Efficacy of Hypnosis on Dental Anxiety and Phobia: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Review Design
2.2. Eligibility Criteria
2.3. Information Sources
2.4. Search Strategy
2.5. Study Selection
2.6. Data Collection, Summary Measures, and Synthesis of Results
2.7. Assessment of Bias across Studies
3. Results
3.1. Measurement of Anxiety Reduction
3.2. DAS (Dental Anxiety Scale)
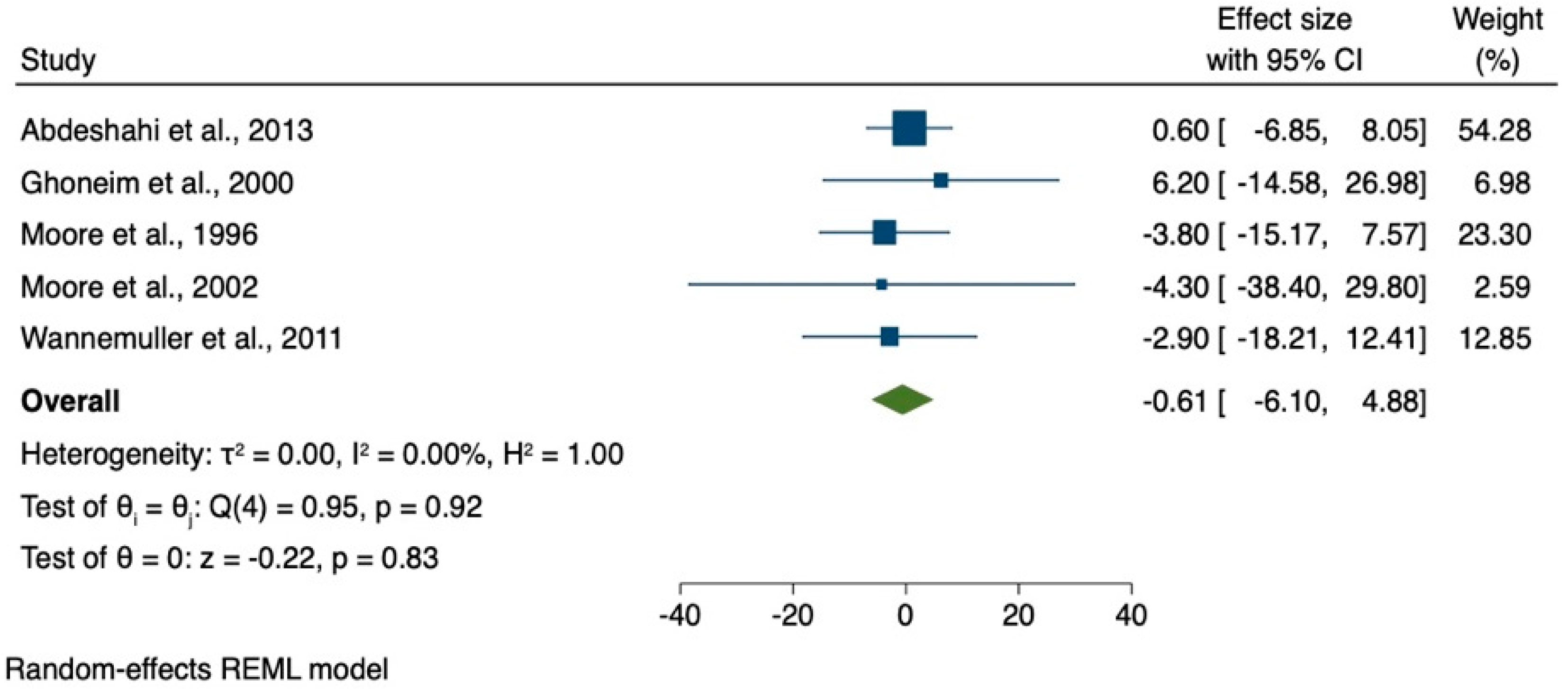
3.3. Visual Analogue Scale (VAS)
3.4. STAI—State-Trait Anxiety Inventory
3.5. Technique for Hypnosis
3.6. Anxiety Reduction by Using Hypnosis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Halsband, U.; Mueller, S.; Hinterberger, T.; Strickner, S. Plasticity changes in the brain in hypnosis and meditation. Contemp. Hypn. 2009, 26, 194–215. [Google Scholar] [CrossRef]
- Rainville, P.; Hofbauer, R.K.; Catherine Bushnell, M.; Duncan, G.H.; Price, D.D. Hypnosis modulates activity in brain structures involved in the regulation of consciousness. J. Cogn. Neurosci. 2002, 14, 887–901. [Google Scholar] [CrossRef]
- Elkins, G.R.; Barabasz, A.F.; Council, J.R.; Spiegel, D. Advancing research and practice: The revised APA Division 30 definition of hypnosis. Am. J. Clin. Hypn. 2015, 57, 378–385. [Google Scholar] [CrossRef] [PubMed]
- Facco, E. Hypnosis and Hypnotic ability between old beliefs and new evidences: An epistemological reflection. Am. J. Clin. Hypn. 2022, 64, 20–35. [Google Scholar] [CrossRef] [PubMed]
- Halsband, U.; Wolf, T.G. Functional changes in brain activity after hypnosis in patients with dental phobia. J. Physiol. Paris 2015, 109, 131–142. [Google Scholar] [CrossRef] [PubMed]
- Anthonappa, R.P.; Ashley, P.F.; Bonetti, D.L.; Lombardo, G.; Riley, P. Non-pharmacological interventions for managing dental anxiety in children. Cochrane Database Syst. Rev. 2017, 2017, CD012676. [Google Scholar] [CrossRef]
- Abdeshahi, S.K.; Hashemipour, M.A.; Mesgarzadeh, V.; Shahidi Payam, A.; Halaj Monfared, A. Effect of hypnosis on induction of local anaesthesia, pain perception, control of haemorrhage and anxiety during extraction of third molars: A case-control study. J. Cranio-Maxillofac. Surg. 2013, 41, 310–315. [Google Scholar] [CrossRef]
- Fabian, T.K.; Fabian, G. Stress of life, stress of death: Anxiety in dentistry from the viewpoint of hypnotherapy. Ann. N. Y. Acad. Sci. 1998, 851, 495–500. [Google Scholar] [CrossRef]
- Glaesmer, H.; Geupel, H.; Haak, R. A controlled trial on the effect of hypnosis on dental anxiety in tooth removal patients. Patient Educ. Couns. 2015, 98, 1112–1115. [Google Scholar] [CrossRef]
- Wolf, T.G.; Faerber, K.A.; Rummel, C.; Halsband, U.; Campus, G. Functional changes in brain activity using hypnosis: A systematic review. Brain Sci. 2015, 109, 131–142. [Google Scholar] [CrossRef]
- Schmierer, A.; Schütz, G. Zahnärztliche Hypnose, Erfolgreiche Hypnose und Kommunikation in der Zahnarztpraxis, 1st ed.; Quintessenz Verlag: Berlin, Germany, 2007; pp. 1–452. [Google Scholar]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Deveraux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PloS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef]
- Maia, L.C.; Antonio, A.G. Systematic Reviews in Dental Research. A Guideline. J. Clin. Pediatric Dent. 2012, 37, 117–124. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- Moore, R.; Brodsgaard, I.; Abrahamsen, R. A 3-year comparison of dental anxiety treatment outcomes: Hypnosis, group therapy and individual desensitization vs. no specialist treatment. Eur. J. Oral Sci. 2002, 110, 287–295. [Google Scholar] [CrossRef]
- Moore, R.; Abrahamsen, R.; Brodsgaard, I. Hypnosis compared with group therapy and individual desensitization for dental anxiety. Eur. J. Oral Sci. 1996, 104, 612–618. [Google Scholar] [CrossRef]
- Wannemueller, A.; Joehren, P.; Haug, S.; Hatting, M.; Elsesser, K.; Sartory, G. A practice-based comparison of brief cognitive behavioural treatment, two kinds of hypnosis and general anaesthesia in dental phobia. Psychother. Psychosom. 2011, 80, 159–165. [Google Scholar] [CrossRef]
- Ghoneim, M.M.; Block, R.I.; Sarasin, D.S.; Davis, C.S.; Marchman, J.N. Tape-recorded hypnosis instructions as adjuvant in the care of patients scheduled for third-molar surgery. Anesth. Analg. 2000, 90, 64–68. [Google Scholar] [CrossRef]
- Hermes, D.; Gerdes, V.; Trübger, D.; Hakim, S.G.; Sieg, P. Evaluation of intraoperative standardized hypnosis with the State-Trait Anxiety Inventory. Mund Kiefer Gesichtschir. 2004, 8, 111–117. [Google Scholar] [CrossRef]
- Ramírez-Carrasco, A.; Butrón-Téllez Girón, C.; Sanchez-Armass, O.; Pierdant-Pérez, M. Effectiveness of hypnosis in combination with conventional techniques of behavior management in anxiety/pain reduction during dental anesthetic infiltration. Pain Res. Manag. 2017, 2017, 1434015. [Google Scholar] [CrossRef]
- Holdevici, I.; Craciun, B.; Craciun, A. Using Ericksonian hypnosis techniques at patients with dental problems. Procedia Soc. Behav. Sci. 2011, 15, 2956–2962. [Google Scholar] [CrossRef][Green Version]
- Eitner, S.; Sokol, B.; Wichmann, M.; Bauer, J.; Engels, D. Clinical use of a novel audio pillow with recorded hypnotherapy instructions and music for anxiolysis during dental implant surgery: A prospective study. Int. J. Clin. Exp. Hypn. 2011, 59, 180–197. [Google Scholar] [CrossRef]
- Di Clementi, J.D.; Deffenbaugh, J.; Jackson, D. Hypnotizability, absorption and negative cognitions as predictors of dental anxiety: Two pilot studies. J. Am. Dent. Assoc. 2007, 138, 1242–1248. [Google Scholar] [CrossRef] [PubMed]
- Eitner, S.; Wichmann, M.; Schultze-Mosgau, S.; Schlegel, A.; Leher, A.; Heckmann, J.; Heckmann, S.; Holst, S. Neurophysiologic and long-term effects of clinical hypnosis in oral and maxillofacial treatment—A comparative interdisciplinary clinical study. Int. J. Clin. Exp. Hypn. 2006, 54, 457–479. [Google Scholar]
- Hermes, D.; Truebger, D.; Hakim, S.G.; Sieg, P. Tape recorded hypnosis in oral and maxillofacial surgery—Basics and first clinical experience. J. Cranio-Maxillofac. Surg. 2005, 33, 123–129. [Google Scholar] [CrossRef] [PubMed]
- Willumsen, T.; Vassend, O.; Hoffart, A. A comparison of cognitive therapy, applied relaxation, and nitrous oxide sedation in the treatment of dental fear. Acta Odontol. Scand. 2001, 59, 290–296. [Google Scholar] [CrossRef]
- Aartman, I.H.; de Jongh, A.; Makkes, P.C.; Hoogstraten, J. Treatment modalities in a dental fear clinic and the relation with general psychopathology and oral health variables. Br. Dent. J. 1999, 186, 467–471. [Google Scholar] [CrossRef] [PubMed]
- Enqvist, B.; Fischer, K. Preoperative hypnotic techniques reduce consumption of analgesics after surgical removal of third mandibular molars: A brief communication. Int. J. Clin. Exp. Hypn. 1997, 45, 102–108. [Google Scholar] [CrossRef]
- Lu, D.P.; Lu, G.P.; Hersh, E.V. Augmenting sedation with hypnosis in drug-dependent patients. Anesth. Prog. 1995, 42, 139–143. [Google Scholar]
- Hammarstrand, G.; Berggren, U.; Hakeberg, M. Psychophysiological therapy vs. hypnotherapy in the treatment of patients with dental phobia. Eur. J. Oral Sci. 1995, 103, 399–404. [Google Scholar] [CrossRef]
- Gerschman, J.A. Hypnotizability and dental phobic disorders. Anesth. Prog. 1989, 36, 131–137. [Google Scholar]
- Klimek, L.; Bergmann, K.C.; Biedermann, T.; Bousquet, J.; Hellings, P.; Jung, K.; Merk, H.; Olze, H.; Schlenter, W.; Stock, P.; et al. Visual analogue scales (VAS)—Measuring instruments for the documentation of symptoms and therapy monitoring in case of allergic rhinitis in everyday health care. Allergo J. Int. 2017, 26, 36–47. [Google Scholar] [CrossRef]
- Saletu, A.; Knaus, A.; Gritsch, F.; Gruber, G.; Anderer, P.; Walter, H. Comparative study of hypnosis using a CD versus live hypnosis in dental treatment. Hypn. Kognit. 2002, 19, 167–175. (In German) [Google Scholar]
- Häuser, W.; Hagl, M.; Schmierer, A.; Hansen, E. The efficacy, safety and applications of medical hypnosis. Dtsch. Arztebl. Int. 2016, 113, 289–296. [Google Scholar]

| No. | Year | Author | Study Design | Scales | Quality Assessment |
|---|---|---|---|---|---|
| 1 | 2017 | Ramírez-Carrasco et al. [20] | RCT | FLACC | good |
| 2 | 2015 | Halsband and Wolf [5] | CT | DFS, HAQ, DAS-R, HGSH | good |
| 3 | 2015 | Glaesmer et al. [9] | RCT | VAS, DAS | good |
| 4 | 2013 | Abdeshahi et al. [7] | CCS | VAS, STAI | good |
| 5 | 2011 | Holdevici et al. [21] | CT | DFS | good |
| 6 | 2011 | Eitner et al. [22] | RCT | AZI | good |
| 7 | 2011 | Wannemueller et al. [17] | CT | DAS, DCQ, IDCI, STAI | good |
| 8 | 2007 | Di Clementi et al. [23] | CT | DAS, HGSHS, STAI, TAS | good |
| 9 | 2006 | Eitner et al. [24] | RCT | DAS, VAS, GFS2 | good |
| 11 | 2005 | Hermes et al. [25] | CT | STAI | fair |
| 10 | 2001 | Willumsen et al. [26] | CT | DAS-R, DAS, DBS, DFS | good |
| 12 | 2002 | Moore et al. [15] | RCT | DAS, DFS, DBS, STAI, GFS1 | good |
| 13 | 2000 | Ghoneim et al. [18] | RCT | STAI, VAS | good |
| 14 | 1999 | Aartman et al. [27] | CT | DAS, S-DAI | good |
| 15 | 1997 | Enqvist and Fischer [28] | RCT | VAS | good |
| 16 | 1996 | Moore et al. [16] | RCT | DAS, DBS, DFS, GFS1, VAS, STAI, SHCS | fair |
| 17 | 1995 | Lu et al. [29] | CT | DAS-R | fair |
| 18 | 1995 | Hammarstrand et al. [30] | RCT | DAS, DSR, GFS1, MACL P, MACL C | fair |
| 19 | 1989 | Gerschman et al. [31] | CT | DAS, DFS, FSS, PRDS, VAS | good |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wolf, T.G.; Schläppi, S.; Benz, C.I.; Campus, G. Efficacy of Hypnosis on Dental Anxiety and Phobia: A Systematic Review and Meta-Analysis. Brain Sci. 2022, 12, 521. https://doi.org/10.3390/brainsci12050521
Wolf TG, Schläppi S, Benz CI, Campus G. Efficacy of Hypnosis on Dental Anxiety and Phobia: A Systematic Review and Meta-Analysis. Brain Sciences. 2022; 12(5):521. https://doi.org/10.3390/brainsci12050521
Chicago/Turabian StyleWolf, Thomas Gerhard, Sina Schläppi, Carla Irene Benz, and Guglielmo Campus. 2022. "Efficacy of Hypnosis on Dental Anxiety and Phobia: A Systematic Review and Meta-Analysis" Brain Sciences 12, no. 5: 521. https://doi.org/10.3390/brainsci12050521
APA StyleWolf, T. G., Schläppi, S., Benz, C. I., & Campus, G. (2022). Efficacy of Hypnosis on Dental Anxiety and Phobia: A Systematic Review and Meta-Analysis. Brain Sciences, 12(5), 521. https://doi.org/10.3390/brainsci12050521








