A Narrative Commentary on the Use of a Rational Emotive Behavior Therapy-Informed Group to Address Irrational Beliefs, Posttraumatic Stress Disorder, and Comorbidities
Abstract
1. Introduction to Irrational Beliefs
2. Presence of Irrational Beliefs in Select Domains
2.1. Irrational Beliefs in PTSD
2.2. Irrational Beliefs in the Military
2.3. Irrational Beliefs in Select Civilian Contexts
2.3.1. Irrational Beliefs in Politics
2.3.2. Irrational Beliefs in Religion
2.3.3. Irrational Beliefs in Academia
3. Rational Emotive Behavior Therapy (REBT)
Relevance of REBT for PTSD
4. The Rational Emotive Behavior Therapy (REBT)-Informed Group
4.1. REBT-Informed Group Structure
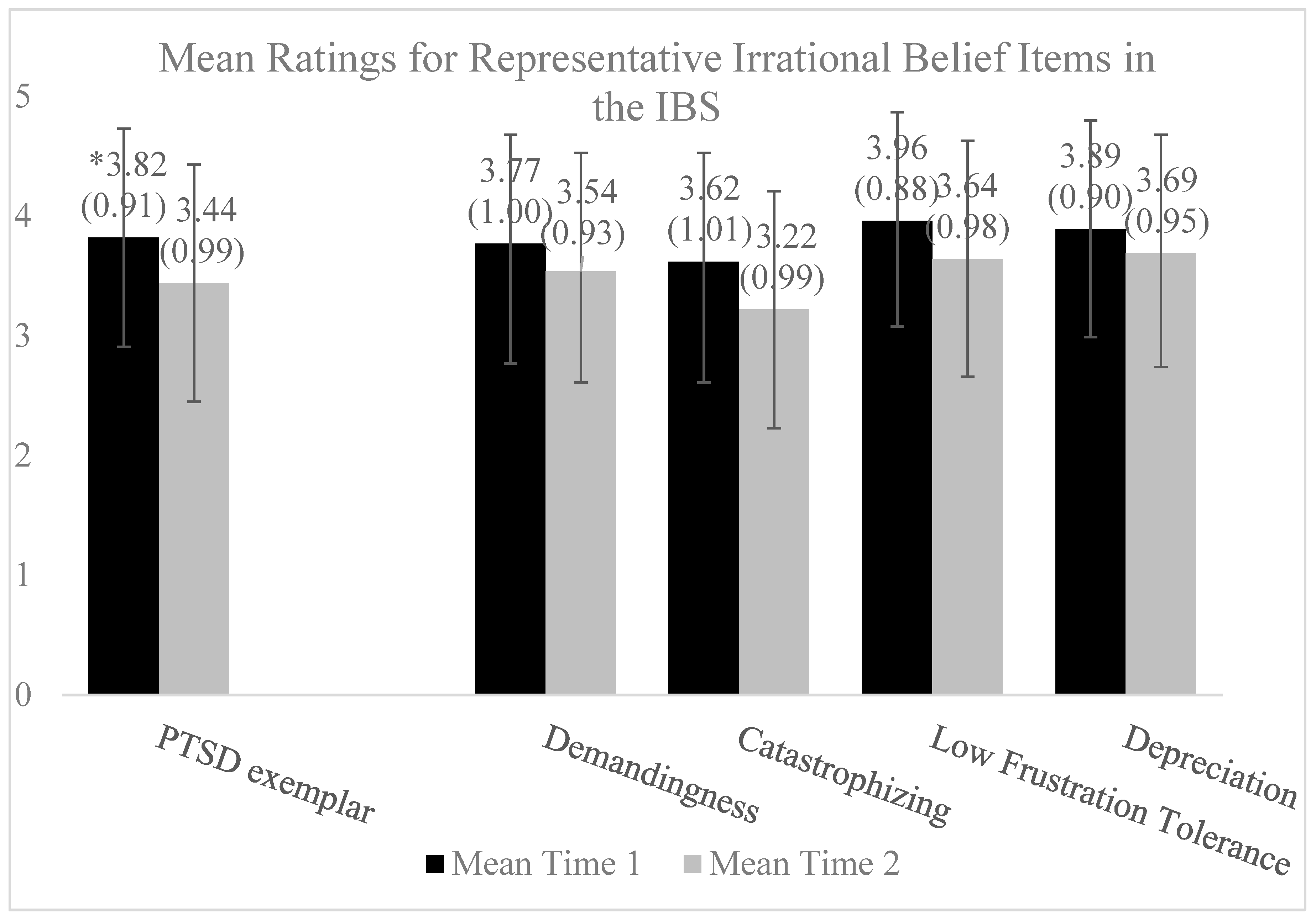
4.2. Prior Research on the REBT-Informed Group and Re-Analysis of Existing Data
5. Discussion
Supplementary Materials
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ellis, A. Reason and Emotion in Psychotherapy; Lyle Stuart: New York, NY, USA, 1962. [Google Scholar]
- Ellis, A. Early theories and practices of Rational Emotive Behavior Therapy and how they have been augmented and revised during the last three decades. J. Ration. Cogn. Ther. 2003, 21, 219–243. [Google Scholar] [CrossRef]
- Grove, A.B.; Kurtz, E.D.; Wallace, R.E.; Sheerin, C.M.; Scott, S.M. Effectiveness of a rational emotive behavior therapy (REBT)-informed group for post-9/11 Veterans with posttraumatic stress disorder (PTSD). Mil. Psychol. 2021, 33, 217–227. [Google Scholar] [CrossRef] [PubMed]
- Bernard, M.E.; Dryden, W. Advances in REBT Theory, Practice, Research, Measurement, Prevention and Promotion, 1st ed.; Springer International Publishing: Berlin/Heidelberg, Germany, 2019. [Google Scholar] [CrossRef]
- Ellis, A. A sadly neglected cognitive element in depression. Cogn. Ther. Res. 1987, 11, 121–145. [Google Scholar] [CrossRef]
- Ellis, A. Group rational-emotive and cognitive-behavioral therapy. Int. J. Group Psychother. 1992, 42, 63–80. [Google Scholar] [CrossRef] [PubMed]
- Grove, A.B.; Sheerin, C.M.; Wallace, R.E.; Green, B.A.; Minnich, A.H.; Kurtz, E.D. The effect of a reduction in irrational beliefs on posttraumatic stress disorder (PTSD), depression, and anxiety symptoms in a group treatment for post-9/11 Veterans. Mil. Psychol. 2023; Epub ahead of printing. [Google Scholar] [CrossRef] [PubMed]
- Hyland, P.; Boduszek, D. Resolving a difference between cognitive therapy and rational emotive behaviour therapy: Towards the development of an integrated CBT model of psychopathology. Ment. Health Rev. J. 2012, 17, 104–116. [Google Scholar] [CrossRef]
- Hyland, P.; Shevlin, M.; Adamson, G.; Boduszek, D. The organization of irrational beliefs in posttraumatic stress symptomology: Testing the predictions of REBT theory using structural equation modelling. J. Clin. Psychol. 2014, 70, 48–59. [Google Scholar] [CrossRef]
- Vîslă, A.; Flückiger, C.; Holtforth, M.G.; David, D. Irrational beliefs and psychological distress: A meta-analysis. Psychother. Psychosom. 2016, 85, 8–15. [Google Scholar] [CrossRef]
- Grove, A.B.; Scott, S.M.; MacPherson, A.R. Rational Emotive Behavior Therapy-Informed Treatment for Anxiety and Depression: Facilitator’s Guide. 2023. Available online: https://www.mirecc.va.gov/visn6/Docs/0987_RICVA_REBT_FacilitatorsGd_F_508.pdf (accessed on 12 January 2023).
- Hyland, P.; Shevlin, M.; Adamson, G.; Boduszek, D. Irrational beliefs in posttraumatic stress responses: A rational emotive behaviour therapy approach. J. Loss Trauma Int. Perspect. Stress Coping 2015, 20, 171–188. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar] [CrossRef]
- Clark, D.A.; Beck, A.T. Cognitive Therapy of Anxiety Disorders; Guilford Press: London, UK, 2010. [Google Scholar]
- Ellis, A. Post-traumatic stress disorder (PTSD): A rational emotive behavioral theory. J. Ration.-Emot. Cogn.-Behav. Ther. 1994, 12, 3–25. [Google Scholar] [CrossRef]
- Ellis, A. Reason and Emotion in Psychotherapy, rev. ed.; Birch Lane: Secaucus, NJ, USA, 1994. [Google Scholar]
- Crumpei, I. Secondary traumatic stress and irrational beliefs in medical students seen as premises of sensitivity to ther-apy training. Procedia-Soc. Behav. Sci. 2014, 142, 296–299. [Google Scholar] [CrossRef][Green Version]
- Resick, P.A.; Wachen, J.S.; Dondanville, K.A.; Pruiksma, K.E.; Yarvis, J.S.; Peterson, A.L.; Mintz, J.; STRONG STAR Consortium. Effect of group vs. individual Cognitive Processing Therapy in activity-duty military seeking treatment for Posttraumatic Stress Disorder: A randomized clinical trial. JAMA Psychiatry 2017, 74, 28–36. [Google Scholar] [CrossRef] [PubMed]
- DiGiuseppe, R.A.; Doyle, K.A.; Dryden, W.; Backx, W. A Practitioner’s Guide to Rational-Emotive Behavior Therapy; Oxford University Press (OUP): Oxford, UK, 2013; ISBN 9780199743049. [Google Scholar]
- Hutson, S.P.; Hall, J.M.; Pack, F.L. Survivor Guilt: Analyzing the concept and its contexts. Adv. Nurs. Sci. 2015, 38, 20–33. [Google Scholar] [CrossRef] [PubMed]
- Barr, N.; Davis, J.P.; Diguiseppi, G.; Keeling, M.; Castro, C. Direct and indirect effects of mindfulness, PTSD, and depression on self-stigma of mental illness in OEF/OIF veterans. Psychol. Trauma Theory, Res. Pract. Policy 2019, 14, 1026–1034. [Google Scholar] [CrossRef] [PubMed]
- Bonfils, K.A.; Lysaker, P.H.; Yanos, P.T.; Siegel, A.; Leonhardt, B.L.; James, A.V.; Brustuen, B.; Luedtke, B.; Davis, L.W. Self-stigma in PTSD: Prevalence and correlates. Psychiatry Res. 2018, 265, 7–12. [Google Scholar] [CrossRef]
- Hoge, C.W.; Castro, C.A.; Messer, S.C.; McGurk, D.; Cotting, D.I.; Koffman, R.L. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N. Engl. J. Med. 2004, 351, 13–22. [Google Scholar] [CrossRef]
- Mittal, D.; Drummond, K.L.; Blevins, D.; Curran, G.; Corrigan, P.; Sullivan, G. Stigma associated with PTSD: Perceptions of treatment seeking combat veterans. Psychiatr. Rehabil. J. 2013, 36, 86–92. [Google Scholar] [CrossRef]
- Harris, J.I.; Farchmin, L.; Stull, L.; Boyd, J.; Schumacher, M.; Drapalski, A.L. Prediction of changes in self-stigma among veterans participating in partial psychiatric hospitalization: The role of disability status and military cohort. Psychiatr. Rehabil. J. 2015, 38, 179–185. [Google Scholar] [CrossRef]
- Marshall-Berenz, E.C.; Vujanovic, A.A.; Bonn-Miller, M.O.; Bernstein, A.; Zvolensky, M.J. Multi-method study of distress tolerance and PTSD symptom severity in a trauma-exposed community sample. J. Trauma. Stress 2010, 23, 623–630. [Google Scholar] [CrossRef]
- Vujanovic, A.A.; Bonn-Miller, M.O.; Potter, C.M.; Marshall-Berenz, E.C.; Zvolensky, M.J. An evaluation of the association between distress tolerance and posttraumatic stress within a trauma-exposed sample. J. Psychopathol. Behav. Assess. 2011, 33, 129–135. [Google Scholar] [CrossRef]
- Boffa, J.W.; Short, N.A.; Gibby, B.A.; Stentz, L.A.; Schmidt, N.B. Distress tolerance as a mechanism of PTSD symptom change: Evidence for mediation in a treatment-seeking sample. Psychiatry Res. 2018, 267, 400–408. [Google Scholar] [CrossRef] [PubMed]
- Kovacs, M.; Beck, A.T. Maladaptive cognitive structures in depression. Am. J. Psychiatry 1978, 135, 525–533. [Google Scholar] [CrossRef] [PubMed]
- Britt, T.W. The stigma of psychological problems in a work environment: Evidence from the screening of service members returning from Bosnia. J. Appl. Soc. Psychol. 2000, 30, 1599–1618. [Google Scholar] [CrossRef]
- Harrington, N. Irrational beliefs and socio-political extremism. J. Ration.-Emot. Cogn.-Behav. Ther. 2013, 31, 167–178. [Google Scholar] [CrossRef]
- Ellis, A. An overview of the clinical theory of rational emotive therapy. In Rational-Emotive Therapy: A Skills-Based Approach; Grieger, R., Boyd, J., Eds.; Van Nostrand and Reinhold: New York, NY, USA, 1980; pp. 1–31. [Google Scholar]
- Trip, S.; Bora, C.H.; Marian, M.; Halmajan, A.; Drugas, M.I. Psychological mechanisms involved in radicalization and extremism. A rational emotive behavioral conceptualization. Front. Psychol. 2019, 10, 437. [Google Scholar] [CrossRef]
- Lazer, D.M.; Baum, M.A.; Benkler, Y.; Berinsky, A.J.; Greenhill, K.M.; Menczer, F.; Metzger, M.J.; Nyhan, B.; Pennycook, G.; Rothschild, D.; et al. The science of fake news. Science 2018, 359, 1094–109635. [Google Scholar] [CrossRef]
- Johnson, W.B. Albert Ellis and the “religionists”: A history of the dialogue. J. Psychol. Christ. 1994, 13, 301–311. [Google Scholar]
- Nielsen, S.L.; Ellis, A. A discussion with Albert Ellis: Reason, emotion and religion. J. Psychol. Christ. 1994, 13, 327–341. [Google Scholar]
- Aldahadha, B. Disputing irrational beliefs among convicted terrorists and extremist beliefs. J. Ration. Cogn. Ther. 2018, 36, 404–417. [Google Scholar] [CrossRef]
- Giannouli, V. Beliefs concerning human nature among university students and high school teachers twenty-four years ago and today. Int. J. Innov. Appl. Stud. 2013, 4, 643–648. [Google Scholar]
- Ledesma, M.C.; Calderon, D. Critical race theory in education: A review of past literature and a look to the future. Qual. Inq. 2015, 21, 206–222. [Google Scholar] [CrossRef]
- Blancke, S.; Boudry, M.; Pigliucci, M. Why do irrational beliefs mimic science? The cultural evolution of pseudoscience. Theoria 2017, 83, 78–97. [Google Scholar] [CrossRef]
- Norris, P. Cancel culture: Myth or reality? Political Stud. 2023, 71, 145–174. [Google Scholar] [CrossRef]
- Ellis, A. Why rational-emotive therapy to rational emotive behavior therapy? Psychother. Theory Res. Pract. Train. 1999, 36, 154–159. [Google Scholar] [CrossRef]
- Matweychuk, W.; DiGiuseppe, R.; Gulyayeva, O. A comparison of REBT with other cognitive behavior therapies. In Advances in REBT; Springer: Cham, Germany, 2019; pp. 47–77. [Google Scholar]
- Lynch, J.R.; Mack, L.J.; Benesek, J.; Marshall, C.; Clevinger, L.; McHenry, S.; Reynolds, S.; Mutchler, B.; Meyer, B.; Panissidi, D.; et al. PTSD Recovery Program: Treatment Manual, 3rd ed. 2015. Available online: https://www.mirecc.va.gov/visn6/Docs/PTSD_Recovery_Group_Participant_Manual_11_1_updated_04_2017_1_.pdf (accessed on 19 February 2019).
- Russo, T. Cognitive counseling for health care compliance. J. Ration. Cogn. Ther. 1987, 5, 125–134. [Google Scholar] [CrossRef]
- Foa, E.B.; Hembree, E.A.; Rothbaum, B.O. Prolonged Exposure Therapy for PTSD: Emotional Processing of Traumatic Experiences: Therapist Guide; Oxford University Press: Oxford, UK, 2007. [Google Scholar]
- Shapiro, F. EMDR, adaptive information processing, and case conceptualization. J. EMDR Pract. Res. 2007, 1, 68–87. [Google Scholar] [CrossRef]
- Asmundson, G.J.; Thorisdottir, A.S.; Roden-Foreman, J.W.; Baird, S.O.; Witcraft, S.M.; Stein, A.T.; Smits, J.A.J.; Powers, M.B. A meta-analytic review of cognitive processing therapy for adults with posttraumatic stress disorder. Cogn. Behav. Ther. 2019, 48, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.R.; Hung, K.W.; Tsai, J.C.; Chu, H.; Chung, M.H.; Chen, S.R.; Liao, Y.M.; Ou, K.L.; Chang, Y.C.; Chou, K. Efficacy of eye-movement desensitization and reprocessing for patients with posttraumatic-stress disorder: A meta-analysis of randomized controlled trials. PLoS ONE 2014, 9, e103676. [Google Scholar] [CrossRef]
- Powers, M.B.; Halpern, J.M.; Ferenschak, M.P.; Gillihan, S.J.; Foa, E.B. A meta-analytic review of prolonged exposure for posttraumatic stress disorder. Clin. Psychol. Rev. 2010, 30, 635–641. [Google Scholar] [CrossRef]
- Veterans Affairs/Department of Defense [VA/DoD]. Management of posttraumatic stress disorder and acute stress disorder. In Clinical Practice Guidelines; U.S. Government Printing Office: Washington, DC, USA, 2023. [Google Scholar]
- Kitchiner, N.J.; Lewis, C.; Roberts, N.P.; Bisson, J.I. Active duty and ex-serving military personnel with post-traumatic stress disorder treated with psychological therapies: Systematic review and meta-analysis. Eur. J. Psychotraumatol. 2019, 10, 1684226. [Google Scholar] [CrossRef]
- Fala, N.C.; Coleman, J.A.; Lynch, J.R. Anticipatory anxiety in the treatment of combat veterans with posttraumatic stress disorder. J. Aggress. Maltreatment Trauma 2016, 25, 210–229. [Google Scholar] [CrossRef]
- Edwards-Stewart, A.; Smolenski, D.J.; Bush, N.E.; Cyr, B.; Beech, E.H.; Skopp, N.A.; Belsher, B.E. Posttraumatic stress disorder treatment dropout among military and veteran populations: A systematic re-view and meta-analysis. J. Trauma. Stress 2021, 34, 808–818. [Google Scholar] [CrossRef] [PubMed]
- Burns, D.D. Feeling Good: The New Mood Therapy; Avon Books: New York, NY, USA, 1980. [Google Scholar]
- David, D.; Cotet, C.; Matu, S.; Mogoase, C.; Stefan, S. 50 years of rational-emotive and cognitive-behavioral therapy: A systematic review and meta-analysis. J. Clin. Psychol. 2018, 74, 304–318. [Google Scholar] [CrossRef] [PubMed]
- Bryant, R.A.; Moulds, M.L.; Guthrie, R.M.; Dang, S.T.; Nixon, R.D.V. Imaginal exposure alone and imaginal exposure with cognitive restructuring in treatment of posttraumatic stress disorder. J. Consult. Clin. Psychol. 2003, 71, 706–712. [Google Scholar] [CrossRef]
- Sloan, D.M.; Feinstein, B.A.; Gallagher, M.W.; Beck, J.G.; Keane, T.M. Efficacy of group treatment for posttraumatic stress disorder symptoms: A meta-analysis. Psychol. Trauma Theory Res. Pract. Policy 2013, 5, 176–183. [Google Scholar] [CrossRef]
- Rogers, C.R. The necessary and sufficient conditions of therapeutic personality change. J. Consult. Psychol. 1957, 21, 95–103. [Google Scholar] [CrossRef]
- David, D.O.; Sucală, M.; Coteț, C.; Șoflău, R.; Vălenaș, S. Empirical research in REBT theory and practice. In Advances in REBT; Springer: Cham, Germany, 2019; pp. 101–119. [Google Scholar]
- Malouff, J.M.; Schutte, N.S. Development and validation of a measure of irrational belief. J. Consult. Clin. Psychol. 1986, 54, 860–862. [Google Scholar] [CrossRef]
- Malouff, J.M.; Schutte, N.S.; McClelland, T. Examination of the relationship between irrational beliefs and state anxiety. Pers. Individ. Differ. 1992, 13, 451–456. [Google Scholar] [CrossRef]
- McDermut, J.F.; Haaga, D.A.F.; Bilek, L.A. Cognitive bias and irrational beliefs in major depression and dysphoria. Cogn. Ther. Res. 1997, 21, 459–476. [Google Scholar] [CrossRef]
- Glass, G.V.; McGaw, B.; Smith, M.L. Meta-Analysis in Social Research; Sage Publications: Beverly Hills, CA, USA, 1981. [Google Scholar]
- Cohen, J. Statistical power analysis. Curr. Dir. Psychol. Sci. 1992, 1, 98–101. [Google Scholar] [CrossRef]
- Blevins, C.A.; Weathers, F.W.; Davis, M.T.; Witte, T.K.; Domino, J.L. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. J. Trauma. Stress 2015, 28, 489–498. [Google Scholar] [CrossRef] [PubMed]
- Weathers, F.W.; Litz, B.T.; Keane, T.M.; Palmieri, P.A.; Marx, B.P.; Schnurr, P.P. The PTSD Checklist for DSM-5 (PCL-5). Scale available from the National Center for PTSD. 2013. Available online: https://www.ptsd.va.gov/professional/assessment/documents/PCL5_Standard_form.pdf (accessed on 18 August 2023).
- David, D.; Szentagotai, A.; Lupu, V.; Cosman, D. Rational emotive behavior therapy, cognitive therapy, and medication in the treatment of major depressive disorder: A randomized clinical trial, posttreatment outcomes, and six-month follow-up. J. Clin. Psychol. 2008, 64, 728–746. [Google Scholar] [CrossRef] [PubMed]
- Flory, J.D.; Yehuda, R. Comorbidity between post-traumatic stress disorder and major depressive disorder: Alternative explanations and treatment considerations. Dialog-Clin. Neurosci. 2015, 17, 141–150. [Google Scholar] [CrossRef] [PubMed]
- Hyland, P.; Shevlin, M.; Adamson, G.; Boduszek, D. The role of trauma-specific irrational beliefs and sociodemographic risk factors in posttraumatic stress re-sponses. J. Ration.-Emot. Cogn.-Behav. Ther. 2013, 31, 152–166. [Google Scholar] [CrossRef]
| 1. | 2. | 3. | 4. | 5. | |
|---|---|---|---|---|---|
| 1. Irrational beliefs | -- | ||||
| 2. Re-experiencing symptoms | .45 * | -- | |||
| 3. Avoidance symptoms | .44 * | .49 * | -- | ||
| 4. Mood and Cognitions | .55 * | .57 * | .56 * | -- | |
| 5. Hyperarousal symptoms | .50 * | .55 * | .53 * | .66 * | -- |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grove, A.B.; Green, B.A.; Kaye, S.M.; Sheerin, C.M. A Narrative Commentary on the Use of a Rational Emotive Behavior Therapy-Informed Group to Address Irrational Beliefs, Posttraumatic Stress Disorder, and Comorbidities. Brain Sci. 2024, 14, 129. https://doi.org/10.3390/brainsci14020129
Grove AB, Green BA, Kaye SM, Sheerin CM. A Narrative Commentary on the Use of a Rational Emotive Behavior Therapy-Informed Group to Address Irrational Beliefs, Posttraumatic Stress Disorder, and Comorbidities. Brain Sciences. 2024; 14(2):129. https://doi.org/10.3390/brainsci14020129
Chicago/Turabian StyleGrove, Allen B., Brooke A. Green, Savannah M. Kaye, and Christina M. Sheerin. 2024. "A Narrative Commentary on the Use of a Rational Emotive Behavior Therapy-Informed Group to Address Irrational Beliefs, Posttraumatic Stress Disorder, and Comorbidities" Brain Sciences 14, no. 2: 129. https://doi.org/10.3390/brainsci14020129
APA StyleGrove, A. B., Green, B. A., Kaye, S. M., & Sheerin, C. M. (2024). A Narrative Commentary on the Use of a Rational Emotive Behavior Therapy-Informed Group to Address Irrational Beliefs, Posttraumatic Stress Disorder, and Comorbidities. Brain Sciences, 14(2), 129. https://doi.org/10.3390/brainsci14020129






