Severity and Changes in OCD Dimensions during COVID-19: A Two-Year Longitudinal Study
Abstract
1. Introduction
Study Aims
2. Material and Method
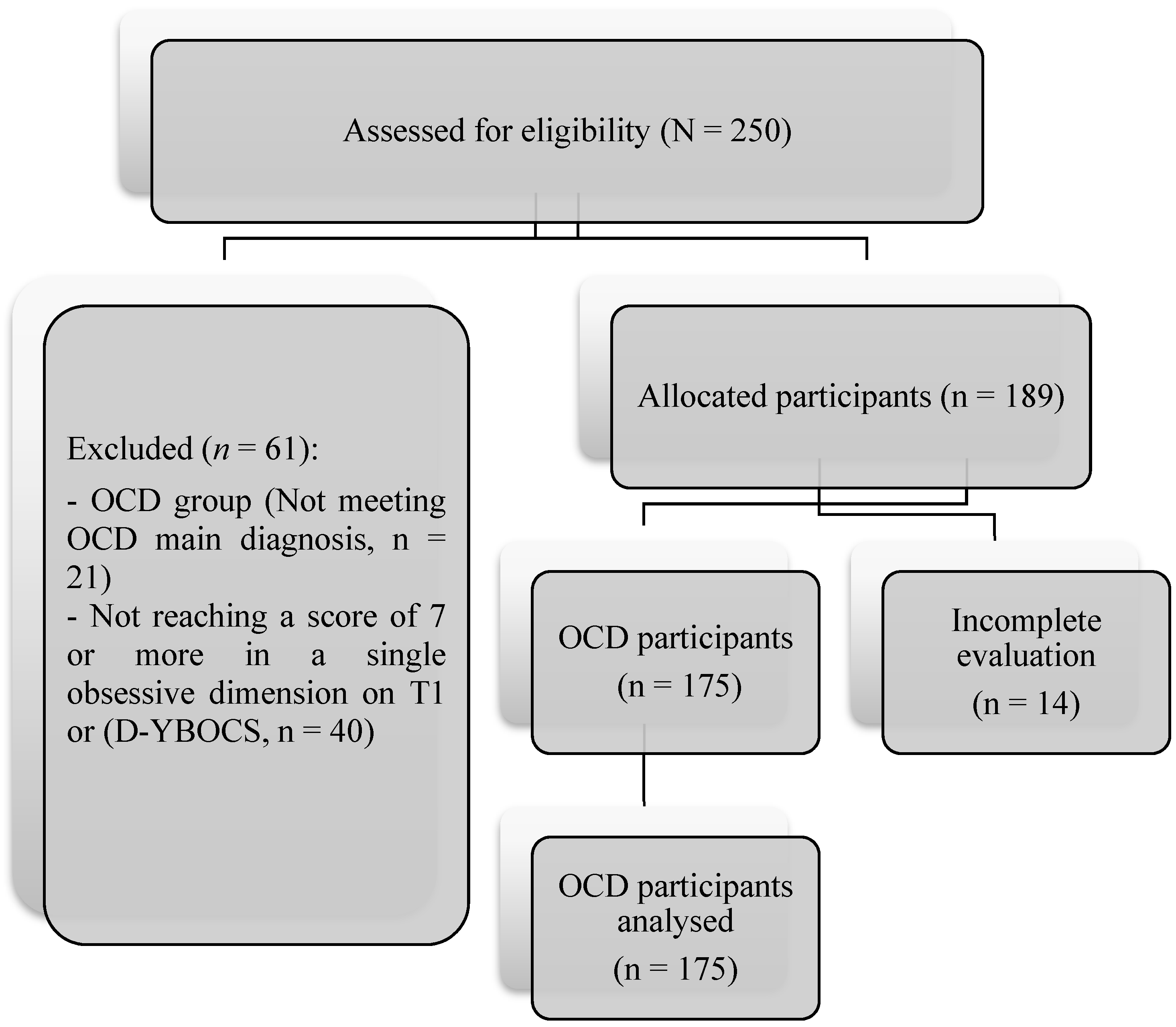
2.1. Participants
2.2. Procedure
2.3. Measures
- -
- Protocol socio-demographic and clinical variables: gender, age, educational level, marital status, duration of disorder. Sociodemographic data: age, gender, civil status, education level, employment situation, changes in employment, and/or income during the pandemic.
- -
- The Yale–Brown Obsessive Compulsive Scale (Y-BOCS) [30] is comprised of 10 items assessing severity of OCD. It contains two subscales, obsessions (range = 0–20) and compulsions (range = 0–20), and a total score (range = 0–40). The scale has a high internal consistency (α = 0.87–0.90), and good convergent validity (r = 0.74–r = 0.47). A total average greater than or equal to 16 is considered of clinical significance. Cronbach’s alpha in this study was 0.87.
- -
- Dimensional Yale–Brown Obsessive Compulsive Scale [31] evaluates the presence and severity of OC symptom dimensions (aggressive, sexual, religious, symmetry, ordering, counting, contamination, hoarding, collecting, somatic, miscellaneous obsessions, and compulsions). The D-YBOCS is in two parts. The sum of these two scores corresponds to the DYBOCS total global score (ranging from 0 to 30). The scale was administered to the clinic. Cronbach’s alpha in this study was 0.85.
- -
- Hospital Anxiety and Depression Scale [32]. Self-report measure of anxiety and depression developed of 14 items rated on a 4-point Likert scale (0 a 3). It was divided into an Anxiety subscale (HADS-A) and a Depression subscale (HADS-D), both containing seven items. Cronbach’s alpha in this study was: Depression (α = 0.81), anxiety (α = 0.79) and Total (α = 0.84).
2.4. Data Analysis
3. Results
3.1. Differences before and during COVID-19
3.2. ANOVA Mixed of Group Dimensions
3.3. Anxiety and Depression Relationship with the Y-BOCS in Each Obsessive Dimension
3.4. Mixed ANOVA Obsessive Dimensions, Anxiety and Depression
3.5. Changes in Obsessive Dimensions at T1 and T2
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Brailovskaia, J.; Margraf, J. Predicting adaptive and maladaptive responses to the Coronavirus (COVID-19) outbreak: A prospective longitudinal study. Int. J. Clin. Health Psychol. 2020, 20, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Costa, A.D.; Fernandes, A.; Ferreira, S.; Couto, B.; Machado-Sousa, M.; Moreira, P.S.; Picó-Pérez, M.; Morgado, P. Longitudinal trajectory of obsessive-compulsive symptoms in the general population during the COVID-19 pandemic. Neurosci. Appl. 2023, 2, 101112. [Google Scholar] [CrossRef]
- Bueno-Notivol, J.; Gracia-García, P.; Olaya, B.; Lasheras, I.; López-Antón, R.; Santabárbara, J. Prevalence of depression during the COVID-19 outbreak: A meta-analysis of community-based studies. Int. J. Clin. Health Psychol. 2020, 21, 100196. [Google Scholar] [CrossRef] [PubMed]
- Mazza, M.G.; De Lorenzo, R.; Conte, C.; Poletti, S.; Vai, B.; Bollettini, I.; Melloni, E.M.T.; Furlan, R.; Ciceri, F.; Rovere-Querini, P.; et al. Anxiety and depression in COVID-19 survivors: Role of inflammatory and clinical predictors. Brain Behav. Immun. 2020, 89, 594–600. [Google Scholar] [CrossRef]
- Fineberg, N.A.; Van Ameringen, M.; Drummond, L.; Hollander, E.; Stein, D.J.; Geller, D.; Pallanti, S.; Pellegrini, L.; Zohar, J.; Rodriguez, C.I.; et al. How to manage obsessive-compulsive disorder (OCD) under COVID-19: A clinician’s guide from the International College of Obsessive Compulsive Spectrum Disorders (ICOCS) and the Obsessive-Compulsive Research Network (OCRN) of the European College of Neuropsychopharmacology. Compr. Psychiat. 2020, 100, 152174. [Google Scholar] [CrossRef]
- Rivera, R.M.; Carballea, D. Coronavirus: A trigger for OCD and illness anxiety disorder? Psychol. Trauma. Theory Res. Pr. Policy 2020, 12, S66. [Google Scholar] [CrossRef]
- Silva, R.M.; Shavitt, R.G.; Costa, D.L. Obsessive-compulsive disorder during the COVID-19 pandemic. Rev. Bras. Psiquiatr. 2021, 43, 108. [Google Scholar] [CrossRef]
- Ivbijaro, G.; Brooks, C.; Kolkiewicz, L.; Sunkel, C.; Long, A. Psychological impact and psychosocial consequences of the COVID 19 pandemic Resilience, mental well-being, and the coronavirus pandemic. Indian J. Psychiatry 2020, 62, S395. [Google Scholar] [CrossRef]
- Prestia, D.; Pozza, A.; Olcese, M.; Escelsior, A.; Dettore, D.; Amore, M. The impact of the COVID-19 pandemic on patients with OCD: Effects of contamination symptoms and remission state before the quarantine in a preliminary naturalistic study. Psychiatry Res. 2020, 291, 113213. [Google Scholar] [CrossRef]
- Fontenelle, L.F.; Miguel, E.C. The impact of COVID-19 in the diagnosis and treatment of obsessive-compulsive disorder. Depress. Anxiety 2020, 37, 510–511. [Google Scholar] [CrossRef]
- Pozza, A.; Mucci, F.; Marazziti, D. Risk for pathological contamination fears at coronavirus time: Proposal of early intervention and prevention strategies. Clin. Neuropsychiatry 2020, 17, 100–102. [Google Scholar] [CrossRef]
- Jelinek, L.; Göritz, A.S.; Miegel, F.; Moritz, S.; Kriston, L. Predictors of trajectories of obsessive-compulsive symptoms during the COVID-19 pandemic in the general population in Germany. Transl. Psychiatry 2021, 11, 323. [Google Scholar] [CrossRef]
- Samuels, J.; Holingue, C.; Nestadt, P.S.; Bienvenu, O.J.; Phan, P.; Nestadt, G. Contamination-related behaviors, obsessions, and compulsions during the COVID-19 pandemic in a United States population sample. J. Psychiat. Res. 2021, 138, 155–162. [Google Scholar] [CrossRef]
- Abba-Aji, A.; Li, D.; Hrabok, M.; Shalaby, R.; Gusnowski, A.; Vuong, W.; Surood, S.; Nkire, N.; Li, X.M.; Greenshaw, A.J.; et al. COVID-19 Pandemic and Mental Health: Prevalence and Correlates of New-Onset Obsessive-Compulsive Symptoms in a Canadian Province. Int. J. Environ. Res. Public. Health 2020, 17, 6986. [Google Scholar] [CrossRef]
- Alonso, P.; Bertolín, S.; Segalàs, J.; Tubío-Fungueiriño, M.; Real, E.; Mar-Barrutia, L.; Fernández-Prieto, M.; Carvalho, S.; Carracedo, A.; Menchón, J.M. How is COVID-19 affecting patients with obsessive–compulsive disorder? A longitudinal study on the initial phase of the pandemic in a Spanish cohort. Eur. Psychiatry 2021, 64, e45. [Google Scholar] [CrossRef]
- Khosravani, V.; Aardema, F.; Ardestani, S.M.; Bastan, F.S. The impact of the coronavirus pandemic on specific symptom dimensions and severity in OCD: A comparison before and during COVID-19 in the context of stress responses. J. Obs.Compuls. Relat. Disord 2021, 29, 100626. [Google Scholar] [CrossRef]
- Zanjani, Z.; Jandaghian, M.; Alvani, S.R.; Ghorbani, V.; Joekar, S. COVID-19 Anxiety and Washing Obsessive-compulsive Symptoms: Stress Coping Styles as a Mediator. Curr. Psychiatry Res. Rev. 2023, 19, 79–88. [Google Scholar] [CrossRef]
- Taylor, S.; Landry, C.A.; Paluszek, M.M.; Fergus, T.A.; McKay, D.; Asmundson, G.J. COVID stress syndrome: Concept, structure, and correlates. Depress. Anxiety 2020, 37, 706–714. [Google Scholar] [CrossRef]
- Rosa-Alcázar, Á.; García-Hernández, M.D.; Parada-Navas, J.L.; Olivares-Olivares, P.J.; Martínez-Murillo, S.; Rosa-Alcázar, A.I. Coping strategies in obsessive-compulsive patients during Covid-19 lockdown. Int. J. Clin. Health Psychol. 2021, 21, 100223. [Google Scholar] [CrossRef]
- Wheaton, M.G.; Messner, G.R.; Marks, J.B. Intolerance of uncertainty as a factor linking obsessive-compulsive symptoms, health anxiety and concerns about the spread of the novel coronavirus (COVID-19) in the United States. J. Obs. Compuls. Relat. Disord. 2021, 28, 100605. [Google Scholar] [CrossRef]
- Nissen, J.B.; Højgaard, D.R.; Thomsen, P.H. The immediate effect of COVID-19 pandemic on children and adolescents with obsessive compulsive disorder. BMC Psychiatry 2020, 20, 511. [Google Scholar] [CrossRef] [PubMed]
- Seçer, İ.; Ulaş, S. An Investigation of the Effect of COVID-19 on OCD in Youth in the Context of Emotional Reactivity, Experiential Avoidance. Depression and Anxiety. Int. J. Ment. Health Addict. 2020, 19, 2306–2319. [Google Scholar] [CrossRef] [PubMed]
- Jassi, A.; Shahriyarmolki, K.; Taylor, T.; Peile, L.; Challacombe, F.; Clark, B.; Veale, D. OCD and COVID-19: A new frontier. Cogn. Behav. Therap. 2020, 13, e27. [Google Scholar] [CrossRef] [PubMed]
- Cunning, C.; Hodes, M. The COVID-19 pandemic and obsessive–compulsive disorder in young people: Systematic review. Clin. Child Psychol. Psychiatry 2022, 27, 18–34. [Google Scholar] [CrossRef]
- Storch, E.A.; Sheu, J.C.; Guzick, A.G.; Schneider, S.C.; Cepeda, S.L.; Rombado, B.R.; Gupta, R.; Hoch, C.T.; Goodman, W.K. Impact of the COVID-19 pandemic on exposure and response prevention outcomes in adults and youth with obsessive-compulsive disorder. Psychiatry Res. 2021, 295, 113597. [Google Scholar] [CrossRef]
- Liao, J.; Liu, L.; Fu, X.; Feng, Y.; Liu, W.; Yue, W.; Yan, J. The immediate and long-term impacts of the COVID-19 pandemic on patients with obsessive-compulsive disorder: A one-year follow-up study. Psychiatry Res. 2021, 306, 114268. [Google Scholar] [CrossRef]
- Rosa-Alcázar, Á.; Parada-Navas, J.L.; García-Hernández, M.D.; Martínez-Murillo, S.; Olivares-Olivares, P.J.; Rosa-Alcázar, A.I. Coping strategies, anxiety and depression in OCD and schizophrenia: Changes during COVID-19. Brain Sci. 2021, 11, 926. [Google Scholar] [CrossRef]
- Benatti, B.; Albert, U.; Maina, G.; Fiorillo, A.; Celebre, L.; Girone, N.; Fineberg, N.; Bramante, S.; Rigardetto, S.; Dell’Osso, B. What Happened to Patients With Obsessive Compulsive Disorder During the COVID-19 Pandemic? A Multicentre Report From Tertiary Clinics in Northern Italy. Front. Psychiatry 2020, 11, 720. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Goodman, W.K.; Price, L.H.; Rasmussen, S.A.; Mazure, C.; Fleischmann, R.L.; Hill, C.L.; Heninger, G.R.; Charney, D.S. The Yale-Brown obsessive compulsive scale: I. Development, use, and reliability. Arch. Gen. Psychiatry 1989, 46, 1006–1011. [Google Scholar] [CrossRef]
- Rosario-Campos, M.C.; Miguel, E.C.; Quatrano, S.; Chacon, P.; Ferrao, Y.; Findley, D.; Katsovich, L.; Scahill, L.; King, R.A.; Woody, S.R.; et al. The Dimensional Yale–Brown Obsessive–Compulsive Scale (DY-BOCS): An instrument for assessing obsessive–compulsive symptom dimensions. Mol. Psychiatry 2006, 11, 495–504. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The Hospital Anxiety and Depression Scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef]
- Lewis, K.J.; Lewis, C.; Roberts, A.; Richards, N.A.; Evison, C.; Pearce, H.A.; Lloyd, K.; Meudell, A.; Edwards, B.; Robinson, C.; et al. The effect of the COVID-19 pandemic on mental health in individuals with pre-existing mental illness. BJPsych Open 2022, 8, e59. [Google Scholar] [CrossRef]
- Adams, T.G.; Kelmendi, B.; Brake, C.A.; Gruner, P.; Badour, C.L.; Pittenger, C. The role of stress in the pathogenesis and maintenance of obsessive-compulsive disorder. Chronic Stress 2018, 2, 2470547018758043. [Google Scholar] [CrossRef]
- Fullana, M.A.; Tortella-Feliu, M.; Caseras, X.; Taberner, J.; Torrubia, R.; Mataix-Cols, D. Temporal stability of obsessive-compulsive symptom dimensions in an undergraduate sample: A prospective 2-year follow-up study. Behav. Modif. 2007, 31, 815–824. [Google Scholar] [CrossRef]

| Characteristics | OCD 2022 (n = 175) |
|---|---|
| Age (Mean ± SD) | 33.33 ± 9.42 |
| Sex n (%) | |
| Men | 99 (56.6) |
| Women | 76 (43.4) |
| Marital status n (%) | |
| Single | 114 (65.1) |
| Married | 49 (28.0) |
| Divorced | 12 (6.9) |
| Educational level n (%) | |
| Elementary | 9 (5.1) |
| Secondary education | 37 (21.1) |
| High school | 38 (21.7) |
| University student | 91 (52.1) |
| Whom did you live with? (%) | |
| Alone | 17 (9.7) |
| Friends/Partner/Flatmate | 85 (48.6) |
| Family | 73 (41.7) |
| T1 (April–May 2020) Mean ± SD | T2 April–May 2022 Mean ± SD | t | 95% I.C. Lower/Upper | |
|---|---|---|---|---|
| Total Y-BOCS | 20.16 ± 6.07 | 23.41 ± 7.13 | −18.17 (174); p < 0.001 | −3.59; −2.88 |
| Y-BOCS obsessions | 10.09 ± 3.06 | 11.77 ± 3.64 | −18.18 (174); p < 0.001 | −1.86; −1.50 |
| Y-BOCS compulsions | 10.07 ± 3.02 | 11.62 ± 3.53 | −16.46 (174); p < 0.001 | −1.74; −1.36 |
| N | T1 Mean ± SD | T2 Mean ± SD | F | η2 | |||
|---|---|---|---|---|---|---|---|
| Total Y-BOCS | Contamination Aggressive Sexual Hoarding Somatic Religious Miscellaneous | 42 39 12 4 33 18 27 | 22.07 ± 7.40 19.12 ± 5.19 18.16 ± 3.95 16.00 ± 0.20 21.84 ± 6.57 19.88 ± 5.75 18.33 ± 4.55 | 25.42 ± 8.24 22.33 ± 6.68 19.42 ± 4.69 17.00 ± 1.15 25.93 ± 7.17 23.05 ± 7.01 21.66 ± 5.44 | F (time) F (interaction) F (group) | 142.86; p < 0.001 2.956; p = 0.009 2.73; p = 0.015 | 0.46 0.096 0.089 |
| Contamination | Aggressive | Sexual | Hoarding | Somatic | Religious | Miscellaneous | ||
|---|---|---|---|---|---|---|---|---|
| T1 | Anxiety | 0.658 ** | 0.626 ** | 0.571 * | 0.098 | 0.488 * | 0.546 * | 0.384 * |
| Depression | 0.937 ** | 0.771 ** | 0.883 ** | 0.123 | 0.919 ** | 0.814 ** | 0.714 * | |
| T2 | Anxiety | 0.710 ** | 0.748 ** | 0.633 * | 0.125 | 0.642 ** | 0.689 * | 0.520 * |
| Depression | 0.896 ** | 0.810 ** | 0.887 ** | 0.133 | 0.872 ** | 0.855 ** | 0.669 ** |
| N | T1 Mean ± SD | T2 Mean ± SD | F | η2 | |||
|---|---|---|---|---|---|---|---|
| Anxiety | Contamination Aggressive Sexual Hoarding Somatic Religious Miscellaneous | 42 39 12 4 33 18 27 | 10.04 ± 4.72 11.43 ± 4.89 9.16 ± 2.72 12.50 ± 0.57 13.15 ± 3.78 12.00 ± 4.18 11.93 ± 4.67 | 12.40 ± 4.73 13.43 ± 4.89 11.16 ± 2.72 14.75 ± 0.50 15.15 ± 3.75 14.00 ± 4.16 13.03 ± 4.59 | F (time) F (interaction) F (group) | 8995.25; p < 0.001 9.12; p > 0.001 2.73; p = 0.084 | 0.998 0.246 0.063 |
| Depression | Contamination Aggressive Sexual Hoarding Somatic Religious Miscellaneous | 42 39 12 4 33 18 27 | 8.71 ± 5.11 7.21 ± 3.64 6.58 ± 2.57 6.50 ± 0.57 9.24 ± 4.34 7.61 ± 4.43 7.22 ± 4.19 | 10.71 ± 5.11 9.22 ± 3.69 8.58 ± 2.56 8.50 ± 0.55 11.24 ± 4.74 9.61 ± 4.34 9.22 ± 3.50 | F (time) F (interaction) F (group) | 193.00; p < 0.001 6.12; p = 0.045 1.40; p = 0.214 | 0.993 0.203 0.048 |
| T2 | Total | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Contamination | Aggressive | Sexual | Hoarding | Somatic | Religious | Miscella Neous | ||||
| T1 | Contamination | Frequency | 39 | 0 | 0 | 0 | 2 | 1 | 0 | 42 |
| % | 2.3 | 0 | 0 | 0 | 1.1 | 0.6 | 0 | 24.0 | ||
| Aggressive | Frequency | 8 | 24 | 0 | 0 | 6 | 1 | 0 | 39 | |
| % | 4.6 | 13.7 | 0 | 0 | 3.4 | 6 | 0 | 22.3 | ||
| Sexual | Frequency | 0 | 2 | 9 | 0 | 1 | 0 | 0 | 12 | |
| % | 0 | 1.1 | 5.1 | 0 | 0.6 | 0 | 0 | 6.9 | ||
| Hoarding | Frequency | 0 | 0 | 0 | 2 | 2 | 0 | 0 | 4 | |
| % | 0 | 0 | 0 | 1.1 | 1.1 | 0 | 0 | 2.3 | ||
| Somatic | Frequency | 7 | 3 | 0 | 0 | 22 | 1 | 0 | 33 | |
| % | 4.0 | 1.7 | 0 | 0 | 12.6 | 0.6 | 0 | 18.9 | ||
| Religious | Frequency | 2 | 1 | 1 | 0 | 2 | 12 | 0 | 18 | |
| % | 1.1 | 0.6 | 0.6 | 0 | 1.1 | 6.9 | 0 | 10.3 | ||
| Miscellaneous | Frequency | 3 | 2 | 0 | 0 | 4 | 0 | 18 | 27 | |
| % | 1.7 | 1.1 | 0 | 0 | 2.3 | 0 | 10.3 | 15.4 | ||
| Total | Frequency | 59 | 32 | 10 | 2 | 39 | 15 | 18 | 175 | |
| % | 33.7 | 18.3 | 5.7 | 1.1 | 22.3 | 8.6 | 10.3 | 100 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rosa-Alcázar, Á.; Parada-Navas, J.L.; García-Hernández, M.D.; Pozza, A.; Tondi, P.; Rosa-Alcázar, A.I. Severity and Changes in OCD Dimensions during COVID-19: A Two-Year Longitudinal Study. Brain Sci. 2023, 13, 1151. https://doi.org/10.3390/brainsci13081151
Rosa-Alcázar Á, Parada-Navas JL, García-Hernández MD, Pozza A, Tondi P, Rosa-Alcázar AI. Severity and Changes in OCD Dimensions during COVID-19: A Two-Year Longitudinal Study. Brain Sciences. 2023; 13(8):1151. https://doi.org/10.3390/brainsci13081151
Chicago/Turabian StyleRosa-Alcázar, Ángel, Jose Luis Parada-Navas, Maria Dolores García-Hernández, Andrea Pozza, Paolo Tondi, and Ana Isabel Rosa-Alcázar. 2023. "Severity and Changes in OCD Dimensions during COVID-19: A Two-Year Longitudinal Study" Brain Sciences 13, no. 8: 1151. https://doi.org/10.3390/brainsci13081151
APA StyleRosa-Alcázar, Á., Parada-Navas, J. L., García-Hernández, M. D., Pozza, A., Tondi, P., & Rosa-Alcázar, A. I. (2023). Severity and Changes in OCD Dimensions during COVID-19: A Two-Year Longitudinal Study. Brain Sciences, 13(8), 1151. https://doi.org/10.3390/brainsci13081151






