Predicting Long-Term Recovery of Consciousness in Prolonged Disorders of Consciousness Based on Coma Recovery Scale-Revised Subscores: Validation of a Machine Learning-Based Prognostic Index
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Patient Samples
2.2. Cluster Estimation and External Validation
- (i).
- Gathering the CRS-R subscores of each patient in the reference database.
- (ii).
- Estimating centroids with partitional clustering algorithms (K-means++ clustering, 500 random initializations) [20] for each training fold of a five-fold cross-validation split.
- (iii).
- Applying a twin-sample validation approach to each validation set [21] which involved conducting both the cluster training and the validation phases on the training as well as the validation sets and obtaining two cluster labels for each sample. The two different sets of labels for the validation data were compared achieving the twin-validation accuracy for each validation fold. These metrics allowed us to check the stability of the clustering process.
- (iv).
- Aggregating twin-validation accuracies across folds in order to obtain a k-fold cross-validated twin-sample accuracy. The centroids from the fold resulting in the minimum twin-validation error were employed.
- (v).
- Assigning each patient in the external validation set (IBIA DoC-SIG database) to the cluster with minimum 6-dimensional Euclidean distance between her/his CRS-R subscores and the two cluster centroids. Thus, the assignment to a specific cluster (CDI = 0 or CDI = 1) represents the CDI of that patient.
- (i).
- The clinical diagnosis at study entry (i.e., VS/UWS vs. MCS).
- (ii).
- A binary CRS-R total score using 8 as cut-off (hence CRS-R8).
- (iii).
- A binary CRS-R total score using 10 as cut-off (hence CRS-R10)
2.3. Multivariate Analysis
3. Results
3.1. Cohort Comparison
3.2. Cluster Estimation and Validation
3.3. Multivariate Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Giacino, J.T.; Katz, D.I.; Schiff, N.D.; Whyte, J.; Ashman, E.J.; Ashwal, S.; Barbano, R.; Hammond, F.M.; Laureys, S.; Ling, G.S.F.; et al. Practice guideline update recommendations summary: Disorders of consciousness: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology; the American Congress of Rehabilitation Medicine; and the National Institute on Disability, Independent Living, and Rehabilitation Research. Neurology 2018, 91, 450–460. [Google Scholar] [CrossRef]
- Kondziella, D.; Bender, A.; Diserens, K.; van Erp, W.; Estraneo, A.; Formisano, R.; Laureys, S.; Naccache, L.; Ozturk, S.; Rohaut, B.; et al. European Academy of Neurology guideline on the diagnosis of coma and other disorders of consciousness. Eur. J. Neurol. 2020, 27, 741–756. [Google Scholar] [CrossRef]
- Laureys, S.; Celesia, G.G.; Cohadon, F.; Lavrijsen, J.; León-Carrión, J.; Sannita, W.G.; Sazbon, L.; Schmutzhard, E.; Von Wild, K.R.; Zeman, A.; et al. Unresponsive wakefulness syndrome: A new name for the vegetative state or apallic syndrome. BMC Med. 2010, 8, 68. [Google Scholar] [CrossRef]
- Giacino, J.T.; Ashwal, S.; Childs, N.; Cranford, R.; Jennett, B.; Katz, D.I.; Kelly, J.P.; Rosenberg, J.H.; Whyte, J.; Zafonte, R.D.; et al. The minimally conscious state: Definition and diagnostic criteria. Neurology 2002, 58, 349–353. [Google Scholar] [CrossRef]
- Sattin, D.; Morganti, L.; De Torres, L.; Dolce, G.; Arcuri, F.; Estraneo, A.; Cardinale, V.; Piperno, R.; Zavatta, E.; Formisano, R.; et al. Care pathways models and clinical outcomes in Disorders of consciousness. Brain Behav. 2017, 7, e00740. [Google Scholar] [CrossRef]
- Estraneo, A.; Masotta, O.; Bartolo, M.; Pistoia, F.; Perin, C.; Marino, S.; Lucca, L.; Pingue, V.; Casanova, E.; Romoli, A.; et al. Multi-center study on overall clinical complexity of patients with prolonged disorders of consciousness of different etiologies. Brain Inj. 2021, 35, 1–7. [Google Scholar] [CrossRef]
- Fins, J.J.; Bernat, J.L. Ethical, palliative, and policy considerations in disorders of consciousness. Neurology 2018, 91, 471–475. [Google Scholar] [CrossRef]
- Estraneo, A.; Moretta, P.; Loreto, V.; Lanzillo, B.; Cozzolino, A.; Saltalamacchia, A.; Lullo, F.; Santoro, L.; Trojano, L. Predictors of recovery of responsiveness in prolonged anoxic vegetative state. Neurology 2013, 80, 464–470. [Google Scholar] [CrossRef]
- Estraneo, A.; Trojano, L. Prognosis in disorders of consciousness. In Coma and Disorders of Consciousness; Schnakers, C., Ed.; Springer: Cham, Switzerland, 2018; pp. 17–36. [Google Scholar]
- Thibaut, A.; Schiff, N.; Giacino, J.; Laureys, S.; Gosseries, O. Therapeutic interventions in patients with prolonged disorders of consciousness. Lancet Neurol. 2019, 18, 600–614. [Google Scholar] [CrossRef]
- Feng, Y.; Zhang, J.; Zhou, Y.; Bai, Z.; Yin, Y. Noninvasive brain stimulation for patients with a disorder of consciousness: A systematic review and meta-analysis. Rev. Neurosci. 2020, 31, 905–914. [Google Scholar] [CrossRef]
- Giacino, J.T.; Kalmar, K.; Whyte, J. The JFK Coma Recovery Scale-Revised: Measurement characteristics and diagnostic utility. Arch. Phys. Med. Rehabil. 2004, 85, 2020–2029. [Google Scholar] [CrossRef] [PubMed]
- Estraneo, A.; De Bellis, F.; Masotta, O.; Loreto, V.; Fiorenza, S.; Sapio, M.L.; Trojano, L. Demographical and clinical indices for long-term evolution of patients in vegetative or in minimally conscious state. Brain Inj. 2019, 33, 1633–1639. [Google Scholar] [CrossRef] [PubMed]
- Estraneo, A.; Fiorenza, S.; Magliacano, A.; Formisano, R.; Mattia, D.; Grippo, A.; Romoli, A.M.; Angelakis, E.; Cassol, H.; Thibaut, A.; et al. Multicenter prospective study on predictors of short-term outcome in disorders of consciousness. Neurology 2020, 95, e1488–e1499. [Google Scholar] [CrossRef] [PubMed]
- Estraneo, A.; Magliacano, A.; Fiorenza, S.; Formisano, R.; Grippo, A.; Angelakis, E.; Cassol, H.; Thibaut, A.; Gosseries, O.; Lamberti, G.; et al. Risk factors for 2-year mortality in patients with prolonged disorders of consciousness: An international multicentre study. Eur. J. Neurol. 2022, 29, 390–399. [Google Scholar] [CrossRef] [PubMed]
- Portaccio, E.; Morrocchesi, A.; Romoli, A.M.; Hakiki, B.; Taglioli, M.P.; Lippi, E.; Di Renzone, M.; Grippo, A.; Macchi, C. Score on Coma Recovery Scale-Revised at admission predicts outcome at discharge in intensive rehabilitation after severe brain injury. Brain Inj. 2018, 32, 730–734. [Google Scholar] [CrossRef] [PubMed]
- Seel, R.T.; Sherer, M.; Whyte, J.; Katz, D.I.; Giacino, J.T.; Rosenbaum, A.M.; Hammond, F.M.; Kalmar, K.; Pape, T.L.-B.; Zafonte, R.; et al. Assessment Scales for Disorders of Consciousness: Evidence-Based Recommendations for Clinical Practice and Research. Arch. Phys. Med. Rehabil. 2010, 91, 1795–1813. [Google Scholar] [CrossRef]
- Annen, J.; Filippini, M.M.; Bonin, E.; Cassol, H.; Aubinet, C.; Carrière, M.; Gosseries, O.; Thibaut, A.; Barra, A.; Wolff, A.; et al. Diagnostic accuracy of the CRS-R index in patients with disorders of consciousness. Brain Inj. 2019, 33, 1409–1412. [Google Scholar] [CrossRef]
- Liuzzi, P.; De Bellis, F.; Magliacano, A.; Estraneo, A.; Mannini, A. Consciousness-Domain Index: A data-driven clustering-based consciousness labeling. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2022, 2022, 1062–1065. [Google Scholar] [CrossRef]
- Sinaga, K.P.; Yang, M.-S. Unsupervised K-Means Clustering Algorithm. IEEE Access 2020, 8, 80716–80727. [Google Scholar] [CrossRef]
- Halkidi, M.; Batistakis, Y.; Vazirgiannis, M. On Clustering Validation Techniques. J. Intell. Inf. Syst. 2001, 17, 107–145. [Google Scholar] [CrossRef]
- Bodien, Y.G.; Carlowicz, C.A.; Chatelle, C.; Giacino, J.T. Sensitivity and Specificity of the Coma Recovery Scale–Revised Total Score in Detection of Conscious Awareness. Arch. Phys. Med. Rehabil. 2016, 97, 490–492. [Google Scholar] [CrossRef]
- Estraneo, A.; Moretta, P.; De Tanti, A.; Gatta, G.; Giacino, J.T.; Trojano, L. An Italian multicentre validation study of the coma recovery scale-revised. Eur. J. Phys. Rehabil. Med. 2015, 51, 627–634. [Google Scholar]
- Ramspek, C.L.; Jager, K.J.; Dekker, F.W.; Zoccali, C.; van Diepen, M. External validation of prognostic models: What, why, how, when and where? Clin. Kidney J. 2020, 14, 49–58. [Google Scholar] [CrossRef]
- Cabitza, F.; Campagner, A.; Soares, F.; de Guadiana-Romualdo, L.G.; Challa, F.; Sulejmani, A.; Seghezzi, M.; Carobene, A. The importance of being external. methodological insights for the external validation of machine learning models in medicine. Comput. Methods Programs Biomed. 2021, 208, 106288. [Google Scholar] [CrossRef]
- Baricich, A. Recovery from vegetative state of patients with a severe brain injury: A 4-year real-practice prospective cohort study. Funct. Neurol. 2017, 32, 131–136. [Google Scholar] [CrossRef]
- Mosenthal, A.C.; Lavery, R.F.; Addis, M.; Kaul, S.; Ross, S.; Marburger, R.; Deitch, E.A.; Livingston, D.H. Isolated Traumatic Brain Injury: Age Is an Independent Predictor of Mortality and Early Outcome. J. Trauma 2002, 52, 907–911. [Google Scholar] [CrossRef]
- Gutchess, A. Plasticity of the aging brain: New directions in cognitive neuroscience. Science 2014, 346, 579–582. [Google Scholar] [CrossRef]
- Chen, H.; Epstein, J.; Stern, E. Neural Plasticity After Acquired Brain Injury: Evidence from Functional Neuroimaging. PMR 2010, 2, S306–S312. [Google Scholar] [CrossRef]
- Mikolic, A.; Groeniger, J.O.; Zeldovich, M.; Wilson, L.; van Lennep, J.E.R.; van Klaveren, D.; Polinder, S.; Åkerlund, C.; Amrein, K.; Andreassen, L.; et al. Explaining Outcome Differences between Men and Women following Mild Traumatic Brain Injury. J. Neurotrauma 2021, 38, 3315–3331. [Google Scholar] [CrossRef]
- Moretta, P.; Estraneo, A.; De Lucia, L.; Cardinale, V.; Loreto, V.; Trojano, L. A study of the psychological distress in family caregivers of patients with prolonged disorders of consciousness during in-hospital rehabilitation. Clin. Rehabil. 2014, 28, 717–725. [Google Scholar] [CrossRef]
- D’Ippolito, M.; Aloisi, M.; Azicnuda, E.; Silvestro, D.; Giustini, M.; Verni, F.; Formisano, R.; Bivona, U. Changes in Caregivers Lifestyle after Severe Acquired Brain Injury: A Preliminary Investigation. BioMed Res. Int. 2018, 2018, 2824081. [Google Scholar] [CrossRef]
- Formisano, R.; Azicnuda, E.; Sefid, M.K.; Zampolini, M.; Scarponi, F.; Avesani, R. Early rehabilitation: Benefits in patients with severe acquired brain injury. Neurol. Sci. 2017, 38, 181–184. [Google Scholar] [CrossRef]
- Formisano, R.; Contrada, M.; Aloisi, M.; Buzzi, M.G.; Cicinelli, P.; Della Vedova, C.; Laurenza, L.; Matteis, M.; Spanedda, F.; Vinicola, V.; et al. Improvement rate of patients with severe brain injury during post-acute intensive rehabilitation. Neurol. Sci. 2018, 39, 753–755. [Google Scholar] [CrossRef]
- Schnakers, C.; Hirsch, M.; Noé, E.; Llorens, R.; Lejeune, N.; Veeramuthu, V.; De Marco, S.; Demertzi, A.; Duclos, C.; Morrissey, A.-M.; et al. Covert Cognition in Disorders of Consciousness: A Meta-Analysis. Brain Sci. 2020, 10, 930. [Google Scholar] [CrossRef]
- Estraneo, A.; Loreto, V.; Masotta, P.O.; Pascarella, A.; Trojano, L. Do Medical Complications Impact Long-Term Outcomes in Prolonged Disorders of Consciousness? Arch. Phys. Med. Rehabil. 2018, 99, 2523–2531.e3. [Google Scholar] [CrossRef]
- Liuzzi, P.; Magliacano, A.; De Bellis, F.; Mannini, A.; Estraneo, A. Predicting outcome of patients with prolonged disorders of consciousness using machine learning models based on medical complexity. Sci. Rep. 2022, 12, 13471. [Google Scholar] [CrossRef]
| Reference (N = 190) | IBIA DoC-SIG (N = 143) | p | |
|---|---|---|---|
| Age, years | 58.5 (21.6) | 53 (35) | 0.001 |
| Sex, M | 130 (68.4) | 102 (71.3) | 0.568 |
| Time post-injury, days | 39 (33) | 56 (54) | <0.001 |
| Etiology | 0.013 | ||
| TBI | 65 (34.2) | 55 (38.5) | -- |
| HI/A | 33 (17.4) | 35 (24.5) | -- |
| Vascular | 82 (43.2) | 53 (37.1) | -- |
| Other | 10 (5.2) | 0 (0) | -- |
| Diagnosis, MCS | 97 (51.1) | 75 (52.4) | 0.801 |
| CRS-R, total score | 7 (6) | 7 (7) | 0.927 |
| Auditory | 1 (1) | 1 (2) | 0.645 |
| Visual | 1 (3) | 1 (3) | 0.607 |
| Motor | 2 (2) | 2 (4) | 0.306 |
| Oro-motor | 1 (0) | 1 (1) | 0.057 |
| Communication | 0 (0) | 0 (0) | 0.099 |
| Arousal | 2 (1) | 2 (1) | 0.991 |
| 6-month outcome, eMCS | 86 (45.3) | 54 (37.8) | 0.170 |
| 12-month outcome, eMCS | -- | 62 (43.4) | -- |
| 24-month outcome, eMCS | -- | 65 (45.5) | -- |
| Fold n | Au | V | M | OM | C | AR |
|---|---|---|---|---|---|---|
| CDI = 1 | ||||||
| 1 | 2.42 | 2.56 | 3.26 | 1.51 | 0.47 | 1.95 |
| 2 | 2.50 | 2.74 | 3.22 | 1.56 | 0.44 | 2.02 |
| 3 | 2.33 | 2.65 | 3.37 | 1.37 | 0.46 | 1.98 |
| 4 | 2.41 | 2.72 | 3.45 | 1.36 | 0.50 | 2.00 |
| 5 | 2.27 | 2.60 | 3.33 | 1.47 | 0.51 | 1.91 |
| Median | 2.41 | 2.65 | 3.33 | 1.47 | 0.47 | 1.98 |
| IQR | 0.09 | 0.12 | 0.11 | 0.14 | 0.04 | 0.05 |
| CDI = 0 | ||||||
| 1 | 0.85 | 0.58 | 1.28 | 0.66 | 0.01 | 1.31 |
| 2 | 0.82 | 0.55 | 1.41 | 0.69 | 0.03 | 1.32 |
| 3 | 0.81 | 0.54 | 1.24 | 0.66 | 0.01 | 1.28 |
| 4 | 0.91 | 0.61 | 1.22 | 0.70 | 0.01 | 1.34 |
| 5 | 0.89 | 0.54 | 1.21 | 0.73 | 0.01 | 1.30 |
| Median | 0.85 | 0.55 | 1.24 | 0.69 | 0.01 | 1.31 |
| IQR | 0.07 | 0.04 | 0.06 | 0.04 | 0.00 | 0.02 |
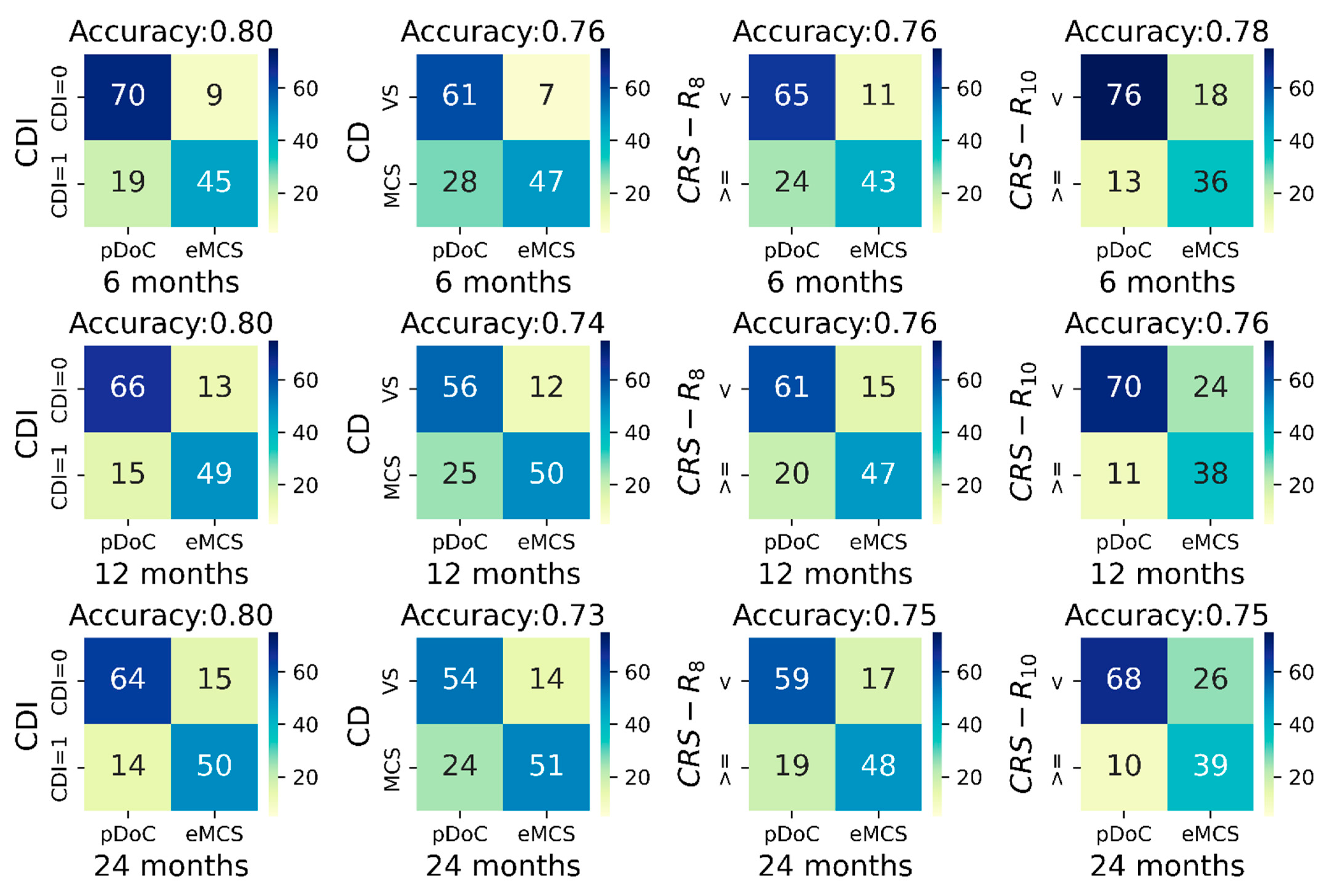
| CDI | Clinical Diagnosis | CRS-R8 | CRS-R10 | |
|---|---|---|---|---|
| 6 months | χ2 = 52.226(1), p < 0.001 | χ2 = 41.623(1), p < 0.001 | χ2 = 37.432(1), p < 0.001 | χ2 = 39.268(1), p < 0.001 |
| 12 months | χ2 = 52.013(1), p < 0.001 | χ2 = 34.895(1), p < 0.001 | χ2 = 36.859(1), p < 0.001 | χ2 = 34.461(1), p < 0.001 |
| 24 months | χ2 = 49.873(1), p < 0.001 | χ2 = 32.335(1), p < 0.001 | χ2 = 34.869(1), p < 0.001 | χ2 = 34.050(1), p < 0.001 |
| A | R2 = 0.621, AuROC = 0.902 | R2 = 0.619, AuROC = 0.898 | R2 = 0.645, AuROC = 0.907 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | |
| Age | 0.967 | 0.935–0.999 | 0.044 | 0.951 | 0.920–0.983 | 0.003 | 0.936 | 0.904–0.970 | <0.001 |
| Sex (F) | 0.359 | 0.116–1.112 | 0.076 | 0.345 | 0.113–1.050 | 0.061 | 0.305 | 0.097–0.954 | 0.051 |
| TPI | 0.971 | 0.956–0.987 | <0.001 | 0.976 | 962–991 | 0.002 | 0.977 | 0.962–0.992 | 0.003 |
| Etiology (TBI) | 0.927 | 0.246–3.833 | 0.968 | 0.338 | 0.084–1.363 | 0.127 | 0.344 | 0.082–1.442 | 0.145 |
| Etiology (HI/A) | 0.510 | 0.131–1.984 | 0.331 | 0.208 | 0.053–0.817 | 0.025 | 0.179 | 0.043–0.735 | 0.017 |
| CDI = 1 | 16.699 | 11.288–119.310 | <0.01 | 32.740 | 10.694–100.234 | <0.001 | 35.892 | 11.027–116.821 | <0.001 |
| B | R2 = 0.595, AuROC = 0.897 | R2 = 0.519, AuROC = 0.866 | R2 = 0.539, AuROC = 0.876 | ||||||
| OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | |
| Age | 0.975 | 0.945–1.007 | 0.126 | 0.964 | 0.937–0.993 | 0.014 | 0.953 | 0.925–0.982 | 0.002 |
| Sex (F) | 0.322 | 0.106–0.978 | 0.046 | 0.368 | 0.135–1.004 | 0.051 | 0.347 | 0.127–0.949 | 0.039 |
| TPI | 0.963 | 0.946–0.980 | <0.001 | 0.973 | 0.959–0.987 | <0.001 | 0.974 | 0.960–0.988 | <0.001 |
| Etiology (TBI) | 1.963 | 0.514–7.496 | 0.320 | 0.721 | 0.216–2.411 | 0.595 | 0.743 | 0.220–2.511 | 0.633 |
| Etiology (HI/A) | 0.490 | 0.131–1.839 | 0.291 | 0.256 | 0.075–0.880 | 0.031 | 0.241 | 0.069–0.837 | 0.025 |
| Diagnosis (MCS) | 32.109 | 10.753–142.243 | <0.001 | 16.431 | 5.866–46.025 | <0.001 | 15.079 | 5.366–42.376 | <0.001 |
| C | R2 = 0.573, AuROC =0.890 | R2 = 0.558, AuROC = 0.882 | R2 = 0.588, AuROC = 0.891 | ||||||
| OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | |
| Age | 0.967 | 0.937–0.999 | 0.041 | 0.954 | 0.924–0.984 | <0.001 | 0.940 | 0.910–0.972 | <0.001 |
| Sex (F) | 0.336 | 0.114–0.990 | 0.049 | 0.326 | 0.114–0.931 | 0.036 | 0.294 | 0.101–0.857 | 0.025 |
| TPI | 0.964 | 0.946–0.980 | <0.001 | 0.969 | 0.955–0.984 | <0.001 | 0.970 | 0.955–0.985 | <0.001 |
| Etiology (TBI) | 1.487 | 0.408–5.417 | 0.547 | 0.554 | 0.155–1.978 | 0.363 | 0.554 | 0.150–2.045 | 0.375 |
| Etiology (HI/A) | 0.525 | 0.141–1.953 | 0.336 | 0.234 | 0.064–0.858 | 0.028 | 0.206 | 0.054–0.781 | 0.020 |
| CRS-R8 (≥8) | 29.554 | 8.900–98.145 | <0.001 | 23.186 | 7.629–70.471 | <0.001 | 24.577 | 7.730–78.147 | <0.001 |
| D | R2 = 0.550, AuROC = 0.880 | R2 = 0.510, AuROC = 0.865 | R2 = 0.556, AuROC = 0.886 | ||||||
| OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | |
| Age | 0.973 | 0.945–1.002 | 0.070 | 0.960 | 0.932–0.988 | 0.006 | 0.946 | 0.917–0.976 | <0.001 |
| Sex (F) | 0.512 | 0.180–1.456 | 0.209 | 0.486 | 0.180–1.313 | 0.155 | 0.425 | 0.151–1.191 | 0.104 |
| TPI | 0.970 | 0.955–0.984 | <0.001 | 0.976 | 0.963–0.989 | <0.001 | 0.976 | 0.963–0.990 | <0.001 |
| Etiology (TBI) | 1.809 | 0.515–6.352 | 0.355 | 0.669 | 0.200–2.245 | 0.515 | 0.661 | 0.190–2.307 | 0.517 |
| Etiology (HI/A) | 0.633 | 0.166–2.414 | 0.503 | 0.278 | 0.077–1.007 | 0.051 | 0.238 | 0.061–0.923 | 0.038 |
| CRS-R10 (≥10) | 22.585 | 7.607–67.052 | <0.001 | 15.808 | 5.767–43.438 | <0.001 | 19.324 | 6.518-57.296 | <0.001 |
| E | R2 = 0.608, AuROC = 0.895 | R2 = 0.589, AuROC = 0.890 | R2 = 0.612, AuROC = 0.901 | ||||||
| OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | |
| Age | 0.967 | 0.937–0.998 | 0.035 | 0.953 | 0.923–0.984 | 0.003 | 0.940 | 0.909–0.972 | <0.001 |
| Sex (F) | 0.503 | 0.171–1.476 | 0.211 | 0.461 | 0.163–1.301 | 0.144 | 0.410 | 0.142–1.182 | 0.099 |
| TPI | 0.961 | 0.944–0.978 | <0.001 | 0.967 | 0.952–0.983 | <0.001 | 0.968 | 0.952–0.984 | <0.001 |
| Etiology (TBI) | 1.757 | 0.480–6.427 | 0.395 | 0.601 | 0.170–2.120 | 0.428 | 0.596 | 0.164–2.158 | 0.430 |
| Etiology (HI/A) | 0.635 | 0.160–2.524 | 0.519 | 0.254 | 0.064–0.998 | 0.050 | 0.220 | 0.053–0.909 | 0.036 |
| CRS-R total | 1.503 | 1.298–1.741 | <0.001 | 1.467 | 1.277–1.685 | <0.001 | 1.477 | 1.278–1.708 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Magliacano, A.; Liuzzi, P.; Formisano, R.; Grippo, A.; Angelakis, E.; Thibaut, A.; Gosseries, O.; Lamberti, G.; Noé, E.; Bagnato, S.; et al. Predicting Long-Term Recovery of Consciousness in Prolonged Disorders of Consciousness Based on Coma Recovery Scale-Revised Subscores: Validation of a Machine Learning-Based Prognostic Index. Brain Sci. 2023, 13, 51. https://doi.org/10.3390/brainsci13010051
Magliacano A, Liuzzi P, Formisano R, Grippo A, Angelakis E, Thibaut A, Gosseries O, Lamberti G, Noé E, Bagnato S, et al. Predicting Long-Term Recovery of Consciousness in Prolonged Disorders of Consciousness Based on Coma Recovery Scale-Revised Subscores: Validation of a Machine Learning-Based Prognostic Index. Brain Sciences. 2023; 13(1):51. https://doi.org/10.3390/brainsci13010051
Chicago/Turabian StyleMagliacano, Alfonso, Piergiuseppe Liuzzi, Rita Formisano, Antonello Grippo, Efthymios Angelakis, Aurore Thibaut, Olivia Gosseries, Gianfranco Lamberti, Enrique Noé, Sergio Bagnato, and et al. 2023. "Predicting Long-Term Recovery of Consciousness in Prolonged Disorders of Consciousness Based on Coma Recovery Scale-Revised Subscores: Validation of a Machine Learning-Based Prognostic Index" Brain Sciences 13, no. 1: 51. https://doi.org/10.3390/brainsci13010051
APA StyleMagliacano, A., Liuzzi, P., Formisano, R., Grippo, A., Angelakis, E., Thibaut, A., Gosseries, O., Lamberti, G., Noé, E., Bagnato, S., Edlow, B. L., Lejeune, N., Veeramuthu, V., Trojano, L., Zasler, N., Schnakers, C., Bartolo, M., Mannini, A., & Estraneo, A., on behalf of IBIA DoC-SIG. (2023). Predicting Long-Term Recovery of Consciousness in Prolonged Disorders of Consciousness Based on Coma Recovery Scale-Revised Subscores: Validation of a Machine Learning-Based Prognostic Index. Brain Sciences, 13(1), 51. https://doi.org/10.3390/brainsci13010051









