Abstract
Background. After the declaration of the pandemic status in several countries, the continuity of face-to-face visits in psychiatric facilities has been delayed or even interrupted to reduce viral spread. Little is known about the personality factors associated with medication beliefs and adherence amongst individuals with mental illness during the COVID-19 pandemic. This brief report describes a preliminary naturalistic longitudinal study that explored whether the Big Five personality traits prospectively moderate the effects of medication beliefs on changes in adherence during the pandemic for a group of outpatients with psychosis or bipolar disorder. Methods. Thirteen outpatients undergoing routine face-to-face follow-up assessments during the pandemic were included (41 observations overall) and completed the Revised Italian Version of the Ten-Item Personality Inventory, the Beliefs about Medicines Questionnaire, the Morisky Medication Adherence Scale—8-item and the Beck Depression Inventory—II. Results. Participants had stronger concerns about their psychiatric medications rather than beliefs about their necessity, and adherence to medications was generally low. Participants who had more necessity beliefs than concerns had better adherence to medications. People scoring higher in Conscientiousness and Neuroticism traits and more concerned about the medication side effects had poorer adherence. Conclusions. These preliminary data suggest the importance of a careful assessment of the adherence to medications amongst people with psychosis/bipolar disorder during the pandemic. Interventions aimed to improve adherence might focus on patients’ medication beliefs and their Conscientiousness and Neuroticism personality traits.
1. Introduction
After the declaration of the pandemic status in several countries, to reduce viral spread, the continuity of face-to-face follow-up visits in psychiatric facilities has been delayed or interrupted [1,2]. As a consequence of this change in psychiatric settings, reduced access to mental health services has become one of the predictors of poor adherence to oral medications, which in turn has increased the risk of symptom deterioration and relapse [3,4,5,6].
Regardless of the stressful effects of the pandemic, poor adherence to psychiatric medications, such as antipsychotics and mood stabilizers, is a relevant phenomenon in people with mental illness, as around 40% of people with psychosis or bipolar disorder show poor adherence, including discontinuation/intermittent intake of medication [7,8]. Such behavior can negatively impact the clinical outcomes, thus increasing the risk of recurrence of episodes [7,9,10].
Several conceptualizations have been developed to understand the factors that influence medication adherence in several medical settings, amongst the most important of which are the beliefs that patients hold about their treatment pathway and medicines [11,12,13,14,15]. According to the Necessity–Concerns Framework [16,17], these beliefs comprise the necessity of medicines in terms of potential for effectiveness but also concerns about possible adverse consequences. Based upon these beliefs, patients may decide not to continue with the prescribed medication if they perceive the necessity or the chances of success to be low or the costs (e.g., possible side effects) to be high. An increasing amount of data support the validity of this model and suggest that poor adherence is associated with beliefs of high concern and low necessity [18,19,20]. The model has received empirical support also in samples of individuals with mental illness. For example, Clatworthy and colleagues [21] found that low adherence was predicted by greater doubts about personal need for treatment and stronger concerns about potential negative effects, and that these predictors were independent of current mood state, illness, and demographic characteristics. In line with the Necessity–Concerns Framework, it has been found that medication beliefs change over time and temporal changes in medication beliefs can predict changes in adherence in the long run [22].
The Big Five model of personality [23,24] assumes that individual differences in personality characteristics can be organized into five broad trait domains: Extraversion (extraverted people experience high levels of happiness and life satisfaction), Agreeableness (individuals high in this trait are helpful, warm, and emphatic), Conscientiousness (persons high in this trait tend to be well-organized, goal-directed, and persistent), Neuroticism (persons high in this trait tend to experience strong levels of distress), and Openness (people high in openness have broad interests and seek experiences).
A relatively large number of studies have investigated the relationship between the Big Five personality traits and medication adherence in patients with chronic medical conditions [24,25]. Findings from systematic reviews showed that amongst the Big Five factors, Neuroticism and Conscientiousness are negatively and positively associated with medication adherence, respectively [26,27].
Some authors explored the role of Big Five personality traits in medication adherence amongst people with psychiatric disorders, showing that only low Conscientiousness predicted lower adherence [28]. Other researchers reported that in people with chronic diseases, Agreeableness and Conscientiousness were positively related to medication adherence, while Neuroticism was negatively associated with adherence behavior [29].
Rationale and Objectives of the Present Study
In summary, little is known about the factors associated with medication adherence amongst individuals with mental illness during the pandemic. Since face-to-face psychiatric visits have been delayed or even interrupted during the pandemic, a clearer picture of the psychological variables related to medication adherence during this stressful period may help clinicians and policymakers to plan specific interventions aimed at increasing the adherence of patients with mental disorders, in order to improve the delivery of psychiatric care and the overall effectiveness of services in the long run, when highly stressful events similar to the pandemic occur.
Starting from the available evidence, the role of medication beliefs on adherence might be moderated by specific Big Five personality traits. This brief report describes a preliminary naturalistic study that explored whether the Big Five personality traits moderated the effects of medication beliefs on changes in adherence during the pandemic for a group of outpatients with mental illness.
2. Materials and Methods
2.1. Sample Population, Eligibility Criteria, and Design
The present study was conducted in outpatients with mental illness, i.e., psychosis or bipolar disorder, recruited at the Psychiatry Unit of the Santa Maria alle Scotte University Hospital of Siena, Italy. Participants were included if: they met the criteria for a primary diagnosis of psychotic/bipolar disorder according to the Diagnostic and Statistical Manual of Mental Disorders—fifth edition (DSM-5) [30]; they were on antipsychotics and/or mood stabilizers; they were aged 18 years or older; and they provided informed consent. Participants were excluded if they had a neurological disorder, mental disability, and/or difficulty understanding written Italian. Through a longitudinal design, each one of the included patients completed the measures (for a detailed description of the measures, see paragraph below) during every monthly/bimonthly routine face-to-face follow-up psychiatric assessment from November 2020 to April 2021.
2.2. Measures
The Beliefs about Medicines Questionnaire (BMQ) [31] was used to assess patients’ cognitions regarding the medications. The BMQ is an 11-item questionnaire comprising two subscales assessing beliefs about medication prescribed for a condition, relating to perceptions about the personal need for medication (Necessity subscale) and concerns about potential negative effects from medication (Concerns subscale). The following are representative items for the Necessity and Concerns subscales, respectively: “My life would be impossible without these medications”, “I sometimes worry about the long-term effects of these medications”. The Italian translation showed good reliability [32].
The Morisky Medication Adherence Scale—8-item (MMAS-8) [33,34,35] was used to measure adherence to medications. It is an 8-item questionnaire on a 5-point Likert scale that measures adherence to medications for a given condition. It showed acceptable reliability [36].
The Beck Depression Inventory—II (BDI-II) [37] was used to assess depressive symptoms. The BDI-II is a 21-item questionnaire that rates the severity of depressive symptoms. Higher scores denote higher depression. The Italian version showed excellent reliability [38].
The Revised Italian Version of the Ten-Item Personality Inventory (I-TIPI) [39] was used to assess the Big Five personality factors. The I-TIPI is a revised version of the Ten-Item Personality Inventory [40], a questionnaire consisting of 10 items on a seven-point Likert scale that evaluates personality traits through five scales corresponding to the Big Five factors. It showed good reliability [39].
2.3. Statistical Analyses
Owing to the longitudinal design, a generalized estimating equation (GEE) model was selected to examine the relationship between a dependent variable (medication adherence, measured by the MMAS-8) and a set of predictors (beliefs about medication, BMQ; symptoms of depression, BDI-II; personality traits, I-TIPI). The difference between the BMQ Necessity and BMQ Concerns subscales (ΔBMQ) was used as an independent variable. A number of models were estimated, including models with main effects and models with both main effects and interaction terms. The goodness of fit was assessed through the quasi-likelihood under independence model criterion (QIC) and corrected QIC (QICC), looking at the model that minimized these two indices. A post-hoc power analysis was performed according to the formula proposed by Li and McKeague [41]. Given a power of 90%, a type 1 error of 0.01, an effect size of 0.025, and a conditional marginal variance estimated at 1.24, the results provided a sample size of 13 clusters (subjects) with at least 2 measurements. The assumptions of the final model were checked, and the significance level was set at p < 0.05. The analyses were performed using the Statistical Packages for Social Science (SPSS) v. 25, IBM, Chicago (USA).
3. Results
3.1. Descriptive Characteristics
Thirteen outpatients undergoing routine psychiatric face-to-face follow-up were included (socio-demographic/clinical features in Table 1). These subjects received a mean of three face-to-face assessments.

Table 1.
Socio-demographic characteristics and clinical features of the group (n = 13).
The scores of the questionnaires for all the measurements are summarized in Table 2. The subscales of the BMQ showed that respondents had stronger concerns about their medication than beliefs about the necessity of these medical treatments; the difference between the two subscale scores (BMQ) was 7 (IQ range = 6), showing that patients’ perceptions about medical treatments were mainly driven by their concerns. The degree of medication adherence, measured by the MMAS-8, was quite low: its median value was 3.5 (IQ range = 2) and only one patient showed the maximum score of 6, reflecting medium adherence. A mild level of symptoms of depression on the BDI-II was found (median = 14; IQ range = 16) but, taking into account all the measurements collected at the different time points, 4/40 (10.0%) revealed severe symptoms of depression and 9/40 (22.5%) showed a moderate level of depression.

Table 2.
Descriptive statistics of the BMQ, MMAS-8, BDI-II, and I-TIPI scores.
Participants’ personality traits are described through the I-TIPI score: this group of subjects was characterized by high levels of Agreeableness, Conscientiousness, and Neuroticism, but low levels of Extraversion and Openness. Concerning Extraversion and Openness, respectively, 67.5% and 97.5% of the patients were below the normative data according to age and sex. Concerning Agreeableness, Conscientiousness, and Neuroticism, respectively, 65%, 55%, and 70% of the patients were above the norms.
3.2. Effects of Depression, Big Five Personality Traits, and Medication Beliefs on Adherence: Main and Interaction Effects
With the aim of exploring the relationship between the dependent variable, expressed by the degree of medication adherence, and its predictors (symptoms of depression, personality traits, and beliefs about medicines), a series of GEE models were estimated, choosing the model that minimized both the QIC and QICC criteria. The final model included three predictors: the main effect of ΔBMQ, and two interaction terms (I-TIPI Conscientiousness and I-TIPI Neuroticism) with ΔBMQ. The model’s QIC and QICC were 49.7 and 45.5, respectively, and the lack of multicollinearity was confirmed by comparison between Type I and Type III sum of squares estimation. The results of the model estimation are listed in Table 3. All the parameters were significant. The positive sign of ΔBMQ showed that an increasing perception about the treatment necessity compared to concerns produced a stronger degree of medication adherence (p = 0.000). However, the model showed that some personality traits, such as Conscientiousness and Neuroticism, affected adherence to medications when they interacted with beliefs about medications: higher scores in neuroticism and conscientiousness resulted in a significant decrease in medication adherence (respectively, p = 0.001; p = 0.004).

Table 3.
Results of the model estimation.
A dichotomous value of I-TIPI Conscientiousness and Neuroticism was used, according to the normative data proposed by Goslin and colleagues [42], to better characterize the differences. Both personality traits showed that, when Conscientiousness and Neuroticism scored low, an increase in ΔBMQ did not change MMAS-8 scores. On the contrary, a direct relationship between beliefs about medications and adherence to medications was typical of subjects with high Conscientiousness and Neuroticism.
The interaction effects of personality traits on the relationship between beliefs about medications and adherence to medications are displayed in Figure 1.
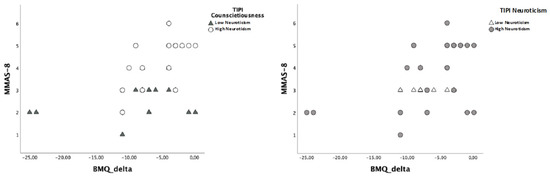
Figure 1.
Relationship between ΔBMQ and MMAS-8 scores according to different levels of I-TIPI Conscientiousness and Neuroticism.
4. Discussion
As for people with medical disorders [43,44], the COVID-19 pandemic has represented a severely stressful life event for individuals with psychiatric conditions. The results of the present study showed that, during the pandemic, people with mental illness have shown stronger concerns about their psychiatric medications than beliefs about the necessity of these treatments, and that adherence to medications is generally low in this population. The perceived necessity of the medications seems to have a more important role in adherence than perceived concerns: people who have more necessity beliefs than concerns would have better adherence to medications.
The present findings expand current knowledge about the role of medication beliefs on adherence, highlighting the moderating effects of specific personality traits. Interestingly, specific Big Five personality traits seem to moderate the relationship between medication beliefs and adherence; in particular, people with higher levels of Conscientiousness or Neuroticism traits and who perceived more concerns than necessity about the medication side effects seem to have poorer adherence. This appears to be partly consistent with the findings reported in samples with psychiatric or other chronic medical disorders assessed before the pandemic [27,28,29], where Neuroticism was a predictor of poorer medication adherence. The moderating role of Neuroticism might be related to the fact that it can include bodily self-focusing tendencies that could increase the perception of negative side effects, as reported in previous research [45].
The fact that high Conscientiousness moderates the effect of perceived concerns seems to be slightly inconsistent with the literature and the Big Five model, which assumes that Conscientiousness is a functional, goal-directed trait [24]. An explanation might be that if people who endorse higher concerns about the side effects of their medicines also have a Conscientiousness trait, they could have a persistent and goal-directed mental attitude towards a negative consideration of the side effects, which in turn could increase the likelihood of poor adherence. This explanation seems to be consistent with data highlighting the so-called downside of high levels of Conscientiousness for psychological wellbeing (i.e., the effect of high levels of Conscientiousness on low levels of wellbeing), as previously suggested [46,47]. In addition, high levels of Conscientiousness might be associated with excessive attention focused on bodily signals, typical of hypochondriac and/or obsessive–compulsive traits, which can generally be related to a catastrophic perception of the side effects of medications [48,49]. The role of Conscientiousness traits influencing a greater perception of the side effects appears to be in line also with data showing that high levels of this trait are related to a poorer understanding of the clinical information received from healthcare professionals [50].
Overall, these findings suggest the importance of the careful assessment of adherence to psychiatric medications amongst people with mental illness during the pandemic. Health education interventions aimed to improve patients’ awareness of treatment characteristics and adherence to medications during the pandemic should focus on the beliefs that individuals endorse about the medicines that they take [51]. In addition, people with Neuroticism and Conscientiousness traits and high concerns about medicines should be considered as a subgroup of patients potentially at risk of low adherence.
The small sample size should be considered as a strong limitation that might have influenced the statistical power of the analyses and prevented further analysis. Another issue is the fact that we did not explore the effects of other variables, such as different types of medications, phases of the pandemic, number of visits with psychiatric professionals during the pandemic, or patients’ socio-demographics, such as gender and foreign status, which should be analyzed in future research, since previous research showed that they are related to adherence or the clinical picture of psychosis or bipolar disorders [52,53,54]. Another shortcoming concerns the fact that the durations of the primary diagnosis and psychiatric treatment were not very homogenous, as they were around seven years, with a standard deviation or around six years. In addition, the self-report measures used to assess medication adherence should be integrated with other sources of information, such as instruments completed by informal caregivers and biological markers. Another aspect that deserves future consideration is whether the effect of personality traits and medication beliefs on adherence can, in turn, predict a higher risk of relapse.
5. Conclusions
This brief report showed that during the pandemic individuals with mental illness had stronger concerns about their oral psychiatric medications rather than beliefs about their necessity, and adherence to oral psychiatric medications was generally low. Individuals who had more necessity beliefs than concerns had better adherence to medications. People scoring higher in Conscientiousness and Neuroticism traits and more concerned about the medication side effects had poorer adherence. The present findings underline the importance of a careful assessment of the adherence to medications amongst people with these conditions during the pandemic. Interventions aimed to improve adherence might focus on patients’ medication beliefs and their Conscientiousness and Neuroticism personality traits.
Author Contributions
Conceptualization, F.F., A.C. (Anna Coluccia) and A.P.; methodology, F.F., A.G., P.F.L. and A.P.; software, F.F.; validation, A.C. (Alessandro Cuomo) and S.B.; formal analysis, F.F. and A.P.; investigation, F.F., A.G., A.F. and A.P.; resources, A.P.; data curation, F.F., P.F.L., R.C., I.C., A.D.L., J.M., O.G., G.S., G.G. and L.L.; writing—original draft preparation, F.F., A.F., A.C. (Anna Coluccia) and A.P.; writing—review and editing, V.T. and A.F.; visualization, A.C. (Alessandro Cuomo); supervision, A.C. (Anna Coluccia), A.F. and V.T.; project administration, F.F. and A.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was approved by Comitato Etico Regionale per la Sperimentazione Clinica della Regione Toscana on 15 July 2019 (approval code n° 15006). In accordance with the Helsinki Declaration, patients provided written informed consent to participate in the study.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patients to publish this paper.
Data Availability Statement
Data can be made available by the corresponding author upon request.
Acknowledgments
The MMAS-8 scale, content, name, and trademarks are protected by US copyright and trademark laws. Permission for use of the scale and its coding is required. A license agreement is available from MMAR, LLC., Donald E. Morisky, ScD, ScM, MSPH, 294 Lindura Ct., USA; donald.morisky@moriskyscale.com (accessed on 5 September 2022).
Conflicts of Interest
The authors declare no conflict of interest.
References
- Fagiolini, A.; Cuomo, A.; Frank, E. COVID-19 diary from a psychiatry department in Italy. J. Clin. Psychiatry 2020, 81, 13357. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, S.S.; MalatheshBarikar, C.; Mukherjee, A. Impact of COVID-19 pandemic on pre-existing mental health problems. Asian J. Psychiatr. 2020, 51, 102071. [Google Scholar] [CrossRef] [PubMed]
- Diolaiuti, F.; Marazziti, D.; Beatino, M.F.; Mucci, F.; Pozza, A. Impact and consequences of COVID-19 pandemic on complicated grief and persistent complex bereavement disorder. Psychiatry Res. 2021, 300, 113916. [Google Scholar] [CrossRef] [PubMed]
- Kølbæk, P.; Jefsen, O.H.; Speed, M.; Østergaard, S.D. Mental health of patients with mental illness during the COVID-19 pandemic lockdown: A questionnaire-based survey weighted for attrition. Nord. J. Psychiatry 2022, 76, 338–347. [Google Scholar] [CrossRef]
- Pozza, A.; Mucci, F.; Marazziti, D. Risk for pathological contamination fears at coronavirus time: Proposal of early intervention and prevention strategies. Clin. Neuropsychiatry 2020, 17, 100–102. [Google Scholar]
- Kane, H.; Gourret Baumgart, J.; Rusch, E.; Absil, G.; Deloyer, J.; El-Hage, W.; Marazziti, D.; Pozza, A.; Thome, J.; Tucha, O.; et al. COVID-19 and Physical Distancing Measures: Experience of Psychiatric Professionals in Europe. Int. J. Environ. Res. Public Health 2022, 19, 2214. [Google Scholar] [CrossRef]
- Sajatovic, M.; Valenstein, M.; Blow, F.C.; Ganoczy, D.; Ignacio, R.V. Treatment adherence with antipsychotic medications in bipolar disorder. Bipolar Disord. 2006, 8, 232–241. [Google Scholar] [CrossRef]
- Pozza, A.; Dèttore, D. Modular cognitive-behavioral therapy for affective symptoms in young individuals at ultra-high risk of first episode of psychosis: Randomized controlled trial. J. Clin. Psychol. 2020, 76, 392–405. [Google Scholar] [CrossRef]
- Di Capite, S.; Upthegrove, R.; Mallikarjun, P. The relapse rate and predictors of relapse in patients with first-episode psychosis following discontinuation of antipsychotic medication. Early Interv. Psychiatry 2018, 12, 893–899. [Google Scholar] [CrossRef]
- Kishi, T.; Ikuta, T.; Matsui, Y.; Inada, K.; Matsuda, Y.; Mishima, K.; Iwata, N. Effect of discontinuation v. maintenance of antipsychotic medication on relapse rates in patients with remitted/stable first-episode psychosis: A meta-analysis. Psychol. Med. 2019, 49, 772–779. [Google Scholar] [CrossRef]
- Smith, D.; Lovell, J.; Weller, C.; Kennedy, B.; Winbolt, M.; Young, C.; Ibrahim, J. A systematic review of medication non-adherence in persons with dementia or cognitive impairment. PLoS ONE 2017, 12, e0170651. [Google Scholar] [CrossRef] [PubMed]
- Gherman, A.; Schnur, J.; Montgomery, G.; Sassu, R.; Veresiu, I.; David, D. How are adherent people more likely to think? A meta-analysis of health beliefs and diabetes self-care. Diabetes Educ. 2011, 37, 392–408. [Google Scholar] [CrossRef] [PubMed]
- Massey, E.K.; Tielen, M.; Laging, M.; Beck, D.K.; Khemai, R.; van Gelder, T.; Weimar, W. The role of goal cognitions, illness perceptions and treatment beliefs in self-reported adherence after kidney transplantation: A cohort study. J. Psychosom. Res. 2013, 75, 229–234. [Google Scholar] [CrossRef]
- Pozza, A.; Coradeschi, D.; Dèttore, D. Do dysfunctional beliefs moderate the negative influence of comorbid severe depression on outcome of residential treatment for refractory OCD? A pilot study. Clin. Neuropsychiatry 2013, 10, 72–83. [Google Scholar]
- Zwikker, H.E.; van Dulmen, S.; den Broeder, A.A.; van den Bemt, B.J.; van den Ende, C.H. Perceived need to take medication is associated with medication non-adherence in patients with rheumatoid arthritis. Patient Prefer. Adher. 2014, 8, 1635. [Google Scholar] [CrossRef] [PubMed]
- Horne, R.; Chapman, S.C.; Parham, R.; Freemantle, N.; Forbes, A.; Cooper, V. Understanding patients’ adherence-related beliefs about medicines prescribed for long-term conditions: A meta-analytic review of the Necessity-Concerns Framework. PLoS ONE 2013, 8, e80633. [Google Scholar] [CrossRef] [PubMed]
- Horne, R.; Cooper, V.; Wileman, V.; Chan, A. Supporting adherence to medicines for long-term conditions: A perceptions and practicalities approach based on an extended common-sense model. Eur. Psychol. 2019, 24, 82. [Google Scholar] [CrossRef]
- De las Cuevas, C.; Betancort, M.; de Leon, J. The necessity-concern framework in the assessment of treatment adherence of psychiatric patients and the role of polypharmacy in a Spanish sample. Hum. Psychopharmacol. 2020, 35, e2721. [Google Scholar] [CrossRef]
- De las Cuevas, C.; Villasante-Tezanos, A.G.; Motuca, M.; de Leon, J. Effect of necessity-concern framework and polypharmacy on treatment adherence in psychiatric patients. Comparing an Argentinian with a Spanish sample. Hum. Psychopharmacol. 2021, 36, e2776. [Google Scholar] [CrossRef]
- Foot, H.; La Caze, A.; Gujral, G.; Cottrell, N. The necessity–concerns framework predicts adherence to medication in multiple illness conditions: A meta-analysis. Patient Educ. Counsel. 2016, 99, 706–717. [Google Scholar] [CrossRef]
- Clatworthy, J.; Bowskill, R.; Parham, R.; Rank, T.; Scott, J.; Horne, R. Understanding medication non-adherence in bipolar disorders using a Necessity-Concerns Framework. J. Affect. Disord. 2009, 116, 51–55. [Google Scholar] [CrossRef] [PubMed]
- Schüz, B.; Wurm, S.; Ziegelmann, J.P.; Warner, L.M.; Tesch-Römer, C.; Schwarzer, R. Changes in functional health, changes in medication beliefs, and medication adherence. Health Psychol. 2011, 30, 31–39. [Google Scholar] [CrossRef]
- McCrae, R.R.; Costa, P.T., Jr. Personality in Adulthood: A Five-Factor Theory Perspective, 2nd ed.; Guilford: New York, NY, USA, 2003. [Google Scholar]
- Graham, E.K.; Weston, S.J.; Gerstorf, D.; Yoneda, T.B.; Booth, T.; Beam, C.R.; Mroczek, D.K. Trajectories of big five personality traits: A coordinated analysis of 16 longitudinal samples. Eur. J. Pers. 2020, 34, 301–321. [Google Scholar] [CrossRef] [PubMed]
- Molloy, G.J.; O’Carroll, R.E.; Ferguson, E. Conscientiousness and medication adherence: A meta-analysis. Ann. Behav. Med. 2014, 47, 92–101. [Google Scholar] [CrossRef] [PubMed]
- Bruce, J.M.; Hancock, L.M.; Arnett, P.; Lynch, S. Treatment adherence in multiple sclerosis: Association with emotional status, personality, and cognition. J. Behav. Med. 2010, 33, 219–227. [Google Scholar] [CrossRef]
- Driesenaar, J. Beliefs and Adherence Regarding Inhaled Corticosteroids; Gildeprint: Enschede, The Netherlands, 2018. [Google Scholar]
- Strickland, J.C.; Stoops, W.W.; Kincer, M.A.; Rush, C.R. The impact of financial strain on medication non-adherence: Influence of psychiatric medication use. Psychiatry Res. 2019, 271, 389–395. [Google Scholar] [CrossRef]
- Axelsson, M.; Brink, E.; Lundgren, J.; Lötvall, J. The influence of personality traits on reported adherence to medication in individuals with chronic disease: An epidemiological study in West Sweden. PLoS ONE 2011, 6, e18241. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Horne, R.; Weinman, J.; Hankins, M. The Beliefs about Medicines Questionnaire: The development and evaluation of a new method for assessing the cognitive representation of medication. Psychol. Health 1999, 14, 1–24. [Google Scholar] [CrossRef]
- Argentero, P.; Torchio, E.; Tibaldi, G.; Horne, R.; Clatworthy, J.; Munizza, C. The beliefs about drug treatments. The Italian version of the BMQ (the beliefs about medicines questionnaire): Its validity and applicability. Epidemiol. Psychiatr. Sci. 2010, 19, 86–92. [Google Scholar]
- Morisky, D.E.; Ang, A.; Krousel-Wood, M.; Ward, H. Predictive Validity of Medication Adherence Measure in an Outpatient Setting. J. Clin. Hypertens. 2008, 10, 348–354. [Google Scholar] [CrossRef]
- Berlowitz, D.R.; Foy, C.G.; Kazis, L.E.; Bolin, L.; Conroy, L.B.; Fitzpatrick, P.; Gure, T.R.; Kimmel, P.L.; Kirscner, K.; for the SPRINT Study Research Group; et al. Impact of Intensive Blood Pressure Therapy on Patient-Reported Outcomes: Outcomes Results from the SPRINT Study. N. Engl. J. Med. 2017, 377, 733–744. [Google Scholar] [CrossRef] [PubMed]
- Bress, A.P.; Bellows, B.K.; King, J.; Hess, R.; Beddhu, S.; Zhang, Z.; Berlowitz, D.R.; Conroy, M.B.; Fine, L.; for the SPRINT Research Group and the SPRINT Economics and Health Related Quality of Life Subcommittee; et al. Cost-Effectiveness of Intensive versus Standard Blood Pressure Control. N. Engl. J. Med. 2017, 77, 745–755. [Google Scholar] [CrossRef] [PubMed]
- Vezzani, S.; Giannetta, E.; Altieri, B.; Barbonetti, A.; Bellastella, G.; Certo, R.; Santi, D. An Italian survey of compliance with major guidelines for l-thyroxine of primary hypothyroidism. Endocr. Pract. 2018, 24, 419–428. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.T.; Steer, R.A.; Ball, R.; Ranieri, W.F. Comparison of Beck Depression Inventories-IA and-II in psychiatric outpatients. J. Pers. Assess. 1996, 67, 588–597. [Google Scholar] [CrossRef]
- Sica, C.; Ghisi, M. The Italian versions of the Beck Anxiety Inventory and the Beck Depression Inventory-II: Psychometric properties and discriminant power. In Leading-Edge Psychological Tests and Testing Research; Lange, M.A., Ed.; Nova Science Publishers: Hauppauge, NY, USA, 2007; pp. 27–50. [Google Scholar]
- Chiorri, C.; Bracco, F.; Piccinno, T.; Modafferi, C.; Battini, V. Psychometric properties of a revised version of the Ten Item Personality Inventory. Eur. J. Psychol. Assess. 2015, 31, 109–119. [Google Scholar] [CrossRef]
- Gosling, S.D.; Rentfrow, P.J.; Swann, W.B., Jr. A very brief measure of the Big-Five personality domains. J. Res. Pers. 2003, 37, 504–528. [Google Scholar] [CrossRef]
- Li, Z.; McKeague, I.W. Power and sample size calculations for generalized estimating equations via local asymptotics. Stat. Sin. 2013, 23, 231–250. [Google Scholar] [CrossRef]
- Gosling, S.D.; Rentfrow, P.J.; Potter, J. Norms for the Ten Item Personality Inventory. Unpublished Data. Available online: https://gosling.psy.utexas.edu/scales-weve-developed/ten-item-personality-measure-tipi/ (accessed on 25 July 2022).
- Carrillo-de-la-Peña, M.T.; González-Villar, A.; Triñanes, Y. Effects of the COVID-19 pandemic on chronic pain in Spain: A scoping review. Pain Rep. 2021, 6, e899. [Google Scholar] [CrossRef]
- Pugi, D.; Dèttore, D.; Marazziti, D.; Ferretti, F.; Coluccia, A.; Coccia, M.E.; Pozza, A. Fertility-related quality of life in men undergoing medically assisted reproduction during the pandemic: Perfectionism and thought control beliefs moderate the effects of the type of treatment. Clin. Neuropsychiatry 2021, 18, 312–323. [Google Scholar]
- Christensen, A.J.; Wiebe, J.S.; Edwards, D.L.; Michels, J.D.; Lawton, W.J. Body consciousness, illness-related impairment, and patient adherence in hemodialysis. J. Consult. Clin. Psychol. 1996, 64, 147–152. [Google Scholar] [CrossRef]
- Boyce, C.J.; Wood, A.M.; Brown, G.D. The dark side of conscientiousness: Conscientious people experience greater drops in life satisfaction following unemployment. J. Res. Pers. 2010, 44, 535–539. [Google Scholar] [CrossRef]
- Carter, N.T.; Guan, L.; Maples, J.L.; Williamson, R.L.; Miller, J.D. The downsides of extreme conscientiousness for psychological well-being: The role of obsessive-compulsive tendencies. J. Pers. 2016, 84, 510–522. [Google Scholar] [CrossRef] [PubMed]
- Cox, B.J.; Borger, S.C.; Asmundson, G.J.; Taylor, S. Dimensions of hypochondriasis and the five-factor model of personality. Pers. Individ. Diff. 2000, 29, 99–108. [Google Scholar] [CrossRef]
- Sugarman, M.A.; Kirsch, I.; Huppert, J.D. Obsessive-compulsive disorder has a reduced placebo (and antidepressant) response compared to other anxiety disorders: A meta-analysis. J. Affect. Disord. 2017, 218, 217–226. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, E.; Semper, H.; Yates, J.; Fitzgerald, J.E.; Skatova, A.; James, D. The ‘dark side’and ‘bright side’of personality: When too much conscientiousness and too little anxiety are detrimental with respect to the acquisition of medical knowledge and skill. PLoS ONE 2014, 9, e88606. [Google Scholar] [CrossRef]
- Pozza, A.; Osborne, R.H.; Elsworth, G.R.; Ferretti, F.; Coluccia, A. Italian validation of the health education impact questionnaire (heiQ) in people with chronic conditions. Health Qual. Life Outcomes 2020, 18, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Coluccia, A.; Ferretti, F.; Fagiolini, A.; Pozza, A. Incidence and risk factors for psychosis among migrants in Europe: A meta-analysis of cross-sectional case-control studies. Rass. Ital. Criminol. 2015, 9, 29–39. [Google Scholar]
- Riecher-Rössler, A.; Butler, S.; Kulkarni, J. Sex and gender differences in schizophrenic psychoses—A critical review. Arch. Women’s Ment. Health 2018, 21, 627–648. [Google Scholar] [CrossRef]
- Chen, S.L.; Lee, W.L.; Liang, T.; Liao, I.C. Factors associated with gender differences in medication adherence: A longitudinal study. J. Adv. Nurs. 2014, 70, 2031–2040. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).