cognitive Behavioral Healthy Lifestyle Intervention for PTSD Improves Sleep and Physical Activity. Brain Sciences, 13(11), 1565. https://doi.org/10.3390/brainsci13111565







