A Special Case of Relapsing–Remitting Bilateral Encephalitis: Without Epilepsy, but Responding to Rituximab and with a Brain Biopsy Coinciding with Rasmussen Encephalitis
Abstract
1. Introduction
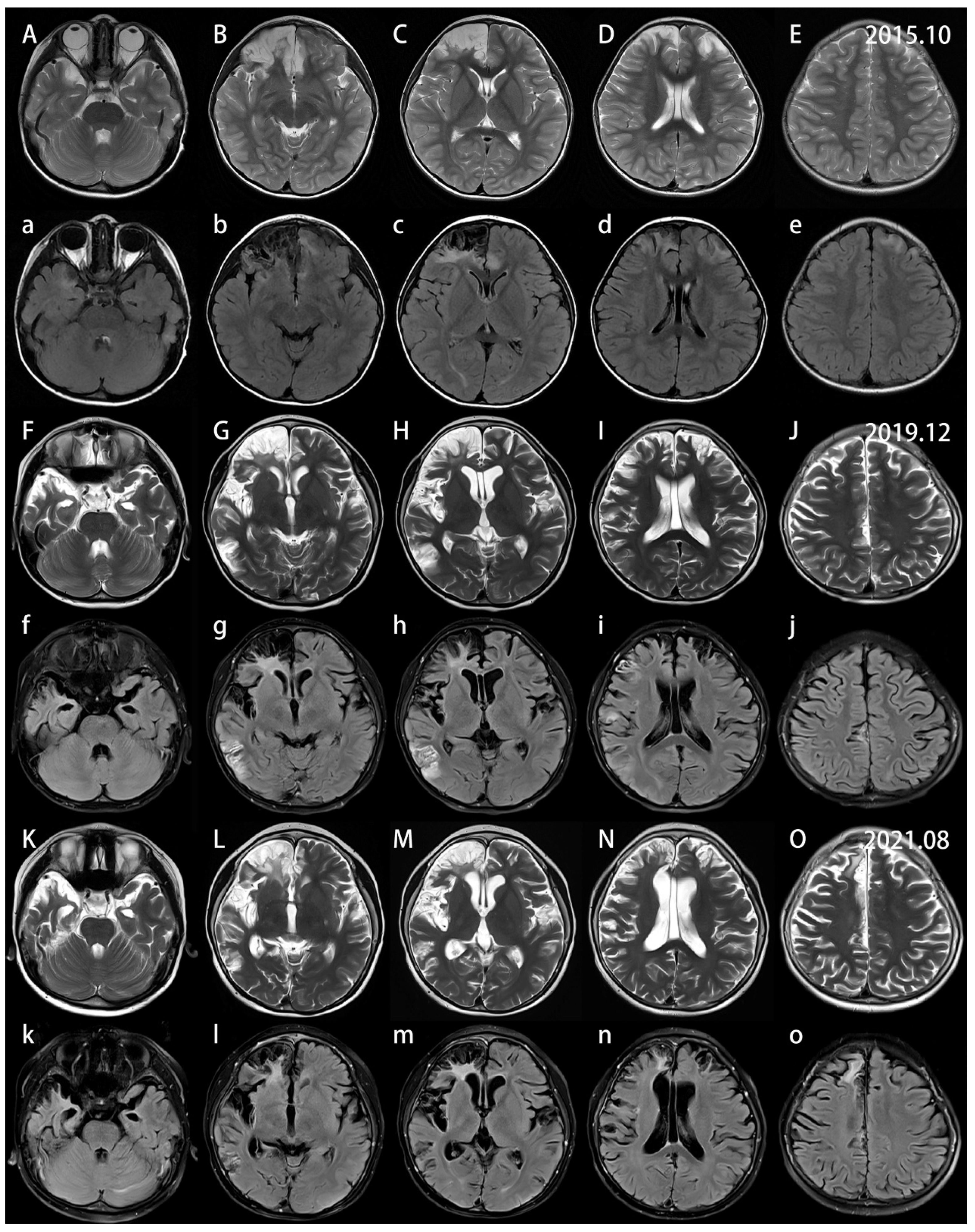
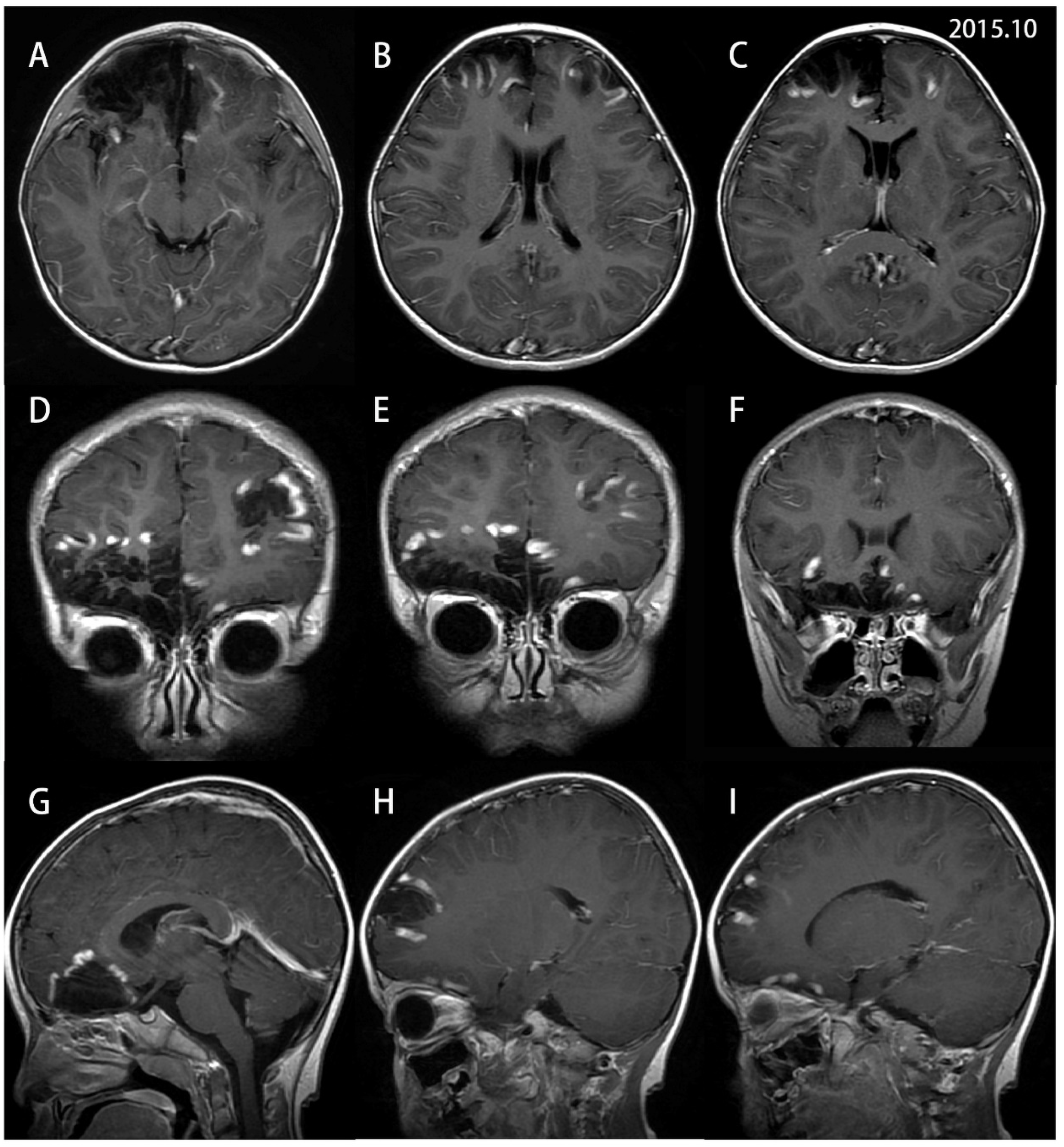
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bien, C.G.; Granata, T.; Antozzi, C.; Cross, J.H.; Dulac, O.; Kurthen, M.; Lassmann, H.; Mantegazza, R.; Villemure, J.G.; Spreafico, R.; et al. Pathogenesis, diagnosis and treatment of Rasmussen encephalitis: A European consensus statement. Brain 2005, 128, 454–471. [Google Scholar] [CrossRef] [PubMed]
- Varadkar, S.; Bien, C.G.; Kruse, C.A.; Jensen, F.E.; Bauer, J.; Pardo, C.A.; Vincent, A.; Mathern, G.W.; Cross, J.H. Rasmussen’s encephalitis: Clinical features, pathobiology, and treatment advances. Lancet Neurol. 2014, 13, 195–205. [Google Scholar] [CrossRef]
- Bien, C.G.; Tiemeier, H.; Sassen, R.; Kuczaty, S.; Urbach, H.; von Lehe, M.; Becker, A.J.; Bast, T.; Herkenrath, P.; Karenfort, M.; et al. Rasmussen encephalitis: Incidence and course under randomized therapy with tacrolimus or intravenous immunoglobulins. Epilepsia 2013, 54, 543–550. [Google Scholar] [CrossRef]
- Longaretti, F.; Dunkley, C.; Varadkar, S.; Vargha-Khadem, F.; Boyd, S.G.; Cross, J.H. Evolution of the EEG in children with Rasmussen’s syndrome. Epilepsia 2012, 53, 1539–1545. [Google Scholar] [CrossRef] [PubMed]
- Pradeep, K.; Sinha, S.; Saini, J.; Mahadevan, A.; Arivazhagan, A.; Bharath, R.D.; Bindu, P.S.; Jamuna, R.; Rao, M.B.; Chandramouli, B.A.; et al. Evolution of MRI changes in Rasmussen’s encephalitis. Acta Neurol. Scand. 2014, 130, 253–259. [Google Scholar] [CrossRef]
- Bhatjiwale, M.G.; Polkey, C.; Cox, T.C.; Dean, A.; Deasy, N. Rasmussen’s encephalitis: Neuroimaging findings in 21 patients with a closer look at the basal ganglia. Pediatr. Neurosurg. 1998, 29, 142–148. [Google Scholar] [CrossRef] [PubMed]
- Hennessy, M.J.; Koutroumanidis, M.; Dean, A.F.; Jarosz, J.; Elwes, R.D.; Binnie, C.D.; Polkey, C.E. Chronic encephalitis and temporal lobe epilepsy: A variant of Rasmussen’s syndrome? Neurology 2001, 56, 678–681. [Google Scholar] [CrossRef]
- Bien, C.G.; Widman, G.; Urbach, H.; Sassen, R.; Kuczaty, S.; Wiestler, O.D.; Schramm, J.; Elger, C.E. The natural history of Rasmussen’s encephalitis. Brain 2002, 125, 1751–1759. [Google Scholar] [CrossRef]
- Chinchilla, D.; Dulac, O.; Robain, O.; Plouin, P.; Ponsot, G.; Pinel, J.F.; Graber, D. Reappraisal of Rasmussen’s syndrome with special emphasis on treatment with high doses of steroids. J. Neurol. Neurosurg. Psychiatry 1994, 57, 1325–1333. [Google Scholar] [CrossRef]
- Tobias, S.M.; Robitaille, Y.; Hickey, W.F.; Rhodes, C.H.; Nordgren, R.; Andermann, F. Bilateral Rasmussen encephalitis: Postmortem documentation in a five-year-old. Epilepsia 2003, 44, 127–130. [Google Scholar] [CrossRef]
- Korn-Lubetzki, I.; Bien, C.G.; Bauer, J.; Gomori, M.; Wiendl, H.; Trajo, L.; Ovadia, H.; Wilken, B.; Hans, V.H.; Elger, C.E.; et al. Rasmussen encephalitis with active inflammation and delayed seizures onset. Neurology 2004, 62, 984–986. [Google Scholar] [CrossRef] [PubMed]
- Bien, C.G.; Elger, C.E.; Leitner, Y.; Gomori, M.; Ran, B.; Urbach, H.; Wilken, B.; Korn-Lubetzki, I. Slowly progressive hemiparesis in childhood as a consequence of Rasmussen encephalitis without or with delayed-onset seizures. Eur. J. Neurol. 2007, 14, 387–390. [Google Scholar] [CrossRef] [PubMed]
- McLachlan, R.S.; Girvin, J.P.; Blume, W.T.; Reichman, H. Rasmussen’s chronic encephalitis in adults. Arch. Neurol. 1993, 50, 269–274. [Google Scholar] [CrossRef] [PubMed]
- DeToledo, J.C.; Smith, D.B. Partially successful treatment of Rasmussen’s encephalitis with zidovudine: Symptomatic improvement followed by involvement of the contralateral hemisphere. Epilepsia 1994, 35, 352–355. [Google Scholar] [CrossRef]
- Hart, Y.M.; Andermann, F.; Fish, D.R.; Dubeau, F.; Robitaille, Y.; Rasmussen, T.; Berkovic, S.; Marino, R.; Yakoubian, E.M.; Spillane, K.; et al. Chronic encephalitis and epilepsy in adults and adolescents: A variant of Rasmussen’s syndrome? Neurology 1997, 48, 418–424. [Google Scholar] [CrossRef]
- Takahashi, Y.; Kubota, H.; Fujiwara, T.; Yagi, K.; Seino, M. Epilepsia partialis continua of childhood involving bilateral brain hemispheres. Acta Neurol. Scand. 1997, 96, 345–352. [Google Scholar] [CrossRef]
- Silver, K.; Andermann, F.; Meagher-Villemure, K. Familial alternating epilepsia partialis continua with chronic encephalitis: Another variant of Rasmussen syndrome? Arch. Neurol. 1998, 55, 733–736. [Google Scholar] [CrossRef][Green Version]
- Guan, Y.; Luan, G.; Zhou, J.; Liu, X. Bilateral Rasmussen encephalitis. Epilepsy Behav. 2011, 20, 398–403. [Google Scholar] [CrossRef]
- Frigeri, T.; Hemb, M.; Paglioli, E.; Hoefel, J.R.; Silva, V.; Vinters, H.; Palmini, A. Bilateral Rasmussen’s encephalitis associated with type II focal cortical dysplasia: Dormant ‘second’ epileptogenic zone in contralateral disease. Epilepsy Behav. Case Rep. 2013, 1, 66–68. [Google Scholar] [CrossRef][Green Version]
- Peariso, K.; Standridge, S.M.; Hallinan, B.E.; Leach, J.L.; Miles, L.; Mangano, F.T.; Greiner, H.M. Presentation, diagnosis and treatment of bilateral Rasmussen’s encephalitis in a 12-year-old female. Epileptic Disord. 2013, 15, 324–332. [Google Scholar] [CrossRef]
- Olson, H.E.; Lechpammer, M.; Prabhu, S.P.; Ciarlini, P.D.; Poduri, A.; Gooty, V.D.; Anjum, M.W.; Gorman, M.P.; Loddenkemper, T. Clinical application and evaluation of the Bien diagnostic criteria for Rasmussen encephalitis. Epilepsia 2013, 54, 1753–1760. [Google Scholar] [CrossRef] [PubMed]
- Faingold, R.; Onyekwelu, O.A. MRI appearance of Rasmussen encephalitis. Pediatr. Radiol. 2009, 39, 756. [Google Scholar] [CrossRef] [PubMed]
- Bien, C.G.; Urbach, H.; Deckert, M.; Schramm, J.; Wiestler, O.D.; Lassmann, H.; Elger, C.E. Diagnosis and staging of Rasmussen’s encephalitis by serial MRI and histopathology. Neurology 2002, 58, 250–257. [Google Scholar] [CrossRef] [PubMed]
- Sener, R.N. Rasmussen’s encephalitis: Proton MR spectroscopy and diffusion MR findings. J. Neuroradiol. 2000, 27, 179–184. [Google Scholar]
- Fiorella, D.J.; Provenzale, J.M.; Coleman, R.E.; Crain, B.J.; Al-Sugair, A.A. (18)F-fluorodeoxyglucose positron emission tomography and MR imaging findings in Rasmussen encephalitis. AJNR Am. J. Neuroradiol. 2001, 22, 1291–1299. [Google Scholar]
- Abboud, H.; Probasco, J.C.; Irani, S.; Ances, B.; Benavides, D.R.; Bradshaw, M.; Christo, P.P.; Dale, R.C.; Fernandez-Fournier, M.; Flanagan, E.P.; et al. Autoimmune encephalitis: Proposed best practice recommendations for diagnosis and acute management. J. Neurol. Neurosurg. Psychiatry 2021, 92, 757–768. [Google Scholar] [CrossRef]
- Derry, C.; Dale, R.C.; Thom, M.; Miller, D.H.; Giovannoni, G. Unihemispheric cerebral vasculitis mimicking Rasmussen’s encephalitis. Neurology 2002, 58, 327–328. [Google Scholar] [CrossRef]
- Ai, J.; Wang, Y.; Liu, D.; Fan, D.; Wang, Q.; Li, T.; Luan, G.; Wang, P.; An, J. Genetic Factors in Rasmussen’s Encephalitis Characterized by Whole-Exome Sequencing. Front. Neurosci. 2021, 15, 744429. [Google Scholar] [CrossRef]
- Thilo, B.; Stingele, R.; Knudsen, K.; Boor, R.; Bien, C.G.; Deuschl, G.; Lang, N. A case of Rasmussen encephalitis treated with rituximab. Nat. Rev. Neurol. 2009, 5, 458–462. [Google Scholar] [CrossRef]
- Jagtap, S.A.; Patil, S.; Joshi, A.; Kurwale, N.; Jain, V.; Deshmukh, Y. Rituximab in Rasmussen’s encephalitis: A single center experience and review of the literature. Epilepsy Behav. Rep. 2022, 19, 100540. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, P.; Lin, X.; Zong, S.; Yan, Y.; Liu, Z.; Lu, Q.; Chang, Q.; Wu, S. A Special Case of Relapsing–Remitting Bilateral Encephalitis: Without Epilepsy, but Responding to Rituximab and with a Brain Biopsy Coinciding with Rasmussen Encephalitis. Brain Sci. 2023, 13, 17. https://doi.org/10.3390/brainsci13010017
Liu P, Lin X, Zong S, Yan Y, Liu Z, Lu Q, Chang Q, Wu S. A Special Case of Relapsing–Remitting Bilateral Encephalitis: Without Epilepsy, but Responding to Rituximab and with a Brain Biopsy Coinciding with Rasmussen Encephalitis. Brain Sciences. 2023; 13(1):17. https://doi.org/10.3390/brainsci13010017
Chicago/Turabian StyleLiu, Pei, Xuemei Lin, Shenghua Zong, Yan Yan, Zhongzhong Liu, Qingli Lu, Qiaoqiao Chang, and Songdi Wu. 2023. "A Special Case of Relapsing–Remitting Bilateral Encephalitis: Without Epilepsy, but Responding to Rituximab and with a Brain Biopsy Coinciding with Rasmussen Encephalitis" Brain Sciences 13, no. 1: 17. https://doi.org/10.3390/brainsci13010017
APA StyleLiu, P., Lin, X., Zong, S., Yan, Y., Liu, Z., Lu, Q., Chang, Q., & Wu, S. (2023). A Special Case of Relapsing–Remitting Bilateral Encephalitis: Without Epilepsy, but Responding to Rituximab and with a Brain Biopsy Coinciding with Rasmussen Encephalitis. Brain Sciences, 13(1), 17. https://doi.org/10.3390/brainsci13010017





